Abstract
Reminiscence interventions are potentially effective in improving well-being of persons with memory loss (PWMLs) and may also enhance relationships with family and professional caregivers. Using a parallel convergent mixed-methods design, the feasibility of “Memory Matters” (MM), a mobile device application developed to promote reminiscence, was evaluated. Eighteen PWMLs and eight family members were enrolled from a long-term care facility and asked to use MM for 4 weeks. Participants were observed using MM at enrollment and 2 weeks and completed 1-month interviews. Six staff participants also completed a system review checklist and/or focus group at 1 month. Three qualitative domains were identified: (a) context of use, (b) barriers to use, and (c) MM influences on outcomes. Participants reported real-time social engagement, ease of use, and other benefits. However, PWMLs were unlikely to overcome barriers without assistance. Empirical data indicated that family and staff perceived MM favorably. Participants agreed that MM could provide stimulating, reminiscence-based activity.
In the United States, an estimated 5.3 million adults have Alzheimer’s disease, a prevalence expected to increase by 40% within the next decade (Alzheimer’s Association, 2015; Centers for Disease Control and Prevention, 2013). Persons with memory loss (PWMLs) face numerous challenges, including declines in their ability to communicate and increased emotional distress. Professionals and family members also experience stress related to caring for individuals with Alzheimer’s disease, which often negatively influences their ability to provide ongoing support (Qualls & Zarit, 2009). Nonetheless, family caregivers contribute approximately 20 billion unpaid hours caring for their loved ones with memory loss (Alzheimer’s Association, 2015).
A number of nonpharmacological, psychosocial interventions have been developed to improve the well-being of PWMLs and family caregivers. Such interventions range from exercise to music therapy, with various degrees of success (Cochrane Collaboration, 2015). Reminiscence therapy is a psychosocial intervention that recalls the life and experiences of an individual with the aim to help the PWML maintain positive mental health (Woods, Spector, Jones, Orrell, & Davis, 2005). Reminiscence therapy is defined by Woods et al. (2005) as “the discussion of past activities, events and experiences with another person or group of people, usually with the aid of tangible prompts such as photographs, household and other familiar items from the past, music and archive sound recordings” (p. 1). Reminiscence therapy can help improve communication between caregivers and PWMLs, thereby reducing caregiver stress (Allen, 2009). Reminiscence therapy also has the potential to improve mood, well-being, quality of life, social interaction, cognition, autobiographical memory, and staff knowledge of PWMLs (Chen, Li, & Li, 2012; Cotelli, Manenti, & Zanetti, 2012; Lazar, Demiris, & Thompson, 2015; Subramaniam & Woods, 2012). However, these findings are not consistent across high-quality research designs (Cochrane Collaboration, 2015; Woods et al., 2005).
Prior evaluations of reminiscence therapy have typically relied on static materials, such as photographs and personal items (Lazar, Thompson, & Demiris, 2014). Existing technology-based reminiscence therapy aids include Computer Interactive Reminiscence and Conversation Aid (CIRCA; Alm et al., 2004), LifeZig (n.d.), SimpleC (n.d.), Reminiscence Enhanced Material Profiling in Alzheimer’s and other Dementias (REMPAD; Yang et al., 2013), and Story Frame (Chen, Lin, & Liang, 2013). These aids largely rely on pictures and audio clips loaded onto computers. However, technology-based applications have the potential to provide a more dynamic reminiscence experience. Technology-based reminiscence therapy activities can be rapidly downloaded and ready for use or quickly personalized to the individual and family. Smaller mobile devices and a wider availability of wireless networks have also increased portability. Studies show that using computers with PWMLs is highly rated by staff and participants (Alm et al., 2004; Astell et al., 2010; Tamura et al., 2007). A recent study of tablet use suggests its potential to engage older adults socially (DeLello & McWhorter, 2015). However, a review of technology-based interventions indicated that although such platforms hold promise, few rely on the dynamic, personalized capabilities of hand-held devices (e.g., tablets) to help facilitate reminiscence (Lazar et al., 2014).
The primary aim of the current study was to test the feasibility and acceptability of a mobile tablet application to enhance reminiscence among PWMLs, called “Memory Matters” (MM). MM was designed to stimulate long-term memories through “cognitive exercise” in which users physically tap on-screen tiles, relying on the assumption that activities involving cognitive and physical interaction are more likely to engage users than passive viewing and listening activities. The goal of the current study was to determine whether PWMLs, family members, or professional caregivers could easily use MM to facilitate and enhance reminiscence.
METHOD
Memory Matters
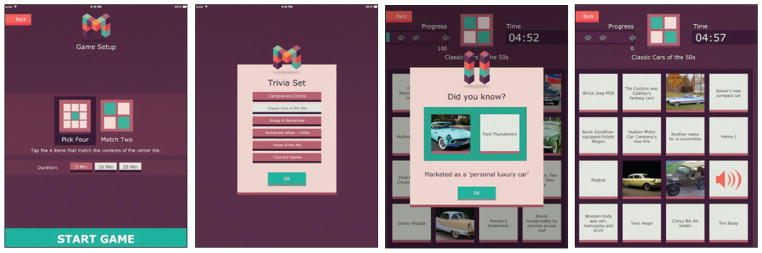
Moai Technologies, LLC developed the interactive digital memory game (i.e., MM) for mobile tablets and designed it specifically to facilitate the reminiscence process in PWMLs. The application also promotes cognitive stimulation, which can benefit individuals with dementia (Aguirre, Woods, Spector, & Orrell, 2013). The application involves the matching of items covering various cultural trends and historical events from 1920–1980 and is organized around time periods (i.e., “Fabulous 50s” or content themes, such as “Rock and Roll Hits”). Figure 1 shows screenshots of the MM application. Content is presented as text, audio clips (e.g., songs, voices), and visual cues (e.g., photographs). On average, it took PWMLs 4.17 minutes (SD = 4.52 minutes; range = 0.07 to 30.93 minutes) to play each MM game in the current study.
Figure 1.
Memory Matters gameplay screenshots.
Procedure and Sample
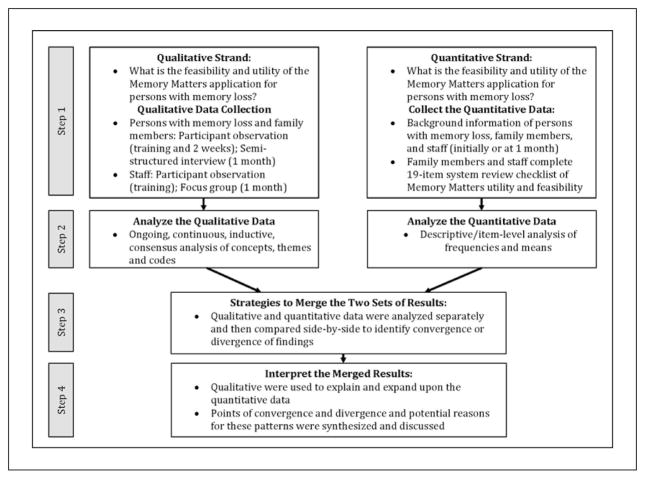
A parallel convergent mixed-methods design was used to generate qualitative and quantitative data on the feasibility and utility of the MM application (Creswell & Plano Clark, 2011). The various data elements included in the study and their integration are presented in Figure 2.
Figure 2.
Schematic of data elements and integration strategies.
The study was approved by the University of Minnesota Institutional Review Board. The study was conducted at a nursing home and assisted living facility in a metropolitan area in the upper Midwestern United States. Facility staff who expressed interest in participating in the study were provided written informed consent and training on MM (n = 6). Following training, staff identified and approached residents with memory loss and their family members to obtain permission for the research team to contact them about the study. Inclusion criteria for PWMLs were diagnosis of Alzheimer’s disease or related dementia and a willingness to use MM. Once informed consent was obtained from family members, the PWML was asked to complete a brief memory assessment (i.e., Saint Louis University Mental Status Examination [SLUMS]; Tariq, Tumosa, Chibnall, Perry, & Morley, 2006) and provide verbal assent.
A hands-on tutorial was conducted with each PWML and family participant. Each training session lasted 30 to 45 minutes and was conducted by one trainer (D.K.) and one research assistant (A.V.H. or T.L.S.). Staff and family were encouraged to use MM with the PWML weekly. A research assistant conducted an observation of each PWML playing MM at 2 weeks. At 1 month, semi-structured interviews were conducted with each PWML (n = 18) and family participant (n = 8). A focus group was conducted with staff at 1-month follow up (n = 3). Staff (n = 6) and family (n = 8) also completed a system review checklist at 1-month follow up.
Data Collection
Demographic/Background Data
Family participants provided background information on the PWML and his/her family. Staff also provided background information (Table 1).
TABLE 1.
STUDY SAMPLE CHARACTERISTICS
| PWMLs (n = 18)a | Family Members (n = 8)a | Staff (n = 6) | ||||
|---|---|---|---|---|---|---|
| Variable | Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SD) | n (%) |
| Age (years) | 84 (10.74) | 59.38 (4.57) | 42.83 (13.39) | |||
| Female | 16 (94.1) | 6 (75) | 6 (100) | |||
| Non-Hispanic/Latino Caucasian | 17 (100) | 8 (100) | 6 (100) | |||
| Married/living with partner | 2 (11.8) | 5 (62.5) | 3 (50) | |||
| Widowed | 14 (82.4) | 0 | 0 | |||
| Employed full-time | 4 (50) | 6 (100) | ||||
| Living children | 3.20 (2.27) | 2.13 (0.99) | ||||
| Highest level of educationb | 4.12 (1.73) | 4.13 (0.64) | 6.17 (0.98) | |||
| Household incomec | 6 (2.2) | 9.33 (1.03) | ||||
| Physician visit for memory concerns | 12 (80)d | |||||
| Time since first physician visit for memory concerns (months) | 94.5 (100.01) | |||||
| Alzheimer’s disease or dementia diagnosis | 7 (41.2) | |||||
| No diagnosis reported | 7 (41.2) | |||||
| SLUMS score | 17.06 (6.7) | |||||
| Length of stay (months) | 42.12 (30.07) | |||||
| Receives Medicaid | 7 (41.2) | |||||
| Time since memory symptoms first recognized (months) | 82.75 (99.84) | |||||
| Adult child of PWML | 8 (100) | |||||
| Provided help to PWML due to memory loss | 5 (62.5) | |||||
| Primary caregiver of PWML | 5 (62.5) | |||||
| Duration of care to PWML (months) | 102 (117.58) | |||||
| Length of employment at current facility (months) | 97.16 (122.16) | |||||
Note. PWML = person with memory loss; SLUMS = St. Louis University Mental Status Examination.
One family member provided consent to participate but did not complete background information for resident or family member.
1 = did not complete junior high/middle school to 8 = graduate degree.
1 = <$5,000 to 10 = ≥$80,000.
Two additional family members did not provide data.
MM System Review Checklist
A 19-item system review checklist was administered to family participants and staff 1 month following PWMLs’ enrollment. The checklist was specially designed to assess the feasibility and utility of MM. Each item was scored on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) (Table 2).
TABLE 2.
SYSTEM REVIEW CHECKLIST OF MEMORY MATTERS
| Percent (n) Agreed or Strongly Agreed | ||
|---|---|---|
| Checklist Item | Family Members (n = 8) | Staff (n = 6) |
| Memory Matters was easy to use. | 75 (6) | 83.3 (5) |
| The information on the introductory screen of Memory Matters was clear to me. | 75 (6) | 100 (6) |
| The information and screens of Memory Matters were clear. | 75 (6) | 83.3 (5) |
| I was able to understand the games on Memory Matters. | 75 (6) | 100 (6) |
| The instructions on how to use Memory Matters were helpful. | 62.5 (5) | 100 (6) |
| I valued how individualized Memory Matters was for the person with memory loss. | 50 (4) | 66 (4) |
| After using Memory Matters, I thought that the person with memory loss was more socially engaged. | 57.2 (4)a | 16.7 (1) |
| I thought that the person with memory loss was more cognitively stimulated after using Memory Matters. | 62.5 (5) | 33.3 (2) |
| My use of Memory Matters led to more positive interactions/communication with the person with memory loss. | 75 (6) | 33.3 (2) |
| There are time constraints to me being able to use Memory Matters with the person with memory loss. | 14.3 (1)a | 50 (3) |
| I am planning on using Memory Matters regularly with the person with memory loss. | 62.5 (5) | 50 (3) |
| I believe the person with memory loss will use Memory Matters regularly. | 37.5 (3) | 66.7 (4) |
| The games and other content on Memory Matters were concise and clear. | 62.5 (5) | 100 (6) |
| The person with memory loss was lost using Memory Matters. | 50 (4) | 16.7 (1) |
| I wish I would have known about Memory Matters sooner. | 57.2 | 83.3 (5) |
| After using Memory Matters, the person with memory loss seems happier. | 37.5 (3) | 33.3 (2) |
| The overall layout, text, and design of Memory Matters is very confusing to me. | 12.5b (1) | 0c |
| I would be willing to use Memory Matters on my own without (the trainer’s) guidance. | 37.5 (3) | 83.3 (5) |
| I would recommend Memory Matters to others in a similar situation as I. | 87.5 (7) | 100 (6) |
Data missing from one respondent.
62.5% strongly disagreed.
50% strongly disagreed.
Qualitative Components
Detailed field notes were taken during trainings and observations. The 1-month interview guide for PWMLs and family participants as well as the staff focus group guide are included in Table A (available in the online version of this article). Training sessions for PWMLs and family members averaged 30 to 40 minutes each; observations averaged 20 to 30 minutes each, and interviews averaged 20 minutes each. Staff training and focus group sessions were 60 and 40 minutes, respectively.
Table A.
Semi-Structured Interview/Focus Group Guide: 1-Month (Family Members and Staff)
|
Introduction Thank you so much for participating in our evaluation of Memory Matters (MM). To follow-up on your participation, I would like to ask some open-ended questions. My objective in this interview is to determine why MM benefited you and the person/persons with memory loss or not. |
Opening Question
|
Introductory Question
|
Benefits
|
| Harm and drawbacks |
|
| MM components and outcomes |
|
| Ending Question |
|
Data Analysis
Qualitative data collection and analysis were simultaneous and continuous. Field notes and interview data were audiotaped and transcribed verbatim. Two coders (A.V.N., T.L.S.), both trained in qualitative data analysis methods, individually coded each transcript using open-coding methods (Luborsky, 1994; Morse & Field, 1995; Morse & Niehaus, 2009). Transcripts were then coded using a thematic analysis approach with a qualitative data management program (NVivo 10). To ensure themes reflected intended meanings of participants, codes were reviewed by three of the authors (A.V.H., T.L.S., J.E.G.) to reach consensus on concepts, themes, and their organization. Quantitative data were analyzed using descriptive statistics (e.g., frequencies, means) to examine family and staff perceptions of MM’s feasibility, function, and utility based on the MM system review checklist.
The qualitative and quantitative components were mixed by first analyzing the domains and themes that emerged from the multiple sources of qualitative data (e.g., observations/field notes, interviews, focus group). Descriptive empirical results were then examined and compared to organized themes to determine how and why MM was deemed acceptable or useful by participants and whether the qualitative and quantitative data converged or diverged (Creswell & Plano Clark, 2011).
RESULTS
Sample Characteristics
Eighteen PWMLs participated in the study; five resided in an assisted living facility, eight in a nursing home, and five in a memory care/special care unit. As shown in Table 1, most PWMLs were female, widowed, and had a high school education. More than 40% were on Medicaid. All PWMLs were Caucasian and were on average 84 years old. The average SLUMS score was 17.06, which suggested presence of dementia (Tariq et al., 2006). PWMLs resided in their current location for a mean of 3.25 years. Family members of PWMLs had a mean age of 60, most were women, and all were Caucasian. More than one half were married and employed full-time and on average had completed an Associate’s degree with an annual income of $40,000–$59,999. Family participants provided a mean of 7.5 years of care to PWMLs. All staff (n = 6) were Caucasian, female, and had a mean age of 40. All participating staff members were employed full-time and worked in the current setting for a mean of 8 years.
Feasibility and Utility of MM
Qualitative Data Structure
Approximately 11 hours of observation, interview, and focus group data resulted in 264 pages of transcribed text. Following qualitative analysis, three concepts emerged that included eight specific themes (Table 3). Emergent concepts and themes are presented below and compared alongside empirical results of the MM system review checklist.
TABLE 3.
CONCEPTS AND THEMES DEVELOPED DURING PARTICIPANT OBSERVATION AND SEMISTRUCTURED INTERVIEWS OF PERSONS WITH MEMORY LOSS, FAMILY MEMBERS, AND STAFF
| Concept | Theme | Representative Quote |
|---|---|---|
| Context of Use | Resident Context | “...it does occupy his time. There’s not always something to do. I hate to think of him lying in his bed watching TV and just napping off and on. But this gave him something to think about and something to do.” (Wife, final interview) |
| “She was snapping along and dancing, and then there’s the part in the song where the drums kick in, and before that she said, ‘Oh here it comes.’ So she was ready for that. She was smiling, she was enjoying the song.” (Observer, 2-week observation) | ||
| Training Experience | “I think even this would be a fun group activity to do…. Imagine the engagement, the conversation that would come up. And the laughing...thinking about these old shows and music and everything…. Gather a group around, put it on the big screen, and all play it together, which would be great.” (Staff member, focus group) | |
| “Part of the reason that you would do it is because somebody provides a good motivation. This will be fun. Or, they give you a demonstration of how it works. Well, it could pique your interest a little bit.” (PWML, final interview) | ||
| Feasibility | “It’s geared more toward people who have very little memory impairment, or the least amount. Because they would know to go and check the iPad… then the other ones it’s all in how involved their family members are.” (Staff member, focus group) | |
| “It tickled my brain a little bit, and I had a good chance, in a way, because it was all during the 1940s. It was my time during the 1940s. And that was easy, cause I knew all the people that were popular then. And it just seemed real easy, it was fun.” (PWML, final interview) | ||
| Barriers to Use | User Barriers | “In order to see the [screen], she needed to sit up in her wheelchair. After a while she [said], ‘Oh, it’s kind of uncomfortable. I have to sit up to see the game’...then we stopped playing the game, because…her back was getting kind of uncomfortable from having to sit up.” (Observer, training session) |
| “They feel like fear is a barrier for utilization, whether it’s fear of playing or fear of getting an answer wrong, or fear of breaking the iPad, fear of losing the iPad. That fear is a barrier for playing the game.” (Observer, staff focus group) | ||
| Environmental Barriers | “I really would have liked to use it more than I did, but…we’re so busy around here. They have so many activities and I’ve got a big family. Eight of my kids live in town, and they’re in and out and taking me here and there.” (PWML, final interview) | |
| Memory Matters Influence on Outcomes | Social Engagement | “I would say the process itself, in the moment, when you’re doing it, was a social engagement You were laughing and you were looking at things, and you were complimenting them and saying good job.” (Staff member, final focus group) |
| “I guess I couldn’t say that it helped her like with her specific memories, or something like that. I do think that it helped her stay active and kept her mind working…making her think and interact and that was a good thing.” (Son, final interview) | ||
| “The staff liked one-on-one engagement with residents. They felt like it was a positive interaction. They also felt like they were able to learn more about the residents, just from when they remembered certain things. And sometimes when they remember certain things then they would…end up telling a story about it. And so that part was helpful for them.” (Observer, staff focus group) | ||
| “You know, it was humorous. We were humored by what we remembered and the old times and...people we knew from those times. And that was very nice for him. It was a very pleasant experience. I enjoyed it, too. And it did enable us to connect…in a way that we have not connected since before the stroke…it gave us some pleasant time together that we normally have not had after the stroke.” (Wife, final interview) | ||
| Reminiscence | “[The song] In The Mood, oh I get just hysterical almost. I just loved it…I was going to school at that time in the Union Hall…you could dance during the day if you wanted to. So there was a couple always dancing… with that song…and I’d stop and watch them, and listen, and it is fun.” (PWML, final interview) | |
| “And then we talked a little bit about [how] she grew up on a farm…. This came from my just asking her about when she grew up. It wasn’t anything that was stimulated really from the iPad other than I transitioned into it because she…remembered reading a comic.” (Observer, 2-week observation) | ||
| “One of the songs was by Buddy Holly, and that triggered them to start talking about when their plane crashed with all the musicians on it. The resident said to his wife, ‘Oh, I heard they’re re-opening the plane crash investigation.’ Then she said, ‘Yeah, it’s suspicious that there were so many people that died [of] plane crashes during that period of time.’” (Observer, training session) |
Note. PWML = person with memory loss.
Context of Use Concept
The context of PWMLs’ MM use emerged as a concept. Quotes representing each theme within the context of use concept are presented in Table 3. The user context theme included codes such as motivation and reasons for participating. Residents and family saw the application as an additional activity. Multiple family participants discussed preferring this activity to time-passing activities, such as television. Participant preferences also influenced MM use. These preferences reflected the empirical system review checklist data (Table 2), with more than one half of family participants and two thirds of staff reporting the individualized aspects of MM as positive. Qualitative data suggested PWMLs and their family preferred the dataset with songs. Games that included pictures were also popular. The objectives of the song and picture-matching datasets appeared easier for PWMLs to understand, in contrast to text-based matching, which required more prompting. Some participants requested additional topics to reflect their interests.
Within the training experience theme, it was frequently noted that MM could be used as a group activity. This finding may have explained family participants’ reluctance to agree or strongly agree that the PWML would use MM regularly (37.5%) or without a trainer’s guidance (37.5%). Staff were more positive when appraising PWMLs’ future use (66.7%) and MM use without a trainer present (83.3%) (Table 2). However, PWMLs, staff, and family participants consistently indicated the potential of MM as a partner or group activity. The qualitative data reflected that users’ experiences of MM could be improved with the support of another individual.
All staff and more than 70% of family participants believed the MM training was helpful. Staff suggested that training of all facility staff and increased staff engagement could help PWMLs feel more comfortable using the tablet. Empirical data indicated 50% of staff and 62.5% of family members planned on using MM regularly with residents, and 14.3% and 50% of family and staff, respectively, indicated time constraints (Table 2). Qualitative data sources explained potential time constraints in more detail. For example, codes within the theme of feasibility implied that residents who experienced less cognitive impairment and whose use of MM featured more staff and family involvement were more likely to use MM. Some residents were excited about trying the tablet, whereas others were more apprehensive; overall residents appeared to be more comfortable with using the tablet and MM in subsequent time periods. Residents, family members, and staff also indicated that time constraints and an increased level of participation in outside activities were factors that hindered use of MM.
Barriers to Use Concept
Empirical ratings were highly positive about the various facets of MM usability. For example, 75% of family participants and 100% of staff found MM understandable. Three quarters of family participants and 83.3% of staff indicated the information on MM was presented clearly. Similarly, only 12.5% of family participants and no staff found the design of MM confusing. Nonetheless, staff, PWMLs, and family participants all identified various impediments to MM use. One half of family participants indicated the PWML was lost using MM; this is in contrast to the 16.7% of staff members’ response to this item. Within the barriers to use concept, three themes emerged at the levels of the users, the environment, and technology (Table 3). The most frequent user barriers were sensory, aural, and visual. Several participants also faced physical barriers to MM use. Residents in wheelchairs reported and were observed having difficulty finding a comfortable and sustainable position to hold the tablet and manipulate the touchscreen. Some found the device too heavy for prolonged gameplay, requiring a surface or another individual to hold it for them. Some residents also displayed emotional responses to MM, which presented an additional obstacle to use. Liability for the device, apprehension of technology, and concern of judgment were all noted by PWMLs, family participants, and staff.
Technological barriers occurred within the program and were caused by the device. Most often participants were unsure that they had made a selection. In these instances, although the PWML had verbally indicated the correct answer, he/she would mis-tap the selection, leading the application to falsely indicate an error. Tablet operations, such as knowing how to turn it on, were difficult for residents and led participants to believe that MM could not be used without assistance. Despite these barriers, staff and family reported they found MM easy to use (83% and 75%, respectively) (Table 2).
MM Influence on Outcomes
As identified in Table 3, the third concept encompassed outcomes related to MM participation. Outcome themes were social engagement and reminiscence. In assessing relational benefits, staff and family drew comparisons between real-time and long-term outcomes. Participants described benefits during a MM session that were not observed after MM play stopped. This finding may explain the lower empirical ratings staff (16.7%) and, to a lesser extent, family members (57.2%) provided regarding PWMLs’ increased social engagement following MM use (Table 2). In their focus group, staff indicated that MM positively influenced their interactions with residents while using the application. The discordance with the low empirical data rating (33.4%) provided by staff may reflect the different perceptions of real-time versus the perceived long-term benefits of MM use.
Perhaps most importantly, family members indicated that MM provided an opportunity to interact with their loved one in ways they had not been able in some time. Family participants reported enjoying discussing their earlier days, learning more about the PWML, and re-engagement while playing MM with PWMLs who were typically more withdrawn. These perceptions were reflected in the empirical checklist rating (75%) (Table 2).
Reminiscence was observed and noted to have occurred with residents and staff, participant observers (A.V.H., T.L.S.), and family. On several occasions when residents shared remote memories, it was in direct response to prompts provided by MM, such as hearing a long-loved song or seeing a familiar name or face. On other occasions, MM use appeared to stimulate reminiscence on topics not directly related to the application’s content, but would instead lead participants to discuss something from their past. Reminiscence would also occur by making a connection from MM to an event that touched both participants’ lives and was linked to current events.
The pattern of qualitative findings seems to support the real-time benefit of MM, but also the need for ongoing use of the device to sustain such benefits; the latter sentiment may explain the lower empirical ratings related to the potential outcomes of MM use as noted in Table 2 (particularly among staff). For example, 37.5% of family members and 33.4% of staff indicated that PWMLs were happier after using MM, although 62.5% of family members and only 33.3% of staff reported that the PWML was cognitively stimulated following MM use. Nonetheless, family members and staff were favorable overall in their assessment of MM, with 57.2% of family members and 83.3% of staff indicating that they wished they had known about MM sooner.
DISCUSSION
Participants viewed their use of MM favorably, and PWMLs were able to overcome obstacles to use. Although some became proficient and used MM frequently, others only played MM when in the researchers’ presence. Similar studies reported that participants were able to use tablet touchscreens with little prompting from others (Astell et al., 2010; Gowans et al., 2004), although ongoing training was often needed for older adults to become facile at using tablets for social engagement purposes (DeLello & McWhorter, 2015). At the facility in which the current study was conducted, participants reported active, full days that impeded MM use; PWMLs and staff alike found making time for or finding someone to assist them with the use of MM difficult. This finding implies the need for more formal integration of MM use in the context of scheduled group activities or staff–resident interactions.
Social engagement was observed and reported as a result of MM. Family members discussed being able to relate to the PWML in ways they had not prior to the onset of cognitive impairment. Staff found that discussions stimulated by MM use provided new information about PWMLs (e.g., Anderson, Taha, & Hosier, 2009). PWMLs, who only interacted minimally or had never spoken before, interacted and supported each other while playing the application, which supports the social engagement potential of mobile devices that include stimulating, interactive content (Bleakley et al., 2015; DeLello & McWhorter, 2015). Active reminiscence was also observed, either in direct response to the application or through conversation encouraged by MM. Moments of reminiscence ranged from singing along to a familiar tune to sharing stories. Some residents were able to draw connections between content on MM and current events. Taken together, these findings indicate that MM is a potentially enjoyable and beneficial activity for PWMLs, family members, and professional caregivers. These findings are similar to recent reviews suggesting the potential of adapting reminiscence therapies with various forms of easy-to-use technologies (Lazar et al., 2014). MM may be best used in a setting where family or staff are able to provide support and capitalize on the social engagement and reminiscence opportunities as they arise and to incorporate such insights into longer-term, more sustained activities and/or care plans.
Empirical data suggested that social engagement and cognitive stimulation were less evident in the period following MM use. Various mechanisms may have led to this perceived lack of long-term benefit, such as duration of the current study, time constraints, and independent MM initiation by residents. More than one half of family and staff thought the PWML would use MM regularly; however, some PWMLs indicated having busy schedules and staff indicated level of cognitive impairment and family involvement as hindrances to MM use. In contrast to staff, most family members indicated they would not use MM on their own. Thus, although most family members and staff would recommend MM use to others, the need to extend MM to ensure sustainable, long-term use (through formal or group-based activities) would likely enhance the application’s ability to exert meaningful benefits for PWMLs, family members, and professional caregivers.
LIMITATIONS
In addition to the various barriers reported, other limitations must be considered. No control group was used, thus conclusions about the effectiveness or efficacy of MM are not possible. The MM system review checklist was developed specifically for the current study and not validated prior to administration. Comprehensive data were not collected on prior technology or tablet use, which may influence the acceptability and utility of the MM application among potential users. The small and homogeneous sample reduced the generalizability of findings across more diverse samples and settings.
IMPLICATIONS FOR NURSING PRACTICE AND CONCLUSION
The current study findings emphasize that MM may be most beneficial to PWMLs when used in partnership as demonstrated in prior studies (Haesner, Steinert, O’Sullivan, & Weichenberger, 2015; Lazar et al., 2015). Facility staff who made time to play MM together with PWMLs found that the application provided an opportunity to better know the individuals under their care. MM also appeared to enhance interactions between residents and family caregivers and provided a conversational focal point upon which to share experiences.
When applying MM to memory care practice, MM has the potential to facilitate well-being among PWMLs and family members through reminiscence and increased social engagement. Such benefits could provide staff and family members with new information about the individuals they are caring for and provide distraction from present-day, short-term memory loss by prompting reflection and sharing preserved long-term memories. Using MM in a group context may also enhance memory care programming often provided by gerontological nurses in residential long-term care. For these various reasons, MM is a potentially innovative and useful supplement to activity and other psychosocial components of optimal memory care for older adults.
Semi-Structured Interview Guide for Persons with Memory Loss: 1-Month
|
Introduction Thank you so much for participating in our evaluation of Memory Matters (MM). To follow-up on your participation, I would like to ask some open-ended questions. My objective in this interview is to determine why MM benefited you or not. |
Introductory Question
|
Benefits
|
Harm and drawbacks
|
Ending Question
|
Acknowledgments
This research was supported by R43 LM012085 from the National Library of Medicine to Moai Technologies (D. Klassen, Principal Investigator [PI]) and K02 AG029480 from the National Institute on Aging to the University of Minnesota (J.E. Gaugler, PI). The authors thank Kari Johnson for her training expertise, Gary Havey of Advanced Medical Electronics for his assistance, and Dr. Robert Woods for his consultation.
The authors also thank the residents, family members, and staff of Martin Luther Care Center in Bloomington, Minnesota, for their gracious contribution of time.
Footnotes
Mr. Havey and Dr. Klassen are paid employees of Moai Technologies, LLC. The remaining authors have disclosed no potential conflicts of interest, financial or otherwise.
Contributor Information
Ms. Aimee V. Hamel, PhD Student, School of Nursing, Center on Aging, University of Minnesota, Minneapolis.
Ms. Tai L. Sims, PhD Student, School of Nursing, Center on Aging, University of Minnesota, Minneapolis. Assistant Professor, Minnesota State University-Mankato, Mankato, Minnesota.
Dr. Dan Klassen, Vice President of Software Development, Moai Technologies, Minneapolis, Minnesota.
Mr. Thomas Havey, Chief Executive Officer, Moai Technologies, Minneapolis, Minnesota.
Dr. Joseph E. Gaugler, Professor, School of Nursing, Center on Aging, University of Minnesota, Minneapolis.
References
- Aguirre E, Woods RT, Spector A, Orrell M. Cognitive stimulation for dementia: A systematic review of the evidence of effectiveness from randomised controlled trials. Ageing Research Reviews. 2013;12:253–262. doi: 10.1016/j.arr.2012.07.001. [DOI] [PubMed] [Google Scholar]
- Allen RS. The Legacy Project intervention to enhance meaningful family interactions: Case examples. Clinical Gerontologist. 2009;32:164–176. doi: 10.1080/07317110802677005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alm N, Ellis M, Astell A, Dye R, Gowans G, Campbell J. A cognitive prosthesis and communication support for people with dementia. Neuropsychological Rehabilitation. 2004;14:117–134. doi: 10.1080/09602010343000147. [DOI] [Google Scholar]
- The Alzheimer’s Association. 2015 Alzheimer’s disease facts and figures. 2015 doi: 10.1016/j.jalz.2015.02.003. Retrieved from http://www.alz.org/facts/downloads/facts_figures_2015.pdf. [DOI] [PubMed]
- Anderson KA, Taha RD, Hosier AF. Know thy residents: An exploration of long-term care nursing staff’s knowledge. Research in Gerontological Nursing. 2009;2:69–76. doi: 10.3928/19404921-20090101-03. [DOI] [PubMed] [Google Scholar]
- Astell AJ, Ellis MP, Bernardi L, Alm N, Dye R, Gowans G, Campbell J. Using a touch screen computer to support relationships between people with dementia and caregivers. Interacting with Computers. 2010;22:267–275. doi: 10.1016/j.intcom.2010.03.003. [DOI] [Google Scholar]
- Bleakley CM, Charles D, Porter-Armstrong A, McNeill MDJ, McDonough SM, McCormack B. Gaming for health: A systematic review of the physical and cognitive effects of interactive computer games in older adults. [10.1177/0733464812470747];Journal of Applied Gerontology. 2015 34 doi: 10.1177/0733464812470747. N -NP189. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. The state of aging and health in America 2013. 2013 Retrieved from http://www.cdc.gov/features/agingandhealth/state_of_aging_and_health_in_america_2013.pdf.
- Chen HC, Lin YC, Liang RH. Study through designing reminiscing activities for the elderly. Digital Creativity. 2013;24:327–341. doi: 10.1080/14626268.2013.776972. [DOI] [Google Scholar]
- Chen TJ, Li HJ, Li J. The effects of reminiscence therapy on depressive symptoms of Chinese elderly: Study protocol of a randomized controlled trial. BMC Psychiatry. 2012;12:189. doi: 10.1186/1471-244X-12-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane Collaboration. Cochrane Dementia and Cognitive Improvement Group. 2015 Retrieved from http://dementia.cochrane.org/our-reviews.
- Cotelli M, Manenti R, Zanetti O. Reminiscence therapy in dementia: A review. Maturitas. 2012;72:203–205. doi: 10.1016/j.maturitas.2012.04.008. [DOI] [PubMed] [Google Scholar]
- Creswell J, Plano Clark V. Designing and conducting mixed methods research. 2. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- DeLello JA, McWhorter RR. Reducing the digital divide: Connecting older adults to iPad technology. Journal of Applied Gerontology. 2015 doi: 10.1177/0733464815589985. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Gowans G, Campbell J, Alm N, Dye R, Astell A, Ellis M. CHI’04 Extended Abstracts on Human Factors in Computing Systems. New York, NY: Association for Computing Machinery; 2004. Designing a multimedia conversation aid for reminiscence therapy in dementia care environments; pp. 825–836. [Google Scholar]
- Haesner M, Steinert A, O’Sullivan JL, Weichenberger M. Evaluating an online cognitive training platform for older adults: User experience and implementation requirements. Journal of Gerontological Nursing. 2015;41(8):22–31. doi: 10.3928/00989134-20150710-44. [DOI] [PubMed] [Google Scholar]
- Lazar A, Demiris G, Thompson HJ. Involving family members in the implementation and evaluation of technologies for dementia: A dyad case study. Journal of Gerontological Nursing. 2015;41(4):21–26. doi: 10.3928/00989134-20150309-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazar A, Thompson H, Demiris G. A systematic review of the use of technology for reminiscence therapy. Health Education & Behavior. 2014;41(Suppl 1):51S–61S. doi: 10.1177/1090198114537067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LifeZig Program. Welcome to LifeZig. n.d Retrieved from http://www.lifezig.com/index.html.
- Luborsky MR. The identification and analysis of themes and patterns. In: Gubrium JF, Sankar A, editors. Qualitative methods in aging research. Thousand Oaks, CA: Sage; 1994. pp. 189–210. [Google Scholar]
- Morse JM, Field PA. Qualitative research methods for health professionals. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Morse JM, Niehaus L. Mixed method design: Principle and procedures. Walnut Creek, CA: Left Coast Press; 2009. [Google Scholar]
- Qualls SH, Zarit SH, editors. Aging families and caregiving. Vol. 3. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]
- SimpleC. Community support products. n.d Retrieved from http://www.simplec.com/community_connect.
- Subramaniam P, Woods B. The impact of individual reminiscence therapy for people with dementia: Systematic review. Expert Review of Neurotherapeutics. 2012;12:545–555. doi: 10.1586/ern.12.35. [DOI] [PubMed] [Google Scholar]
- Tamura T, Ohsumi M, Oikawa D, Higashi Y, Fujimoto T, Suenaga T, Kuwahara N. Reminiscence: A comparison of conventional therapeutic and computer-based interactive methods. Journal of Robotics and Mechatronics. 2007;19:724–727. [Google Scholar]
- Tariq SH, Tumosa N, Chibnall JT, Perry HM, III, Morley JE. The Saint Louis University Mental Status (SLUMS) Examination for detecting mild cognitive impairment and dementia is more sensitive than the Mini-Mental Status Examination (MMSE): A pilot study. American Journal of Geriatric Psychiatry. 2006;14:900–910. doi: 10.1097/01.JGP.0000221510.33817.86. [DOI] [PubMed] [Google Scholar]
- Woods B, Spector A, Jones C, Orrell M, Davis S. Reminiscence therapy for dementia. Cochrane Database of Systematic Reviews. 2005;2:CD001120. doi: 10.1002/14651858.CD001120.pub2. [DOI] [PubMed] [Google Scholar]
- Yang Y, Caprani N, Bermingham A, O’Rourke J, Collins R, Gurrin C, Smeaton AF. Design and field evaluation of REMPAD: A recommender system supporting group reminiscence therapy. In: O’Grady MJ, Vahdat-Nejad H, Wolf KH, Dragone M, Ye J, Röcker C, O’Hare G, editors. Evolvingambient intelligence. Heidelberg, Germany: Springer International; 2013. pp. 13–22. [Google Scholar]