Abstract
Background
Variation exists in cardiac arrest (CA) survival among institutions. We sought to determine institutional-level characteristics of academic medical centers (AMCs) associated with CA survival.
Methods
We examined discharge data from AMCs participating with Vizient clinical database–resource manager. We identified cases using ICD-9 diagnosis code 427.5 (CA) or procedure code 99.60 (CPR). We estimated hospital-specific risk-standardized survival rates (RSSRs) using mixed effects logistic regression, adjusting for individual mortality risk. Institutional and community characteristics of AMCs with higher than average survival were compared with those with lower survival.
Results
We analyzed data on 3,686,296 discharges in 2012, of which 33,700 (0.91%) included a CA diagnosis. Overall survival was 42.3% (95% CI 41.8–42.9) with median institutional RSSR of 42.6% (IQR 35.7–51.0; Min-Max 19.4–101.6). We identified 28 AMCs with above average survival (median RSSR 61.8%) and 20 AMCs with below average survival (median RSSR 26.8%). Compared to AMCs with below average survival, those with high CA survival had higher CA volume (median 262 vs.119 discharges, p = 0.002), total beds (722 vs. 452, p = 0.02), and annual surgical volume (24,939 vs. 13,109, p<0.001), more likely to offer cardiac catheterization (100% vs. 72%, p = 0.007) or cardiac surgery (93% vs. 61%, p = 0.02) and cared for catchment areas with higher household income ($61,922 vs. $49,104, p = 0.004) and lower poverty rates (14.6% vs. 17.3%, p = 0.03).
Conclusion
Using discharge data from Vizient, we showed AMCs with higher CA and surgical case volume, cardiac catheterization and cardiac surgery facilities, and catchment areas with higher socioeconomic status had higher risk-standardized CA survival.
Background
In-hospital cardiac arrest (IHCA) is an important issue for institutions caring for the sick and injured. In the United States, an estimated 209,000 IHCA may occur annually.[1] Mortality from IHCA is significant, ranging from 58 to 100% with only small improvements in the last quarter century.[2, 3] In addition, it varies widely between institutions and has been associated with institutional size, geographic location, and teaching status. [4], [5]
Unlike out-of-hospital cardiac arrest, which is largely a random event, IHCA is often a predictable event where progressive deterioration in clinical status leads to respiratory failure and/or cardiogenic shock. Despite the publication of clinical care guidelines for primary and secondary prevention of cardiac arrest, [6] [7] wide variations persist in institutional survival, suggesting potential associations with additional institutional characteristics.
Using data from Vizient (formerly the University HealthSystem Consortium) clinical database–resource manager [CDB/RM], we sought to evaluate hospital variations in cardiac arrest survival and identify institutional characteristics that distinguish between best and weakest performers.
Methods
Study design
In this investigation, we conducted a retrospective cohort analysis of hospital discharge data from Vizient’s clinical database–resource manager (CDB/RM) linked with the American Hospital Association (AHA) institutional database and the American Community Survey (ACS). The study was approved by the Institutional Review Board of the University of Alabama at Birmingham.
Study setting
Vizient includes, but is not now limited to, a consortium of approximately 300 hospitals across 120 academic health systems in the United States. Vizient CBD/RM members share performance data to facilitate quality improvement and dissemination of best practices.
Data sources
The Vizient CBD/RM contains clinical, discharge, procedure, and outcome data for each hospital encounter among member institutions. We linked the Vizient CBD/RM to annual survey data from the American Hospital Association (AHA) to ascertain institutional characteristics. [8] Institution catchment areas were defined by combining surrounding ZIP codes into Hospital Service Areas (HSAs). Socioeconomic characteristics of HSAs were gathered from the American Community Survey (ACS) through the National Historical Geographic Information System (NHGIS).[9] Specifically, we extracted demographic data by ZIP code tabulation area using ACS 5-year data for years 2008–2012.
Study population
We examined all participating Vizient institutions contributing data to the CDB/RM between January 1, 2012, and December 31, 2012. We defined cardiac arrest as any discharge with an International Classification of Diseases, Version 9 (ICD-9) code for cardiac arrest (427.5).[10] While this approach is unable to differentiate between in-hospital cardiac arrest (IHCA) and out-of-hospital cardiac arrest (OHCA), this approach has been previously used in studies characterizing cardiac arrest epidemiology.[4, 11] In addition, we extended the definition to include discharges with an ICD-9 procedure code for cardiopulmonary resuscitation (CPR; ICD-9: 99.60) as the sole indication for CPR is cardiac arrest. We excluded patients under 18 years of age, prisoners, pregnant, under hospice care, admitted to a psychiatric unit, or transferred in from another acute care hospital. We excluded hospitals reporting fewer than twenty-five cardiac arrest discharges during the study period.
Discharge, institution, and community characteristics
Using the Vizient CBD/RM, we identified discharge characteristics including age, gender, race, insurance type, admission to the intensive care unit (ICU), length of stay, and comorbidities. To evaluate patient comorbidities, we identified individual Elixhauser comorbidities. [12] For risk adjustment purposes, we obtained Vizient CBD/RM expected probability of mortality, which is estimated using diagnosis-related group (DRG)-specific risk models. Specifically, the risk prediction models incorporate admission mortality risk scores derived from the 3M™ APR-DRG grouper, All Patients Refined risk of mortality class (Minor, Moderate, Major, or Extreme), relevant comorbidities, admission characteristics, diagnoses, and procedures. We did not base our definition of cardiac arrest on DRG, primary diagnosis, or data suggesting cardiac arrest was present on arrival.
From the AHA survey database, we obtained institutional characteristics including hospital control, number of beds and surgical operations performed, clinical services offered, teaching hospital certification, Census region, population setting, and the number of Medicaid discharges. For teaching hospital certification, we identified institutions certified by the Accreditation Council for Graduate Medical Education (ACGME) as well as the Council of Teaching Hospitals and Health Systems (COTH) during the study period. We categorized the referral population using the National Center for Health Statistics Urban-Rural Classification Scheme, with counties classified as part of a large metropolitan area or smaller area (medium, small, or micropolitan). We defined safety net hospitals as those with Medicaid discharges that were more than one standard deviation above the national average. We assessed both total number and percentage of all discharges.
To characterize the socioeconomic status of the catchment area surrounding each hospital, we obtained the percentage living below the federal poverty level and median household income at the ZIP code level from the ACS. To better define catchment areas, we combined ZIP codes into Hospital Service Areas (HSAs), and aggregated the measures appropriately. For household income, we calculated a weighted mean based on the total population of each ZIP code within an HSA.
Outcome measure
The primary outcome for this study was inpatient survival. We identified inpatient deaths using discharge disposition status codes available in the CDB/RM. Discharge status codes in the Vizient CBD/RM have demonstrated high concordance with results obtained via patient-level case audits. [13]
Data analysis
For each part of our cardiac arrest definition, we calculated the percent surviving and estimated confidence intervals using the exact binomial method. We compared discharge characteristics between those who died during hospitalization and those who survived using t-tests of equal means for continuous variables and Pearson chi-square tests of association for categorical variables. To obtain risk-standardized survival rates (RSSRs) for each hospital, we fit a mixed effects logistic regression model, adjusting for Vizient CBD/RM expected mortality and specifying random intercepts. We chose to use Vizient CBD/RM expected mortality for risk adjustment, despite its proprietary nature, as it allows for a valid comparison across admitting conditions and exhibited good discrimination among cardiac arrest cases (C-statistic 0.74). Using reliability-adjusted Empirical Bayes estimates of the log odds obtained from the model, we calculated RSSRs by transforming to percentages at the average risk of mortality for the full population.[14]
We defined high performing (high survival outlier) hospitals as institutions with an RSSR significantly higher than the study cohort average (lower confidence interval limits excluding the average) and poor performing hospitals (low survival outlier) as institutions with an RSSR significantly lower than the average (upper confidence intervals excluding the average). Institutional characteristics were compared between high, low, and non-outlier survival hospitals using non-parametric Kruskal-Wallis tests of equal distribution for continuous variables, Fisher-Irwin Exact tests for categorical variables with cell sizes <5, and Pearson chi-square tests for categorical variables with cell sizes ≥5. We also examined the linear prediction of mean RSSR, modeled using volume-weighted ordinary least squares regression with restricted cubic splines over values of cardiac arrest volume (specifying 7 knots). All analyses were performed using Stata 13.1 (College Station, TX).
Results
During 2012, the Vizient CBD/RM contained data on 3,686,296 patients admitted to 213 hospitals and a total of 33,700 (0.91%) were documented and coded cardiac arrest. (Table 1) Overall survival for all admitted patients was 97.8% (95% confidence interval (CI) 97.7–97.8) as compared to 42.3% (95% confidence interval (CI) 41.8–42.9) for those documented and coded cardiac arrest. Among those with cardiac arrest, survivors were younger and more likely to be male, Caucasian, privately insured, and have hospital stays greater than seven days. Survivors generally had fewer comorbidities compared to non-survivors, with hypertension and obesity the only comorbidities more likely among survivors. (Table 2)
Table 1. Cardiac arrest survival by patient type.
| Number of Visits | Inpatient Survival | |
|---|---|---|
| N (%) | % (95% CI) | |
| All Visits | 3,686,296 | 97.8 (97.7–97.8) |
| Any Cardiac Arrest (Diagnosis or CPR) | 33,700 (0.8) | 42.3 (41.8–42.9) |
| Arrest Diagnosis | 28,954 (0.8) | 44.9 (44.3–45.4) |
| Present on Admission | 12,245 (0.3) | 51.5 (50.7–52.4) |
| Not Present on Admission | 16,971 (0.5) | 39.9 (39.1–40.6) |
| Received CPR | 15,644 (0.4) | 31.4 (30.7–32.1) |
| Arrest Diagnosis and Received CPR | 10,898 (0.3) | 33.4 (32.5–34.3) |
Data from 179 Vizient CDB/RM hospitals in 2012. Excludes hospitals with fewer than 25 eligible cardiac arrest cases. Excluding patients aged <18 years, prisoners, transfers, and hospice patients.
Table 2. Cardiac arrest patient characteristics by inpatient mortality.
| Died | Survived | p | |
|---|---|---|---|
| N (%) | N (%) | ||
| 19,435 | 14,265 | ||
| Age (Years) (Mean; SD)* | 63.8 (17.1) | 61.1 (15.8) | <0.001 |
| Age (Years)* | <0.001 | ||
| 18–40 | 1,993 (10.3) | 1,565 (11.0) | |
| 41–60 | 5,633 (29.0) | 4,939 (34.6) | |
| 61–80 | 8,301 (42.8) | 6,246 (43.8) | |
| 81+ | 3,485 (18.0) | 1,513 (10.6) | |
| Gender** | <0.001 | ||
| Male | 11,254 (57.9) | 8,875 (62.2) | |
| Female | 8,177 (42.1) | 5,390 (37.8) | |
| Race*** | <0.001 | ||
| White/Caucasian | 11,513 (60.8) | 9,330 (66.5) | |
| Black/African American | 4,964 (26.2) | 3,201 (22.8) | |
| Other | 2,472 (13.1) | 1,507 (10.7) | |
| Pay type | <0.001 | ||
| Medicare | 11,811 (60.8) | 7,795 (54.6) | |
| Medicaid | 2,747 (14.1) | 1,941 (13.6) | |
| Private Insurance | 3,027 (15.6) | 3,472 (24.3) | |
| Self-Pay | 1,365 (7.0) | 674 (4.7) | |
| Other | 485 (2.5) | 383 (2.7) | |
| Pay type (among 17,494 aged <65 yrs) | <0.001 | ||
| Medicare | 2,566 (27.1) | 2,022 (25.2) | |
| Medicaid | 2,522 (26.6) | 1,828 (22.8) | |
| Private Insurance | 2,731 (28.8) | 3,202 (39.9) | |
| Self-Pay | 1,244 (13.1) | 634 (7.9) | |
| Other | 410 (4.3) | 335 (4.2) | |
| ICU During Admission† | <0.001 | ||
| Yes | 14,623 (76.6) | 11,342 (80.9) | |
| No | 4,461 (23.4) | 2,677 (19.1) | |
| Length of Stay (days)‡ | <0.001 | ||
| ≤ 2 | 8,047 (42.3) | 1,455 (10.8) | |
| 3–6 | 4,488 (23.6) | 3,261 (24.1) | |
| ≥ 7 | 6,509 (34.2) | 8,812 (65.1) | |
| Weighted Charlson Comorbidity Score | <0.001 | ||
| 0 | 2,693 (13.9) | 2,037 (14.3) | |
| 1 | 3,151 (16.2) | 3,134 (22.0) | |
| ≥ 2 | 13,591 (69.9) | 9,094 (63.8) | |
| Elixhauser Comorbidity Group | |||
| Valvular Disease | 1,650 (8.5) | 855 (6.0) | <0.001 |
| Congestive Heart Failure | 3,816 (19.6) | 2,072 (14.5) | <0.001 |
| Pulmonary Circulation Disease | 1,675 (8.6) | 755 (5.3) | <0.001 |
| Chronic Pulmonary Disease | 4,388 (22.6) | 3,007 (21.1) | 0.002 |
| Hypertension | 10,217 (52.6) | 7,785 (54.6) | <0.001 |
| Diabetes | 6,429 (33.1) | 4,629 (32.5) | 0.147 |
| Renal Failure | 5,714 (29.4) | 3,740 (26.2) | <0.001 |
| Liver Disease | 1,500 (7.7) | 633 (4.4) | <0.001 |
| Metastatic Cancer | 1,038 (5.3) | 261 (1.8) | <0.001 |
| Solid Tumor | 695 (3.6) | 276 (1.9) | <0.001 |
| Coagulopathy | 3,274 (16.9) | 1,350 (9.5) | <0.001 |
| Anemia | 5,156 (26.5) | 3,445 (24.2) | <0.001 |
| Obesity | 2,622 (13.5) | 2,514 (17.6) | <0.001 |
Data from 179 Vizient CDB/RM hospitals in 2012. Excludes hospitals with fewer than 25 eligible cardiac arrest cases.
* 25 missing age.
** 4 missing gender.
*** 713 missing race.
† 597 missing ICU admission.
‡ 1,128 missing length of stay. Excluding those aged <18 years, prisoners, transfers, and hospice patients. P-values from Pearson chi-square tests of association.
Among 179 institutions reporting more than 25 cardiac arrest patients, there was wide regional variation in the number of cardiac arrest cases (Table 3), variation in the hospital volume (median 162; IQR 91–250, Table 4), and observed survival (40.5; 34.6–46.6), and RSSRs (38.2; 34.1–42.5). (Table 5) After adjusting for expected mortality, the intraclass correlation among study hospitals was 0.032 (95% CI 0.024–0.043), suggesting substantial variation in survival across institutions.
Table 3. Cardiac arrest by geographic region.
| Arrest Diagnosis | Received CPR | |
|---|---|---|
| N (%) | N (%) | |
| Census Region | ||
| Northeast (N = 9,074) | 7,822 (86.2) | 4,060 (44.7) |
| Midwest (N = 8,553) | 7,406 (86.6) | 4,305 (50.3) |
| South (N = 11,509) | 9,962 (86.6) | 5,151 (44.8) |
| West (N = 4,564) | 4,026 (88.2) | 2,128 (46.6) |
Data from 179 Vizient CDB/RM hospitals in 2012, including 33,700 discharges with cardiac arrest. Excludes hospitals with fewer than 25 eligible cardiac arrest cases. Excluding patients aged <18 years, prisoners, transfers, and hospice patients. P-value for Arrest Diagnosis = <0.001, CPR = <0.001.
Table 4. Characteristics of Vizient CDB/RM hospitals, 2012.
| Median (IQR) | Min | 10th Pct | 90th Pct | Max | |
|---|---|---|---|---|---|
| Total Patients | 22,869 (12,952–32,892) | 1,817 | 7,942 | 48,325 | 112,379 |
| Cardiac Arrest Cases | 162 (91–250) | 25 | 39 | 369 | 768 |
| Number of Cardiac Arrest Patients Surviving | 66 (29–108) | 6 | 14 | 160 | 364 |
| Observed Cardiac Arrest Survival (%) | 40.5 (34.6–46.6) | 17.1 | 28.0 | 52.3 | 74.1 |
| RSSR (%) | 38.2 (34.1–42.5) | 22.0 | 29.7 | 46.2 | 59.6 |
N = 179 Vizient CDB/RM hospitals. Excludes hospitals with fewer than 25 eligible cardiac arrest cases. Excluding those aged <18 years, prisoners, transfers, and hospice patients. IQR = interquartile range, RSSR = risk-standardized survival rate. RSSRs estimated using Empirical Bayes log odds estimates obtained from a random intercept logistic regression model adjusted for expected mortality. All RSSR estimates were transformed to percentages and are provided for discharges at the average expected mortality value (probability of mortality = 0.24).
Table 5. Institutional characteristics by risk-standardized survival rate performance.
| Hospital Characteristic | RSSR Performance | p | ||
|---|---|---|---|---|
| Average; 29.9–45.7% (N = 131) | Low; 22.0–32.5% (N = 20) | High; 43.3–59.6% (N = 28) | ||
| CA Volume (Median, IQR) | 133 (62–233) | 119 (95–223) | 262 (159–376) | <0.001 |
| CA Volume per 10k Disch (Median, IQR) | 83.8 (65.0–105.5) | 85.2 (71.3–126.1) | 91.1 (78.9–113.4) | 0.19 |
| CA Volume per 10 Beds (Median, IQR) | 3.6 (2.9–4.7) | 3.7 (2.8–4.4) | 4.4 (3.0–5.2) | 0.20 |
| Hospital Control (N, %) | 0.19 | |||
| Government, Non-Federal | 33 (25.2) | 10 (50.0) | 7 (25.0) | |
| Non-Government, Not-for-Profit | 93 (71.0) | 10 (50.0) | 21 (75.0) | |
| Investor-Owned | 5 (3.8) | 0 (0) | 0 (0) | |
| Total Number of Beds (Median, IQR) | 396 (210–596) | 452 (277–559) | 722 (447–839) | <0.001 |
| Services Offered (N, %) | ||||
| Cardiac Catheterization* | 106 (84.8) | 13 (72.2) | 27 (100.0) | 0.03 |
| Cardiac Surgery* | 91 (72.8) | 11 (61.1) | 25 (92.6) | 0.04 |
| Transplant* | 68 (54.4) | 11 (61.1) | 23 (85.2) | 0.01 |
| Neurological* | 121 (96.8) | 18 (100.0) | 27 (100.0) | — |
| Oncology* | 122 (97.6) | 18 (100.0) | 27 (100.0) | — |
| Trauma* | 74 (59.2) | 11 (61.1) | 24 (88.9) | 0.01 |
| Therapeutic Hypothermia | 128 (97.7) | 20 (100.0) | 28 (100.0) | — |
| Annual Number of Surgical Operations (Median, IQR) | 13,954 (7,945–22,184) | 13,109 (9,793–18,611) | 24,939 (16,661–38,661) | <0.001 |
| Hospital Teaching Certification (N, %) | ||||
| ACGME | 97 (74.1) | 16 (80.0) | 25 (89.3) | 0.22† |
| COTH | 79 (60.3) | 14 (70.0) | 25 (89.3) | 0.01 |
| Census Region (N, %) | 0.49† | |||
| Northeast | 36 (27.5) | ** | 11 (39.3) | |
| Midwest | 37 (28.2) | ** | 7 (25.0) | |
| South | 41 (31.3) | 9 (45.0) | 5 (17.9) | |
| West | 17 (13.0) | ** | 5 (17.9) | |
| Population Setting (N, %) | 0.29 | |||
| Large Metropolitan Area | 94 (71.8) | 14 (70.0) | ** | |
| Micro/Small/Med Metropolitan Area | 37 (28.2) | 6 (30.0) | ** | |
| Population Socioeconomic Profile | ||||
| Percentage Medicaid Discharges (Median, IQR)€ | 19.6 (13.7–25.6) | 29.7 (17.5–37.8) | 21.9 (15.8–29.1) | 0.01 |
| Safety Net (Num of Disch) (N, %)€ | 67 (51.5) | 12 (60.0) | 23 (82.1) | 0.01 |
| Safety Net (Perc Medicaid) (N, %)€ | 27 (20.8) | 9 (45.0) | 7 (25.0) | 0.06 |
| HSA Median Household Income (Median, IQR) | 58,363 (50,140–68,476) | 49,104 (45,681–60,516) | 61,922 (58,255–67,414) | 0.02 |
| HSA % in Poverty (Median, IQR) | 15.1 (11.0–17.8) | 17.3 (15.5–22.5) | 14.6 (11.6–17.8) | 0.03 |
N = 179 Vizient CDB/RM hospitals. Excludes hospitals with fewer than 25 eligible cardiac arrest cases. Excluding those aged <18 years, prisoners, transfers, and hospice patients.
* 9 hospitals missing data.
** Suppressed due to count <5.
€ 1 hospital missing data.
P-values from Kruskal-Wallis tests of equal distribution for continuous variables and Pearson Chi-Square tests of association or Fisher’s Exact tests (†) for categorical variables.
RSSR = risk-standardized survival rate; IQR = interquartile range (25th-75th percentiles); COTH = member of Council of Teaching Hospital of the Association of American Medical Colleges; ACGME = residency training approval by Accreditation Council for Graduate Medical Education; HSA = hospital service area.
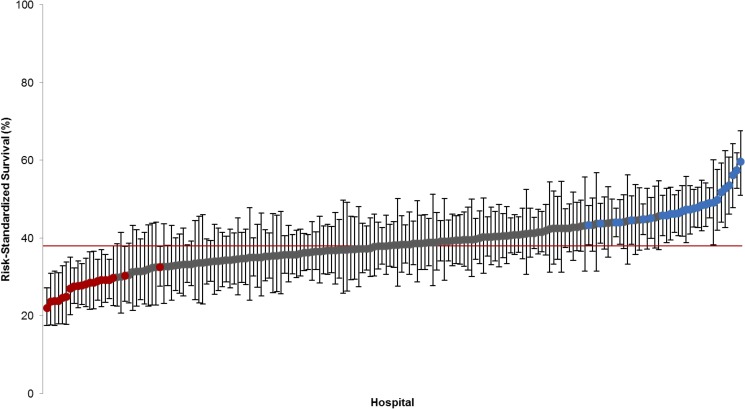
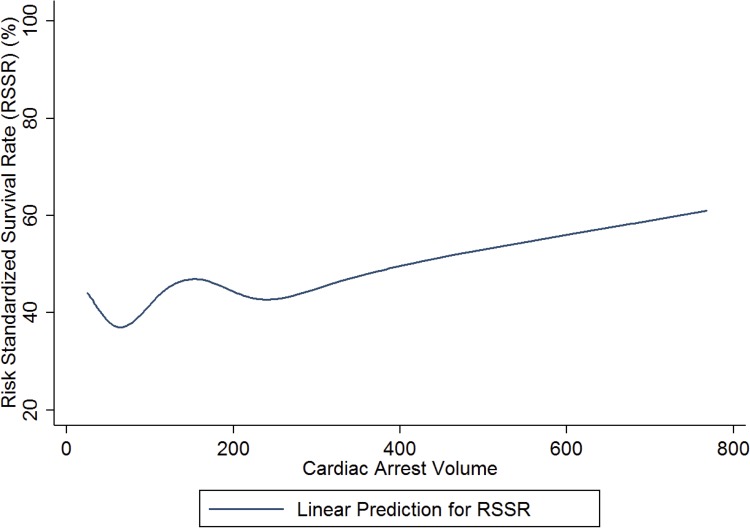
There were 28 hospitals (15.6%) with higher than average survival (median RSSR 47.3%; interquartile range (IQR) 45.4–49.5; Min-Max 43.3–59.6) and 20 hospitals (11.2%) with lower than average survival (median RSSR 28.0%; IQR 24.8–29.2; Min-Max 29.9–45.7). (Fig 1) Compared to hospitals with lower than average cardiac arrest survival, those with high survival had higher cardiac arrest volume, a greater number of beds, higher annual surgical volume, and were more likely to be teaching hospitals and offer cardiac catheterization, cardiac surgery, trauma, and transplant services. (Fig 2) High survival hospitals also had a lower percentage of Medicaid discharges and surrounding HSA catchment areas that consisted of populations with higher median household income and lower percentage living in poverty. (Table 5)
Fig 1. Institutional variation in risk-standardized survival rate.
N = 179 Vizient CDB/RM hospitals. RSSRs estimated using Empirical Bayes log odds estimates obtained from a random intercept logistic regression model adjusted for expected mortality. All RSSR estimates were transformed to percentages and are provided for discharges at the average expected mortality value (probability of mortality = 0.24). Markers indicate hospitals performing significantly worse (Red, N = 20) or better (Blue, N = 28) than the average. Red reference line indicates overall population survival at the average expected mortality (38.0%). Error bars represent 95% confidence interval limits.
Fig 2. Risk standardized survival rate as a function of hospital volume.
N = 179 Vizient CDB/RM hospitals. RSSRs estimated using Empirical Bayes log odds estimates obtained from a random intercept logistic regression model adjusted for expected mortality. All RSSR estimates were transformed to percentages and are provided for discharges at the average expected mortality value (probability of mortality = 0.24). Linear prediction represents the predicted mean RSSR modeled using volume-weighted ordinary least squares regression with restricted cubic splines over values of cardiac arrest volume.
Discussion
In this analysis of hospitals affiliated with academic medical centers, we observed wide variations in cardiac arrest survival, even after accounting for differences in expected mortality. Institutions with higher risk-standardized cardiac arrest survival were larger, had larger cardiac arrest and surgical case volume, higher catchment area socioeconomic status, and greater availability of trauma and cardiac surgery services. Multiple factors support the external validity of these findings. Our analysis is derived from the Vizient CDB/RM, encompassing more than 3.5 million hospital admissions across 179 academic institutions in 2012, or approximately 10% of annual hospital admissions in the United States. Our findings are novel as they represent the most recent observational, risk-adjusted assessment of hospital level operational characteristics that contribute to improved cardiac arrest survival.
The identification of hospital-level factors associated with cardiac arrest outcomes suggests that there may be variation in the care of cardiac arrest patients. For the first time in 2015, the evidenced-based AHA guidelines for emergency cardiac care include recommendations for systems of resuscitation care for cardiac arrest, regardless of location.[6] Some of those criteria, such as the availability of percutaneous coronary intervention (PCI), are supported by our investigation. Our data did not have information to evaluate other guideline recommended response elements such as appropriate institutional surveillance (i.e. early warning system), dedicated in-hospital response, (i.e. rapid response team), and availability of a comprehensive, post cardiac arrest service.
Our results support previous epidemiological studies suggesting higher cardiac arrest survival among large, teaching institutions [4] [5] that care for high cardiac arrest volume. [15] The association between case volume and outcome has previously been demonstrated in other critical illnesses such as stroke,[16] trauma,[17] and myocardial infarction[18] where quality treatment is similarly time-dependent. However, unlike these previous studies, our analysis demonstrated specific hospital offerings, for example, cardiac catheterization and cardiac surgery, and higher annual surgery volume were associated with higher than average survival. While previous meta-analysis has demonstrated an association between cardiac arrest survival and PCI, [19] the characteristics identified by our results suggest that these hospital offerings may serve as surrogates for a concentration of expertise in caring for the critically ill.
A number of experts have drawn a clear association between lower socioeconomic status, predominately minority, neighborhoods and survival from cardiac arrest. [20] Previously those associations have been linked to pre-hospital factors such as 9-1-1 access and bystander CPR rates. [21] While such pre-hospital factors clearly impact survival to hospital discharge from cardiac arrest, our investigation is novel in that it demonstrates an association between the socioeconomic status of the hospital catchment area and cardiac arrest outcomes. These findings suggest that some portion of the geographic variation in survival from cardiac arrest may reflect characteristics of the institutional referral base in addition to the quality of the treatment delivered or the systems of care employed.
Our investigation in academic center-affiliated hospitals identified wide variation in cardiac arrest survival. While such variation in survival has previously been demonstrated, [4] our investigation quantified a three-fold difference in survival between best and weakest performing study hospitals suggesting opportunities to improve cardiac arrest care. Further research should be directed to exploring causes for the institutional variations we observed and clarifying the role of the institutional factors in cardiac arrest survival performance. If survival can be causally linked to hospital characteristics, then mechanisms for developing systems of care to reduce geographic variation and optimize care for all victims of cardiac arrest are achievable.
Limitations
Our observations derive from data submitted by hospitals affiliated with academic medical centers, some of which have mature systems of care to maximize cardiac arrest outcomes. As such, survival rates may differ for non-academic centers. We excluded transfers from outside hospitals, as the reason for transfer could not be determined from the data, and therefore this “non-native” population could have impacted the associations identified between risk factors and survival.
The greatest limitation of this investigation arises from the use of discharge diagnoses for case-definition and outcome measures. Reliance on such administrative classification assumes concordance between medical coding technicians and treating clinicians. While this strategy may lead to significant under-classification as suggested by Coppler et. al.,[22] it has been used in previous epidemiologic studies examining cardiac arrest [4] [11] and other complex conditions. [23] [24] Furthermore, our analysis is strengthened by the novel use of the ICD-9 procedure code for CPR (ICD-9: 99.60) as inclusion criteria, which yielded 4,746 (16.4%) additional subjects.
We did not have access to initial cardiac rhythm, timing of defibrillation (when appropriate), duration and quality of CPR, or other Utstein factors previously demonstrated to impact survival. [25] While the Vizient CDB/RM risk models provide a comprehensive strategy for risk adjustment, our estimated RSSRs did not reflect traditionally collected Utstein factors that may provide improved model discrimination. In addition, these data do not allow for further description of neurologic status upon discharge, a more meaningful qualifier of treatment success beyond mere survival.
Conclusion
Among study cohort hospitals, there was wide variation in cardiac arrest survival and institutions with higher cardiac arrest and surgical case volume, availability of catheterization and cardiac surgery services, and higher catchment area socioeconomic status demonstrated higher risk-standardized survival. Further efforts should seek to examine these observations in greater detail and identify specific strategies for improving outcomes among hospitals with low cardiac arrest survival.
Data Availability
The data originating from the Vizient Clinical Database are third party data and cannot be made publicly available. Applications for Vizient data, including data to recreate this analysis, can be requested through participating institutions or by contacting Samuel F. Hohmann, PhD, Research Analytics Director, Center for Advanced Analytics, Vizient Incorporation, at Sam.Hohmann@vizientinc.com. The URL outlining this Vizient policy appears at https://www.vizientinc.com/What-we-do/Patient-Impact/Clinical-analytics-and-benchmarking. Annual survey data from the American Hospital Association (AHA) are also third party data and may accessed with permission of the AHA. Interested researchers may purchase these data here: http://www.ahadata.com/. Data from the United States Government American Community Survey (ACS) are freely available through the National Historical Geographic Information System (NHGIS) at https://www.nhgis.org/. The authors confirm that interested researchers may apply for access or purchase these data in the manner described.
Funding Statement
Mr. Donnelly’s effort was supported by grant T32-HS013852 from the Agency for Healthcare Research and Quality, Rockville, Maryland.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ballew KA, Philbrick JT, Caven DE, Schorling JB. Predictors of survival following in-hospital cardiopulmonary resuscitation. A moving target. Archives of internal medicine. 1994;154(21):2426–32. [PubMed] [Google Scholar]
- 3.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. [DOI] [PubMed] [Google Scholar]
- 4.Carr BG, Goyal M, Band RA, Gaieski DF, Abella BS, Merchant RM, et al. A national analysis of the relationship between hospital factors and post-cardiac arrest mortality. Intensive Care Med. 2009;35(3):505–11. doi: 10.1007/s00134-008-1335-x [DOI] [PubMed] [Google Scholar]
- 5.Girotra S, Cram P, Spertus JA, Nallamothu BK, Li Y, Jones PG, et al. Hospital variation in survival trends for in-hospital cardiac arrest. J Am Heart Assoc. 2014;3(3):e000871 PubMed Central PMCID: PMCPMC4309112. doi: 10.1161/JAHA.114.000871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kronick SL, Kurz MC, Lin S, Edelson DP, Berg RA, Billi JE, et al. Part 4: Systems of Care and Continuous Quality Improvement: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S397–413. [DOI] [PubMed] [Google Scholar]
- 7.Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PW Jr., et al. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation. 2013;127(14):1538–63. doi: 10.1161/CIR.0b013e31828b2770 [DOI] [PubMed] [Google Scholar]
- 8.Association AH. AHA annual survey database™ fiscal year 2012. 2012.
- 9.System NHGI. American Community Survey, 2008–2012 American Community Survey 5 Year Estimates. 2008–2012
- 10.International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)
- 11.Fugate JE, Brinjikji W, Mandrekar JN, Cloft HJ, White RD, Wijdicks EF, et al. Post-cardiac arrest mortality is declining: a study of the US National Inpatient Sample 2001 to 2009. Circulation. 2012;126(5):546–50. doi: 10.1161/CIRCULATIONAHA.111.088807 [DOI] [PubMed] [Google Scholar]
- 12.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 13.Sutton JM, Hayes AJ, Wilson GC, Quillin RC 3rd, Wima K, Hohmann S, et al. Validation of the University HealthSystem Consortium administrative dataset: concordance and discordance with patient-level institutional data. J Surg Res. 2014;190(2):484–90. doi: 10.1016/j.jss.2014.03.044 [DOI] [PubMed] [Google Scholar]
- 14.Dimick JB, Staiger DO, Birkmeyer JD. Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res. 2010;45(6 Pt 1):1614–29. PubMed Central PMCID: PMCPMC2976775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80(1):30–4. doi: 10.1016/j.resuscitation.2008.09.001 [DOI] [PubMed] [Google Scholar]
- 16.Saposnik G, Hill MD, O'Donnell M, Fang J, Hachinski V, Kapral MK, et al. Variables associated with 7-day, 30-day, and 1-year fatality after ischemic stroke. Stroke. 2008;39(8):2318–24. doi: 10.1161/STROKEAHA.107.510362 [DOI] [PubMed] [Google Scholar]
- 17.Nathens AB, Jurkovich GJ, Maier RV, Grossman DC, MacKenzie EJ, Moore M, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285(9):1164–71. [DOI] [PubMed] [Google Scholar]
- 18.Canto JG, Every NR, Magid DJ, Rogers WJ, Malmgren JA, Frederick PD, et al. The volume of primary angioplasty procedures and survival after acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. N Engl J Med. 2000;342(21):1573–80. doi: 10.1056/NEJM200005253422106 [DOI] [PubMed] [Google Scholar]
- 19.Camuglia AC, Randhawa VK, Lavi S, Walters DL. Cardiac catheterization is associated with superior outcomes for survivors of out of hospital cardiac arrest: review and meta-analysis. Resuscitation. 2014;85(11):1533–40. doi: 10.1016/j.resuscitation.2014.08.025 [DOI] [PubMed] [Google Scholar]
- 20.Vaillancourt C, Lui A, De Maio VJ, Wells GA, Stiell IG. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79(3):417–23. doi: 10.1016/j.resuscitation.2008.07.012 [DOI] [PubMed] [Google Scholar]
- 21.Sasson C, Magid DJ, Chan P, Root ED, McNally BF, Kellermann AL, et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367(17):1607–15. PubMed Central PMCID: PMCPMC3515681. doi: 10.1056/NEJMoa1110700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coppler PJ, Rittenberger JC, Wallace DJ, Callaway CW, Elmer J, Pittsburgh Post Cardiac Arrest S. Billing diagnoses do not accurately identify out-of-hospital cardiac arrest patients: An analysis of a regional healthcare system. Resuscitation. 2016;98:9–14. PubMed Central PMCID: PMCPMC4715911. doi: 10.1016/j.resuscitation.2015.09.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang HE, Addis DR, Donnelly JP, Shapiro NI, Griffin RL, Safford MM, et al. Discharge diagnoses versus medical record review in the identification of community-acquired sepsis. Crit Care. 2015;19:42 PubMed Central PMCID: PMCPMC4340494. doi: 10.1186/s13054-015-0771-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang HE, Donnelly JP, Shapiro NI, Hohmann SF, Levitan EB. Hospital variations in severe sepsis mortality. Am J Med Qual. 2015;30(4):328–36. doi: 10.1177/1062860614534461 [DOI] [PubMed] [Google Scholar]
- 25.Cummins RO, Chamberlain D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital 'Utstein style'. American Heart Association. Circulation. 1997;95(8):2213–39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data originating from the Vizient Clinical Database are third party data and cannot be made publicly available. Applications for Vizient data, including data to recreate this analysis, can be requested through participating institutions or by contacting Samuel F. Hohmann, PhD, Research Analytics Director, Center for Advanced Analytics, Vizient Incorporation, at Sam.Hohmann@vizientinc.com. The URL outlining this Vizient policy appears at https://www.vizientinc.com/What-we-do/Patient-Impact/Clinical-analytics-and-benchmarking. Annual survey data from the American Hospital Association (AHA) are also third party data and may accessed with permission of the AHA. Interested researchers may purchase these data here: http://www.ahadata.com/. Data from the United States Government American Community Survey (ACS) are freely available through the National Historical Geographic Information System (NHGIS) at https://www.nhgis.org/. The authors confirm that interested researchers may apply for access or purchase these data in the manner described.