Abstract
A 15-item checklist, including physical and behavioral features frequently observed in fragile X syndrome, was used in a prospective study of 188 mentally retarded males in order to identify males at risk for this syndrome. Of the 188 males, 19 were found to have the fragile X syndrome, while the remaining 169 males had no recognizable cause of their mental retardation, including normal chromosomes. Significant differences (p<0.01) were found between mentally retarded males with and without the fragile X syndrome with increased hyperactivity; shorter attention span; more tactile defensiveness, hand-flapping, perseverative speech, and hyperextensibility; large ears and testes; higher frequency of simian creases or Sydney lines and plantar creases; and more positive family histories of mental retardation in the fragile X syndrome males. Multiple regression and discriminant analyses of the 188 males indicated several physical features were useful predictors for inclusion in the fragile X syndrome group. An overall correct classification rate of 93% was achieved based on 6 variables (plantar crease, simian crease, hyperflexibility, large testes, large ears, and a positive family history of mental retardation) that were entered into the discriminant equation. Therefore, our experience with a 15-item checklist suggests the potential of screening for the fragile X syndrome in mentally retarded males and that 6 of the 15 variables were particularly good predictors of this syndrome.
Keywords: correlations, fragile X chromosome, Martin-Bell syndrome, multiple regression and discriminant analyses, physical and behavioral features, predictors, screening
Fragile X or Martin-Bell syndrome is characterized by mental retardation; macroorchidism; large, prominent ears; long, narrow face; hyperextensibility of joints and a folate-sensitive chromosome fragile site at Xq27.3 (Chudley & Hagerman 1987, Hagerman 1987, Butler 1988). It is the most common inherited cause of mental retardation and autism (Neri et al. 1988, Hagerman et al. 1986). The overall incidence of this syndrome approaches one per 1000 males while one per 500 females carry the fragile X chromosome, with approximately 30% of those females having mental retardation (Webb et al. 1986, Hagerman 1987). Screening studies have shown that 3 to 6% of institutionalized mentally retarded males have the fragile X syndrome. However, the cost of cytogenetic screening of all mentally retarded males is generally prohibitive and the variability of some of the features (e.g. macroorchidism), particularly before puberty, has made it difficult to identify consistently those males at risk for the fragile X syndrome. Nonetheless, fragile X syndrome screening checklists based on physical characteristics (e.g., large ears) and/or medical history (e.g., hyperactivity) have been developed for identifying males at risk for the fragile X syndrome and for subsequent cytogenetic analysis (Thake et al. 1985, Turner et al. 1986, Hagerman 1987). We report here our experience with a modification of a checklist previously reported (Hagerman 1987) in screening a relatively large number of mentally retarded males for the fragile X syndrome.
Material and Methods
Subjects
One hundred and eighty-eight learning disabled or mentally retarded males were included in this study to determine the usefulness of a 15-item checklist in identifying those individuals with the fragile X syndrome. Nineteen of these 188 males from 15 families (average age of 21.3 years with a range of 3.7 to 71.9 years; average fragile X chromosome expression of 23% with a range of 3 to 46%) had the fragile X syndrome. One hundred and sixty-nine of the 188 males were from 167 families (average age of 40.4 years with a range of 3.8 to 85.7 years) and did not have a recognizable cause of their mental retardation, including normal chromosomes. Seventy-nine percent of the fragile X syndrome group were white, while 78% of the non-fragile X syndrome group were white. The remaining individuals in each group were black.
Fragile X Syndrome Checklist
Prior to cytogenetic studies, a modification of a fragile X syndrome screening checklist reported by Hagerman (1987) was completed for each subject by one of the authors (M.G.B.). Our checklist consisted of 15 items, including the 13 items reported by Hagerman (1987) which were mental retardation, large ears, large testes, hyperactivity, family history of mental retardation or autism, short attention span, tactile defensiveness, hyperextensible finger joints, perseverative speech, hand-flapping, hand-biting, poor eye contact and simian crease or Sydney line as well as plantar crease and pale blue eyes (particularly in white males). The latter two features may also be over-represented in fragile X syndrome males (Turner et al. 1980).
The checklist was completed with information obtained from the medical records, from the patient’s history obtained from the parents or guardians, and from the physical examination. Each item was scored according to criteria established by Hagerman (1987). An item received a score of 2 if it was definitely present; a score of 1 if present in the past, questionably or borderline present; or a score of 0 if never present.
For example, patients with tactile defensiveness, as determined by an aversion to touch or tactile stimuli, received a score of 2. Hand-biting (including wrist-biting), was recorded but nail-biting was omitted. Hyperextensibility was present if the metacarpophalangeal joints could be extended ≥90° with the palm flat. The testes were enlarged if the volume was ≥2 SD for age. The ears were considered large if ≥2 SD for age. The presence or absence of simian creases or Sydney lines of the palms and plantar creases which were greater than 1 cm in length between the first and second toes were recorded. A score of 2 for family history of mental retardation was recorded if a first-degree relative (e.g., siblings) or second-degree relative (e.g., uncle) was mentally retarded. If a third-degree relative (e.g., first cousin) was mentally retarded, then a score of 1 was recorded. A total score of 30 points was possible based on our 15-item checklist.
Cytogenetics
Peripheral blood cultures were established in M199 supplemented with 5% fetal calf serum, phytohemagglutinin, and antibiotics with pH adjusted to 7.8. The cultures were incubated at 37°C for 96 h and colcemid (0.15 mg/ml) added 45 min prior to harvest.
Peripheral blood samples were also cultured by using RPMI 1640 medium, supplemented with 15% fetal calf serum, phytohemagglutinin, and antibiotics. The cultures were incubated for 96 h at 37°C with FUdR (10−7M) added 24 h prior to harvest and colcemid (0.15 mg/ml) added 45 min before harvest.
Cells were harvested following treatment with 0.56% KCl hypotonic solution for 8 min at 37°C. Cells were fixed with 3:1 methanol-acetic acid and washed four times. Chromosome slides were air-dried by using conventional methods and stained with Giemsa. A minimum of 75 cells (e.g., 50 from M199, 25 from RPMI 1640 with FUdR) were analyzed for chromosome lesions from each individual. If chromosome breaks and gaps resembling fragile sites were observed, then the cells were destained and banded with the GTG method. The location of the site was determined and the presence of the Xq27.3 site recorded.
Statistical Tests
Chi-square, Mann-Whitney U, Pearson product-moment correlation and stepwise multiple regression and discriminant analyses were used in this study for determination of statistical differences in the checklist items between mentally retarded males with and without the fragile X syndrome, as well as for identification of predictive variables for screening mentally retarded males for the fragile X syndrome.
Results
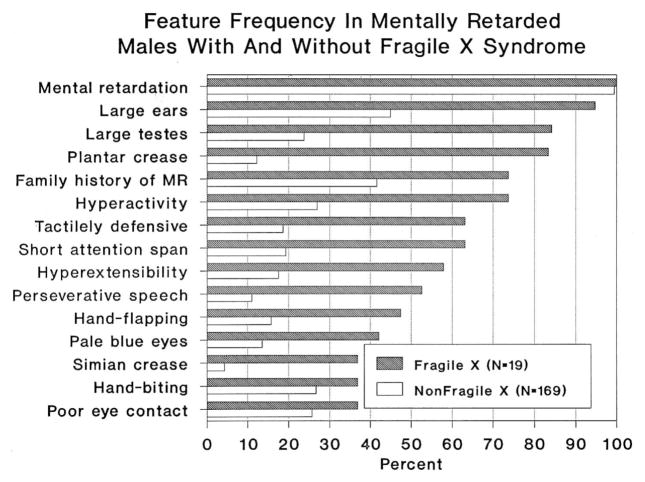
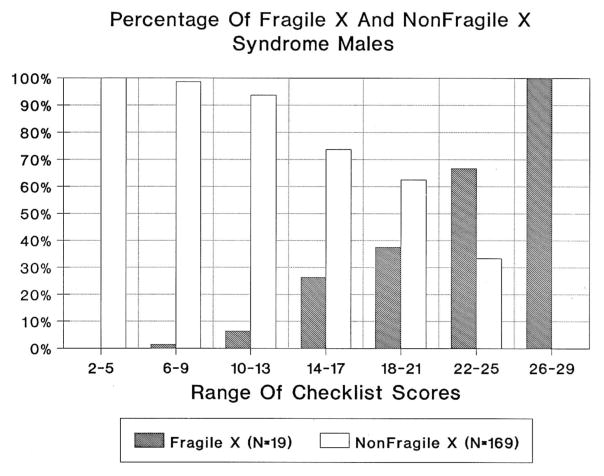
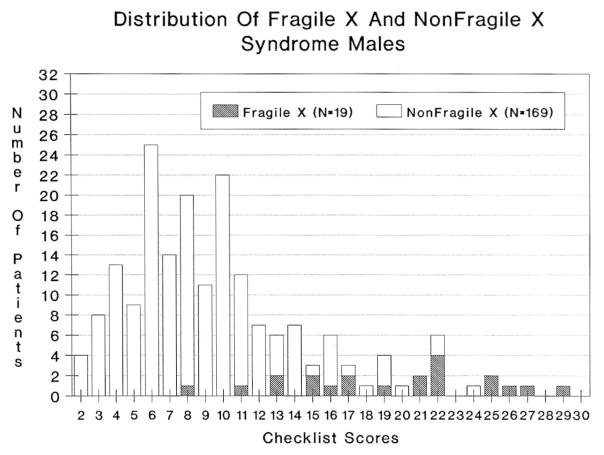
The average total score for the fragile X syndrome males was 18.6 ± 5.4 SD with a range of 8 to 29. The average total score for the mentally retarded males without the fragile X syndrome was 8.8 ± 4.2 SD with a range of 2 to 24. A significant difference (p < 0.001) was found in the average total score between mentally retarded males with and without the fragile X syndrome. Fig. 1 shows the frequency of each feature for the two groups of mentally retarded males. Fig. 2 shows the percentage of males in each assigned checklist score interval. Fig. 3 shows the total distribution of scores for the two groups of mentally retarded males.
Fig. 1.
Frequency of each checklist item on the mentally retarded males with and without the fragile X syndrome.
Fig. 2.
Percentage of mentally retarded males with and without the fragile X syndrome assigned to each checklist score interval.
Fig. 3.
The distribution of checklist scores for the mentally retarded males with and without the fragile X syndrome.
Chi-square analysis was undertaken to determine the items more frequently seen in fragile X syndrome patients when screening mentally retarded males. Table 1 shows the fragile X syndrome checklist data from the 188 mentally retarded males and the chi-square values for each parameter. Features which were found to be significantly more frequent (p < 0.05) in the fragile X syndrome males included: large ears, large testes, plantar crease, simian crease, pale blue eyes, hyperextensibility, hyperactivity, tactile defensiveness, hand flapping, perseverative speech, short attention span, and positive family history of mental retardation.
Table 1.
Fragile X checklist data from 188 males with and without fragile X syndrome
| Parameters | Fragile X males % (no. observed/total) | Non fragile X males % (no. observed/total) | Chi square value |
|---|---|---|---|
| Mental retardation | 100.0% (19/19) | 99.4% (168/169) | 1.761 |
| Large ears | 94.7% (18/19) | 49.9% (75/167) | 15.007d |
| Large testes | 84.2% (16/19) | 23.7% (37/156) | 26.559d |
| Plantar crease* | 83.3% (15/19) | 12.2% (20/164) | 48.365d |
| Hyperactivity | 73.7% (14/19) | 26.9% (45/167) | 15.115d |
| Family history of mental retardation or autism | 73.7% (14/19) | 41.6% (64/154) | 5.812a |
| Short attention span | 63.2% (12/19) | 19.3% (32/166) | 15.769d |
| Tactilely defensive | 63.2% (12/19) | 18.7% (31/166) | 16.498d |
| Hyperextensible finger joints | 57.9% (11/19) | 17.6% (29/165) | 13.996c |
| Perseverative speech | 52.6% (10/19) | 11.0% (10/91) | 15.630d |
| Hand-flapping | 47.4% (9/19) | 15.8% (26/165) | 9.096b |
| Pale blue eyes* | 42.1% (8/19) | 13.5% (21/155) | 7.988b |
| Hand-biting | 36.8% (7/19) | 26.7% (44/165) | 0.446 |
| Poor eye contact | 36.8% (7/19) | 25.6% (40/156) | 0.587 |
| Simian crease or Sydney line | 36.8% (7/19) | 4.2% (7/165) | 21.329d |
p < 0.05;
p < 0.01;
p < 0.001;
p < 0.0001;
Parameter in addition to Hagerman’s Checklist (Hagerman 1987).
Several checklist variables were found to be significantly different (p < 0.01) between mentally retarded males with and without the fragile X syndrome when analyzed with the Mann-Whitney U test. These variables included: increased hyperactivity; shorter attention span; more tactile defensiveness, hand-flapping, perseverative speech, and hyperextensibility; larger ears and testes; higher frequency of simian creases or Sydney lines and plantar creases; and more positive family histories of mental retardation in the fragile X syndrome males.
No significant correlations were found when comparing fragile X chromosome expression with age (r = 0.32; p = 0.09) or fragile X expression with the total checklist scores (r = 0.05; p = 0.42). However, significant intervariable correlations (p < 0.001) were found in the fragile X syndrome males. These variables included: hyperactivity and short attention span; short attention span and hyperactivity, tactile defensiveness; and tactile defensiveness and short attention span. Additionally, several significant intervariable correlations (p < 0.001) were also found for the mentally retarded males without the fragile X syndrome. These variables included: mental retardation and hyperextensibility, simian crease; hyperactivity and short attention span, hand-biting, poor eye contact; short attention span and hyperactivity, tactile defensiveness, hand-biting, poor eye contact; tactile defensiveness and short attention span, hand-flapping, perseverative speech; hand-flapping and tactile defensiveness, perseverative speech; hand-biting and hyperactivity, short attention span, poor eye contact, perseverative speech, hyperextensibility; poor eye contact and hyperactivity, short attention span, hand-biting; perseverative speech and tactile defensiveness, hand-flapping, hand-biting, simian crease; hyperextensibility and mental retardation, hand-biting; simian crease and mental retardation, perseverative speech.
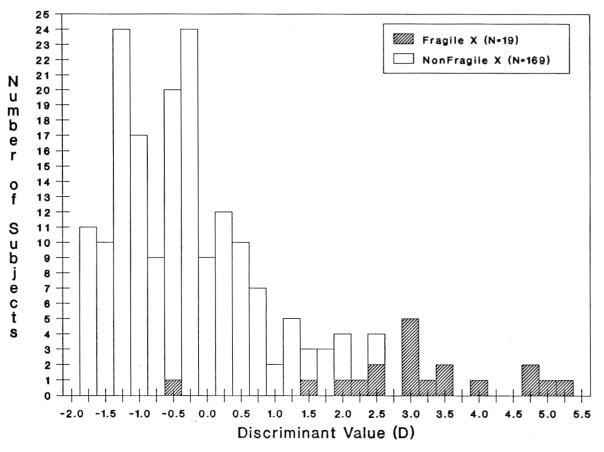
To further clarify which features from the 15-item checklist were more frequently seen in fragile X syndrome males and to determine the most useful or discriminating variables in predicting which mentally retarded males had the fragile X syndrome, stepwise multiple regression and discriminant analyses were undertaken. With the stepwise regression analysis of all mentally retarded males, dermatoglyphic findings (e.g., plantar and simian creases) were found to be the best predictors for the fragile X syndrome. Other useful predictors identified with regression analysis included: large testes, large ears, hyperextensibility and a positive family history of mental retardation. In our forward stepwise discriminant analysis of the 188 mentally retarded individuals, an overall correct classification rate of 93% was achieved based on 6 variables (plantar crease, simian crease, hyperflexibility, large testes, large ears, and a positive family history of mental retardation) that were entered into the discriminant equation (Fig. 4). The average discriminant values were 3.72 and −0.045, respectively, for males with and without the fragile X syndrome.
Fig. 4.
Histogram depicting mentally retarded males with and without the fragile X syndrome classified by discriminant analysis. The discriminant equation is as follows: D = −1.848 + 0.902 (plantar crease) + 0.258 (family history of MR) + 1.182 (simian crease) + 0.396 (large testes) + 0.338 (large ears) + 0.477 (hyperextensibility). To calculate the discriminant value, insert the checklist score for each of the variables into the equation [score = 2 (if definitely present); 1 (if present in past or borderline); 0 (never present)].
Discussion
We report our experience with a 15-item checklist containing both physical and behavioral features thought to be useful in identifying fragile X syndrome males in a group of 188 mentally retarded males without a previous diagnosis or cause of their mental retardation. Although the number of fragile X syndrome males in our prospective study is relatively small in relationship to the mentally retarded males without a recognizable cause for their mental retardation, our study did identify significant differences with several statistical tests between the two groups of mentally retarded males. Of the checklist variables, the largest chi-square value was found with plantar crease (present in 83% of fragile X males and only 12% of males without fragile X) followed by large testes (present in 84% of fragile X males and 24% of males without fragile X). The smallest chi-square value was found with hand-biting (present in 37% of fragile X males and 27% of males without fragile X) followed by poor eye contact (present in 37% of fragile X males and 26% of males without fragile X).
A total checklist score of 21 or higher from a maximum score of 30 indicated a high degree of certainty for the fragile X syndrome with 47% of the fragile X syndrome males achieving a score ≥21 while only 1.7% of the males without the fragile X syndrome had a similar score. Conversely, 80% of the males without the fragile X syndrome had a score ≤11, whereas only 11% of fragile X syndrome males had a similar score. In addition, several of the checklist parameters were found with both regression and discriminant analysis for the fragile X syndrome to be good predictors. These predictors were primarily physical features (e.g., simian and plantar creases, large ears and testes and hyperflexibility) and not behavioral variables (e.g., poor eye contact).
A classification rate of 93% was achieved with discriminant analysis based on 6 of the 15 checklist variables (Fig. 4). We are encouraged by this overall correct classification rate and the usefulness of the checklist variables in identifying mentally retarded males for chromosome analysis at risk for the fragile X syndrome. Additionally, six anthropometric variables were described recently, that discriminated 34 patients with the fragile X syndrome from 71 mentally retarded males without the fragile X syndrome at an overall correct classification rate of 97.1% (Butler et al. 1991). The six variables were: testicular volume, ear width, bizygomatic diameter, head breadth, hand breadth and hand length. Additional testing with a larger sample of fragile X syndrome individuals is needed to test the power of discrimination of the checklist variables to distinguish patients with fragile X syndrome from mentally retarded males without the fragile X syndrome.
In summary, the observations presented in this report suggest the potential of screening for fragile X syndrome males and identifying those males with the use of this checklist at high risk for this syndrome. Specifically, 6 of the 15 checklist variables were good predictors for the fragile X syndrome in mentally retarded males without a recognizable cause of their mental retardation.
Acknowledgments
We thank Pamela Grimm for expert preparation of the manuscript and also Andy Allen and Judy Haynes for their assistance in data collection and analysis. This research has been funded by the Tennessee Department of Mental Health and Mental Retardation and the Clinical Research Center, Meharry Medical College, Nashville, Tennessee.
References
- Butler MG. Fragile X syndrome: a major cause of X-linked mental retardation. Comprehensive Ther. 1988;14:3–7. [PMC free article] [PubMed] [Google Scholar]
- Butler MG, Allen GA, Haynes JL, Singh DN, Watson MS, Breg WR. Anthropometric comparison of mentally retarded males with and without the fragile X syndrome. Am J Med Genet. 1991 doi: 10.1002/ajmg.1320380220. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chudley AE, Hagerman RJ. Fragile X syndrome. J Pediatr. 1987;20:821–824. doi: 10.1016/s0022-3476(87)80392-x. [DOI] [PubMed] [Google Scholar]
- Hagerman RJ. Fragile X syndrome. Curr Probl Pediatr. 1987;17:621–674. doi: 10.1016/0045-9380(87)90011-9. [DOI] [PubMed] [Google Scholar]
- Hagerman RJ, Jackson AW, Levitas A, Rimland B, Braden M. An analysis of autism in 50 males with the fragile X syndrome. Am J Med Genet. 1986;23:359–374. doi: 10.1002/ajmg.1320230128. [DOI] [PubMed] [Google Scholar]
- Neri G, Opitz JM, Mikkelsen M, Jacobs PA, Davies K, Turner G. Conference report: Third International Workshop on the Fragile X and X-linked Mental Retardation. Am J Med Genet. 1988;30:1–29. [Google Scholar]
- Thake A, Todd J, Bundey SE, Webb T. Is it possible to make a clinical diagnosis of the fragile X syndrome in a boy? Arch Dis Child. 1985;60:1001–1007. doi: 10.1136/adc.60.11.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner G, Robinson H, Laing S, Purvis-Smith S. Preventive screening for the fragile X syndrome. NEJM. 1986;315:607–608. doi: 10.1056/NEJM198609043151002. [DOI] [PubMed] [Google Scholar]
- Turner G, Brookwell R, Daniel A, Selikowitz M, Zilibowitz M. Heterozygous expression of X-linked mental retardation and X-chromosome marker fra(X)(q27) NEJM. 1980;303:662–664. doi: 10.1056/NEJM198009183031202. [DOI] [PubMed] [Google Scholar]
- Webb TP, Bundy SE, Thake AL, Todd J. Population incidence and segregation ratios in the Martin-Bell syndrome. Am J Med Genet. 1986;23:573–580. doi: 10.1002/ajmg.1320230151. [DOI] [PubMed] [Google Scholar]