Abstract
Background
Paroxysmal atrioventricular block (P-AVB) is a well-known cause of syncope; however, its underlying mechanism is difficult to determine. This study aimed to evaluate a new ECG index, the “vagal score (VS),” to determine the mechanism of P-AVB.
Methods
We evaluated the VS in 20 patients with P-AVB (13 men, 7 women; aged 25–78 years [mean, 59.3 years]). The VS was developed by assigning 1 point each for the following: (1) no AVB or intraventricular conduction disturbance on the baseline ECG, (2) PR prolongation immediately before P-AVB, (3) sinus slowing immediately before P-AVB, (4) initiation of P-AVB by PP prolongation, (5) sinus slowing during ventricular asystole, and (6) resumption of AV conduction with PP shortening, and by assigning –1 point each for (7) the initiation of P-AVB by a premature beat, and (8) resumption of AV conduction by an escape beat. Based on the clinical situations and electrophysiologic findings, we considered the mechanism of P-AVB as vagally mediated or intrinsic conduction disease (ICD).
Results
The VS ranged from 5 to –2 points for each patient. Five patients with a definite vagally mediated P-AVB had high VSs (3–5 points). We observed characteristic ECG findings of ICD consisting of changes in AV conduction by an extrasystole and/or escape beat in only 5 of the 6 patients (83%) with a low VS (1 to –2).
Conclusions
The VS is simple and potentially useful for determining the mechanism of P-AVB. P-AVB with a VS ≥3 strongly suggested a vagally mediated mechanism.
Keywords: Paroxysmal atrioventricular block, Electrocardiogram (ECG), Mechanism, Vagally mediated, Intrinsic conduction disease
1. Introduction
Paroxysmal atrioventricular block (P-AVB) is a well-known cause of syncope. However, it is probably underreported because of poor recognition, limited information in medical literature, its unpredictability, and the lack of a clear marker for AV conduction disease between culprit episodes [1]. In addition, the underlying mechanism of P-AVB is difficult to determine. Identifying the etiology of P-AVB is important because cases of vagally mediated P-AVB are usually benign and do not necessarily require cardiac pacemaker implantation [2]. Although ECG findings are reported to be important for predicting the mechanism of P-AVB [1], [2], no clinically useful ECG scoring system for P-AVB is currently available. This study aimed to evaluate a new ECG index, the “vagal score (VS),” for determining the mechanism of P-AVB.
2. Material and methods
2.1. Clinical characteristics of the study population
The study population consisted of 20 patients (13 men and seven women), with a mean age of 59.3±14.7 years (range, 25–78 years). These patients had clinically documented P-AVB with clear ECG recordings in our institutions. P-AVB was defined as a sudden onset of complete AVB with two or more consecutive blocked P waves and ventricular asystole of >3 s. The clinical characteristics of the study patients are shown in Table 1. Their symptoms were syncope in 13 patients (including 1 patient with convulsion during sleep), faintness in 4, and none in 3. Baseline 12-lead ECG showed PR prolongation (>0.22 s) in 6 patients, right bundle branch block (RBBB) in 4 including 2 with left axis deviation (LAD), intraventricular conduction disturbance (IVCD) in 1, and no AVB or IVCD in the remaining 10. Structural heart disease was observed in 6 patients: coronary artery disease in 4 patients (including 2 patients with a previous myocardial infarction), cardiac tumor involving the left ventricle in 1, and mitral valve prolapse without mitral regurgitation in 1. The ECG-documented maximum ventricular asystole during P-AVB varied from 3.6 to 60 s. The index ECG was recorded by ambulatory Holter ECG monitoring for 8 patients, in-hospital ECG monitoring for 6, standard 12-lead ECG for 4, and an implantable loop recorder for 2. An electrophysiologic study (EPS) was performed for 11 patients. Abnormal AV conduction was recognized in 4 patients. A cardiac pacemaker was implanted in 13 patients.
Table 1.
Clinical characteristics of study patients.
 |
2.2. Definition of vagal score
The VS was developed by assigning 1 point for patients with each of the following: (1) no AVB or IVCD on the baseline ECG, (2) PR prolongation immediately before P-AVB, (3) sinus slowing immediately before P-AVB, (4) initiation of P-AVB by PP prolongation, (5) sinus slowing during ventricular asystole, and (6) resumption of AV conduction with PP shortening, and by assigning –1 point each for (7) the initiation of P-AVB by a premature beat, and (8) resumption of AV conduction by an escape beat. We copied the index-ECG recording of P-AVB in all 20 patients. ECG scoring was performed in each index-ECG recording by 3 blinded investigators. Scoring discrepancies were resolved by the principal investigator (MS).
2.3. Possible mechanism of P-AVB
Based on the clinical situations and EPS results, we considered the mechanism of P-AVB either vagally mediated or intrinsic conduction disease (ICD).
3. Results
3.1. Diagnosis of vagally mediated P-AVB
The mechanism underlying the P-AVB in 5 patients (cases 1, 2, and 4–6) was definitely a vagal mechanism based on the following reasons:
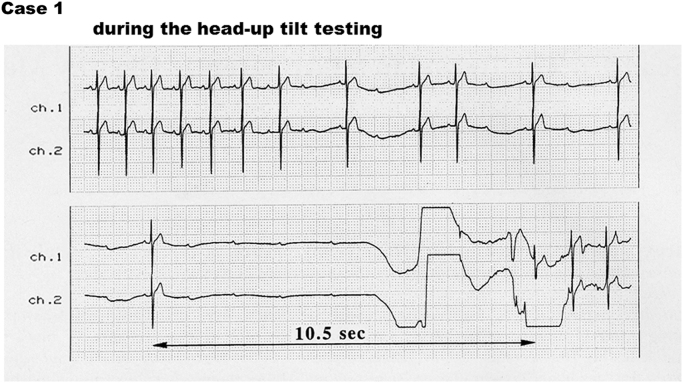
In case 1, a head-up tilt test was conducted as in a healthy volunteer. The patient had syncope due to P-AVB during the head-up tilt test (Fig. 1) [3].
Fig. 1.
Episode in case 1. Paroxysmal atrioventricular block (P-AVB) was induced during the head-up tilt test [3]. The vagal score (VS) was 5 points: normal baseline ECG, PR prolongation and sinus slowing immediately before P-AVB, initiation of P-AVB by PP prolongation, and sinus slowing during ventricular asystole.
In case 2, the patient had a history of cough syncope. Syncope with P-AVB was induced by carotid sinus massage. We recommended implantation of cardiac pacemaker; however, the patient rejected the recommendation.
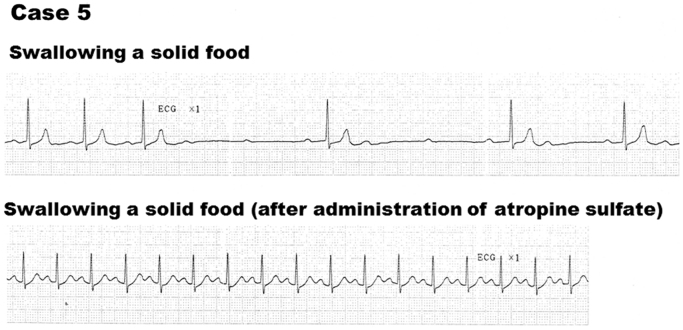
In 2 patients (cases 4 and 5), swallowing induced P-AVB, which was inhibited after an intravenous administration of atropine sulfate (Fig. 2). The baseline EPS was normal in case 3; however, swallowing a solid food repeatedly induced paroxysmal A-H block. In case 6, the patient experienced P-AVB during meals as shown in the Holter ECG recording. The resting ECG revealed a first-degree to second-degree Wenckebach AVB. P-AVB was provoked by Valsalva maneuver; however, it was inhibited after an intravenous atropine injection. A-H Wenckebach block was observed during the EPS; however, it was recovered to the first-degree AVB with an A-H interval of 400 ms after intravenous administration of atropine sulfate.
Fig. 2.
Episode in case 5. Swallowing induced paroxysmal atrioventricular block (P-AVB) (upper ECG), which was inhibited after an administration of intravenous atropine (lower ECG). The vagal score (VS) was 3 points: sinus slowing just before and during P-AVB, and the initiation of P-AVB by PP prolongation.
3.2. Diagnosis of P-AVB due to ICD
Of the 11 patients who had the EPS, P-AVB due to ICD was diagnosed in 3 patients: 2 with A-H block (cases 15 and 20) and 1 with intra-His block (case 14). In case 14, the patient had P-AVB, which was reproduced as bradycardia-dependent H-V block during the EPS. Intra-His block was diagnosed because the QRS morphology of the escape beats was identical to that of the conducted beats.
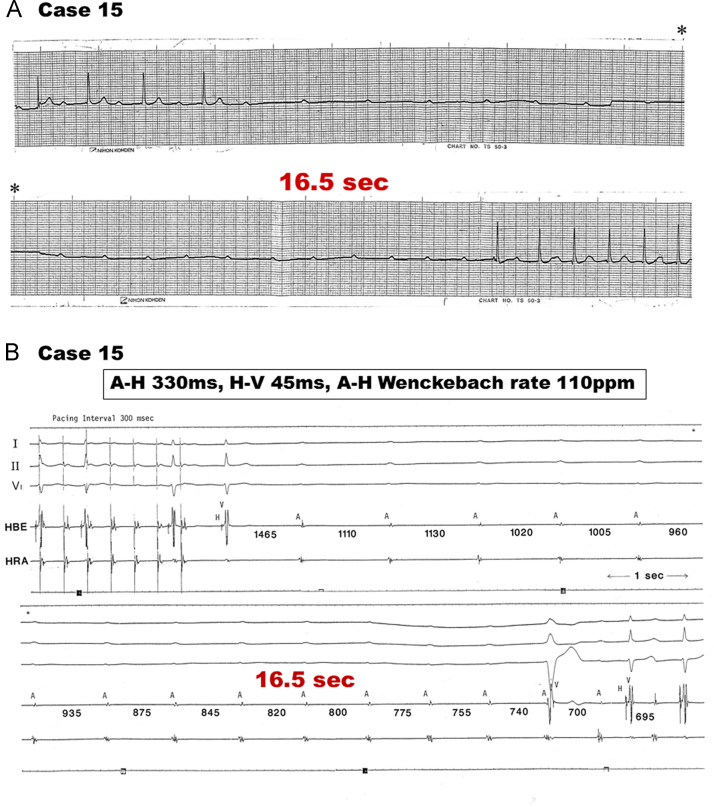
In case 15, baseline ECG showed first-degree AVB. P-AVB was recorded on ECG monitoring with a long asystole of 16.5 s (Fig. 3A). EPS revealed a prolonged AH interval of 330 ms and a normal HV interval of 45 ms. The cessation of rapid atrial pacing of 200 bpm induced a long P-P interval and then a bradycardia-dependent P-AVB occurred (Fig. 3B). During a long asystole, sinus acceleration was observed, and AV conduction was resumed by a ventricular escape.
Fig. 3.
(A) Episode in case 15. Baseline ECG showed the first-degree atrioventricular block (AVB). Paroxysmal AVB (P-AVB) was recorded on the ECG monitoring with a long asystole of 16.5 . The vagal score was 1 point: sinus slowing immediately before P-AVB and the initiation of P-AVB by PP prolongation but the resumption of AV conduction by a junctional escape. (B) Electrophysiologic study (EPS) findings in case 15 EPS revealed a prolonged AH interval of 330 ms and a normal HV interval of 45 ms. The cessation of rapid atrial pacing of 200 bpm induced paroxysmal atrioventricular block with an asystole of 16.5 s. During a long asystole, sinus acceleration was observed and AV conduction was resumed by a ventricular escape.
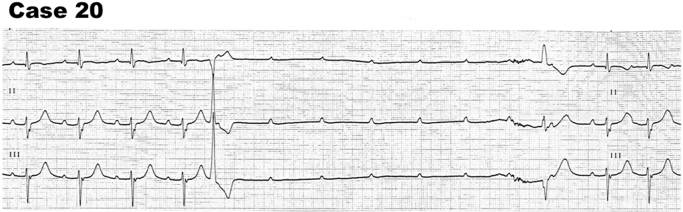
In case 20, the patient experienced PR prolongation of 0.28 s with RBBB and LAD (trifascular block pattern) on baseline ECG. EPS revealed an abnormal AV conduction with A-H Wenckebach rate of 80 bpm and a prolonged effective refractory period of AV node (720 ms). The episodic ECG indicated bradycardia-dependent AVB with an initiation of paroxysmal AVB by a ventricular premature beat and the resumption of AV conduction by a ventricular escape (Fig. 4).
Fig. 4.
Episode in case 20. Baseline ECG showed a trifascular block pattern: first-degree atrioventricular block (AVB) with right bundle branch block and left axis deviation. The vagal score (VS) was –2: initiation of paroxysmal AVB by a ventricular premature beat and the resumption of AV conduction by a ventricular escape.
3.3. Vagal score of the study patients
The VS values ranged from 5 to –2 points (average 1.75) among the 20 patients (Table 2). We divided the study patients into three groups according to VS: eight patients with a high VS (3–5 points), 6 with an intermediate VS (2 points), and 6 with a low VS (1 to –2 points).
Table 2.
Vagal score in each patient.
 |
3.3.1. High VS (3–5 points) group
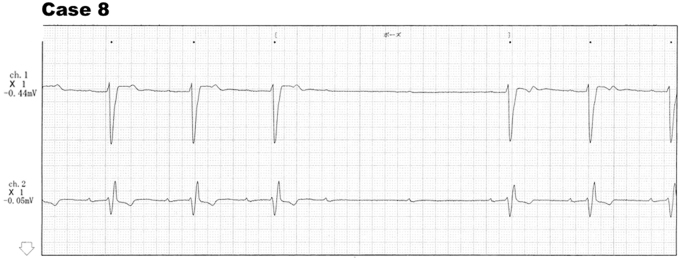
One of the 8 patients in the high-VS group was asymptomatic. The resting ECG showed no conduction abnormality in 5 of the high-VS patients (63%). EPS was performed in 3 patients: two normal and 1 with AH prolongation. In addition, 1 patient (case 8) with a trifascular block (first-degree AVB with RBBB and LAD) on the baseline ECG had a high VS of 3 points (Fig. 5). All 5 patients (cases 1, 2, and 4–6) diagnosed with vagally mediated P-AVB were included in this group (Table 2).
Fig. 5.
Episode in case 8. The patient had a trifascular block, first-degree atrioventricular block (AVB) with right bundle branch block and left axis deviation, on the baseline ECG. The vagal score (VS) was 3 points: PR prolongation just before paroxysmal AVB, sinus slowing during ventricular pause, and the resumption of AV conduction with PP shortening.
3.3.2. Intermediate VS (2 points) group
Two of the 6 patients in the intermediate-VS group were asymptomatic. The resting ECG revealed no conduction abnormality in 4 patients (67%). An EPS was conducted in 5 patients: the results were normal in 4 patients and abnormal in one patient (case 14) diagnosed with bradycardia-dependent intra-His block.
3.3.3. Low VS (1 to –2) group
All 6 patients in the low VS group were symptomatic. The resting ECG showed no conduction abnormality in only 1 patient (17%). An EPS was performed in 3 patients revealing abnormal AH block in 2 patients with bradycardia-dependent AVB (cases 15 and 20) (Figs. 3 and 4) and normal results in the resting patient. Five of the 6 patients (83%) showed characteristic ECG findings; P-AVB was initiated by a premature beat (three patients), and AV conduction was resumed by an escape beat (five patients) (Figs. 3 and 4), which were not observed in the high-VS or intermediate-VS groups.
4. Discussion
4.1. Main findings
The VS is simple and may be useful for determining the mechanism of P-AVB. A VS ≥3 strongly suggested a vagally mediated mechanism.
4.2. Characteristic ECG findings and mechanism of P-AVB
4.2.1. Vagally mediated P-AVB
The differential diagnosis between vagally mediated AVB and intrinsic AVB is based on the behavior of the sinus rate [2]. A vagal input depresses sinus node function and AV nodal conduction; however, it does not influence the conductivity in the His-Purkinje system (HPS) [2]. Vagally mediated AVB can be diagnosed when a simultaneous decrease in sinus node function and AV conduction occurs [2].
The following reported ECG findings suggest vagally mediated P-AVB: (1) significant PR prolongation or Wenckebach block before the initiation of AVB [1], [2], (2) prolongation of P-P interval during ventricular asystole [1], [2], (3) significant PR prolongation on the resumption of AV conduction [1], (4) resumption of AV conduction on sinus acceleration (shortening P-P interval) [1], [2], and (5) no retrograde activation of the His bundle with a ventricular or His extrasystole to reset and abolish AVB [1]. PR and QRS intervals are generally normal in most patients with vagally mediated AVB [1]. In addition, a clinical history highly suggestive of heightened vagal tone (i.e., during micturition, phlebotomy, etc.) may be present [1].
4.2.2. P-AVB due to ICD
P-AVB due to ICD usually occurs in the HPS as an intra-His or infra-His block [1]. In patients with intrinsic AVB, evidence of distal conduction disease at baseline ECG is often present including RBBB, LBBB, and IVCD [1]. The ECG findings suggestive of ICD can be summarized as follows. First, P-AVB is initiated by atrial, His, or ventricular premature extrasystole [1], [2]. In addition, tachycardia can initiate P-AVB via suppression of AV conduction [1]. Second, sinus acceleration occurs during ventricular asystole without affecting the block [1], [2]. (3) Unidirectonal anterograde block with preservation of retrograde conduction is the mechanism by which an escape beat can reset and resume 1:1 AV conduction in P-AVB [1], [2]. This finding was explained as a phase 4-block mechanism [4]; however, this conclusion is controversial [5].
4.2.3. ATP-sensitive P-AVB
The other recently proposed mechanism of P-AVB is the so-called “idiopathic” or “ATP-sensitive” P-AVB, described by European investigators [6], [7]. Patients with ATP-sensitive AVB have no structural heart disease and show normal ECG without baseline conduction abnormalities and negative EPS results [6]. These patients are reported to have low baseline adenosine plasma levels (the so-called “low adenosine syncope” [8]) and to show increased susceptibility to exogenous adenosine, i.e., high sensitivity to ATP [6], [7]. The ECG findings suggestive of ATP-sensitive P-AVB can be summarized as follows: (1) normal ECG, without baseline conduction abnormalities [6]; (2) stable PR interval before and at the end of the pause [6]; (3) P-AVB occurrence with or without minimal P-P cycle lengthening [6]; and (4) P-AVB not initiated by any extrasystole, increased heart rate (tachycardia dependent), or decreased heart rate (bradycardia-dependent) [6].
4.3. Clinical significance of the vagal score
We constructed a scoring system for ECG findings to investigate the mechanisms of P-AVB, particularly for the differential diagnosis between vagally mediated and ICD, because the former type of P-AVB could be treated without pacemaker implantation in some cases. In our VS system, we assigned 1 point each for ECG findings suggesting a vagal mechanism and –1 point each for ECG findings suggesting ICD. The cases of definite vagally mediated P-AVB showed 3–5 VS points in our study patients. Therefore, a VS ≥3 may strongly suggest a vagal mechanism. However, 1 patient (case 8) with a trifascular block (first-degree AVB with RBBB and LAD) also had a high VS (3 points) (Fig. 5). We believe that the P-AVB of this patient may occur with some vagal stimulation because vagally mediated AVB can be induced in not only healthy persons but also diseased patients.
In ICD cases, the VS may be low or may be negative. Some intrinsic AVB may be tachycardia-dependent or bradycardia-dependent. The differential diagnosis of tachycardia-dependent AVB with vagally mediated AVB is relatively easy. However, the differential diagnosis between bradycardia-dependent AVB and vagally mediated AVB is difficult because of the similar behavior of their sinus rates: sinus-slowing initiates P-AVB and sinus-acceleration resumes AV conduction [2]. The initiation of P-AVB by an extrasystole and the resumption of AV conduction by an escape beat are common in patients with ICD [1], [2]. These ECG findings are strongly suggestive of ICD. Therefore, we assigned –1 point each for these ECG findings. In our study patients, we observed a change in AV conduction by an extrasystole or escape beat in 5 of the 6 patients (83%) in the low-VS group; however, these ECG findings were not observed in the high-VS or intermediate-VS groups.
The VS may be 1 point (no AVB or IVCD on baseline ECG) in patients with typical ATP-sensitive P-AVB, as reported [6]. However, whether our study patients included those with or without ATP-sensitive P-AVB could not be determined because we did not measure the plasma adenosine values or perform the ATP test. The VS in patients with ATP-sensitive P-AVB is expected to be intermediate between vagal and intrinsic mechanisms, although a significant overlap is possible.
4.4. Study limitations
This study has several limitations. First, the differential diagnosis between vagally mediated AVB and intrinsic AVB may be difficult when only a slight increase in PR or PP intervals is observed [2]. Second, vagally mediated AVB does not deny the necessity of a pacemaker. The ISSUE 3 study [9] showed the clinical benefit of pacemaker implantation in patients with the cardio-inhibitory type of vasovagal syncope. In our study, 2 patients with definite vagal AVB required a pacemaker implantation because of frequent syncope. Third, we could not perform an EPS in all patients. However, the significance of an EPS is controversial. Although an EPS is specific for P-AVB due to ICD, a negative EPS result does not exclude P-AVB due to ICD as a probable cause of syncope [1]. Fourth, we observed intrinsic AH block in 2 patients with bradycardia-dependent P-AVB. Unidirectonal anterograde block with preservation of retrograde conduction, as is commonly observed in infra-nodal block but not in AV nodal block, is the mechanism by which an escape beat is able to reset and resume 1:1 AV conduction in P-AVB [1], [2]. Two patients (cases 15 and 20) had the above-mentioned ECG finding. Thus, we believe that AVB may occur in the His bundle (intra-His block) with a misrecording of the proximal His potential in our patients. Finally, we evaluated a limited number of patients (20 cases) in this study. More studies with greater number of patients are required to ascertain the clinical value of the VS.
5. Conclusions
The VS is simple and potentially useful for determining the mechanism of P-AVB. A VS ≥3 is strongly suggestive of a vagally mediated mechanism.
Conflict of interest
All authors declare no conflict of interest related to this study.
References
- 1.Lee S., Wellens H.J.J., Josephson M.E. Paroxysmal atrioventricular block. Heart Rhythm. 2009;6:1229–1234. doi: 10.1016/j.hrthm.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 2.Alboni P., Holz A., Brignole M. Vagally mediated atrioventricular block: pathophysiology and diagnosis. Heart. 2013;99:904–908. doi: 10.1136/heartjnl-2012-303220. [DOI] [PubMed] [Google Scholar]
- 3.Sumiyoshi M., Nakata Y., Mineda Y. Paroxysmal atrioventricular block induced during head-up tilt testing in an apparently healthy man. J Cardiovasc Electrophysiol. 1997;8:561–564. doi: 10.1111/j.1540-8167.1997.tb00824.x. [DOI] [PubMed] [Google Scholar]
- 4.Rosenbaum M.B., Elizare M.V., Levi R.J. Paroxysmal atrioventricular block related to hypopolarization and spontaneous diastolic depolarization. Chest. 1973;63:678–688. doi: 10.1378/chest.63.5.678. [DOI] [PubMed] [Google Scholar]
- 5.El-Sherif N., Jalife J. Paroxysmal atrioventricular block: are phase 3 and phase 4 block mechanisms or misnomers? Heart Rhythm. 2009;6:1514–1521. doi: 10.1016/j.hrthm.2009.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brignole M., Deharo J.-C., Roy L.D. Syncope due to idiopathic paroxysmal atrioventricular block. Long-term follow-up of a distinct form of atrioventricular block. J Am Coll Cardiol. 2011;58:167–173. doi: 10.1016/j.jacc.2010.12.045. [DOI] [PubMed] [Google Scholar]
- 7.Blanc J.-J., Dauphin C.L. Syncope associated with documented paroxysmal atrioventricular block reproduced by adenosine 5ʹ triphosphate injection. Europace. 2014;16:923–927. doi: 10.1093/europace/eut322. [DOI] [PubMed] [Google Scholar]
- 8.Deharo J.-C., Guieu R., Mechulan A. Syncope without prodromes in patients with normal heart and normal electrocardiogram: a distinct entity. J Am Coll Cardiol. 2013;62:1075–1080. doi: 10.1016/j.jacc.2013.05.060. [DOI] [PubMed] [Google Scholar]
- 9.Brignole M., Menozzi C., Moya A. Pacemaker therapy in patients with neurally mediated syncope and documented asystole. Third International Study on Syncope of Uncertain Etiology (ISSUE-3). A randomized trial. Circulation. 2012;125:2566–2571. doi: 10.1161/CIRCULATIONAHA.111.082313. [DOI] [PubMed] [Google Scholar]