Abstract
Objective
To examine how psychological stress changes over time in young and middle-aged patients after experiencing an acute myocardial infarction (AMI) and whether these changes over time differ between men and women.
Methods
We analyzed data obtained from 2,358 women and 1,151 men aged 18–55 years hospitalized for an AMI. Psychological stress was measured using the 14-item Perceived Stress Scale (PSS-14) at initial hospitalization and at 1 and 12 months after AMI. We used linear mixed effects models to examine changes in PSS-14 scores over time and sex differences in these changes, while adjusting for patient characteristics and accounting for correlation among repeated observations within patients.
Results
Overall, patients’ perceived stress decreased over time, especially during the first month after AMI. Women had higher levels of perceived stress than men throughout the 12-month period (difference in PSS-14 score = 3.63, 95% confidence interval [CI] = 3.08 to 4.18, p<.001), but they did not differ in how stress changed over time. Adjustment for patient characteristics did not alter the overall pattern of sex difference in changes of perceived stress over time other than attenuating the magnitude of sex difference in PSS-14 score (difference between women and men = 1.74, 95% CI: 1.32 to 2.16, p<.001). The magnitude of sex differences in perceived stress was similar in patients with versus without post-AMI angina, even though patients with angina experienced less improvement in PSS-14 score than those without angina.
Conclusions
In young and middle-aged patients with AMI, women reported higher levels of perceived stress than men throughout the first 12 months of recovery. However, women and men had a similar pattern in how perceived stress changed over time.
Keywords: Myocardial infarction, sex difference, psychological stress, recovery
INTRODUCTION
As a life-threatening and unpredictable condition, acute myocardial infarction (AMI) can exert substantial distress on patients both during and after the event (1–4). Lack of control and feelings of uncertainty and helplessness are commonly reported in patients after an AMI (3, 5). The resulting psychological stress may not only impair patients’ emotional well-being, but also adversely affect cardiovascular health and post-AMI recovery (6–8). Therefore, understanding how perceived stress changes over time as patients recover from the event can help guide clinical care to better meet patients’ needs (e.g., when patients need most help with stress management, and whether acute or longer term stress programs may be more beneficial). However, data on the trajectory of patients’ perceived stress after AMI are lacking.
Having an AMI may be particularly burdensome for younger patients. Younger age has been associated with higher levels of perceived stress in population-based surveys (9, 10). Moreover, because of its unexpectedness at younger ages and disturbance to both work and personal life, an AMI may be perceived more negatively in younger patients than older patients (3). Literature on posttraumatic stress disorder (PTSD) suggests that both the incidence of PTSD and posttraumatic stress symptoms after AMI are higher among younger patients than older patients (3, 11). Nonetheless, PTSD only reflects the experience of patients enduring more severe psychological impact. We know little about how perceived stress in general evolves over time in the younger AMI patient population and research on younger patients with AMI has been sparse.
In addition, women tend to report higher levels of perceived stress than men (10). Prior research has shown that women experience more intense PTSD symptoms following an AMI and have less improvement in symptoms over time, compared with men (3, 12). Even 5 years after an AMI, women report lower psychological well-being and higher psychological distress than men (13). As women and men have different cardiovascular reactions to mental stress (e.g., increased platelet aggregation in women versus more elevated blood pressure in men) (14), it is important to understand sex differences in perceived stress after AMI, which may shed light on potentially different recovery paths of women and men. Yet such data on younger women and men are still lacking, as few studies of sex comparisons have focused on younger patients with AMI and prior research often lacked sufficient sample sizes to closely examine younger women patients. Younger patients may have very different stress profiles than older patients. Thus we do not know whether and how patterns of sex difference in perceived stress among younger patients with AMI may differ from the general population.
Therefore, the purpose of this study was to characterize perceived stress at 1 and 12 months after AMI, relative to baseline, in a large sample of young and middle-aged patients aged 18–55 years, and to examine differences between women and men in how perceived stress changed over time. We also assessed whether patient demographic, health, and psychosocial characteristics explained any differences in perceived stress between women and men. The findings will enhance our understanding of the longitudinal evolvement of psychological stress among young and middle-aged patients after AMI and may inform strategies to better tailor care for younger patients, especially young female patients.
METHODS
Data Source and Study Sample
Data for this study came from the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) project. VIRGO was designed to address an important gap in AMI research by providing data on a large prospective sample of younger patients and in particular, younger women and therefore oversampled women than men with a 2:1 ratio (15, 16). Details about VIRGO study design have been reported previously (16). In brief, all participants were 18 to 55 years of age (2,397 women and 1,175 men) and had at least 1 cardiac biomarker above the 99th percentile of the upper reference limit within 24 hours of admission, along with evidence of acute myocardial ischemia (including at least 1 of the following: symptoms of ischemia, electrocardiogram changes indicative of new ischemia, or other evidence of myocardial necrosis) (16, 17). Patients must have presented directly to the enrolling institution or have been transferred within the first 24 hours of presentation to ensure that primary clinical decision making occurred at the enrolling site. Patients were excluded if their elevated cardiac markers were due to a complication of elective coronary revascularization, or their AMI was caused by physical trauma. Patients were also ineligible if they did not speak either English or Spanish, were unable to provide consent or contact information for follow-up, or were prisoners. All eligible women at participating hospitals were screened. To minimize potential biased selection of male patients (as there were a larger number of men than women eligible for the study), men were screened chronologically (i.e., the next male patient admitted to the hospital was screened after every two females were enrolled). This chronological order helped maintain the random nature of men screened. VIRGO participants were recruited from 103 hospitals in the U.S., 24 in Spain and 3 in Australia during August 2008 – January 2012. The Yale Human Investigation Committee and institutional review boards at each institution approved this study, and all patients gave informed consent.
Study coordinators conducted baseline interviews during the initial hospitalization for AMI (average number of days between admission and baseline interview = 3.2 days). Interview data were supplemented by clinical measures from medical record review, physical measurements, and analysis of blood specimens. Follow-up interviews were conducted at 1 month and 12 months after discharge from the initial hospitalization, and were administered by the Yale Follow-Up Center in the U.S., a dedicated contract research organization in Spain, and site coordinators in Australia. All staff involved in data abstraction and interview administration received specific training to ensure consistency in data collection.
Measures
The outcome measure for this study was patients’ self-perceived psychological stress in life. It was assessed by the 14-item Perceived Stress Scale (PSS-14), reflecting patients’ appraisal about how “unpredictable, uncontrollable, and overloading” their life situation was over the past month (18). Example items include, “In the last month, how often have you been upset because of something that happened unexpectedly” and, “In the last month, how often have you felt that you were unable to control the important things in your life.” Answer options to each item included never, almost never, sometimes, fairly often, and very often, taking values from 0 to 4, respectively. Positive items were reverse-coded. Responses to all 14 items were summed to generate the overall PSS-14 score following the scoring method in Cohen et al. (18). A higher value reflected a greater level of stress (score range: 0–56, Cronbach’s alpha = 0.87). We allowed for missing data on 3 or fewer items and for these patients (4.9% of the sample), we imputed the missing items with the average score of the non-missing items (19–21). The PSS-14 score was available at baseline, 1 month, and 12 months after AMI.
Key explanatory variables included sex (female versus male) and time (1-month post-AMI, 12-months post-AMI, versus baseline). To account for factors that may confound sex differences in perceived stress, we also adjusted for other patient characteristics as covariates, which were selected based on clinical relevance. These covariates included: 1) sociodemographic variables at baseline (age, race, education, marital status, number of children living in household, financial status, employment status), 2) number of comorbid conditions at baseline (measured as a count of the following conditions that the patient had: diabetes mellitus, hypertension, hypercholesterolemia, chronic lung disease, chronic renal dysfunction, history of cancer, prior stroke, and prior heart disease), 3) AMI characteristics at initial admission (ST-segment-elevation myocardial infarction (STEMI) versus non-STEMI, cardiogenic shock upon hospital admission, ejection fraction <40%, Global Registry of Acute Coronary Events (GRACE) risk score >99 (22), hemodynamic instability on arrival (cardiac arrest pre-hospitalization and/or a systolic blood pressure <90 mm Hg), presentation to the hospital more than 6 hours after symptom onset, and length of stay during the initial hospitalization), 4) angina-related health status (including angina frequency and angina-related physical limitation based on the Seattle Angina Questionnaire (SAQ)) (23), 5) psychosocial risk factors (including the INTERHEART stressful life events scale (24), low social support determined by the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Social Support Inventory (ESSI) (25–27), and depression as evaluated by the Patient Health Questionnaire (PHQ-9) (28)), and 6) country of residence (Spain or Australia versus U.S.). Because psychosocial risk factors and angina-related health status could change substantially over time, we measured them as time-varying variables.
Statistical Analysis
Descriptive statistics of patients’ baseline characteristics were calculated for women and men. Sex differences in these characteristics were assessed using chi-square tests for categorical variables and student’s t tests for continuous variables.
Using the PSS-14 score as the dependent variable, we performed multivariable regression analyses to examine sex differences in stress after AMI and in changes of stress between time points. We used linear mixed effects models to account for correlation in repeated measures within the same individual over time. We first estimated a model including only female sex and time indicators as explanatory variables. Coefficient estimates on female sex reflected the difference in perceived stress between women and men (overall across the 3 time points), while coefficient estimates on the time variables revealed how PSS-14 scores at 1-month and 12-months post-AMI, respectively, compared with baseline. We tested potential interaction effects between female sex and time indicators to determine whether women and men differed in how their perceived stress changed over time.
We then estimated a series of models by sequentially adding blocks of patient characteristics variables. Coefficient estimates associated with each patient characteristic revealed their association with the PSS-14 score (overall across the 3 time points). Reduction in estimated sex differences across these models indicates the relative contribution of the additional patient characteristics in explaining observed sex differences in perceived stress. Because there was evidence for country differences in how the PSS-14 score changed over time, we included indicators for country in all models, as well as interaction terms between country and time. Potential collinearity among explanatory variables were examined and ruled out by assessing Spearman correlation coefficients and the variance inflation factors.
To further elucidate how recurrent cardiac events might alter the trajectory of perceived stress post-AMI (29), we performed a sensitivity analysis examining sex difference in PSS-14 scores over time among patients with versus without post-AMI angina separately. Patients with an SAQ angina frequency score less than 100 at either 1-month or 12-month interviews were regarded as having angina post-AMI, while those with a score of 100 at both interviews were considered as not having angina post-AMI.
For any given explanatory variable, less than 5% of the sample had missing data. We imputed their values using multiple imputation. As 3 interview time points and 3 countries were involved in the analysis, we used step-down Bonferroni adjusted p values to account for multiple comparisons when conducting pairwise comparison of perceived stress between time points or countries. A sensitivity analysis on patients who completed all 3 interviews (baseline, 1-month post-AMI, and 12-month post-AMI) with adequate PSS-14 data found no meaningful difference in the main results. P values less than 0.05 were considered statistically significant.
Our primary analysis was conducted using PSS-14 to best utilize information on all 14 items collected. However, to facilitate comparison of our estimated sex difference in perceived stress with published population norm data on psychological stress, which was based on a shorter version of the PSS using 10 of the 14 items (10), we also reported descriptive estimates of PSS-10 scores (score range: 0–40, Cronbach’s alpha = 0.88). All analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
Sample Characteristics
Of the 3,572 participants in VIRGO, a small proportion (1.8%) had insufficient data on the PSS-14 scale at baseline (i.e., more than 3 missing items) and were excluded from analysis. This resulted in a final analytic sample of 3,509 patients (2,358 women and 1,151 men).
Baseline characteristics of these 3,509 patients are presented in Table 1. The mean age was 47.0 for women (standard deviation (SD) = 6.3) and 46.9 for men (SD = 5.9) (p = 0.53). Approximately 30% of the patients were younger than 45 years of age. Compared with their male counterparts, women tended to have more risk factors for stress at baseline. On average, women had 2.5 ± 1.4 comorbid conditions, as opposed to 2.3 ± 1.2 in men (p<.001). Women also reported more categories of stressful life events over the past year than men (1.7 ± 1.4 versus 1.4 ± 1.3, p<.001) and were more likely to have depression (38.7% versus 21.9%, p<.001). In terms of financial status, more than a third of women (36.1%) reported that they did not have enough to make ends meet at the end of the month, compared with 24.4% of the men (p<.001). However, a higher proportion of men worked extended hours (13.9% versus 3.8%), while a larger percentage of women were not working for pay (43.6% versus 27.1%) (p<.001).
Table 1.
Baseline sample characteristics.
| Sample Characteristics | Men (N=1,151) | Women (N=2,358) | P value |
|---|---|---|---|
| Age | .056 | ||
| 18–34 | 41 (3.6%) | 119 (5.0%) | |
| 35–44 | 308 (26.8%) | 572 (24.3%) | |
| 45–55 | 802 (69.7%) | 1667 (70.7%) | |
| Race | <.001 | ||
| White | 964 (83.9%) | 1802 (76.6%) | |
| Black | 108 (9.4%) | 422 (17.9%) | |
| Other | 77 (6.7%) | 130 (5.5%) | |
| Education | .075 | ||
| Less than high school | 46 (4.1%) | 137 (5.9%) | |
| High school | 479 (42.6%) | 951 (41.0%) | |
| More than high school | 600 (53.3%) | 1233 (53.1%) | |
| Marital status | <.001 | ||
| Married/living with a partner as if married | 738 (64.5%) | 1300 (55.3%) | |
| Not married | 406 (35.5%) | 1052 (44.7%) | |
| Number of children living in household | .019 | ||
| 0 | 553 (48.4%) | 1031 (43.9%) | |
| 1–2 | 472 (41.3%) | 1088 (46.3%) | |
| ≥ 3 | 118 (10.3%) | 230 (9.8%) | |
| Finances at the end of the month | <.001 | ||
| Some money left over | 435 (38.2%) | 618 (26.4%) | |
| Just enough to make ends meet | 427 (37.5%) | 877 (37.5%) | |
| Not enough to make ends meet | 278 (24.4%) | 843 (36.1%) | |
| Employment status | <.001 | ||
| Not working for pay | 300 (27.1%) | 1016 (43.6%) | |
| Working part time (<35 hours) | 102 (9.2%) | 362 (15.5%) | |
| Working full time (35–55 hours) | 553 (49.9%) | 861 (37.0%) | |
| Working full time with extended hours (>55 hours) | 154 (13.9%) | 89 (3.8%) | |
| Number of comorbid conditions, mean ± SD | 2.3 ± 1.2 | 2.5 ± 1.4 | <.001 |
| SAQ angina frequency, mean ± SD | 86.6 ± 17.9 | 82.8 ± 21.4 | <.001 |
| SAQ angina-related physical limitation, mean ± SD | 87.1 ± 20.6 | 78.6 ± 26.9 | <.001 |
| INTERHEART stressful life events scale, mean ± SD | 1.4 ± 1.3 | 1.7 ± 1.4 | <.001 |
| Low social support (based on ESSI) | 239 (21.0%) | 497 (21.4%) | 0.79 |
| Depression (based on PHQ) | 245 (21.9%) | 880 (38.7%) | <.001 |
| AMI severity | |||
| STEMI | 687 (59.7%) | 1138 (48.3%) | <.001 |
| Cardiogenic shock upon hospital admission | 5 (0.5%) | 16 (0.7%) | .38 |
| Ejection fraction <40% | 124 (11.1%) | 239 (10.5%) | .60 |
| GRACE risk score >99 | 88 (7.8%) | 200 (8.7%) | .35 |
| Hemodynamic instability | 92 (8.0%) | 209 (8.9%) | .39 |
| Present >6 hours after symptom onset | 418 (36.4%) | 1047 (44.5%) | <.001 |
| Length of hospital stay, in days, mean ± SD | 4.3 ± 3.4 | 4.8 ± 4.9 | <.001 |
| Country | .84 | ||
| United States | 956 (83.1%) | 1972 (83.6%) | |
| Spain | 173 (15.0%) | 338 (14.3%) | |
| Australia | 22 (1.9%) | 48 (2.0%) | |
| PSS-14 score | 23.4 ± 9.1 | 26.9 ± 9.9 | <.001 |
| PSS-10 score | 16.4 ± 7.6 | 19.7 ± 8.2 | <.001 |
Differences in characteristics between women and men were assessed using chi-square tests for categorical variables and student’s t tests for continuous variables.
AMI = acute myocardial infarction; ESSI = Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Social Support Inventory; GRACE = Global Registry of Acute Coronary Events; PHQ-9 = Patient Health Questionnaire; PSS-14 = 14 item Perceived Stress Scale; SAQ = Seattle Angina Questionnaire; SD = standard deviation; STEMI = ST-segment-elevation myocardial infarction
Women were less likely than men to have STEMI (48.3% versus 59.7%, p<.001) but more likely to present later than 6 hours after symptom onset (44.5% versus 36.4%, p<.001). At baseline hospitalization, women reported worse angina frequency and angina-related physical function compared with men (SAQ score = 82.8 ± 21.4 versus 86.6 ± 17.9, p<.001; and 78.6 ± 26.9 versus 87.1 ± 20.6, p<.001; respectively), and they stayed in the hospital longer than men (4.8 ± 4.9 days versus 4.3 ± 3.4 days, p<.001).
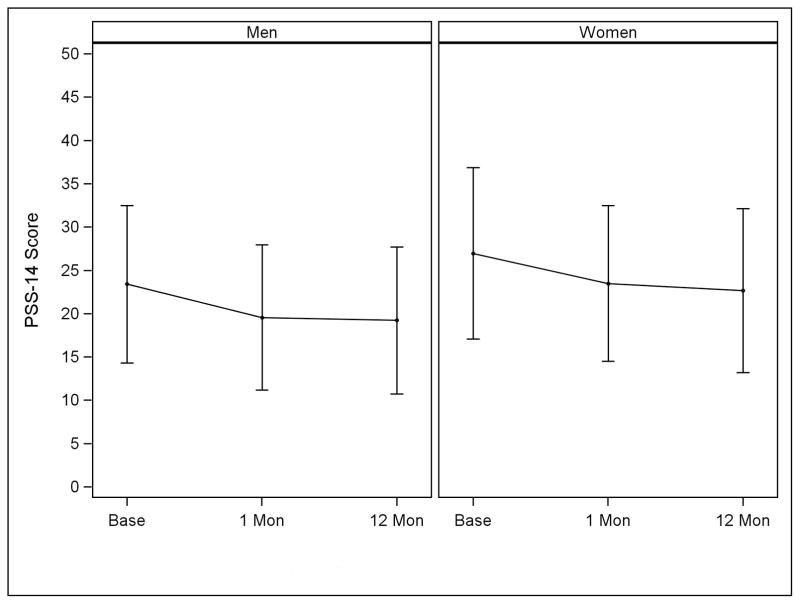
Sex Differences in Perceived Stress before Adjustment for Patient Characteristics
Women had higher levels of stress than men throughout the first 12 months after the AMI. Their observed PSS-14 score decreased from 26.9 ± 9.9 at baseline to 22.7 ± 9.5 at 12-months post-AMI, while the score declined from 23.4 ± 9.1 to 19.2 ± 8.5 for men over the same time period (Figure 1). After accounting for repeated observations over time and country effect, women were found to have a PSS-14 score 3.63 points higher than that of men (95% confidence interval [CI]: 3.08 to 4.18, p<.001; Model 1 in Table 2).
Figure 1.
Observed perceived stress scale (PSS)-14 score over time, by sex.
PSS-14 score range: 0–56 (higher score indicates greater stress). The top and bottom error bars reflect one standard deviation above and below the corresponding mean PSS-14 score, respectively.
Table 2.
Sex differences in perceived stress scale (PSS)-14 score over time after acute myocardial infarction.
| Explanatory variable | Model 1 (without adjustment for patient characteristics) | Model 2 (with adjustment for baseline sociodemographic and health characteristics) | Model 3 (with further adjustment for AMI severity) | Model 4 (with further adjustment for angina health and psychosocial risk factors) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Coefficient | P value | Coefficient | P value | Coefficient | P value | Coefficient | P value | |
| Female (vs. male) | 3.63 | <.001 | 2.76 | <.001 | 2.72 | <.001 | 1.74 | <.001 |
| Time | ||||||||
| 1 month (vs. baseline) | −3.99 | <.001a | −3.96 | <.001a | −3.96 | <.001a | −2.00 | <.001a |
| 12 months (vs. baseline) | −4.72b | <.001a | −4.64c | <.001a | −4.64d | <.001a | −2.36e | <.001a |
| Country | ||||||||
| Spain (vs. U.S.) | −0.97 | 0.29a | −0.77 | 0.73a | −1.06 | 0.25a | −0.44 | >.99a |
| Australia (vs. U.S.) | −1.77 | 0.77a | −0.43 | >.99a | −0.52 | >.99a | 0.53 | >.99a |
| Interaction terms | ||||||||
| Spain x 1 month | 3.01 | <.001 | 3.01 | <.001 | 3.01 | <.001 | 2.79 | <.001 |
| Spain x 12 months | 4.44 | <.001 | 4.42 | <.001 | 4.42 | <.001 | 3.07 | <.001 |
| Australia x 1 month | 0.78 | 0.50 | 0.66 | 0.56 | 0.67 | 0.55 | −0.21 | 0.84 |
| Australia x 12 months | 0.88 | 0.51 | 0.64 | 0.63 | 0.65 | 0.63 | −0.82 | 0.50 |
Coefficient estimates and p values were based on results from multivariable linear mixed effects models to account for correlation in repeated measures within the same individual over time. AMI = acute myocardial infarction.
Model 1 adjusted for patient sex, time, and country.
Model 2 further adjusted for patient’s baseline age, race, education, marital status, number of children living in household, financial status, employment status, and number of comorbid conditions at baseline, in addition to all variables in Model 1.
Model 3 further adjusted for AMI characteristics at initial admission, including ST-segment-elevation myocardial infarction (STEMI) versus non-STEMI, cardiogenic shock upon hospital admission, ejection fraction <40%, Global Registry of Acute Coronary Events (GRACE) risk score >99, hemodynamic instability on arrival, presentation to the hospital >6 hours after symptom onset, and length of stay during the initial hospitalization, in addition to all variables in Model 2.
Model 4 further adjusted for time-varying measures of Seattle Angina Questionnaire (SAQ) angina frequency and angina-related physical limitation scores, the INTERHEART stressful life events scale, low social support determined by the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Social Support Inventory (ESSI), and depression based on the Patient Health Questionnaire (PHQ-9), in addition to all variables in Model 3.
P value adjusted with step-down Bonferroni.
Implied a difference of −0.74 between 1-month and 12-month follow-up (p<.001).
Implied a difference of −0.68 between 1-month and 12-month follow-up (p<.001).
Implied a difference of −0.68 between 1-month and 12-month follow-up (p<.001).
Implied a difference of −0.37 between 1-month and 12-month follow-up (p=0.26).
Change in perceived stress over time did not differ by sex (p value for interaction effect between sex and time indicators = 0.50). Most of the reduction in perceived stress occurred during the first month after the AMI. For patients in the U.S., PSS-14 score decreased by 3.99 points between baseline and 1-month follow-up (95% CI: −4.32 to −3.65, p<.001) and by 0.74 points between 1- and 12-month follow-up (95% CI: −1.07 to −0.41, p<.001) (Model 1 in Table 2). A similar pattern was observed for Australia, while patients in Spain experienced less reduction in perceived stress, as indicated by the significant and positive interaction terms between Spain and time indicators (Model 1 in Table 2) (see Figure S1, Supplemental Digital Content 1, which depicts change in PSS-14 score over time by country).
Sex Differences in Perceived Stress after Adjustment for Patient Characteristics
Table 2 also reports sex differences in perceived stress after sequentially adjusting for different patient characteristics (Models 2–4). In general, adjustment for patient demographic, health, and psychosocial characteristics did not alter the overall pattern of sex differences in how perceived stress changed over time other than attenuating the difference in PSS-14 score between women and men (adjusted difference = 1.74, 95% CI: 1.32 to 2.16, p<.001, Model 4 in Table 2; also see Table S1, Supplemental Digital Content 1, which reports complete results from regression Model 4). A test of interaction effect between female sex and time indicators in Model 4 showed that women and men did not differ in changes of PSS-14 score over time even after adjusting for patient characteristics (p value for the interaction effect = 0.12).
Estimated sex differences in perceived stress attenuated the most after adjustment for patient baseline sociodemographic characteristics (Model 2 in Table 2) and time-varying measures of angina-related health status and psychosocial risk factors (Model 4 in Table 2). Patients’ AMI characteristics at the initial hospitalization had minimal impact on sex differences in perceived stress (Model 3 in Table 2).
Sex Differences in Perceived Stress Stratified by Angina Status Post-AMI
Table 3 summarized key results on sex differences in perceived stress before versus after fully adjusting for patient characteristics, stratified by angina status post-AMI. In patients who experienced angina during the follow-up period, difference in PSS-14 score between women and men was 3.31 (95% CI: 2.47 to 4.16, p<.001) in unadjusted analysis, which was attenuated to 1.72 (95% CI: 1.08 to 2.36, p<.001) after adjustment for patient characteristics. A similar sex difference in PSS-14 scores was observed among patients who did not report angina post-AMI (unadjusted difference = 3.20, 95% CI: 2.51 to 3.90, p<.001; adjusted difference = 1.80, 95% CI: 1.21 to 2.39, p<.001). The overall reduction in perceived stress after AMI was more substantial in patients who did not experience angina post-AMI than those who did. After adjustment for other demographic, health, and psychosocial characteristics, the PSS-14 score was reduced by 1.88 points at 12 months after AMI in patients with angina (95% CI: −2.42 to −1.34, p<.001, p<.001), in comparison to 3.10 points for those without angina (95% CI: −3.60 to −2.60, p<.001).
Table 3.
Sex differences in perceived stress scale (PSS)-14 score over time, stratified by whether patient experienced angina after acute myocardial infarction (AMI)
| Explanatory variable | Patients with Angina after AMI | Patients without Angina after AMI | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Before adjustment for patient characteristicsa | After adjustment for patients characteristicsb | Before adjustment for patient characteristicsa | After adjustment for patients characteristicsb | |||||
|
| ||||||||
| Coefficient | P value | Coefficient | P value | Coefficient | P value | Coefficient | P value | |
| Female (vs. male) | 3.31 | <.001 | 1.72 | <.001 | 3.20 | <.001 | 1.80 | <.001 |
| Time | ||||||||
| 1 month (vs. baseline) | −3.20 | <.001c | −1.40 | <.001c | −4.69 | <.001c | −2.72 | <.001c |
| 12 months (vs. baseline) | −3.95d | <.001c | −1.88e | <.001c | −5.45f | <.001c | −3.10g | <.001c |
Coefficient estimates and p values were based on results from multivariable linear mixed effects models to account for correlation in repeated measures within the same individual over time.
Model adjusted for patient sex, time, and country.
Model adjusted for patient’s sex, time, and country; baseline age, race, education, marital status, number of children living in household, financial status, employment status, and number of comorbid conditions at baseline; AMI characteristics at initial admission, including ST-segment-elevation myocardial infarction (STEMI) versus non-STEMI, cardiogenic shock upon hospital admission, ejection fraction <40%, Global Registry of Acute Coronary Events (GRACE) risk score >99, hemodynamic instability on arrival, presentation to the hospital >6 hours after symptom onset, and length of stay during the initial hospitalization; and time-varying measures of Seattle Angina Questionnaire (SAQ) angina-related physical limitation score, the INTERHEART stressful life events scale, low social support determined by the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Social Support Inventory (ESSI), and depression based on the Patient Health Questionnaire (PHQ-9).
P value adjusted with step-down Bonferroni.
Implied a difference of −0.75 between 1-month and 12-month follow-up (p=0.04).
Implied a difference of −0.48 between 1-month and 12-month follow-up (p=0.48).
Implied a difference of −0.76 between 1-month and 12-month follow-up (p=.007).
Implied a difference of −0.38 between 1-month and 12-month follow-up (p=0.73).
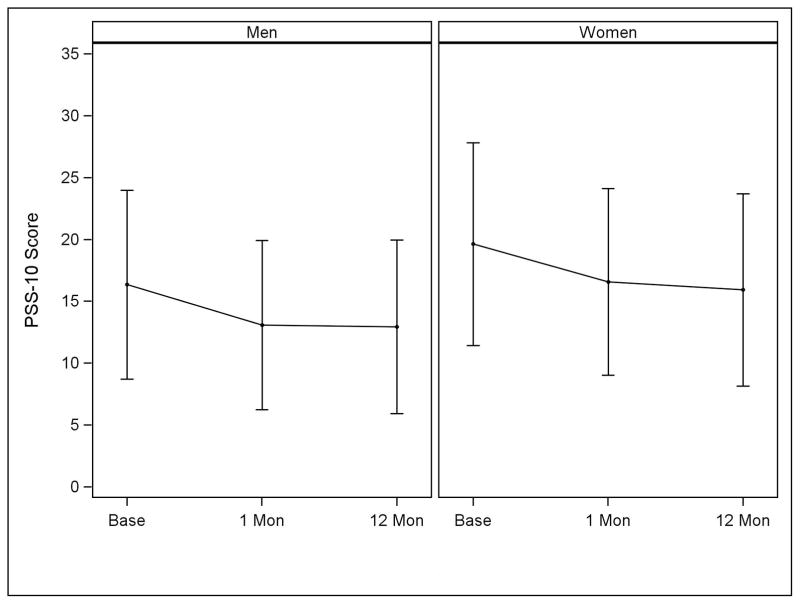
Perceived Stress Measured in PSS-10
When evaluated using PSS-10, perceived stress decreased from 19.7 ± 8.2 at baseline to 16.6 ± 7.5 at 1-month follow-up and 15.9 ± 7.8 at 12-month follow-up for women (Figure 2). In contrast, the score declined from 16.4 ± 7.6 to 13.1 ± 6.8 and 12.9 ± 7.0 for men at these interview time points.
Figure 2.
Observed perceived stress scale (PSS)-10 score over time, by sex.
PSS-10 score range: 0–40 (higher score indicates greater stress). The top and bottom error bars reflect one standard deviation above and below the corresponding mean PSS-10 score, respectively.
DISCUSSION
In young and middle-aged patients, perceived stress generally decreased over time during the 12 months after AMI, with most reduction occurring within the first month. Women reported higher levels of perceived stress than men throughout the 12-month period after an AMI. Adjustment for patients’ demographic, health, and psychosocial characteristics partially explained this difference in perceived stress between women and men, but significant sex difference remained. The rate of reduction in perceived stress over time did not vary by sex.
There has been a lack of longitudinal data on how patients’ perceived stress evolves over time after an AMI, especially for younger patients. Such information can guide clinical care to help optimize patient outcomes. Psychosocial stress has been shown as an independent risk factor for poor cardiovascular outcomes even after adjustment for other factors such as anxiety and depression (24, 30). Growing evidence supports that perceived stress influences cardiovascular health via physiological as well as behavioral mechanisms (7, 31). Perceived stress can directly affect both intrinsic and extrinsic vascular processes (e.g., atherosclerotic plaque formation, platelet reactivity) and possibly delay subsequent care-seeking by patients after an AMI (7, 8, 32). Perceived stress may also induce negative emotional response such as anger and hostility which could adversely affect cardiovascular health (7, 10, 31, 33). Greater psychological distress after AMI has been associated with increased risk for cardiovascular-related hospital readmissions (4). Recent research also linked higher levels of perceived stress at the time of AMI to worse recovery in quality of life and mental health in young and middle-aged patients (34). Therefore, it is important to understand patients’ status of psychological stress after AMI and how it changes over time. In this regard, our analyses showed that patients’ perceived stress reduced rapidly during the first month after AMI and stabilized afterwards as they recover from the event. Heightened stress management during the immediate post-AMI period maybe particularly beneficial.
The 2009 U.S. population normative data on PSS-10 score reported a mean of 16.1 for women (SD = 7.6) and 15.5 for men (SD = 7.4) (10). A 2006 study evaluating psychometric properties of the PSS-10 scale in a heterogeneous sample of adults without AMI in Spain reported a mean score of 18.9 for women (SD = 6.7) and 16.4 for men (SD = 6.4) (35). Therefore, our estimated PSS-10 scores suggest that patients in our sample tend to have higher than population average stress around the time of AMI, which then reduced to a level below population average at 12 months after the AMI. Although exact reasons for the below-population-average stress at 12-month follow-up warrant further investigation, this finding is consistent with theories of disability paradox (ill patients report good quality of life despite physical limitations) and response shift (patients may adjust their life priorities after experiencing an AMI) (36–38).
Importantly, our observed difference between women and men in PSS-10 scores reflects nearly half of a standard deviation of the population norm, suggesting a medium effect size of sex (39). This magnitude was larger than the sex difference in the general population. Part of the difference in perceived stress between women and men with AMI in our sample was due to their differences in demographic, health, and psychosocial characteristics, as our regression analyses suggest that adjustment of these factors reduced sex differences in perceived stress. Nonetheless, women continued to have higher perceived stress after adjusting for these characteristics.
The higher levels of perceived stress in women after an AMI can place them at increased risk for subsequent cardiac events compared with men (7). In addition, recent work by Vaccarino et al. showed a higher proportion of young female AMI survivors (50 years of age or younger) experiencing myocardial ischemia in response to a standardized mental stress task than similarly aged men, suggesting that women may be more prone to mental stress-induced myocardial ischemia (40). Together, higher levels of perceived stress and greater susceptibility to the adverse impact of stress in younger women may result in a worse recovery compared with that of younger men (41). Xu and colleagues (34) showed that adjustment for perceived stress at the time of AMI partially reduced sex differences in physical and mental health recovery at 1-month post-AMI in young and middle-aged patients. Further research on the role of post-AMI stress in influencing recovery would provide additional insights, and more studies on the pathophysiological mechanisms of the sex-stress-recovery relationship would inform strategies to reduce sex differences in outcomes. Moreover, stress management programs in clinical care should pay particular attention to younger female patients.
Finally, we observed a distinct pattern of changes in perceived stress among patients in Spain, whose stress level remained relatively stable over time. This is similar to findings from an earlier study in Spain that reported largely unchanged mental health status at 3 months after AMI or unstable angina despite substantial improvement in physical health (42). The exact reason for this distinct pattern is unknown, as cross-country comparisons of patients’ psychosocial status after AMI are rare. Contextual differences across countries in social welfare programs, sick leave benefits, and work environments (e.g., work hours and labor demand) may influence patients’ experience after AMI. Future studies investigating how country contextual characteristics and sociocultural factors may affect patients’ recovery would be informative. Moreover, our study focused on patients’ trajectory of perceived stress after AMI as we lacked data on their perceived stress prior to AMI. This precluded us from comparing patients’ perceived stress before versus after the AMI event. Additional research with detailed information on levels of perceived stress pre-AMI and longer-term follow-ups would allow for a more comprehensive understanding of the impact of an AMI on perceived stress.
We recognize several limitations of this study. First, our data were based on voluntary participants in VIRGO and may not represent all young and middle-aged patients with AMI in the 3 countries. However, comparison of clinical characteristics between patients in our sample and those reported in other studies of young and middle-aged adults hospitalized for AMI in the U.S. and Spain, such as the proportion with STEMI and prior AMI, suggest that they are largely comparable (43–46). Despite our relatively small sample size for Australia, the findings still provide informative data for understanding Australian patients’ experience with psychological stress after AMI. Second, some patients missed 1 or more follow-up interviews or did not have sufficient PSS-14 data at all interviews. Of the 3,509 patients in our sample, 92.4% completed at least 2 interviews with adequate PSS-14 data and 75.9% completed all 3 interviews with sufficient PSS-14 data (see Table S2, Supplemental Digital Content 1, which compares baseline characteristics of patients who completed all 3 interviews versus those who did not). Patients who did not have complete data at all 3 interviews were slightly younger and had worse financial and health status at baseline compared with patients who had complete data at all interviews. Thus, we may underestimate patients’ perceived stress during the recovery period. However, given our observation that most changes in perceived stress occurred during the first month after AMI and that 92% of our sample completed the 1-month interview, the impact of patients’ loss to follow-up on our key findings should be minimal. Third, self-perceived stress is a subjective measure and may be susceptible to bias in patient reporting. However, previous research of the PSS instrument demonstrated no meaningful differential item functioning by sex (47). Hence the measure should perform reasonably well in capturing sex difference in perceived stress. Future studies using other methods for assessing stress (e.g., measuring cortisol levels for biological stress) or assessing specific, rather than global, perceived stress (e.g., occupational stress, family stress) could provide additional insights.
To summarize, focusing on a unique sample of young and middle-aged patients with AMI, we delineated how patients’ perceived stress changed over time during the first 12 months of recovery. Perceived stress lessened over time for both women and men with most of the decrease occurring during the first month after AMI. However, women persistently experienced higher levels of perceived stress throughout the 12 months compared with their male counterparts, and this difference remained significant after adjustment for patients’ demographic, health, and psychosocial characteristics. Psychological stress may play an important role in explaining sex differences in cardiovascular health progression after an AMI and warrants close attention in future research. Clinical care for AMI should address how best to alleviate patients’ perceived stress and the potential impact of these strategies on recovery from AMI.
Supplementary Material
Acknowledgments
SOURCE OF FUNDING
This research project was supported by R01 HL081153 from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD. IMJOVEN (VIRGO in Spain) was supported by PI 081614 from the Fondo de Investigaciones Sanitarias del Instituto de Salud Carlos III, Ministry of Science and Technology, and additional funds from the Centro Nacional de Investigaciones Cardiovasculares (CNIC), Madrid, Spain. VIRGO Australia was supported in part by the Hospital Research Foundation Program Grant for the Vascular Disease Therapeutic Research Group, Adelaide, SA, Australia. Dr. Krumholz was supported by grant U01 HL105270 from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD during the time the work was conducted. Dr. Bueno was supported in part by grant BA08/90010 from the Fondo de Investigaciónes Sanitarias del Instituto de Salud Carlos III, Madrid, Spain.
Dr. Krumholz reports that he is the recipient of research agreements from Medtronic and from Johnson & Johnson (Janssen), through Yale University, to develop methods of clinical trial data sharing and is chair of a cardiac scientific advisory board for UnitedHealth. Dr. Bueno has received advisory/consulting fees from AstraZeneca, Bayer, BMS, Daichii-Sankyo, Eli-Lilly, Menarini, Novartis, Sanofi, and Servier, and research grants from AstraZeneca. Dr. Spertus discloses having received grants from Gilead, Genentech, Lilly, Abbott Vascular and Amorcyte. He provides consulting services to Amgen, Novartis, Janssen and Regeneron. He owns the copyright to the SAQ, KCCQ and PAQ and has an equity interest in Health Outcomes Sciences.
ACRONYMS USED IN TEXT
- AMI
acute myocardial infarction
- ENRICHD ESSI
Enhancing Recovery in Coronary Heart Disease Patients Social Support Inventory
- GRACE
Global Registry of Acute Coronary Events
- PHQ
Patient Health Questionnaire
- PSS
Perceived Stress Scale
- PTSD
posttraumatic stress disorder
- SAQ
Seattle Angina Questionnaire
- SD
standard deviation
- STEMI
ST-segment-elevation myocardial infarction
- VIRGO
Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients
Footnotes
CONFLICTS OF INTEREST
The other authors reported no conflicts of interest.
References
- 1.Alsen P, Brink E, Persson LO, Brandstrom Y, Karlson BW. Illness perceptions after myocardial infarction: relations to fatigue, emotional distress, and health-related quality of life. J Cardiovasc Nurs. 2010;25:E1–E10. doi: 10.1097/JCN.0b013e3181c6dcfd. [DOI] [PubMed] [Google Scholar]
- 2.Ginzburg K, Solomon Z, Bleich A. Repressive coping style, acute stress disorder, and posttraumatic stress disorder after myocardial infarction. Psychosom Med. 2002;64:748–57. doi: 10.1097/01.psy.0000021949.04969.2e. [DOI] [PubMed] [Google Scholar]
- 3.Hari R, Begre S, Schmid JP, Saner H, Gander ML, von Kanel R. Change over time in posttraumatic stress caused by myocardial infarction and predicting variables. J Psychosom Res. 2010;69:143–50. doi: 10.1016/j.jpsychores.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 4.von Kanel R, Hari R, Schmid JP, Saner H, Begre S. Distress related to myocardial infarction and cardiovascular outcome: a retrospective observational study. BMC Psychiatry. 2011;11:98. doi: 10.1186/1471-244X-11-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stevens S, Thomas SP. Recovery of midlife women from myocardial infarction. Health Care Women Int. 2012;33:1096–113. doi: 10.1080/07399332.2012.684815. [DOI] [PubMed] [Google Scholar]
- 6.Arnold SV, Smolderen KG, Buchanan DM, Li Y, Spertus JA. Perceived stress in myocardial infarction: long-term mortality and health status outcomes. J Am Coll Cardiol. 2012;60:1756–63. doi: 10.1016/j.jacc.2012.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 8.Alonzo AA. Acute myocardial infarction and posttraumatic stress disorder: the consequences of cumulative adversity. J Cardiovasc Nurs. 1999;13:33–45. doi: 10.1097/00005082-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Cohen S, Williamson G. Psychological stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988. pp. 31–67. [Google Scholar]
- 10.Cohen S, Janicki-Deverts D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006 and 2009. Journal of Applied Social Psychology. 2012;42:1320–34. [Google Scholar]
- 11.Rocha LP, Peterson JC, Meyers B, Boutin-Foster C, Charlson ME, Jayasinghe N, Bruce ML. Incidence of posttraumatic stress disorder (PTSD) after myocardial infarction (MI) and predictors of PTSD symptoms post-MI--a brief report. Int J Psychiatry Med. 2008;38:297–306. doi: 10.2190/PM.38.3.f. [DOI] [PubMed] [Google Scholar]
- 12.Roberge MA, Dupuis G, Marchand A. Post-traumatic stress disorder following myocardial infarction: prevalence and risk factors. Can J Cardiol. 2010;26:e170–5. doi: 10.1016/s0828-282x(10)70386-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drory Y, Kravetz S, Hirschberger G Israeli Study Group on First Acute Myocardial Infarction. Long-term mental health of women after a first acute myocardial infarction. Arch Phys Med Rehabil. 2003;84:1492–8. doi: 10.1016/s0003-9993(03)00316-2. [DOI] [PubMed] [Google Scholar]
- 14.Samad Z, Boyle S, Ersboll M, Vora AN, Zhang Y, Becker RC, Williams R, Kuhn C, Ortel TL, Rogers JG, O’Connor CM, Velazquez EJ, Jiang W REMIT Investigators. Sex differences in platelet reactivity and cardiovascular and psychological response to mental stress in patients with stable ischemic heart disease: insights from the REMIT study. J Am Coll Cardiol. 2014;64:1669–78. doi: 10.1016/j.jacc.2014.04.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim ES, Menon V. Status of women in cardiovascular clinical trials. Arteriosclerosis, thrombosis, and vascular biology. 2009;29:279–283. doi: 10.1161/ATVBAHA.108.179796. [DOI] [PubMed] [Google Scholar]
- 16.Lichtman JH, Lorenze NP, D’Onofrio G, Spertus JA, Lindau ST, Morgan TM, Herrin J, Bueno H, Mattera JA, Ridker PM, Krumholz HM. Variation in Recovery: Role of Gender on Outcomes of Young AMI patients (VIRGO) study design. Circ Cardiovasc Qual Outcomes. 2010;3:684–93. doi: 10.1161/CIRCOUTCOMES.109.928713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D’Onofrio G, Safdar B, Lichtman JH, Strait K, Dreyer RP, Geda M, Spertus JA, Krumholz HM. Sex differences in reperfusion in young patients with ST-segment–elevation myocardial infarction results from the VIRGO study. Circulation. 2015;131:1324–32. doi: 10.1161/CIRCULATIONAHA.114.012293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 19.Glei DA, Goldman N, Shkolnikov VM, Jdanov D, Shkolnikova M, Vaupel JW, Weinstein M. Perceived stress and biological risk: is the link stronger in Russians than in Taiwanese and Americans? Stress. 2013;16:411–20. doi: 10.3109/10253890.2013.789015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roth PL, Switzer FSI, Switzer DM. Missing data in multiple item scales: a Monte Carlo analysis of missing data techniques. Organ Res Methods. 1999;2:211–232. [Google Scholar]
- 21.Shrive FM, Stuart H, Quan H, Ghali WA. Dealing with missing data in a multi-question depression scale: a comparison of imputation methods. BMC Med Res Methodol. 2006;6:57. doi: 10.1186/1471-2288-6-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, Goodman SG, Granger CB, Steg PG, Gore JM, Budaj A, Avezum A, Flather MD, Fox KA GRACE Investigators. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA. 2004;291:2727–33. doi: 10.1001/jama.291.22.2727. [DOI] [PubMed] [Google Scholar]
- 23.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–41. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 24.Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthi-Amorn C, Sato H, Yusuf S INTERHEART Investigators. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:953–62. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 25.The ENRICHD Investigators. Enhancing Recovery in Coronary Heart Disease patients (ENRICHD): study design and methods. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, Froelicher ES, Czajkowski S, Youngblood M, Huber M, Berkman LF. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. J Cardiopulm Rehabil. 2003;23:398–403. doi: 10.1097/00008483-200311000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Vaglio J, Jr, Conard M, Poston WS, O’Keefe J, Haddock CK, House J, Spertus JA. Testing the performance of the ENRICHD Social Support Instrument in cardiac patients. Health Qual Life Outcomes. 2004;2:24. doi: 10.1186/1477-7525-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Endrighi R, Waters AJ, Gottlieb SS, Harris KM, Wawrzyniak AJ, Bekkouche NS, Li Y, Kop WJ, Krantz DS. Psychological stress and short-term hospitalisations or death in patients with heart failure. Heart. 2016 Jun 29; doi: 10.1136/heartjnl-2015-309154. pii: heartjnl-2015-309154. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kivimäki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A, Clays E, De Bacquer D, Dragano N, Ferrie JE, Geuskens GA, Goldberg M, Hamer M, Hooftman WE, Houtman IL, Joensuu M, Jokela M, Kittel F, Knutsson A, Koskenvuo M, Koskinen A, Kouvonen A, Kumari M, Madsen IE, Marmot MG, Nielsen ML, Nordin M, Oksanen T, Pentti J, Rugulies R, Salo P, Siegrist J, Singh-Manoux A, Suominen SB, Väänänen A, Vahtera J, Virtanen M, Westerholm PJ, Westerlund H, Zins M, Steptoe A, Theorell T IPD-Work Consortium. Job strain as a risk factor for coronary heart disease: A collaborative meta-analysis of individual participant data. Lancet. 2012;380:1491–7. doi: 10.1016/S0140-6736(12)60994-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parker MM, Ettinger R. Understanding Psychology. 2. Redding, CA: Redding: Horizon Textbook Publishing; 2007. Chapter 9 Emotion and Stress. [Google Scholar]
- 32.Kershaw KN, Brenes GA, Charles LE, Coday M, Daviglus ML, Denburg NL, Kroenke CH, Safford MM, Savla T, Tindle HA, Tinker LF, Van Horn L. Associations of stressful life events and social strain with incident cardiovascular disease in the Women’s Health Initiative. J Am Heart Assoc. 2014;3(3):e000687. doi: 10.1161/JAHA.113.000687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 34.Xu X, Bao H, Strait K, Spertus JA, Lichtman JH, D’Onofrio G, Spatz E, Bucholz EM, Geda M, Lorenze NP, Bueno H, Beltrame JF, Krumholz HM. Sex differences in perceived stress and early recovery in young and middle-aged patients with acute myocardial infarction. Circulation. 2015;131:614–23. doi: 10.1161/CIRCULATIONAHA.114.012826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Remor E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS) Span J Psychol. 2006;9:86–93. doi: 10.1017/s1138741600006004. [DOI] [PubMed] [Google Scholar]
- 36.Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med. 1999;48:977–88. doi: 10.1016/s0277-9536(98)00411-0. [DOI] [PubMed] [Google Scholar]
- 37.Norekval TM, Wahl AK, Fridlund B, Nordrehaug JE, Wentzel-Larsen T, Hanestad BR. Quality of life in female myocardial infarction survivors: a comparative study with a randomly selected general female population cohort. Health Qual Life Outcomes. 2007;5:58. doi: 10.1186/1477-7525-5-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sprangers MA, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med. 1999;48:1507–15. doi: 10.1016/s0277-9536(99)00045-3. [DOI] [PubMed] [Google Scholar]
- 39.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 40.Vaccarino V, Shah AJ, Rooks C, Ibeanu I, Nye JA, Pimple P, Salerno A, D’Marco L, Karohl C, Bremner JD, Raggi P. Sex differences in mental stress-induced myocardial ischemia in young survivors of an acute myocardial infarction. Psychosom Med. 2014;76:171–80. doi: 10.1097/PSY.0000000000000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Orth-Gomér K, Deter HC. Sex and Gender Issues in Cardiovascular Research. Psychosom Med. 2015;77:1067–8. doi: 10.1097/PSY.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 42.Failde II, Soto MM. Changes in health related quality of life 3 months after an acute coronary syndrome. BMC Public Health. 2006;6:18. doi: 10.1186/1471-2458-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang Z, Fang J, Gillespie C, Wang G, Hong Y, Yoon PW. Age-specific gender differences in in-hospital mortality by type of acute myocardial infarction. Am J Cardiol. 2012;109:1097–103. doi: 10.1016/j.amjcard.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 44.Awad HH, McManus DD, Anderson FA, Jr, Gore JM, Goldberg RJ. Young patients hospitalized with an acute coronary syndrome. Coron Artery Dis. 2013;24:54–60. doi: 10.1097/MCA.0b013e32835b0bf7. [DOI] [PubMed] [Google Scholar]
- 45.Morillas P, Bertomeu V, Pabón P, Ancillo P, Bermejo J, Fernández C, Arós F PRIAMHO II Investigators. Characteristics and outcome of acute myocardial infarction in young patients. The PRIAMHO II study. Cardiology. 2007;107:217–25. doi: 10.1159/000095421. [DOI] [PubMed] [Google Scholar]
- 46.Tisminetzky M, McManus DD, Gore JM, Yarzebski J, Coles A, Lessard D, Goldberg RJ. 30-year trends in patient characteristics, treatment practices, and long-term outcomes of adults aged 35 to 54 years hospitalized with acute myocardial infarction. Am J Cardiol. 2014;113:1137–41. doi: 10.1016/j.amjcard.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cole SR. Assessment of differential item functioning in the Perceived Stress Scale-10. J Epidemiol Community Health. 1999;53:319. doi: 10.1136/jech.53.5.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.