Abstract
Objective
The current study examined effects of a preventive intervention on patterns of change in symptoms of anxiety and depression in a sample of children of depressed parents.
Method
Parents with a history of depression (N = 180) and their children (N = 242; 50% female; Mage = 11.38; 74% Euro-American) enrolled in an intervention to prevent psychopathology in youth. Families were randomized to a family group cognitive behavioral intervention (FGCB) or a written information (WI) control condition. Parents and youth completed the Child Behavior Checklist and Youth Self Report at baseline, 6-, 12-, 18-, and 24-month follow up.
Results
Youth in the FGCB intervention reported significantly greater declines in symptoms of both anxiety and depression at 6-, 12-, and 18-months compared to youth in the WI condition. Youth with higher baseline levels of each symptom (e.g., anxiety) reported greater declines in the other symptom (e.g., depression) from 0 to 6-months for in the FGCB intervention only. Changes in anxiety symptoms from 0–6 months predicted different patterns of subsequent changes in depressive symptoms from 6–12 months for the two conditions, such that declines in anxiety preceded and predicted greater declines in depression for FGCB youth but lesser increases in depression for WI youth.
Conclusions
Findings inform transdiagnostic approaches to preventive interventions for at-risk youth, suggesting both initial symptom levels and initial magnitude of change in symptoms are important to understand subsequent patterns of change in response to intervention.
Keywords: anxiety, depression, prevention, transdiagnostic, parental depression
Anxiety and depression are important targets, both separately and conjointly, for preventive interventions with children and youth (e.g., Barrett et al., 2006; Dobson, Hopkins, Fata, Scherrer, & Allan, 2010; Flanery-Schroeder, 2006; Garber & Weersing, 2010). Anxiety and depression are highly prevalent in childhood and adolescence, and the early onset of these symptoms and disorders predicts a worse course across the lifespan (e.g., Merikangas et al., 2010). Further, diagnostic and dimensional approaches indicate high rates of comorbidity and the frequent co-occurrence of symptoms of anxiety and depression, while there is also considerable evidence that these symptoms occur independently in youth (e.g., Achenbach, Dumenci, & Rescorla, 2003; Boots & Wareham, 2009; Cummings et al., 2014; van Lang et al., 2005; Moffitt et al., 2007; Seeley, Kosty, Farmer, & Lewinsohn, 2001). Taken together, these findings suggest that anxiety and depression are distinct yet related sets of symptoms or disorders in childhood and adolescence.
The association between anxiety and depression has led to the development of transdiagnostic approaches to the treatment of these symptoms under unified protocols (e.g., Chu, 2012; Chu, Hoffman, Johns, Reyes-Portillo, & Hansford, 2014; Queen, Barlow, & Ehrenreich-May, 2014) and also suggests the potential importance of transdiagnostic preventive interventions (e.g., Barrett, Farrell, Ollendick, & Dadds, 2006; Dozois, Seeds, & Collins, 2009; Martinsen, Kendall, Stark, & Neumer, 2014). Specifically, transdiagnostic preventive interventions have emerged to target symptoms of anxiety and depression in children and adolescents (e.g., Ehrenreich-May & Bilek, 2012; Farchione et al., 2012; Seligman, Schulman, & Tryon, 2007). As these approaches continue to develop, it is important to understand whether transdiagnostic interventions lead to change in both symptoms and anxiety and it is further important to understand the dynamics of change in these symptoms; i.e., the temporal relation between the magnitude of change in one set of symptoms as a predictor of the magnitude of change in the other type of symptoms during and after an intervention. Although transdiagnostic approaches have shown promising evidence that both symptoms of anxiety and depression can be changed within the same intervention protocol, there is little understanding of how these symptoms affect one another as they change within and following an intervention.
Research has examined the temporal relationship of anxiety and depression during childhood and adolescence outside of the context of interventions and findings have varied. Although some studies have found that symptoms of anxiety developmentally precede symptoms of depression (e.g., Cole, Peeke, Martin, Truglio, & Seroczynski, 1998; Keenan, Feng, Hipwell, & Klostermann. 2009; Snyder et al., 2009), there is a growing record of evidence to support a bidirectional relationship between these symptoms across development (e.g., Hale, Raaijmakers, Muris, van Hoof, & Meeus, 2009; Lavigne, Hopkins, Gouze, & Bryant, 2015; Moffitt et al., 2007). For example, Hale et al. (2009) found that in a sample of children and adolescents at-risk for anxiety, higher levels of anxiety symptoms positively predicted the slope of depressive symptoms over time and vice versa, such that initially high levels of symptoms predicted less reduction in the parallel symptom. Lavigne et al. (2015) built upon previous research examining the bidirectional relationship between anxiety and depression across three points in time (ages 4, 5, 6), assessing multiple indicators of the latent constructs of anxiety and depression. In this study, the authors found a bidirectional influence of anxiety and depressive symptoms on one another in a community sample of children, such that symptoms of anxiety and depression were associated with higher levels of one another one year later. Thus, evidence suggests that these symptoms influence one another over time throughout childhood and adolescence.
With regard to the temporal relationship between symptoms of anxiety and depression in the context of interventions, data analytic approaches have been used to test both static and dynamic patterns of association. First, studies have examined how the initial intercept of symptom A (i.e., a static measure of symptoms at one point in time) predicts the subsequent magnitude or rate of change in symptom B (e.g., Hale et al., 2009; Young et al., 2012). These analyses have been largely used to answer the question of whether youth presenting with symptom A are more or less able to benefit from intervention in regard to symptom B (e.g., do youth enrolled in anxiety treatment with co-morbid depressive symptoms benefit less from treatment?). Whether initial symptom levels will predict subsequent change in the other symptom has important clinical utility for intervention and may inform how to appropriately intervene with children or adolescents depending on their initial symptom presentation. Relatively fewer studies have used a novel approach to examine the dynamics of change in symptoms of anxiety and depression in an intervention, or how the magnitude of change of symptom A predicts the subsequent magnitude of change of symptom B over time (e.g., Schumm, Dickstein, Walter, Owens, & Chard, 2015). Given that these symptoms may be dynamic in the context of an intervention, understanding how change in one set of symptoms impacts subsequent change in another set of symptoms may provide important additional information for interventions aimed at these symptoms. These analyses may answer the question of whether in the context of an intervention, changes in one symptom lead to changes in the other symptom. More specifically, analyses examining dynamics of change in symptoms of anxiety and depression in interventions may highlight the potential importance of producing change in one type of symptoms to contribute to subsequent change in the other type of symptoms.
Using the first data analytic approach, a number of studies have examined the impact of comorbid anxiety and depression on the effects of treatment in children and adolescents, and findings have been mixed (e.g., Berman, Weems, Silverman, & Kurtines, 2000; Brent et al., 1998; Curry et al., 2006; Rapee et al., 2013; Rohde, Clarke, Lewinsohn, Seeley, & Kaufman, 2001; Southam-Gerow, Kendall, & Weersing, 2001). A meta-analysis examining the role of comorbidities in affective and anxiety disorders concluded that there is little evidence to support the impact of comorbid depression on anxiety treatment outcome, and some evidence to support a negative impact of comorbid anxiety on outcome in treatment for mood disorders (Ollendick, Jarrett, Grills-Taquechel, Hovey, & Wolff, 2008). Others have found evidence that co-morbidity hinders treatment success (e.g., Curry et al., 2006; Hilton et al, 2013; O’Neil & Kendall, 2012). For example, O’Neil and Kendall (2012) found that children with higher self-reported depressive symptoms at the start of a cognitive behavioral treatment (CBT) for anxiety demonstrated higher pre-treatment anxiety severity scores and showed less reduction in anxiety immediately post-treatment (O’Neil & Kendall, 2012). Lastly, other studies have found the presence of one symptom to predict more favorable treatment outcomes (e.g., Brent et al., 1998; Rohde et al., 2001). Rohde et al. (2001) found that the presence of an anxiety disorder was associated with greater depressive symptom severity at initial intake and greater symptom reduction post-intervention. Thus, the findings on the effect of initial symptoms on subsequent change in related symptoms have been quite mixed.
A limited number of studies have examined the relationship between symptoms of anxiety and depression in preventive interventions for children and adolescents (e.g., Lowry-Webster et al., 2001, 2003; Roberts, Kane, Thomson, Bishop, & Hart, 2003; Young et al., 2012). These studies have largely focused on whether the intervention changed the secondary symptom (e.g., changes in anxiety in a depression prevention program), but have not examined how changes in these symptoms are associated with one another. For example, Lowry-Webster et al. (2001, 2003) found that an anxiety prevention program was more effective at reducing depressive symptoms for youth with high levels of anxiety symptoms (i.e., scoring above the clinical cutoff on an anxiety measure) at initial assessment compared to youth with high levels of anxiety in the control condition. In one of the few prevention studies examining how initial symptoms of one type predict later change in the other symptom, Interpersonal Psychotherapy Adolescent Skills Training (IPT-AST) was compared to school counseling to prevent depression in high-risk adolescents (Young et al., 2012). The study found significant intervention effects for both anxiety and depression from pre- to post-intervention. Findings indicated the presence of comorbid anxiety symptoms at initial assessment was associated with slower declines depressive symptoms during the course of intervention and over the follow-up period, suggesting a delayed effect of the intervention for adolescents experiencing high levels of anxiety symptoms. However, the converse (i.e., whether initial levels of depressive symptoms predicted subsequent changes in anxiety symptoms) was not examined in this study. Thus, findings within the prevention literature are limited and offer mixed evidence for the impact of one symptom set on another.
The current study examines the temporal relationship between symptoms of anxiety and depression in offspring of parents with a history of major depressive disorder (MDD) for youth enrolled in a family group cognitive-behavioral preventive selective intervention (FGCB) (masked reference). Children of depressed parents offer an important opportunity to examine the relationship between symptoms anxiety and depression in the context of a preventive intervention, as they are at a greater risk for developing internalizing psychopathology, including symptoms of anxiety and depression, than children of non-depressed parents (Goodman et al., 2011). Further, children of depressed parents experience high rates of co-occurring symptoms of anxiety and depression (Goodman et al., 2011; Sellers et al., 2013).
The 12-session preventive intervention, which aimed to prevent MDD and internalizing and externalizing symptoms in high-risk youth, included a parent component that taught parenting skills to parents who have experienced MDD and a child component that taught children skills to cope with the stress of living with a depressed parent (masked reference). The FGCB intervention was compared to a written-information (WI) control condition in which families received information about stress and depression in families over the course of two months. Previous reports have examined intervention effects on episodes of depression, internalizing problems, and mixed anxiety-depression symptoms, but have not separately examined symptoms of anxiety and depression or the temporal relationship between symptoms (masked references).
The first aim of the current study was to examine whether baseline levels of symptoms of anxiety predict change in symptoms of depression during the intervention and vice versa in both the intervention and control conditions. As reported above, previous findings from treatment and prevention studies are mixed, with evidence suggesting the presence of one symptom may hinder, have no effect, or may benefit youth in regard to the other symptom’s improvement (e.g., Curry et al., 2006; Rohde et al., 2001; Ollendick et al., 2008). Given significant heterogeneity within the field regarding whether initial symptom levels predict change in other symptoms in both treatment and prevention, we did not hypothesize a specific direction for these effects. The second aim of the study was to examine whether changes in depression predict subsequent changes in anxiety and vice versa in both conditions. Because no studies have previously examined whether change in anxiety predicts subsequent change in depression (and vice versa) in a preventive intervention, did not hypothesize a specific direction for these effects using this novel data analytic approach.
Method
Participants
The current study included 180 parents (20 fathers, 160 mothers; Mage = 41.61, SD = 7.17) with a history of depression and their children (N = 242; 121 boys, 121 girls) between the ages of 9 and 15 years (M = 11.38, SD = 2.00) from the area in and around two cities in southeastern and northeastern U.S. All families were enrolled in a preventive intervention aimed to prevent depression in children of depressed parents (for additional details, see masked reference). Parents met criteria for at least one episode of major depressive disorder (MDD) during the lifetime of their child(ren). Families also met the following criteria: (a) parent had no history of bipolar I, schizophrenia, or schizoaffective disorders and did not meet current criteria for alcohol or substance use; (b) children had no history of autism spectrum disorders, mental retardation, bipolar I disorder, or schizophrenia; and (c) children did not currently meet criteria for depression (MDD, dysthymia, or depression-not otherwise specified), conduct disorder, or substance/alcohol abuse or dependence. Parents and children could meet criteria for anxiety disorder(s) at the time of study enrollment. The age range of 9 to 15 years old was selected to include youth prior to mid-adolescence, when rates of depression increase significantly for youth (Hankin et al., 2015), and old enough to be able to learn the skills assessed in the group.
Six percent of parents completed less than high school, 9% completed high school, 30% completed some college, 32% had a college degree, and 23% began or completed graduate education. Eighty-two percent of parents were European American, 12% African American, 2% Hispanic American, 1% Asian American, 1% Native American, and 2% mixed ethnicity. Seventy-four percent of children were European American, 13% African American, 3% Asian American, 2% Hispanic American, 1% Native American, and 7% mixed ethnicity. Annual family income ranged from less than $5,000 to more than $180,000 (median = $40,000 to 60,000). Sixty-two percent of parents were married/partnered, 22% divorced, 5% separated, 10% had never married, and 1% were widowed.
Forty-eight parents (27%) were in a current episode of major depression and 132 parents (73%) were not in episode at the time of the baseline assessment. At baseline, 147 (82%) parents reported experiencing multiple episodes of depression during their child’s/children’s life (Median number of episodes = 3), 27 (15%) reported experiencing only a single episode during their child’s/children’s life, and five (2.7%) reported dysthymic disorder during their child’s life (one parent did not provide enough information to determine frequency of depressive episodes).
Measures
Demographics
Parents reported the child’s age and race/ethnicity and self-reported age, race/ethnicity, family income, and highest obtained education level.
History of MDD
For study eligibility, parents and children completed diagnostic interviews to assess for depressive disorders. Parents’ current and past history of MDD was assessed with the Structured Clinical Interview for DSM (SCID; First, Spitzer, Gibbon, & Williams, 2001). Interviewers were trained by the PIs on the study using a number of methods, including listening to previously recorded interviews, practicing using role-plays, observation of interviews, and being observed conducting interviews by the project PIs. Inter-rater reliability, calculated on a randomly selected subset of these interviews, indicated 93% agreement (k = 0.71) for diagnoses of MDD. Similarly, children and parents completed the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997). Inter-rater reliability for diagnoses of MDD in children and adolescents, calculated on a randomly selected subset of these interviews, indicated a 96% agreement (k = 0.76) for diagnoses of MDD. Parents and children completed diagnostic interviews at baseline, and 6-, 12-, 18-, and 24-month follow-ups (see masked reference).
Child symptoms of anxiety and depression
Parents and children completed measures of children’s symptoms of anxiety and depression 5 times over a 2-year period (pre-intervention and 6-, 12-, 18-, and 24-months post intervention). Parents completed the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) about their child. The CBCL includes a 118-item checklist of problem behaviors during the previous 6 months that parents rate on a 0–2 scale about their child in the past 6 months. The CBCL assesses a number of problem areas in children, including anxiety and depression, and demonstrates well-established reliability and validity. Youth completed the Youth Self Report (YSR; Achenbach & Rescorla, 2001), the self-report version of the CBCL for adolescents 11–18 years of age. Reliability and validity of the CBCL and YSR are well established. Children who were 9 or 10 years of age completed the YSR to allow for complete data on all measures. The CBCL and YSR have been used extensively in intervention research (e.g., Clarke et al., 2001; Tein, Sandler, Ayers, & Wolchik, 2006; Wolchik et al., 2000, 2002).
Because we were interested in examining changes in symptoms of anxiety and depression, the Affective Problems and Anxiety Problems DSM scales were selected for analyses. These scales were derived to reflect DSM symptoms of depression and anxiety disorders. The Affective Problems scale is comprised of 13 items, including symptoms such as sadness, sleep problems, and feelings of worthlessness. The Anxiety Problems scale includes 6 items assessing symptoms such as nervousness, fears, and worries. There are no overlapping items on the Affective Problems and Anxiety Problems scales. The DSM scales of the CBCL and YSR demonstrate good convergent and discriminant validity (e.g., Achenbach et al., 2003; Ebesutani et al. 2010; Nakamura, Ebesutani, Bernstein, & Chorpita, 2009). The Anxiety and Affective scales have been shown to predict their target disorders (e.g., DSM Anxiety scale predicting Anxiety diagnoses) in children and adolescents (Ebustani et al., 2010; Nakamura et al., 2009). Internal consistency for the current sample at baseline ranged from α = 0.71 to 0.79 for the YSR and α = 0.64 to 0.74 for the CBCL.
Procedures
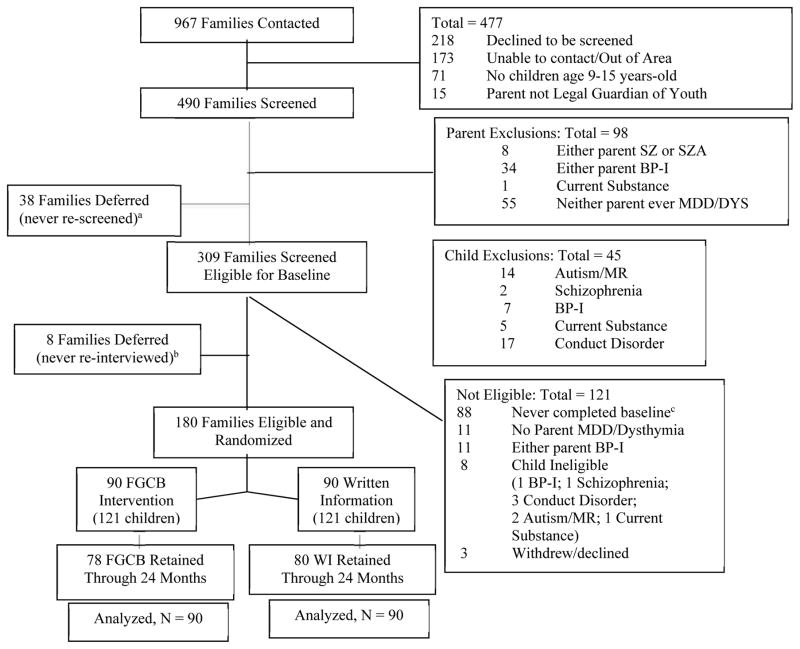
Participants were invited to enroll in a study comparing two programs for parents with a history of MDD and their children. Figure 1 depicts screening and enrollment. Families enrolled in the study were randomized to either a 12-session (8 weekly sessions and 4 monthly booster sessions) FCGB selective preventive intervention or a WI control condition. The FCGB intervention included two primary components: 1) teaching effective parenting skills to parents (e.g., warmth and structure) and 2) teaching secondary control coping skills (e.g., acceptance, cognitive reappraisal) to children to cope with stress in their families (for additional details, see masked references). The WI control condition was modeled after previous self-study and lecture-based programs used in family-based interventions (Beardslee, Wright, Gladstone, & Forbes, 2007; Wolchik et al., 2000) and included psycho-education about depression, effects of depression on families, and how to recognize depression in children. Participants completed assessments at baseline (prior to randomization), 6-, 12-, 18-, and 24-month follow up periods. The spacing of assessments was intentional based on the design of the clinical trial, such that participants were assessed immediately following the intervention (6-month follow up) and subsequent 6-month intervals out to 24-months. Follow up assessments opened at each of the appointed times (i.e., 6-, 12-, 18-, or 24-months) and windows remained open for 3-months. All study procedures were approved by the Institutional Review Boards at the two sites. All assessments and intervention sessions were conducted in the psychology departments of the two universities. Two licensed PhD clinical psychologists conducted weekly supervision for clinical interviews and the intervention groups.
Figure 1.
Participant screening and randomization.
a = 15 families deferred due to youth MDE; b = 5 families deferred due to youth MDE; c = 8 youth not interested; 56 parent not interested; 3 families moved; 1 parent not legal guardian; 19 not reachable; 1contacted study after enrollment closed
Data Analytic Approach
The present study used a similar data analytic approach as employed by (masked references) to test for the effects of the FGCB intervention at 6-, 12-, 18- and 24-months within a partially nested design. The present study utilizes a three-level partially nested design: children are nested within families, and for the FGCB intervention, families are nested within groups. Families in the WI group are non-nested due to their independence. In partial nesting designs, the presence or absence of clustering is systematically paired with a covariate (intervention), and different model-implied variances are anticipated in the nested and non-nested conditions. To accommodate the dependencies generated by this design, univariate (Bauer, Sterba, & Hallfors, 2008) and multivariate (masked references; Sterba, 2015; Sterba et al., 2014) partially nested multilevel models have been developed. In the first set of analyses, we used a three-level multivariate version of the partially nested multilevel model to test the effect of condition on outcomes at the 6-, 12-, 18-, and 24-month follow ups, treating the baseline measure of the outcome as a global covariate (see masked reference).
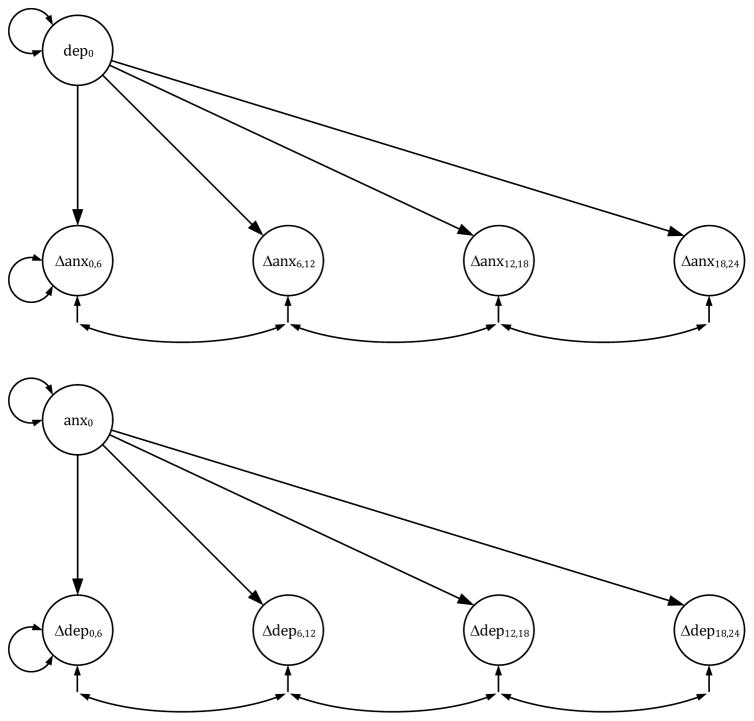
To examine the first aim of the study, we used a partially-nested version of univariate latent change score (LCS) model (McArdle & Hamagami, 2001; Ram & Nesselroade, 2007; Selig & Preacher, 2009) to examine how baseline scores on the YSR/CBCL Affective (or Anxiety) Problems scales were associated with change in symptoms of the other syndrome, Anxiety (or Affective) problems. For each condition, we examined these relationships, across 6-month intervals between consecutive time points at baseline, 6-, 12-, 18-, and 24-month follow up, separately for parent-report and child-report (see Figure 2); the use of a LCS model requires equally spaced assessments (e.g., 6-month intervals between each assessment). The traditional univariate LCS model was extended to account for partial nesting in the manner described above with the exception that the family-level variance component was near-zero and its inclusion led to estimation problems; hence it was omitted in this and the third set of analyses.
Figure 2.
Univariate latent change score models used in the first analyses. These diagrams depict the model testing whether baseline of one kind of symptom (Affective or Anxiety) predicts subsequent magnitude of change in the other symptom (Affective or Anxiety).
To examine the second aim of the study, we used a partially-nested version of a bivariate LCS model (McArdle & Nesselroade, 2003) to examine how change across 6-month intervals in one kind of symptom (YSR/CBCL Affective or Anxiety Problems) predicts change at the subsequent 6-month interval in the other kind of symptom, controlling for prior change. Figure 3 depicts this model of change in symptom A predicting change in symptom B and vice versa. The second and third sets of analyses were conducted in Mplus v7.31. The LCS models used in the current study differ from models using observed or algebraic difference scores. There are a number of methodological limitations associated with the use of observed or algebraic difference scores (see Edwards, 1994, 2009; Laird & De Los Reyes, 2013; Laird & Weems, 2011), and LCS models are not subject to these same methodological concerns. Specifically, LCS models retain the component variables as separate variables and impose a theoretically guided model relating the components, test a theoretically guided model relating these components to an outcome, and the t1 and t2 measures are commensurate.
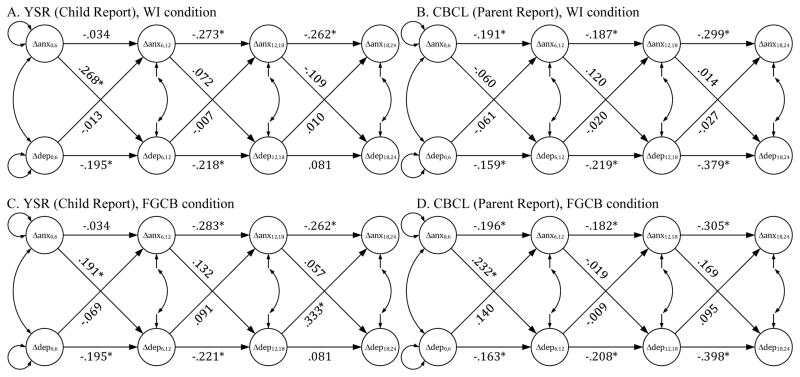
Figures 3a–3d.
The figures depict the observed mean trajectory of symptom change in the FGCB and WI conditions based on self- and parent report of youth anxiety and depressive symptoms at 6-month intervals.
Results
Preliminary Analyses
Several preliminary analyses were conducted prior to the tests the primary hypotheses. First, families assigned to the FGCB and WI conditions were compared at baseline on parents’ baseline depression status and child baseline depressive and anxiety symptoms across the four follow-up assessments (6-, 12-, 18-, and 24-months). The FGCB and WI conditions did not significantly differ on any of these variables at time of initial assessment. Further, because not all parents and children provided complete data at all assessment points, a variable reflecting the amount of missing data was derived to compare across conditions. The amount of missing data did not differ between families assigned to the FGCB condition versus WI condition. In addition, previous analyses found no significant moderator effects on internalizing symptoms for age or gender in this sample (masked reference), and therefore, we did not include these variables in the current analyses.
For the purposes of describing the sample and allowing for comparison to other studies, means and standard deviations for youth symptoms of anxiety and depression were examined at initial assessment. As expected in this at-risk sample, baseline youth depressive symptoms as measured by the YSR Affective Problems Scale (mean T = 56.54) and the CBCL Affective Problems scale (mean T = 60.43) reflected moderate levels of depressive symptoms at initial assessment. Similarly, youth Anxiety Problems on the YSR (mean T = 55.36) and CBCL (mean T = 58.22) were moderately elevated at initial assessment. The percent of children in the clinical range on the Affective Problems scale (i.e., T score > 70) was 5.2% on the YSR and 16.2% on the CBCL (based on normative data, 2% would be expected to exceed this cutoff). The percent of children in the clinical range on the Anxiety Problems scale was 6.5% on the YSR and 12.6% on the CBCL. These levels of symptoms are consistent with levels of internalizing symptoms reported on the CBCL for children of depressed parents in other studies, suggesting the current study sample is representative of children of parents with a history of depression (e.g., STAR*D trial, Foster et al., 2008).
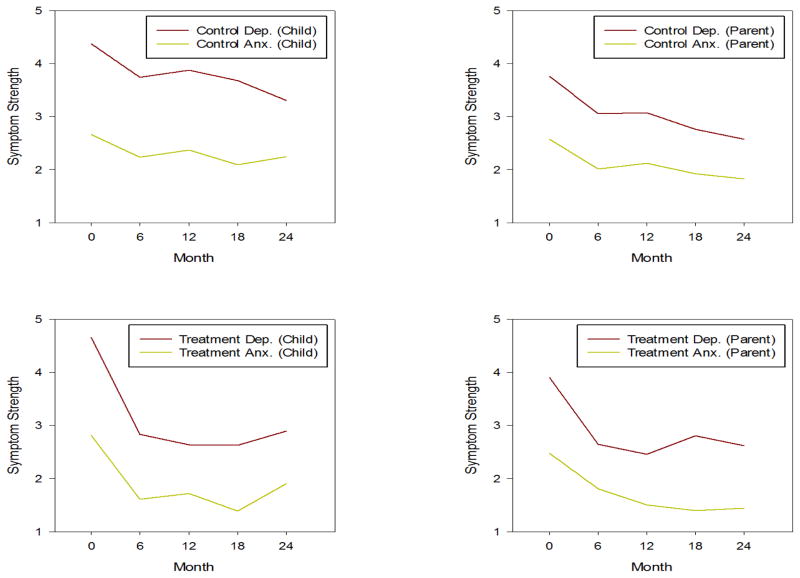
Bivariate correlations between parent and child report for youth symptoms of anxiety and depression at each time point were conducted. Correlations between parent and child report on the Affective Problems scale (r = .32 to .50, p < .01) and Anxiety Problems scale (r = .30 to .40, p < .01) were significant at each time point. Further, correlations between youth self-reported anxiety and depressive symptoms (r = .62 to .67, p < .01) and parent-report of youth anxiety and depressive symptoms (r = .49 to .59, p < .01) were significantly correlated at each time point. Finally, observed mean trajectories for depressive and anxiety symptoms are depicted in Figure 4, broken down by condition (WI vs. FGCB) and youth vs. parent report.
Figures 4a–4d.
Univariate latent change score models used in the second analyses. Models showing magnitude of change predicting subsequent magnitude of change for YSR and CBCL Affective and Anxiety Problems by condition.
The main effects of condition on each outcome variable were examined, controlling for the baseline score of the outcome. Consistent with previous analyses using the broad internalizing and mixed anxiety-depression scales (masked reference), youth in the FGCB intervention reported significantly lower symptoms than those in the WI condition on YSR Affective Problems and YSR Anxiety Problems at 6-, 12-, and 18-months (d’s ranged from .50 to .59). Parents in the FGCB intervention reported fewer youth CBCL Anxiety Problems at 12-months only. Group differences on the CBCL Affective Problems were not significant at any time-point.
Effect of Initial Symptoms on Symptom Change Over Time
The effect of the baseline intercept of symptoms of anxiety and depression on change in the alternate symptom was examined at each interval (0–6 months; 6–12 months; 12–18 months; 18–24 months) for the FGCB and WI conditions (see Table 1). For the FGCB condition, youth self-reported initial levels of anxiety symptoms on the YSR predicted change in depressive symptoms from 0–6 months (β = −0.27; SE = 0.11), indicating that higher levels of initial anxiety predicted greater immediate decline in depressive symptoms. To illuminate this pattern of results in Table 1, consult Figure 3, Panel C, which shows a negative mean trend in depressive symptoms between months 0 and 6 for the FGCB condition. A significant negative coefficient linking anxiety symptoms at month 0 to change in depressive symptoms between months 0 and 6 indicates that FGCB individuals with higher anxiety at month 0 tended to have a steeper decline in depressive symptoms between months 0 and 6. Similarly, for the FGCB condition, youth self-reported initial levels of depressive symptoms on the YSR predicted change in anxiety symptoms from 0–6 months (β = −0.34; SE = 0.10), indicating that higher levels of initial depressive symptoms predicted greater immediate decline in anxiety symptoms (Figure 3, Panel C). In addition, parent-report of initial youth anxiety symptoms on the CBCL predicted change in depressive symptoms from 6–12 months (β = −0.24; SE = 0.12), indicating that higher levels of initial anxiety symptoms predict greater decline in depressive symptoms from 6–12 months (Figure 3, Panel D).
Table 1.
Effects for intercept predicting magnitude of change at 6-, 12-, 18-, and 24-month follow ups.
| FGCB Condition | ||||
|---|---|---|---|---|
| Time 2 B (SE) |
Time 3 B (SE) |
Time 4 B (SE) |
Time 5 B (SE) |
|
| Predictor: YSR Affective Problems (baseline) | ||||
| Change in YSR Anxiety Problems | −0.34* (0.10) | 0.10 (0.10) | 0.03 (0.10) | 0.19 (0.11) |
| Predictor: CBCL Affective Problems (baseline) | ||||
| Change in CBCL Anxiety Problems | 0.03 (0.15) | −0.19 (0.12) | 0.02 (0.12) | 0.11 (0.12) |
| Predictor: YSR Anxiety Problems (baseline) | ||||
| Change in YSR Affective Problems | −0.27* (0.11) | −0.06 (0.11) | 0.11 (0.12) | 0.18 (0.12) |
| Predictor: CBCL Anxiety Problems (baseline) | ||||
| Change in CBCL Affective Problems | −0.10 (0.14) | −0.24* (0.12) | 0.08 (0.14) | −0.11 (0.13) |
| WI Condition | ||||
| Predictor: YSR Affective Problems (baseline) | ||||
| Change in YSR Anxiety Problems | −0.10 (0.11) | 0.06 (0.11) | 0.10 (0.10) | 0.09 (0.11) |
| Predictor: CBCL Affective Problems (baseline) | ||||
| Change in CBCL Anxiety Problems | 0.20* (0.09) | 0.20* (0.10) | 0.02 (0.10) | 0.21* (0.09) |
| Predictor: YSR Anxiety Problems (baseline) | ||||
| Change in YSR Affective Problems | 0.06 (0.10) | 0.04 (0.11) | 0.13 (0.10) | 0.29* (0.10) |
| Predictor: CBCL Anxiety Problems (baseline) | ||||
| Change in CBCL Affective Problems | 0.09 (0.09) | −0.07 (0.09) | 0.07 (0.09) | 0.13 (0.09) |
For the WI condition, Table 1 indicates that youth self-reported baseline anxiety symptoms on the YSR predicted depressive symptoms from 18–24 months (β = 0.28; SE = 0.10), indicating higher levels of initial anxiety predicted less of a decrease in depressive symptoms from 18–24 months (Figure 3, Panel A). Parent-reported initial depressive symptoms on the CBCL in the WI condition predicted change in anxiety from 0–6 months (β = 0.20; SE = 0.09), 6–12 months (β = 0.20; SE = 0.10), and 18–24 months (β = 0.21; SE = 0.09). Based on parent-report, youths with higher initial depressive symptoms demonstrate less of a decrease/more of an increase in anxiety over time (Figure 3, Panel B).
Effect of Symptom Change on Subsequent Symptom Change Over Time
Finally, we examined whether change in symptom A predicted subsequent change in symptom B controlling for previous change in symptom A (and vice versa) by condition for each interval (0–6 months, 6–12 months, 12–18 months, 18–24 months) (see Figure 4). For the FGCB condition, youth self-reported change in anxiety symptoms on the YSR from 0–6 months predicted subsequent change in depressive symptoms from 6–12 months. Specifically, a greater decrease in anxiety during the intervention phase (0–6 months) predicted a subsequent greater decline in depressive symptoms from 6 to 12 months (β = 0.19) (Figure 4). To understand this pattern of results, consult Figure 3, Panel C, which shows a negative mean trend in anxiety symptoms between months 0 and 6, and a slight negative mean trend in depressive symptoms between months 6 and 12. A significant positive coefficient linking change in anxiety between months 0 and 6 to change in depressive symptoms between months 6 and 12 indicates that FGCB individuals experiencing greater decline in anxiety between months 0 and 6 tended to have a greater decline in depressive symptoms between months 6 and 12. These findings were also found in parent-report of youth symptoms on the CBCL in the FGCB condition, with parent-report of declines in youth anxiety symptoms at 0–6 months predicting subsequent decline in depressive symptoms from 6–12 months (β = 0.23; see Figure 3 and Figure 4, Panel D). In addition, change in youth self-reported depressive symptom on the YSR from 12–18 months predicted subsequent change in anxiety symptoms, indicating that a greater decline in depressive symptoms was associated with a smaller increase in anxiety symptoms from 18–24 months (β = 0.33; see Figure 3 and Figure 4, Panel C).
In the WI condition, Figure 3 indicates that youth self-reported change in anxiety symptoms on the YSR from 0–6 months predicted subsequent change in depressive symptoms, such that a greater decline in anxiety during the WI phase was associated with a smaller increase in depressive symptoms from 6–12 months (β = 0.27; see Figure 3 and Figure 4, Panel A). That is, as anxiety symptoms in the WI condition decreased from 0–6 months, the increase in depressive symptoms was smaller from 6–12 months. No parent-reported youth symptom change on the CBCL was a significant predictor of subsequent symptom change for symptoms of anxiety or depression (see Figure 3 and Figure 4, Panel B).
Discussion
The present study expands upon research examining interventions for symptoms of anxiety and depression in youth in a number of ways. The study is the first to examine both static and dynamic approaches to analyzing the associations between symptoms of anxiety and depression in a preventive intervention for children of depressed parents. Given the growing focus on transdiagnostic approaches to interventions targeting internalizing symptoms in youth, understanding how both initial levels of symptoms and changes in levels of symptoms effect one another can provide useful information for further development and enhancement of interventions in at-risk youth.
Results from the first aim of the study demonstrate that for youth in the FGCB condition, high levels of co-morbid symptoms were associated with greater declines in symptoms during the intervention in both directions (i.e., initial levels of anxiety predicted change in depression during the intervention phase and vice versa). As noted above, findings regarding the role of co-morbid symptoms in treatment outcomes have varied (e.g., Curry et al., 2006; O’Neil & Kendall, 2012; Rohde et al., 2001), and the few studies have examined this research question in prevention trials have also yielded mixed findings (e.g., Young et al., 2012). In contrast to Young et al. (2012), the current study suggests that youth with high levels of symptoms of anxiety and depression can initially benefit more than those with lower initial symptoms in a preventive intervention. There are several of possible explanations for these findings. The moderate levels of anxiety and depression in the current at-risk sample may have served to increase the motivation of children and adolescents to learn the skills taught in the FCGB intervention without interfering in their ability to implement these skills. Notably, the sample in Young et al. (2012) was an indicated sample, with all adolescents entering the study with elevated depression symptoms (i.e., the mean depressive symptoms score for participants was above the clinical cutoff for mild/significant symptoms). Further, symptoms of anxiety and depression are associated with levels of stress (e.g., Grant, Compas, Thurm, McMahon, & Gipson, 2004). It is possible then that youth with higher initial symptom levels were experiencing higher levels of stress, and thus these youth may have had more opportunity to use the coping skills that they learned during the intervention phase. Therefore, youth with moderate elevations in initial symptoms may have more opportunity to benefit from the skills in the initial intervention phase, whereas youth with lower levels of symptoms may not see immediate benefits from the skills.
For youth in the WI condition, however, the converse was true. Higher levels of depressive symptoms at baseline predicted less of a decrease and/or more of an increase in anxiety symptoms at 3 of 4 subsequent intervals based on parent report. Notably, the WI condition received minimal intervention (i.e., psycho-education on stress and depression in families). Thus, these findings are not unexpected given that in the absence of a skills-based intervention, it is expected that symptoms would increase over time as youth progress into adolescence, particularly for a selected at-risk sample (Avenevoli, Swendsen, He, Burnstein, & Merkiangas, 2015; Copeland, Angold, Shanahan, & Costello, 2014).
In the most novel aspect of this study, we examined the temporal sequence of changes in symptoms of anxiety and depression over time in both conditions across parent and youth report. In the FGCB condition, both parent and youth reports showed that magnitude of initial changes in anxiety preceded and predicted subsequent changes in depressive symptoms, such that greater magnitude of decline in anxiety symptoms during the intervention phase predicted greater subsequent magnitude of decline in depressive symptoms. The converse was not true; initial change in depressive symptoms did not predict subsequent change in anxiety symptoms. These findings shed light on dynamic processes of change in symptoms and highlight the benefit of initial change specifically in anxiety symptoms in transdiagnostic interventions. Specifically, these findings suggest that transdiagnostic interventions may be most effective if designed to optimize decreases in anxiety symptoms early in the intervention in order to optimize later decreases in depressive symptoms. The group format in the current intervention may have contributed to early anxiety change, such that attending a weekly group could have acted as an exposure for youth, contributing to initial anxiety decline. Further, the coping skills taught in the group to manage stress and increase positive mood through scheduling “fun activities” may have taken hold as the group was completed and thus contributed to greater subsequent depression symptom change. Further, later decline in depressive symptoms at 12–18 months predicted subsequent shallower increase in anxiety symptoms at 18–24 months for the FGCB group. Given that youth-reported symptoms of anxiety and depression were not significantly different across conditions at the 24-month follow up, previous decline in depressive symptoms may prevent some of the uptick in anxiety symptoms at the end of the follow up period for youth enrolled in the intervention condition.
In the WI condition, youth report indicated that initial reduction in anxiety symptoms predicted a subsequent shallower increase in depressive symptoms as depressive symptoms increased from 6–12 months. That is, a steeper decrease in anxiety during the preventive intervention predicted a slower increase in depressive symptoms in the follow up phase. Notably, these findings highlight the importance of initial change in symptoms of anxiety for both conditions; regardless of condition, youth were better off in the follow up phase if they demonstrated greater magnitude of decline in anxiety symptoms during the FGCB intervention and WI reading phase. It is noteworthy that symptoms of anxiety and depression changed differently between the two conditions, such that (1) the FGCB condition demonstrated significantly greater change compared to the WI condition, (2) initial symptom levels predicted greater symptom decline in the FGCB condition as compared with less symptom decline in the WI condition, and (3) the FGCB and WI conditions demonstrated different patterns in the analyses examining the dynamics of symptom change Therefore, these findings do not simply reflect a regression to the mean, but rather suggest that these two sets of symptoms are related in different ways in and outside of an intervention context.
The present study has several strengths and limitations. One important strength of the current study is that it is the first study to examine the relationship between symptoms of anxiety and depression in an intervention both by examining how initial symptom levels impact future change in symptoms and examining the dynamics of these changes in symptoms over time. Previous studies examining symptoms of anxiety and depression in interventions for youth have been limited to examining one set of symptoms or how comorbidity impacts treatment in one direction. Consistent with previous descriptive studies (e.g., Hale et al., 2009; Lavigne et al., 2015), the current study found evidence of bidirectional effects of symptoms of anxiety and depression, both for initial symptom levels and symptom changes over time, offering a more complete picture of how these symptoms are related over the course of a preventive intervention. Further, the study provides multi-informant reports of symptoms over time. Lastly, the study utilizes LCS models to test the two primary study aims, which offers an important methodological contribution to the field. While these methods have been used in previous research, to date no study has used LCS models to examine questions of static and dynamic associations between anxiety and depression in an intervention context. In addition, as noted previously, LCS models are not subject to the same methodological problems as simple difference scores (e.g., Edwards, 2009; Laird & De Los Reyes, 2013; Laird & Weems, 2011).
One limitation for the current study is that the Affective and Anxiety Problems scales are brief (13- and 6-items, respectively), with one alpha not in the acceptable range (CBCL Anxiety Problems). Given that alpha is directly related to the number of items, it is not unexpected that the Anxiety Problems scale would have lower reliability than the Affective Problems scale. Despite concerns regarding these scales, both the Affective Problems and Anxiety Problems scales have demonstrated associations with the diagnosis that each scale targets, and the Anxiety Problems scale has shown associations with diagnoses of generalized anxiety disorder and social anxiety disorder (Ebustani et al., 2010; Ferdinand et al., 2008; Nakamura et al., 2009). The six items on the Anxiety Problems scale are expected to capture generalized anxiety, social anxiety, and simple phobia; therefore this scale may be a measure of broad anxiety symptoms rather than a reflection of any one specific diagnosis (Nakamura et al., 2009). Future research may benefit from using broader measures of anxiety and depressive symptoms.
In addition, in the first set of analyses, 7 of 16 possible effects were significant when examining changes in symptoms of anxiety and depression by condition over time. However, it is noteworthy that given findings from previous reports of this sample (masked reference), it is not unexpected that findings would be limited to youth report of symptom change. In the second set of analyses, 7 of 32 (22%) possible effects were significant when examining the impact of initial levels of symptoms on symptom change. In the final set of analyses, 4 of 24 (17%) possible effects were significant when examining magnitude of change in one symptom predicting subsequent magnitude of change in the other. With multiple outcomes examined at multiple time points, there is a possibility that some significant findings emerge by chance, however, the number of findings are well above the expected rate of 5% that might occur by chance. It is noteworthy that the effects of change predicting subsequent change were predominantly found for the initial assessment points during (0–6 months) and immediately following (6–12 months) intervention. In addition, follow up assessment windows remained open for three months at a time, and therefore participants may have completed their 6-, 12-, 18-, and 24-month assessments at varying points within each follow up window (i.e., 6–9 months, etc.). It is worth noting LCS models could be expanded to accommodate individually varying measurement occasions using definition variable methodology (Sterba, 2014); however, this has not yet been done for LCS models. Furthermore, empirical investigations of the consequences of ignoring individual variation in measurement occasions for related models have indicated that the changes to estimates were small and did not alter substantive conclusions (see Blozis & Cho, 2008; Sterba, 2014). Finally, the current study sample was predominantly Euro-American, limiting the generalizability of findings across different racial and ethnic groups.
Taken together, the findings reported here have implications for transdiagnostic effects of a family-based preventive intervention for high-risk youth. It is important to note the context of these findings is a preventive intervention for children of depressed parents. Although there is a long history of research in the prevention of depression in at risk youth (see Brunwasser & Garber, 2015; Gladstone, Beardslee, & O’Connor, 2011), no studies of efforts in children of depressed parents have examined the dynamics of change among symptoms of anxiety and depression. Results from the present study suggest knowing both the initial levels of youth symptoms at the start of an intervention for these youth as well as understanding how their symptoms change over the course of the initial intervention can provide important information about subsequent symptom change. Initial levels of anxiety and depressive symptoms may be indicators of greater initial response to intervention in the prevention context across both sets of symptoms, indicating youth demonstrating elevated symptom levels may particularly receptive to learning skills to cope with and manage stress. Further, early change in anxiety symptoms may lead to greater decline in depressive symptom outcomes at subsequent intervals, suggesting the potential importance of identifying skills and strategies that target anxiety in the initial phase of an preventive intervention. Future research examining a sample that also includes children of parents with a history of anxiety may provide a broader understanding of how these symptoms are associated in high-risk youth.
Notably, the prevention program the FGCB families completed taught youth how to cope with uncontrollable stress, in this case, specifically the stress of living with a depressed parent (masked reference). Skills for coping with or adapting to uncontrollable stress include acceptance, distraction, engaging in fun activities, and cognitive reappraisal. A number of studies have demonstrated the association between coping and emotion regulation skills and internalizing psychopathology, including symptoms of anxiety and depression, in children and adolescents (e.g., Aldao & Nolen-Hoeksema, 2010; Bettis et al., 2015; Compas et al., 2014). Previous reports from the current trial found that coping was a mediator of mixed anxious/depressed symptoms in this sample (masked reference). These findings suggest that exploring how coping may impact the dynamics of change among anxiety and depression symptoms will be an important next step in this research. For example, exploring if specific coping skills map onto early anxiety symptom change vs. depression symptom change may guide the structure of future preventive interventions. Further, the second component of the intervention was a parenting skills component. Future research that examines how parenting may play a role in the dynamics between symptoms of anxiety and depression is needed. In addition, future research is needed to replicate the current findings and future research that explores whether the relations between changes in anxiety and depression are similar or different across intervention modalities (prevention vs. treatment; CBT vs. IPT) is an important next step. The present study highlights the importance of understanding the dynamics of symptoms of anxiety and depression over time in order to refine targets of transdiagnostic intervention.
Acknowledgments
This research was supported by Grants R01MH069940 and R01MH069928 from the National Institute of Mental Health and by a gift from Patricia and Rodes Hart.
Contributor Information
Alexandra H. Bettis, Vanderbilt University
Rex Forehand, University of Vermont.
Sonya K. Sterba, Vanderbilt University
Kris J. Preacher, Vanderbilt University
Bruce E. Compas, Vanderbilt University
References
Note. Citations for masked references have been removed.
- Achenbach TM, Dumenci L, Rescorla LA. DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of Clinical Child and Adolescent Psychology. 2003;32:328–340. doi: 10.1207/S15374424JCCP3203_02. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Avenevoli S, Swendsen J, He J, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54:37–44. doi: 10.1016/j.jaac.2014.10.010. http://dx.doi.org.proxy.library.vanderbilt.edu/10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett PM, Farrell LJ, Ollendick TH, Dadds M. Long-term outcomes of an Australian universal prevention trial of anxiety and depression symptoms in children and youth: An evaluation of the FRIENDS Program. Journal of Clinical Child and Adolescent Psychology. 2006;35:403–411. doi: 10.1207/s15374424jccp3503_5. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Sterba SK, Hallfors DD. Evaluating group-based interventions when control participants are ungrouped. Multivariate Behavioral Research. 2008;43(2):210–236. doi: 10.1080/00273170802034810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Wright EJ, Gladstone TRG, Forbes P. Long-term effects from a randomized trial of two public health preventive interventions for parental depression. Journal of Family Psychology. 2007;21:703–713. doi: 10.1037/0893-3200.21.4.703. http://dx.doi.org.proxy.library.vanderbilt.edu/10.1037/0893-3200.21.4.703. [DOI] [PubMed] [Google Scholar]
- Berman SL, Weems CF, Silverman WK, Kurtines WM. Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy. 2000;31(4):713–731. [Google Scholar]
- Bettis AH, Forehand R, McKee L, Dunbar JP, Watson KH, Compas BE. Testing specificity: Associations of stress and coping with symptoms of anxiety and depression in youth. Journal of Child and Family Studies. 2016;25(3):949–958. doi: 10.1007/s10826-015-0270-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blozis SA, Cho Y. Coding and centering of time in latent curve models in the presence of interindividual time heterogeneity. Structural Equation Modeling. 2008;15:413–433. [Google Scholar]
- Boots DP, Wareham J. Does controlling for comorbidity matter? DSM-Oriented scales and violent offending in Chicago youth. Aggressive Behavior. 2010;35:1–17. doi: 10.1002/ab.20338. Retrieved from http://search.proquest.com/docview/622197775?accountid=14816. [DOI] [PubMed] [Google Scholar]
- Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, Holder D. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(9):906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- Brunwasser SM, Garber J. Programs for the prevention of youth depression: Evaluation of efficacy, effectiveness, and readiness for dissemination. Journal of Clinical Child & Adolescent Psychology. 2015 doi: 10.1080/15374416.2015.1020541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu BC. Translating transdiagnostic approaches to children and adolescents. Cognitive and Behavioral Practice. 2012;19(1):1–4. doi: 10.1016/j.cbpra.2011.06.003. [DOI] [Google Scholar]
- Chu BC, Hoffman L, Johns A, Reyes-Portillo J, Hansford A. Transdiagnostic behavior therapy for bullying-related anxiety and depression: Initial development and pilot study. Cognitive and Behavioral Practice. 2015;22:415–429. doi: 10.1016/j.cbpra.2014.06.007. [DOI] [Google Scholar]
- Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Beardslee W, … Seeley J. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Archives of General Psychiatry. 2001;58:1127–1134. doi: 10.1001/archpsyc.58.12.1127. [DOI] [PubMed] [Google Scholar]
- Cole DA, Peeke LG, Martin JM, Truglio R, Seroczynski AD. A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of Consulting and Clinical Psychology. 1998;66(3):451–460. doi: 10.1037/0022-006X.66.3.451. [DOI] [PubMed] [Google Scholar]
- Compas BE, Jaser S, Dunbar JP, Watson KH, Bettis AH, Gruhn M, Williams E. Coping and emotion regulation from childhood to early adulthood: Points of convergence and divergence. Australian Journal of Psychology. 2014;66(2):71–81. doi: 10.1111/ajpy.12043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal patterns of anxiety from childhood to adulthood: The great smoky mountains study. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53:21–33. doi: 10.1016/j.jaac.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, … Team T. Predictors and moderators of acute outcome in the treatment for adolescents with depression study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(12):1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas SA, Goodman KL, Kundey SMA. Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology. 2013;9:123–149. doi: 10.1146/annurev-clinpsy-050212-185617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobson KS, Hopkins JA, Fata L, Scherrer M, Allan LC. The prevention of depression and anxiety in a sample of high-risk adolescents: A randomized control trial. Canadian Journal of School Psychology. 2010;25:291–310. doi: 10.1177/0829573510386449. [DOI] [Google Scholar]
- Dozois DJA, Seeds PM, Collins KA. Transdiagnostic approaches to the prevention of depression and anxiety. Journal of Cognitive Psychotherapy: An International Quarterly. 2009;23:44–59. doi: 10.1891/0889-8391.23.1.44. [DOI] [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura BJ, Chorpita BF, Higa-McMillan C, Weisz JR. Concurrent validity of the child behavior checklist DSM-oriented scales: Correspondence with DSM diagnoses and comparison to syndrome scales. Journal of Psychopathology and Behavioral Assessment. 2010;32:373–384. doi: 10.1007/s10862-009-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JR. The study of congruence in organizational behavior research: Critique and a proposed alternative. Organizational Behavior and Human Decision Processes. 1994;58:51–100. doi: 10.1006/obhd.1994.1029. [DOI] [Google Scholar]
- Edwards JR. Latent variable modeling in congruence research: Current problems and future directions. Organizational Research Methods. 2009;12:34–62. doi: 10.1177/1094428107308920. [DOI] [Google Scholar]
- Ehrenreich-May J, Bilek EL. The development of a transdiagnostic, cognitive behavioral group intervention for childhood anxiety disorders and co-occurring depression symptoms. Cognitive and Behavioral Practice. 2012;19(1):41–55. http://dx.doi.org.proxy.library.vanderbilt.edu/10.1016/j.cbpra.2011.02.003. [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … Barlow DH. Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy. 2012;43(3):666–678. doi: 10.1016/j.beth.2012.01.001. http://10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdinand RF. Validity of the CBCL/YSR DSM-IV scales anxiety problems and affective problems. Journal of Anxiety Disorders. 2008;22:126–134. doi: 10.1016/j.janxdis.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Flanery-Schroeder EC. Reducing anxiety to prevent depression. American Journal of Preventive Medicine. 2006;31:136–142. doi: 10.1016/j.amepre.2006.07.006. [DOI] [PubMed] [Google Scholar]
- Foster CE, Webster MC, Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, … King CA. Remission of maternal depression: Relations to family functioning and youth internalizing and externalizing symptoms. Journal of Clinical Child and Adolescent Psychology. 2008;37:714–724. doi: 10.1080/15374410802359726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Weersing VR. Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clinical Psychology Science and Practice. 2010;17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladstone TR, Beardslee WR, O’Connor EE. The prevention of adolescent depression. Psychiatry Clinics of North America. 2011;34(1):35–53. doi: 10.1016/j.psc.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant KE, Compas BE, Thurm AE, McMahon SD, Gipson PY. Stressors and child/adolescent psychopathology: Measurement issues and prospective effects. Journal of Clinical Child and Adolescent Psychology. 2004;33:412–425. doi: 10.1207/s15374424jccp3302_23. [DOI] [PubMed] [Google Scholar]
- Hale WM, Raaijmakers Q, Muris P, van Hoof A, Meeus W. One factor or two parallel processes? Comorbidity and development of adolescent anxiety and depressive disorder symptoms. Journal of Child Psychology and Psychiatry. 2009;50(10):1218–1226. doi: 10.1111/j.1469-7610.2009.02115.x. [DOI] [PubMed] [Google Scholar]
- Hamilton JL, Potter CM, Olino TM, Abramson LY, Heimberg RG, Alloy LB. The temporal sequence of social anxiety and depressive symptoms following interpersonal stressors during adolescence. Journal of Abnormal Child Psychology. 2015 doi: 10.1007/s10802-015-0049-0. [DOI] [PMC free article] [PubMed]
- Hedges L, Citkowicz M. Estimating effect size when there is clustering in one treatment group. Behavior Research Methods. 2015 doi: 10.3758/s13428-014-0538-z. [DOI] [PubMed] [Google Scholar]
- Hilton RC, Rengasamy M, Mansoor B, He J, Mayes T, Emslie GJ, … Brent DA. Impact of treatments for depression on comorbid anxiety, attentional, and behavioral symptoms in adolescents with selective serotonin reuptake inhibitor–resistant depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(5):482–492. doi: 10.1016/j.jaac.2013.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Feng X, Hipwell A, Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. Journal of Child Psychology and Psychiatry. 2009;50(9):1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. Journal of Abnormal Psychology. 2003;112:437–447. doi: 10.1037/0021-843X.112.3.437. [DOI] [PubMed] [Google Scholar]
- Laird RD, De Los Reyes A. Testing informant discrepancies as predictors of adolescent psychopathology: Why difference scores cannot tell you what you want to know and how polynomial regression may. Journal of Abnormal Child Psychology. 2013;41:1–14. doi: 10.1007/s10802-012-9659-y. [DOI] [PubMed] [Google Scholar]
- Laird RD, Weems CF. The equivalence of regression models using difference scores and models using separate scores for each informant: Implications for the study of informant discrepancies. Psychological Assessment. 2011;23:388–397. doi: 10.1037/a0021926. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Hopkins J, Gouze KR, Bryant FB. Bidirectional influences of anxiety and depression in young children. Journal of Abnormal Child Psychology. 2015;43:163–176. doi: 10.1007/s10802-014-9884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry-Webster H, Barrett PM, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: Preliminary data from an Australian study. Behaviour Change. 2001;18(1):36–50. http://0.1375/bech.18.1.36. [Google Scholar]
- Lowry-Webster H, Barrett PM, Lock S. A universal prevention trial of anxiety symptomology during childhood: Results at 1-year follow-up. Behaviour Change. 2003;20(1):25–43. http://10.1375/bech.20.1.25.24843. [Google Scholar]
- Martinsen KD, Kendall PC, Stark K, Neumer S. Prevention of anxiety and depression in children: Acceptability and feasibility of the transdiagnostic EMOTION program. Cognitive and Behavioral Practice. 2014 doi: 10.1016/j.cbpra.2014.06.005. [DOI]
- McArdle JJ, Hamagami F. Latent difference score structural models for linear dynamic analyses with incomplete longitudinal data. In: Collins L, Sayer A, editors. New methods for the analysis of change. Washington, DC: American Psychological Association; 2001. pp. 139–175. [Google Scholar]
- McArdle JJ, Nesselroade JR. Growth curve analysis in contemporary psychological research. In: Schinka J, Velicer W, editors. Handbook of psychology. Vol. 2. New York: Pergamon; 2003. pp. 447–480. [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendensen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Nakamura BJ, Ebesutani C, Bernstein A, Chorpita BF. A psychometric analysis of the Child Behavior Checklist DSM-oriented scales. Journal of Psychopathology and Behavioral Assessment. 2009;31:178–189. doi: 10.1007/s10862-008-9119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, Jarrett MA, Grills-Taquechel A, Hovey LD, Wolff JC. Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clinical Psychology Review. 2008;28(8):1447–1471. doi: 10.1016/j.cpr.2008.09.003. [DOI] [PubMed] [Google Scholar]
- O’Neil KA, Kendall PC. Role of comorbid depression and co-occurring depressive symptoms in outcomes for anxiety-disordered youth treated with cognitive-behavioral therapy. Child & Family Behavior Therapy. 2012;34:197–209. doi: 10.1080/07317107.2012.707086. [DOI] [Google Scholar]
- Queen AH, Barlow DH, Ehrenreich-May J. The trajectories of adolescent anxiety and depressive symptoms over the course of a transdiagnostic treatment. Journal of Anxiety Disorders. 2014;28:511–521. doi: 10.1016/j.janxdis.2014.05.007. [DOI] [PubMed] [Google Scholar]
- Ram N, Nesselroade JR. Modeling contextual effects in longitudinal studies. Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 2007. Modeling intraindividual and intracontextual change: Rendering developmental contextualism operational; pp. 325–342. [Google Scholar]
- Rapee RM, Lyneham HJ, Hudson JL, Kangas M, Wuthrich VM, Schniering CA. Effect of comorbidity on treatment of anxious children and adolescents: Results from a large, combined sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(1):47–56. doi: 10.1016/j.jaac.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Rohde P, Clarke GN, Lewinsohn PM, Seeley JR, Kaufman NK. Impact of comorbidity on a cognitive-behavioral group treatment for adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(7):795–802. doi: 10.1097/00004583-200107000-00014. http://10.1097/00004583-200107000-00014. [DOI] [PubMed] [Google Scholar]
- Roberts C, Kane R, Thomson H, Bishop B, Hart B. The prevention of depressive symptoms in rural school children: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2003;71(3):622–628. doi: 10.1037/0022-006X.71.3.622. [DOI] [PubMed] [Google Scholar]
- Schleider JL, Krause ED, Gillham JE. Sequential comorbidity of anxiety and depression in youth: Present knowledge and future directions. Current Psychiatry Reviews. 2014;10:75–87. doi: 10.2174/1573400509666131217010652. [DOI] [Google Scholar]
- Schumm JA, Dickstein BA, Walter KH, Owens GP, Chard KM. Changes in posttraumatic cognitions predict changes in posttraumatic stress disorder symptoms during cognitive processing therapy. Journal of Consulting and Clinical Psychology. 2015 doi: 10.1037/ccp0000040. [DOI] [PubMed]
- Seeley JR, Kosty DB, Farmer RF, Lewinsohn PM. The modeling of internalizing disorders on the basis of patterns of lifetime comorbidity: Associations with psychosocial functioning and psychiatric disorders among first-degree relatives. Journal of Abnormal Psychology. 2011;120(2):308–321. doi: 10.1037/a0022621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Mediation models for longitudinal data in developmental research. Research in Human Development. 2009;6(2–3):144–164. http://10.1080/15427600902911247. [Google Scholar]
- Seligman MEP, Schulman P, Tryon AM. Group prevention of depression and anxiety symptoms. Behaviour Research and Therapy. 2007;45(6):1111–1126. doi: 10.1016/j.brat.2006.09.010. http://10.1016/j.brat.2006.09.010. [DOI] [PubMed] [Google Scholar]
- Sellers R, Collishaw S, Rice F, Thaper AK, Potter R, Mars B, … Thapar A. Risk of psychopathology in adolescent offspring of mothers with psychopathology and recurrent depression. The British Journal of Psychiatry. 2013;202:108–114. doi: 10.1192/bjp.bp.111.104984. [DOI] [PubMed] [Google Scholar]
- Snyder J, Bullard L, Wagener A, Leong PK, Snyder J, Jenkins M. Childhood anxiety and depressive symptoms: Trajectories, relationship, and association with subsequent depression. Journal of Clinical Child and Adolescent Psychology. 2009;38(6):837–849. doi: 10.1080/15374410903258959. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow M, Kendall PC, Weersing VR. Examining outcome variability: Correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology. 2001;30(3):422–436. doi: 10.1207/S15374424JCCP3003_13. http://10.1207/S15374424JCCP3003_13. [DOI] [PubMed] [Google Scholar]
- Sterba SK. Fitting nonlinear latent growth curve models with individually varying time points. Structural Equation Modeling. 2014;21:630–647. [Google Scholar]
- Sterba SK. Partially nested designs in psychotherapy trials: A review of modeling developments. Psychotherapy Research. 2016 doi: 10.1080/10503307.2015.1114688. In press. [DOI] [PubMed] [Google Scholar]
- Sterba SK, Preacher KJ, Forehand R, Hardcastle EJ, Cole DA, Compas BE. Structural equation modeling approaches for analyzing partially nested data. Multivariate Behavioral Research. 2014;49:93–118. doi: 10.1080/00273171.2014.882253. [DOI] [PubMed] [Google Scholar]
- Tein J, Sandler IN, Ayers TS, Wolchik SA. Mediation of the effects of the family bereavement program on mental health problems of bereaved children and adolescents. Prevention Science. 2006;7(2):179–195. doi: 10.1007/s11121-006-0037-2. http://10.1007/s11121-006-0037-2. [DOI] [PubMed] [Google Scholar]
- Treatment for Adolescents With Depression Study (TADS) Team. Fluoxetine, Cognitive-Behavioral Therapy, and Their Combination for Adolescents With Depression: Treatment for Adolescents With Depression Study (TADS) Randomized Controlled Trial. JAMA. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- van Lang NDJ, Ferdinand RF, Oldehinkel AJ, Ormel J, Verhulst FC. Concurrent validity of the DSM-IV scales affective problems and anxiety problems of the youth self-report. Behaviour Research and Therapy. 2005;43(11):1485–1494. doi: 10.1016/j.brat.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, … Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. The New England Journal of Medicine. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. http://dx.doi.org.proxy.library.vanderbilt.edu/10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolchik SA, West SG, Sandler IN, Tein JY, Coatsworth D, Lengua L, … Griffin WA. An experimental evaluation of theory-based mother and mother–child programs for children of divorce. Journal of Consulting and Clinical Psychology. 2000;68:843–856. http://10.1037/0022-006X.68.5.843. [PubMed] [Google Scholar]
- Wolchik SA, Sandler IN, Millsap RE, Plummer BA, Greene SM, Anderson ER, … Haine RA. Six-year follow-up of preventive interventions for children of divorce. A randomized controlled trial. JAMA: Journal of the American Medical Association. 2002;288(15):1874–1881. doi: 10.1001/jama.288.15.1874. http://10.1001/jama.288.15.1874. [DOI] [PubMed] [Google Scholar]
- Young JF, Makover HB, Cohen JR, Mufson L, Gallop RJ, Benas JS. Interpersonal psychotherapy-adolescent skills training: Anxiety outcomes and impact of comorbidity. Journal of Clinical Child & Adolescent Psychology. 2012;41(5):640–653. doi: 10.1080/15374416.2012.704843. Retrieved from http://search.proquest.com/docview/1348796035?accountid=14816. [DOI] [PMC free article] [PubMed] [Google Scholar]