Synopsis
Neonatal neurobehavioral assessment has become a standardized component of clinical care provided to newborn infants, guiding neonatal clinical care and subsequent access to early interventions and services. Links between neonatal assessment and neurosensory and motor impairments in high-risk infants have been relatively well established. In contrast, the extent to which newborn neurobehavioral assessment might also facilitate the early identification of infants susceptible to social-emotional impairments in early childhood is less well documented. This review examines longitudinal links between the neonatal neurobehavioral assessment, temperament, and socio-emotional outcomes in early childhood.
Keywords: Neonate, assessment, neurobehavioral, temperament, socio-emotional impairment
INTRODUCTION
Neonatal neurobehavioral assessment has become a standardized and common component of clinical care provided to newborn infants.1 Early editions of neonatal neurobehavioral assessments date back to the 1900’s2 and primarily emphasized the evaluation of central nervous system (CNS) organization and maturation.3–6 More recent assessments include items that focus on newborn neurobehavioral development, relating the developing nervous system to functional behavior in the postnatal environment.2,7 Strength-based neurobehavioral measures highlight the importance of assessing infant capabilities according to the infant’s developmental milieu.2,4,8,9 Neonatal neurobehavioral assessments not only guide clinical decisions regarding care in the Neonatal Intensive Care Unit (NICU), but also help to determine which infants will need longer-term support via targeted therapeutic interventions and the early involvement of specialist developmental services following hospital discharge.4,5,8,10,11
To determine the clinical utility of neonatal screening measures, a growing body of evidence has begun to document the extent to which neonatal assessment predicts long-term cognitive and motor outcomes.12–14 However, less is known regarding the utility of neonatal assessments for the identification infants at risk of socio-emotional impairments. As such, the current review will provide an overview of empirical studies linking newborn neurobehavioral assessments to socio-emotional outcomes in early childhood. Given that existing reviews have already highlighted strong associations between newborn neurological assessments and later neurodevelopmental impairments,12,15 this review will focus on neurobehavioral assessments only.
Assessment of the Newborn
The initial mechanism by which newborns, defined as infants in the first 28 days of life, are identified as having disturbances in CNS and neurobehavioral development is through routine clinical assessment in neonatal care units.5 In addition to detailed physical and neurological exams, a number of standardized assessments are widely available to clinicians and researchers that provide a comprehensive evaluation of the newborn’s neurobehavioral capabilities. Newborn assessments typically have at least one of three primary objectives:
to identify high-risk infants with CNS and neurobehavioral disturbances in need of treatment and/or intervention,
to evaluate developmental progress in response to NICU interventions and family-centered therapies, and/or
to prognosticate longer-term neurodevelopmental outcomes.5,8,16
Due to the recent rise of family-centered approaches in neonatal care, an additional objective included in some assessments concerns the evaluation of the infant in the context of the parent-infant dyad to promote infant health and the caregiving relationship.14,17
Neonatal Neurobehavioral Assessments
Provided in Table 1 is a general description of established neonatal neurobehavioral assessments. Variation exists across the assessments in terms of the domains examined, test construction, and differences in administration approaches regarding infant observation and/or manipulation/handling.4,16 Most measures, however, have a dual emphasis on the assessment of CNS functions and the neurobehavioral profile.2,6 Systematic assessment of neonatal CNS maturity and organization involves the evaluation of primitive reflexes, spontaneous/elicited movements, and sensory behaviors.2,4,8 Reflexive and sensory behaviors undergo rapid sequential changes in the neonatal period,4,9 and as such, they are useful neurophysiological constructs to discriminate compromised CNS function in high-risk versus healthy neonates. In addition to CNS function, assessment of the newborn neurobehavioral profile involves the evaluation of three key capacities:
Table 1.
A General Description of Neonatal Neurobehavioral Assessments
| Test | General Description | Components | Age Range | Administration Time (minutes) | Scoring |
|---|---|---|---|---|---|
| The Assessment of Preterm Infants Behavior (APIB) | Observation of infant’s responses to handling & manipulation by the clinician, emphasis on newborn behavior during interaction with the environment | Autonomic movement, motor activity, state, self-regulation, attention, interaction | 28 weeks postmenstru al age to 1 month | 30 – 60 | Unstandardized; 6 main system scores derived from 81 scores; 3 status scores available for 4 of the systems: Baseline, Response, Post-Intervention; percentile used for clinical cut-offs |
| Neurobehavioral Assessment of the Preterm Infant (NAPI) | Observation of preterm infant’s responses to handling & manipulation by the clinician, assessing the functional maturity of preterm infants. Limited to medically stable preterm infants | Autonomic movement, reflexes, motor vigor, state attention, irritability | 32-weeks postmenstru al age to term age | 30 | Standardized; 7 clusters assessed using 41 items; item scores, observational state ratings & summary ratings (least mature’ to ‘most mature’) available, centiles used for age-norms |
| Neonatal Behavioral Assessment Scale (NBAS) | Observation of infant’ responses to handling & manipulation by the clinician to identify functional impairment & predict outcomes | Autonomic movement, reflexes, motor activity, state, attention/interaction capabilities | 36 weeks postmenstru al age to 6 weeks | None specified, usually around 30 | Unstandardized; 6 domains; 46 items & 7 supplementary items |
| Newborn Behavioral Observations system (NBO) | Nursing intervention, structured observations assessing infant competencies/vulnerabilities in the context of parent-infant dyad after care-giving sessions, encourages parent education & active caregiving | Motor tone, sensory capacities (visual & auditory), activity, habituation, self-regulation (crying & consolability), response to stress, interaction capabilities | Term to 3 months | 20 – 30 | Unstandardized; 18 items; additional post-intervention interview used to assess caregiver perceptions of the NBO as a learning tool |
| NICU Network Neurobehavioral Scale (NNNS) | Observation of infant’s responses to handling & manipulation by the clinician, identifies functional impairments in preterm & at-risk term infants | Tone, reflexes, behavior, stress/abstinence signs | 30 weeks postmenstru al age to 4 months | <30 | Standardized; 45 items administered in 12 packages; item scores range 1–11; items can also be clustered into 13 domain summary scores; 7 stress packages available; stress items scored ‘yes’/’no’ |
active/passive motor activity,
state-organization/regulation of arousal, and
attention/interactive abilities.
The assessment of newborn neurobehavior has proven useful for the prediction of general neurodevelopmental outcomes by age 2 years, with some research suggesting potentially to a greater extent than CNS abnormalities identified by cranial ultrasound.5
Recently developed and commonly used neonatal neurobehavioral screening measures include The Assessment of Preterm Infants’ Behavior (APIB),18 Neurobehavioral Assessment of the Preterm Infant (NAPI),19 Neonatal Behavioral Assessment Scale (NBAS),20 and the NICU Network Neurobehavioral Scale (NNNS).1 Regarding test administration, the NBAS and NNNS are similar in terms of items being administered in clusters or packages, but differ in that they were created to evaluate behavior in healthy versus high-risk infants,12 respectively. A relative strength of the NNNS is its flexible administration that takes the arousal state of the infant into account.8 Also from an infant-centered perspective, the NBAS focuses on behavioral strengths and views the infant as an active participant who is capable of communicating through behavior.2,12 Of the assessments, the NNNS is considered the most comprehensive as it integrates principals and components from the NBAS, NAPI, and APIB.12 Furthermore, a recent review found that the NNNS and APIB have strong psychometric properties that make them ideal for research purposes, whereas the NAPI demonstrates stronger clinical ultility.16
The APIB, ENNAS, NAPI, NBAS, and NNNS provide an objective quantification of infant behavior observed during the clinician-infant interaction. As family-centered developmental approaches have become integrated in NICUs, the Newborn Behavioral Observations system (NBO)17 and Newborn Individualized Developmental Care and Assessment Program (NIDCAP)21 were developed to evaluate the infant in the context of the caregiver-infant relationship. The NBO is a strengths-based assessment that yields an individualized description of an infant’s hierarchically-organized neurobehavioral capabilites.22 Throughout the NBO, the clinician involves the parent(s) in baby-led assessments, developing handling and caregiving techniques that parent(s) can use in the home environment to sensitively respond to infant behavioral cues. Likewise, the NIDCAP is a family-centered systems-based protocol that focuses on newborn autonomic, motor, state-organization, attention/interaction, and self-regulation systems, observed before and after caregiving.21 The unique aspect of the NIDCAP is to provide neonatal assessment/observation in a way that is developmentally-sensitive and individualized, which includes adapting the postnatal environment to accommodate the infant’s threshold for sensory input and/or neurobehavioral regulatory capacities.14
The Neurobiological Framework of Newborn Neurobehavior
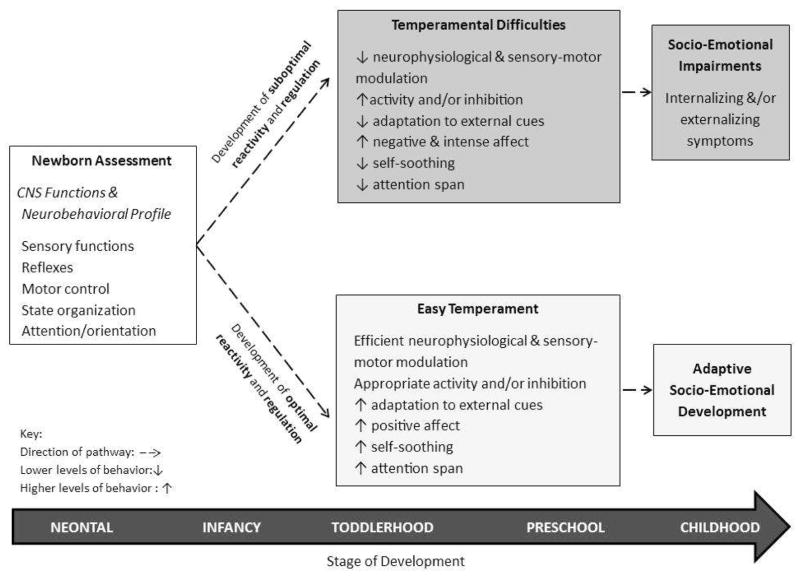
The APIB, NBAS, and NIDCAP were developed on the basis of the Synactive framework14 which proposes that optimal biobehavioral development depends on the integration of mature of CNS and neurobehavioral systems. Specifically, the Synactive Theory of Neonatal Behavioral Organization23 conceptualizes infant development as the progressive organization and integration of five systems/domains including: physiology, motor control, state-organization/arousal, attention/interaction capabilities, and self-regulation.22 Integrated and synchronized systems help a mature infant to manage sensory input and regulate behavior.9 As illustrated in Figure 1, neonatal screening focuses on the developing CNS (i.e., sensory functions and reflexes) and the integrated neurobehavioral profile (i.e., motor control/regulation, state-organization, attention/orientation capabilities), impairments in which relate to low sensitivity thresholds/high reactivity and poor regulation in the infant.9,24 Given the interrelated nature of newborn neurobehavioral systems, and that neonatal assessments demonstrate conceptual overlap with measures of temperament,25 neonatal screening measures may capture some of the early neurobehavioral and physiological alterations underlying regulation and reactivity in infancy that, in turn, relate to socio-emotional development in childhood.
Figure 1.
A conceptual framework linking newborn assessment of CNS functions and the neurobehavioral profile to temperamental difficulties and socio-emotional impairments in childhood.
Neonatal Assessment and Infant Temperament
Temperament is the biologically-based construct that, with environmental experience, underpins and shapes early personality traits and risks for socio-emotional impairments.26,27 Rudimentary aspects of temperament are observable within the first year of life. From 1 to 12 months old, one of the infant’s primary developmental tasks is to regulate behavior using basic neuro-physiological modulatory mechanisms, such as disengaging from adverse stimuli and engaging in self-soothing behavior, to modulate high levels of arousal and/or distress.9,22,28 From 9 to 12 months old, sensory-motor regulation steadily improves as motor skills mature, facilitating simple goal-directed behavior as well as the redirection of behavior when needed.28 As focused attention and shifting attention skills develop in parallel with sensory-motor regulation skills, infants are increasingly able to regulate reactivity and emotional distress.28,29
Temperament in infancy and childhood has been broadly categorized into “easy” and “difficult” dimensions defined by positive/negative affect, intensity of reactions, approach and withdrawal behaviors, and the predictability of behavior across situations.30,31 Conceptually, models of temperament show considerable overlap with constructs included in neonatal screening measures, both often assessing state-organization/arousal, self-regulation, and attention/orientation. Concurrent relationships between neonatal assessments and maternal-report of infant temperament have been reported up to 1 month of age. In 100 mother-infant dyads, principal component analysis (PCA) was performed using the NNNS, the Early Infant Temperament Questionnaire (EITQ) and the Infant Sensory Profile (ISP).25 Results of the PCA yielded a 3 factor model comprised of Sensory-Affective Reactivity, Engagement, and State Regulation-Motor Competence. Specific findings showed that the NNNS Regulation and Stress scales loaded onto all three factors, and NNNS Arousal loaded onto both the Sensory-Affective Reactivity and State Regulation-Motor Competence factors. In addition, EITQ Distractibility, Activity Level, Threshold, Persistence; and ISP Low Threshold also mapped onto Sensory-Affective Reactivity and Engagement constructs. Although correlations were strongest between parent-reports of infant temperament and sensory processing, the PCA results suggested a common latent structure between the NNNS, temperament, and sensory processing in early infancy.
In addition to concurrent relationships in the first month of life, neonatal screening measures also show longitudinal associations with temperament in later infancy. In a study by Tirosh and colleuges,32 a small group of healthy neonates (n= 40) was assessed with the NBAS 48–72 hours after birth. NBAS clusters of interest included Physiological Regulation, Motor and State Control, and Orientation and Habituation to Stimuli. The state-regulation behaviors, comprised of Cuddliness and Consolability items, and the Defense subscale from the NBAS Motor cluster were strong predictors of temperament at age 4 months, explaining 57% of variance in total Infant Characteristics Questionnaire scores. As well as being an antecedent of infant temperament, neonatal neurobehavior has been found to moderate the relationship between prenatal exposure to maternal glucocorticoids and emotion regulation at age 6 months. Bolten and colleagues33 used the NNNS to assess neonatal reactivity to stimulation at 10–14 days corrected age, and found that high levels of reactivity moderated the association between heightened maternal HPA axis activity during pregnancy and fewer infant self-soothing activities observed at age 6 months. When taken together, these studies suggest that neonatal neurobehavior relates to temperament within the first year of life, and that emerging aspects of temperament may be observable within the neonatal period.
Extending findings from late infancy, neonatal screening measures have also been linked to temperament in early childhood. For example, Costa and Figueiredo34 assessed 94 infants (80% normal and born at term) with the NBAS at 8 weeks old. Measures of social withdrawal and neuroendocrine reactivity to inoculation were also collected between 8 and 12 weeks old. Cluster analysis was used on the neurobehavioral, social, and neuroendocrine reactivity measures, which produced three psychophysiological groups defined as Withdrawn, Extroverted and Underaroused. Costa and Figueiredo34 then compared these three groups across the maternal-report Infant Behavior Questionnaire (IBQ) at 1 year follow-up. Findings showed that the Withdrawn group had significantly lower Activity Level ratings on the IBQ than the Extroverted group, and the Underaroused group had lower Perceptual Sensitivity ratings on the IBQ compared to the Withdrawn group. Findings highlight that maternal perceptions of infant temperament varied as a function of neonatal psychophysiological profile, suggesting that the NBAS may capture some of the early neurobehavioral and physiological alterations related to differences in temperament.
Also using the NBAS, Canals and colleagues35 examined prospective associations between the NBAS administered at 3 and 30 days old in a sample of healthy infants (n=72), and temperament outcomes to age 6 years. Findings showed significant correlations between the NBAS and parent-ratings on the Infant Behavior Record at ages 4 and 12 months and the Dimensions of Temperament Survey-Revised at age 6 years old, though some correlations were modest. Interestingly, NBAS Autonomic Nervous System (ANS) Stability predicted Affect at age 4 months and Attention at age 12 months, while NBAS State Regulation predicted Affect at 4 months and General Activity at age 6 years. Furthermore, NBAS Endurance scores related to General Activity and Persistence/attention at age 6 years. When taken together, the findings of Costa and Figueiredo34 and Canals and colleagues35 indicate that the NBAS demonstrates relationships with temperament up to age 6 years. In particular, ANS stability and state-regulation may be relatively stable markers of temperament, highlighting developmental continuity within these constructs.
Neonatal Assessment and Socio-Emotional Impairments in Childhood
As outlined above, follow-up studies have reported associations between neonatal neurobehavioral development and temperament in childhood.35,36 Temperament is, in turn, a good marker of the regulatory and affective problems that underlie socio-emotional problems in childhood.27,37–40 Thus, neonatal neurobehavioral screening may help identify infants at-risk of socio-emotional impairments in childhood.39,41 Socio-emotional impairments, including internalizing and externalizing problems, are commonly assessed using dimensional screening tools such as the Child Behavior Checklist (CBCL) and the Strengths and Difficulties Questionnaire (SDQ).42 For example, a large cohort of infants (n=1248) was assessed with the NNNS at 1 month of age as part of a longitudinal study by Liu and colleagues.43 Results of latent class analysis indicated that 5.8% of study infants were characterized by an extremely negative NNNS profile. These infants obtained the poorest NNNS scores for Attention with Handling, Self-Regulation, Hypotonicity, Non-Optimal and Asymmetric Reflexes, Quality of Movement, and Stress Abstinence Signs. Infants in the extremely negative NNNS profile group had significantly higher odds ratios for Externalizing (2.05), Internalizing (2.72), and Total Problems (2.37) on the CBCL relative to the other NNNS profile groups at age 3 years, after adjusting for gestational age and socio-economic status. In a sample of cocaine exposed infants (n=360), structural equation modelling similarly showed sequential relationships between the NNNS administered at 1 month of age and temperament at age 4 months, which was in turn, predictive of CBCL Externalizing, Internalizing, and Total Problem scores at age 3 years.39
Like the NNNS, the NBAS demonstrates significant associations with the CBCL44,45 and the SDQ46 at follow-up. Canals, Esparo and Fernandez-Ballart44 examined the extent to which clusters of the NBAS, administered at ages 3 days and 4 weeks old in healthy infants (n=80), predicted CBCL Internalizing and Externalizing Problem scores at age 6 years. Findings showed that lower Orientation and higher Motor and Habituation cluster scores on day 3 of life predicted externalizing outcomes, whereas lower Habituation cluster scores at age 4 weeks predicted internalizing outcomes. Results were adjusted for mother’s employment status and mental health and infant birthweight and sex. Another study found that the NBAS administered at 40 and 44 weeks postmenstrual age was able to correctly identify around 75% and 95% of clinical versus normal ratings on the Total Difficulties scale of the SDQ at age 7–8 years, respectively.46
In contrast, a more recent longitudinal study45 of preterm infants born 25–35 weeks gestational age without perinatal complications or high-grade brain injury, reported that a NBAS composite score comprised of the State and Regulation of State clusters did not significantly relate to CBCL Total Problem scores at age 10 years. Feldman45 instead found that the NBAS composite score was correlated with children’s levels of cognitive and emotional empathy, assessed via direct observation and self-ratings of emotional responses. Differences in methodological approaches might account for the discrepancy in results. While Canals, Esparo and Fernandez-Ballart44 examined individual associations between each of the NBAS clusters and scales of the CBCL, Feldman45 examined a NBAS composite cluster score in relation to Total Problems on the CBCL. Thus, the extent to which the NBAS predicts internalizing, externalizing or combined adjustment problems in childhood remains unclear.
SUMMARY/DISCUSSION
When taken together, findings of existing studies suggest that neonatal neurobehavioral assessments may be useful for early identification of infants at-risk for socio-emotional impairments in early childhood. Consistent links were found between less optimal performance on neonatal screening measures and poorer temperament outcomes.32,34,35,39 In addition to temperamental difficulties increasing risks of socio-emotional problems,27,28,30,39,40 there was evidence for direct associations between newborn NBAS and NNNS assessments and externalizing46 and internalizing43,44 outcomes in childhood. Although one study45 did not find a longitudinal relationship with combined externalizing and internalizing outcomes, they did report an association with emotional empathy which is a component of socio-emotional development.47 Therefore, while newborn assessments have traditionally been developed from the disciplines of medicine, behavioral pediatrics and occupational therapy,25 the inclusion of mental health perspectives is also needed to address the increased risk of socio-emotional problems among highly reactive and dysregulated infants.
Conceptually, the findings of the reviewed studies support existing models of temperament and developmental continuity. A number of study findings were consistent with Rothbart’s model of temperament29 which highlights reactivity and regulation as the central tenants underlying individual differences in activity/impulsivity, effortful-control, and attention. For example, neonates with lower levels of ANS stability and state-regulation were more likely to be perceived as fussy, poorly regulated and/or highly reactive toddlers, and in turn, be rated more highly on measures of socio-emotional problems in childhood.32,35,45 Similarly, neonates who had poorer state-regulation and motor activity, were viewed as unpredictable and highly active in early childhood and subsequently rated at risk of externalizing problems.44,46 The apparent developmental continuity between neonatal behavior, temperament, and socio-emotional problems indicates that aspects of neonatal neurobehavioral and socio-emotional development may be longitudinally expressed components of the same phenotype, and thus stable, within early childhood.48,26
In addition to developmental continuity, patterns of heterotypic continuity were found in some studies.32,35,44 These studies found that a specific component of neonatal neurobehavior was related to a range of socio-emotional outcomes in early childhood. For example, one study found NBAS Autonomic Nervous System Stability predicted both affective and attention outcomes within the first year of life35 and another study found that NBAS Habituation scores predicted internalizing and externalizing problems at age 6 years.44 Heterotypic continuity between early neonatal behavior and various socio-emotional outcomes occurs when an innate characteristic (e.g., the capacity for regulation) underlies a set of conceptually related outcomes (e.g., emotional regulation, inhibitory control).35,48 As such, specific aspects of neonatal behavior may be useful markers for a diverse range of socio-emotional problems in childhood.
Although neonatal screening demonstrates developmental continuity with socio-emotional outcomes, a number of issues remain. First, many of the reported associations between neonatal and socio-emotional development were established using correlation35,45 or linear regression methods.32,39 While this provides insight on the nature of relations between neonatal and socio-emotional measures, it is difficult to determine the extent of agreement between these measures in terms of caseness. To the knowledge of the authors, just two studies reported classification agreement between neonatal assessment and socio-emotional measures using estimated coefficients from logistic regression.44,46 Specificity/sensitivity approaches appear to be more common in studies evaluating the validity of neonatal assessment for later motor and cognitive impairments.4,13,15 As such, there may be some benefit in applying sensitivity/specificity approaches to similarly evaluate the prognostic accuracy of neonatal screening for socio-emotional outcomes.
Second, methodological differences between studies may explain mixed findings. Regarding the NBAS and NNNS, some studies examined the utility of cluster scores,32,35,43,44 composite or latent summary scores,39,45 or study-specific total item summary scores.34,46 Differences were also noted in terms of the use of individual CBCL Externalizing and Internalizing Problem scales43,44 or the overall Total Problem scales45 as outcome measures. Additional research is needed to elucidate specific relationships between neonatal neurobehavioral and socio-emotional sub-scales in order to determine if neonatal makers are more sensitive to particular socio-emotional domains. Future research should also consider evaluating the utility of neonatal assessments besides the NBAS and NNNS, and link findings beyond CBCL and SDQ symptom screening measures to clinical evaluations of child psychopathology.
Clinical Applications
Despite methodological differences across studies, neonatal neurobehavioral measures appear to capture emerging indicators of reactivity and regulation problems that lead to socio-emotional difficulties, as early as the newborn period. Based upon neonatal screening results, at-risk infants and their families may benefit from embedded child mental health surveillance and intervention provided as part of long-term follow-up after Nursery discharge. Strategies to monitor and support early socio-emotional outcomes among at-risk infants include the promotion of infant capabilities within the context of the mother-child dyad.
Family-centered neonatal interventions, such as the NBO and NIDCAP, help parents transition to the caregiving role and promote parenting efficacy. Short-term preliminary findings show that the NBO supports the transition to motherhood,50 reduces post-partum depression symptoms,51 and promotes quality caregiving among mothers of high-risk infants.52 Importantly, these interventions help parents recognize and interpret infant behavioral cues and respond to the infant’s needs in a timely and sensitive manner.21,22 Interventions that enhance caregiving-sensitivity and attachment-based parenting have been shown to promote behavioral and cognitive resiliency in at-risk infants and children.53,54 While a recent meta-analysis did not find any evidence to suggest that the NIDCAP protocol improves long-term neurosensory, motor and cognitive outcomes in preterm infants,14 socio-emotional outcomes were not assessed. Thus, NIDCAP may still improve the goodness-of-fit in parent-infant dyads, and in turn, support the development of infant temperament and emotion regulation.24,55 Of note, a systematic Cochrane review evaluating the NBO and NBAS as interventions that improve a wide range of caregiver and infant outcomes is currently underway.56
Conclusions
Neonatal neurobehavioral screening measures assess CNS functions in conjunction with the neurobehavioral profile of the newborn. The vast majority of newborn assessments evaluate sensory behavior, reflexes, motor control, state-organization, and attention/interactive capabilities. In high-risk neonates, neonatal neurobehavioral assessments demonstrate clinical utility for the identification of neurosensory, cognitive and motor impairments in childhood. When used in the same fashion, neonatal screening measures also appear to capture some of the early physiological and neurobehavioral markers related to longer-term differences in temperament and socio-emotional development, due to the 1) conceptual overlap between neonatal and socio-emotional outcome measures, and 2) developmental continuity in reactivity and regulatory behaviors. Therefore, assessment of the newborn’s neurobehavior can inform preventative interventions that target high-risk mother-infant dyads to better support infant socio-emotional development and alter trajectories to prevent childhood psychiatric disorders.
Key Points.
Neonatal neurobehavioral assessment is one key mechanism by which neonates with central nervous system and neurobehavioral disturbances are identified.
Neonates with highly reactive and dysregulated neurobehavioral profiles are at greater risk of temperamental difficulties by late infancy.
The NNNS and NBAS show significant associations with externalizing, internalizing, and emotion regulation problems in early-to-middle childhood, suggesting that neonatal screening measures capture early physiological and neurobehavioral markers related to longer-term differences in early mental health.
Psychiatric services should be embedded in wrap-around longitudinal care for at-risk newborns to support socio-emotional development in the context of the caregiver-infant relationship.
Footnotes
Disclosure statement: The authors have no commercial or financial conflicts of interest. Dr. Smyser is funded by the National Institutes of Health K02 NS089852, UL1 TR000448, U54 HD087011; Cerebral Palsy International Research Foundation; and The Dana Foundation. Dr. Rogers is funded by the National Institutes of Health NICHD K23 MH105179 and KL2 TR000450.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Rachel E. Lean, Department of Psychiatry, Washington University School of Medicine, 660 South Euclid Avenue, Campus Box 8504, St. Louis, MO 63110, USA. Phone: 314-362-5523.
Chris D. Smyser, Departments of Neurology, Radiology and Pediatrics, Washington University School of Medicine, 660 South Euclid Avenue, Campus Box 8111, St. Louis, MO 63110, USA. Phone: 314-454-6120.
Cynthia Rogers, Departments of Psychiatry and Pediatrics, Washington University School of Medicine, 660 South Euclid Avenue, Campus Box 8504, St. Louis, MO 63110, USA. Phone: 314-286-0540.
References
- 1.Lester BM, Tronick E. Behavioral assessment scales: The NICU Network Neurobehavioral Scale, the Neonatal Behavioral Assessment Scale, and the Assessment of the Preterm Infant’s Behavior. In: Singer LT, Zeskind PS, editors. Biobehavioral Assessment of the Infant. Vol. 2001. New York, NY: Guilford Press; 2001. pp. 363–380. [Google Scholar]
- 2.Brown N, Spittle A. Neurobehavioral Evaluation in the Preterm and Term Infant. Current Pediatric Reviews. 2014;10:65–72. doi: 10.2174/157339631001140408121310. [DOI] [PubMed] [Google Scholar]
- 3.Morgan AM, Koch V, Lee V, Aldag J. Neonatal Neurobehavioral Examination. Phys Ther. 1988;68:1352–1358. doi: 10.1093/ptj/68.9.1352. [DOI] [PubMed] [Google Scholar]
- 4.El-Dib M, Massaro AN, Glass P, Aly H. Neurodevelopmental Assessment of The Newborn: An opportunity for prediction of outcome. Brain Dev. 2011;33:95–105. doi: 10.1016/j.braindev.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Gardner JM, et al. Arousal, Attention, and Neurobehavioral Assessment in the Neonatal Period: Implications for Intervention and Policy. J Policy Pract Intellect Disabil. 2006;3:22–32. [Google Scholar]
- 6.Majnemer A, Mazer B. Neurologic Evaluation of The Newborn Infant: Definition and psychometric properties. Dev Med Child Neurol. 1998;40:708–715. doi: 10.1111/j.1469-8749.1998.tb12332.x. [DOI] [PubMed] [Google Scholar]
- 7.Hammock EA, Levitt P. The Discipline of Neurobehavioral Development: The emerging interface of processes that build circuits and skills. Hum Dev. 2006;49:294–309. [Google Scholar]
- 8.Majnemer A, Snider L. A Comparison of Developmental Assessments of The Newborn and Young Infant. Ment Retard Dev Disabil Res Rev. 2005;11:68–73. doi: 10.1002/mrdd.20052. [DOI] [PubMed] [Google Scholar]
- 9.Vandenberg KA. Individualized Developmental Care for High Risk Newborns in The NICU: A practice guideline. Early Hum Dev. 2007;83:433–442. doi: 10.1016/j.earlhumdev.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Berenbaum SA. Neuropsychological Follow-Up in Neonatal Screening: Issues, methods and findings. Acta Paediatr Suppl. 1999;88:83–87. doi: 10.1111/j.1651-2227.1999.tb01167.x. [DOI] [PubMed] [Google Scholar]
- 11.Calciolari G, Montirosso R. Neonatal Neurobehavioral Assessment in Healthy and At-Risk Infants. Early Hum Dev. 2013;89:S58–S59. [Google Scholar]
- 12.El-Dib M, Massaro AN, Glass P, Aly H. Neurobehavioral Assessment as a Predictor of Neurodevelopmental Outcome in Preterm Infants. J Perinatol. 2012;32:299–303. doi: 10.1038/jp.2011.100. [DOI] [PubMed] [Google Scholar]
- 13.Harijan P, Beer C, Glazebrook C, et al. Predicting Developmental Outcomes in Very Preterm Infants: Validity of a neonatal neurobehavioral assessment. Acta Paediatr. 2012;101:e275–e281. doi: 10.1111/j.1651-2227.2012.02663.x. [DOI] [PubMed] [Google Scholar]
- 14.Ohlsson A, Jacobs SE. NIDCAP: A Systematic Review and Meta-analyses of Randomized Controlled Trials. PEDIATRICS. 2013;131:e881–e893. doi: 10.1542/peds.2012-2121. [DOI] [PubMed] [Google Scholar]
- 15.Craciunoiu O, Holsti L. A Systematic Review of the Predictive Validity of Neurobehavioral Assessments during the Preterm Period. Phys Occup Ther Pediatr. 2016;00:1–16. doi: 10.1080/01942638.2016.1185501. [DOI] [PubMed] [Google Scholar]
- 16.Noble Y, Boyd R. Neonatal Assessments for the Preterm Infant up to 4 Months Corrected Age: A systematic review. Dev Med Child Neurol. 2012;54:129–139. doi: 10.1111/j.1469-8749.2010.03903.x. [DOI] [PubMed] [Google Scholar]
- 17.Nugent KJ, Keefer CH, Minear S, Johnson LC, Blanchard Y. Understanding Newborn Behavior and Early Relationships: The Newborn Behavioral Observations (NBO) System Handbook. Baltimore, MD: Brookes; 2007. [Google Scholar]
- 18.Als H, Butler S, Kosta S, McAnulty G. The Assessment of Preterm Infants’ Behavior (APIB): Furthering the understanding and measurement of neurodevelopmental competence in preterm and full-term infants. Ment Retard Dev Disabil Res Rev. 2005;11:94–102. doi: 10.1002/mrdd.20053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Korner AF, Thom VA. Neurobehavioral Assessment of the Preterm Infant (NAPI) San Antonio, TX: The Psychological Corporation; 1990. [Google Scholar]
- 20.Brazelton TB, Nugent JK. Neonatal Behavioral Assessment Scale. Cambridge, MA: Cambridge University Press; 1995. [Google Scholar]
- 21.Westrup B. Newborn Individualized Developmental Care and Assessment Program (NIDCAP): Family-centered developmentally supportive care. Early Hum Dev. 2007;83:443–449. doi: 10.1016/j.earlhumdev.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Nugent KJ. The Newborn Behavioural Observation (NBO) System as a Form of Intervention. Zero Three. 2015;36:2–10. [Google Scholar]
- 23.Als H. Toward a Synactive Theory of Development: Promise for the assessment and support of infant individuality. Infant Ment Health. 1982;3:229–243. [Google Scholar]
- 24.Keenan K. Emotion Dysregulation as a Risk Factor for Child Psychopathology. Clin Psychol Sci Pract. 2000;7:418–434. [Google Scholar]
- 25.DeSantis A, Harkins D, Tronick E, Kaplan E, Beeghly M. Exploring an Integrative Model of Infant Behavior: What is the relationship among temperament, sensory processing, and neurobehavioral measures? Infant Behav Dev. 2011;34:280–292. doi: 10.1016/j.infbeh.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bornstein MH, et al. Infant Temperament: Stability by age, gender, birth order, term status, and socioeconomic status. Child Dev. 2015;86:844–863. doi: 10.1111/cdev.12367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Derauf C, et al. Infant Temperament and High Risk Environment Relate to Behavior Problems and Language in Toddlers. J Dev Behav Pediatr. 2011;32:125–135. doi: 10.1097/DBP.0b013e31820839d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berger A, Kofman O, Livneh U, Henik A. Multidisciplinary Perspectives on Attention and the Development of Self-Regulation. Prog Neurobiol. 2007;82:256–286. doi: 10.1016/j.pneurobio.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 29.Rothbart MK, Posner MI, Kieras J. Temperament, Attention, and the Development of Self- Regulation. In: McCartney K, Phillips D, editors. Handbook of Early Childhood Development. Malden: 2006. pp. 338–357. [Google Scholar]
- 30.Wasserman RC, DiBlasio CM, Bond LA, Young PC, Colletti RB. Infant Temperament and School Age Behavior: 6-year longitudinal study in a pediatric practice. Pediatrics. 1990;85:801–807. [PubMed] [Google Scholar]
- 31.Rothbart MK, Chew KH, Gartstein MA. Assessment of Temperament in Early Development. In: Singer LT, Zeskind PS, editors. Biobehavioural Assessment of the Infant. New York, NY: Guilford Press; 2001. pp. 190–108. [Google Scholar]
- 32.Tirosh E, Harel J, Abadi J, Berger A, Cohen A. Relationship between Neonatal Behavior and Subsequent Temperament. Acta Paediatr. 1992;81:829–831. doi: 10.1111/j.1651-2227.1992.tb12112.x. [DOI] [PubMed] [Google Scholar]
- 33.Bolten M, Nast I, Skrundz M, Stadler C, Hellhammer D, Meinlschmidt G. Prenatal Programming of Emotion Regulation: Neonatal reactivity as a differential susceptibility factor moderating the outcome of prenatal cortisol levels. J Psychosom Res. 2013;75:351–357. doi: 10.1016/j.jpsychores.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 34.Costa R, Figueiredo B. Infant’s Psychophysiological Profile and Temperament at 3 and 12 Months. Infant Behav Dev. 2011;34:270–279. doi: 10.1016/j.infbeh.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 35.Canals J, Hernández-Martínez C, Fernández-Ballart JD. Relationships between Early Behavioural Characteristics and Temperament at 6 Years. Infant Behav Dev. 2011;34:152–160. doi: 10.1016/j.infbeh.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 36.Rueda MR, Rothbart MK. The Influence of Temperament on the Development of Coping: The role of maturation and experience. New Dir Child Adolesc Dev. 2009;124:19–31. doi: 10.1002/cd.240. [DOI] [PubMed] [Google Scholar]
- 37.Sentse M, Veenstra R, Lindenberg S, Verhulst FC, Ormel J. Buffers and Risks in Temperament and Family for Early Adolescent Dsychopathology: Generic, conditional, or domain-specific effects? The trails study. Dev Psychol. 2009;45:419–430. doi: 10.1037/a0014072. [DOI] [PubMed] [Google Scholar]
- 38.Zentner MR. Temperament, Psychological Development and Psychopathology. Correlations, explanatory models and forms of intervention. Z Klin Psychol Psychopathol Psychother. 1993;41:43–68. [PubMed] [Google Scholar]
- 39.Lester BM, Bagner DM, Liu J, et al. Infant Neurobehavioral Dysregulation Related to Behavior Problems in Children with Prenatal Substance Exposure. Pediatrics. 2009;124:1355–1362. doi: 10.1542/peds.2008-2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eisenberg N, Cumberland A, Spinrad T, et al. The Relations of Regulation and Emotionality to Children’s Externalizing and Internalizing Problem Behavior. Child Dev. 2001;72:1112–1134. doi: 10.1111/1467-8624.00337. [DOI] [PubMed] [Google Scholar]
- 41.Eiden RD, Coles CD, Schuetze P, Colder CR. Externalizing Behavior Problems Among Polydrug Cocaine-Exposed Children: Indirect pathways via maternal harshness and self-regulation in early childhood. Psychol Addict Behav. 2014;28:139–153. doi: 10.1037/a0032632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warnick EM, Bracken MB, Kasl S. Screening Efficiency of the Child Behavior Checklist and Strengths and Difficulties Questionnaire: A systematic review. Child & Adolescent Mental Health. 2008;13:140–147. doi: 10.1111/j.1475-3588.2007.00461.x. [DOI] [PubMed] [Google Scholar]
- 43.Liu J, Bann C, Lester B, et al. Neonatal Neurobehavior Predicts Medical and Behavioral Outcome. Pediatrics. 2010;125:e90–e98. doi: 10.1542/peds.2009-0204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Canals J, Esparó G, Fernández-Ballart JD. Neonatal Behaviour Characteristics and Psychological Problems at 6 Years. Acta Pædiatrica. 2006;95:1412–1417. doi: 10.1080/08035250600760790. [DOI] [PubMed] [Google Scholar]
- 45.Feldman R. Mutual Influences Between Child Emotion Regulation and Parent–Child Reciprocity Support Development Across the First 10 Years of Life: Implications for developmental psychopathology. Dev Psychopathol. 2015;27:1007–1023. doi: 10.1017/S0954579415000656. [DOI] [PubMed] [Google Scholar]
- 46.Ohgi S, Takahashi T, Nugent JK, Arisawa K, Akiyama T. Neonatal Behavioral Characteristics and Later Behavioral Problems. Clin Pediatr. 2003;42:679–686. doi: 10.1177/000992280304200803. [DOI] [PubMed] [Google Scholar]
- 47.Thompson RA. Empathy and emotional understanding: The early development of empathy. In: Eisenberg N, Strayer J, editors. Empathy and It’s Development. New York, NY: Cambridge University Press; 1987. pp. 119–145. [Google Scholar]
- 48.Caspi A, Roberts BW. Personality Development Across the Life Course: The argument for change and continuity. Psychol Inq. 2001;12:49–66. [Google Scholar]
- 49.Cooper LG, Gooding JS, Gallagher J, Sternesky L, Ledsky R, Berns SD. Impact of Family-Centered Care Initiative on NICU Care, Staff, and Families. J Perinatol. 2007;27:S32–S37. doi: 10.1038/sj.jp.7211840. [DOI] [PubMed] [Google Scholar]
- 50.Cheetham NB, Hanssen TA. The Neonatal Behavioral Observation System: A tool to enhance the transition to motherhood. Nord J Nurs Res. 2014;34:48–52. [Google Scholar]
- 51.Nugent JK, Bartlett JD, Valim C. Effects of an Infant-Focused Relationship-Based Hospital and Home Visiting Intervention on Reducing Symptoms of Postpartum Maternal Depression: A pilot study. Infants Young Child. 2014;27:292–304. [Google Scholar]
- 52.McManus BM, Nugent JA. A Neurobehavioral Intervention Incorporated into a State Early Intervention Program is Associated with Higher Perceived Quality of Care among Parents of High-Risk Newborns. J Behav Health Serv Res. 2014;41:381–389. doi: 10.1007/s11414-012-9283-1. [DOI] [PubMed] [Google Scholar]
- 53.Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Less is More: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull. 2003;129:195–215. doi: 10.1037/0033-2909.129.2.195. [DOI] [PubMed] [Google Scholar]
- 54.Jaffee SR. Sensitive, Stimulating Caregiving Predicts Cognitive and Behavioral Resilience in Neurodevelopmentally At-Risk Infants. Dev Psychopathol. 2007;19:631–647. doi: 10.1017/S0954579407000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van den Akker AL, Deković M, Prinzie P, Asscher JJ. Toddlers’ Temperament Profiles: Stability and relations to negative and positive parenting. J Abnorm Child Psychol. 2010;38:485–495. doi: 10.1007/s10802-009-9379-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bartram SC, Barlow J, Wolke D. The Neonatal Behavioral Assessment Scale (NBAS) and Newborn Behavioral Observations system (NBO) for Supporting Caregivers and Improving Outcomes in Caregivers and Their Infants. Cochrane Database of Systematic Reviews. 2015;6:1–14. doi: 10.1002/14651858.CD011754. [DOI] [PMC free article] [PubMed] [Google Scholar]