ABSTRACT
Bee stings can cause severe reactions and have caused many victims in the last years. Allergic reactions can be triggered by a single sting and the greater the number of stings, the worse the prognosis. The poisoning effects can be systemic and can eventually cause death. The poison components are melitin, apamin, peptide 401, phospholipase A2, hyaluronidase, histamine, dopamine, and norepinephrine, with melitin being the main lethal component. Acute kidney injury (AKI) can be observed in patients suffering from bee stings and this is due to multiple factors, such as intravascular hemolysis, rhabdomyolysis, hypotension and direct toxicity of the venom components to the renal tubules. Arterial hypotension plays an important role in this type of AKI, leading to ischemic renal lesion. The most commonly identified biopsy finding in these cases is acute tubular necrosis, which can occur due to both, ischemic injury and the nephrotoxicity of venom components. Hemolysis and rhabdomyolysis reported in many cases in the literature, were demonstrated by elevated serum levels of indirect bilirubin and creatine kinase. The severity of AKI seems to be associated with the number of stings, since creatinine levels were higher, in most cases, when there were more than 1,000 stings. The aim of this study is to present an updated review of AKI associated with bee stings, including the currently advised clinical approach.
Keywords: Bee stings, Hymenoptera, Complications, Acute kidney injury
INTRODUCTION
The order Hymenoptera represents a large group of arthropods whose venom is in general, well tolerated. In most cases, the sting causes erythema, edema and local pain. However, the sting may trigger immediate allergic reactions mediated by immunoglobulin E (IgE), with urticaria, angioedema, respiratory symptoms (dyspnea or asthma) and cardiovascular symptoms (hypotension and anaphylactic shock)1.
Africanized bees have their origin in Brazil after the accidental crossing between the African species Apis mellifera scutellata and the European species Apis mellifera lingustica during the 1950s2,3. They are characterized by their aggressiveness and their violent mass attacks3,4,5.
The allergic reaction can be triggered by a single sting, and the greater the number of stings, the worse the prognosis because multiple stings lead to inoculation of a higher amount of venom5. Insect venom of the Hymenoptera order (bees and wasps) is responsible for 14% of the cases of anaphylactic reactions, constituting the second place among the causes, second only to food antigens (33 to 34%)1.
The effects of the poison can be systemic and can eventually cause death6. Mortality rates for multiple bee stings were approximately 15-25% in previously published studies. The poison components are melitin, apamin, peptide 401, phospholipase A2, hyaluronidase, histamine, dopamine, and norepinephrine, with melitin being the main lethal component2,6. Allergic manifestations due to bee stings are well known and yet most incidents continue to be underreported in Brazil5. This fact is of concern, since other less usual manifestations, such as intravenous hemolysis, rhabdomyolysis, thrombocytopenia, acute kidney injury, hepatic aggression and myocardial infarction may be life threatening. Africanized bees have spread across the Americas, reaching as far as the Southern region of the United States (Texas, New Mexico, Arizona, and California). Currently, the number of cases of acute kidney injury due to bee stings in the American continent is up to six times greater than in other continents5.
Acute kidney injury (AKI) is determined by impaired renal function over a period of hours and, subsequently, by renal failure, thus leading to the accumulation of nitrogen products and electrolyte imbalance. In cases of bee venom inoculation a direct toxic effect on renal function has been observed3. However, the mechanism through which renal damage occurs is not fully understood. It is believed that shock, rhabdomyolysis, hemolysis and direct tubular nephrotoxicity play an important role in this aspect6.
BEE VENOM CHARACTERISTICS
Bee venom is a complex mixture of proteins, peptides and low molecular-weight components with a higher percentage of proteins and peptides. Among the proteins, phospholipase A2 and hyaluronidase enzymes are the main ones. Melitin is the main peptide and is the main component of bee venom, and apamin is also present, as well as phospholipids, some histamine and myoglobin, epinephrine, norepinephrine, aminobutyric acid, alpha-amino acids, glucose, fructose, complex ethers, phosphorus, calcium, and magnesium2,6,7,8.
Bee venom has medicinal properties and is used worldwide against several disorders and diseases. The venom components act on vascular resistance, thereby altering blood pressure and activating the immune system7.
Phospholipase A2 is the major allergen and melitin is the most abundant substance of venom composition. Both are neuromuscular blocking agents, which can cause respiratory paralysis. Additionally, they are potential causes of hemolysis and rhabdomyolysis due to the membrane destruction action. Melitin promotes the release of catecholamines and has depressive and cardiotoxic effects9. Melitin in large quantities causes cardiac spasm and cardiovascular collapse, which is the cause of death in envenomation accidents caused by multiple bee stings. Apamin acts as a neurotoxin with a motor action, causing systemic vasodilation, generating severe hypotension and increased heart rate. The set of functions of the venom components generates a systemic hypoperfusion and, therefore, it decreases renal blood flow, which can predispose to AKI.
PHYSIOPATHOLOGY OF KIDNEY INJURY
Africanized bees are usually identified as insects responsible for nephrotoxic acute tubular necrosis, as they attack in clusters. Acute kidney injury can be observed in patients suffering from bee stings and this is due to multiple factors, such as intravascular hemolysis, rhabdomyolysis, hypotension, and direct toxicity of the venom components to the renal tubules1,2. Arterial hypotension plays an important role in this type of AKI, leading to ischemic renal lesion10.
Bee venom, which has as its main components hyaluronidase, phospholipase A2, melitin and apamin, contributes to renal damage due to synergistic toxic and hypotensive effects1,11. Moreover, these substances can induce the release of several other mediators, such as histamine, serotonin, bradykinin and prostaglandin. These substances are vasoactive and may lead to a reduction in systemic blood pressure1,12. A reduction in the norepinephrine content was observed in rats inoculated with bee venom, suggesting a great release of this mediator13. In cardiac tissue, this can cause ischemic lesions and acute myocardial infarction, reducing the cardiac output and, consequently, leading to a reduction in renal blood flow14. Due to renal hypoperfusion, the renin-angiotensin-aldosterone system activation and increase in the adrenergic neural stimulus occurs, with catecholamine secretion. All these factors induce vasoconstriction of afferent and efferent arterioles, with reduced glomerular and peritubular blood flow, leading to ischemia and the development of acute tubular necrosis10,15. The most commonly identified biopsy finding in these cases is acute tubular necrosis, which can occur both due to ischemic injury and nephrotoxicity of venom components15,16
Hemolysis and rhabdomyolysis were observed in many cases reported in the literature, demonstrated by elevated serum levels of indirect bilirubin and creatine kinase (CK)17-22. The presence of myoglobin and muscle actin in cylinders formed in the renal tubules of rats submitted to the inoculation of Africanized bee venom was detected through immunohistochemistry23.
Microscopic examination of muscles demonstrated the presence of rhabdomyonecrosis associated with a diffuse inflammatory process and vascular congestion3. The association between rhabdomyolysis and AKI is well known and has been described in the literature19,23,24. The main mechanisms involved in AKI caused by rhabdomyolysis are renal vasoconstriction, formation of intratubular deposits of myoglobin and direct cytotoxicity of myoglobin to the renal tubule cell4,23,24,25.
Renal vasoconstriction is due to hypovolemia and heme protein binding to nitric oxide (endothelial relaxing factor). Dehydration, decreased urinary pH and flow, and the presence of the Tamm-Horsfall protein (THP) contribute to the formation of myoglobin cylinders in the renal tubules25. The direct cytotoxicity of myoglobin to the renal tubule cell occurs through the heme portion, which induces the production of free radicals causing lipid peroxidation and cell damage. Another factor that contributes to renal impairment is the possible occurrence of disseminated intravascular coagulation, described in rhabdomyolysis. This phenomenon leads to the release of thromboplastin, causing the formation of micro thrombi in the glomeruli, with the consequent glomerular filtration rate reduction25.
In an experimental study in AKI induced by bee venom toxins, performed by Reis et al.10, no changes were observed in the glomeruli, interstitium or renal vessels. Only the occurrence of acute tubular necrosis with formation of intratubular pigment deposits was verified3. The proximal tubules and the large ascending branch of the Henle loop were dilated, with brush border attenuation, loss of epithelial integrity and cell desquamation. Large mitotic figures were observed in tubular cells, especially in the cortical region10.
Evidence from clinical and experimental studies showed that some bee venom toxins can directly injure renal tubules10,13,16,20,21,22. It was observed that the proximal portion of renal tubules is more susceptible to the toxic effects of bee venom, and this is due to the great reabsorption of toxic substances at this site, associated to intense metabolic activity, with energy expenditure and vulnerability of the enzymatic system10.
A study carried out by França et al.20 observed the presence of venom and phospholipase A2 in the plasma and urine of patients who had been stung by bees through immune enzyme techniques, demonstrating renal excretion of these substances, contributing to direct toxic effects of bee venom on the kidneys. Phospholipase A2 was detected in serum and urine of five patients that had been victims of multiple bee stings20. The substance has been detected for more than 50 hours after the accidents in two cases, and the amount of circulating venom was estimated at 27 mg, one hour after the stings20.
Sodium and potassium excretion fractions were increased suggesting the involvement of proximal nephron portions and distal tubule preservation13. The above-mentioned studies suggest that the venom of Africanized bees is freely filtered by the renal glomeruli and is reabsorbed mainly by the proximal tubules.
It was also observed, in an experimental study, that bee venom decreases the transport of water through the collecting ducts13. This reduction is probably due to the large release of prostaglandins from mast cells and the phospholipid metabolism of the damaged cells, which interfere with the action of ADH in the collecting tubule cells13. The occurrence of proteinuria has been described in some clinical studies, with the development of nephrotic syndrome after bee sting accidents26-31.
In cases of patients with pre-existing minimal alteration, it was observed that many of these patients show an increase in IgE and IL-13 levels after exposure to the venom. IL-13 may favor the production of IgE over IgM by B cells and induce CD80 expression by podocytes. This change may be responsible for the development of proteinuria and increased levels of IgE3. Another study in rats showed that CD80 induction by podocytes results in proteinuria with fusion of glomerular podocyte extensions. Additionally, urinary CD80 levels increased in patients with dilated cardiomyopathy (DCM) during recurrence and it returned to normal after remission. Consequently, recent studies suggest that IL-13 can mediate proteinuria in patients with DCM because of their ability to directly induce CD80 expression in podocytes31.
In a recently published case, glomerulonephritis was observed, with increment of IgE levels and serum complement reduction26. In cases in which a renal biopsy was performed, there were non-specific changes and presence of podocyte fusion27,30.
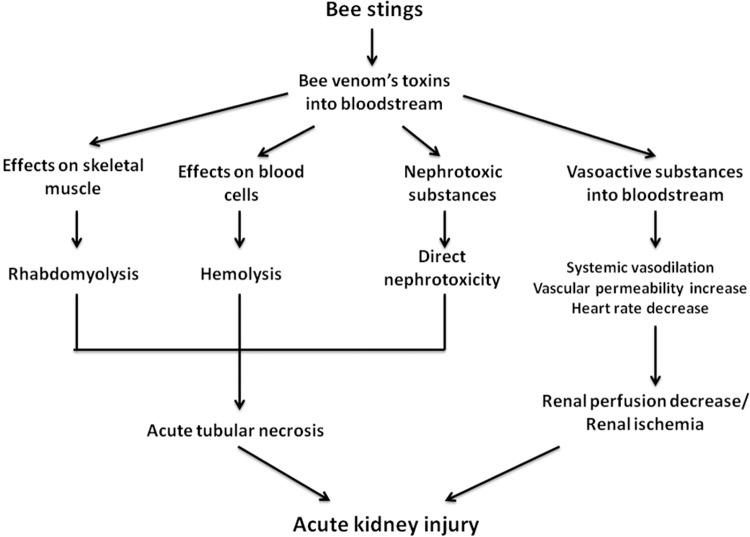
The pathophysiology of AKI induced by bee stings is shown in Figure 1.
Figure 1. Pathophysiology of AKI induced by bee stings.
CLINICAL CHARACTERISTICS AND LABORATORY ABNORMALITIES
A common complication in bee sting accidents is acute kidney injury (AKI). The onset of the first manifestations of this complication occurs 24 to 48 hours after the accident, and it is due to the great amount of inoculated poison. Other manifestations that may occur are oligo-anuria, macroscopic hematuria and other changes in the urine analysis. Other signs and symptoms resulting from the toxic effects of bee venom are nausea, vomiting, hyperventilation (acid breathing), generalized edema, myalgia, arthralgia, headache, restlessness and consciousness alteration. At the time of hospital admission some patients present stupor, a semi-comatose status, often suffering from severe respiratory failure3-6,10,11,15,16,18. The severity of AKI seems to be associated with the number of stings, since creatinine levels were higher, in most cases, when there were more than 1,000 stings3-5.
Changes in the urine analysis include reduction in urinary density, proteinuria, hemoglobinuria, hematuria, leukocyturia and hemoglobin or myoglobin pigment cylinders. The value of the sodium excretion fraction is commonly elevated, showing a picture of predominantly renal AKI15. Some patients may present thrombocytopenia, which could be due to the alterations caused by the toxins in the vascular endothelium or by more severe complications such as disseminated intravascular coagulation. Reduction in hemoglobin levels can also be found and can be explained by the occurrence of hemolysis caused once more by the action of the bee venom components phospholipase A2 and melitin.
Hyperkalemia (K+ > 5 mEq/L), metabolic acidosis can occur in these patients. Evidence of rhabdomyolysis and hemolysis has been detected with increased serum creatine kinase (CK) levels ranging from 588 to 91,000 IU/L, aspartate aminotransferase (AST) from 106 to 2,085 IU/L and lactate dehydrogenase (LDH) from 614 to 85,000 UI/L.
We have recently seen a patient admitted to the emergency room with severe AKI and rhabdomyolysis following multiple bee stings, presenting anasarca and disseminated erythematous-crusty lesions (Figures 2 and 3). Laboratory tests evidenced creatine kinase 74,331 IU/L, creatinine 5.1 mg/dL and urea 156 mg/dL, and hemodialysis was required. After an intensive care, he presented a complete recovery of the renal function and resolution of clinical manifestations (Figure 4).
Figure 2. Facial edema in a 26-year-old man victim of multiple honeybee stings in Macapá, Amapá, Brazil (authors’ archive).
Figure 3. Lower limb edema in a 26-year-old man victim of multiple honeybee stings in Macapá, Amapá, Brazil (authors’ archive).
Figure 4. A 26-year-old man victim of multiple honeybee stings in Macapá, Amapá, Brazil, after intensive care support, at the time of hospital discharge, showing no facial or lower limb edema.
Prognosis is usually good in patients who survive, and full renal function recovery occurs in most cases, and the required time for renal function recovery ranges from 4 to 120 days.
Other complications due to bee stings include acute myocardial infarction32,33, pulmonary hemorrhage34,35, optic neuropathy36 and nephrotic syndrome26-31.
THERAPEUTIC APPROACH
The therapeutic approach of the patient victim of multiple bee stings should be considered a medical emergency. The following initial care steps should be followed:
Removal of the causative agent: the removal of previously inoculated stings should be carried out as soon as possible. The longer the sting-to-skin contact time, the higher the venom inoculation rate3. The type of removal (by scraping or pinching) was considered irrelevant in the context of clinical evolution, unlike the exposure time, which should be as short as possible5,37. It is important to remove the stinger without squeezing it. Nonetheless, this approach should not delay the medical treatment.
-
Anaphylaxis treatment/prophylaxis:
According to the European Academy of Allergy and Clinical Immunology most recent guidelines, assessment using the ABCD (Airway, Breathing, Circulation, Disability and Exposure) approach should promptly applied to patients with anaphylaxis38. Cardiopulmonary resuscitation should be immediately instituted if cardiorespiratory arrest occurs38;
Epinephrine: treatment with intramuscular epinephrine is recommended as a first-line intervention before other approaches. The use of epinephrine is the first and most effective measure to be taken in the management of the anaphylaxis treatment. It should be used in all patients who are victims of a bee attack, regardless of the existence of possible comorbidities such as arrhythmias and hypertension, since it is the most effective action in the treatment of anaphylaxis and, considering the life-threatening condition, its use should not be postponed38. A dose of 0.5 mg has to be injected into the vastus lateralis of the thigh and this injection may be repeated every 5 to 15 minutes if systemic symptoms persist. The intramuscular route is preferable to the intravenous one (if used, apply adrenaline at a concentration of 1:1.000)39. Auto-injectable epinephrine (AIE) may be considered in patients reporting previous large local reactions to insect stings because they are at risk for developing systemic reactions, but there is no consensus on its cost-effectiveness, so the decision of providing AIE is left to the patient’s care physician39;
Lower-limb elevation: patients should be placed in the supine position and have their lower limbs elevated38,39;
Volume replacement: crystalloids are the fluid of choice38, and volumes of 5 mL/kg up to 30 mL/kg are recommended, depending on the patient’s hemodynamic status;
Oxygen: place an oximeter as soon as possible and provide 100% oxygen through a face mask. Observe signs of respiratory failure or laryngeal stridor, which may arise due to airway edema and, if they are observed, perform an orotracheal intubation;
Other medications: For possible cutaneous symptoms of urticaria and angioedema, associate antihistamines with H1 and H2 blockers38,39. Corticosteroids should be started aiming at preventing a late anaphylaxis reaction and should be maintained for 5 days in conjunction with antihistamines, particularly in patients with asthma and biphasic reactions38. For bronchospasm, inhalations can be prescribed with a B2-agonist38,39. Glucagon, via parenteral, is useful in patients with anaphylaxis who are unresponsive to epinephrine, particularly in those taking beta-blockers38.
The management of acute kidney injury (AKI) caused by bee sting is based on the same principles of AKI treatment for other causes. Bladder catheterization is crucial in these patients, who must have their urinary output closely monitored40. In cases of anuria or oliguria, furosemide can be used to convert them into a more favorable fluid balance condition40.
Some requested tests are urea, creatinine, serum electrolytes, urine analysis and hemoglobinuria. It is important to investigate intravascular hemolysis and rhabdomyolysis, as these are significant aggravating factors of kidney injury40. Among hydroelectrolyte disorders, hyperkalemia, treated with exchange resins, insulin solutions containing glucose and sodium bicarbonate should be considered of utmost importance, especially when metabolic acidosis is present. A potassium-restricted diet is also recommended40.
Fluid volume correction should be based on data from the patient’s physical examination40. Hypervolemia may be a frequent finding due to the low urinary output treated by crystalloid infusion. Blood pressure should be maintained at adequate levels40.
In more severe cases, refractory to conservative treatment, dialysis should be used, which, in addition to being indicated in uremia, hyperpotassemia, hypervolemia, metabolic acidosis refractory to treatment, also plays an important role in eliminating low molecular-weight venom toxins, such as melittin38,39.
There is no consensus in the literature on which type of dialysis is more effective for the treatment of AKI caused by bee sting; however, many authors have reported on the effectiveness of hemodialysis in these cases. Plasmapheresis has been used in conjunction with hemodialysis in some situations as an important means of removing venom19,41. There is still no specific serum against bee venom41. In a study of 43 cases of AKI caused by Africanized bees, 86% of the patients required dialysis, with hemodialysis and peritoneal dialysis being equally effective when compared to the other procedures42.
MORTALITY
Different causes of death have been described in the setting of bee stings accidents, including respiratory failure, acute myocardial infarction, acute renal failure or anaphylactic shock20,22,43. AKI caused by bee sting accidents was associated with a high mortality (22%), in a study of 27 cases. Of these, six patients died, two of them within the first 24 hours due to acute respiratory failure and hypovolemic shock20,44.
CONCLUSIONS
Some above-mentioned topics are worth mentioning:
The therapeutic approach of a patient victim of bee stings constitutes a medical emergency condition;
Bee stings should be removed from the victim’s body as quickly as possible, aiming at decreasing the exposure time to the venom;
Anaphylaxis should always be suspected and treated after bee stings. The use of epinephrine is the basis for the treatment of anaphylaxis and is considered the most effective measure among others;
Treatment of AKI caused by bee stings is based on the same principles of other renal injuries. Urinary output, serial physical and laboratory tests and blood pressure should be closely monitored. Dialysis should be indicated, when necessary, following current standard guidelines, always keeping in mind that time is crucial. Early dialysis institution is lifesaving in many situations;
Mortality due to accidents with multiple bee stings is estimated at 15% to 25%.
REFERENCES
- 1.1. Mingomataj EC, Bakiri AH, Ibranji A, Sturm GJ. Unusual reactions to hymenoptera stings: what should we keep in mind. Clin Rev Allergy Immunol. 2014;47:91-9. [DOI] [PubMed]; Mingomataj EC, Bakiri AH, Ibranji A, Sturm GJ. Unusual reactions to hymenoptera stings: what should we keep in mind. Clin Rev Allergy Immunol. 2014;47:91–99. doi: 10.1007/s12016-014-8434-y. [DOI] [PubMed] [Google Scholar]
- 2.2. Oliveira EC, Pedroso PM, Meirelles AE, Pescador CA, Gouvêa AS, Driemeier D. Pathological findings in dogs after multiple Africanized bee stings. Toxicon. 2007;49:1214-8. [DOI] [PubMed]; Oliveira EC, Pedroso PM, Meirelles AE, Pescador CA, Gouvêa AS, Driemeier D. Pathological findings in dogs after multiple Africanized bee stings. Toxicon. 2007;49:1214–1218. doi: 10.1016/j.toxicon.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 3.3. Daher EF, Oliveira RA, Silva LS, Silva EM, Morais TP. Insuficiência renal aguda por picada de abelhas: relato de casos. Rev Soc Bras Med Trop. 2009;42:209-12. [DOI] [PubMed]; Daher EF, Oliveira RA, Silva LS, Silva EM, Morais TP. Insuficiência renal aguda por picada de abelhas: relato de casos. Rev Soc Bras Med Trop. 2009;42:209–212. doi: 10.1590/s0037-86822009000200024. [DOI] [PubMed] [Google Scholar]
- 4.4. Bridi RA, Balbi AL, Neves PM, Ponce D. Acute kidney injury after massive attack of Africanised bees. BMJ Case Rep. 2014;2014:bcr2013201381. [DOI] [PMC free article] [PubMed]; Bridi RA, Balbi AL, Neves PM, Ponce D. Acute kidney injury after massive attack of Africanised bees. BMJ Case Rep. 20142014:bcr2013201381. doi: 10.1136/bcr-2013-201381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.5. Daher EF, Silva Junior GB, Bezerra GP, Pontes LB, Martins AM, Guimarães JA. Acute renal failure after massive honeybee stings. Rev Inst Med Trop São Paulo. 2003;45:45-50. [DOI] [PubMed]; Daher EF, Silva GB, Junior, Bezerra GP, Pontes LB, Martins AM, Guimarães JA. Acute renal failure after massive honeybee stings. Rev Inst Med Trop São Paulo. 2003;45:45–50. doi: 10.1590/s0036-46652003000100010. [DOI] [PubMed] [Google Scholar]
- 6.6. Grisotto LS, Mendes GE, Castro I, Baptista MA, Alves VA, Yu L, et al. Mechanisms of bee venom-induced acute renal failure. Toxicon. 2006;48:44-54. [DOI] [PubMed]; Grisotto LS, Mendes GE, Castro I, Baptista MA, Alves VA, Yu L, et al. Mechanisms of bee venom-induced acute renal failure. Toxicon. 2006;48:44–54. doi: 10.1016/j.toxicon.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 7.7. Arruda VM, Alves Junior VV, Moraes MM, Chaud Netto J, Suárez YR. Análise morfológica da glândula de veneno de Apis mellifera L. (Hymenoptera: Apidae) em populações de Mato Grosso do Sul. Neotrop Entomol. 2007;36:203-9. [DOI] [PubMed]; Arruda VM, Alves VV, Junior, Moraes MM, Chaud J, Netto, Suárez YR. Análise morfológica da glândula de veneno de Apis mellifera L. (Hymenoptera: Apidae) em populações de Mato Grosso do Sul. Neotrop Entomol. 2007;36:203–209. doi: 10.1590/s1519-566x2007000200006. [DOI] [PubMed] [Google Scholar]
- 8.8. Bogdanov S. Bee venom: composition, health, medicine: a review. Muehlethurnen: Bee Product Science; 2016. [cited 2017 Jan 31]. Available from: http://www.bee-hexagon.net/files/file/fileE/Health/VenomBookReview.pdf ; Bogdanov S. Bee venom: composition, health, medicine: a review. Muehlethurnen: Bee Product Science; 2016. [cited 2017 Jan 31]. http://www.bee-hexagon.net/files/file/fileE/Health/VenomBookReview.pdf. [Google Scholar]
- 9.9. Schmidt JO. Toxinology of venoms from the honeybee genus Apis. Toxicon. 1995;33:917-27. [DOI] [PubMed]; Schmidt JO. Toxinology of venoms from the honeybee genus Apis. Toxicon. 1995;33:917–927. doi: 10.1016/0041-0101(95)00011-a. [DOI] [PubMed] [Google Scholar]
- 10.10. Reis MA, Costa RS, Coimbra TM, Teixeira VP. Acute renal failure in experimental envenomation with Africanized bee venom. Ren Fail. 1998;20:39-51. [DOI] [PubMed]; Reis MA, Costa RS, Coimbra TM, Teixeira VP. Acute renal failure in experimental envenomation with Africanized bee venom. Ren Fail. 1998;20:39–51. doi: 10.3109/08860229809045088. [DOI] [PubMed] [Google Scholar]
- 11.11. Nandi M, Sarkar S. Acute kidney injury following multiple wasp stings. Pediatr Nephrol. 2012;27:2315-17. [DOI] [PubMed]; Nandi M, Sarkar S. Acute kidney injury following multiple wasp stings. Pediatr Nephrol. 2012;27:2315–2317. doi: 10.1007/s00467-012-2250-5. [DOI] [PubMed] [Google Scholar]
- 12.12. Ferreira DB, Costa RS, Oliveira JS, Muccillo G. Cardiac noradrenaline in experimental rat nevenomation with Africanized bee venom. Exp Toxicol Pathol. 1994;45:507-11. [DOI] [PubMed]; Ferreira DB, Costa RS, Oliveira JS, Muccillo G. Cardiac noradrenaline in experimental rat nevenomation with Africanized bee venom. Exp Toxicol Pathol. 1994;45:507–511. doi: 10.1016/S0940-2993(11)80516-6. [DOI] [PubMed] [Google Scholar]
- 13.13. Reis MA, Costa RS, Coimbra TM, Dantas M, Gomes UA. Renal changes induced by envenomation with Africanized bee venom in female Wistar rats. Kidney Blood Press Res. 1997;20:271-7. [DOI] [PubMed]; Reis MA, Costa RS, Coimbra TM, Dantas M, Gomes UA. Renal changes induced by envenomation with Africanized bee venom in female Wistar rats. Kidney Blood Press Res. 1997;20:271–277. doi: 10.1159/000174157. [DOI] [PubMed] [Google Scholar]
- 14.14. Ferreira DB, Costa RS, De Oliveira JA, Muccillo G. An infarct-like myocardial lesion experimentally induced in Wistar rats with Africanized bee venom. J Pathol. 1995;177:95-102. [DOI] [PubMed]; Ferreira DB, Costa RS, De Oliveira JA, Muccillo G. An infarct-like myocardial lesion experimentally induced in Wistar rats with Africanized bee venom. J Pathol. 1995;177:95–102. doi: 10.1002/path.1711770114. [DOI] [PubMed] [Google Scholar]
- 15.15. Muñoz-Arizpe R, Velásquez-Jones L, Roremo-Navarro B, Gómez-Chico R. Insuficiencia renal aguda por picadura de abejas africanizadas. Bol Med Hosp Infant Mex. 1992;49:388-90. [PubMed]; Muñoz-Arizpe R, Velásquez-Jones L, Roremo-Navarro B, Gómez-Chico R. Insuficiencia renal aguda por picadura de abejas africanizadas. Bol Med Hosp Infant Mex. 1992;49:388–390. [PubMed] [Google Scholar]
- 16.16. Hommel D, Bollandard F, Hulin A. Multiple African honeybee stings and acute renal failure. Nephron. 1998;78:235-6. [DOI] [PubMed]; Hommel D, Bollandard F, Hulin A. Multiple African honeybee stings and acute renal failure. Nephron. 1998;78:235–236. doi: 10.1159/000044923. [DOI] [PubMed] [Google Scholar]
- 17.17. Bourgain C, Pauti MD, Fillastre JP, Godin M, François A, Leroy JP, et al. Envenomation massive après piqûres d’abeilles africaines. Presse Med. 1998;27:1099-101. [PubMed]; Bourgain C, Pauti MD, Fillastre JP, Godin M, François A, Leroy JP, et al. Envenomation massive après piqûres d’abeilles africaines. Presse Med. 1998;27:1099–1101. [PubMed] [Google Scholar]
- 18.18. Bresolin NL, Carvalho LC, Goes EC, Fernandes R, Barotto AM. Acute renal failure following massive attack by Africanized bee stings. Pediatr Nephrol. 2002;17:625-7. [DOI] [PubMed]; Bresolin NL, Carvalho LC, Goes EC, Fernandes R, Barotto AM. Acute renal failure following massive attack by Africanized bee stings. Pediatr Nephrol. 2002;17:625–627. doi: 10.1007/s00467-002-0888-0. [DOI] [PubMed] [Google Scholar]
- 19.19. Díaz-Sánchez CL, Lifshitz-Guinzberg A, Ignacio-Ibarra G, Halabe-Cherem J, Quinones-Galvan A. Survival after massive (>2000) africanized honeybee sting. Arch Intern Med. 1998;158:925-7. [DOI] [PubMed]; Díaz-Sánchez CL, Lifshitz-Guinzberg A, Ignacio-Ibarra G, Halabe-Cherem J, Quinones-Galvan A. Survival after massive (>2000) africanized honeybee sting. Arch Intern Med. 1998;158:925–927. doi: 10.1001/archinte.158.8.925. [DOI] [PubMed] [Google Scholar]
- 20.20. França FO, Benvenuti LA, Fan HW, Dos Santos DR, Hain SH, Picchi-Martins FR, et al. Severe and fatal mass atacks by “killer” bees (Africanized honey bees – Apis mellifera scutellata) in Brazil: clinicopathological studies with measurement of serum venom concentrations. Q J Med. 1994;87:269-82. [PubMed]; França FO, Benvenuti LA, Fan HW, Dos Santos DR, Hain SH, Picchi-Martins FR, et al. Severe and fatal mass atacks by “killer” bees (Africanized honey bees – Apis mellifera scutellata) in Brazil: clinicopathological studies with measurement of serum venom concentrations. Q J Med. 1994;87:269–282. [PubMed] [Google Scholar]
- 21.21. Humblet Y, Sonnet J, van Ypersele de Strihou C. Bee stings and acute tubular necrosis. Nephron. 1982;31:187-8. [DOI] [PubMed]; Humblet Y, Sonnet J, van Ypersele de Strihou C. Bee stings and acute tubular necrosis. Nephron. 1982;31:187–188. doi: 10.1159/000182643. [DOI] [PubMed] [Google Scholar]
- 22.22. Mejia G, Arbelaez M, Henao JE, Sus AA, Arango JL. Acute renal failure due to multiple stings by Africanized bees. Ann Intern Med. 1986;104:210-1. [DOI] [PubMed]; Mejia G, Arbelaez M, Henao JE, Sus AA, Arango JL. Acute renal failure due to multiple stings by Africanized bees. Ann Intern Med. 1986;104:210–211. doi: 10.7326/0003-4819-104-2-210. [DOI] [PubMed] [Google Scholar]
- 23.23. Daher EF, Cordeiro NF. Insuficiência renal aguda por rabdomiólise. Rev Bras Med. 1998;55:526-33.; Daher EF, Cordeiro NF. Insuficiência renal aguda por rabdomiólise. Rev Bras Med. 1998;55:526–533. [Google Scholar]
- 24.24. Vanholder R, Sever MS, Erek E, Lameire N. Rhabdomyolysis. J Am Soc Nephrol. 2000;11:1553-61. [DOI] [PubMed]; Vanholder R, Sever MS, Erek E, Lameire N. Rhabdomyolysis. J Am Soc Nephrol. 2000;11:1553–1561. doi: 10.1681/ASN.V1181553. [DOI] [PubMed] [Google Scholar]
- 25.25. Zager RA. Rhabdomyolysis and myohemoglobinuric acute renal failure. Kidney Int. 1996;49:314-26. [DOI] [PubMed]; Zager RA. Rhabdomyolysis and myohemoglobinuric acute renal failure. Kidney Int. 1996;49:314–326. doi: 10.1038/ki.1996.48. [DOI] [PubMed] [Google Scholar]
- 26.26. Light WC, Reisman RE, Shimizu M, Arbesman CE. Unusual reactions following insect stings. Clinical features and immunologic analysis. J Allergy Clin Immunol. 1977;59:391-7. [DOI] [PubMed]; Light WC, Reisman RE, Shimizu M, Arbesman CE. Unusual reactions following insect stings. Clinical features and immunologic analysis. J Allergy Clin Immunol. 1977;59:391–397. doi: 10.1016/0091-6749(77)90024-0. [DOI] [PubMed] [Google Scholar]
- 27.27. Olivero JJ, Ayus JC, Eknoyan G. Nephrotic syndrome developing after bee stings. South Med J. 1981;74:82-3. [DOI] [PubMed]; Olivero JJ, Ayus JC, Eknoyan G. Nephrotic syndrome developing after bee stings. South Med J. 1981;74:82–83. doi: 10.1097/00007611-198101000-00030. [DOI] [PubMed] [Google Scholar]
- 28.28. Tareyeva IE, Nikolaev AJ, Janushkevitch TN. Nephrotic syndrome induced by insect sting. Lancet. 1982;2:825. [DOI] [PubMed]; Tareyeva IE, Nikolaev AJ, Janushkevitch TN. Nephrotic syndrome induced by insect sting. 825Lancet. 1982;2 doi: 10.1016/s0140-6736(82)92718-0. [DOI] [PubMed] [Google Scholar]
- 29.29. Tasic V. Nephrotic syndrome in a child after a bee sting. Pediatr Nephrol. 2000;15:245-7. [DOI] [PubMed]; Tasic V. Nephrotic syndrome in a child after a bee sting. Pediatr Nephrol. 2000;15:245–247. doi: 10.1007/s004670000452. [DOI] [PubMed] [Google Scholar]
- 30.30. Venters HD, Vernier RL, Worthen HG, Good RA. Bee sting nephrosis: a study of the immunopathologic mechanisms. Am J Dis Child. 1961;102:688-9.; Venters HD, Vernier RL, Worthen HG, Good RA. Bee sting nephrosis: a study of the immunopathologic mechanisms. Am J Dis Child. 1961;102:688–689. [Google Scholar]
- 31.31. Ceri M, Kurultak I. Relapse of nephrotic syndrome after a bee sting. Indian J Nephrol. 2012;22:151-2. [DOI] [PMC free article] [PubMed]; Ceri M, Kurultak I. Relapse of nephrotic syndrome after a bee sting. Indian J Nephrol. 2012;22:151–152. doi: 10.4103/0971-4065.97147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.32. Ceyhan C, Ercan E, Teklen T, Kirilmaz B, Onder R. Myocardial infarction following a bee sting. Int J Cardiol. 2001;80:251-3. [DOI] [PubMed]; Ceyhan C, Ercan E, Teklen T, Kirilmaz B, Onder R. Myocardial infarction following a bee sting. Int J Cardiol. 2001;80:251–253. doi: 10.1016/s0167-5273(01)00477-6. [DOI] [PubMed] [Google Scholar]
- 33.33. Magadle R, Weiner P, Waizman J, Pelled B. Acute myocardial infarction after honey bee sting. Harefuah. 2000;138:543-5,614. [PubMed]; Magadle R, Weiner P, Waizman J, Pelled B. Acute myocardial infarction after honey bee sting. Harefuah. 2000;138:543-5–54614. [PubMed] [Google Scholar]
- 34.34. Lam SM. Acute pulmonary hemorrhage following a honeybee sting: a case report. J Microbiol Immunol Infect. 1998;31:133-6. [PubMed]; Lam SM. Acute pulmonary hemorrhage following a honeybee sting: a case report. J Microbiol Immunol Infect. 1998;31:133–136. [PubMed] [Google Scholar]
- 35.35. Mukhopadhyay A, Fong KY, Lim TK. Diffuse alveolar haemorrhage: a rare reaction to insect sting. Respirology. 2002;7:157-9. [DOI] [PubMed]; Mukhopadhyay A, Fong KY, Lim TK. Diffuse alveolar haemorrhage: a rare reaction to insect sting. Respirology. 2002;7:157–159. doi: 10.1046/j.1440-1843.2002.00385.x. [DOI] [PubMed] [Google Scholar]
- 36.36. Maltzman JS, Lee AG, Miller NR. Optic neuropathy occurring after bee and wasp sting. Ophthalmology. 2000;107:193-5. [DOI] [PubMed]; Maltzman JS, Lee AG, Miller NR. Optic neuropathy occurring after bee and wasp sting. Ophthalmology. 2000;107:193–195. doi: 10.1016/s0161-6420(99)00020-2. [DOI] [PubMed] [Google Scholar]
- 37.37. Visscher PK, Vetter RS, Camazine S. Removing bee stings. Lancet. 1996;348:301-2. [DOI] [PubMed]; Visscher PK, Vetter RS, Camazine S. Removing bee stings. Lancet. 1996;348:301–302. doi: 10.1016/s0140-6736(96)01367-0. [DOI] [PubMed] [Google Scholar]
- 38.38. Muraro A, Roberts G, Worm M, Bilò MB, Brockow K, Fernández Rivas M, et al. Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy. 2014;69:1026-45. [DOI] [PubMed]; Muraro A, Roberts G, Worm M, Bilò MB, Brockow K, Fernández Rivas M, et al. Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy. 2014;69:1026–1045. doi: 10.1111/all.12437. [DOI] [PubMed] [Google Scholar]
- 39.39. Lieberman P, Nicklas RA, Randolph C, Oppenheimer J, Bernstein D, Bernstein J, et al. Anaphylaxis – a practice parameter update 2015. Ann Allergy Asthma Immunol. 2015;115:341-84. [DOI] [PubMed]; Lieberman P, Nicklas RA, Randolph C, Oppenheimer J, Bernstein D, Bernstein J, et al. Anaphylaxis – a practice parameter update 2015. Ann Allergy Asthma Immunol. 2015;115:341–384. doi: 10.1016/j.anai.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 40.40. Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int. 2012;2 Suppl:1-138.; Acute Kidney Injury Work Group KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int. 2012;2(Suppl):1–138. [Google Scholar]
- 41.41. Beccari M. Dialysis or plasmapheresis for acute renal failure due to Africanized honeybee stings. Arch Intern Med. 1999;159:1255-6. [DOI] [PubMed]; Beccari M. Dialysis or plasmapheresis for acute renal failure due to Africanized honeybee stings. Arch Intern Med. 1999;159:1255–1256. doi: 10.1001/archinte.159.11.1255. [DOI] [PubMed] [Google Scholar]
- 42.42. Schumacher MJ, Egen NB. Significance of Africanized bees for public health: a review. Arch Intern Med.1995;155:2038-43. [PubMed]; Schumacher MJ, Egen NB. Significance of Africanized bees for public health: a review. Arch Intern Med. 1995;155:2038–2043. [PubMed] [Google Scholar]
- 43.43. Mendes RP, Meira DA, Teixeira UA, Molinari H, Rodrigues PS, Coelho KY. Acidente por múltiplas picadas de abelhas: relato de dois casos, revisão da literatura e discussão da patogenia e tratamento. Arq Bras Med. 1990;64:81-8.; Mendes RP, Meira DA, Teixeira UA, Molinari H, Rodrigues PS, Coelho KY. Acidente por múltiplas picadas de abelhas: relato de dois casos, revisão da literatura e discussão da patogenia e tratamento. Arq Bras Med. 1990;64:81–88. [Google Scholar]
- 44.44. Nittner-Marszalska M, Małolepszy J, Młynarczewski A, Niedziółka A. Toxic reaction induced by hymenoptera stings. Pol Arch Med Wewn. 1998;100:252-6. [PubMed]; Nittner-Marszalska M, Małolepszy J, Młynarczewski A, Niedziółka A. Toxic reaction induced by hymenoptera stings. Pol Arch Med Wewn. 1998;100:252–256. [PubMed] [Google Scholar]