Abstract
Background
Postoperative cognitive dysfunction (POCD) is a postoperative complication after surgery and anesthesia. Whether ABO blood types are associated with POCD in elderly patients undergoing unilateral total hip arthroplasty surgery in China is unclear.
Material/Methods
Firstly, 142 elderly patients were divided into a POCD group and a non-POCD group according to the Mini Mental State Examination (MMSE) scores and ABO blood types were analyzed. Secondly, according to ABO blood type, the selected 226 patients were divided into 4 groups: type A group, type B group, type AB group, and type O group. Then, all patients completed the MMSE before and after surgery. Finally, the occurrence of POCD was recorded and related data were analyzed.
Results
Firstly, there was a significant difference in both groups in terms of distribution of ABO blood types, and elderly patients who developed POCD were more likely to have type A blood and less likely to have type O blood. Secondly, compared with elderly patients with type A blood, those with type O had higher MMSE scores on the first day and the seventh day after surgery. Finally, the risk of developing POCD was significantly higher in patients with type A blood and on the first day and the seventh day after surgery the risk of developing POCD was significantly lower in patients with type O blood.
Conclusions
Elderly patients with type A blood have higher risk of developing early POCD and those with type O blood have less risk of developing early POCD.
MeSH Keywords: ABO Blood-Group System, Cognitive Dissonance, Frail Elderly
Background
Postoperative cognitive dysfunction (POCD), a postoperative complication of the central nervous system, is characterized by disordered consciousness, cognition, orientation, thinking, memory, and sleep after surgery and anesthesia. POCD delays recovery time and prolongs hospitalization, and patients may even develop permanent cognitive impairment and decreased quality of life after surgery and anesthesia [1–3].
Recently, some studies showed that age, education, type of surgery, operation time and anesthesia contribute to its occurrence [4]. The pathogenesis of POCD is still unclear. Many risk factors were reported to have a multifactorial association with the occurrence of POCD, such as age, alcohol abuse, and pre-existing cerebral, cardiac, and vascular diseases [5]. Recently, some studies also showed that stress reaction induced by harmful stimulation was a very important risk factor of POCD [6,7]. In addition, some studies showed that patients with different ABO blood types had different degrees of stress reaction induced by harmful stimulation [8,9]. Therefore, we speculated that ABO blood types were possibly related to the occurrence of POCD.
However, whether ABO blood types had an effect on POCD and the association between ABO blood types and POCD was not clear. Our study aimed to determine whether ABO blood type had an effect on POCD and the association between ABO blood type and POCD in elderly patients undergoing unilateral total hip arthroplasty surgery in China.
Material and Methods
Patients
This clinical study involved 368 elderly patients undergoing unilateral total hip arthroplasty surgery (age >60 years, American Society of Anesthesiologists [ASA] grade I–III) at the Affiliated Hospital of Southwest Medical University, Luzhou, China, between April 2014 and April 2016. Exclusion criteria were: (i) history of neurologic or psychiatric disease (e.g., depression, Alzheimer’s disease, stroke, and psychosis); (ii) current use of antidepressant or antianxiety medication; (iii) history of drug dependence or alcohol abuse; (iv) history of severe coronary artery, peripheral arterial, or cerebrovascular disease, or severe heart, lung, liver, or kidney disease; (v) severe visual, auditory, or motor disability; and (vi) preoperative hemoglobin <85 g/l. Written informed consent was obtained from the participants prior to enrolment and the study was approved by the Affiliated Hospital of Southwest Medical University Health and the Human Research Ethics Committee. The registration was completed (Research Registry UIN: researchregistry1669).
Anesthesia and surgery
All unilateral total hip arthroplasty surgeries were performed by the same surgery team. No preoperative medication was administered. The protocols of anesthesia were standardized: induction with midazolam (0.03–0.04 mg/kg, i.v.), fentanyl (0.002–0.003 mg/kg, i.v.), vecuronium (0.15–0.2 mg/kg, i.v.), propofol (1.5–2.0 mg/kg, i.v.); maintenance with propofol (6–10 mg/kg/h, continuous i.v. infusion), remifentanil (9–12 ug/kg/h, continuous i.v. infusion), fentanyl (intermittent i.v. infusion), and vecuronium (intermittent i.v. infusion). Bispectral indices (BIS) were monitored during the operation and a target range of 30–60 was maintained during anesthesia.
All of the enrolled patients accepted postoperative analgesia via a patient-controlled analgesia device for the last 72 h after surgery (a constant infusion rate of 2 mL/h with a lock time of 15 min) of 1.5 mg of fentanyl, 12 mg of tropisetron plus 5–10 mg of butorphanol tartrate according to the patients’ age, weight, and ASA (American Society of Anesthesiologists) classification.
Study tools
Basic information: The basic information of enrolled elderly patients was measured by 2 senior nurses, including age, gender, education level, and family structure.
The Mini Mental State Examination (MMSE) test: the Chinese version of the MMSE was used to assess cognitive function before surgery, and on the first, seventh, and thirtieth days after surgery. The MMSE assesses orientation, memory, calculation, language, visual spatial awareness, concentration and attention, and is suitable for detecting cognitive dysfunction.
The Chinese version of the visual analogue scale (VAS) was used to assess pain after the surgery, using a scale ranging from 0 (no pain) to 10 (severe pain).
Study process, POCD assessment, and grouping
The questionnaires were administered by trained study staff. Patients answered the questions and the study staff filled in the questionnaire; samples were collected on the spot. Study staff were blinded to whether the patients had POCD in completing the postoperative questionnaires. According to MMSE score and the ΔMMSE >2, the patient was considered to have developed POCD [10]. In our study, 142 elderly patients were divided into a POCD group and a non-POCD group according to MMSE score, and ABO blood types were analyzed. Secondly, according to ABO blood types, 226 patients were divided into type A group, type B group, type AB group, and type O group, and the occurrence of postoperative cognitive dysfunction was analyzed.
Statistical analysis
All data were analyzed using SPSS 19.0 and GraphPad Prism 5.0. The data are presented as the mean ±SD or n (%). The unpaired t test was used for statistical analysis of continuous data, and the chi-square test was used for statistical analysis of categorical data. In the presence of 3 or more independent variables, ratios and percentages were used to determine the difference with the multiwall chi-square test. A P value <0.05 was considered to represent a statistically significant difference.
Results
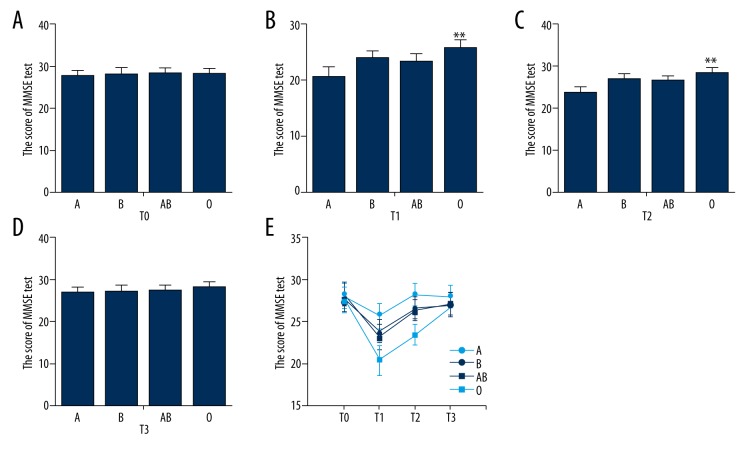
The study analyzed data from 380 elderly patients undergoing unilateral total hip arthroplasty surgery; of these, 12 patients did not meet the inclusion criteria (2 had depressive disease, 3 had Alzheimer’s disease, and 7 had other diseases). Therefore, 368 patients were included in our study. Firstly, according to the occurrence of POCD, 142 elderly patients were enrolled to analyze the ABO blood types. Secondly, according to blood types, 226 additional selected patients were divided into type A group, type B group, type AB group, and type O group to analyze the occurrence of POCD (Figure 1).
Figure 1.
Included and excluded elderly patients in this study.
According to POCD assessment, among 142 elderly patients, the occurrence of POCD was 29.0% at the seventh day after surgery. There was no significant difference between the POCD group and the non-POCD group in gender, whole family structure, pre-existing conditions, and postoperative pain (all P>0.05, Table 1.). The elderly patients who developed POCD had higher age, lower education level, and more intraoperative hypotension (Table 1). In addition, there was a significant difference in distribution of ABO blood type, and elderly patients who developed POCD were more likely to have type A blood and less likely to have type O in ABO/Rh blood type. Among elderly patients who developed POCD, 52.3% had type A blood, 16.7% had type B blood, 9.6% had type AB blood, and 24.4% had type O blood; however, those who did not develop POCD had 43.0%, 15.0%, 8.0%, and 34.0%, respectively (Table 2).
Table 1.
Demographic, clinical and surgical characteristics between POCD patients and non-POCD patients undergoing unilateral total hip arthroplasty surgery.
| Characteristic | POCD (n=43) | Non-POCD (n=99) |
|---|---|---|
| Age (years)a* | 68.5±3.9 | 64.0±3.4 |
| Gender (F/M)b | 23/20 | 54/45 |
| Education (years)a* | 4.5±1.5 | 7.4±1.9 |
| Whole family structureb | 30/43 | 78/99 |
| Hypertensionb | 28/43 | 62/99 |
| Diabetesb | 23/43 | 54/99 |
| COPDb | 15/43 | 24/99 |
| MMSE test before surgerya | 27.6±1.5 | 27.9±1.6 |
| SDS test before surgerya | 52.7±2.6 | 51.3±2.4 |
| SAS test before surgerya | 48.5±2.3 | 47.9±2.9 |
| Time of surgery (min)a | 132.1±16.5 | 128.3±14.4 |
| Time of anaesthesia (min)a | 142.6±6.2 | 144.5±10.3 |
| Intraoperative hypotensionb* | 19/43 | 22/99 |
| Blood loss (ml)a | 1010±100 | 1050+165 |
| Postoperative VASa | 0.68±0.08 | 0.70±0.10 |
Data were presented as mean ±SD or −/−; COPD – chronic obstructive pulmonary disease; FAD – Family Assessment Device; MMSE – Mini-Mental State Examination; SDS – Self-Rating Depression Scale; SAS – Self-Rating Anxiety Scale; VAS – Visual Analogue Scale pain score;
unpaired t tests;
Chi-square test;
statistically significant between-group difference (P<0.05).
Table 2.
Comparison of ABO blood group between the POCD patients and the non-POCD patients.
| ABO blood group** | POCD | Non-POCD |
|---|---|---|
| A blood group | 22/42 (52.3%) | 43/100 (43.0%) |
| B blood group | 7/42 (16.7%) | 15/100 (15.0%) |
| AB blood group | 4/42 (9.6%) | 8/100 (8.0%) |
| O blood group | 9/42 (21.4%) | 34/100 (34.0%) |
P<0.01.
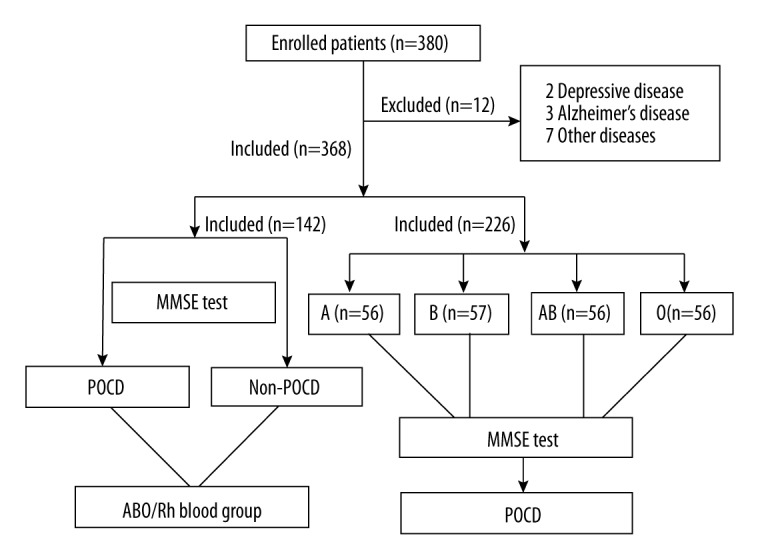
To investigate whether ABO blood types were associated with POCD, 226 selected elderly patients were divided into type A group, type B group, type AB group, and type O type, according to ABO blood types. There was also no significant difference among those groups in age, gender, education, pre-existing condition, and postoperative pain (all P>0.05, Table 3). The results showed that there was no significant difference in MMSE score among those groups before surgery and at the thirtieth day after surgery; however, compared with elderly patients with type A blood, those with type O had the highest MMSE scores on the first and seventh days after surgery (Figure 2). According to POCD assessment, among those patients, the risk of developing POCD was significantly higher in those with type A blood, and the risk of developing POCD was significantly lower in patients with type O blood on the first and seventh days after surgery (Table 4).
Table 3.
Demographic, clinical and surgical characteristics among different group patients undergoing unilateral total hip arthroplasty surgery.
| Characteristic | A (n=56) | B (n=57) | AB (n=56) | O (n=56) |
|---|---|---|---|---|
| Age (years)a | 65.4±5.5 | 66.8±5.3 | 65.8±4.1 | 65.2±4.8 |
| Gender (F/M)b | 24/32 | 26/31 | 25/31 | 26/30 |
| Education (years)a | 5.8±2.4 | 6.2±1.8 | 6.3±2.0 | 6.0±2.1 |
| Whole family structureb | 31/56 | 35/57 | 35/56 | 38/56 |
| Hypertensionb | 32/56 | 29/57 | 31/56 | 34/56 |
| Diabetesb | 30/56 | 28/57 | 27/56 | 30/56 |
| COPDb | 20/56 | 18/57 | 17/56 | 22/56 |
| MMSE test before surgerya | 27.6±1.5 | 27.9±1.6 | 28.2±1.4 | 28.0±1.5 |
| SDS test before surgerya | 51.7±2.6 | 50.3±2.4 | 52.5±2.4 | 51.2±2.8 |
| SAS test before surgerya | 48.7±2.3 | 47.9±2.9 | 47.5±2.1 | 48.9±2.4 |
| Time of surgery (min)a | 132.1±15.5 | 128.3±15.4 | 134.1±16.5 | 129.3±14.4 |
| Time of anaesthesia (min)a | 138.6±7.2 | 140.5±9.3 | 141.5±8.1 | 142.5±6.9 |
| Intraoperative hypotensionb | 18/56 | 20/57 | 22/56 | 22/56 |
| Blood loss (ml)a | 1015±95 | 1000+110 | 1020±95 | 1050+100 |
| Postoperative VASa | 0.68±0.05 | 0.67±0.08 | 0.70±0.1 | 0.65±0.06 |
Data were presented as mean ±SD or −/−; COPD – chronic obstructive pulmonary disease; FAD – Family Assessment Device; MMSE – Mini-Mental State Examination; SDS – Self-Rating Depression Scale; SAS – Self-Rating Anxiety Scale; VAS – Visual Analogue Scale pain score;
unpaired t tests;
Chi-square test;
statistically significant between-group difference (P<0.05).
Figure 2.
(A–E) MMSE scores of elderly patients with different ABO blood type; A – elderly patients with type A; B – elderly patients with type B; AB – elderly patients with type AB; O – elderly patients with type O; T0 – before surgery; T1 – on the first day after surgery; T2 – on the seventh day after surgery; T3 – on the thirtieth day after surgery. ** P<0.01.
Table 4.
Comparison of the occurrence of POCD at different time among different group patients undergoing unilateral total hip arthroplasty surgery.
| ABO blood group | T0 | T1** | T2** | T3 |
|---|---|---|---|---|
| A group | 0/56 | 38/56 (67.8%) | 27/56 (48.2%) | 12/56 (21.4%) |
| B group | 0/57 | 24/57 (42.1%) | 14/57 (24.5%) | 10/57 (17.5%) |
| AB group | 0/56 | 26/56 (38.8%) | 15/56 (26.7%) | 8/56 (14.2%) |
| O group | 0/56 | 17/56 (30.3%) | 10/56 (17.8%) | 6/56 (10.7%) |
T0 – before surgery; T1 – at the first day after surgery; T2 – at the seventh day after surgery; T3 – at the thirtieth day after surgery.
P<0.01.
Discussion
This study found, for the first time, that the ABO blood types of elderly patients are associated with the occurrence of POCD. To investigate the association between ABO blood types and POCD, we divided 142 elderly patients into a POCD group and a non-POCD group according to MMSE scores on the seventh day after surgery. The results showed that elderly patients who developed POCD had higher age, lower education level, and more intraoperative hypotension, and there was a higher percentage of type A blood and a lower percentage of type O blood in the ABO/Rh blood type. To further investigate the association between ABO blood types and POCD, according to ABO blood types, we selected 226 patients and divided them into a type A group, type B group, type AB group, and type O group, and recorded the occurrence of POCD. The results showed that compared with elderly patients with type A blood, those with type O had higher MMSE scores on the first and seventh days after surgery. We also found that the risk of developing POCD was significantly higher in group A and the occurrence of developing POCD was significantly lower in group O on the first and seventh days after surgery. However, the MMSE scores and the occurrence POCD in these groups were not significantly different on the thirtieth day after surgery. Therefore, we found that ABO blood type is associated with POCD, elderly patients undergoing unilateral total hip arthroplasty surgery with type A blood have higher risk of developing early POCD, and those with type O blood are less likely to develop early POCD.
Previous studies reported a relationship between ABO blood type and cognitive impairment. For example, a study showed that having type AB increased risk of cognitive impairment in elderly subjects and showed the role of ABO blood type in cognition and (perhaps) memory [11]. Another study showed that, compared with those with type O, the occurrence of dementia was decreased in subjects with type A [12]. Therefore, these studies support our hypothesis that there is a definite relationship between ABO blood type and POCD. However, in the present study, we found that elderly patients with type A blood had the higher risk of developing early POCD. Possible reasons for this difference are differences in area, disease, and race, and there are many factors that may influence the occurrence of POCD.
In this study, elderly patients with type A blood had lower MMSE scores and higher risk of developing early POCD. Possible mechanisms are that activated reaction from patients with type A blood might be stronger; they may have more catecholamine secretion, platelet adhesion, and intravascular red blood cell aggregation; and they may have hastened ischemia hypoxia and apoptosis of nerve cells in the central nervous system [13,14]. In addition, we also found that type A blood was independently associated with trauma or severe sepsis, which implicates the plasma levels of inflammatory and endothelial injury [15]. We found that patients with type A blood had increased risk of POCD. In this study, elderly patients with type O blood had higher MMSE scores and lower risk of developing early POCD. Possible mechanisms are lower risk factor of heart and cerebrovascular embolization with type O blood [16], which increase risk of POCD. The exact mechanism is still unclear and needs further study.
The study also has some limitations. Firstly, the sample size was small. Secondly, all of the patients in this study only underwent total hip arthroplasty surgery.
Conclusions
ABO blood type has an impact on POCD. Elderly patients undergoing unilateral total hip arthroplasty surgery who have type A blood have higher risk of developing early POCD, and those with type O blood have lower risk of developing early POCD.
Footnotes
Source of support: Departmental sources
Ethics approval
KY2009011 approval was obtained from the Ethics Committee at Affiliated Hospital of Southwest Medical University, Luzhou, China.
Conflicts of interest
All authors declare that they have no conflict of interest.
References
- 1.Hartholt KA, van der Cammen TJ, Klimek M. Postoperative cognitive dysfunction in geriatric patients. Z Gerontol Geriatr. 2012;45:411–16. doi: 10.1007/s00391-012-0326-2. [DOI] [PubMed] [Google Scholar]
- 2.Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet. 1998;351:857–61. doi: 10.1016/s0140-6736(97)07382-0. [DOI] [PubMed] [Google Scholar]
- 3.Schupf N, Tang MX, Albert SM, et al. Decline in cognitive and functional skills increases mortality risk in nondemented elderly. Neurology. 2005;65:1218–26. doi: 10.1212/01.wnl.0000180970.07386.cb. [DOI] [PubMed] [Google Scholar]
- 4.Jungwirth B, Zieglgansberger W, Kochs E, Rammes G. Anesthesia and postoperative cognitive dysfunction (POCD) Mini Rev Med Chem. 2009;9:1568–79. doi: 10.2174/138955709791012229. [DOI] [PubMed] [Google Scholar]
- 5.Rundshagen I. Postoperative cognitive dysfunction. Dtsch Arztebl Int. 2014;111:119–25. doi: 10.3238/arztebl.2014.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y, Chen Z, Zhao Y, et al. Epigenetics as a new therapeutic target for postoperative cognitive dysfunction. Med Hypotheses. 2013;80:249–51. doi: 10.1016/j.mehy.2012.11.041. [DOI] [PubMed] [Google Scholar]
- 7.Chen C, Cheng X, Li J, et al. Extracellular RNAs as a chemical initiator for postoperative cognitive dysfunction. Med Hypotheses. 2016;94:47–50. doi: 10.1016/j.mehy.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 8.Locong AH, Roberge AG. Cortisol and catecholamines response to venisection by humans with different blood groups. Clin Biochem. 1985;18:67–69. doi: 10.1016/s0009-9120(85)80026-6. [DOI] [PubMed] [Google Scholar]
- 9.Moberg L, Korsgren O, Nilsson B. Neutrophilic granulocytes are the predominant cell type infiltrating pancreatic islets in contact with ABO-compatible blood. Clin Exp Immunol. 2005;142:125–31. doi: 10.1111/j.1365-2249.2005.02883.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang J, Chen Z, Liang B, et al. The change of circulating insulin like growth factor binding protein 7 levels may correlate with postoperative cognitive dysfunction. Neurosci Lett. 2015;588:125–30. doi: 10.1016/j.neulet.2014.12.046. [DOI] [PubMed] [Google Scholar]
- 11.Alexander KS, Zakai NA, Gillett S, et al. ABO blood type, factor VIII, and incident cognitive impairment in the REGARDS cohort. Neurology. 2014;83:1271–76. doi: 10.1212/WNL.0000000000000844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vasan SK, Rostgaard K, Ullum H, et al. ABO blood group and dementia risk – a Scandinavian record-linkage study. PLoS One. 2015;10:e0129115. doi: 10.1371/journal.pone.0129115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Franchini M, Mannucci PM. ABO blood group and thrombotic vascular disease. Thromb Haemost. 2014;112:1103–9. doi: 10.1160/TH14-05-0457. [DOI] [PubMed] [Google Scholar]
- 14.Dentali F, Sironi AP, Ageno W, et al. ABO blood group and vascular disease: An update. Semin Thromb Hemost. 2014;40:49–59. doi: 10.1055/s-0033-1363460. [DOI] [PubMed] [Google Scholar]
- 15.Reilly JP, Anderson BJ, Mangalmurti NS, et al. The ABO histo-blood group and AKI in critically ill patients with trauma or sepsis. Clin J Am Soc Nephrol. 2015;10:1911–20. doi: 10.2215/CJN.12201214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blais C, Germain M, Delage G, Gregoire Y. The association between blood group and the risk of vascular disease in Quebec blood donors. Blood Transfus. 2016;14:455–59. doi: 10.2450/2016.0303-15. [DOI] [PMC free article] [PubMed] [Google Scholar]