Abstract
Objective
The purpose of this investigation was to examine the indirect effects of Integrative Cognitive-Affective Therapy (ICAT-BN) and Cognitive-Behavioral Therapy-Enhanced (CBT-E) on bulimia nervosa (BN) treatment outcome through three hypothesized maintenance variables: emotion regulation, self-directed behavior, and self-discrepancy.
Method
Eighty adults with BN were randomized to 21 sessions of ICAT-BN or CBT-E. A regression-based bootstrapping approach was used to test the indirect effects of treatment on outcome at end of treatment through emotion regulation and self-directed behavior measured at mid-treatment, as well as the indirect effects of treatment at follow-up through emotion regulation, self-directed behavior, and self-discrepancy measured at end of treatment.
Results
No significant differences in outcome between treatment conditions were observed, and no significant direct or indirect effects were found. Examination of the individual paths within the indirect effects models revealed comparable treatment effects. Across treatments, improvements in emotion regulation and self-directed behavior between baseline and mid-treatment predicted improvements in global eating disorder scores but not binge eating and purging frequency at end of treatment. Baseline to end of treatment improvements in emotion regulation and self-directed behavior also predicted improvements in global eating disorder scores at follow-up. Baseline to end of treatment improvements in emotion regulation predicted improvements in binge eating and baseline to end of treatment increases in positive self-directed behavior predicted improvements in purging at follow-up.
Discussion
These findings suggest that emotion regulation and self-directed behavior are important treatment targets and that ICAT-BN and CBT-E are comparable in modifying these psychological processes among individuals with BN.
Keywords: bulimia nervosa, integrative cognitive-affective therapy, cognitive-behavioral therapy, emotion regulation, emotion-focused therapy
Several efficacious treatments for bulimia nervosa (BN) have been identified,1,2 including cognitive-behavioral therapy (CBT3) and its updated enhanced version (CBT-E4,5). Recently, integrative cognitive-affective therapy for bulimia nervosa (ICAT-BN6), a newly developed psychotherapy treatment, was found to not differ from CBT-E in a randomized controlled trial.6 ICAT-BN is an emotion-focused individual psychotherapy treatment based on a conceptual model that emphasizes the role of momentary emotion in the maintenance of bulimic symptoms.7,8,9,10
The central role of emotion regulation in ICAT-BN is based on research demonstrating that individuals with BN display greater emotion dysregulation than controls,11,12 and that higher levels of emotion dysregulation in BN are associated with greater levels of eating disorder psychopathology.12,13 To target emotion dysregulation, ICAT-BN aims to modify several psychological factors that are hypothesized to precipitate momentary negative emotion associated with bulimic behavior, including self-directed behavior and self-discrepancy.9,10 Self-directed behavior (also described as introjects by Benjamin14,15) refers to coping strategies directed toward the self and includes both positive (e.g., self-acceptance, self-protection) and negative (e.g., self-attack, self-neglect, self-control) behaviors. For example, self-control strategies may be characterized by excessive dietary restriction in the form of fasting, and self-attack may be exhibited by the expression of intense self-criticism. Previous empirical examination of the ICAT model indicated that individuals with BN scored higher on a measure of negative self-directed behavior and lower on positive self-directed behavior than non-eating disorder control participants.8 Self-discrepancy was originally conceptualized by Higgins16 as the differences between perceptions of the “actual” self (i.e., how the individual believes they actually are) and the “ideal” self (i.e., how the individual ideally desires to be) or “ought” self (i.e., how the individual believes they must be). Self-discrepancy has been targeted successfully in the treatment of depression,17 has been found to be higher among individuals with BN than non-eating disorder control participants,8 and has been observed to correlate with bulimic symptoms and negative body image.18
Although resembling ICAT-BN in its initial emphasis on self-monitoring, behavioral techniques, and planned meal and snack consumption, CBT-E differs from ICAT-BN in its explicit focus on reducing dietary restraint, shape and weight checking, and dominance of shape, weight, and eating control in self-evaluation. In addition, although instruction in mood tolerance is included for a subgroup of individuals whose eating behaviors are clearly linked with negative affect, CBT-E focuses on problem-solving of emotion-related events rather than experiencing and identifying momentary emotions. Unlike ICAT-BN, CBT-E does not conceptualize momentary emotion as a central maintenance factor in BN. In summary, ICAT-BN was designed to include aspects of cognitive-behavioral treatment thought to be especially effective in treating BN (including self-monitoring, planned meal consumption, and relapse prevention). However, the two treatments are based on different conceptual models of psychopathology with ICAT-BN targeting emotion regulation, self-directed behavior, and self-discrepancy and CBT-E targeting dietary restraint, body checking/avoidance, and over-evaluation of shape and weight.
In a recent randomized controlled trial comparing ICAT-BN to CBT-E, both treatments were associated with significant improvements in treatment outcome for eating disorder symptoms as well as hypothesized maintenance mechanisms (e.g., emotion regulation, self-discrepancy, and self-directed behavior) at end of treatment and follow-up, with no significant differences between these two treatments.6 These findings are notable because ICAT-BN and CBT-E are based on different theoretical models of psychopathology and target unique mechanisms of change, but they both appear to be potentially efficacious for the treatment of BN as well as putative maintenance mechanisms. However, the mechanisms by which these treatments work and their impact on hypothesized maintenance variables are unclear. Examining mediational effects is an especially useful way of identifying how changes in hypothesized psychopathology mechanisms are associated with treatment outcome. Traditional mediational analysis as described by Baron and Kenny19 involves a series of steps in which associations within the hypothesized mediational framework are examined. The first step requires establishing a significant total effect of the independent variable (e.g., treatment type) on the dependent variable (e.g., outcome); additional effects are tested only if this total effect is significant. However, more modern bootstrapping-based approaches20 facilitate the examination of indirect effects (e.g., the effect of an independent variable on a dependent variable through a mediating variable) even in the absence of a significant total effect. Characterizing potential indirect effects within a mediational model can be particularly informative when different treatments are associated with comparable outcomes. Identifying these treatments’ influence on putative maintenance mechanisms of psychopathology is especially critical to determine how these particular treatments may work as well as to improve and develop more effective interventions.21,22
In summary, understanding how treatments work through an examination of hypothesized underlying mechanisms is essential for strengthening existing treatments, developing new efficacious treatments, and delineating psychopathology maintenance mechanisms that can be targeted in treatment. The primary objective of this investigation was to examine the indirect effects within the mediation model of BN treatment type (i.e., ICAT-BN versus CBT-E) on outcome through putative psychological maintenance variables. Given the theoretical differences between the two treatments, 10 it was hypothesized that significant indirect effects of treatment type on outcome would be observed. Specifically, it was hypothesized that there would be a stronger indirect effect of ICAT-BN (versus CBT-E) on eating disorder treatment outcome at end of treatment (as measured by binge eating, purging, and global eating disorder psychopathology) through changes in emotion regulation and self-directed behavior between mid-treatment and end of treatment. Similarly, it was hypothesized that there would be a stronger indirect effect of ICAT-BN (versus CBT-E) on treatment outcome at 4-month follow-up through changes between baseline and end of treatment measures of emotion regulation, self-directed behavior, and self-discrepancy.
Method
Participants
As described previously in the main treatment outcome results,6 participants included 80 adults (average age = 27.3 years, SD = 9.6; average BMI = 23.9 kg/m2, SD = 5.5; 87.5% Caucasian; 90% female; 45.0% college degree or higher) recruited from community and clinical settings at two USA sites: Fargo, North Dakota and Minneapolis, Minnesota. Participants met either full- or subthreshold DSM-IV23 criteria for BN as diagnosed by the Eating Disorder Examination (EDE).24 Although the majority of participants met full DSM-IV criteria (72.5%), a minority (27.5%) were diagnostically subthreshold in that they reported weekly compensatory behaviors accompanied by either subjective bulimic episodes or by objective bulimic episodes that occurred less than twice per week. Potential participants were excluded if they were pregnant or lactating, had a past or present diagnosis of psychosis or bipolar disorder, had a current diagnosis of substance abuse or dependence, had recent changes in psychotropic medication, had a measured BMI of less than 18 kg/m2, or were medically unstable, at acute risk of suicide, or receiving current psychotherapy.
Assessment and Measures
The EDE24 is an investigator-based interview used to assess eating disorder symptoms that includes four subscales (restraint, eating concern, shape concern, weight concern), a global severity score, and a diagnostic algorithm for DSM-IV BN diagnosis. The EDE has extensive psychometric data supporting its reliability and validity. 4,25 Trained interviewers were blind to participant randomization status. Inter-rater reliability based on a subsample of 20% of study participants selected at random indicated reliability ratings of 0.95 to 0.98 on EDE subscales.6 Cronbach’s alphas for the EDE global scores were .85 at baseline, .85 at end of treatment, and .88 at 4-month follow-up. EDE binge eating (i.e., frequency of objective bulimic episodes) and purging frequency as well as the global score were used as measures of treatment outcome at end of treatment and 4-month follow-up.
The Difficulties in Emotion Regulation Scale (DERS26) is a widely used, 36-item measure of emotion regulation that includes six subscales: non-acceptance of emotional responses, difficulties engaging goal-directed behavior when distressed, difficulties with impulse control when distressed, lack of emotional awareness, limited access to emotion regulation strategies, and lack of emotional clarity. The reliability and validity of the DERS have been demonstrated in samples of individuals with eating disorders.27,28 The DERS total score was used as a measure of emotion regulation at baseline, session #14 (mid-treatment), and end of treatment.
The Structural Analysis of Social Behavior Intrex questionnaire, short form29 is an eight-item measure that was used to examine changes in positive self-directed behavior (i.e., the tendency to accept, value, and appreciate one’s self) and negative self-directed behavior (i.e., the tendency to attack, reject, and blame one’s self). Previous data support the reliability and validity of this version of the Intrex.30 In this study, the positive and negative self-directed behavior items were administered at baseline, session #14 (mid-treatment), and end of treatment.
The Selves Interview31 was designed to measure self-discrepancy, including the difference between the actual-ideal and the actual-ought selves. During the interview, participants are asked to generate words associated with their actual, ideal, and ought selves. This measure was scored based on procedures designed by Higgins and colleagues.32 Previous research on the reliability of self-discrepancies using this interview observed an intra-class correlation of .86 for a sample that included individuals with BN.8 For these analyses, changes in the actual-ought and the actual-ideal discrepancies were examined between baseline and end of treatment only (because this interview was not administered at session #14).
Treatments
Participants were randomized to 21, 50-minute sessions of ICAT or CBT-E (focused) over 17 weeks, with sessions held twice weekly for the first month then weekly for the remainder of treatment. As described previously,6,9 ICAT-BN includes four phases. The first phase emphasizes motivation as well as the importance of emotions. The second phase focuses on meal planning for nutritional rehabilitation, adaptive coping for managing urges, and continuing to identify eating-related emotions. The third phase emphasizes emotion regulation including changing bulimic behaviors in the context of momentary negative emotions and reducing precipitants of negative emotion including self-discrepancy, interpersonal patterns, and self-directed behaviors. The final phase of treatment focuses on healthy lifestyle planning and relapse prevention. Similarly, CBT-E4 includes four stages. The first stage emphasizes engagement, psychoeducation, alternative behaviors, planned meals/snacks, weekly weighing, and self-monitoring. The second brief stage includes an evaluation of progress and plans for the third stage. The third stage of CBT-E targets dietary restraint/restriction, shape checking, feeling fat, self-evaluation, mood intolerance, and problem-solving. The final stage of CBT-E focuses on relapse prevention and maintenance plans.
Experienced doctoral-level clinicians provided both ICAT-BN and CBT-E. For both treatments, therapists were trained initially in a didactic session and participated in weekly supervision. A random selection of therapy session audiotapes was coded at an independent site at the University of Wisconsin and indicated high levels of adherence for both treatments.6 Participants were randomized in blocks of four, stratified by site, therapist, and diagnosis (full-versus subthreshold BN).
This study was approved by the institutional review boards at each institution.
Statistical Analysis
A regression-based bootstrapping approach19 (5,000 bias-corrected resamples, 95% confidence intervals) was used to examine the hypothesized indirect effects. This approach has several benefits over the traditional causal steps approach, including greater statistical power and the ability to test for significant indirect (i.e., mediational) effects in the absence of a significant total (i.e., main) effect. Two sets of indirect effect analyses were conducted, with treatment type included as the independent variable and baseline treatment outcome score (e.g., EDE global, binge eating, purging) included as a covariate in each set of analyses. In the first set, change scores reflecting the difference between baseline and session #14 (mid-treatment) for the DERS total score and the Intrex positive and negative self-directed behavior scores were calculated and served as the mediating variables, with the treatment outcome score at end of treatment used as the dependent variable. Measures from the treatment mid-point were selected rather than those from session #8 to ensure that participants had received at least a portion of the third phase of ICAT-BN treatment in which self-directed behaviors and emotion regulation are targeted as precipitants of negative affect. For the second set of analyses, change scores between baseline and end of treatment for the DERS total score, the Intrex positive and negative self-directed behavior scores, and the Selves Interview actual-ought and actual-ideal discrepancy scores were calculated and served as the mediating variables, with treatment outcome at 4-month follow-up as the dependent variable. The use of the change scores between baseline and end of treatment provided a separate examination by which the impact of receiving the full “dose” of treatment on outcome at follow-up could be examined. Analyses were conducted using the PROCESS macro for SPSS, and indirect effect estimates were interpreted as significant if the corresponding confidence intervals did not contain zero. Significance level was set at <.01 given the number of models examined. Sample size determination was based on the methods described by Fritz and MacKinnon.33 Based upon the bias-corrected bootstrap method that was used in the current paper, a sample size of 71 provides adequate power (.80) to detect a medium effect (.39) for both paths (i.e., a & b) of the indirect effect.
Results
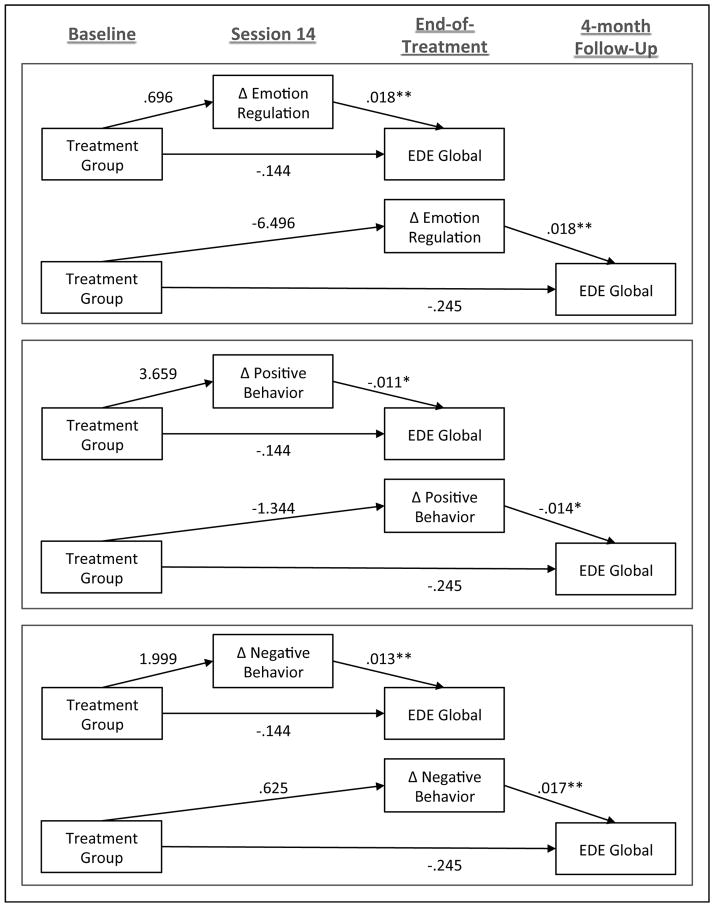
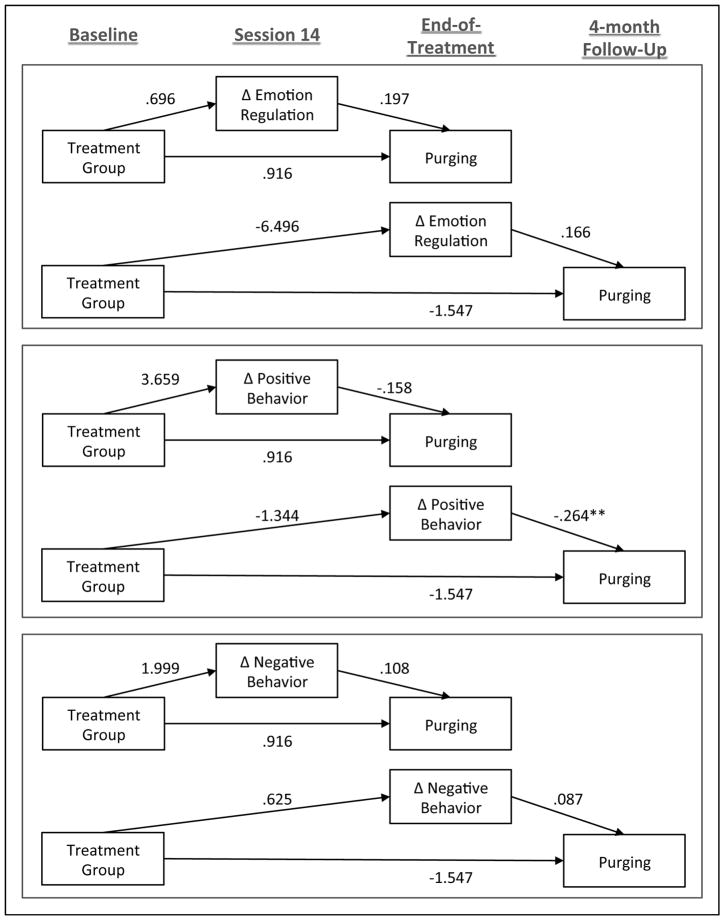
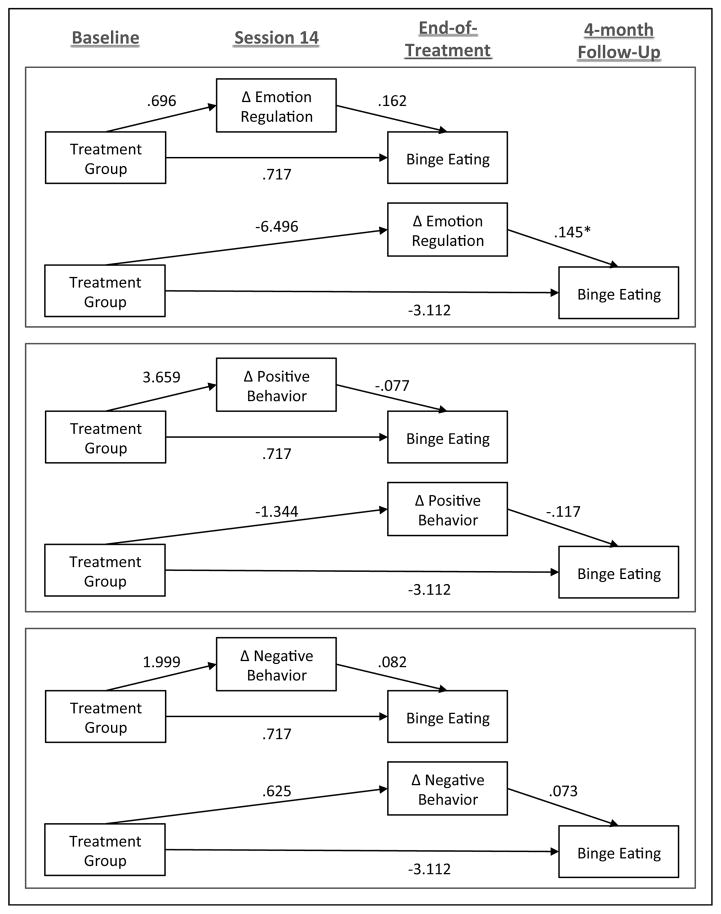
Of the 80 participants, 64 (80%) (n = 34, 85% of ICAT participants; n = 30, 75% of CBT-E participants, no significant differences in attrition) completed treatment. As shown in Tables 1 – 4 (and Tables 4 and 5 as supplemental materials in the online appendix), none of the indirect effects that were tested were found to be significant. As a result, the separate paths comprising each of the indirect effect models were examined (see Tables 1–4 and Figures 1–3 as well as Tables 5 and 6 in the online appendix): the a path (independent variable to mediator; i.e., association between treatment type and change in hypothesized psychological variable), the b path (mediator to dependent variable; i.e., association between change in hypothesized psychological variable and outcome), the c path (total effect of independent variable on dependent variable; i.e., association between treatment condition and outcome), and the c′ path (direct effect of independent variable on dependent variable; e.g., association between treatment condition and outcome, controlling for change in hypothesized psychological variable).
Table 1.
Indirect effects of change in emotion regulation (DERS) and self-directed behavior (Intrex) from baseline to session 14 on the association between treatment and eating disorder psychopathology (EDE-Global) at end of treatment
| Mediator | Path | Coefficient/Effect | SE | t | p | 95% CI
|
|
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Δ Emotion Regulation (BL to Session 14; DERS) | a | 0.696 | 4.183 | 0.166 | 0.868 | −7.631 | 9.023 |
| b | 0.018 | 0.005 | 3.723 | <.001 | 0.009 | 0.028 | |
| c | −0.144 | 0.196 | −0.734 | 0.466 | −0.533 | 0.246 | |
| Total | −0.144 | 0.196 | −0.734 | 0.466 | −0.533 | 0.246 | |
| Direct | −0.158 | 0.181 | −0.873 | 0.385 | −0.519 | 0.203 | |
| Indirecta | 0.013 | 0.079 | −0.123 | 0.195 | |||
|
| |||||||
| Δ Positive Behavior (BL to Session 14; Intrex) | a | 3.659 | 5.881 | 0.622 | 0.536 | −8.049 | 15.367 |
| b | −0.011 | 0.004 | −2.926 | 0.005 | −0.018 | −0.003 | |
| c | −0.144 | 0.196 | −0.734 | 0.466 | −0.533 | 0.246 | |
| Total | −0.144 | 0.196 | −0.734 | 0.466 | −0.533 | 0.246 | |
| Direct | −0.109 | 0.187 | −0.581 | 0.563 | −0.482 | 0.264 | |
| Indirecta | −0.039 | 0.066 | −0.184 | 0.079 | |||
|
| |||||||
| Δ Negative Behavior (BL to Session 14; Intrex) | a | 1.999 | 4.625 | 0.432 | 0.667 | −7.209 | 11.207 |
| b | 0.013 | 0.005 | 2.676 | 0.009 | 0.003 | 0.023 | |
| c | −0.144 | 0.196 | −0.734 | 0.466 | −0.533 | 0.246 | |
| Total | −0.144 | 0.196 | −0.734 | 0.466 | −0.533 | 0.246 | |
| Direct | −0.178 | 0.189 | −0.942 | 0.349 | −0.554 | 0.198 | |
| Indirecta | 0.026 | 0.067 | −0.092 | 0.183 | |||
Note. BL = Baseline. Session 14 = Treatment midpoint. DERS = Difficulties in Emotion Regulation Scale. Intrex = Structural Analysis of Social Behavior INTREX questionnaire. EDE-Global = Eating Disorder Examination Global score. Significant results (α < .01) are bolded.
Number of bootstrap samples = 5,000
Table 4.
Indirect effects of change in emotion regulation, self-directed behavior, and self-discrepancy from baseline to end of treatment on the association between treatment and eating disorder pathology (EDE-Global) at 4-month follow-up
| Mediator | Path | Coefficient/Effect | SE | t | p | 95% CI
|
|
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Δ Emotion Regulation (BL to EOT; DERS) | a | −6.496 | 4.851 | −1.339 | 0.184 | −16.155 | 3.162 |
| b | 0.018 | 0.005 | 3.622 | <.001 | 0.008 | 0.027 | |
| c | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Total | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Direct | −0.132 | 0.212 | −0.622 | 0.536 | −0.553 | 0.290 | |
| Indirecta | −0.115 | 0.094 | −0.333 | 0.043 | |||
|
| |||||||
| Δ Positive Behavior (BL to EOT; Intrex) | a | −1.344 | 5.526 | −0.243 | 0.808 | −12.347 | 9.658 |
| b | −0.014 | 0.004 | −3.160 | 0.002 | −0.023 | −0.005 | |
| c | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Total | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Direct | −0.267 | 0.213 | −1.253 | 0.214 | −0.692 | 0.158 | |
| Indirecta | 0.019 | 0.080 | −0.123 | 0.208 | |||
|
| |||||||
| Δ Negative Behavior (BL to EOT; Intrex) | a | 0.625 | 5.467 | 0.114 | 0.909 | −10.258 | 11.509 |
| b | 0.017 | 0.005 | 3.610 | <.001 | 0.007 | 0.026 | |
| c | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Total | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Direct | −0.267 | 0.210 | −1.273 | 0.207 | −0.684 | 0.151 | |
| Indirecta | 0.010 | 0.096 | −0.187 | 0.205 | |||
|
| |||||||
| Δ Actual-Ideal Discrepancy (BL to EOT; SELVES) | a | 0.150 | 0.727 | 0.206 | 0.838 | −1.298 | 1.598 |
| b | 0.034 | 0.035 | 0.963 | 0.338 | −0.036 | 0.104 | |
| c | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Total | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Direct | −0.251 | 0.226 | −1.114 | 0.269 | −0.700 | 0.198 | |
| Indirecta | 0.005 | 0.038 | −0.050 | 0.126 | |||
|
| |||||||
| Δ Actual-Ought Discrepancy (BL to EOT; Selves) | a | −0.682 | 0.600 | −1.136 | 0.260 | −1.876 | 0.513 |
| b | 0.081 | 0.043 | 1.883 | 0.064 | −0.005 | 0.167 | |
| c | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Total | −0.245 | 0.225 | −1.089 | 0.280 | −0.694 | 0.203 | |
| Direct | −0.195 | 0.223 | −0.872 | 0.386 | −0.639 | 0.250 | |
| Indirecta | −0.055 | 0.070 | −0.283 | 0.023 | |||
Note. BL= Baseline. EOT = End of treatment. DERS = Difficulties in Emotion Regulation Scale. Intrex = Structural Analysis of Social Behavior INTREX questionnaire. Selves = Selves Interview. EDE-Global = Eating Disorder Examination Global score. Significant results (α < .01) are bolded.
Number of bootstrap samples = 5,000
Table 5.
Indirect effects of change in emotion regulation, self-directed behavior, and self-discrepancy from baseline to end of treatment on the association between treatment and binge eating (EDE) at 4-month follow-up
| Mediator | Path | Coefficient/ Effect | SE | t | p | 95% CI
|
|
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Δ Emotion Regulation (BL to EOT; DERS) | a | −6.496 | 4.851 | −1.339 | 0.184 | −16.155 | 3.162 |
| b | 0.145 | 0.050 | 2.913 | 0.005 | 0.046 | 0.245 | |
| c | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Total | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Direct | −2.168 | 2.161 | −1.003 | 0.319 | −6.472 | 2.136 | |
| Indirecta | −0.943 | 0.938 | −3.759 | 0.163 | |||
|
| |||||||
| Δ Positive Behavior (BL to EOT; Intrex) | a | −1.344 | 5.526 | −0.243 | 0.808 | −12.347 | 9.658 |
| b | −0.117 | 0.044 | −2.636 | 0.010 | −0.205 | −0.029 | |
| c | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Total | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Direct | −3.261 | 2.157 | −1.512 | 0.135 | −7.556 | 1.035 | |
| Indirecta | 0.157 | 0.677 | −1.120 | 1.752 | |||
|
| |||||||
| Δ Negative Behavior (BL to EOT; Intrex) | a | 0.625 | 5.467 | 0.114 | 0.909 | −10.258 | 11.509 |
| b | 0.073 | 0.046 | 1.590 | 0.116 | −0.018 | 0.164 | |
| c | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Total | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Direct | −3.155 | 2.216 | −1.424 | 0.159 | −7.569 | 1.259 | |
| Indirecta | 0.046 | 0.528 | −0.737 | 1.259 | |||
|
| |||||||
| Δ Actual-Ideal Discrepancy (BL to EOT; SELVES) | a | 0.150 | 0.727 | 0.206 | 0.838 | −1.298 | 1.598 |
| b | −0.252 | 0.349 | −0.722 | 0.473 | −0.948 | 0.444 | |
| c | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Total | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Direct | −3.074 | 2.245 | −1.369 | 0.175 | −7.546 | 1.398 | |
| Indirecta | −0.038 | 0.289 | −0.918 | 0.374 | |||
|
| |||||||
| Δ Actual-Ought Discrepancy (BL to EOT; Selves) | a | −0.682 | 0.601 | −1.136 | 0.260 | −1.878 | 0.513 |
| b | 0.479 | 0.422 | 1.135 | 0.260 | −0.361 | 1.318 | |
| c | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Total | −3.112 | 2.238 | −1.391 | 0.168 | −7.568 | 1.344 | |
| Direct | −2.788 | 2.252 | −1.238 | 0.220 | −7.273 | 1.697 | |
| Indirecta | −0.326 | 0.496 | −2.008 | 0.151 | |||
Note. BL = Baseline. EOT = End of treatment. DERS = Difficulties in Emotion Regulation Scale. Intrex = Structural Analysis of Social Behavior INTREX questionnaire. Selves = Selves Interview. EDE = Objective bulimic episodes (28 days). Significant results (α < .01) are bolded.
Number of bootstrap samples = 5,000
Figure 1.
Indirect effects of changes in emotion regulation and self-directed behavior on the association between treatment and eating disorder pathology as measured by the EDE Global score. A regression-based bootstrapping approach (5,000 bias-corrected resamples, 95% confidence intervals) was used to examine the hypothesized indirect effects, with treatment type included as the independent variable and baseline EDE global score included as a covariate in each set of analyses. For each of the three mediating variables, two models were conducted. In the first model, the mediating variable was defined as change from baseline to session 14 and the dependent variable was defined as EDE global score at end of treatment. In the second model, the mediating variable was defined as change from baseline to end of treatment and the dependent variable was defined as EDE global score at 4-month follow-up. The figure shows that, in all six models, only the b paths (mediator to dependent variable) were significant.
*p < .01
**p < .001
Figure 3.
Indirect effects of changes in emotion regulation and self-directed behavior on the association between treatment and eating disorder pathology as measured by purging (EDE). A regression-based bootstrapping approach (5,000 bias-corrected resamples, 95% confidence intervals) was used to examine the hypothesized indirect effects, with treatment type included as the independent variable and baseline EDE purging frequency included as a covariate in each set of analyses. For each of the three mediating variables, two models were conducted. In the first model, the mediating variable was defined as change from baseline to session 14 and the dependent variable was defined as EDE purging frequency at end of treatment. In the second model, the mediating variable was defined as change from baseline to end of treatment and the dependent variable was defined as EDE purging frequency at 4-month follow-up. The figure shows that, in all six models, only the b paths (mediator to dependent variable) were significant.
*p < .01
**p < .001
Table 6.
Indirect effects of change in emotion regulation, self-directed behavior, and self-discrepancy from baseline to end of treatment on the association between treatment and purging (EDE) at 4-month follow-up
| Mediator | Path | Coefficient/Effect | SE | t | p | 95% CI
|
|
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Δ Emotion Regulation (BL to EOT; DERS) | a | −6.496 | 4.851 | −1.339 | 0.184 | −16.155 | 3.162 |
| b | 0.166 | 0.080 | 2.073 | 0.042 | 0.007 | 0.325 | |
| c | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Total | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Direct | −0.470 | 3.444 | −0.137 | 0.892 | −7.330 | 6.390 | |
| Indirecta | −1.075 | 1.181 | −4.750 | 0.208 | |||
|
| |||||||
| Δ Positive Behavior (BL to EOT; Intrex) | a | −1.344 | 5.526 | −2.430 | 0.808 | −12.347 | 9.658 |
| b | −0.264 | 0.066 | −4.010 | <.001 | −3.960 | −0.133 | |
| c | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Total | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Direct | −1.908 | 3.181 | −0.600 | 0.551 | −8.243 | 4.428 | |
| Indirecta | 0.356 | 1.505 | −2.752 | 3.418 | |||
|
| |||||||
| Δ Negative Behavior (BL to EOT; Intrex) | a | 0.625 | 5.467 | 0.114 | 0.909 | −10.258 | 11.509 |
| b | 0.087 | 0.072 | 1.201 | 0.234 | −0.057 | 0.231 | |
| c | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Total | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Direct | −1.600 | 3.467 | −0.462 | 0.646 | −8.506 | 5.306 | |
| Indirecta | 0.054 | 0.589 | −0.893 | 1.741 | |||
|
| |||||||
| Δ Actual-Ideal Discrepancy (BL to EOT; SELVES) | a | 0.150 | 0.727 | 0.206 | 0.838 | −1.298 | 1.598 |
| b | 0.303 | 0.547 | 0.554 | 0.582 | −0.786 | 1.391 | |
| c | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Total | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Direct | −1.593 | 3.494 | −0.456 | 0.650 | −8.551 | 5.366 | |
| Indirecta | 0.045 | 0.435 | −0.577 | 1.377 | |||
|
| |||||||
| Δ Actual-Ought Discrepancy (BL to EOT; Selves) | a | −0.682 | 0.601 | −1.136 | 0.260 | −1.878 | 0.513 |
| b | 1.064 | 0.654 | 1.626 | 0.108 | −0.240 | 2.367 | |
| c | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Total | −1.547 | 3.477 | −0.445 | 0.658 | −8.471 | 5.377 | |
| Direct | −0.823 | 3.469 | −0.237 | 0.813 | −7.733 | 6.086 | |
| Indirecta | −0.723 | 0.792 | −2.992 | 0.276 | |||
Note. BL= Baseline. EOT = End of treatment. DERS = Difficulties in Emotion Regulation Scale. Intrex = Structural Analysis of Social Behavior INTREX questionnaire. Selves = Selves Interview. EDE = Purging episodes (28 days). Significant results (α < .01) are bolded.
Number of bootstrap samples = 5,000
Treatment condition (a paths) was not found to be associated with change in any of the mediator variables. Further, consistent with prior reported findings,6 no significant total or direct effects were observed for treatment condition (c and c′ paths, respectively). However, as shown in Table 1 and Figure 1, improvement in emotion regulation (DERS) from baseline to session #14 was associated with improvements in global eating disorder psychopathology (EDE global) at end of treatment. Similarly, improvements in both positive and negative self-directed behavior from baseline to session #14 as measured by the Intrex were associated with improvements in EDE global scores at end of treatment (all b paths). In contrast, changes in emotion regulation (DERS) and self-directed behaviors (Intrex) between baseline and session #14 were not significantly associated with changes in EDE binge eating or purging frequency at end of treatment (see Tables 3 and 4 as well as Figures 1 and 2).
Table 3.
Indirect effects of change in emotion regulation (DERS) and self-directed behavior (Intrex) from baseline to session 14 on the association between treatment and purging frequency (EDE) at end of treatment
| Mediator | Path | Coefficient/Effect | SE | t | p | 95% CI
|
|
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Δ Emotion Regulation (BL to Session 14; DERS) | a | 0.696 | 4.183 | 0.166 | 0.868 | 0.868 | 9.023 |
| b | 0.197 | 0.092 | 2.157 | 0.034 | 0.034 | 0.380 | |
| c | 0.916 | 3.453 | 0.265 | 0.792 | 0.792 | 7.791 | |
| Total | 0.916 | 3.453 | 0.265 | 0.792 | 0.792 | 7.791 | |
| Direct | 0.780 | 3.374 | 0.231 | 0.818 | 0.818 | 7.500 | |
| Indirecta | 0.137 | 0.887 | 2.125 | ||||
|
| |||||||
| Δ Positive Behavior (BL to Session 14; INTREX) | a | 3.659 | 5.881 | 0.622 | 0.536 | 0.536 | 15.367 |
| b | −0.158 | 0.066 | −2.388 | 0.019 | 0.019 | −0.026 | |
| c | 0.916 | 3.453 | 0.265 | 0.792 | 0.792 | 7.791 | |
| Total | 0.916 | 3.453 | 0.265 | 0.792 | 0.792 | 7.791 | |
| Direct | 1.488 | 3.361 | 0.443 | 0.659 | 0.659 | 8.181 | |
| Indirecta | −0.576 | 1.018 | 0.944 | ||||
|
| |||||||
| Δ Negative Behavior (BL to Session 14; INTREX) | a | 1.999 | 4.625 | 0.432 | 0.667 | 0.667 | 11.207 |
| b | 0.108 | 0.084 | 1.282 | 0.204 | 0.204 | 0.276 | |
| c | 0.916 | 3.453 | 0.265 | 0.792 | 0.792 | 7.791 | |
| Total | 0.916 | 3.453 | 0.265 | 0.792 | 0.792 | 7.791 | |
| Direct | 0.700 | 3.443 | 0.203 | 0.839 | 0.839 | 7.557 | |
| Indirecta | 0.216 | 0.639 | −0.632 | 2.067 | |||
Note. BL = Baseline. Session 14 = Treatment mid-point. DERS = Difficulties in Emotion Regulation Scale. Intrex = Structural Analysis of Social Behavior INTREX questionnaire. EDE = purging episodes (28 days). Significant results (α < .01) are bolded.
Number of bootstrap samples = 5,000
Figure 2.
Indirect effects of changes in emotion regulation and self-directed behavior on the association between treatment and eating disorder pathology as measured by binge eating (EDE objective bulimic episode frequency). A regression-based bootstrapping approach (5,000 bias-corrected resamples, 95% confidence intervals) was used to examine the hypothesized indirect effects, with treatment type included as the independent variable and baseline EDE binge eating included as a covariate in each set of analyses. For each of the three mediating variables, two models were conducted. In the first model, the mediating variable was defined as change from baseline to session 14 and the dependent variable was defined as EDE binge eating frequency at end of treatment. In the second model, the mediating variable was defined as change from baseline to end of treatment and the dependent variable was defined as EDE binge eating frequency at 4-month follow-up. The figure shows that, in all six models, only the b paths (mediator to dependent variable) were significant.
*p < .01
**p < .001
As shown in Table 4 and Figure 1, improvements in emotion regulation (DERS) from baseline to end of treatment were associated with improvements in EDE global scores at 4-month follow-up. In addition, increases in positive self-directed behavior and reductions in negative self-directed behavior from baseline to end of treatment as measured by the Intrex were associated with improvements in EDE global scores at 4-month follow-up (all b paths). For binge eating and purging frequency, improvements in emotion regulation (DERS) from baseline to end of treatment were associated with reductions in binge eating at 4-month follow-up. Improvements in positive self-directed behavior from baseline to end of treatment as measured by the Intrex were associated with improvements in purging at 4-month follow-up. No significant associations were found between changes in actual-ideal or actual-ought self-discrepancy (as measured by the Selves from baseline to end of treatment) and EDE global scores, binge eating, or purging at 4-month follow-up. In post-hoc exploratory analyses to test whether treatment moderated the b path between changes in mediators and outcome at end of treatment and follow-up, no significant effects were found.
Discussion
The results of this investigation were surprising in that they did not support the hypothesized indirect effects of treatment condition on outcome through changes in putative maintenance mechanisms based on the ICAT model (i.e., emotion regulation, self-directed behavior, and self-discrepancy). In order to further understand these findings, the individual paths within the model that comprise each of the indirect effects (i.e., the a and b paths) were examined. Examination of the a paths revealed no significant associations between treatment condition and changes in the hypothesized psychological mechanisms, indicating that both ICAT-BN and CBT-E produced comparable changes in these hypothesized psychological variables, as well as in treatment outcome.
The fact that changes in these psychological variables were non-specific to treatment may be the result of several factors. First, because ICAT-BN was intentionally designed to retain several components of previously established psychotherapeutic treatments for BN including CBT, some aspects of the treatment content were similar between the two conditions. Further, although ICAT-BN targets the specified psychological processes directly (i.e., emotion regulation, self-directed behavior), CBT-E’s emphasis on eliminating body checking behavior, using problem-solving strategies, and reducing the importance of shape and weight in self-evaluation may have a similar impact on these processes through mood enhancement, behavioral disconfirmation, and/or reductions in distress and self-oriented cognitions as a result of exposure. These overlaps in treatment content and the potentially similar effects on underlying mechanisms across ICAT-BN and CBT-E may explain the lack of differences observed in treatment outcomes. Changes in hypothesized mechanisms may have been the result of non-specific therapeutic factors that were similar in both treatments.34 Alternatively, these findings may have been impacted by potential moderators identified in a previous study.35 In addition, the lack of treatment effects may be a reflection of the study sample size and limited statistical power; future replication using a larger sample is needed to examine potential differences in treatment.
Examination of the b paths revealed that changes in two of the hypothesized psychological mechanisms—emotion regulation and self-directed behavior—were associated with treatment outcome as measured by global EDE scores across both treatment conditions. Specifically, baseline to mid-treatment improvements in emotion regulation, positive self-directed behavior, and negative self-directed behavior predicted improvements in eating disorder psychopathology at end of treatment. Similarly, changes in emotion regulation and self-directed behavior between baseline and end of treatment predicted improvements in eating disorder psychopathology at 4-month follow-up. Notably, the pattern of results was different when binge eating and purging frequencies were examined as outcome variables. Changes in emotion regulation and self-directed behavior between baseline and mid-treatment were not predictive of changes in binge eating and purging between baseline and end of treatment. However, changes in emotion regulation between baseline and end of treatment were predictive of changes in binge eating frequency at 4-month follow-up, and increases in positive self-directed behavior were predictive of change in purging frequency at 4-month follow-up. The differences in results depending on outcome variable suggest that changes in emotion regulation and self-directed behavior may have a more robust impact on eating disorder psychopathology related to dietary restraint and eating, weight, and shape concerns than on bulimic behaviors. Nonetheless, these findings suggest that treatments that impact emotion regulation and self-directed behavior may contribute to reductions in global eating disorder psychopathology, and, to some extent, bulimic behavior, and may be important clinical targets. In contrast, although the ICAT-BN model conceptualizes self-discrepancy as an important precipitant of negative momentary emotion that contributes to BN symptom maintenance,9 baseline to end of treatment changes in the discrepancy between perceptions of the actual-ideal self as well as the actual-ought self were not associated with outcome at 4-month follow-up. Because the Selves Interview was not administered during the course of treatment and changes were examined only for baseline to end of treatment, the possibility that changes in self-discrepancy between baseline and mid-treatment were associated with improvement at end of treatment could not be examined. Nonetheless, the fact that changes over the course of treatment were not associated with 4-month outcome suggests that further examination of self-discrepancy and whether it actually plays a significant role in the maintenance of BN is needed.
Several strengths of this study are notable, including the use of a multisite BN sample, a randomized design with assessors who were blind to treatment condition, the examination of changes in hypothesized psychological mechanisms at both mid-treatment and end of treatment, and the inclusion of individuals with both full and subthreshold BN which may increase the generalizability of the findings. However, several limitations are important to note in interpreting these results. First, the sample size was relatively small, limiting its generalizability and statistical power. Second, the study relied on self-report using interview and traditional questionnaire methods of assessment; future studies would be strengthened by the inclusion of additional methodologies to assess emotion regulation, self-directed behavior, and self-discrepancy (e.g., psychophysiological and ecological momentary assessment measures). Third, because only the overall DERS score was used in this study, further research is needed to examine changes in the DERS subscales in the course of treatment and their relationship to treatment outcome to better understand the role of identifying, accepting, understanding, and responding to emotions. Fourth, because changes may occur prior to mid-treatment, future research is needed to examine potential indirect effects related to changes that occur earlier in treatment. Fifth, this study was limited by the inclusion of hypothesized maintenance factors specified in the ICAT-BN model. Given that the EDE was not administered mid-treatment, putative maintenance variables specified by the CBT-E model (e.g., dietary restraint, over-evaluation of shape and weight) could not be examined. Finally, although significant, the fact that the predictive effects of changes in hypothesized mechanisms observed in the current study were relatively small underscores the need for replication.
In summary, although indirect effects were not observed, this study suggests that changes in emotion regulation and self-directed behavior over the course of treatment predict aspects of treatment outcome in BN in both ICAT-BN and CBT-E. These data support clinical efforts to impact these psychological processes using ICAT-BN and CBT-E as well as other potential treatments, such as dialectical behavioral therapy,36 compassion-focused therapy37 and emotion-focused therapy.38 In addition, this study highlights the importance of identifying and targeting putative BN maintenance mechanisms using current and developing treatments. Future investigations are needed to further delineate treatment-specific indirect effects to improve treatment efficacy.
Supplementary Material
Table 2.
Indirect effects of change in emotion regulation (DERS) and self-directed behavior (Intrex) from baseline to session 14 on the association between treatment and binge eating frequency (EDE) at end of treatment
| Mediator | Path | Coefficient/Effect | SE | t | p | 95% CI
|
|
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Δ Emotion Regulation (BL to Session 14; DERS) | a | 0.696 | 4.183 | 0.166 | 0.868 | 1.392 | 9.023 |
| b | 0.162 | 0.069 | 2.356 | 0.021 | 0.025 | 0.300 | |
| c | 0.717 | 2.608 | 0.275 | 0.784 | −4.476 | 5.910 | |
| Total | 0.717 | 2.608 | 0.275 | 0.784 | −4.476 | 5.910 | |
| Direct | 0.593 | 2.535 | 0.234 | 0.816 | −4.455 | 5.641 | |
| Indirecta | 0.113 | 0.753 | −1.266 | 1.982 | |||
|
| |||||||
| Δ Positive Behavior (BL to Session 14; Intrex) | a | 3.659 | 5.881 | 0.622 | 0.536 | −8.049 | 15.367 |
| b | −0.077 | 0.045 | −1.540 | 0.128 | −0.176 | 0.023 | |
| c | 0.717 | 2.608 | 0.275 | 0.784 | −4.476 | 5.910 | |
| Total | 0.717 | 2.608 | 0.275 | 0.784 | −4.476 | 5.910 | |
| Direct | 0.994 | 2.591 | 0.384 | 0.702 | −4.167 | 6.155 | |
| Indirecta | −0.281 | 0.508 | −1.653 | 0.505 | |||
|
| |||||||
| Δ Negative Behavior (BL to Session 14; Intrex) | a | 1.999 | 4.625 | 0.432 | 0.667 | −7.209 | 11.207 |
| b | 0.082 | 0.064 | 1.289 | 0.201 | −0.045 | 0.208 | |
| c | 0.717 | 2.608 | 0.275 | 0.784 | −4.476 | 5.910 | |
| Total | 0.717 | 2.608 | 0.275 | 0.784 | −4.476 | 5.910 | |
| Direct | 0.552 | 2.600 | 0.212 | 0.832 | −4.626 | 5.730 | |
| Indirecta | 0.164 | 0.551 | −0.444 | 1.843 | |||
Note. BL=Baseline. Session 14= Treatment mid-point. DERS=Difficulties in Emotion Regulation Scale. Intrex=Structural Analysis of Social Behavior INTREX questionnaire. EDE= Objective bulimic episodes (28 days). Significant results (α < .01) are bolded.
Number of bootstrap samples = 5,000
Acknowledgments
The authors with to thank Drs. Tricia Cook Myers, Kathryn Miller, and Lorraine Swan-Kremeier for serving as therapists on the study, Li Cao, M.S. and Ann Erickson for their contributions to data analysis, Nora Durkin, M.A., Scott Engel, Ph.D., Leah Jappe, Ph.D., and Heather Simonich, M.A., for their assistance with data collection, assessment interviewing, and manuscript preparation.
This study was supported by grants R01DK61912, R01DK 61973, and P30 DK 60456 from the National Institute of Diabetes and Digestive and Kidney Diseases, grants R34MH077571, R01MH059674, T32MH082761, K02 MH65919 from the National Institute of Mental Health, and the Neuropsychiatric Research Institute.
Ross Crosby, Ph.D., is a statistical consultant for Health Outcomes Solutions (Winter Park, Florida). Stephen Wonderlich, Ph.D., Carol Peterson, Ph.D., Tracey Smith, Ph.D., Marjorie Klein, Ph.D., James Mitchell, M.D., and Scott Crow, M.D., are co-authors of “Integrative Cognitive-Affective Therapy for Bulimia Nervosa: A Treatment Manual” (Guilford Press, 2015).
Clinical Trials.gov Identifier: NCT00773617
References
- 1.Kass AE, Kolko RP, Wilfley DE. Psychological treatments for eating disorders. Cur Opin Psychiatry. 2013;26:549–555. doi: 10.1097/YCO.0b013e328365a30e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute for Clinical Excellence. NICE Clinical Guideline No. 9. London: NICE; 2004. Eating Disorders – Core interventions in the treatment and management of anorexia nervosa, bulimia nervosa, related eating disorders. [Google Scholar]
- 3.Fairburn CG, Marcus MD, Wilson GT. Cognitive-behavioral therapy for binge eating and bulimia nervosa: A comprehensive treatment manual. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. New York: Guilford Press; 1993. pp. 361–404. [Google Scholar]
- 4.Fairburn CG. Cognitive behavior therapy and eating disorders. New York: Guilford; 2008. [Google Scholar]
- 5.Fairburn CG, Cooper Z, Doll H, O’Connor ME, Bohn K, Hawker DM, Wales JA, Palmer RL. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166:311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wonderlich SA, Peterson CB, Crosby RD, Smith TL, Klein MH, Mitchell JE, Crow SJ. A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychological Medicine. 2014;44:543–553. doi: 10.1017/S0033291713001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smyth J, Wonderlich SA, Heron K, Sliwinski M, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress predict binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- 8.Wonderlich SA, Engel SG, Peterson CB, Robinson MD, Crosby RD, Mitchell JE, Smith TL, Klein MH, Lysne CM, Crow SJ, Strauman TJ, Simonich HK. Examining the conceptual model for integrative cognitive-affective therapy for bulimia nervosa: Two assessment-related studies. Int J Eat Disord. 2008;41:748–754. doi: 10.1002/eat.20551. [DOI] [PubMed] [Google Scholar]
- 9.Wonderlich SA, Peterson CB, Smith TL, Klein M, Mitchell JE, Crow SJ, Engel SG. Integrative cognitive-affective therapy for bulimia nervosa. In: Grilo CG, Mitchell JE, editors. The Treatment of Eating Disorders: A Clinical Handbook. New York: Guilford Press; 2010. pp. 317–338. [Google Scholar]
- 10.Wonderlich SA, Peterson CB, Smith TL, Klein HM, Mitchell JE, Crow SJ. Integrative Cognitive-Affective Therapy for Bulimia Nervosa: A Treatment Manual. New York: Guilford; 2015. [Google Scholar]
- 11.Harrison A, Sullivan K, Tchanturia K, Treasure J. Emotional functioning in eating disorders: attentional bias, emotion recognition and emotion regulation. Psychol Med. 2010;40:1887–1897. doi: 10.1017/S0033291710000036. [DOI] [PubMed] [Google Scholar]
- 12.Svaldi J, Griepenstroh J, Tuschen-Caffier B, Ehring T. Emotion regulation deficits in eating disorders: A marker of eating pathology or general psychopathology? Psychiatr Res. 2012;197:103–111. doi: 10.1016/j.psychres.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Lavender JM, Wonderlich SA, Peterson CB, Crosby RD, Engel SG, Mitchell JE, Crow SJ, Smith TL, Klein MH, Goldschmidt AG, Berg KC. Dimensions of emotion dysregulation in bulimia nervosa. European Eating Disorders Review. 2014;22:212–216. doi: 10.1002/erv.2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benjamin LS. Structural analysis of social behavior. Psychol Rev. 1974;81:392–425. [Google Scholar]
- 15.Benjamin LS. Interpersonal Diagnosis and Treatment of Personality Disorder. New York: Guilford; 1993. [Google Scholar]
- 16.Higgins ET. Self-discrepancy: A theory relating self and affect. Psychol Rev. 1987;94:319–340. [PubMed] [Google Scholar]
- 17.Strauman TJ, Vieth AZ, Merrill KA, Kolden GG, Woods TE, Klein MH, Papadakis AA, Schneider KL, Kwapil L. Self-system therapy as an intervention for self-regulatory dysfunction in depression: A randomized comparison with cognitive therapy. J Consult Clin Psychol. 2006;74:367–376. doi: 10.1037/0022-006X.74.2.367. [DOI] [PubMed] [Google Scholar]
- 18.Strauman TJ, Vookles J, Berenstein V, Chaiken S, Higgins ET. Self-discrepancies and vulnerability to body dissatisfaction and disordered eating. J Pers Soc Psychol. 1991;61:946–956. doi: 10.1037//0022-3514.61.6.946. [DOI] [PubMed] [Google Scholar]
- 19.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Personality Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 20.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-based Approach. New York: Guilford; 2013. [Google Scholar]
- 21.Rieger E, Van Buren DJ, Bishop M, Tanofsky-Kraff M, Welch R, Wilfley DE. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): Causal pathways and treatment implications. Clin Psychol Rev. 2010;30:400–410. doi: 10.1016/j.cpr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 22.Strauman TJ, Merrill KA. The basic science/clinical science interface and treatment development. Clin Psychol: Science Pract. 2004;11:263–266. [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 24.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. 12. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- 25.Berg KC, Peterson CB, Frazier P, Crow SC. Psychometric evaluation of the Eating Disorder Examination and Eating Disorder Examination-Questionnaire: A systematic review of the literature. Int J Eat Disord. 2012;45:428–438. doi: 10.1002/eat.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assessm. 2004;26:41–54. [Google Scholar]
- 27.Cooper JL, O’Shea AE, Atkinson MJ, Wade TD. Examination of the Difficulties in Emotion Regulation Scale and its relation to disordered eating in a young female sample. Int J Eat Disord. 2014;47:630–639. doi: 10.1002/eat.22278. [DOI] [PubMed] [Google Scholar]
- 28.Racine SE, Wildes JE. Emotion dysregulation and symptoms of anorexia nervosa: The unique roles of lack of emotional awareness and impulse control difficulties when upset. Int J Eat Disorder. 2013;46:713–720. doi: 10.1002/eat.22145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benjamin LS. Intrex User’s Manual. Salt Lake City: University of Utah; 2000. [Google Scholar]
- 30.Pincus AL, Gurtman MB, Ruiz MA. Structural analysis of social behavior (SASB): Circumplex analyses and structural relations with the interpersonal circle and five factor model of personality. J Pers Soc Psychol. 1998;74:1629–1645. [Google Scholar]
- 31.Higgins ET, Bond RN, Klein K, Strauman T. Self-discrepancies and emotional vulnerability: How magnitude, accessibility, and type of discrepancy influence affect. J Pers Soc Psychol. 1986;51:5–15. doi: 10.1037/0022-3514.51.1.5. [DOI] [PubMed] [Google Scholar]
- 32.Higgins ET, Klein R, Strauman T. Self-concept discrepancy theory: A psychological model for distinguishing among different aspects of depression and anxiety. Soc Cogn. 1985;3:51–76. [Google Scholar]
- 33.Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychol Science. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Accurso EC, Fitzsimmons-Craft EE, Ciao A, Cao L, Crosby RD, Smith TL, Klein MH, Mitchell JE, Crow SJ, Wonderlich SA, Peterson CB. Therapeutic alliance in a randomized clinical trial for bulimia nervosa. J Consult Clin Psychol. 2015;83:637–642. doi: 10.1037/ccp0000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Accurso EC, Wonderlich SA, Crosby RD, Smith TL, Klein MH, Mitchell JE, Crow SJ, Berg KC, Peterson CB. Predictors and moderators of treatment outcome in a randomized clinical trial for adults with symptoms of bulimia nervosa. J Consult Clin Psychol. 2016;84:178–84. doi: 10.1037/ccp0000073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Safer DL, Telch CF, Chen EY. Dialectical Behavior Therapy for Binge Eating and Bulimia. New York: Guilford Press; 2009. [Google Scholar]
- 37.Gale C, Gilbert P, Read N, Goss K. An evaluation of the impact of introducing compassion focused therapy to a standard treatment program for people with eating disorders. Clin Psychol Psychother. 2014;21:1–12. doi: 10.1002/cpp.1806. [DOI] [PubMed] [Google Scholar]
- 38.Wnuk SM, Greenberg L, Dolhanty J. Emotion-focused group therapy for women with symptoms of bulimia nervosa. Eat Disord. 2015;23:253–261. doi: 10.1080/10640266.2014.964612. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.