Abstract
Supplemental Digital Content is available in the text.
We present our increasing experience using blunt tipped filler cannulas for local anesthesia infiltration to minimize pain and bruising during upper lid blepharoplasty. Avoiding injection pain enables the patient to enjoy the benefits of wide awake surgery without the inconveniences of sedation. We present educational videos on how to perform the local anesthetic infiltration using blunt tipped cannulas, the blepharoplasty procedure itself on a wide awake patient, and a video on the patient's perspective of wide awake blepharoplasty.
Upper lid blepharoplasty is typically performed using local anesthesia with or without sedation.1 Many surgeons still prefer to use sedation to decrease patient discomfort with the local injection and the procedure. We present our increasing experience2 using blunt tipped filler cannulas for local anesthesia infiltration to minimize pain and bruising. Avoiding injection pain enables the patient to enjoy the benefits of wide awake surgery without the inconveniences of sedation. We have performed over 30 upper lid blepharoplasties with this technique.
We used a blunt tipped cannula for painless local anesthesia infiltration (see video, Supplemental Digital Content 1, which displays blunt tipped cannula for painless local anesthetic infiltration technique for wide awake upper lid blepharoplasty, http://links.lww.com/PRSGO/A433).
Video Graphic 1.

See video, Supplemental Digital Content 1, which displays blunt tipped cannula for painless local anesthetic infiltration technique for wide awake upper lid blepharoplasty. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A433.
A 30-gauge needle is used to inject 0.25–0.5 ml of local at the lateral most extent of the planned skin excision.
Firmly pinching the entry site skin distracts the pain nerves stimulated by the needle poke. We have observed that needles hurt less if the skin is pinched into the needle rather than pushing the needle into the skin.
We numb both lateral eyelids with this initial bleb of local. We then insert a 20-gauge needle in the first numbed side to make a skin hole in which we easily insert the blunt 27-gauge 1.5 inch filler cannula (see video, Supplemental Digital Content 2, which displays the authors using a blunt tipped cannula for local anesthesia infiltration, http://links.lww.com/PRSGO/A434).
Video Graphic 2.
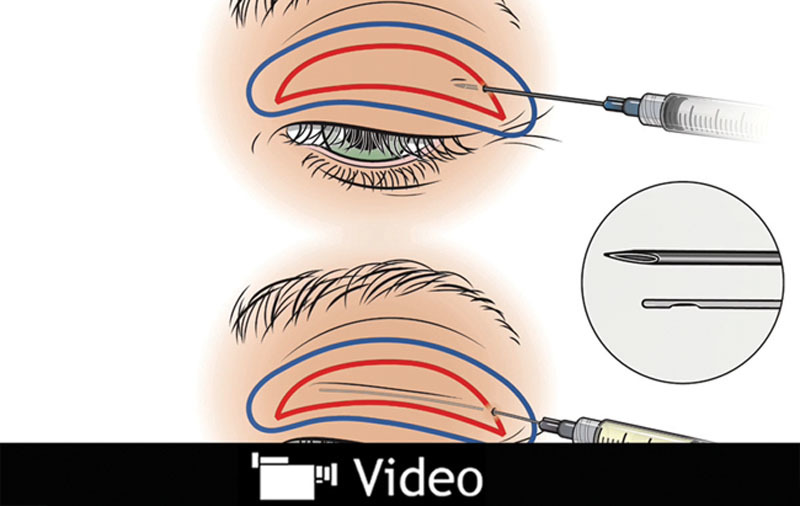
See video, Supplemental Digital Content 2, which displays the authors using a blunt tipped cannula for local anesthesia infiltration. After numbing the area, create an introducer puncture with a large gauge needle, then introduce the cannula through this hole. The tumescent fluid injected (blue) should extend beyond the planned surgical incisions (red). This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A434.
The cannula slides through fat unless it becomes obstructed by ligaments, in which case we back up and bypass the obstruction by heading in a slightly different direction. Unlike sharp needle tips, cannulas do not lacerate nerves and vessels. They therefore decrease pain and bruising.
We use buffered room temperature local anesthesia, slow infiltration, and encourage patient feedback.3
We routinely use 3–6 ml of 1% lidocaine with 1:100,000 epinephrine buffered 10 ml:1 ml with 8.4% bicarbonate and a small amount of bupivacaine per side. We add 1 ml of 0.05% bupivacaine with 1:200,000 epinephrine to 10 ml of the lidocaine/bicarbonate mixture in a 10 ml syringe.
Wide awake upper blepharoplasty procedure (see video, Supplemental Digital Content 3, which displays the authors performing an upper blepharoplasty procedure without sedation, http://links.lww.com/PRSGO/A435):
Video Graphic 3.

See video, Supplemental Digital Content 3, which displays the authors performing an upper blepharoplasty procedure without sedation. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A435.
Waiting 30 minutes after the injection of the local anesthetic before starting the surgery is important. Half an hour of waiting has been shown to produce one-third the blood loss of waiting only 7 minutes.4 The patient may go to the restroom during this waiting period.
We use surgical procedure time to educate the fully alert patient and give them postoperative instructions to decrease complications.
Bipolar cautery hurts less than monopolar cautery.
Fat pads can be anesthetized by injecting more local with either sharp needles or blunt cannulas.
The patient sits upright during surgery to ensure a good result against gravity when ptosis repair is required.
Patient satisfaction is high with wide awake blepharoplasty (see video, Supplemental Digital Content 4, which displays a patient’s perspective after undergoing wide awake upper blepharoplasty, http://links.lww.com/PRSGO/A436).
Video Graphic 4.

See video, Supplemental Digital Content 4, which displays a patient’s perspective after undergoing wide awake upper blepharoplasty. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A436.
Avoiding sedation provides many patient benefits in addition to considerably reduced cost.5
They do not suffer the inconveniences of intravenous insertion, preoperative testing, postoperative nausea and vomiting, and extra time in a recovery room. They simply get up and go home as they do after a dental procedure.
They do not need to fast or change medication schedules, which is particularly helpful in diabetics or patients with comorbidities.
PATIENT CONSENT
The patient provided written consent for the use of her image.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Friedland JA, Lalonde DH, Rohrich RJ. An evidence-based approach to blepharoplasty. Plast Reconstr Surg. 2010;126:2222–2229.. [DOI] [PubMed] [Google Scholar]
- 2.Lalonde D, Wong A. Local anesthetics: what’s new in minimal pain injection and best evidence in pain control. Plast Reconstr Surg. 2014;134(4 Suppl 2):40S–49S.. [DOI] [PubMed] [Google Scholar]
- 3.Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg. 2013;132:675–684.. [DOI] [PubMed] [Google Scholar]
- 4.McKee DE, Lalonde DH, Thoma A, et al. Optimal time delay between epinephrine injection and incision to minimize bleeding. Plast Reconstr Surg. 2013;131:811–814.. [DOI] [PubMed] [Google Scholar]
- 5.Lalonde DH, Price C, Wong AL, et al. Minimally painful local anesthetic injection for cleft lip/nasal repair in grown patients. Plast Reconstr Surg Glob Open. 2014;2:e171. [DOI] [PMC free article] [PubMed] [Google Scholar]


