Abstract
Background
Fatigue and physical inactivity, critical problems facing cancer survivors, impact overall health and functioning. Our group designed a novel methodology to evaluate the temporal, dynamic patterns in real world settings.
Objective
Using real-time technology, describe and compare the temporal, dynamic relationship between real-time fatigue and free-living in cancer survivors who were treated with hematopoietic stem cell transplantation (n = 25) and age- and gender-matched healthy controls (n = 25).
Methods
Subjects wore wrist actigraphs on their non-dominant hand to assess free-living physical activity, measured in one-minute epochs, over seven days. Subjects entered real-time fatigue assessments directly into the subjective event marker of the actigraph five times per day. Running averages of mean one-minute activity counts 30, 60, and 120 minutes before and after each real-time fatigue score were correlated with real-time fatigue using generalized estimating equations,
Results
A strong inverse relationship exists between real-time fatigue and subsequent free-living physical activity. This inverse relationship suggests that increasing real-time fatigue limits subsequent physical activity (B range= −.002 to −.004; p<.001). No significant differences in the dynamic patterns of real-time fatigue and free-living physical activity were found between groups.
Conclusions
To our knowledge, this is the first study to document the temporal and potentially causal relationship between real-time fatigue and free-living physical activity in real-world setting. These findings suggest that fatigue drives the subsequent physical activity and the relationship may not be bi-directional.
Implications for Practice
Understanding the temporal, dynamic relationship may have important health implications for developing interventions to address fatigue in cancer survivors.
Introduction
Fatigue, a pervasive and distressing cancer symptom, impacts all aspects of a cancer survivor’s life. The more aggressive or intensive the cancer therapy, the more likely one is to develop fatigue.1–4 Hematopoietic stem cell transplantation (HCT) is considered curative for numerous hematologic malignancies, such as acute myeloid leukemia.5 HCT, including the preparatory high-dose chemotherapy with or without radiation therapy, is also a prime example of an intensive cancer treatment with a high propensity to result in persistent fatigue.6–9 Moderate to severe persistent fatigue occurs following HCT in over 40% of cancer survivors10–15; thus, there is a critical need to understand this distressing symptom and its impact on the lives of cancer survivors.
The exact cause of persistent fatigue is not known; however, severe, persistent fatigue in cancer survivors has been closely associated with reductions in physical activity.16–18 It is not known, however, if fatigue leads to reductions in physical activity or vice versa. This lack of understanding represents an important knowledge gap. Physical inactivity in HCT survivors is associated with a number of complications, including increased incidence of cardiovascular events.19,20 Though a few studies have documented persistent fatigue in long-term HCT survivors, no studies to our knowledge, other than our pilot work, objectively examined physical activity in HCT survivors.21 This may be due, in part, to the methodological difficulties associated with quantifying objective measures of physical activity in HCT survivors.
Understanding the interaction between fatigue and physical activity is crucial for reducing and/or mitigating poor outcomes in HCT survivors and vitally important for advancing symptom science. Fatigability has been introduced as a concept that integrates fatigue and physical activity. Fatigability is broadly defined as how fatigued or how fast one becomes fatigued while performing a standardized task or other measure of physical activity.22 This definition is distinct from the one commonly used in the exercise and neuromuscular literature to denote muscle endurance. While conceptual and operational definitions of the term are still evolving, most studies operationalize fatigability to include a subjective component (fatigue or change in perceived fatigue) in the context of performance on a standardized and/or objectively measured task.23,24 As a result of this operational definition, fatigability testing most frequently occurs in a clinical and/or laboratory environment. Findings from these types of measures, while important, do not provide information regarding the interplay between fatigue and physical activity in a natural environment.
In addition, the temporal, dynamic relationship between fatigue and physical activity requires further exploration to identify potential targets for therapeutic intervention. Examining the dynamic, temporal relationship in real-world settings would further our understanding. Ecological momentary assessment methodology (real-time technology) provides a means to capture these data in natural settings,25 such as real-time fatigue.26,27 Our group designed a novel method to assess the dynamic, temporal relationship between fatigue and physical activity using real-time data. Our proposed method is different from fatigability measures as it focuses on the relationship between real-time fatigue and free-living physical activity in real world settings using ecological momentary assessment technology; thus, minimizing the potential reactive effects of testing in a clinical or laboratory environment for physical activity as well as recall biases for fatigue. The purpose of this pilot study report is to (1) explain the methodology used to explore the relationship between real-time fatigue and free-living physical activity; and (2) describe and compare the temporal, dynamic relationship between real-time fatigue and free-living physical activity in HCT cancer survivors with persistent fatigue (n = 25) compared to age- and gender-matched healthy controls (n = 25), specifically examining the relationship between real-time fatigue and the physical activity that occurs 30, 60, and 120 minutes before and after each real-time fatigue rating. This pilot study was part of a parent study examining fatigue, physical activity, sleep, emotional distress, cognitive functioning, and biological measures in HCT survivors with persistent fatigue lasting more than 6 months compared to age- and gender-matched healthy controls with occasional tiredness that resolves with rest.21 The reader is referred to that article for a complete description of study procedures. The methods for exploring the dynamic relationship between real-time fatigue and free-living physical activity and the findings were not addressed or reported in the parent study.
Conceptual Framework
The parent study employed the Fatigue Adaptation Model as an organizing framework and guided the selection of potential biobehavioral correlates of persistent fatigue.28 Understanding the differences between occasional tiredness that occurs as part of everyday life and persistent fatigue in HCT survivors is a difficult problem facing researchers interested in studying fatigue in cancer survivors and clinicians who provide care. How does occasional tiredness experienced as part of everyday life differ from persistent fatigue experienced by HCT survivors? The Fatigue Adaptation Model suggests that tiredness, and fatigue represent distinct behavioral states that exist upon a continuum, with tiredness anchoring one end and exhaustion the other.28 Tiredness precedes fatigue, and fatigue precedes exhaustion. Differences in key biobehavioral domains, such as physical activity, sleep, emotional distress, and cognitive functioning, exist as one moves from tiredness to fatigue to exhaustion. The specific relationship between fatigue and physical activity, however, is complex; thus, establishing the need for this pilot study. Does fatigue lead to physical inactivity or physical inactivity lead to fatigue and/or is the relationship bi-directional? Determining if this relationship is different in HCT survivors and healthy controls and whether there is temporal precedence (fatigue precedes physical activity or vice versa) in real world settings would be an important step toward establishing causality.
Method
Design
This study used a prospective, comparative descriptive design to evaluate the relationship between real-time fatigue and free-living physical activity. Fatigue is defined as a subjective lack of physical and/or mental energy that is perceived as out proportion to recent activity and interferes with usual and desired activities over time despite adequate access to sleep or rest periods.29 Persistent fatigue in HCT survivors is operationalized as fatigue lasting more than six months and generally not relieved with rest. Subjects included HCT survivors with persistent fatigue (n = 25) and age- and gender-matched healthy controls with occasional tiredness that resolves with rest (n = 25). A wrist-worn accelerometer with a subjective event marker on the face of the device was used to capture patient-reported real-time fatigue and objective free-living physical activity. Subjects wore the device continuously for 7 days. Each subject produced a maximum of 35 real-time fatigue intensity ratings (5 ratings per day × 7 days) and 10,800 epochs of 1-minute physical activity counts (1,440 1-minute physical activity epochs per day × 7 days).
Sample
The sample (N = 50) included adult HCT survivors with persistent fatigue (n = 25) and age- and gender-matched healthy controls with occasional tiredness (n = 25). Subjects were recruited through local transplant programs (HCT survivors), local flyers, web advertisements (BMT Info Network – HCT Survivors; ResearchMatch – Healthy Controls), and word of mouth. All subjects were screened over the telephone to determine eligibility. Screening information was self-reported. Eligibility criteria for all subjects included: (1) at least 18 years of age; (2) able to ambulate without assistance; (3) no history of major psychiatric disorder; (4) no current major anxiety or depressive disorder; and, (5) no current diagnosis of a sleep disorder, such as sleep apnea. All shift workers, regardless of group, were excluded. Eligibility specific to healthy controls included: (1) self-reported occasional tiredness in the past 7 days; (2) tiredness generally relieved with rest; (3) no history of a chronic condition, such as diabetes, heart disease, cancer, etc.; and (4) no history of a condition in which fatigue is a common complication, such as multiple sclerosis. Healthy control subjects were excluded if they had any infectious, autoimmune/inflammatory diseases or were taking immunosuppressive medications. The healthy controls were matched to the HCT survivors by gender and age (within 5 years). Eligibility criteria specific to HCT survivors included: (1) complete remission of cancer for at least 1 year post allogeneic or autologous HCT; (2) self-reported persistent fatigue during the previous 6 months; and, (3) fatigue generally not relieved with rest. HCT survivors with severe acute graft-versus-host disease (Grade III and IV), extensive chronic graft-versus-host disease, and/or taking steroids for another medical condition were excluded from the study.
Setting
All data collection took place in the subject’s natural environment.
Instrumentation
Real-Time Fatigue
Real-time fatigue was measured with a 1-item, global fatigue intensity scale using computerized ecological momentary assessment (real-time assessment). The Actiwatch-Score® (Phillips Respironics, Bend, OR) contains a subjective event marker on the face of the physical activity monitor. The subjective event marker was used as a real-time, single-item, global, self-report scale to measure real-time fatigue intensity. Fatigue intensity scores range from 0 (no fatigue) to 10 (worst). Subjects enter the data directly into the subjective event marker of the wrist actigraph. This method of collecting real-time fatigue intensity ratings was chosen due to ease of use and ability to capture repeated real-time measurements of fatigue throughout the day. While numeric intensity ratings do not provide information regarding the multidimensional nature of fatigue, this 0 to 10 rating scale is suggested for use as a fatigue-screening device in clinical situations.29–31 A computerized ecological momentary assessment approach to collecting real-time fatigue data was employed to avoid problems with recall inaccuracies and objectively time-stamp real-time fatigue data entries.32 Data entered into the subjective event marker were stored in the onboard memory of the device. We successfully used this computerized methodological approach previously to assess real-time fatigue in HCT patients.27
Free-living physical activity
Physical activity was objectively measured using a wrist-worn accelerometer (Actiwatch-Score®, Philips Respironics, Bend, OR). The occurrence, degree, and magnitude of physical activity are captured via an omni-directional accelerometer. The piezoelectric motion sensor integrates degree and speed of motion and stores the information as activity counts in 1-minute epochs in the Actiwatch-Score® memory. The accelerometer is sensitive to < .01 g-force. Each 24-hour period produces 1440 one-minute epochs of physical activity counts. Intra-instrument and inter-instrument reliability for the wrist-worn accelerometer were established using a shaker table under 6 different conditions of various intensity,33 as well as concurrent validity in people with chronic illnesses.34 Wrist actigraphy has been successfully used in HCT patients, with expected reductions in physical activity immediately following HCT providing further support for convergent validity.35
Data Collection Schedule and Procedures
Institutional Review Board approval was obtained prior to subject engagement. Potential subjects responded to recruitment efforts as detailed above. Subjects self-identified as HCT survivors with persistent fatigue or healthy controls with occasional tiredness per the parent study.21 A telephone screening script was used to determine eligibility. Eligible potential subjects who expressed interest were mailed informed consent documents. Upon return of the signed written informed consent document, the wrist actigraph along with study instructions were shipped to subjects. Subjects were contacted by telephone to verify receipt and review study procedures. Subjects placed the device on their nondominant wrist. Subjects were instructed to wear the device continuously for the next 7 days and carry on with normal activities, including showering. Subjects were also asked to rate their fatigue intensity “at that moment in time” 5 times per day (upon awakening, 10:00 am, 2:00 pm, 6:00 pm, and at bedtimes). An activated audible alarm reminded subjects at preset times (10:00 am, 2:00 pm, and 6:00 pm) to complete the real-time fatigue assessments. Because of the expected time variability associated with awakening and going to bed, it was not possible to program the wrist actigraph to alarm at these times. Subjects entered the real-time rating directly into the subjective event marker of the wrist actigraph. At the end of data collection, subjects returned the device via a pre-postage paid box.
Method to Explore the Dynamic Relationship between Real-time Fatigue and Free-Living Physical Activity
Upon return of the wrist worn accelerometer, the real-time fatigue and physical activity data were downloaded using the Actiware® software (V. 6.0). The continuous 1-minute physical activity epochs and real-time fatigue intensity scores for all 7 days of data collection were exported to Excel and examined. Data were cleaned using the following rules: (1) each subject must have provided 7 days and 7 nights of real-time physical activity data, including weekday and weekend information; (2) only 7 days/nights of activity were included in the analysis; (3) subjects must have worn the device for a minimum of 14 hours during normal wake-time hours for the day to be included in this analysis; and (4) physical activity intervals of 120 minutes or more of 1-minute physical activity counts with a score of 0 during normal day-time hours (6:00 am to 10:00 pm) were excluded as off-wrist time. All real-time fatigue assessments were included in the analysis. Missing data were not replaced. One research team member reviewed the data for completeness and performed the initial cleaning of data. The PI (EH) reviewed all files to determine completeness and made the final decisions regarding data inclusion/exclusion. Using a system of moving averages in Excel, the 1-minute physical activity counts were averaged over 30, 60, and 120 minutes before and after each real-time fatigue score (see Figure 1).
Figure 1.
Real-Time Fatigue and Free-Living Physical Activity Sampling
PA: Physical Activity
Notes: Notes: The physical activity intervals (colored blocks) represent the physical activity counts before and after each real-time fatigue score averaged over: (1) 30 minutes (light); (2) 60 minutes (medium); and, (3) 120 minutes (dark).
Real-time fatigue and free-living physical activity upon awakening and at bedtime not illustrated due to time variability.
Data Analysis
Descriptive statistics were computed for all clinical and demographic characteristics. Generalized estimating equations were employed to examine temporal relationships between real-time fatigue scores and each of the 6 physical activity time intervals (mean 1-minute physical activity counts 30, 60, and 120 minutes before and after each real-time fatigue score). Generalized estimating equations control for biases estimates due to correlation problems.36,37 Because of the repeated measure nature of the data, we expect temporal correlations among mean one-minute physical activity counts across time intervals within subjects. To identify differences in dynamic relationship patterns between HCT survivors with persistent fatigue and healthy controls, separate generalized estimating equations for each of the 6 time intervals were computed using autoregressive 1st order correlational structure.
Results
Demographic and Clinical Characteristics
Demographic characteristics for all subjects and clinical characteristics for HCT survivors are displayed in Table 1. Briefly, the mean age of the sample was 52.8 (SD = 11.8) and consisted of 56% males (n = 28) and 44% females (n = 22). The majority of subjects were White (n = 42, 84%) and highly educated, completing some college (n = 13, 26%), graduated from college (n = 16, 32%) or graduate education (n = 17, 34%). The HCT survivors were transplanted for a variety of hematological malignancies. Most HCT survivors received an allogeneic transplant (n = 19, 76%).
Table 1.
Demographic Characteristics (N = 50)
| Characteristics | Value | ||
|---|---|---|---|
| Overall (N = 50) |
HCT Survivors (n = 25) |
Healthy Controls (n = 25) |
|
| Age, M (SD) | 52.8 (11.8) | 53.4 (11.5) | 52.3 (12.2) |
| Gender, N (%) | |||
| Male | 28 (56) | 14 (56) | 14 (56) |
| Female | 22 (44) | 11 (44) | 11 (44) |
| Race, N (%) | |||
| African American | 3 (6) | 3 (12) | |
| Asian | 1 (2) | 1 (4) | |
| Hispanic | 1 (2) | 1 (4) | |
| White | 42 (84) | 22 (88) | 20 (80) |
| Not Reported | 3 (6) | 3 (12) | |
| Education, N (%) | |||
| Graduated from High School | 2 (4) | 1 (4) | 1 (4) |
| Some College | 13 (26) | 4 (16) | 9 (36) |
| Graduated from College | 16 (32) | 10 (40) | 6 (24) |
| Graduate Education after College | 17 (34) | 8 (32) | 9 (36) |
| Not Reported | 2 (4) | 2 (8) | |
| Months from Transplant, M (SD) | 63 (52) | ||
| Months from Transplant, Median (Range) | 43 (13–238) | ||
| Diagnosis, N (%) | |||
| Acute Myelogenous/ Lymphoblastic Leukemia |
8 (32) | ||
| Chronic Myelogenous Leukemia | 2 (8) | ||
| Myelodysplastic Syndrome | 2 (8) | ||
| Lymphoma | 7 (28) | ||
| Multiple Myeloma | 3 (12) | ||
| Other | 3 (12) | ||
| Donor Type, N (%) | |||
| Autologous | 6 (24) | ||
| Sibling | 13 (52) | ||
| Matched Donor | 4 (16) | ||
| Haploidentical | 2 (8) | ||
Frequency and Diurnal Pattern of Real-Time Fatigue Ratings
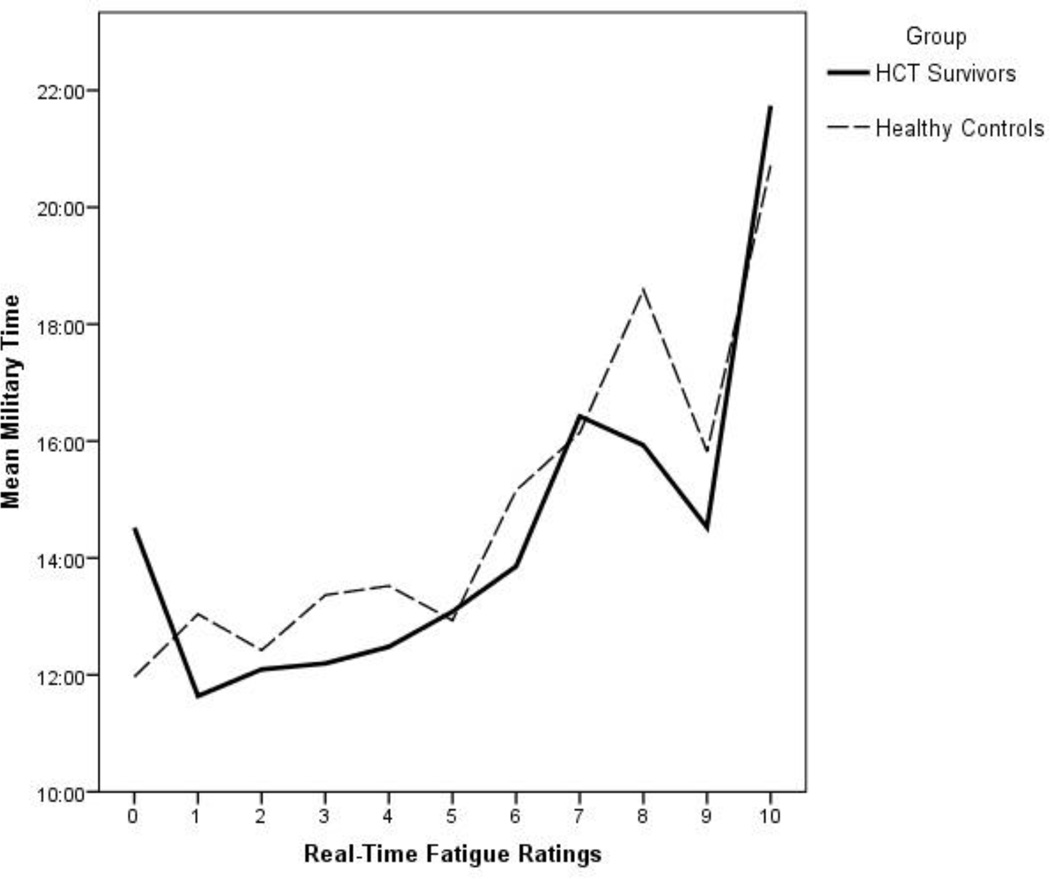
A total of 1414 real-time fatigue ratings were provided (HCT survivors, n = 692; healthy controls, n = 722). Subjects provided an average of 28 (80%) real-time fatigue ratings out of a possible 35 (SD = 5). There were no significant differences between groups on the number of real-time fatigue ratings provided. The frequency of the specific real-time fatigue ratings on a scale of 0 to 10 are displayed in Figure 2. The specific real-time fatigue ratings differ substantially between HCT survivors and healthy controls. The pattern reveals that HCT survivors more frequently report moderate to moderate/severe fatigue, while healthy controls more frequently report no fatigue or mild fatigue. Both groups reported a similar number of severe fatigue (ratings of 9 and 10). Figure 3 displays the diurnal pattern of real-time fatigue intensity scores. The mean time for reporting real-time fatigue scores of 0 (no fatigue) to 6 (high end of moderate fatigue) occurred in the early afternoon, while severe ratings of fatigue (7 to 10) occurred in the late evening.
Figure 2.
Frequency of Real-Time Fatigue Scores for HCT Survivors and Healthy Controls
Figure 3.
Timing of Real-Time Fatigue Scores in HCT Survivors and Healthy Controls
Dynamic Patterns of Real-Time Fatigue and Physical Activity (All Subjects)
Generalized estimating equations indicate that a significant inverse relationship exists between real-time fatigue and the mean 1-minute physical activity counts that occurred before or after real-time fatigue ratings for the following time intervals: (1) 60 minutes before real-time fatigue (B = −0.001, p = .006); (2) 30 minutes after real-time fatigue (B = −.002, p < .001); (3) 60 minutes after real-time fatigue (B = −.003, p < .001); and (4) 120 minutes after real-time fatigue (B = −.004, p < .001) (Table 2). The inverse relationship between real-time fatigue and mean 1-minute physical activity counts averaged over time became stronger as the time interval progressed up to 120 minutes following the real-time fatigue score.
Table 2.
Relationships between Real-Time Fatigue and Free-Living Physical Activity (Mean One-Minute Physical Activity Counts)
| Total Sample (HCT Survivors and Healthy Controls, N = 50) | ||||
|---|---|---|---|---|
| Parameter | B | Std. Error | Hypothesis Test | |
| Wald Chi- Square |
p value. | |||
| 120 minutes before | −.001 | .0004 | 2.214 | .137 |
| 60 minutes before* | −.001 | .0004 | 7.631 | .006 |
| 30 minutes before | −.001 | .0004 | 2.034 | .154 |
| 30 minutes after* | −.002 | .0004 | 26.438 | .000 |
| 60 minutes after* | −.003 | .0004 | 56.441 | .000 |
| 120 minutes after* | −.004 | .0005 | 68.761 | .000 |
| HCT survivors (n = 25) | ||||
| 120 minutes before | −.001 | .0006 | .780 | .377 |
| 60 minutes before | −.001 | .0005 | 3.330 | .068 |
| 30 minutes before | −.001 | .0005 | 2.169 | .141 |
| 30 minutes after* | −.002 | .0006 | 15.051 | .000 |
| 60 minutes after* | −.003 | .0005 | 31.779 | .000 |
| 120 minutes after* | −.004 | .0006 | 37.717 | .000 |
| Healthy Controls (n = 25) | ||||
| 120 minutes before | .000 | .0004 | .997 | .318 |
| 60 minutes before | −.001 | .0005 | 2.399 | .121 |
| 30 minutes before | .000 | .0005 | .294 | .588 |
| 30 minutes after* | −.002 | .0007 | 12.206 | .000 |
| 60 minutes after* | −.003 | .0006 | 25.249 | .000 |
| 120 minutes after* | −.004 | .0007 | 30.796 | .000 |
Note: Generalized Estimating Equations used to examine the relationship between real-time fatigue and the mean 1-minute physical activity counts that occurred before or after real-time fatigue ratings for the following time intervals: (1) 120 minutes before real-time fatigue; (2) 60 minutes before real-time fatigue; (3) 30 minutes before real-time fatigue; (4) 30 minutes after real-time fatigue; (5) 60 minutes after real-time fatigue; and, (6) 120 minutes after real-time.
Significant: p< .05
Comparison between HCT Survivors and Healthy Controls
Generalized estimating equations indicated no significant differences between groups for real-time fatigue and the mean 1-minute physical activity counts occurring 30, 60, and 120 minutes before and after real-time fatigue. Figure 4 displays the relationship between real-time fatigue and the mean 1-minute physical activity counts 30, 60, and 120 minutes, respectively, before the real-time fatigue score. No identifiable patterns were noted in either group. Figure 5 displays the relationship between real-time fatigue and the mean 1-minute physical activity counts 30, 60, and 120 minutes, respectively, after the real-time fatigue score. A strong pattern existed when the mean 1-minute physical activity counts (30, 60, and 120 minutes after real-time fatigue, respectively) were plotted against the real-time fatigue intensity ratings. The pattern suggests that greater real-time fatigue limits subsequent physical activity (30, 60, and 120 minutes after the rating) for both groups.
Figure 4.
Mean One-Minute Free-Living Physical Counts 30, 60, and 120 Minutes Before Real-Time Fatigue.
Figure 5.
Mean One-Minute Free-Living Physical Counts 30, 60, and 120 Minutes after Real-Time Fatigue.
Dynamic Patterns of Real-Time Fatigue and Physical Activity (HCT Survivors and Healthy Controls)
The relationship between real-time fatigue and free-living physical activity using generalized estimating equations was examined separately for each group (Table 2).
HCT Survivors
Generalized estimating equations indicated that a significant inverse relationship existed between real-time fatigue and the mean 1-minute physical activity counts that occurred after real-time fatigue score for the following intervals: (1) 30 minutes after real-time (B = −.002, p < .001); (2) 60 minutes after real-time fatigue (B = −.003, p < .001); and (3) 120 minutes after real-time fatigue (B = −.004, p < .001). All other relationships were non-significant.
Healthy Controls
Generalized estimating equations indicated that a significant inverse relationship existed between real-time fatigue and the mean 1-minute physical activity counts that occurred real-time fatigue for the following intervals: (1) 30 minutes after real-time fatigue (B = −.002, p < .001); (2) 60 minutes after real-time fatigue (B = −.003, p < .001); and (3) 120 minutes after real-time fatigue (B = −.004, p < .001). All other relationships were non-significant.
Discussion
This pilot study is the first, to our knowledge, to describe a novel methodology examining the temporal, dynamic relationship between real-time fatigue and free-living physical activity in real-world settings and then test this methodology in HCT survivors with persistent fatigue versus age- and gender-matched healthy controls. Study findings indicated that HCT survivors more frequently reported moderate and moderate to severe levels of real-time fatigue, while healthy controls more frequently reported no or mild fatigue. The real-time fatigue followed a diurnal pattern with fatigue worsening as the day progressed for HCT survivors and healthy controls. Most importantly, this study documents the relationship between real-time fatigue and free-living physical activity in the natural environment, as opposed to clinical and/or laboratory testing environments. The findings suggest: (1) there is an inverse relationship between real-time fatigue and free-living physical activity and (2) higher real-time fatigue temporally precedes reductions in subsequent physical activity. Free-living physical activity prior to the real-time fatigue scoring does not appear to play a significant role in the perception of fatigue. Additional study is required given the small sample. Even so, the findings may have important implications for persistent fatigue interventions in HCT survivors. More focus may need to be placed on the perception of fatigue rather than physical activity, a frequent target for reducing fatigue in HCT cancer survivors.
Although fatigue is highly distressing and pervasive in HCT survivors, very few research studies addressed whether the real-time fatigue experienced by HCT survivors is different from the fatigue experienced by the general public during everyday life. Furthermore, many fatigue instruments, such as the PROMIS instruments,38 ask subjects to evaluate their fatigue status retrospectively (i.e., fatigue during the past 7 days). This approach, while certainly valuable, requires subjects not only to remember their fatigue during the past week but also to average and evaluate these perceptions over time, a cognitively difficult task.
This study used an ecological momentary assessment approach to assess real-time fatigue repeatedly over time in the subjects’ natural environment, providing valuable insight into the dynamic nature of persistent fatigue in HCT survivors over the course of multiple consecutive days. More than 1400 real-time fatigue ratings were provided over 7 days by 25 HCT survivors and 25 healthy controls. The findings clearly indicated, as expected, that HCT survivors more frequently reported moderate and moderate to severe real-time fatigue and less frequently reported mild to moderate real-time fatigue. Conversely, healthy controls more frequently reported no to mild real-time fatigue and less frequently reported moderate or moderate to severe real-time fatigue. Surprisingly, less than 5% of all real-time fatigue ratings were in the very severe range for either group (ratings of 9 or 10: HCT survivors, n = 37; healthy controls, n = 29). The real-time fatigue findings may be important for developing interventions, given the potential to target fatigue based on timing, intensity, or both.
Fatigue and physical activity are frequently intertwined in the cancer survivor literature, although the temporal relationship is not clear. To begin addressing whether fatigue leads to changes in physical activity or vice versa, our methodology of using moving averages of objectively obtained free-living physical activity counts in the 30, 60, and 120 minutes before and after each real-time fatigue score provides researchers with a system to explore this relationship. Because the device to collect the real-time fatigue and free-living physical activity data is relatively non-intrusive (resembles a wrist watch), the findings are less likely to be influenced by artificial testing environments. General estimating equations, a statistical method that takes into account repeated measures of correlated observations, is ideal for analyzing the relationship among real-time fatigue and free-living physical activity.36,37 Most importantly, findings from studies that examine real-time fatigue and free-living physical activity using a method like this may provide essential information for designing interventions and explicating the underlying mechanisms of effective fatigue interventions in real-world settings. Furthermore, this method has widespread applicability for examining fatigue and physical activity across a broad range of clinical populations, given the non-intrusiveness of the data collection as well as the relatively straightforward method for analyzing the temporal, dynamic nature of the real-time fatigue and free-living physical activity.
Other researchers have examined the relationship between fatigue and physical activity to further understand how symptoms impact functional ability.39,40 Fatigability, a relatively new concept that integrates the interaction between fatigue and physical activity, has generated much research interest. Although fatigability is defined in multiple ways, Eldadah defined it as a characteristic that describes how fatigued one becomes in response to defined activity.22 Multiple methods for assessing fatigability have been introduced, but a gold standard has not emerged. Most measures of fatigability evaluate fatigue or change in self-reported fatigue (subjective component) in response to a defined objectively measured activity, such as the 6-minute walk.23,24 Self-report measures of fatigability have also been published.41
There are key similarities as well as differences in our approach to assessing the relationship between real-time fatigue and free-living physical activity and measuring fatigability (fatigability methods that include subjective and objective components). First, both approaches require subjects to self-report fatigue intensity levels in real-time or close to real-time. We asked subjects to rate their fatigue intensity level at “that moment in time.” Most fatigability measures require subjects to rate their fatigue in a similar manner, such as within a very short period of time (i.e., fatigue ratings before and after a specific task) or the change in fatigue from baseline to completion of a task. Incorporating objectively observed physical activity into the measure is another similarity. A key difference, however, is that most measures of fatigability specify a pre-defined activity task that is generally tested in a clinical or laboratory environment. Our approach assesses free-living physical activity in a natural environment and does not ask subjects to rate their fatigue in response or relation to any particular activity. Thus, though both approaches examine the relationship between real-time fatigue and physical activity, findings from studies that subjectively assess fatigue and objectively assess physical activity may be different, given the focus on standardized testing with fatigability measures versus free-living physical activity in our approach.
Our study produced valuable results but potential study limitations should be noted. First, our sample included 25 HCT survivors and 25 healthy controls, a relatively low sample size. Even so, the mean completion rate for real-time fatigue ratings was over 80%, indicating substantial compliance with research procedures. Only 2 of 50 subjects fell below 60% real-time fatigue completion rate. Second, this is the first report for our method to evaluate the relationship between real-time fatigue and free-living physical activity. As such, the methods must be subjected to further research and the findings from this study interpreted with caution. The study also relied on a global, single-item fatigue intensity rating scale. While this measurement does not address the multidimensional nature of fatigue, it is recommended for clinical screening. Lastly, the findings suggest that real-time fatigue limits subsequent physical activity. It is possible that just asking subjects to rate their fatigue intensity, regardless of their activity status in real-time, may make subjects more self-conscious of their fatigue status. The conscious evaluation of higher levels of fatigue may result in potentially limiting physical activity following the fatigue evaluation and vice versa. In future studies, it will be important to ask HCT survivors about how they perceive fatigue and physical activity to interact in their lives (i.e., do you limit physical activity because you fear becoming fatigued?).
Understanding real-time fatigue in HCT cancer survivors and the relationship between real-time fatigue and free-living physical activity is a ripe area for future research. Building upon our findings, a number of methodological strategies in future studies will further advance our knowledge. Increasing the sample size is an obvious and important first step. The inclusion of two control groups (HCT survivors with occasional tiredness and age- and gender-matched healthy controls with occasional tiredness) would strengthen the design considerably. The age- and gender-matched healthy controls with occasional tiredness would serve as a comparison to the general population while the HCT survivors with occasional tiredness would serve as a comparison to those who have received similar treatment. Additionally, the potential research implications from this study extend beyond the HCT cancer survivor population. This study was specifically designed to minimize subject burden and maximize compliance. The methods for evaluating the temporal, dynamic relationship between real-time fatigue and free-living physical activity are relatively straightforward. As a result, the aims and methods can be easily replicated in other clinical populations including those that experience long-standing problems with fatigue. The ability to examine fatigue and the relationship to physical activity in other equally challenging populations would extend the generalizability of our preliminary findings.
Conclusion
This study, the first to our knowledge, describes a novel methodology for exploring the temporal, dynamic relationship between real-time fatigue and free-living physical activity in real-world settings. A wrist actigraph with a subjective event marker was used to capture subjective real-time fatigue ratings and objective physical activity in HCT survivors and age- and gender-matched healthy controls over 7 days. HCT survivors more frequently reported moderate and moderate to severe levels of real-time fatigue, while healthy controls more frequently reported no or mild fatigue. Real-time fatigue worsens during the evening, following a diurnal pattern for both groups. The study findings provide preliminary evidence that an inverse relationship exists between real-time fatigue and free-living physical activity. Importantly, our data suggested that the relationship between real-time fatigue and free-living physical activity was unidirectional, with fatigue driving the subsequent physical activity. These findings must be interpreted with caution given the small sample size and novelty of the methodology. Even so, the study findings have important implications for designing interventions and explicating the underlying mechanisms of effective fatigue interventions. As the first study to document this temporal relationship between real-time fatigue and free-living physical activity in real-world settings among HCT survivors and healthy controls, additional study is required.
Acknowledgments
This study was supported in part by the National Cancer Institute, Alliance for Clinical Trials in Oncology grant, previously the Cancer and Leukemia Group B through Grant CA037447 (E. Hacker, PI) and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1TR000050. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors thank Kevin Grandfield, Publication Manager of the UIC Department of Biobehavioral Health Science, for editorial assistance.
Footnotes
Disclosures
There are no conflicts of interest.
REFERENCES
- 1.Servaes P, Verhagen S, Schreuder HW, Veth RP, Bleijenberg G. Fatigue after treatment for malignant and benign bone and soft tissue tumors. J. Pain Symptom Manage. 2003;26(6):1113–1122. doi: 10.1016/j.jpainsymman.2003.03.001. [DOI] [PubMed] [Google Scholar]
- 2.de Jong N, Candel MJ, Schouten HC, Abu-Saad HH, Courtens AM. Prevalence and course of fatigue in breast cancer patients receiving adjuvant chemotherapy. Ann. Oncol. 2004;15(6):896–905. doi: 10.1093/annonc/mdh229. [DOI] [PubMed] [Google Scholar]
- 3.Bower JE, Ganz PA, Desmond KA, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106(4):751–758. doi: 10.1002/cncr.21671. [DOI] [PubMed] [Google Scholar]
- 4.Woo B, Dibble SL, Piper BF, Keating SB, Weiss MC. Differences in fatigue by treatment methods in women with breast cancer. Oncol. Nurs. Forum. 1998;25(5):915–920. [PubMed] [Google Scholar]
- 5.Ljungman P, Bregni M, Brune M, et al. Allogeneic and autologous transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe 2009. Bone Marrow Transplant. Feb 45;(2):219–234. doi: 10.1038/bmt.2009.141. [DOI] [PubMed] [Google Scholar]
- 6.Grulke N, Albani C, Bailer H. Quality of life in patients before and after haematopoietic stem cell transplantation measured with the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Core Questionnaire QLQ-C30. Bone Marrow Transplant. 2012;47(4):473–482. doi: 10.1038/bmt.2011.107. [DOI] [PubMed] [Google Scholar]
- 7.Baker F, Zabora J, Polland A, Wingard J. Reintegration after bone marrow transplantation. Cancer Pract. 1999;7(4):190–197. doi: 10.1046/j.1523-5394.1999.74005.x. [DOI] [PubMed] [Google Scholar]
- 8.Mosher CE, DuHamel KN, Rini C, Corner G, Lam J, Redd WH. Quality of life concerns and depression among hematopoietic stem cell transplant survivors. Support. Care Cancer. 2011;19(9):1357–1365. doi: 10.1007/s00520-010-0958-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jim HS, Sutton SK, Jacobsen PB, Martin PJ, Flowers ME, Lee SJ. Risk factors for depression and fatigue among survivors of hematopoietic cell transplantation. Cancer. 2016;122(8):1290–1297. doi: 10.1002/cncr.29877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conner-Spady BL, Cumming C, Nabholtz JM, Jacobs P, Stewart D. A longitudinal prospective study of health-related quality of life in breast cancer patients following high-dose chemotherapy with autologous blood stem cell transplantation. Bone Marrow Transplant. 2005;36(3):251–259. doi: 10.1038/sj.bmt.1705032. [DOI] [PubMed] [Google Scholar]
- 11.Gielissen MF, Schattenberg AV, Verhagen CA, Rinkes MJ, Bremmers ME, Bleijenberg G. Experience of severe fatigue in long-term survivors of stem cell transplantation. Bone Marrow Transplant. 2007;39(10):595–603. doi: 10.1038/sj.bmt.1705624. [DOI] [PubMed] [Google Scholar]
- 12.Mosher CE, Redd WH, Rini CM, Burkhalter JE, Duhamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psychooncology. 2008 Aug 1; doi: 10.1002/pon.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andrykowski MA, Carpenter JS, Greiner CB, et al. Energy level and sleep quality following bone marrow transplantation. Bone Marrow Transplant. 1997;20(8):669–679. doi: 10.1038/sj.bmt.1700949. [DOI] [PubMed] [Google Scholar]
- 14.Andrykowski MA, Bishop MM, Hahn EA, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J. Clin. Oncol. 2005;23(3):599–608. doi: 10.1200/JCO.2005.03.189. [DOI] [PubMed] [Google Scholar]
- 15.Hjermstad MJ, Knobel H, Brinch L, et al. A prospective study of health-related quality of life, fatigue, anxiety and depression 3–5 years after stem cell transplantation. Bone Marrow Transplant. 2004;34(3):257–266. doi: 10.1038/sj.bmt.1704561. [DOI] [PubMed] [Google Scholar]
- 16.Servaes P, Verhagen S, Bleijenberg G. Determinants of chronic fatigue in disease-free breast cancer patients: a cross-sectional study. Ann. Oncol. 2002;13(4):589–598. doi: 10.1093/annonc/mdf082. [DOI] [PubMed] [Google Scholar]
- 17.Lynch BM, Cerin E, Newman B, Owen N. Physical activity, activity change, and their correlates in a population-based sample of colorectal cancer survivors. Ann. Behav. Med. 2007;34(2):135–143. doi: 10.1007/BF02872668. [DOI] [PubMed] [Google Scholar]
- 18.Winters-Stone KM, Bennett JA, Nail L, Schwartz A. Strength, physical activity, and age predict fatigue in older breast cancer survivors. Oncol. Nurs. Forum. 2008;35(5):815–821. doi: 10.1188/08.ONF.815-821. [DOI] [PubMed] [Google Scholar]
- 19.Tichelli A, Bhatia S, Socie G. Cardiac and cardiovascular consequences after haematopoietic stem cell transplantation. Br J Haematol. 2008;142(1):11–26. doi: 10.1111/j.1365-2141.2008.07165.x. [DOI] [PubMed] [Google Scholar]
- 20.Slater ME, Steinberger J, Ross JA, et al. Physical Activity, Fitness, and Cardiometabolic Risk Factors in Adult Survivors of Childhood Cancer with a History of Hematopoietic Cell Transplantation. Biol. Blood Marrow Transplant. 2015;21(7):1278–1283. doi: 10.1016/j.bbmt.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hacker ED, Fink AM, Peters T, Park C, Fantuzzi G, Rondelli D. Persistent Fatigue in Hematopoietic Stem Cell Transplantation Survivors. Cancer Nurs. 2016 Jun 21; doi: 10.1097/NCC.0000000000000405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eldadah BA. Fatigue and fatigability in older adults. PM & R : the journal of injury, function, and rehabilitation. 2010;2(5):406–413. doi: 10.1016/j.pmrj.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 23.Barbosa JF, Bruno SS, Cruz NS, de Oliveira JS, Ruaro JA, Guerra RO. Perceived fatigability and metabolic and energetic responses to 6-minute walk test in older women. Physiotherapy. 2016;102(3):294–299. doi: 10.1016/j.physio.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 24.Buchowski MS, Simmons SF, Whitaker LE, et al. Fatigability as a function of physical activity energy expenditure in older adults. Age. 2013;35(1):179–187. doi: 10.1007/s11357-011-9338-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 26.Curran SL, Beacham AO, Andrykowski MA. Ecological momentary assessment of fatigue following breast cancer treatment. J. Behav. Med. 2004;27(5):425–444. doi: 10.1023/b:jobm.0000047608.03692.0c. [DOI] [PubMed] [Google Scholar]
- 27.Hacker ED, Ferrans CE. Ecological momentary assessment of fatigue in patients receiving intensive cancer therapy. J. Pain Symptom Manage. 2007;33(3):267–275. doi: 10.1016/j.jpainsymman.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 28.Olson K. A new way of thinking about fatigue: a reconceptualization. Oncol Nurs Forum. 2007;34(1):93–99. doi: 10.1188/07.ONF.93-99. [DOI] [PubMed] [Google Scholar]
- 29.Berger AM, Abernethy AP, Atkinson A, et al. Cancer-related fatigue. J Natl Compr Canc Netw. 2010;8(8):904–931. doi: 10.6004/jnccn.2010.0067. [DOI] [PubMed] [Google Scholar]
- 30.Denlinger CS, Ligibel JA, Are M, et al. Survivorship: fatigue, version 1.2014. J. Natl. Compr. Canc. Netw. 2014;12(6):876–887. doi: 10.6004/jnccn.2014.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glaus A. Assessment of fatigue in cancer and non-cancer patients and in healthy individuals. Support. Care Cancer. 1993;1(6):305–315. doi: 10.1007/BF00364968. [DOI] [PubMed] [Google Scholar]
- 32.Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient non-compliance with paper diaries. BMJ. 2002;324(7347):1193–1194. doi: 10.1136/bmj.324.7347.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Esliger DW, Tremblay MS. Technical reliability assessment of three accelerometer models in a mechanical setup. Med Sci Sports Exerc. 2006;38(12):2173–2181. doi: 10.1249/01.mss.0000239394.55461.08. [DOI] [PubMed] [Google Scholar]
- 34.Steele BG, Holt L, Belza B, Ferris S, Lakshminaryan S, Buchner DM. Quantitating physical activity in COPD using a triaxial accelerometer. Chest. 2000;117(5):1359–1367. doi: 10.1378/chest.117.5.1359. [DOI] [PubMed] [Google Scholar]
- 35.Hacker ED, Ferrans C, Verlen E, et al. Fatigue and physical activity in patients undergoing hematopoietic stem cell transplant. Oncol Nurs Forum. 2006;33(3):614–624. doi: 10.1188/06.ONF.614-624. [DOI] [PubMed] [Google Scholar]
- 36.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 37.Hardin JW, Hilbe JM. Generalized Estimating Equations. 2nd. Boca Raton, FL: Chapman & Hall/CRC Press; 2012. [Google Scholar]
- 38.Garcia SF, Cella D, Clauser SB, et al. Standardizing patient-reported outcomes assessment in cancer clinical trials: a patient-reported outcomes measurement information system initiative. J. Clin. Oncol. 2007;25(32):5106–5112. doi: 10.1200/JCO.2007.12.2341. [DOI] [PubMed] [Google Scholar]
- 39.Murphy SL, Smith DM. Ecological measurement of fatigue and fatigability in older adults with osteoarthritis. J. Gerontol. A Biol. Sci. Med. Sci. 2010;65(2):184–189. doi: 10.1093/gerona/glp137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simonsick EM, Schrack JA, Glynn NW, Ferrucci L. Assessing fatigability in mobility-intact older adults. J. Am. Geriatr. Soc. 2014;62(2):347–351. doi: 10.1111/jgs.12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Glynn NW, Santanasto AJ, Simonsick EM, et al. The Pittsburgh Fatigability scale for older adults: development and validation. J. Am. Geriatr. Soc. 2015;63(1):130–135. doi: 10.1111/jgs.13191. [DOI] [PMC free article] [PubMed] [Google Scholar]