Abstract
Introduction:
Along with the increase of osteoporotic patients in an aging society, complications in surgeries associated with osteoporosis are also increasing. In cementless total knee arthroplasty (TKA), poor primary stability and subsequent initial loosening of the implant may be seen.
Case Report:
The patient, a 75-year-old Asian woman with a history of osteoporosis, underwent cementless TKA. Knee radiography at 5 weeks postoperatively showed radiolucent lines outlined beneath the tibial tray and around the stem. The tibial component was considered unstable due to loosening. A 56.5 µg weekly dose of teriparatide (rh [1-34] parathyroid hormone) was administered. After 2 months of treatment, knee pain and knee swelling had disappeared. Tomosynthesis taken after 6 months of treatment confirmed complete ingrowth of the component to the bone.
Conclusion:
This case showed that a weekly teriparatide administration of 56.5 µg improved initial loosening of the tibial implant in cementless TKA. Administration of teriparatide in cases of the osteoporotic patient who has loosening in cementless TKA may be a useful adjuvant to achieve bone ingrowth again.
Keywords: Total knee arthroplasty, cementless total knee arthroplasty, teriparatide, loosening, tomosynthesis, osteoporosis
What to Learn from this Article?
We recommend to administrate a teriparatide to patient with initial loosening of the implant in cementless TKA.
Introduction
The incidence of osteoporosis continues to increase in the aging societies of developed countries. The main problem for osteoporotic patients is unequivocally the risk of fracture [1, 2]. However, several complications in surgery are also significant problems. In arthroplasty, in particular, osteoporosis often causes periprosthetic fracture and subsidence of the prosthesis. In cementless total knee arthroplasty (TKA), poor bone ingrowth of the tibial implant due to osteoporosis in the proximal metaphyseal part of the tibia can be a significant problem.
Cementless TKA is beneficial in that it achieves biological fixation between a porous-coated implant and the bone surface [3]. The clinical results of cementless TKA have been described as satisfactory. However, the results of radiological assessment, especially in the tibial implant, have been varied. Some studies have shown good fixation in cases of cementless TKA [3]. Conversely, poor ingrowth of bone into the porous-coated tibial implant surface has also been reported [4]. For elderly patients, this poor bone ingrowth may be the result of osteoporosis in the proximal metaphyseal part of the tibia. Several studies have shown a high rate of occurrence of osteolysis and radiolucent lines around the tibial component [5, 6]. To avoid loosening and to achieve more stable results with a cementless prosthesis, a high degree of primary stability and initial fixation is essential [7].
Recently, anabolic agents such as teriparatide have been used for osteoporotic patients. Teriparatide modulates bone formation and bone remodeling and results in increased bone density. Teriparatide is also reported to be useful for the healing of bony fracture and nonunion [1, 8] and for the re-ingrowth of bone in cases of aseptic loosening of hip prostheses [9, 10].
This paper reports a case in which a patient with initial aseptic loosening following cementless TKA was treated with teriparatide acetate. To our knowledge, no similar cases have been reported previously.
Case Report
A 75-year-old Asian woman underwent cementless TKA (Cementless Vanguard, Biomet, Warsaw, IL, USA) in November, 2012, for severe osteoarthritis of the left knee (Fig. 1). The medical history included hypertension treated with oral amlodipine and losartan. Preoperative bone mineral density (BMD) examined by a dual-energy X-ray absorptiometry (DEXA) scan was 0.43 g/cm2 which suggested osteoporosis (T score: −4.1).
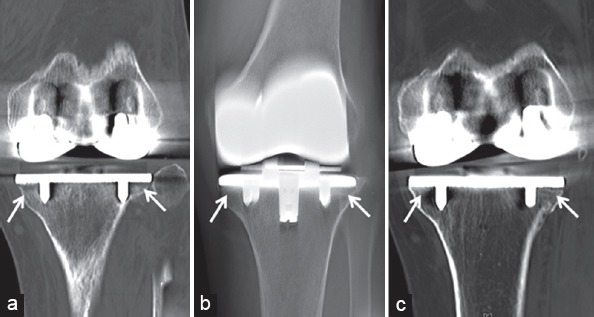
Figure 1.
Computed tomography and tomosynthesis of the knee. (a) Computed tomography taken at 6 weeks postoperatively showing loosening around the tibial component. (b) Tomosynthesis taken after 6 months of teriparatide therapy showing no spaces between the tibial component and the osteotomy load surface. (c) Computed tomography taken at 1 year postoperatively showing no spaces beneath the tibial component.
The patient started to stand and walk on day 2 postoperatively. However, she reported continuing knee pain and knee swelling after surgery. Laboratory tests on day 14 postoperatively revealed a white blood cell count of 7.7 × 109/L and C-reactive protein of 9.81 mg/dL. At 5 weeks postoperatively, knee radiography showed radiolucent lines outlined beneath the tibial tray and around the stem (Fig. 1). The tibial component was considered unstable due to loosening. At first, infection was suspected, and an antibiotic of sulfamethoxazole/trimethoprim was administered. However, a culture of intra-knee fluid and a laboratory test of procalcitonin were both found to be negative for infection. At 6 weeks postoperatively, computed tomography was conducted, which clearly showed loosening around the tibial component (Fig. 2). The patient was diagnosed with aseptic loosening caused by initial unstable fixation.
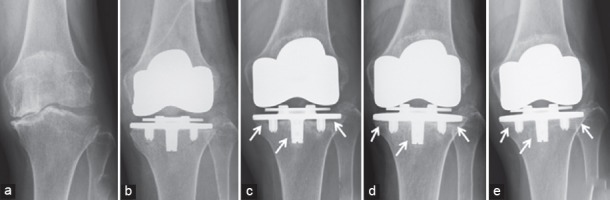
Figure 2.
Radiography of the knee. (a) Plain film of the knee with osteoarthritis before total knee arthroplasty. (b) Plain film taken immediately following the operation. (c) Plain film taken at 5 weeks postoperatively showing radiolucent lines at entire circumference around the tibial tray. (d) Plain film taken after 2 months of teriparatide therapy showing a decrease of previously observed radiolucent lines. (e) Plain film taken at 1 year postoperatively showing complete ingrowth to the tibial bone.
The patient was treated with a 56.5 µg weekly dose of teriparatide (rh [1-34] parathyroid hormone [PTH]). Daily activity such as walking with a cane and housework was permitted during treatment. After 2 months of treatment, knee pain and knee swelling had disappeared, and the patient was able to walk without a cane. Knee radiography at this time exhibited a decrease of previously observed radiolucent lines (Fig. 1). Laboratory tests showed a gradual decrease of C-reactive protein and erythrocyte sedimentation rate, which finally reached a negative value at 3 months after treatment.
After 6 months of teriparatide therapy, the patient achieved tomosynthesis, and no space between either femoral or tibial components and the osteotomy load surfaces was observed (Fig. 2). Upon confirmation that the component had achieved complete ingrowth to the bone, the administration of teriparatide was discontinued. BMD examined using DEXA at this point showed an increase to 0.46 g/cm2, with an increased T-score of −3.6. Knee radiography at 1 year postoperatively showed no radiolucent lines around either the femoral or tibial components and an increase in sclerosis at the pedestal (Fig. 1). Computed tomography also showed no space between the tibial tray and the tibial surface. Although some artifacts were observed around pegs, the implant still achieved ingrowth to the bone (Fig. 2). The patient experienced no pain in her knee and was able to walk freely without a cane. The knee society score improved to 95.
Discussion
Teriparatide is human PTH which has the effect of promoting bone formation unlike conventional bone resorption inhibitors that suppress the activity of osteoclasts such as bisphosphonates. Teriparatide promotes the differentiation of osteoprogenitor cells and osteoblast precursor cells and also promotes bone formation activity by inhibiting apoptosis of osteoblasts. Teriparatide has also been shown to have an effect on the acceleration of bony healing following fracture. The efficacy teriparatide has been shown in several animal models with various bone healing problems such as fracture and nonunion [11, 12]. In humans, Aspenberg et al. reported that in cases of distal radial fracture in postmenopausal women, the time of healing was shorter in cases treated with teriparatide than in a placebo group [1]. Recently, the efficacy of teriparatide has also been reported for bone ingrowth in cases of aseptic loosening of hip prostheses. Oteo-Álvaro et al. reported a patient with aseptic loosening at 3 years following hip hemiarthroplasty. Teriparatide was administered for 24 months, and clinical improvement associated with the disappearance of radiographic loosening was achieved [9]. Zati et al. also reported a patient treated with teriparatide following loosening in the cup of the hip prosthesis, which improved after 8 months of treatment [10].
A 56.5 µg weekly dose of teriparatide was used in this case. This treatment, which was developed in Japan, has been reported to increase BMD and reduce new vertebral fracture in participants with osteoporosis [2, 13]. Nakamura et al. reported that in a study using a weekly teriparatide injection of 56.5 µg, the serum concentration of bone formation maker increased in 4 weeks, declining in 24 weeks, and maintaining increase in serum osteocalcin level until 72 weeks. Conversely, urinary NTX levels exhibited no increase during the entire period and were maintained at a low level [13]. These data indicate that the 56.5 µg weekly dose increased bone formation in 4 weeks. These results were different from a study on a daily teriparatide treatment of 20 µg which reported that the serum concentration of the bone formation marker increased rapidly and remained significantly elevated but that the bone resorption marker also increased significantly and was elevated above baseline [14]. These reports suggest that a weekly 56.5 µg administration of teriparatide directly accelerates bone formation and that a daily 20 µg administration of teriparatide accelerates bone formation with an increasing turnover of bone metabolism. This unique function of the 56.5 µg weekly treatment also seems to have a beneficial effect on fracture healing. Tachiiri et al. reported two cases of delayed union treated with a weekly 56.5 µg administration of teriparatide and stated that the effect of this therapy was observed within 4 weeks [15]. Thus, we chose to treat this case of loosening in cementless TKA with the same weekly teriparatide treatment at a dosage of 56.5 µg.
Conclusion
This case showed that a weekly teriparatide administration of 56.5 µg improved initial loosening of the tibial implant in cementless TKA. Administration of teriparatide in cases of the osteoporotic patient who has loosening in cementless TKA may be a useful adjuvant to achieve bone ingrowth again, but the present result should be interpreted with caution and warrants further study.
Clinical Message.
In cementless TKA, poor bone ingrowth and loosening of the implant is one of the significant problems. We reported that a teriparatide administration improved initial loosening of the tibial implant in cementless TKA. We want to publicize the message that administration of teriparatide may help us from the problem of loosening of cementless TKA occurred in osteoporotic patient.
Biography






Footnotes
Conflict of Interest: Nil
Source of Support: None
References
- 1.Aspenberg P, Genant HK, Johansson T, Nino AJ, See K, Krohn K, et al. Teriparatide for acceleration of fracture repair in humans:A prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J Bone Miner Res. 2010;25(2):404–414. doi: 10.1359/jbmr.090731. [DOI] [PubMed] [Google Scholar]
- 2.Nakano T, Shiraki M, Sugimoto T, Kishimoto H, Ito M, Fukunaga M, et al. Once-weekly teriparatide reduces the risk of vertebral fracture in patients with various fracture risks:Subgroup analysis of the teriparatide once-weekly efficacy research (TOWER) trial. J Bone Miner Metab. 2014;32(4):441–446. doi: 10.1007/s00774-013-0505-2. [DOI] [PubMed] [Google Scholar]
- 3.Hayakawa K, Date H, Tsujimura S, Nojiri S, Yamada H, Nakagawa K. Mid-term results of total knee arthroplasty with a porous tantalum monoblock tibial component. Knee. 2014;21(1):199–203. doi: 10.1016/j.knee.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Sumner DR, Kienapfel H, Jacobs JJ, Urban RM, Turner TM, Galante JO. Bone ingrowth and wear debris in well-fixed cementless porous-coated tibial components removed from patients. J Arthroplasty. 1995;10(2):157–167. doi: 10.1016/s0883-5403(05)80122-6. [DOI] [PubMed] [Google Scholar]
- 5.Berger RA, Lyon JH, Jacobs JJ, Barden RM, Berkson EM, Sheinkop MB, et al. Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat Res. 2001:196–207. doi: 10.1097/00003086-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg VM, Kraay M. The outcome of the cementless tibial component:A minimum 14-year clinical evaluation. Clin Orthop Relat Res. 2004:214–220. doi: 10.1097/01.blo.0000148572.95121.f0. [DOI] [PubMed] [Google Scholar]
- 7.Lombardi AV, Jr, Berasi CC, Berend KR. Evolution of tibial fixation in total knee arthroplasty. J Arthroplasty. 2007;22(4 Suppl 1):25–29. doi: 10.1016/j.arth.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Tamai K, Takamatsu K, Kazuki K. Successful treatment of nonunion with teriparatide after failed ankle arthrodesis for Charcot arthropathy. Osteoporos Int. 2013;24(10):2729–2732. doi: 10.1007/s00198-013-2367-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oteo-Álvaro Á, Matas JA, Alonso-Farto JC. Teriparatide (rh [1-34] PTH) improved osteointegration of a hemiarthroplasty with signs of aseptic loosening. Orthopedics. 2011;34(9):e574–e577. doi: 10.3928/01477447-20110714-50. [DOI] [PubMed] [Google Scholar]
- 10.Zati A, Sarti D, Malaguti MC, Pratelli L. Teriparatide in the treatment of a loose hip prosthesis. J Rheumatol. 2011;38(4):778–780. doi: 10.3899/jrheum.100980. [DOI] [PubMed] [Google Scholar]
- 11.Andreassen TT, Ejersted C, Oxlund H. Intermittent parathyroid hormone (1-34) treatment increases callus formation and mechanical strength of healing rat fractures. J Bone Miner Res. 1999;14(6):960–968. doi: 10.1359/jbmr.1999.14.6.960. [DOI] [PubMed] [Google Scholar]
- 12.Nakajima A, Shimoji N, Shiomi K, Shimizu S, Moriya H, Einhorn TA, et al. Mechanisms for the enhancement of fracture healing in rats treated with intermittent low-dose human parathyroid hormone (1-34) J Bone Miner Res. 2002;17(11):2038–2047. doi: 10.1359/jbmr.2002.17.11.2038. [DOI] [PubMed] [Google Scholar]
- 13.Nakamura T, Sugimoto T, Nakano T, Kishimoto H, Ito M, Fukunaga M, et al. Randomized teriparatide [human parathyroid hormone (PTH) 1-34] once-weekly efficacy research (TOWER) trial for examining the reduction in new vertebral fractures in subjects with primary osteoporosis and high fracture risk. J Clin Endocrinol Metab. 2012;97(9):3097–3106. doi: 10.1210/jc.2011-3479. [DOI] [PubMed] [Google Scholar]
- 14.Miyauchi A, Matsumoto T, Sugimoto T, Tsujimoto M, Warner MR, Nakamura T. Effects of teriparatide on bone mineral density and bone turnover markers in Japanese subjects with osteoporosis at high risk of fracture in a 24-month clinical study:12-month, randomized, placebo-controlled, double-blind and 12-month open-label phases. Bone. 2010;47(3):493–502. doi: 10.1016/j.bone.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 15.Tachiiri H, Okuda Y, Yamasaki T, Kusakabe T. Weekly teriparatide administration for the treatment of delayed union:A report of two cases. Arch Osteoporos. 2014;9:179. doi: 10.1007/s11657-014-0179-y. [DOI] [PubMed] [Google Scholar]


