Abstract
Background
Dissemination is a principle within community-based participatory research (CBPR); however, published research focuses on the dissemination of findings from CBPR projects but less on dissemination of interventions developed through CBPR approaches. To disseminate an evidence-based lifestyle intervention tailored for Native Hawaiians and Pacific Islanders, the PILI 'Ohana Project (POP), an 11-year CBPR initiative, developed an innovative dissemination model.
Objectives
The Community-to-Community Mentoring (CCM) model described in this paper extends the application of CBPR values and principles used in intervention development to intervention dissemination.
Methods
The CCM model combines a CBPR orientation with the Diffusion of Innovation Theory, the Social Cognitive Theory, and key concepts from community organizing and community building to address the multilevel factors that influence uptake of an evidence-based intervention. Grounding the model in CBPR principles provides benefits for intervention dissemination and integrates a focus on community benefits and capacity building.
Conclusions
By establishing co-equal, mutually beneficial relationships at the core of the CCM model, opportunities are created for building critical consciousness, community capacity, and social capital. More research is needed to determine the effectiveness of this model of intervention dissemination which may enhance diffusion of CBPR interventions and empower communities in the process.
Broad dissemination and implementation of evidence-based interventions (EBIs) established through scientific research can improve the overall health of a population. However, there exists a chasm between scientific discoveries and their translation into real-world settings.1,2 For example, Westfall, Mold, & Fagnan (2007) estimated that only 14% of research findings are actually used in clinical practice, and that it takes an average of 17 years for them to be implemented.3
A substantial challenge to the adoption and implementation of EBIs is the lack of diversity in the study samples, which minimizes generalizability to and applicability of EBIs in diverse groups (e.g., ethnicity, socio-economic status (SES), and co-morbidity).2 It is well established that sociocultural and socio-economic barriers increase the risk for chronic diseases, but people who are most impacted by these conditions are often underrepresented in efficacy research. 4-8 In order to address some of these challenges in the translation of research to practice, among other reasons, intervention researchers have turned to community-based participatory research (CBPR).
CBPR is an orientation to research that equitably involves all partners in every aspect of the research process.9-11 Through the establishment of mutually beneficial and trusting relationships based on shared ownership, decision-making, and resources, CBPR helps to balance power between community and academic partners. By partnering with communities throughout the research process and confronting a need important to the community, CBPR-guided studies are positioned to enhance the relevance and usefulness of research and bridge the cultural gaps that may exist between partners.9 Establishing trust and equal partnerships is particularly important among communities that have been harmed by research in the past (e.g. indigenous, minority, and/or other marginalized populations).
The CBPR orientation is characterized by a set of evolving key principles: 1) recognizing community as a unit of identity; 2) building on strengths and resources within the community; 3) facilitating collaborative partnerships in all phases of the research; 4) integrating knowledge and action for mutual benefit of all partners; 5) promoting a co-learning and empowering process that attends to social inequalities; 6) involving a cyclical and iterative process (vs. a linear process); 7) addressing health from both positive and ecological perspectives (e.g., focus on assets); and 8) disseminating findings and knowledge gained to all partners. 9 p. 178-180
Dissemination is included as a principle within CBPR, but dissemination strategies vary widely and there is a dearth of literature on dissemination of interventions developed using a CBPR approach.11 In a 2010 review of published research studies meeting a strict criteria for inclusion as CBPR, Chen, Dias, Lucas and Rosenthal found that, while dissemination of CBPR research is occurring, only 21 of 101 studies included in their review evaluated an intervention. Furthermore, only 33% of these (7 articles) included information on how they disseminated information and knowledge gained. 11 Of those seven articles, just one stated that the intervention was disseminated to another site. 11 This review suggests that although dissemination is valued, there remain substantial barriers to dissemination and variations in how this CBPR principle is applied across studies. 11 One potential approach to promoting wider dissemination of CBPR guided EBIs is through the development of CBPR grounded dissemination models.
The objective of the paper is to describe a model that extends the application of CBPR values, principles, and practices used in intervention development to intervention dissemination. In doing so, we describe the development of a novel, theory-driven, CBPR grounded dissemination model that was used to guide the efforts of the Partnerships to Improve Lifestyle Interventions (PILI) 'Ohana Project, an 11-year CBPR initiative to eliminate obesity disparities in Native Hawaiians and Pacific Peoples (e.g., Samoans, Chuukese, Filipinos). We first briefly describe the PILI 'Ohana CBPR partnership and its progress from intervention development through planning for dissemination as background. We then describe the process of developing and testing the model, which is designed to capitalize on the social capital and capacity already built amongst the founding partners while extending that social capital and capacity to new community-based organizations that might uptake the intervention. Finally, we describe the conceptual foundations and the essential elements of the model.
The PILI 'Ohana Project
In Hawai'i, Native Hawaiians and other Pacific Peoples (NH/PP) have among the highest overweight/obesity prevalence (76-80%) compared to Caucasians (55%) and Japanese (46%). This contributes to higher rates of obesity related diseases (e.g., cardiovascular disease and diabetes mellitus) among NH/PP compared to other ethnic groups.12-13 In 2005, to address obesity and obesity-related disparities experienced by NH/PP in a culturally respectful and scientifically sound way, the PILI 'Ohana Project (POP) was formed. The founding partners include the University of Hawai'i Department of Native Hawaiian Health and four community-based organizations (CBOs) that serve NH/PP. Each of the founding CBOs is represented by a community investigator (CI) who serves on the Intervention Steering Committee (ISC) for the project, along with the principal investigator and project coordinator from the University of Hawai'i (see Table 1; founding CBOs listed as “Mentor” in Table). For more detailed information on the program partners and structure, refer to Nacapoy and colleagues (2006).14 The ISC meets on a monthly basis and to plan, direct, and discuss the activities of the POP.
Table 1. PILI 'Ohana Project Pilot Dissemination Study Mentoring Partnerships and Match Factors.
| Role | Organizations/Associations | Type/Target Population | Location | Characteristics | Match factors |
|---|---|---|---|---|---|
| Mentor* | Kula no na Po'e Hawai'i | Grassroots/Hawaiian Homestead a community | O'ahu - Urban | Non-profit focused on providing Education and Health focused opportunities for Hawaiian Homestead Communities | Previous relationship; Serve similar populations |
| Mentee** | Wai'anae Valley Hawaiian Homestead Community Association | Grassroots/Hawaiian Homestead residents | O'ahu – Rural | Association created to provide leadership and advocate for Homestead community | |
| Mentor | The Association of Hawaiian Civic Clubs b (AHCC) | Grassroots/Hawaiian Civic Club members | Nationwide | Civic and advocacy group for Native Hawaiians | Previous relationship; Same organization type |
| Mentee | Lahaina and Kuini Pi'olani Hawaiian Civic Clubs | Grassroots/Hawaiian Civic Club members | Maui - Rural | Civic and advocacy group Native Hawaiians | |
| Mentor | Ke Ola Mamo, Native Hawaiian Health Care Systems c | Native Hawaiian Health Care Systems (NHHCS) affiliate/Native Hawaiians | O'ahu – Rural & Urban | NHHCS non-profit organization that provides clinical and health promotion programs. | No previous relationship; Mentee expressed interest in program; Mentor availability |
| Mentee | Pana'ewa and Keaukaha Hawaiian Homestead | No formal organization/Hawaiian Homestead residents | Hawai'i Island – Rural | Community members came together to participate in effort to offer a lifestyle intervention for fellow community members. | |
| Mentor | Kōkua Kalihi Valley Comprehensive Family Health Services | Federally Designated Community Health Center/Kalihi Valley residents | O'ahu - Urban | Non-profit health clinic that provides an array of service for community members, which include a number of public housing facilities and immigrants from other Pacific islands. | No previous relationship; Same organization type (Community Center only); Share similar health focus; Mentees expressed interest; |
| Mentee | Moloka'i Community Health Center | Federally Designated Community Health Center/Moloka'i residents | Moloka'i – Rural | Non-profit health clinic that provides an array of service for community members, a larger percentage are Native Hawaiian and/or Filipino. | |
| Mentee | Na Pu'uwai, Native Hawaiian Health Care Systems | Native Hawaiian Health Care Systems affiliate/Native Hawaiians | Moloka'i – Rural | NHHCS non-profit organization that provides health promotion programs. |
Mentors are founding community partners of the PILI 'Ohana Project (POP) who have been involved since its inception. Mentor organizations provide support and guidance to Mentee organizations through process of adoption, adaptation, and implementation. At the inception of the POP, Kalihi Palama Community Health Center was also a founding partner, but did not participate in this dissemination project.
Mentees are CBOs (with varying organizational structures) without previous experience implementing the PILI 'Ohana Lifestyle Program.
Hawaiian Homestead communities were established by the Hawaiian Homes Commission Act of 1920. The act provides government sponsored housing and additional supports to promote economic the self-sufficiency of Native Hawaiians. There are over 50 Hawaiian Homesteads located throughout the Hawaiian Islands. (www.dhhl.hawaii.gov/hhc/laws-and-rules/)
The Association of Hawaiian Civic Clubs (AHCC) is made up of 58 civic clubs throughout the Hawaiian Islands and the continental United States. The AHCC advocates for “the improved welfare of Native Hawaiians in the areas of culture, health, economic development, education, social welfare, and nationhood.” (www.ahcc.org/index.php/about)
The Native Hawaiian Health Care Systems (NHHCS) were created through the Native Hawaiian Health Care Improvement Act of 1988 to address the health needs and improve the health status of Native Hawaiians. The NHHCS affiliates are located on O'ahu, Hawai'i, Maui, Kaua'i and Moloka'i. (http://www.papaolalokahi.org/who-we-are/)
Despite being disproportionally burdened by overweight/obesity and obesity-related diseases, NH/PP are underrepresented in intervention efficacy research. The POP helped to address this imbalance by designing, developing, and testing the PILI 'Ohana Lifestyle Program (PLP). The PLP is a community-led, healthy lifestyle EBI culturally tailored for NH/PP to promote weight loss and weight loss maintenance. For additional details on the PLP, see Mau and colleagues (2010) and Kaholokula and colleagues (2012).15-16 The PLP was found to be effective in a randomized controlled trial and the POP's focus turned to dissemination. 15-16 However, a dissemination model or framework was needed to guide these efforts.
Development of a CBPR Guided Dissemination Model
In formulating the dissemination strategy for sharing the PLP with a broader number of NH/PP communities across Hawai'i, several different dissemination frameworks were examined (e.g., Health Promotion Research Center Dissemination Framework, A Conceptual Model for the Diffusion of Innovations in Service Organizations, Interactive Systems Framework, Policy Framework for Increasing Diffusion of Evidence-based Physical Activity Interventions).17-20 However, none of the models met the objectives of the POP which had a dual focus of disseminating the CBPR guided intervention, while simultaneously building capacity in a way that empowers and directly benefits the participating CBOs. Therefore, the POP developed the Community-to-Community Mentoring (CCM) model, an innovative dissemination model that capitalized on the capacity they developed throughout their long standing CBPR partnership. The CCM model utilizes CBPR principles to orient an approach to dissemination with two objectives; (1) effectively disseminating EBIs while (2) building organizational and community capacity to create sustainable changes required to improve the health and well-being of participating communities.
The primary source of funding for the planning, development, and testing of the PLP was the National Institute of Minority Health and Health Disparities (NIMHD). In anticipation of another grant opportunity from NIMHD focused specifically on dissemination, the POP conducted a pilot dissemination project with sponsorship from the Office of Hawaiian Affairs (OHA), an autonomous public agency whose primary responsibility is to improve the well-being of Native Hawaiians. The project was approved by the institutional review board of the University of Hawai'i at Mānoa.
The CCM model guided the four founding POP community partners (i.e., POP Mentors) who provided mentorship and support to five other NH/PP serving CBOs (i.e., POP Mentees) in their adoption, implementation, and maintenance of the PLP. The Mentors represent four distinct community organizations. They were encouraged to identify new CBOs who were interested in adopting and implementing the PLP from within their organizational affiliations, and most Mentees were identified in this way. However, there were two cases in which the Mentor and Mentee pair had different affiliations (e.g., a Native Hawaiian Health Care Systems affiliate was the Mentor for a Hawaiian Homestead). New CBOs were either contacted directly by a Mentor or referred to a Mentor after they had communicated their interest in the program to the POP principal investigator. Table 1 lists the founding CBOs who serve as Mentors in this model and their respective Mentees as well as characteristics and match factors. Examples from the POP pilot dissemination study will be used to illustrate certain aspects of the CCM, but the focus of the following sections is to describe the theoretical foundations of the CCM and to outline how they are reflected in its major components.
The Conceptual Foundations of the CCM Model
Disseminating and implementing effective, health promoting EBIs involves understanding health behavior change and factors related to the adoption of an innovation at the individual-level (e.g., personal values and outcome expectations), interpersonal-level (e.g., role modeling and positive social reinforcement), and macro-level (e.g., organizational policies).21 As such, the CCM strategies are informed by empirically-supported theories of decision making, behavior change, and community engagement. A multilevel perspective involves using several theories that can explain or affect community change. 22 Specifically, the CCM model combines elements of the Diffusion of Innovations Theory23 (DIT), the Social Cognitive Theory24 (SCT), and key concepts that are common to community organizing and community building25 processes and practices. The blend of a CBPR orientation with these theories and concepts creates the foundation for a dissemination strategy that builds on community strengths, while simultaneously strengthening the community.
The DIT emphasizes the need to plan for the active dissemination of innovations from the beginning as a way to guide the transfer of effective programs into practice. The overall intent is to influence attitude and behavior change at the macro-level.23,26 Dissemination is defined within DIT as the planned and systematic effort designed to make an innovation more widely available.27 Diffusion is the outcome of dissemination and occurs when an innovation is “communicated through certain channels over time among members of a social system.”23,27 The main elements that influence the uptake or pace of diffusion of an innovation include the characteristics of the innovation, characteristics of the adopters, and features of the setting or environmental context. Key characteristics of the innovation that influence diffusion of an innovation are outlined in Table 2. These factors are prominent in the CCM model's innovation component (i.e., the EBI developed through a CBPR approach) and are optimized by the model's CBPR foundation and the mentoring relationship.
Table 2. Definitions of Key Factors from the Major Theories that inform the CCM Model: Diffusion of Innovations Theory27, Social Cognitive Theory28 and Key Concepts in Community Organizing/Community Building25.
| Theory | Key Factors | Definitions |
|---|---|---|
| Diffusion of Innovations Theory27 Pg 319 -320 | Relative advantage | An innovation will only be adopted if it is seen as better than the idea, product, or program it supersedes |
| Compatibility | Innovations that are compatible with the intended users' values, norms, beliefs, and perceived needs are more readily adopted | |
| Complexity | Innovations perceived as easy to use are more likely to be adopted, whereas more complex innovations are less successfully adopted | |
| Trialability | Innovations with which the intended users can experiment on a limited basis are adopted and assimilated more easily | |
| Observability | If the benefits of an innovation are easily identified and visible to others, it will be adopted more easily | |
| Social Cognitive Theory28 Pg 171 | Observational Learning | Learning to perform new behaviors by exposure to interpersonal or media displays of them, particularly through peer modeling |
| Outcome Expectations | Beliefs about the likelihood and value of the consequences of behavioral choices | |
| Self-Efficacy | Beliefs about personal ability to perform behaviors that bring desired outcomes | |
| Collective Efficacy | Beliefs about the ability of a group to perform concerted actions that bring desired outcomes | |
| Facilitation | Providing tools, resources, or environment changes that make new behaviors easier to perform. | |
| Key Concepts in Community Organizing/Community Building25 Pg 294 | Empowerment | Social action process for people to gain mastery over their lives and the lives of their communities |
| Critical Consciousness | A consciousness based on reflection and action in making change | |
| Community Capacity | Characteristics of a community affecting its ability to identify, mobilize, and address problems | |
| Social Capital | Relationships between community members including trust, reciprocity, and civic engagement | |
| Participation/Relevance | Community organizing should “start where the people are” and engage community members as equals. |
All definitions included in Table 2 are directly quoted from cited sources.
The SCT emphasizes learning and knowledge acquisition through the observation of credible others or models at the individual or organizational-level and the development of self-efficacy.28 Peer modeling is an established method used to influence a person's behavior. It is most effective when the observer sees commonality between themselves and the model.28 Self-efficacy is also a critical concept within SCT because the presence or absence of self-efficacy can influence the observer's performance of the modeled behavior. If a person has confidence that they can enact the change that is being promoted, that belief can help them achieve the change they are trying to make. 28 The SCT is the major theory underlying the mentoring relationship in the CCM model as well as many key constructs in the model. Definitions are listed in Table 2.
Finally, CBPR has theoretical roots that overlap with community organizing and community-building paradigms.25,29 Similar orientations toward social action, community-building, and social justice are common to both ideas. While no single model incorporates the different organizing and community-building approaches, there are key concepts that are shared, such as empowerment and critical consciousness.25 Through CBPR, these concepts are operationalized in a research context and inform the CCM model (see Table 2).
Elements of the CCM Model
The CCM uses a CBPR approach applied to EBI dissemination research. It does this through nesting the dissemination of innovations (in this case the EBI) within a CBPR orientation. The EBI is disseminated to new communities through the establishment of a mentoring relationship. Mentors contribute training, guidance, and support in implementing the EBI and Mentees contribute expertise on their community and possible adaptations to the EBI that could improve the effectiveness within their community. The mentoring relationship gives the Mentees an opportunity to engage in observational learning and provides credible role models (i.e., the Mentors) for the Mentees. The Academic Partner is still present, but has a limited role because the Mentors have built their capacity for leadership and expertise on the implementation of the EBI through their own experience as part of the CBPR approach used in intervention development. Figure 1 depicts the CCM model and the contexts in which it operates. There are four major components of the CCM model, which include: 1) the context; 2) the CBPR principles; 3) the partnerships; and 4) the innovation. Table 3 provides examples of the interaction between the theories and model components. Each component is discussed below in more detail.
Figure 1. Community-to-Community Mentoring Model of Intervention Dissemination.
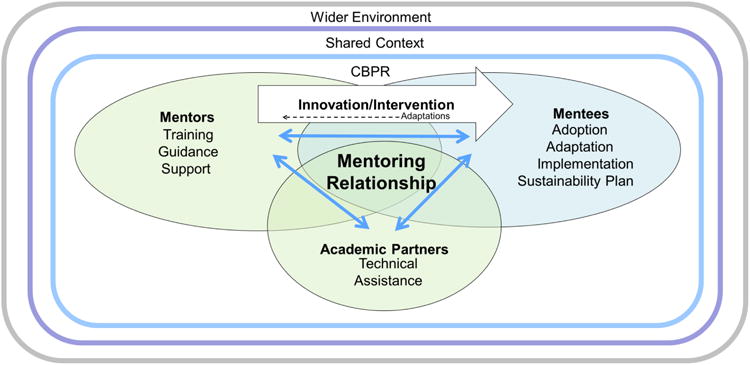
Table 3. Examples of Interactions Between Foundational Concepts within the CCM Model.
| Theories/Key Concepts | |||
|---|---|---|---|
| Model Components | Diffusion of Innovations | Social Cognitive Theory | Community Organizing & Community Building |
| CBPR: | Consideration of the context demonstrates the recognition of community as a unit of identity, which may shape how Mentees adapt the innovation/intervention. | ||
| Context | Matching the mentors and mentees creates some shared context. When the features of the setting are similar it can influence uptake of the innovation. | Because the organizations have a shared context, Mentors are credible role models that are familiar with some of the needs and challenges their Mentees face. | Mentees have agency and can adapt their program to their unique context (wider environment) and needs of the community, which may influence critical consciousness and build relevance for communities. |
| CBPR: | Mentoring relationships promote co-learning to empower CBOs to address the needs they have identified in their communities. | ||
| Partnership | Mentors serve as models and can support Mentees in implementation of EBI to reduce complexity and enhance communication channels. | Mentees engage in observational learning and Mentors provide facilitation which could increase collective efficacy. | Mentoring relationship builds social networks, which could increase social capital and community capacity to make changes they seek. |
| CBPR: | The innovation integrates knowledge and action for the benefit of all partners and incorporates an iterative process whereby Mentees can provide feedback and contribute to the continued improvement and development of the innovation. | ||
| Innovation | The fact that the innovation/intervention was developed through a participatory process may create a relative advantage over other innovations/interventions. The consideration of the contextual factors may positively influence dissemination and diffusion. | Innovations emerging from a CBPR orientation could influence Mentees' outcome expectations or sense of collective efficacy because they are able to observe Mentors successfully implement the change and benefit from their involvement. | The innovation is built from a CBPR orientation, which is reflected in the approach to adoption, adaptation, implementation, and sustainability. Communities are engaged in a way that is respectful, collaborative, and builds trust. |
Context
Context, as indicated in the DIT, is critical to the effective dissemination and eventual diffusion of an intervention.18,23,27,30 In the CCM model, context refers to the environment in which the innovation, partnerships, and organizations are operating. It includes different dimensions that are not limited to socio-economic, political, cultural, and geographical contexts. Some dimensions of the environment may be similar between Mentors and Mentees, such as geographic locations, cultural elements tied to place, and/or the ethnic mix or SES of the communities they serve. These similarities would fall into the shared context component of the CCM model.
The shared context is emphasized in this model because of efforts to match Mentors and Mentees with similar attributes (e.g., type of CBO, mission, ethnicity or SES of population served). Similarities across organizations could ease communication and facilitate trust through a better understanding of each other's perspectives, needs, and challenges. Pairing organizations in this manner is intended to enhance the compatibility (also a key factor of DIT) of the intervention and establish the credibility of the mentoring organization. Other aspects may be different between the Mentee and Mentor. Those aspects would fall into the wider environment context of the model, which may also influence the success of the dissemination effort.
CBPR Approach
The CCM model is nested in a CBPR approach and relies on the guiding principles of CBPR.9 One way in which the dissemination of interventions created in a CBPR context is unique is that the “developers” of the innovation are not separate from the “users” as in existing dissemination models.17,18,31,32 Within CBPR, the community is involved in a co-equal partnership from the initiation of the project; therefore, they are both the developer and the user of the innovation. As a consequence, the potential users of an innovation are actively involved during each phase of development.
In addition, the CBPR approach emphasizes communication as a bi-directional and foundational part of dissemination. The bi-directional lines of communication within the relationship facilitate trust, co-learning, and community-relevant adaptations to the innovation being disseminated. These ongoing conversations allow for possible adaptations to the EBI that may influence the sustainability of the intervention within an organization and make it more effective within the communities it serves. See Table 3 for additional examples of the way in which CBPR principles provide a framework for the model components.
Partnership
The mentoring partnership within the CCM model is the focal point of the dissemination strategy, is based on core principles of CBPR, and is guided by observational learning. 9,24 The establishment of mentoring partners is a strategy that strengthens social networks, which may ultimately build social capital and community capacity.25 Fostering partnerships and extending networks may impact community capacity by expanding potential resources to address shared social problems. 25 The mentoring relationships are between the Mentors (i.e., founding community partners), Mentees (i.e., new CBOs), and Academic Partner.
Mentors are community partners who are seasoned in the CBPR approach and deeply familiar with the intervention. They provide support, guidance, and training for the new organizations. The Mentor organization has developed the capacity to successfully make a change (i.e., the ability to implement the EBI and comprehensively integrate the principles of CBPR), and they now have the ability to be the model of the change.28 In addition, because of their close connection to the communities they serve, they are positioned to be credible role models for others seeking to build their own capacity to engage in research and implement EBIs. The Mentee might be more inclined to adopt and implement a program that a similar organization (i.e., their Mentor) has successfully implemented.
The Mentee organizations observe their Mentors when determining their outcome expectations (or expectancies) for implementing an EBI. 28 Mentee organizations may be more likely to have positive outcome expectations, and therefore be more likely to implement an EBI, if they perceive the Mentor organization as having achieved something of value. Building the capacity of the organization to provide health promotion programs or being recognized for their work are examples of possible valuable outcomes.
Mentee organizations also bring their own strengths and resources to the partnership. In the CCM model, the Mentee CBOs' responsibilities are to adopt, adapt, implement, and hopefully sustain the intervention. Due to the distinct characteristics of the CBOs, these goals will be achieved in different ways for individual organizations. Dissemination of the intervention to new communities is approached from the perspective that Mentee organizations are experts of their communities. Each CBO has the autonomy to define their community and make adaptions to the intervention, with certain cautions regarding changes that may significantly impact the effectiveness of the EBI. These adaptations may be necessary steps that allow them to implement the intervention, but also respond appropriately to the reality of their wider environment (i.e., those contextual elements that are not shared with their Mentor and are often outside of their direct control). In this way, the Mentees are not passive recipients of an EBI, but are engaged participants and expected to make contributions to the intervention that make the program relevant to their specific communities. This aspect reflects the participation/relevance concept in community organizing/community building, whereby communities are engaged in identifying their needs and work to implement their own plan of action.25
The Mentee organizations receive support in EBI implementation through what is described in the SCT as facilitation.28 Facilitation is provided by the Mentor in the form of training, resources, and other available assistance (e.g., provision of curriculum materials, one-on-one facilitator training, consulting on recruitment or retention strategies). Facilitation can lead to increased collective efficacy, which is a concept similar in function and process to self-efficacy, but on a group-level. 28,33 By being supported through the change process, the Mentee builds confidence that their organization can address the health needs identified in their community, which may increase organizational capacity as well as community capacity. This is particularly critical for health interventions that are adopted and implemented by CBOs that are not necessarily identified as health-oriented organizations.
The role of the Academic Partner in the CCM model is central, but less prominent because the expertise around adoption, implementation, and sustaining the intervention is primarily in the hands of the community partners and executed at the community-level. The Academic Partner's role is predominantly technical assistance, which may include some formalized training on the intervention, data analysis, or administrative project support. Studies on dissemination within a CBPR context have found that dissemination can help reinforce and maintain relationships between academic and community partners.11,30 The Academic Partner benefits from the dissemination of the intervention, data sharing, and relationships built with the communities.
The mentoring activities in this model are not prescriptive. Using the POP experience as an example, Mentors provided support and guidance through a variety of modes, including but not limited to regular consultations, material support (e.g., providing incentives or copies of the curriculum for participants), and assistance with problem solving in situations around follow-up or recruitment. Mentors assisted with training by inviting Mentees to observe their staff facilitating an intervention lesson or by helping with the baseline assessment and modeling data collection, so that the Mentee could conduct the follow-up assessments independently.
Innovation
In regards to DIT, the innovation is the new intervention or the change that is being introduced.23,27 The main feature of the innovation, the EBI in the CCM model, is that it is a product of a CBPR orientation. To clarify, it is not simply the intervention that is the “innovation,” but also the application of CBPR in the development of the intervention and the resulting capacity. The innovation can be an intervention related to a variety of health topics and can be a program, policy, or another form of new knowledge, but a critical feature is that it emerges out of community interest and participation. Using the POP experience, the formation of the CBPR partnership to address the problem of obesity is an example of the concept of critical consciousness.25 Identifying an issue they perceive to be a detriment to the communities in which they live and work was the initial step in solidifying the communities' commitment to take action that would positively impact their health status. Thus, the intervention created through partnerships embodies community values, communicates community concepts of health and well-being, addresses community needs, and builds community capacity to make change.
The healthy lifestyle intervention developed by the POP includes culturally relevant references to foods and activities and incorporates discussions about how to successfully implement behavior changes within the family and community context, topics that were gleaned from focus groups conducted with community members. In these ways, the intervention attempts to address some of the cultural and contextual factors, which has been recognized as one of the benefits CPBR offers to intervention research.34 Furthermore, the intervention was tested through a randomized control trial and found to be effective with NH/PP.16
The development of the PLP through a CBPR approach illustrates a key factor identified in the DIT, the characteristics of the innovation. Innovation attributes that could influence the diffusion of an innovation include relative advantage, compatibility, complexity, trialability, and observability.28 The consideration of cultural and contextual factors in a scientific study may be seen by potential adopters as a relative advantage, if adopters have not previously come across an EBI that was culturally tailored and community-based. In addition, compatibility is high when the innovation, or in this case the intervention, is designed with the target community in mind, because the main elements address the needs expressed by the community members. Implementing an EBI that is facilitated through mentoring partnerships may minimize the influence of the three latter factors because of the support offered. Specifically, the mentoring aspect improves the likelihood that a new CBO will implement a complex intervention. In addition, the Mentee has opportunities to observe the Mentor's successful outcomes (e.g., successful intervention implementation and improvements in health outcomes of participants).
Conclusion
The CCM model is a promising approach to the dissemination of EBIs that emerge out of a CBPR project. The model is theory-driven and includes attributes (e.g., compatibility, consideration of environment/context/setting, communication channels, strong links or networks) that have been cited by other researchers as influential to the pace and uptake of an intervention.17,18,23,27 The key CBPR principles also provide a framework that can enhance these critical attributes.
Preliminary results of the POP suggest that the model is helpful in achieving good adoption, implementation, and retention. In the pilot study, all five of the new community partners adopted and implemented the program and reached their target enrollment goals. While the analysis is still being finalized, the initial assessment of the data suggests the few organizations that modified the intervention by abbreviating the schedule, while conducting all the lessons, had weight loss comparable to groups that followed the standard schedule. There were few adaptations to the protocol among the Mentees, but some minor enhancements were added. For example, two groups created social media profiles (i.e., Facebook) for participants to share class information, healthy lifestyle tips, or related news. Within the span of a year, the POP doubled the number of communities that implemented the intervention. We are currently in the midst of a NIMHD-funded dissemination study guided by our CCM model that targets a larger number of potential Mentee communities (i.e., communities served by Hawaiian Homesteads, Hawaiian Civic Clubs, community health centers, and Native Hawaiian Health Systems).
The CCM model extends the key principles of CBPR throughout the process of EBI dissemination by establishing co-equal, mutually beneficial relationships at its core. By strengthening social networks and positioning CBOs as leaders and Mentors, opportunities are created for building critical consciousness, community capacity, and social capital. More research is needed to determine the effectiveness of this model of intervention dissemination which may enhance diffusion of CBPR interventions and empower communities in the process.
Acknowledgments
This project was supported by the Office of Hawaiian Affairs (OHA) and in part by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R24MD001660 (PI: J.K. Kaholokula). AH and CTI were supported in part by funding from the Queen's Health Systems. The content is solely the responsibility of the authors and does not necessarily represent the official views of OHA, the National Institutes of Health, or the Queen's Health Systems. The authors thank the community organizations that participated in the pilot study: Kula no na Po'e Hawai'i, Wai'anae Valley Hawaiian Homestead Community Association, the Association of Hawaiian Civic Clubs, Ke Ola Mamo Native Hawaiian Health Care System, Pana'ewa and Keaukaha Hawaiian Homestead communities, Kōkua Kalihi Valley Comprehensive Family Health Services, Moloka'i Community Health Center, and Nā Pu'uwai Native Hawaiian Health Care System. Finally, we would like to express our gratitude to Mele A. Look and Leimomi Kanagusuku for their input.
References
- 1.Glasgow RE, Green LW, Taylor MV, Stange KC. An evidence integration triangle for aligning science with policy and practice. Am J Prev Med. 2012;42(6):646–54. doi: 10.1016/j.amepre.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glasgow RE, Lichtenstein E, Marcus AC. Why don't we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93(8):1261–7. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Westfall JM, Mold J, Fagnan L. Practice-based research - blue highways on the NIH roadmap. JAMA. 2007;297(4):403. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 4.Davis EM, Clark JM, Carrese JA, Gary TL, Cooper LA. Racial and socioeconomic differences in the weight loss experiences of obese women. Am J Public Health. 2005;95(9):1539–1543. doi: 10.2105/AJPH.2004.047050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 6.Kumankiya S. Obesity treatment in minorities. In: Wadden TA, Stunkard AJ, editors. Obesity: theory and therapy xiii. New York: Guilford Publications, Inc.; 2002. [Google Scholar]
- 7.Mau MK, Wong KN, Efird J, West M, Saito EP, Maddock J. Environmental factors of obesity in communities with Native Hawaiians. Hawaii J Public Health. 2008;67(9):233–6. [PMC free article] [PubMed] [Google Scholar]
- 8.Tinker JE, Tucker JA. Motivations for weight loss and behavior change strategies associated with natural recovery from obesity. Psychol Addict Behav. 1997;11:98–106. [Google Scholar]
- 9.Israel B, Schulz A, Parker E, Becker A. Review of community-based research: Assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 10.Kellogg Health Scholars. WK Kellogg Foundation [Internet] Washington (DC): Community Health Scholars Program; 2015. [2015 July 30]. Available at: http://www.kellogghealthscholars.org/about/community.php. [Google Scholar]
- 11.Chen PG, Diaz N, Lucas G, Rosenthal MS. Dissemination of results in community-based participatory research. Am J Prev Med. 2010 Oct;39(4):372–378. doi: 10.1016/j.amepre.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 12.Nguyen DH, Salvail FR Hawai'i State Department of Health. The Hawai'i Behavioral Risk Factor Surveillance System; 2010 results [Internet] Honolulu (HI): Hawai'i State Department of Health; 2010. [2015 June 1]. revised 2013. Available from: http://health.hawaii.gov/brfss/ [Google Scholar]
- 13.Grandinetti A, Kaholokula JK, Theriault AG, Mor JM, Chang HK, Waslien C. Prevalence of diabetes and glucose intolerance in an ethnically diverse rural community of Hawai'i. Ethn Dis. 2007;17(2):250–5. [PubMed] [Google Scholar]
- 14.Nacapoy AH, Kaholokula JK, West MR, Dillard AY, Leake A, Kekauoha BP, et al. Partnerships to address obesity disparities in Hawai'i: the PILI 'Ohana Project. Hawai'i J Public Health. 2008;67(9):237–41. [PMC free article] [PubMed] [Google Scholar]
- 15.Mau MK, Kaholokula JK, West MR, Leake A, Efird JT, Rose C, et al. Translating diabetes prevention into Native Hawaiian and Pacific Islander communities: the PILI 'Ohana Pilot project. Prog Community Health Partnersh. 2010;4(1):7–16. doi: 10.1353/cpr.0.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaholokula JK, Mau MK, Efird JT, Leake A, West M, Palakiko DM, et al. A family and community focused lifestyle program prevents weight regain in Pacific Islanders: a pilot randomized controlled trial. Health Educ Behav. 2012;39(4):386–395. doi: 10.1177/1090198110394174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris JR, Cheadle A, Hannon PA, Forehand M, Lichiello, Mahoney E, et al. A framework for disseminating evidence based health promotion practices. Prev Chronic Dis. 2012;9:110081. doi: 10.5888/pcd9.110081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, Stillman L. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41:171–181. doi: 10.1007/s10464-008-9174-z. [DOI] [PubMed] [Google Scholar]
- 20.Owen N, Glanz K, Sallis JF, Kelder SH. Evidence-based approaches to dissemination and diffusion of physical activity interventions. Am J Prev Med. 2006;31(Suppl 4):S25–S44. doi: 10.1016/j.amepre.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 21.Smedley BD, Syme SI, editors. Institute of Medicine (US) Committee on Capitalizing on Social Science Research to Improve the Public's Health. Promoting health: intervention Strategies from social and behavioral research. Washington DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 22.Glanz K, Rimer BK, Lewis FM. Health behavior and health education: Theory, research, and Practice. San Francisco: Wiley & Sons; 2008. p. 169. [Google Scholar]
- 23.Rogers EM. Diffusion of Innovations. 5th. New York, NY: The Free Press; 2003. [Google Scholar]
- 24.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 25.Minkler M, Wallerstein N, Wilson N. Improving health through community organization and community building. In: Glanz K, Rimer B, Viswanath K, editors. Health behavior and health education: theory, research, and practice. 4th. San Francisco: Jossey-Bass, John Wiley & Sons; 2008. pp. 291–298. [Google Scholar]
- 26.Wilson PM, Petticrew M, Calnan MW, Nazareth I. Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. Implement Sci. 2010;5(91):1–16. doi: 10.1186/1748-5908-5-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oldenburg B, Glanz K. Diffusion of Innovations. In: Glanz K, Rimer B, Viswanath K, editors. Health behavior and health education: theory, research, and practice. 4th. San Francisco: Jossey-Bass, John Wiley & Sons; 2008. pp. 313–332. [Google Scholar]
- 28.McAlister AL, Perry CL, Parcel GS. How individuals, environments, and behaviors interact, social cognitive theory. In: Glanz K, Rimer B, Viswanath K, editors. Health behavior and health education: theory, research, and practice. 4th. San Francisco: Jossey-Bassm, John Wiley & Sons; 2008. pp. 169–188. [Google Scholar]
- 29.Wallerstein N, Duran B. The theoretical, historical and practice roots of CBPR. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health, from process to outcomes. 2nd. San Francisco, CA: Jossey-Bass, John Wiley & Sons; 2008. pp. 25–46. [Google Scholar]
- 30.Dreisinger ML, Boland EM, Filler CD, Baker EA, Hessel AS, Brownson RC, et al. Contextual factors influencing readiness for dissemination of obesity prevention programs and policies. Health Educ Res. 2012;27(2):292–306. doi: 10.1093/her/cyr063. [DOI] [PubMed] [Google Scholar]
- 31.Rimer BK, Glanz K, Rasband G. Searching for evidence about health education and health behavior interventions. Health Educ Behav. 2001;28(2):231–248. doi: 10.1177/109019810102800208. [DOI] [PubMed] [Google Scholar]
- 32.Klein KJ, Sorra JS. The challenge of innovation implementation. Acad Manage Rev. 1996;21(4):1055–1080. [Google Scholar]
- 33.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 34.Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(Suppl):S40–S6. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]


