Abstract
Superior mesenteric artery syndrome was observed in an adolescent patient. He had a 1-day history of nausea, vomiting, and abdominal pain, without chronic or recurrent symptoms. Diagnosis was established by abdominal plain x-ray, contrast enhanced abdominal computed tomography, and endoscopic examination. The patient was hospitalized, monitorized, and decompressed by nasogastric tube without oral feeding. The symptoms of the patient were gradually relieved by conservative treatment and he was discharged after one week. Clinicians should be careful when facing upper gastrointestinal symptoms that are resistant and non-responsive to treatment, and this syndrome should be kept in mind. This case is presented to draw attention to this disease because of its rare incidence.
1. Introduction
Superior mesenteric artery (SMA) syndrome is a rare cause of upper gastrointestinal obstruction. The defining feature of this syndrome is the compression of the third part of the duodenum between the SMA anteriorly and the aorta posteriorly leading to upper gastrointestinal obstruction. Marked weight loss, external compression of the abdomen, anatomic variation, and surgical alterations of anatomy have been described as causative factors in SMA syndrome.1 The most characteristic symptoms of SMA are post-prandial epigastric fullness with pain, eructation, and bilious vomiting. Acute gastric dilation, which is rarely seen, may result in several complications like dehydration, metabolic alkalosis, gastric necrosis and systemic circulatory failure.2 We think that this disease may be neglected by pediatricians because of the rare incidence among children. In this report; an adolescent boy with SMA syndrome showed gastric dilatation without any previous history and was treated conservatively to draw attention to this disease.
2. Case Presentation
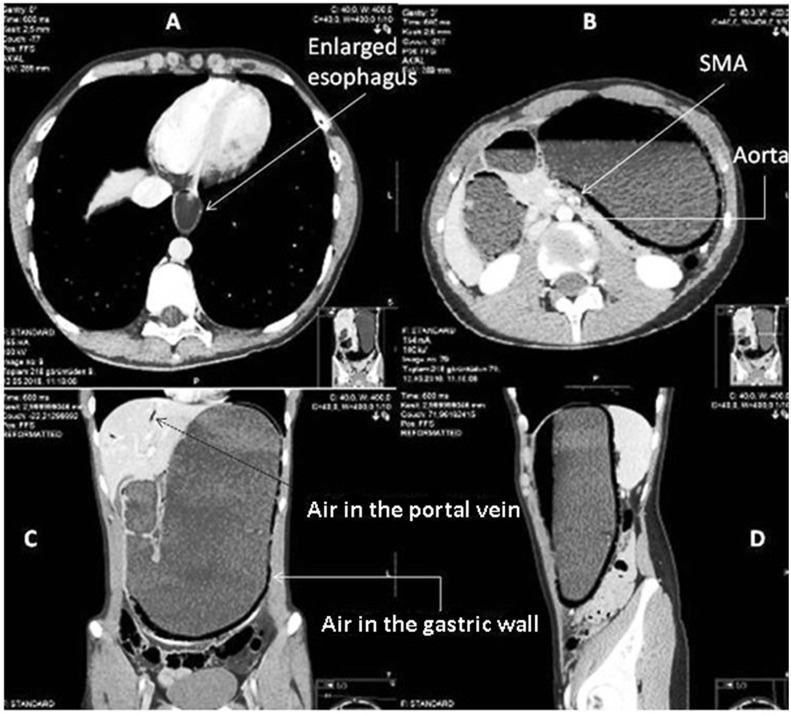
A 17-years-old boy was brought to our emergency department with complaints of vomiting and abdominal pain for the last 14 hours. He vomited almost 20 times during the day, he also had upper abdominal pain, which was gradually getting worse. He was moderately dehydrated, alert, normotensive (110/60 mmHg), and other vital signs were normal. His body weight and height were 55 kg and 185 cm, respectively. Although he had epigastric pain, other abdominal signs were normal; there were no signs of acute abdomen. Because he had moderate dehydration and persistent vomiting, intravenous fluid with isotonic saline, intravenous ondansetron and intravenous ranitidine were administered. After being consulted to the Pediatric Emergency Department, he was hospitalized. White blood cell count (7820/mm3), blood biochemistry including total amylase (57 U/L), CRP (0.4 mg/L, normal: <2.4 mg/L), and urinalysis were in normal ranges. Abdominal X-ray revealed a distended stomach reaching the spina iliaca level, and the walls of the stomach and duodenal bulb were widened with air-fluid levels in it. The presence of two air-fluid levels in the right upper quadrant was suggesting an obstruction in the stomach outflow and/or proximal duodenum (Fig. 1). An abdominal computed tomography (CT) revealed the dilatation of distal esophagus, a prominent distention of the stomach that reaches the pelvis, a dilatation of the first three portions of duodenum –widest part 6 cm-, an obstructed third duodenal portion between SMA and abdominal aorta. Contrast enhanced CT revealed the presence of intramural air in the wall of the stomach and portal vein (Fig. 2). The contrast study of upper gastrointestinal tract revealed the retarded transition of contrast from duodenum to jejunum on supine position and accelerated transition on prone position. The contrast was passed to jejunum in prone position. These clinical and radiological findings were compatible with SMA syndrome. The patient was treated conservatively with nasogastric (NG) decompression and intravenous hydration plus total parenteral nutrition without oral drinking and feeding. On the first day, 1100 ml gastric fluid was drained from the NG tube, 900 ml on the second day and 300 ml on the third day. The color of fluid was brown-dark green. His upper gastrointestinal endoscopic examination was performed on the fourth day; lower esophageal sphincter was seen loose on retroflexion, the large curvature was intensely hyperemic with many large ulcers, and the whole stomach seemed to be edematous. The duodenal bulb and distal parts of duodenum seemed normal, no ulcers or nodularity were noticed. The pathological evaluation revealed chronic superficial gastritis and foveolar hyperplasia. Ischemic finding, atrophy, intestinal metaplasia, lymphoid aggregates, and Helicobacter pylori were not detected by endoscopy.
Fig. 1.
Abdominal X-ray revealed a distended stomach reaching the iliac level, and the walls of stomach and duodenal bulb were widened with air-fluid levels. Linear portal venous gas images were remarked by an arrow in the hepatic region.
Fig. 2.
The abdominal CT revealed a dilatation of distal esophagus (A: First axial section), prominent distention of stomach that reaches the pelvis (D: Sagittal section), dilatation of the first three portions of duodenum (C: Coronal section), an obstructed third duodenal portion between SMA and abdominal aorta (B: Second axial section). The contrast enhanced CT revealed the presence of intramural air in the wall of stomach and portal vein (B, C, and D).
His clinical status gradually improved without hemodynamic deterioration. The first defecation was seen on the fifth day of hospitalization. NG decompression was discontinued after there was no drainage by NG tube, and oral nutrition was started on the sixth day. His control contrast enhanced abdominal CT was performed 6 days after the first one. There was a regression in the presence of air in the portal system and also a significant reduction in massive dilatation of stomach and duodenum. According to these results and his clinical condition, the patient was discharged from the hospital on the 7th day with PPI and sucralfate. On his follow-up, he was found to be asymptomatic three weeks later, he had normal physical examination findings except his low body weight and low body mass index according to his age (56.5 kg, 185 cm, BMI: 16.5). He had put on 1,5 kg after discharge. He was suggested to continue omeprazole treatment and a control endoscopy was planned.
3. Discussion
In SMA syndrome, the third portion of duodenum becomes tightly compressed between the SMA and the abdominal aorta. Normally, the presence of fat and lymphatic tissues around the SMA provides protection to the duodenum against compression. The protection of SMA is diminished among cachectic patients who have decreased fatty tissue around SMA resulting in angulation and reduction in the distance between the aorta and the SMA.[3], [4], [5] His weight was 3% percentile and height was 90–97% percentile. There was not sudden weight loss in his past medical history. His mother said that he has always been asthenic. The correlation between low fat tissue of our patient and this diagnosis was considered to be etiologically significant.
The leading causes of vomiting during childhood are acute viral gastroenteritis, food poisoning and gastritis.[6], [7] Anti-emetic therapy and rehydration usually respond rapidly and well to vomiting in these diseases. In cases which do not respond to these medications, uncommon diseases including gastric pathologies, intestinal obstruction at any level of the gastrointestinal tract or acute pancreatitis usually come to mind. Acute and recurrent vomiting which is resistant to antiemetic and gastric drugs, plus upper abdominal pain and dehydration may be the signs of SMA. Emergency physicians should not overlook this diagnosis.
Acute gastric dilatation due to obstruction raises intragastric pressure and causes gastric wall shear stress resulting in gastric vascular insufficiency.8 The gastric circulatory deterioration causes fragility of the gastric wall, possible tears resulting in mucosal necrosis pose life-threatening complications such as dehydration, and metabolic alkalosis.[5], [9] Although the presented case had severe gastric dilatation extending into the pelvis, there was no vascular collapse and shock. The patient remained stable hemodynamically during hospitalization.
Treatment consisted of conservative measures such as NG decompression and hyperalimentation followed by oral feeding with frequent small meals. If conservative treatment fails, surgical treatment may be considered.10 Requirement of surgical treatment in particularly chronic cases is reported in literature.10 Both clinical and radiological findings significantly improved after NG decompression in the presented patient. Our patient benefited from a conservative approach and did not need surgical treatment.
In conclusion, although vomiting and abdominal pain are frequently seen in minor gastrointestinal diseases including acute gastroenteritis or viral syndrome, less commonly seen diseases such as SMA syndrome should be remembered among patients resistant to medical therapy. In other words, SMA syndrome may present with acute symptoms, which may be misdiagnosed as gastroenteritis. Acute gastric dilatation is a life-threatening condition which must be immediately interfered with and treated.
Acknowledgements
We are grateful to Hakan Şentürk (writing consultant at the Writing Center) for the English revision of this report.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
References
- 1.Su M.C., Lee C.H., Wang C.C. Education and imaging. Gastrointestinal: superior mesenteric artery syndrome initially presenting like reflux esophagitis. J Gastroenterol Hepatol. 2010;25:645. doi: 10.1111/j.1440-1746.2010.06259.x. [DOI] [PubMed] [Google Scholar]
- 2.Cogbill T.H., Bintz M., Johnson J.A., Strutt P.J. Acute gastric dilatation after trauma. J Trauma. 1987;27:1113–1117. doi: 10.1097/00005373-198710000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Singal R., Sahu P.K., Goyal S.L. Superior mesenteric artery syndrome: a case report. North Am J Med Sci. 2010;2:392–394. doi: 10.4297/najms.2010.2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roy A., Gisel J.J., Roy V., Bouras E.P. Superior mesenteric artery (Wilkie's) syndrome as a result of cardiac cachexia. J Gen Intern Med. 2005;20:3–4. doi: 10.1111/j.1525-1497.2005.0201.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdu R.A., Garritano D., Culver O. Acute gastric necrosis in anorexia nervosa and bulimia. Two case reports. Arch Surg. 1987;122:830–832. doi: 10.1001/archsurg.1987.01400190096021. [DOI] [PubMed] [Google Scholar]
- 6.Pickering L.K., Snyder J.D. Gastroenteritis. In: Berhman R.E., Kliegman R.M., Jenson H.B., editors. Nelson's textbook of pediatrics. seventeenth ed. Saunders; Philadelphia, PA: 2004. pp. 1272–1276. [Google Scholar]
- 7.McCollough M., Sharieff G.Q. Abdominal pain in children. Pediatr Clin North Am. 2006;53:109–113. doi: 10.1016/j.pcl.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Todd S.R., Marshall G.T., Tyroch A.H. Acute gastric dilatation revisited. Am Surg. 2000;66:709–710. [PubMed] [Google Scholar]
- 9.Hiroaki S., Toshiko T. Acute gastric dilatation due to superior mesenteric artery syndrome: an autopsy case. BMC Gastroenterol. 2014;14:37. doi: 10.1186/1471-230X-14-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merrett N.D., Wilson R.B., Cosman P., Biankin A.V. Superior mesenteric artery syndrome: diagnosis and treatment strategies. J Gastrointest Surg. 2009;13:287–292. doi: 10.1007/s11605-008-0695-4. [DOI] [PubMed] [Google Scholar]