Abstract
Standards (95th, 50th, and 5th percentiles) in fragile X syndrome for weight, height, head circumference, ear length, and testicular volume are reported. For comparison with fragile X syndrome standardized curves, normal control data from the literature were similarly plotted and curves produced. These standards reflect the physical parameters that are frequently abnormal in males with the fragile X syndrome and should be useful in the medical management of patients with this syndrome. The standards may also be used to help identify those individuals, particularly the younger males, for chromosome studies to confirm the clinical impression of the fragile X syndrome.
The fragile X syndrome is characterized by mental retardation, large ears, an elongated face, macroorchidism, mild connective tissue dysplasia, and expression of the Xq27.3 fragile site in folate-deficient culture conditions.1 The Xq27.3 fragile site is a cytogenetic marker for the gene(s) responsible for features recognized in the fragile X syndrome and is diagnostic if seen in at least 4% of male and 2% of female cells.1–5 Recently, DNA sequences which appear to be unstable have been located at the fragile site and characterization of the molecular structure is under way.2–4 After Down syndrome, the fragile X syndrome is the most common genetic cause of mental retardation and usually affects males, but females can also be affected. The fragile X syndrome accounts for 30% to 50% of families with male mental retardation.
Recently, Hagerman et al.5 reported that the presence of large ears, macroorchidism, and hand calluses in mentally retarded males would yield positive fragile X chromosome results in 50% of these patients. Butler et al.6,7 also reported that certain physical characteristics (eg, ear width, testicular volume, bizygomatic diameter, head breadth, plantar crease, hyperflexibility) could be used to correctly classify fragile X syndrome in 97% of mentally retarded males. However, only a few studies have been reported on the linear growth patterns in individuals with the fragile X syndrome.8–14 There is a paucity of anthropometric standards in fragile X syndrome.
Here, we report standardized curves for males with the fragile X syndrome on five physical measurements frequently obtained in the evaluation of males suspected to have the fragile X syndrome. The standards were developed from 185 males with fragile X syndrome and include weight, height, head circumference, ear length, and testicular volume. These standardized curves should be useful in the clinical setting in the evaluation of males suspected to have the fragile X syndrome and their comparison with other similarly affected males.
MATERIALS AND METHODS
The 185 white males between the ages of 0 and 26 years (average age, 11.1 years ± 7.3 [SD]) included in this study had the fragile X syndrome with an average fragile X chromosome expression of 21% ± 12% (range, 4% to 58%). They were ascertained from males with learning disabilities, mental retardation, hyperactivity, or autism presenting to development centers and/or genetics clinics. The anthropometric measurements consisted of weight, height, head circumference, ear length, and testicular volume. Up to the age of 2 years, length was measured using a horizontal calibrated board, with the subject in a supine position; thereafter, height measurements were taken. Head circumference was measured to the nearest millimeter with a steel or fiber tape. Weight and height were obtained with a balanced beam scale and anthropometer, respectively. Ear length was measured to the nearest millimeter with a ruler, and testicular volume was estimated by the use of a Prader orchidometer (if greater than 25 mL, the length and width were measured with either a sliding caliper or fiber tape, and volume was calculated by the use of the equation π/6 × L × W2).
Curves for the fragile X syndrome were developed according to standards of reliability and precision previously described.15–17 The first criterion is a sample size of five or more per age interval. To meet this criterion for our study, males with the fragile X syndrome were grouped at 1-year age intervals with an average of approximately seven individuals per age interval. The second criterion states that the coefficient of variation, ie, the standard deviation expressed as a percentage of the mean, should be less than 25%. The means and standard deviations were calculated for each age interval, and standardized curves from 0 to 26 years of age for weight, height, and head circumference and from 1 to 26 years of age for ear length and testicular volume were produced after meeting the above two criteria by plotting the mean (or 50th percentile), 5th, and 95th percentiles for each age interval for males with the fragile X syndrome. For comparison with fragile X syndrome curves, normal control anthropometric data were similarly collected18–21 and plotted and then standards (95th, 50th, and 5th percentiles) produced.
RESULTS
Figures 1 through 5 show standardized curves of anthropometric variables for males with the fragile X syndrome and for normal individuals. For weight in males with fragile X syndrome, the 95th, 50th, and 5th percentiles closely approximate the normal 95th, 50th, and 5th percentiles until about 12 years of age, when the fragile X percentiles were above the normal percentiles, but they begin to fall below the normal percentiles at about 20 years of age and older. For height in males with fragile X syndrome, the 95th, 50th, and 5th percentiles approximate the normal 95th, 50th, and 5th percentiles until 15 years of age and older, when they fall below the normal percentiles. For head circumference in males with fragile X syndrome, the 95th, 50th, and 5th percentiles were consistently above the respective normal percentiles, with the greatest increase between 6 months and 6 years. For ear length in males with fragile X syndrome, the 95th, 50th, and 5th percentiles were consistently above the respective normal percentiles for all ages, with the 50th percentile approximating the normal 95th percentile and the 5th percentile approximating the normal 50th percentile. For testicular volume in males with fragile X syndrome, the 95th, 50th, and 5th percentiles were consistently above the respective normal percentile for all ages. The 50th percentile approximates the normal 95th percentile until 6 years of age, when a substantial increase in testicular volume occurred in males with fragile X syndrome and both the 50th and 95th percentiles were markedly above the normal 95th percentile.
Fig 1.
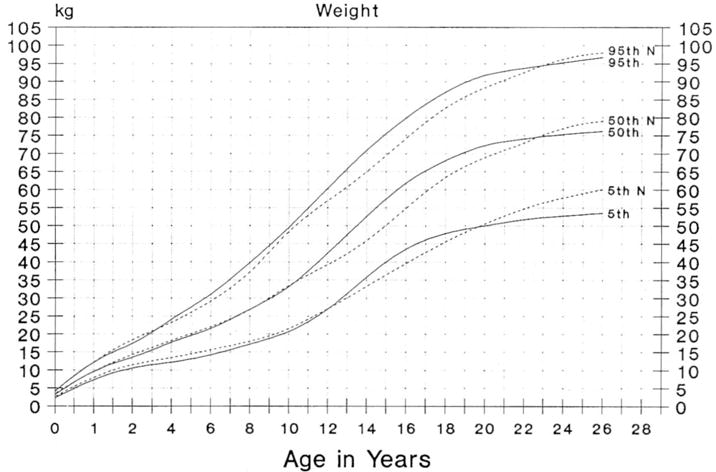
Standardized curves for weight of males with fragile X syndrome (solid line) and normal individuals (broken line).
Fig 5.
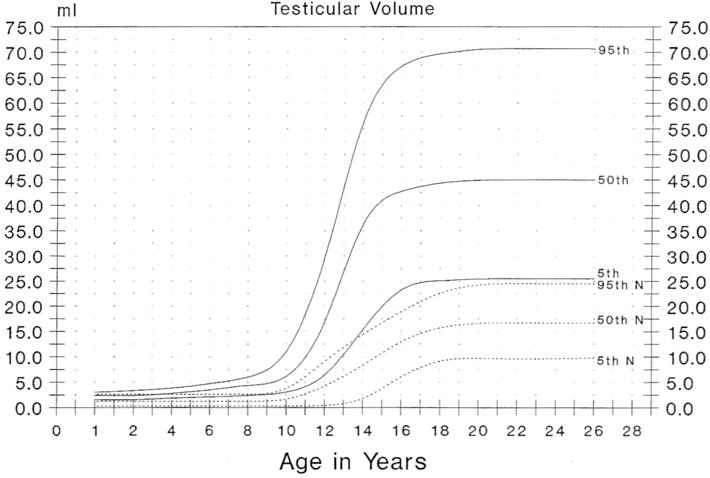
Standardized curves for testicular volume of males with fragile X syndrome (solid line) and normal individuals (broken line).
DISCUSSION
There are several abnormal physical parameters in males with the fragile X syndrome, particularly large ears and testicles, but frequently individuals with this syndrome are also reported to be obese and have a relatively large head size before puberty. These abnormal parameters can readily be appreciated after comparing our fragile X syndrome standards with the standardized curves developed from measurements of unaffected males. Specifically, the large ear length and testicular volume for all ages, proneness to obesity between 12 and 20 years of age, and a large-appearing head between 6 months and 6 years can be observed after analyzing the standardized curves.
Anthropometric standards have been developed for several syndromes17,22,23 and have been used successfully in the medical management of patients. The use of standards has become routine in most clinical genetics centers for monitoring growth and development of patients with specific, previously diagnosed syndromes, but they may also help in establishing the diagnosis in suspected individuals, particularly in younger patients. As for the fragile X syndrome, these standards may assist in identifying those males for fragile X chromosome analysis who may have the fragile X syndrome with or without a family history of mental retardation. We encourage the use of these standards in the evaluation of the fragile X syndrome in males and the comparison of these patients with other similarly affected individuals.
Fig 2.
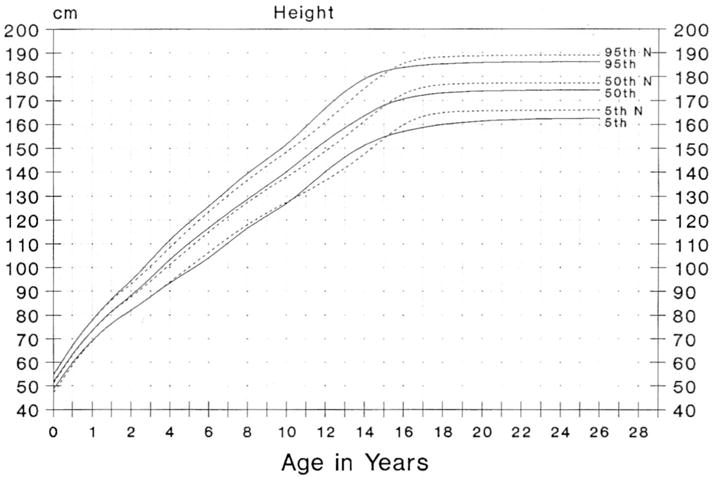
Standardized curves for height of males with fragile X syndrome (solid line) and normal individuals (broken line).
Fig 3.
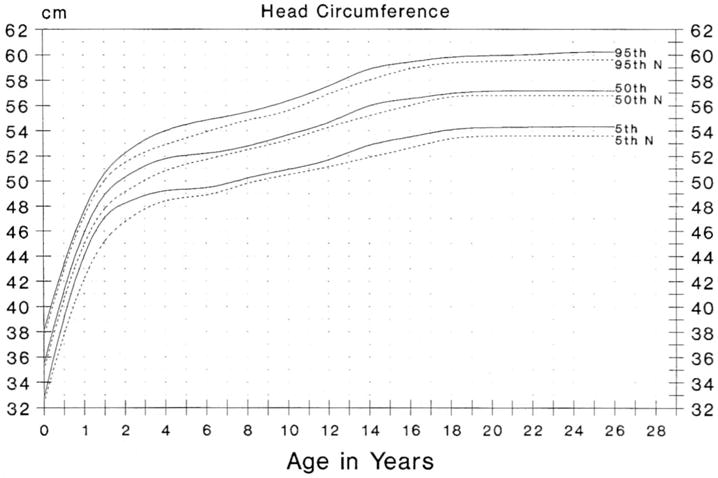
Standardized curves for head circumference of males with fragile X syndrome (solid line) and normal individuals (broken line).
Fig 4.
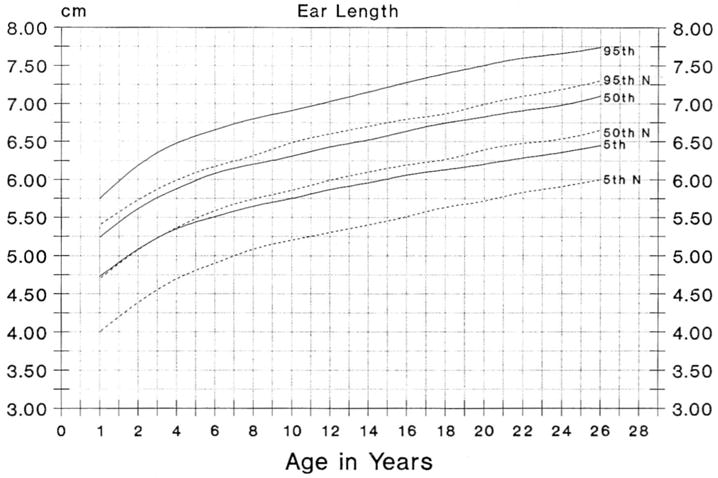
Standardized curves for ear length of males with fragile X syndrome (solid line) and normal individuals (broken line).
Acknowledgments
This research was partially supported by a grant from the Tennessee Department of Mental Health and Mental Retardation and was also supported by the Children’s Hospital Kempe Research Center.
We thank Pamela Grimm for expert preparation of the manuscript and Amy Cronister Silverman and Claire Hull for their assistance.
References
- 1.Hagerman RJ. Fragile X syndrome. Curr Probl Pediatr. 1987;17:621–674. doi: 10.1016/0045-9380(87)90011-9. [DOI] [PubMed] [Google Scholar]
- 2.Yu S, Pritchard M, Kremer E, et al. Fragile X genotype characterized by an unstable region of DNA. Science. 1991;252:1179–1181. doi: 10.1126/science.252.5009.1179. [DOI] [PubMed] [Google Scholar]
- 3.Oberlé I, Rousseau F, Heitz D, et al. Instability of a 550-base pair DNA segment and abnormal methylation in fragile X syndrome. Science. 1991;252:1097–1102. doi: 10.1126/science.252.5009.1097. [DOI] [PubMed] [Google Scholar]
- 4.Verkerk AJMH, Pieretti M, Sutcliffe JS, et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell. 1991;65:905–914. doi: 10.1016/0092-8674(91)90397-h. [DOI] [PubMed] [Google Scholar]
- 5.Hagerman RJ, Berry R, Jackson AW, Campbell J, Smith ACM, McGavran L. Institutional screening for the fragile X syndrome. AJDC. 1988;142:1216–1221. doi: 10.1001/archpedi.1988.02150110094028. [DOI] [PubMed] [Google Scholar]
- 6.Butler MG, Allen GA, Haynes JL, Singh DN, Watson MS, Breg WR. Anthropometric comparison of mentally retarded males with and without the fragile X syndrome. Am J Med Genet. 1991;38:260–268. doi: 10.1002/ajmg.1320380220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Butler MG, Mangrum T, Gupta R, Singh D. A 15 item checklist for screening mentally retarded males for the fragile X syndrome. Clin Genet. 1991;39:347–354. doi: 10.1111/j.1399-0004.1991.tb03041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Partington MW. The fragile X syndrome II: preliminary data on growth and development in males. Am J Med Genet. 1984;17:175–194. doi: 10.1002/ajmg.1320170111. [DOI] [PubMed] [Google Scholar]
- 9.Meryash DL, Cronk CE, Sachs B, Gerald PS. An anthropometric study of males with the fragile X syndrome. Am J Med Genet. 1984;17:159–174. doi: 10.1002/ajmg.1320170110. [DOI] [PubMed] [Google Scholar]
- 10.Loesch DZ, Lafranchi M, Scott D. Anthropometry of Martin-Bell syndrome. Am J Med Genet. 1988;30:149–164. doi: 10.1002/ajmg.1320300113. [DOI] [PubMed] [Google Scholar]
- 11.Butler MG, Allen GA, Singh DN, Carpenter NJ, Hall BD. Preliminary communication: photoanthropometric analysis of individuals with the fragile X syndrome. Am J Med Genet. 1988;30:165–168. doi: 10.1002/ajmg.1320300114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Butler MG, Fletcher M, Gale DD, et al. Metacarpophalangeal pattern profile analysis in fragile X syndrome. Am J Med Genet. 1988;31:767–773. doi: 10.1002/ajmg.1320310406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sutherland GR, Hecht F. Fragile Sites on Human Chromosomes. Oxford, England: Oxford University Press; 1985. p. 13. (Oxford Monograph on Medical Genetics). [Google Scholar]
- 14.Saul RA. Proceedings of the Greenwood Genetic Center. Vol. 7 Clinton, SC: Jacobs Press; 1988. [Google Scholar]
- 15.National Center for Health Statistics. Vital and Health Statistics. Washington, DC: US Government Printing Office; 1973. Selected body measurements of children 6–11 years, United States. (Series 11, No. 123). US Dept of Health, Education, and Welfare publication 73–1605. [Google Scholar]
- 16.Brandt JM, Allen GA, Haynes JL, Butler MG. Normative standards and comparison of anthropometric data of white and black newborn infants. Dysmorph Clin Genet. 1990;4:121–137. [PMC free article] [PubMed] [Google Scholar]
- 17.Butler MG, Meaney J. Standards for selected anthropometric measurements in Prader-Willi syndrome. Pediatrics. 1991;88:853–860. [PMC free article] [PubMed] [Google Scholar]
- 18.Snyder RG, Schneider LW, Owings CL, Reynolds HM, Gollomb DH, Schork MA, editors. Anthropometry of Infants, Children and Youths to Age 18 for Product Safety Design SP-450. Warrendale, PA: Society of Automobile Engineers Inc; 1977. [Google Scholar]
- 19.Goodman RM, Gorlin RJ. Atlas of the Face in Genetic Disorders. St Louis, MO: CV Mosby Co; 1977. [Google Scholar]
- 20.Malina RM, Roche AF. Physical Performance. Vol. 2. New York, NY: Plenum Press; 1983. Manual of Physical Status and Performance in Childhood. [Google Scholar]
- 21.Laron Z, Zilka E. Compensatory hypertrophy of testicle in unilateral cryptorchidism. J Clin Endocrinol Metab. 1969;29:1409. doi: 10.1210/jcem-29-11-1409. [DOI] [PubMed] [Google Scholar]
- 22.Meaney FJ, Farrer LA. Clinical anthropometry and medical genetics: a compilation of body measurements in genetic and congenital disorders. Am J Med Genet. 1986;25:343–359. doi: 10.1002/ajmg.1320250221. [DOI] [PubMed] [Google Scholar]
- 23.Hall JG, Froster-Iskenius UG, Allanson JE, editors. Handbook of Normal Physical Measurements. Oxford, England: Oxford University Press; 1989. [Google Scholar]


