Abstract
Importance
Little contemporary information is available about comparative performance between Veterans Affairs (VA) and non-VA hospitals, particularly related to mortality and readmission rates, 2 important outcomes of care.
Objective
To assess and compare mortality and readmission rates among men in VA and non-VA hospitals. To avoid confounding geographic effects with health care system effects, we studied VA and non-VA hospitals within the same metropolitan statistical area (MSA).
Design
Cross-sectional analysis between 2010 and 2013
Setting
Medicare Standard Analytic Files and Enrollment Database
Participants
Male Medicare Fee-for-Service beneficiaries aged 65 or older hospitalized between 2010 and 2013 in VA and non-VA acute care hospitals for acute myocardial infarction (AMI), heart failure (HF), or pneumonia.
Exposures
Hospitalization in a VA or non-VA hospital in urban MSAs that contained at least 1 VA and non-VA hospital
Main Outcomes and Measures
For each condition, 30-day risk-standardized mortality rates and risk-standardized readmission rates for VA and non-VA hospitals. Mean-aggregated within-MSA differences in mortality and readmission rates were also assessed.
Results
We studied 104 VA and 1,513 non-VA hospitals, with each condition-outcome analysis cohort for VA and non-VA hospitals containing at least 7,900 patients, in 92 MSAs. Mortality rates were lower in VA hospitals than non-VA hospitals for AMI (13.5% vs. 13.7%, p=0.02; −0.2 percentage point difference) and HF (11.4% vs. 11.9%, p=0.008; −0.5 percentage point difference), but higher for pneumonia (12.6% vs. 12.2%, p<0.05; 0.4 percentage point difference). In contrast, readmission rates were higher in VA hospitals for all 3 conditions (AMI: 17.8% vs. 17.2%, 0.6 percentage point difference; HF: 24.7% vs. 23.5%, 1.2 percentage point difference; pneumonia: 19.4% vs. 18.7%, 0.7 percentage point difference, all p<0.001). In within-MSA comparisons, VA hospitals had lower mortality rates for AMI (percentage point difference: −0.22, 95% CI: −0.40 to −0.04) and HF (−0.63, 95% CI: −0.95 to −0.31), and mortality rates for pneumonia were not significantly different (−0.03, 95% CI: −0.46 to 0.40); however, VA hospitals had higher readmission rates (AMI: 0.62, 95% CI: 0.48 to 0.75; HF: 0.97, 95% CI: 0.59 to 1.34; pneumonia: 0.66, 95% CI: 0.41 to 0.91).
Conclusion and Relevance
Among older men with AMI, HF, and pneumonia, hospitalization at VA hospitals, compared with hospitalization at non-VA hospitals, was associated with lower risk-standardized 30-day all-cause mortality rates for AMI and HF, and higher risk-standardized 30 day all-cause readmission rates for all 3 conditions, both nationally and within similar geographic areas, although absolute differences between these outcomes at VA and non-VA hospitals were small.
INTRODUCTION
The Department of Veterans Affairs (VA) and the Centers for Medicare & Medicaid Services (CMS) are collaborating in calculating and reporting hospital performance. The alignment of reporting systems provides an opportunity to compare performance of VA and non-VA hospitals directly with respect to risk-adjusted outcomes for key conditions, including acute myocardial infarction (AMI), heart failure (HF), and pneumonia. Prior studies, which are a decade or more old or are not nationally representative, and occurred before we had validated hospital-level outcomes measures, found that patients who received care at VA hospitals had either similar or lower mortality rates than patients who received care at non-VA hospitals;1–4 with respect to readmission rates, a study in New York found that elderly patients had higher rates of 30-day readmission in VA hospitals compared with non-VA hospitals.5 Contemporary knowledge about hospital-level outcomes would help to better understand quality of care for the approximately 9 million veterans enrolled in the nation’s largest integrated healthcare system compared with those in Medicare.6
Accordingly, we assessed and compared 30-day all-cause risk-standardized mortality rates and 30-day all-cause risk-standardized readmission rates in VA hospitals and non-VA hospitals for patients hospitalized with AMI, HF, and pneumonia. We applied the measure methodology that is utilized to calculate publicly reported mortality and readmission rates. To avoid confounding geographic effects with health care system effects, we studied VA and non-VA hospitals within the same metropolitan statistical area (MSA).
METHODS
Study Population
We utilized a combined dataset of the CMS Standard Analytic Files and Enrollment Database together with VA administrative claims data to identify Medicare Fee-for-Service beneficiaries aged 65 years or older hospitalized from July 1, 2010 through June 30, 2013 with a principal discharge diagnosis of AMI, HF, or pneumonia in VA or non-VA acute-care hospitals in the U.S. using International Classification of Diseases, Ninth Revision, Clinical Modification codes identical to those utilized in the publicly reported mortality and readmission measures;7–12 for VA beneficiaries, we only studied those enrolled in the Medicare Fee-for-Service program. These databases include enrollment status, admissions, patient demographic information, inpatient and outpatient diagnosis codes, mortality, and readmissions; they also include unique patient identifiers that enable the identification of patients across VA and non-VA systems. We excluded beneficiaries for whom a complete claims history for the 12-month period preceding the claim was unavailable because of the use of data in the year before hospitalization in risk adjustment. We included patients admitted to hospitals in urban MSAs that contained at least 1 VA and non-VA hospital to reduce confounding geographic effects from health system effects (see eTable 1 for VA hospitals included in the study).13,14 This also helps minimize potential confounding from the inclusion of non-urban hospitals, given that the challenges faced by rural and urban hospitals differ.15,16 Because >90% of patients in VA hospitals are male,17 we restricted our analyses to men.
The Yale University Human Investigation Committee approved the study and waived the requirement for informed consent.
Risk-Standardized Mortality and Readmission Rates
To calculate 30-day all-cause risk-standardized mortality rates and 30-day all-cause risk-standardized readmission rates for each condition, we used the specifications employed in the measures developed for CMS and endorsed by the National Quality Forum.7–11 Briefly, the technique of risk-adjustment employs a hierarchical logistic regression model to create a hospital-level 30-day risk-standardized mortality or readmission rate. This modeling appropriately accounts for the structure of the data (patients clustered within hospitals), and the underlying risk due to patients’ age and comorbidities when estimating hospital mortality/readmission rates. This approach simultaneously models 2 levels (patient and hospital) to account for the variance in patient outcomes within and between hospitals. At the patient level, the model uses the log-odds of mortality/readmission within 30-days of admission/discharge as the dependent variable and age and selected clinical covariates as the independent variables (or predictors). The second level models the hospital-specific intercepts as arising from a normal distribution. The hospital-specific intercept, or hospital-specific effect, represents the hospital contribution to the risk of mortality/readmission after accounting for patient risk, and can be inferred as a measure of quality. The hospital-specific intercepts are given a distribution in order to account for the clustering (non-independence) of patients within the same hospital.
We defined 30-day mortality as death from any cause within 30 days of the day of admission for an index hospitalization for AMI, HF, or pneumonia. Readmission was defined as ≥1 re-hospitalization for any unplanned cause to any acute care hospital within 30 days of the day of discharge for an index hospitalization for AMI, HF, or pneumonia among patients surviving the index hospitalization; planned readmissions were identified and excluded using planned readmission algorithms (Version 2.1).7–11,18 We utilized the top 25 diagnosis and procedure codes for risk-adjustment across all outcomes and conditions in both VA and non-VA hospitals.
For the mortality cohort for each condition, we randomly selected 1 admission per year for patients with multiple admissions for the same diagnosis during the study period.13 For individuals admitted to both a VA and non-VA hospital (<2.1% of patients for each condition-outcome analysis in our cohort; Table 1), we randomly selected 1 admission from all admissions regardless of location hospitalized. For transfers between hospitals, relevant hospitalizations were linked into a single episode of care, with mortality attributed to the hospital to which the patient was first admitted; transfers between VA and non-VA hospitals were treated similarly to transfers between VA and VA, or non-VA and non-VA, hospitals.
Table 1.
Characteristics of Medicare Beneficiaries Hospitalized in Veterans Affairs and non-Veterans Affairs Hospitals for Acute Myocardial Infarction, Heart Failure, and Pneumonia, 2010–2013.
| Acute myocardial infarction | Heart failure | Pneumonia | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mortality | Readmission | Mortality | Readmission | Mortality | Readmission | |||||||
| VA | Non-VA | VA | Non-VA | VA | Non-VA | VA | Non-VA | VA | Non-VA | VA | Non-VA | |
| Total no. of admissions | 8,012 | 124,220 | 7,929 | 132,276 | 22,882 | 215,312 | 26,231 | 269,856 | 21,092 | 190,798 | 21,229 | 205,060 |
| Total no. of hospitals | 103 | 1,439 | 103 | 1,420 | 104 | 1,500 | 104 | 1,500 | 104 | 1,505 | 104 | 1,506 |
| Demographics | ||||||||||||
| Age, mean (SD), y | 76.2 (8.4) | 77.8 (8.0) | 75.5 (8.1) | 77.5 (7.9) | 77.3 (8.4) | 80.0 (8.1) | 77.0 (8.3) | 79.7 (8.0) | 77.9 (8.5) | 79.8 (8.1) | 77.5 (8.4) | 79.6 (8.1) |
| Race, % | ||||||||||||
| White | 77.0 | 86.1 | 84.4 | 86.4 | 72.6 | 82.4 | 78.8 | 81.6 | 78.3 | 85.2 | 86.1 | 85.2 |
| Black | 11.4 | 7.9 | 12.1 | 7.9 | 15.9 | 12.0 | 18.4 | 12.8 | 10.2 | 8.3 | 11.1 | 8.3 |
| Other | 3.1 | 5.8 | 3.3 | 5.5 | 2.6 | 5.4 | 2.7 | 5.5 | 2.7 | 6.4 | 2.6 | 6.3 |
| Unknown | 8.5 | 0.2 | 0.2 | 0.2 | 8.9 | 0.1 | 0.2 | 0.1 | 8.8 | 0.2 | 0.2 | 0.2 |
| Cardiovascular medical history, % | ||||||||||||
| History of PCI | 12.8 | 18.1 | 14.7 | 19.7 | 7.3 | 15.5 | -- | -- | 3.8 | 9.5 | -- | -- |
| History of CABG | 17.1 | 14.2 | 17.2 | 14.1 | 17.6 | 25.5 | 18.5 | 26.5 | 7.7 | 14.0 | 8.0 | 14.1 |
| Heart failure | 32.8 | 29.2 | 34.6 | 31.4 | 77.7 | 76.4 | 80.7 | 78.9 | 33.7 | 39.2 | 35.4 | 39.3 |
| Anterior myocardial infarction | 3.7 | 9.0 | 3.2 | 7.8 | -- | -- | -- | -- | -- | -- | -- | -- |
| Inferior, lateral, or posterior myocardial infarction | 5.9 | 13.3 | 5.7 | 12.0 | -- | -- | -- | -- | -- | -- | -- | -- |
| Acute coronary syndromes | 23.1 | 20.2 | 25.0 | 22.6 | 14.9 | 18.0 | 16.2 | 19.2 | 6.8 | 8.9 | 7.4 | 8.9 |
| Coronary atherosclerosis | 85.7 | 88.9 | 88.5 | 91.5 | 74.7 | 81.9 | 77.0 | 83.4 | 47.5 | 58.6 | 49.0 | 58.7 |
| Cardiopulmonary-respiratory failure and shock | 9.3 | 9.5 | -- | -- | 19.3 | 25.5 | 21.5 | 27.0 | 17.8 | 21.9 | 20.3 | 22.5 |
| Valvular heart disease | 19.1 | 29.5 | 19.1 | 30.2 | 32.2 | 52.4 | 33.7 | 53.5 | -- | -- | 14.2 | 26.8 |
| Arrhythmia | -- | -- | 34.8 | 37.2 | -- | -- | 67.9 | 73.1 | -- | -- | 42.0 | 50.0 |
| Other unspecified heart disease | -- | -- | -- | -- | -- | -- | 21.7 | 33.8 | -- | -- | -- | -- |
| Comorbid conditions, % | ||||||||||||
| Hypertension | 92.7 | 86.3 | -- | -- | 94.3 | 91.5 | -- | -- | 86.1 | 85.6 | -- | -- |
| Stroke | 10.4 | 7.5 | 10.5 | 7.4 | 11.4 | 10.0 | 11.5 | 10.0 | 11.1 | 10.6 | 11.2 | 10.5 |
| Cerebrovascular disease | 16.6 | 20.7 | 17.2 | 21.0 | -- | -- | -- | -- | 16.6 | 24.3 | -- | -- |
| Renal failure | 34.3 | 27.0 | 35.4 | 28.3 | 52.6 | 53.5 | 55.2 | 55.3 | 32.6 | 34.0 | 33.7 | 34.0 |
| Chronic obstructive pulmonary disease | 31.7 | 29.4 | 32.8 | 29.8 | 51.0 | 48.8 | 53.3 | 49.4 | 59.1 | 54.1 | 61.3 | 54.4 |
| Pneumonia | 20.8 | 23.1 | 20.6 | 22.5 | 32.0 | 45.5 | 33.5 | 45.7 | 39.8 | 42.8 | 43.0 | 44.0 |
| Diabetes | 55.1 | 46.9 | 56.4 | 47.6 | 60.8 | 55.5 | 61.8 | 56.3 | -- | -- | 44.5 | 44.9 |
| Protein-calorie malnutrition | 3.6 | 6.3 | 3.6 | 5.9 | 4.7 | 10.4 | 4.8 | 9.8 | 8.3 | 14.3 | 8.6 | 13.6 |
| Dementia | 16.2 | 17.3 | 14.8 | 16.7 | 17.7 | 22.5 | 17.3 | 21.8 | 26.5 | 30.2 | 25.9 | 29.8 |
| Functional disability | 8.9 | 6.6 | 9.1 | 6.6 | 9.1 | 9.2 | 9.1 | 9.2 | 10.1 | 10.3 | 10.4 | 10.3 |
| Peripheral vascular disease | 28.8 | 28.6 | -- | -- | 34.2 | 42.1 | -- | -- | 28.3 | 35.8 | -- | -- |
| Metastatic cancer | 5.3 | 4.7 | 2.7 | 2.5 | 4.7 | 5.6 | 27.1 | 27.1 | 12.8 | 12.5 | 32.0 | 29.6 |
| Trauma in last year | 29.6 | 28.4 | -- | -- | 34.4 | 38.5 | -- | -- | 35.1 | 38.9 | -- | -- |
| Major psychiatric disorders | 11.7 | 6.9 | -- | -- | 12.3 | 9.6 | 12.8 | 9.7 | 17.0 | 12.8 | 17.2 | 12.9 |
| Chronic liver disease | 2.4 | 1.7 | -- | -- | 4.7 | 3.8 | 10.8 | 12.6 | 3.3 | 2.7 | -- | -- |
| Severe hematological disorders | -- | -- | -- | -- | -- | -- | 3.2 | 4.4 | 3.1 | 4.8 | 3.3 | 4.6 |
| Iron deficiency | -- | -- | 41.9 | 45.6 | -- | -- | 55.4 | 62.6 | 52.8 | 58.9 | 53.5 | 58.5 |
| Depression | -- | -- | -- | -- | -- | -- | 21.2 | 15.5 | 23.6 | 17.9 | -- | -- |
| Seizure disorders or convulsions | -- | -- | -- | -- | -- | -- | -- | -- | 5.2 | 6.6 | -- | -- |
| Fibrosis of lung or other chronic lung disorders | -- | -- | -- | -- | -- | -- | 7.8 | 12.2 | 10.7 | 16.7 | 11.2 | 16.8 |
| Asthma | -- | -- | 3.5 | 5.3 | -- | -- | 4.3 | 7.7 | 5.2 | 9.0 | 5.4 | 9.3 |
| End-stage renal disease | -- | -- | 3.6 | 3.8 | -- | -- | 1.9 | 5.7 | -- | -- | 2.5 | 4.4 |
| Nephritis | -- | -- | -- | -- | -- | -- | 4.2 | 4.4 | -- | -- | -- | -- |
| Urinary tract infection | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 18.5 | 19.7 |
| Urinary tract disorders | -- | -- | 19.1 | 24.7 | -- | -- | 27.1 | 38.2 | -- | -- | 21.8 | 29.8 |
| Pleural effusion/pneumothorax | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 11.5 | 19.1 |
| Other lung disorders | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 34.1 | 47.6 |
| Fluid and electrolyte disorders | -- | -- | 25.8 | 26.1 | -- | -- | 41.5 | 47.7 | -- | -- | 35.5 | 40.2 |
| Other psychiatric disorders | -- | -- | -- | -- | -- | -- | 16.3 | 12.8 | -- | -- | 18.8 | 14.2 |
| Drug/Alcohol abuse | -- | -- | -- | -- | -- | -- | 23.5 | 15.5 | -- | -- | 26.8 | 16.7 |
| Peptic ulcer and other specified GI disorders | -- | -- | -- | -- | -- | -- | 13.7 | 15.6 | -- | -- | -- | -- |
| Other GI disorders | -- | -- | -- | -- | -- | -- | 58.9 | 58.2 | -- | -- | 64.7 | 61.8 |
| Parkinson’s and Huntington’s Diseases | -- | -- | -- | -- | -- | -- | -- | -- | 4.1 | 5.3 | -- | -- |
| Vertebral fractures | -- | -- | -- | -- | -- | -- | -- | -- | 2.2 | 3.8 | 2.2 | 3.8 |
| Other injuries | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 34.5 | 37.0 |
| Decubitus skin ulcer | -- | -- | 8.6 | 7.7 | -- | -- | 14.3 | 16.0 | -- | -- | 10.7 | 12.6 |
| Other history of infection | -- | -- | 27.9 | 25.6 | -- | -- | -- | -- | -- | -- | 37.4 | 39.6 |
| Septicemia/Shock | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 7.8 | 10.0 |
| Percent of patients hospitalized in both VA and non-VA hospitals | 0.06 | 0.97 | 0.27 | 2.07 | 0.13 | 1.55 | ||||||
| Percent of patients discharged alive who died without being readmitted within 30 days, % | N/A | 4.4 | 4.5 | N/A | 4.6 | 5.6 | N/A | 6.0 | 6.0 | |||
| Percent of patients readmitted to non-VA hospitals within 30 days among those initially hospitalized in VA hospitals, % | N/A | 11.4 | N/A | 14.1 | N/A | 12.2 | ||||||
| Percent of patients readmitted to VA hospitals within 30 days among those initially hospitalized in non-VA hospitals, % | N/A | 0.3 | N/A | 0.3 | N/A | 0.3 | ||||||
PCI: percutaneous coronary intervention; CABG: coronary artery bypass graft; y: years; N/A: not applicable
“—”: Not included in risk-adjustment of publicly-reported measures for a given condition and outcome
For the readmission cohort for each condition, we included all admissions for patients with multiple admissions for the same diagnosis during any study year. Hospitalizations within 30 days of discharge from an index hospitalization were considered readmissions and not additional index hospitalizations. Readmission to another system (VA to non-VA or non-VA to VA) was counted as a readmission attributed to the index hospital. For mortality, transfers were linked into a single episode of care, with readmissions attributed to the hospital that discharged the patient to a non-acute setting; transfers between VA and non-VA hospitals were treated as described above. We also calculated the number of patients who died after discharge, but before 30-day readmission, for each condition and within each healthcare system.
Hospital Characteristics
Hospital characteristics, other than Medicare condition-specific 3-year volumes, which were derived from the Standard Analytic Files and Enrollment Database, were derived from the American Hospital Association Annual Survey in the corresponding year.19 These variables include total staffed beds, ownership type, region, teaching status, Joint Commission accreditation, and hospital capacity to provide coronary artery bypass graft surgery or percutaneous coronary intervention. MSA population size data, from April 1, 2010 to July 1, 2012, was obtained from the U.S. Census Bureau.20
Patient Characteristics
Demographic information included age and race (white, black, other); there are no measures of socioeconomic status available in these data. Race (white, black other) for these categories is derived from the Social Security Administration21 and was assessed as a descriptive characteristic of the populations studied. We defined comorbidities according to the specifications employed by CMS to profile hospitals, using principal and secondary diagnosis codes from hospitalizations in the 12 months before the index hospitalization (See eTable 2 for medical history characteristics).7–11
Statistical Analysis
We compared VA and non-VA hospitals for differences in both patient factors (demographic and clinical characteristics) and hospital factors. For the 3 conditions, within the full 3-year pooled sample, we estimated mortality and readmission rates for each VA and non-VA hospital using hierarchical logistic regression models. Each model included age and selected clinical covariates (eTable 2) as well as a hospital-specific random effects intercept. Risk-standardized mortality and readmission rates are calculated as the ratio of the number of “predicted” outcomes to the number of “expected” outcomes (death or readmission), multiplied by the unadjusted rate of the given outcome within our overall sample. We calculated aggregate mortality and readmission for each condition-outcome group for VA and non-VA hospitals by weighting hospital-specific mortality or readmission rate estimates by a hospital’s condition-specific volume.
In addition, for each condition, we calculated the mean-aggregated MSA-specific mortality and readmission rates stratified by VA hospital status to reduce confounding geographic effects from health system effects and minimize potential confounding from the inclusion of non-urban hospitals, and determined the average within-MSA difference between VA and non-VA hospitals. As above, within MSAs, we weighted hospital-specific mortality or readmission rates by their condition-specific volume. After aggregating outcome rates for the VA hospitals and non-VA hospitals within an MSA, we calculated the difference between the rates of VA and non-VA hospitals in each MSA, and then calculated the mean and 95% confidence interval of the differences among all MSAs in our sample. Differences were presented as the rate in VA hospitals minus the rate in non-VA hospitals; values <0 indicate a lower mortality or readmission rate for VA hospitals.
Analyses were performed separately for AMI, HF, and pneumonia. For all 3 conditions, we calculated the mean (95% confidence interval) mortality or readmission rate grouped by VA and non-VA hospitals. The corresponding P values were obtained using t-tests. In the above calculations, weights were added by the condition-specific number of hospitalizations to account for the variability in hospital sample sizes. We considered P values <0.05 (2-sided) to be statistically significant. Analyses were conducted using SAS software, Version 9.3 (SAS Institute, Inc., Cary, NC).
RESULTS
Study Sample
Among 381 MSAs in the U.S., 92 had at least 1 VA and 1 non-VA hospital; 7 MSAs had >1 VA hospital. We studied 104 VA and 1,513 non-VA hospitals, with each condition-outcome analysis cohort for VA and non-VA hospitals containing at least 7,900 patients. For analyses focused on AMI hospitalizations, there were 1,542 hospitals (103 VA hospitals with 8,012 patients and 1,439 non-VA hospitals with 124,220 patients) for mortality analyses and 1,523 hospitals (103 VA hospitals with 7,929 patients and 1,420 non-VA hospitals with 132,276 patients) for readmission analyses; for HF, 1,604 hospitals (104 VA hospitals with 22,882 patients and 1,500 non-VA hospitals with 215,312 patients) for mortality and 1,604 hospitals (104 VA hospitals with 26,231 patients and 1,500 non-VA hospitals with 269,856 patients) for readmission; and for pneumonia, 1,609 hospitals (104 VA hospitals with 21,092 patients and 1,505 non-VA hospitals with 190,798 patients) for mortality and 1,610 hospitals (104 VA hospitals with 21,229 patients and 1,506 non-VA hospitals with 205,060 patients) for readmission (Table 1). There were 124 VA medical centers in our dataset (eTable 1).
Patient Characteristics
For the mortality and readmission analyses for all 3 conditions, patients who received care in VA hospitals were younger and generally less likely to be white than those who received care in non-VA hospitals (Table 1). Among patients hospitalized for AMI, VA patients were more likely to have a history of HF or diabetes. Among patients hospitalized for HF, VA patients were also more likely to have a history of HF or diabetes, but less likely to have a documented history of coronary atherosclerosis or valvular heart disease. Among patients hospitalized for pneumonia, VA patients were more likely to have a history of chronic obstructive pulmonary disease and less likely to have a history of pneumonia, protein-calorie malnutrition, or fibrosis of the lung or other chronic lung disorders.
Hospital Characteristics
VA hospitals were more likely to be teaching hospitals and were larger, with a greater number of hospital beds (p<0.05 for both) (Table 2). For HF and pneumonia hospitalizations, but not for AMI, a greater proportion of VA hospitals had 3-year condition-specific volumes >150 patients.
Table 2.
Hospital Characteristics for Veterans Affairs and non-Veterans Affairs Hospitals, 2010–2013.
| Variable (%) | Acute myocardial infarction | Heart failure | Pneumonia | ||||||
|---|---|---|---|---|---|---|---|---|---|
| VA | Non-VA | P-value for difference | VA | Non-VA | P-value for difference | VA | Non-VA | P-value for difference | |
| Total no. of hospitals* | 99 (6.7) | 1373 (93.3) | -- | 100 (6.5) | 1428 (93.5) | -- | 100 (6.5) | 1434 (93.5) | -- |
| Total no. of staffed beds | |||||||||
| ≤50 | 3 (3.0) | 107 (7.8) | 0.04 | 3 (3.0) | 136 (9.5) | 0.04 | 3 (3.0) | 143 (10.0) | 0.03 |
| 51–100 | 18 (18.2) | 140 (10.2) | 18 (18.0) | 154 (10.8) | 18 (18.0) | 153 (10.7) | |||
| 101–200 | 21 (21.2) | 356 (25.9) | 22 (22.0) | 364 (25.5) | 22 (22.0) | 363 (25.3) | |||
| 201–300 | 24 (24.2) | 272 (19.8) | 24 (24.0) | 275 (19.3) | 24 (24.0) | 275 (19.2) | |||
| >300 | 33 (33.3) | 498 (36.3) | 33 (33.0) | 499 (34.9) | 33 (33.0) | 500 (34.9) | |||
| Medicare condition-specific 3-y volume | |||||||||
| ≤15 | 13 (13.1) | 162 (11.8) | <0.001 | 1 (1.0) | 59 (4.1) | <0.001 | 1 (1.0) | 50 (3.5) | <0.001 |
| 16–45 | 15 (15.2) | 206 (15.0) | 2 (2.0) | 106 (7.4) | 0 (0.0) | 81 (5.6) | |||
| 46–150 | 52 (52.5) | 412 (30.0) | 23 (23.0) | 340 (23.8) | 26 (26.0) | 358 (25.0) | |||
| 151–480 | 18 (18.2) | 511 (37.2) | 66 (66.0) | 598 (41.9) | 67 (67.0) | 702 (49.0) | |||
| >480 | 1 (1.0) | 82 (6.0) | 8 (8.0) | 325 (22.8) | 6 (6.0) | 243 (16.9) | |||
| Ownership | |||||||||
| Public | 99 (100.0) | 161 (11.7) | <0.001 | 100 (100.0) | 179 (12.5) | <0.001 | 100 (100.0) | 181 (12.6) | <0.001 |
| Private not-for-profit | 0 (0.0) | 920 (67.0) | 0 (0.0) | 943 (66.0) | 0 (0.0) | 943 (65.8) | |||
| Private for-profit | 0 (0.0) | 292 (21.3) | 0 (0.0) | 306 (21.4) | 0 (0.0) | 310 (21.6) | |||
| Cardiac facilities | |||||||||
| Open heart surgery | 24 (24.2) | 1014 (73.9) | <0.001 | 24 (24.0) | 1040 (72.8) | <0.001 | 24 (24.0) | 1042 (72.7) | <0.001 |
| Interventional catheterization only | 10 (10.1) | 87 (6.3) | 10 (10.0) | 88 (6.2) | 10 (10.0) | 87 (6.1) | |||
| No interventional catheterization | 9 (9.1) | 135 (9.8) | 9 (9.0) | 145 (10.2) | 9 (9.0) | 145 (10.1) | |||
| Unknown | 56 (56.6) | 137 (10.0) | 57 (57.0) | 155 (10.9) | 57 (57.0) | 160 (11.2) | |||
| Joint Commission accreditation | |||||||||
| No | 1 (1.0) | 178 (13.0) | <0.001 | 1 (1.0) | 201 (14.1) | <0.001 | 1 (1.0) | 205 (14.3) | <0.001 |
| Yes | 98 (99.0) | 1195 (87.0) | 99 (99.0) | 1227 (85.9) | 99 (99.0) | 1229 (85.7) | |||
| Teaching status | |||||||||
| COTH member | 40 (40.4) | 178 (13.0) | <0.001 | 40 (40.0) | 180 (12.6) | <0.001 | 40 (40.0) | 180 (12.6) | <0.001 |
| Residency or fellowship program affiliated | 49 (49.5) | 339 (24.7) | 50 (50.0) | 350 (24.5) | 50 (50.0) | 350 (24.4) | |||
| Nonteaching | 10 (10.1) | 856 (62.3) | 10 (10.0) | 898 (62.9) | 10 (10.0) | 904 (63.0) | |||
| Census division | |||||||||
| New England | 1 (1.0) | 14 (1.0) | 0.31 | 1 (1.0) | 14 (1.0) | 0.43 | 1 (1.0) | 14 (1.0) | 0.43 |
| Middle Atlantic | 13 (13.1) | 224 (16.3) | 14 (14.0) | 227 (15.9) | 14 (14.0) | 227 (15.8) | |||
| South Atlantic | 9 (9.1) | 82 (6.0) | 9 (9.0) | 89 (6.2) | 9 (9.0) | 90 (6.3) | |||
| East North Central | 20 (20.2) | 226 (16.5) | 20 (20.0) | 234 (16.4) | 20 (20.0) | 234 (16.3) | |||
| East South Central | 11 (11.1) | 106 (7.7) | 11 (11.0) | 116 (8.1) | 11 (11.0) | 115 (8.0) | |||
| West North Central | 14 (14.1) | 232 (16.9) | 14 (14.0) | 238 (16.7) | 14 (14.0) | 238 (16.6) | |||
| West South Central | 10 (10.1) | 152 (11.1) | 10 (10.0) | 160 (11.2) | 10 (10.0) | 164 (11.4) | |||
| Mountain | 10 (10.1) | 79 (5.8) | 10 (10.0) | 84 (5.9) | 10 (10.0) | 85 (5.9) | |||
| Pacific | 10 (10.1) | 233 (17.0) | 10 (10.0) | 238 (16.7) | 10 (10.0) | 239 (16.7) | |||
| Other | 1 (1.0) | 25 (1.8) | 1 (1.0) | 28 (2.0) | 1 (1.0) | 28 (2.0) | |||
| MSA population size | |||||||||
| <100,000 | 2 (2.0) | 3 (0.2) | <0.001 | 2 (2.0) | 3 (0.2) | <0.001 | 2 (2.0) | 3 (0.2) | <0.001 |
| 100,000–250,000 | 13 (13.1) | 30 (2.2) | 13 (13.0) | 34 (2.4) | 13 (13.0) | 34 (2.4) | |||
| 250,000–500,000 | 17 (17.2) | 99 (7.2) | 17 (17.0) | 98 (6.9) | 17 (17.0) | 100 (7.0) | |||
| 500,000–1,000,000 | 20 (20.2) | 279 (20.3) | 20 (20.0) | 291 (20.4) | 20 (20.0) | 292 (20.4) | |||
| 1,000,000–2,500,000 | 22 (22.2) | 417 (30.4) | 23 (23.0) | 438 (30.7) | 23 (23.0) | 441 (30.8) | |||
| ≥2,500,000 | 22 (22.2) | 426 (31.0) | 22 (22.0) | 440 (30.8) | 22 (22.0) | 440 (30.7) | |||
| Unknown | 3 (3.0) | 119 (8.7) | 3 (3.0) | 124 (8.7) | 3 (3.0) | 124 (8.6) | |||
Hospital characteristics were not available for 4 VA hospitals and several non-VA hospitals.
COTH = Council of Teaching Hospitals; VA = Veterans Affairs
30-day Mortality Rates
Before risk-adjustment, VA hospitals had lower mortality rates than non-VA hospitals across all 3 conditions (Table 3). After risk-adjustment, VA hospitals had lower mortality rates than non-VA hospitals for AMI (13.5%, 95% CI: 13.4 to 13.7, versus 13.7%, 95% CI: 13.6 to 13.7; −0.2 percentage point difference) and HF (11.4%, 95% CI: 11.1 to 11.8, versus 11.9%, 95% CI: 11.8 to 11.9; −0.5 percentage point difference) (p<0.03 for both; Table 3, Figure 1). However, for pneumonia, VA hospitals had higher mortality rates than non-VA hospitals (12.6%, 95% CI: 12.2 to 13.1, versus 12.2%, 95% CI: 12.1 to 12.3, p<0.05; 0.4 percentage point difference). The distribution of mortality rate performance was not markedly different between VA and non-VA hospitals for all 3 conditions (Figure 1 and eFigure; eTables 3 and 4).
Table 3.
Thirty-day Mortality and Readmission Rates for Medicare Fee-for-Service Beneficiaries Hospitalized with Acute Myocardial Infarction, Heart Failure, and Pneumonia at Veterans Affairs and non-Veterans Hospitals, 2010–2013.
| Observed | Risk-Standardized | Mean-aggregate within-MSA percentage difference between VA and non-VA hospitals (95% CI) | P-value | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| VA hospitals | Non-VA hospitals | P-value | VA hospitals | Non-VA hospitals | P-value | |||
|
| ||||||||
| Acute myocardial infarction | ||||||||
| Mean 30-day mortality rate, % (95% CI) | 11.62 (10.72, 12.52) | 13.88 (13.63, 14.13) | <0.001 | 13.52 (13.38, 13.66) | 13.69 (13.64, 13.74) | 0.02 | −0.22 (−0.40, −0.04) | 0.02 |
| Mean 30-day readmission rate, % (95% CI) | 19.05 (19.10, 21.01) | 17.16 (16.89, 17.43) | <0.001 | 17.84 (17.71, 17.96) | 17.21 (17.17, 17.25) | <0.001 | 0.62 (0.48, 0.75) | <0.001 |
| Heart failure | ||||||||
| Mean 30-day mortality rate, % (95% CI) | 8.92 (8.33, 9.52) | 12.19 (12.01, 12.36) | <0.001 | 11.43 (11.11, 11.75) | 11.87 (11.80, 11.93) | 0.008 | −0.63 (−0.95, −0.31) | <0.001 |
| Mean 30-day readmission rate, % (95% CI) | 24.34 (22.58, 25.11) | 23.51 (23.29, 23.72) | 0.03 | 24.66 (24.31, 25.02) | 23.46 (23.39, 23.53) | <0.001 | 0.97 (0.59, 1.34) | <0.001 |
| Pneumonia | ||||||||
| Mean 30-day mortality rate, % (95% CI) | 11.07 (10.41, 11.72) | 12.33 (12.15, 12.52) | <0.001 | 12.63 (12.19, 13.07) | 12.17 (12.08, 12.26) | 0.05* | −0.03 (−0.46, 0.40) | 0.90 |
| Mean 30-day readmission rate, % (95% CI) | 19.36 (18.61, 20.11) | 18.61 (18.40, 18.82) | 0.04 | 19.44 (19.19, 19.69) | 18.68 (18.63, 18.73) | <0.001 | 0.66 (0.41, 0.91) | <0.001 |
VA = Veterans Affairs; CI = confidence interval
exact p-value = 0.0449
Crude numbers of mortality and readmissions: AMI mortality VA: 931, non-VA: 17,341; AMI readmission VA: 1,590, non-VA: 22,846; HF mortality VA: 2,042, non-VA: 26,428; HF readmission VA: 6,385, non-VA: 63,841; pneumonia mortality VA: 2,334, non-VA: 23,671; pneumonia readmission VA: 4,110, non-VA: 38,440
Figure 1.
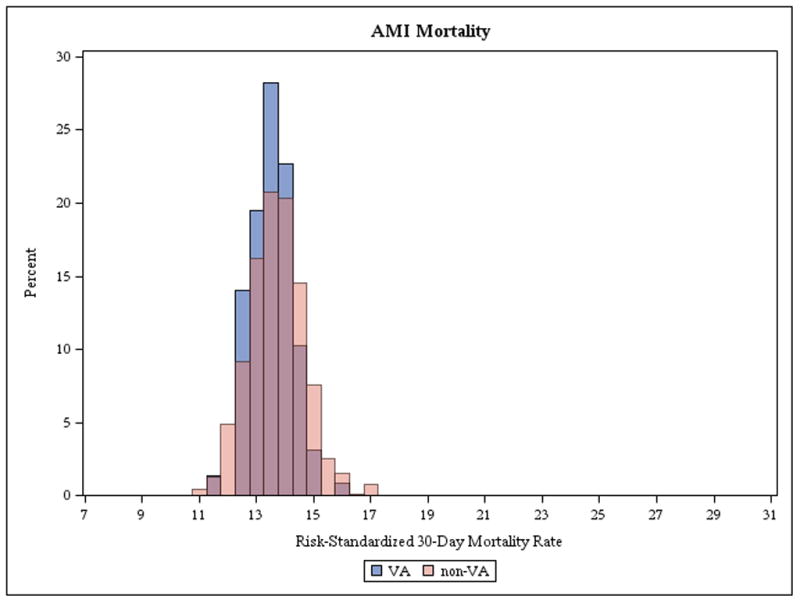
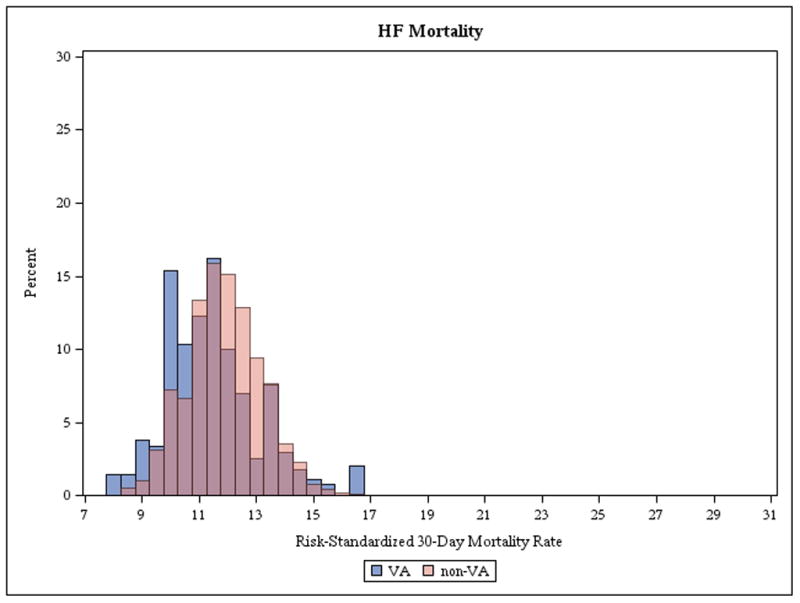
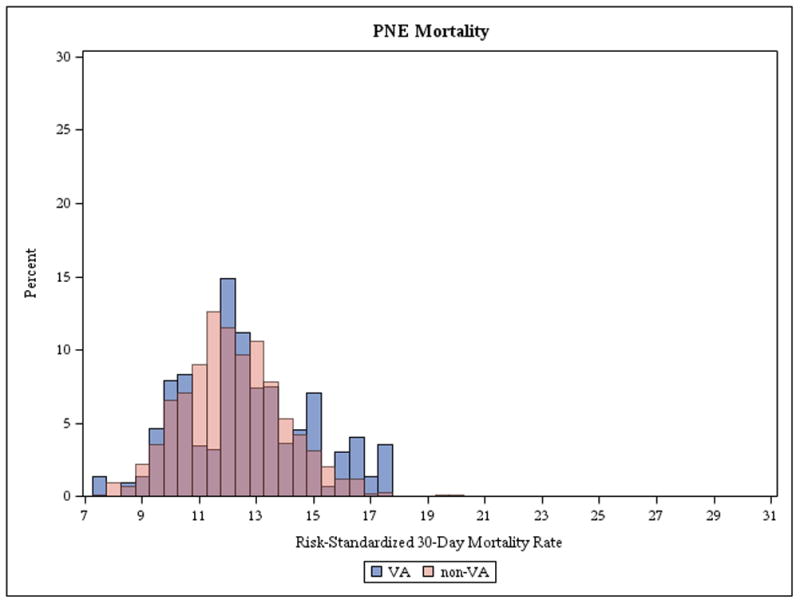
Histogram Comparing Risk-Standardized Mortality Rates for Acute Myocardial Infarction, Heart Failure, and Pneumonia between Veterans Affairs and non-Veterans Affairs Hospitals, 2010–2013.
AMI: acute myocardial infarction, HF: heart failure, PNE: pneumonia. Blue bars and dashed lines indicate VA hospitals, and red bars and dashed lines indicate non-VA hospitals. Bars with purple coloring indicate the overlap of VA and non-VA hospitals.
In within-MSA comparisons, compared with non-VA hospitals, VA hospitals had lower mean-aggregated within-MSA mortality rates for AMI (−0.22 percentage points, 95% CI: −0.40 to −0.04; p<0.02) and HF (−0.63 percentage points, 95% CI: −0.95 to −0.31; p<0.001). However, in contrast with the overall comparison, VA hospitals had mean-aggregated within-MSA mortality rates that were not significantly different for pneumonia (−0.03 percentage points, 95% CI: −0.46 to 0.40; p=0.90).
30-day Readmission Rates
Before risk-adjustment, VA hospitals had higher readmission rates than non-VA hospitals across all 3 conditions (Table 3). After risk-adjustment, VA hospitals had higher readmission rates than non-VA hospitals for all 3 conditions (Table 3; Figure 2). For AMI, the readmission rates were 17.8% (95% CI: 17.7 to 18.0) for VA hospitals versus 17.2% (95% CI: 17.2 to 17.3) for non-VA hospitals (0.6 percentage point difference); for HF, 24.7% (95% CI: 24.3 to 25.0) versus 23.5% (95% CI: 23.4 to 23.5) (1.2 percentage point difference); and for pneumonia, 19.4% (95% CI: 19.2 to 19.7) versus 18.7% (95% CI: 18.6 to 18.7) (0.7 percentage point difference) (p<0.001 for all). The distribution of readmission rate performance differed between VA and non-VA hospitals (Figure 2 and eFigure; eTables 5 and 6): For all 3 conditions, VA hospitals had a greater proportion of hospitals with higher readmission rates compared with non-VA hospitals.
Figure 2.
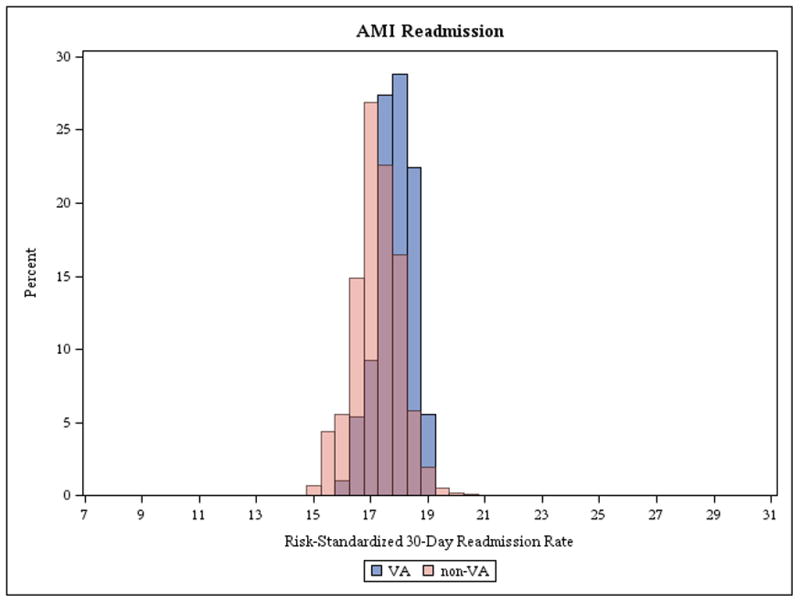
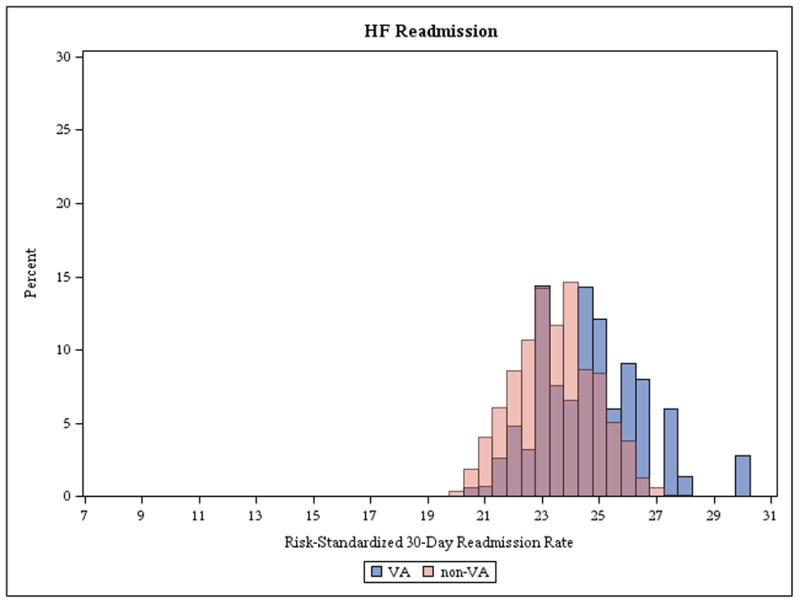
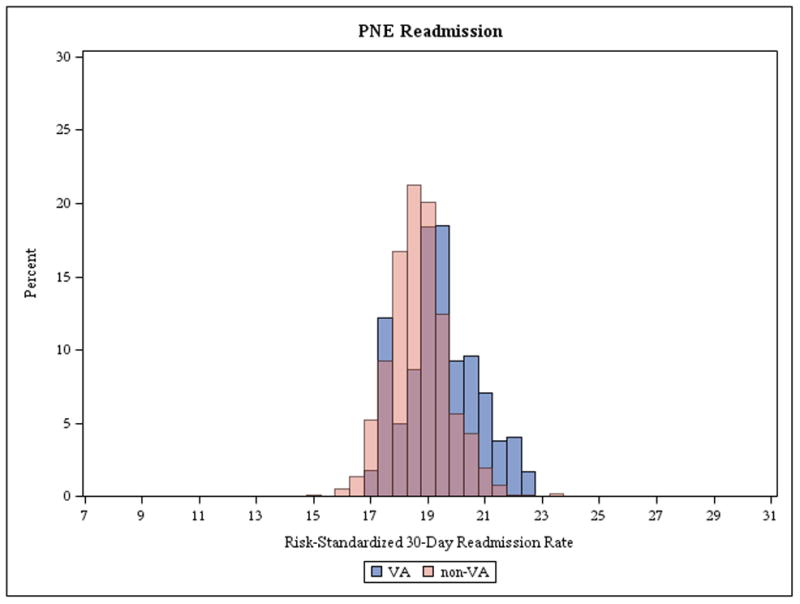
Histogram Comparing Risk-Standardized Readmission Rates for Acute Myocardial Infarction, Heart Failure, and Pneumonia between Veterans Affairs and non-Veterans Affairs Hospitals, 2010–2013.
AMI: acute myocardial infarction, HF: heart failure, PNE: pneumonia. Blue bars and dashed lines indicate VA hospitals, and red bars and dashed lines indicate non-VA hospitals. Bars with purple coloring indicate the overlap of VA and non-VA hospitals.
In within-MSA comparisons, VA hospitals had higher mean-aggregated within-MSA readmission rates than non-VA hospitals for all 3 conditions: 0.62 percentage points (95% CI: 0.48 to 0.75) for AMI, 0.97 percentage points (95% CI: 0.59 to 1.34) for HF, and 0.66 percentage points (95% CI: 0.41 to 0.91) for pneumonia (p<0.001 for all; Table 3).
Across conditions, among those who were initially hospitalized in VA hospitals, approximately 12% were readmitted to non-VA hospitals; among those initially hospitalized in non-VA hospitals, <1% were readmitted to VA hospitals (Table 1).
DISCUSSION
In this national study comparing 30-day mortality and readmission measures publicly reported by CMS for 3 major conditions, we found that VA hospitals have lower mortality rates for AMI and HF compared with non-VA hospitals. However, VA hospitals had higher readmission rates for AMI, HF, and pneumonia than non-VA hospitals. These differences persisted after accounting for geographic variation in hospital location by limiting comparisons of VA and non-VA hospitals to those within the same MSA. In general, however, the magnitudes of differences were small for both measures across all 3 conditions.
We were unable to find another national study using CMS hospital mortality and readmission measures to compare the quality of care between VA hospitals, which comprise the largest integrated healthcare system in the U.S., and non-VA hospitals. This study is also distinct because it compares outcomes between VA and non-VA hospitals within similar geographic areas. The finding that risk-standardized mortality rates for cardiovascular conditions were lower, albeit with small absolute differences, in VA hospitals may reflect higher quality of care in VA hospitals as represented by adherence to process measures.3,22–25 The lower mortality rates may be due to the quality improvement efforts that can be implemented across the VA’s integrated delivery system. For example, upon evidence of possible higher cardiovascular mortality in VA hospitals compared with non-VA hospitals, in 2003 the VA undertook a comprehensive cardiac care improvement initiative across all its hospitals, after which AMI mortality declined.4 Similar initiatives and programs, such as the VA Heart Failure Provider Network,26 may have helped lower mortality rates. However, the lower mortality result for VA hospitals was not consistent for pneumonia, with no difference in mortality rates between VA and non-VA hospitals after accounting for geographic location, and the differences in cardiovascular condition mortality outcomes were modest.
There are several possible reasons for the finding of higher readmission rates in VA hospitals. First, VA hospitals may have a higher propensity to admit. For example, a study that sought to reduce readmissions in VA hospitals by increased access to primary care resulted in an increase in readmissions in the intervention arm.27 Second, the distance VA patients need to travel to the hospital may be greater than that for non-VA patients, which has been associated with higher readmission rates among veterans;28 however, greater distance could also produce lower readmission rates, as patients may be less likely to go to the hospital when they need care. Third, the CMS Hospital Readmission Reduction Program introduced financial penalties for non-VA hospitals in 2012, and national public reporting of, and incentives for reducing, readmissions in non-VA hospitals may have contributed to lower readmission rates for non-VA hospitals during our study period. Nevertheless, the VA has undertaken efforts to prevent readmissions in recent years,29,30 and we are unable to assert whether or how the combination of efforts in VA hospitals and public reporting for non-VA hospitals contributed to relatively lower readmission rates among non-VA hospitals. The results of this study may be helpful to the VA system by highlighting the variation in performance across VA and non-VA hospitals even after case mix adjustment, so that resources could be targeted to reduce unnecessary readmissions. Of note, the range in performance among the hospitals in both groups was as little as approximately 3.5 percentage points, although in some cases it was as much as approximately 13 percentage points. Some readers may consider the difference modest and an indication of little opportunity for improvement. However, it may also be that, for some conditions, hospitals are aggregating around a similar performance but have opportunities for marked improvement, as has been demonstrated with mortality over the last 15 years and more recently by readmission.31,32 In any case, this study sought to compare 2 health systems, and whether they have greater opportunities to improve does not negate the fact that their current performance is separated by only a few percentage points.
While VA outcome data for these 3 key conditions are currently available on Hospital Compare, this initial integration of measures is going to be followed by an expectation that a broader set of quality measures be reported across both VA and non-VA hospitals as part of the Veterans Access, Choice, and Accountability Act of 2014.33 Within this context, our study has multiple implications. First, the availability of this information, with equal standards of reporting, will allow for the assessment of comparative quality, which can inform targeted improvements in VA and non-VA hospitals alike. It also affords a unique opportunity for the VA to partner with public and private entities to test and implement strategies to improve care. The current study serves as an example of national performance comparison for VA and non-VA hospital care, which sets the stage for future performance and quality improvement studies. Moreover, the results of our study and other benchmarking efforts could inform efforts to improve quality in the VA, particularly our findings of variation in performance, by identifying and learning from high performing hospitals and disseminating best practices to lower performing hospitals to elevate the entire performance curve. Finally, given the new Veteran’s Choice Program for the funding of private care for some veterans, VA policymakers should recognize that there is also variation in quality among non-VA hospitals and take steps to encourage veterans who choose to use non-VA hospitals to use the highest quality ones to ensure optimal outcomes and high value care.
Our study has several limitations. First, we only studied elderly, male VA patients and Medicare patients, and are unable to assert whether our findings are generalizable to younger or female populations. Second, we studied administrative claims data, which lack information about clinical disease severity, but these are the same data used for the publicly reported outcomes measures and, at the hospital level, studies have shown that administrative data and clinical data perform similarly for both VA and non-VA hospitalizations.7–9,34 Third, while prior literature suggests that VA and non-VA populations are different, with VA populations generally having worse health status but similar mortality rates,35–37 these reports did not study older populations. Other studies suggest that VA beneficiaries ≥65 years of age, who comprise our cohort, have similar or better physical health status and better mental health status than younger VA beneficiaries,38–40 which is in contrast with non-VA populations where older populations are less healthy. Fourth, we could not study all VA hospitals in the U.S. because some were in rural areas or were not within an urban MSA with another non-VA hospital; nevertheless, studying hospitals within the same urban MSA allowed us to make more direct comparisons between VA and non-VA hospitals by accounting for geographic differences. Fourth, there were hospitals for which hospital characteristics were not available; however, these hospitals represented only approximately 4% of VA or non-VA hospitals in our cohort, so it is unlikely that this would influence the results. Finally, we only studied 3 common conditions among elderly patients, which may not be representative of care for all patients in either VA or non-VA hospitals; however, these outcome metrics are CMS core condition measures.
CONCLUSIONS
Among older men with AMI, HF, and pneumonia, hospitalization at VA hospitals, compared with hospitalization at non-VA hospitals, was associated with lower risk-standardized 30-day all-cause mortality rates for AMI and HF, and higher risk-standardized 30-day all-cause readmission rates for all 3 conditions, both nationally and within similar geographic areas, although absolute differences between these outcomes at VA and non-VA hospitals were small.
Supplementary Material
Acknowledgments
Disclosures: Drs. Ross and Krumholz are the recipients of research agreements from Medtronic and from Johnson & Johnson (Janssen), through Yale University, to develop methods of clinical trial data sharing. Dr. Krumholz chairs a cardiac scientific advisory board for UnitedHealth. Drs. Krumholz, Ross, Normand, Bernheim, and Suter work under contract to the Centers for Medicare & Medicaid Services to develop and maintain performance measures. The other authors do not have disclosures to report.
Funding/Support: Dr. Ross is supported by grant K08 AG032886 from the National Institute on Aging and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. Dr. Krumholz is supported by grant U01 HL105270-05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. Dr. Suter is partially supported by the VA Connecticut Healthcare System.
Role of the Funder/Sponsor: No funder had a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication
Data Access, Responsibility, and Analysis: Dr. Li had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Selim AJ, Kazis LE, Rogers W, et al. Risk-adjusted mortality as an indicator of outcomes: comparison of the Medicare Advantage Program with the Veterans’ Health Administration. Med Care. 2006;44(4):359–365. doi: 10.1097/01.mlr.0000204119.27597.f1. [DOI] [PubMed] [Google Scholar]
- 2.Landrum MB, Guadagnoli E, Zummo R, Chin D, McNeil BJ. Care following acute myocardial infarction in the Veterans Administration Medical Centers: a comparison with Medicare. Health Serv Res. 2004;39(6 Pt 1):1773–1792. doi: 10.1111/j.1475-6773.2004.00317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trivedi AN, Matula S, Miake-Lye I, Glassman PA, Shekelle P, Asch S. Systematic review: comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Med Care. 2011;49(1):76–88. doi: 10.1097/MLR.0b013e3181f53575. [DOI] [PubMed] [Google Scholar]
- 4.Fihn SD, Vaughan-Sarrazin M, Lowy E, et al. Declining mortality following acute myocardial infarction in the Department of Veterans Affairs Health Care System. BMC Cardiovasc Disord. 2009;9:44. doi: 10.1186/1471-2261-9-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weeks WB, West AN, Wallace AE, Fisher ES. Comparing the characteristics, utilization, efficiency, and outcomes of VA and non-VA inpatient care provided to VA enrollees: a case study in New York. Med Care. 2008;46(8):863–871. doi: 10.1097/MLR.0b013e31817d92e1. [DOI] [PubMed] [Google Scholar]
- 6.National Center for Veterans Analysis and Statistics. [Accessed January 4, 2016];Utilization. 2014 http://www.va.gov/vetdata/utilization.asp.
- 7.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1(1):29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 8.Krumholz HM, Lin Z, Drye EE, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4(2):243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindenauer PK, Normand SL, Drye EE, et al. Development, validation, and results of a measure of 30-day readmission following hospitalization for pneumonia. J Hosp Med. 2011;6(3):142–150. doi: 10.1002/jhm.890. [DOI] [PubMed] [Google Scholar]
- 10.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113(13):1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 11.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113(13):1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 12.Bratzler DW, Normand SL, Wang Y, et al. An administrative claims model for profiling hospital 30-day mortality rates for pneumonia patients. PLoS One. 2011;6(4):e17401. doi: 10.1371/journal.pone.0017401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ross JS, Bernheim SM, Lin Z, et al. Based on key measures, care quality for Medicare enrollees at safety-net and non-safety-net hospitals was almost equal. Health Aff (Millwood) 2012;31(8):1739–1748. doi: 10.1377/hlthaff.2011.1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Department Of Labor, Office Of Workers’ Compensation Programs. [Accessed January 4, 2016];Geographic Practice Cost Index Values By Zip Code. 2011 http://www.dol.gov/owcp/regs/feeschedule/fee/fee11/fs11_gpci_by_msa-ZIP.xls.
- 15.Weeks WB, Yano EM, Rubenstein LV. Primary care practice management in rural and urban Veterans Health Administration settings. J Rural Health. 2002;18(2):298–303. doi: 10.1111/j.1748-0361.2002.tb00890.x. [DOI] [PubMed] [Google Scholar]
- 16.Quality through collaboration: The future of rural health care. Washington, DC: The National Academies Press; 2005. [Google Scholar]
- 17.Borrero S, Kwoh CK, Sartorius J, Ibrahim SA. Brief report: Gender and total knee/hip arthroplasty utilization rate in the VA system. J Gen Intern Med. 2006;21(S3):S54–S57. doi: 10.1111/j.1525-1497.2006.00375.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. [Accessed January 4, 2016];Measure methodology reports: Readmission measures. http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic/Page/QnetTier4&cid=1219069855841.
- 19. [Accessed January 4, 2016];AHA data and directories. 2014 http://www.aha.org/research/rc/stat-studies/data-and-directories.shtml.
- 20. [Accessed January 4, 2016];Popluation estimates: Metropolitan and micropolitan statistical areas. 2015 https://www.census.gov/popest/data/metro/totals/2012/
- 21.Services. CFMM. [Accessed January 4, 2016];Denominator file. https://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/IdentifiableDataFiles/DenominatorFile.html.
- 22.Asch SM, McGlynn EA, Hogan MM, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Intern Med. 2004;141(12):938–945. doi: 10.7326/0003-4819-141-12-200412210-00010. [DOI] [PubMed] [Google Scholar]
- 23.Trivedi AN, Grebla RC. Quality and equity of care in the Veterans Affairs health-care system and in Medicare Advantage health plans. Med Care. 2011;49(6):560–568. doi: 10.1097/MLR.0b013e31820fb0f6. [DOI] [PubMed] [Google Scholar]
- 24.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs health care system on the quality of care. N Engl J Med. 2003;348(22):2218–2227. doi: 10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- 25.Werner RM, Bradlow ET. Relationship between Medicare’s hospital compare performance measures and mortality rates. JAMA. 2006;296(22):2694–2702. doi: 10.1001/jama.296.22.2694. [DOI] [PubMed] [Google Scholar]
- 26.Heart Failure Provider Network. [Accessed January 4, 2016]; http://www.queri.research.va.gov/chf/networks/
- 27.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? N Engl J Med. 1996;334(22):1441–1447. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 28.Holloway JJ, Medendorp SV, Bromberg J. Risk-factors for early readmission among Veterans. Health Serv Res. 1990;25(1):213–237. [PMC free article] [PubMed] [Google Scholar]
- 29. [Accessed January 4, 2016];VA Hospital To Home (H2H) Initiative. http://www.queri.research.va.gov/chf/products/h2h/default.cfm.
- 30. [Accessed January 4, 2016];Chronic heart failure goals and activities. http://www.queri.research.va.gov/chf/goals.cfm.
- 31.Gerhardt G, Yemane A, Hickman P, Oelschlaeger A, Rollins E, Brennan N. Data shows reduction in Medicare hospital readmission rates during 2012. Medicare Medicaid Res Rev. 2013;3(2):E1–E11. doi: 10.5600/mmrr.003.02.b01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, hospitalizations, and expenditures for the Medicare population aged 65 years or older, 1999–2013. JAMA. 2015;314(4):355–365. doi: 10.1001/jama.2015.8035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.H.R. 3230 — 113th Congress: Veterans Access, Choice, and Accountability Act of 2014; [Accessed January 4, 2016]. https://www.govtrack.us/congress/bills/113/hr3230. [Google Scholar]
- 34.Ross JS, Maynard C, Krumholz HM, et al. Use of administrative claims models to assess 30-day mortality among Veterans Health Administration hospitals. Med Care. 2010;48(7):652–658. doi: 10.1097/MLR.0b013e3181dbe35d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones LG, Sin MK, Hage FG, et al. Characteristics and outcomes of patients with advanced chronic systolic heart failure receiving care at the Veterans Affairs versus other hospitals: insights from the Beta-blocker Evaluation of Survival Trial (BEST) Circ Heart Fail. 2015;8(1):17–24. doi: 10.1161/CIRCHEARTFAILURE.114.001300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252–3257. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- 37.Rogers WH, Kazis LE, Miller DR, et al. Comparing the health status of VA and non-VA ambulatory patients: the veterans’ health and medical outcomes studies. J Ambul Care Manage. 2004;27(3):249–262. doi: 10.1097/00004479-200407000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Kazis LE, Ren XS, Lee A, et al. Health status in VA patients: results from the Veterans Health Study. Am J Med Qual. 1999;14(1):28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- 39.Payne SM, Lee A, Clark JA, et al. Utilization of medical services by Veterans Health Study (VHS) respondents. J Ambul Care Manage. 2005;28(2):125–140. doi: 10.1097/00004479-200504000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Keyhani S, Cheng E, Arling G, et al. Does the inclusion of stroke severity in a 30-day mortality model change standardized mortality rates at Veterans Affairs hospitals? Circ Cardiovasc Qual Outcomes. 2012;5(4):508–513. doi: 10.1161/CIRCOUTCOMES.111.962936. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


