Abstract
A 41-year-old man with a history of tachycardia refractory to multiple antiarrhythmic drugs was sent to our institution. His 12-lead electrocardiogram demonstrated incessant narrow QRS complex tachycardia with negative P waves in the inferior leads and long RP interval. Occasionally, the tachycardia terminated after a P wave and then was restarted after a sinusal beat. An EP study was performed during tachycardia. Intracardiac electrograms during tachycardia and response to pacing maneuvers are shown. What is the tachycardia mechanism?
Keywords: Orthodromic reciprocating tachycardia, Junctional reciprocating tachycardia, Slowly conducting accessory pathway, Tachycardia-induced cardiomyopathy
1. Case presentation
A 41-year-old man with a history of palpitations refractory to multiple antiarrhythmic agents for several weeks was referred to our department. A 12-lead electrocardiogram (ECG) demonstrated incessant narrow QRS complex tachycardia (cycle length of 580 ms) with prominent negative P waves in the inferior leads and long RP interval. Occasionally, the tachycardia terminated after a P wave and then was restarted after a sinusal beat (Fig. 1). An echocardiography showed mild dilated left heart chambers and moderate ventricular systolic dysfunction.
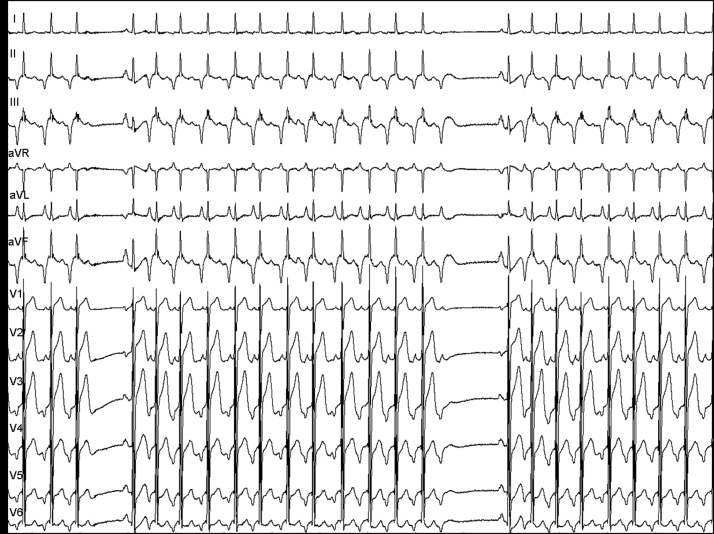
Fig. 1.
Twelve-lead electrocardiogram at the EP Lab: incessant narrow QRS complex tachycardia (cycle length=580 ms), prominent negative P waves in the inferior leads, and long RP interval. Occasionally, the tachycardia terminated after a P wave and then was restarted after a sinusal beat.
An EP study was performed during tachycardia. Two separate quadripolar catheters were placed at the right ventricle and the region of His. Also, a steerable quadripolar catheter was placed in the initial segment of the coronary sinus. The tachycardia cycle length was 600 ms, the HV interval was normal, the VA interval was 470 ms, and the atrial electrogram recorded at the coronary sinus ostium was earliest than of the His.
Tachycardia could be entrained from the right ventricle. The response of tachycardia upon termination of the entrainment is shown in Fig. 2. A ventricular extrastimuli delivered during His bundle refractoriness from the right ventricle reproducibly elicited the response shown in Fig. 2.
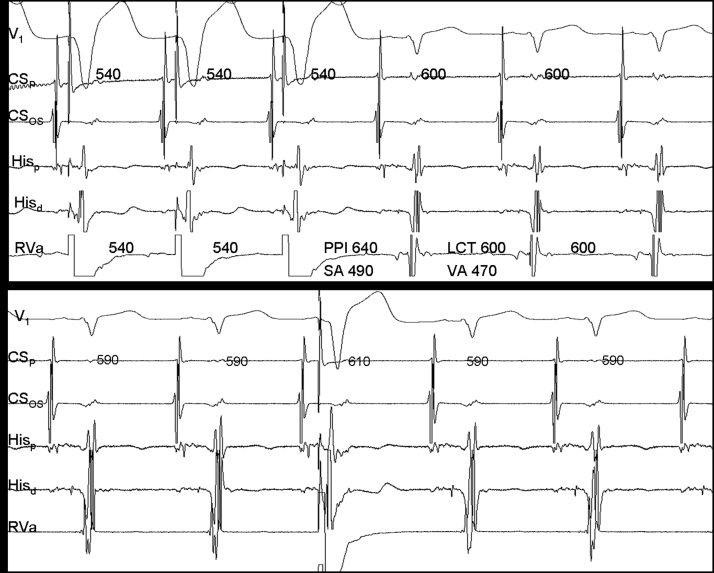
Fig. 2.
Top: Tachycardia response after entrainment from the right ventricular apex: “VAHV” response, PPI-TLC interval 40 ms, and SA-VA interval 20 ms (CSp=proximal coronary sinus, CSos=coronary sinus ostium, Hisp=proximal His-bundle, Hisd=distal His-bundle, RVa=right ventricular apex, PPI=post-pacing interval, TCL=tachycardia cycle length. Intervals in ms). Bottom: A ventricular extrastimuli delivered when the His-bundle is refractory delays the next atrial activation with the same activation sequence (CSp=proximal coronary sinus, CSos=coronary sinus ostium, Hisp=proximal His-bundle, Hisd=distal His-bundle, RVa=right ventricular apex. Intervals in ms).
What is the mechanism of tachycardia?
2. Discussion
The differential diagnosis of a regular, narrow QRS complex tachycardia with long RP interval is orthodromic reciprocating tachycardia using an accessory pathway with slow or decremental conduction properties (permanent form of junctional reciprocating tachycardia [PJRT]), atypical AV nodal reentrant tachycardia (aAVNRT), nodofascicular reentrant tachycardia (NFRT) and atrial tachycardia [1].
The first important ECG finding was the spontaneous termination of tachycardia with AV block. This fact excluded atrial tachycardia. Furthermore, the response of tachycardia after termination of entrainment from the ventricle was a V-A-H-V which also excludes atrial tachycardia [2].
The PPI-TCL difference of 40 ms (<110 ms) and the SA-VA difference of 20 ms (<85 ms) excluded an aAVNRT and almost confirmed a septal accessory pathway [3], [4], [5]. The tachycardia response to the His-bundle refractory ventricular extrastimuli in the case of PJRT can be either advanced or delayed atrial activation. In our case, His-bundle refractory ventricular extrastimuli consistently delayed the next atrial activation while maintaining the same atrial activation sequence. This finding not only confirms the existence of an accessory pathway but their involvement in the tachycardia mechanism. Also, an increase in the SA intervals with the progressive reduction of coupling interval of the ventricular extrastimuli occurred (not shown) which demonstrated the decremental behavior of the accessory pathway.
Long RP tachycardia involving concealed nodofascicular accessory pathways (NFRT) are rare. PJRT and NFRT share electrophysiological features and differential criteria except the ΔAH. ΔAH>40 ms or the paradoxical finding of AH(SVT)<AH(NSR) support the diagnosis of NFRT. During PJRT, the AH interval is a true interval, similar to the AH interval when pacing at the TCL (ΔAH<20 ms). In contrast, during NFRT the AH interval is a pseudo-interval and is shorter than the AH interval when pacing at the TCL. In our case, because of the incessant behavior of the tachycardia, we could not pace the atrium in sinus rhythm. However, the AH(SVT) was similar to the AH(NSR).
PJRT is characterized by an incessant behavior and is associated with tachycardia-induced cardiomyopathy that is reversible with elimination of the tachycardia.
Successful ablation of the accessory pathway was achieved using radiofrequency energy with a standard 4-mm ablation catheter at the bottom of the coronary sinus ostium. Following ablation, no evidence of an accessory pathway conduction or dual AV nodal physiology was demonstrated, and no tachycardia was inducible. One month after the ablation procedure, the size and left ventricular function were normal.
Conflict of interest
All authors declare no conflict of interest related to this study.
References
- 1.Josephson M.E. Supraventricular tachycardias. In: Josephson M.E., editor. Clinical cardiac electrophysiology. Techniques and interpretations. 4th ed. Lippincott Williams & Wilkins; Philadelphia: 2008. pp. 175–284. [Google Scholar]
- 2.Knight B.P., Ebinger M., Oral H. Diagnostic value of tachycardia features and pacing maneuvers during paroxysmal supraventricular tachycardia. J Am Coll Cardiol. 2000;36:574–582. doi: 10.1016/s0735-1097(00)00770-1. [DOI] [PubMed] [Google Scholar]
- 3.Michaud G.F., Tada H., Chough S. Differentiation of atypical AV nodal reentry from orthodromic tachycardia using a septal accessory pathway by the response to ventricular pacing. J Am Coll Cardiol. 2001;38:1163–1167. doi: 10.1016/s0735-1097(01)01480-2. [DOI] [PubMed] [Google Scholar]
- 4.González-Torrecilla E., Almendral J., Atienza F. First post-pacing interval after tachycardia entrainment with correction for atrioventricular node delay: a simpler maneuver for the differential diagnosis of atrioventricular nodal reentrant tachycardias versus orthodromic reciprocating tachycardias. Heart Rhythm. 2006;3:674–679. doi: 10.1016/j.hrthm.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 5.González-Torrecilla E., Almendral J., García-Fernández F.J. Differences in ventriculoatrial intervals during entrainment and tachycardia: a simpler method for distinguishing paroxysmal supraventricular tachycardia with long ventriculoatrial intervals. J Cardiovasc Electrophysiol. 2011;22:915–921. doi: 10.1111/j.1540-8167.2011.02020.x. [DOI] [PubMed] [Google Scholar]