Abstract
To compare the treatment efficacy of spastic flatfoot surgery by 2 different surgical methods: nonfusion subtalar arthroereisis using subtalar joint stabilizer (SJS) and Dennyson–Fulford subtalar arthrodesis (D-FSA).
A total of 26 cases of ambulant children with cerebral palsy diagnosed as spastic flatfoot were surgically treated from January 2011 to December 2014. Preoperative and postoperative American Orthopedic Foot and Ankle Society-Ankle and Hindfoot (AOFAS-AH) scores, anteroposterior–talocalcaneal angles (ATAs), and lateral talar-first metatarsal angles (Meary angles) of the affected foot were recorded.
Among 12 children in the SJS group, the AOFAS-AH scores were median preoperative score of 61 (58–64) versus median postoperative score of 83 (75–92), with significant difference (P < .05). Of the 20 feet treated, only 1 foot developed occasional pain. Postoperative ATA was decreased from preoperative 35° (20°–50°) to 19° (12°–25°); lateral X-ray films showed that the Meary angle was decreased from preoperative 20° (15°–40°) to postoperative 0° (0°–3°). The differences in both findings were statistically significant (P < .05). Fourteen children (22 treated feet) formed the D-FSA group; all demonstrated fusion of the talocalcaneal joint; AOFAS-AH scores were median preoperative score of 61 (58–64) versus median postoperative score of 83 (75–92), with significant difference (P < .05). Only 1 foot had occasional pain. Postoperative ATA was decreased from preoperative 35° (20°–45°) to 16° (12°–25°); lateral X-ray films showed that the Meary angle was decreased from preoperative 19° (10°–40°) to postoperative 2° (0°–5°); the differences in both findings were statistically significant (P < .05).
Both nonfusion subtalar arthroereisis using SJS and D-FSA were effective for the surgical treatment of spastic flatfoot, with similar clinical outcomes.
Keywords: ambulant children with cerebral palsy, Dennyson–Fulford subtalar arthrodesis, nonfusion subtalar arthroereisis, spastic flatfoot
1. Introduction
Ambulant children with cerebral palsy (CP) often present with flatfoot and other musculoskeletal malformations mainly due to muscle spasm, muscle strength imbalance, bone anomaly, and joint capsule relaxation.[1] The pathological changes include the collapse of the medial longitudinal arch of the foot, forefoot supination, and hindfoot valgus.[2] The affected foot often progress into a rigid, painful, and severe deformity, and cause changes of the foot skin such as pressure ulcer, hallux valgus, etc. leading to serious clinical consequences.[3]
Aiona and Sussman[4] believed that the natural history of the spastic flatfoot begins with unbalanced muscles’ strength besides the subtalar joints, then contracture of the muscles causes skeletal changes like heel valgus and lateral displacement of the calcaneus. Upon further progression, secondary skeletal developmental malformation occurs complicated with osteoarthritis of the talocalcaneal joint, the talonavicular joint, and the metatarsophalangeal joint, thereby completely losing the potential of spontaneous relief.[5] With time this deformity becomes more rigid and the talus head is excessively protruded inducing pain and restricting shoe wear, and painful plantar corpus callosum changes occur, restricting independent walking distance or even completely losing walking ability.[6]
Treatments of the spastic flatfoot include conservative or surgical management. Conservative treatments[4] include the use of insole, ankle-foot orthosis (AFO), and the use of assistive devices. Botulinum injection and baclofen pump therapy have also been tried. But because of the weakness of the posterior tibial tendon and of the sustained spasm of peroneus, the therapeutic effects of conservative treatment for spastic flatfoot are poor.[7,8] Ultimately, the presence of pain and fixed deformities require surgical intervention.[9–12]
We used subtalar joint stabilizer (SJS) for subtalar arthroereisis and the Dennyson–Fulford subtalar arthrodesis (D-FSA) as surgical corrective procedures. Our study was based on the hypothesis that the spastic flatfoot can also be treated with SJS.
2. Methods
2.1. General information
Inclusion criteria: Ambulant children with grade I and grade II CP (according to the Gross Motor Function Classification System) were diagnosed with spastic flatfoot based on history, physical examination, and X-ray; foot surgery had not been previously performed; the affected foot was without bony deformities such as tarsal coalitions, vertical talus, etc.; foot pain was present and could not be relieved by conservative treatment.
Included subjects were treated from January 2011 to December 2014. Twelve patients (20 feet) were treated with SJS including 8 boys and 4 girls aged 5 to 12 years old (average 7.8 years old). Among them, 8 cases underwent bilateral surgery. The average follow-up time in the SJS group was 28.3 ± 7.9 months (20–48 months). In addition, 14 children (22 feet) were treated with D-FSA including 9 boys and 5 girls aged 6 to 15 years (average 9.2 years old). Among them, 8 cases underwent bilateral surgery. The average follow-up time in the D-FSA group was 31.9 ± 10.7 months (22–60 months).
This research was approved by the Medical ethics committee of Hunan provincial people's hospital.
2.2. Surgical approaches
General anesthesia was administered to all patients undergoing both surgeries and all the patients maintained a supine position during surgery. A lateral tarsal sinus approach was used for the children treated with the SJS. A skin incision of 1 to 2 cm was performed at the anterior–inferior tarsal sinus to the lateral malleolus and the soft tissue was bluntly dissected. The guiding needle was placed in the tarsal canal through the tarsal sinus. An appropriate size of the test mold was selected, and the appropriate size of stabilizer was placed with the foot in neutral position, assuring that the subtalar joint maintained a movement range of 30° to 40°. The precise placement of SJS was confirmed by fluoroscopy.
An oblique skin incision was performed along the normal dermatoglyphics above the anterior lateral tarsal sinus of the affected foot in patients who underwent D-FSA. The dorsal talar neck was completely exposed through the interval between the extensor longus digitorum and anterior tibial neurovascular bundle. The calcaneus was rotated under the talus, and the forefoot was maintained in the normal neutral position and plantarflexion. Under the assistance of fluoroscopy, the articulatio talonavicularis was confirmed, as well as the inserted position of the guiding needle along the direction from the talar neck to the calcaneus with about 5° in the anteroposterior position. The drill was first performed without tapping, and then hollow screws with the appropriate size (4.5 mm diameter) were screwed to maintain the position of the foot. Another incision was performed at the partes iliaca. The cancellous iliac bone was reserved. The lower surface of talus and the upper surface of the cartilage-free surface of the calcaneus were roughened by the raspatory. The cancellous iliac bone was transplanted to fill the tarsal sinus.
Muscle force adjustment surgery was additionally performed in all children. The Achilles tendon lengthening was performed in children with Achilles tendon tension in the 10 patients in the SJS group and 13 patients in the D-FSA group. Gastrocnemius tendon lengthening was performed in the remaining children who did not undergo the Achilles tendon lengthening. Peroneus lengthening was jointly performed in the children with peroneus tension in the SJS group and the D-FSA group for 8 and 10 cases, respectively.
2.3. Postoperative management
All children were stabilized with the long leg plaster cast for 4 weeks after surgery. The plaster cast was removed and replaced by hinged AFO in the SJS group 4 weeks later. The screws were routinely left in the tarsal sinus without removal if there were no symptoms in the children.
2.4. Efficacy assessment
The patients were reviewed in the outpatient department every 3 months after discharge for a year. Then a 6-monthly outpatient visit was requested. The clinical effects of the affected foot were assessed according to the American Orthopedic Foot and Ankle Society-Ankle and Hindfoot score (AOFAS-AH) by the same physician at every review in the outpatient department. X-ray examinations were performed every 3 months to compare the changes of the anteroposterior–talocalcaneal angle (ATA) and positive lateral talar-first metatarsal angle (Meary angle).
2.5. Statistical analysis
The data were analyzed by SPSS software, and the measurement data were represented as median (Min, Max). The Wilcoxon Signed Ranks Test was used to compare the difference of preoperative and postoperative scores and imaging parameters in each group, the Mann–Whitney test was used to compare the difference of preoperative and postoperative scores and imaging parameters between 2 groups, and the α value of 0.05 in 2-tailed test was considered as significant.
3. Results
All patients were followed up to 20 to 60 months with an average follow-up time of 30.2 ± 9.5 months. No wound-related problem or vital vascular and nerve injury was found during follow-up. One patient in each group complained of local pain. Both children had undergone bilateral surgery and the pain was present in 1 foot. The pain was relieved after the internal fixation removal surgery. Such a secondary surgery was not performed in the remaining children. Screw fracture appeared in only 1 patient (1 foot in the D-FSA group) during the follow-up period (Fig. 3). However, the pain and movement disorders were absent in all other patients and the family members did not request for the removal of the internal fixation. No loosening or fracture of the internal fixation devices were found in other patients. The postoperative pain and foot arrangement were largely improved in all patients. Children in the SJS group were followed up after surgery with AOFAS-AH scores: the median preoperative score was 61 (58–64), and the median postoperative score was 83 (75–92) (Table 1). There was a significant difference between the preoperative and postoperative scores (P < .05), and only 1 foot (as described earlier) had occasional pain. Postoperative ATA was decreased from preoperative 35° (20°–50°) to 19° (12°–25°). Lateral X-ray films showed that Meary angle was decreased from preoperative 20° (15°–40°) to 0° (0°–3°), and the differences in both angle findings were statistically significant (P < .05) (Fig. 1). All children in the D-FSA group had good fusion of the talocalcaneal joint, and the postoperative AOFAS-AH scores were as follows: median preoperative score was 61 (58–64) and median postoperative score was 83 (75–92) (Fig. 2). There was a significant difference between the preoperative and postoperative scores (P < .05), and only 1 foot (as described earlier) had occasional pain. Postoperative ATA was decreased from preoperative 35° (20°–45°) to postoperative 16° (12°–25°). Lateral X-ray films showed the Meary angle was decreased from preoperative 19° (10°–40°) to postoperative 2° (0°–5°), and the differences in both findings were statistically significant (P < .05) (Tables 1–5).
Figure 3.

Boy, aged 6, Case No. 1, bilateral spastic flatfoot, Gross Motor Function Classification System grade II. Screw fracture of the right foot was found at 18 months follow-up. Right foot American Orthopedic Foot and Ankle Society-Ankle and Hindfoot (AOFAS-AH) scoring was 58 points during the preoperative assessment and 75 points at the last (60 months) follow-up. The talocalcaneal angle was 35° during the preoperative assessment and 20° at the last follow-up. The Meary angle was 20° during the preoperative assessment and 2° at the last follow-up. Left foot AOFAS-AH scoring was 61 points during preoperative assessment and 83 points at the last follow-up. The talocalcaneal angle was 45° during the preoperative assessment and 25° at the last follow-up. The Meary angle was 24° during the preoperative assessment and 3° at the last follow-up.
Table 1.
Details of patients in the subtalar joint stabilizer group.

Figure 1.
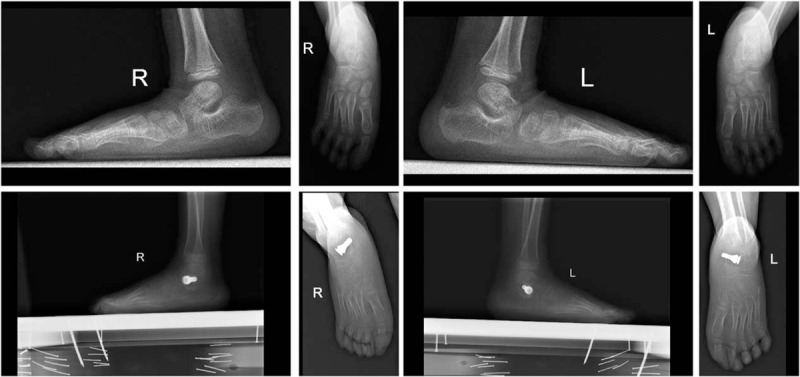
Boy, aged 6, Case No. 10, bilateral spastic flatfoot, Gross Motor Function Classification System grade II in the subtalar joint stabilizer group. Right foot American Orthopedic Foot and Ankle Society-Ankle and Hindfoot (AOFAS-AH) scoring was 64 points during preoperative assessment and 92 points at 30 months follow-up. The talocalcaneal angle was 30° in the preoperative assessment and 15° at 30 months follow-up. The Meary angle was 30° during the preoperative assessment and 0° at 30 months follow-up. Left foot AOFAS-AH scoring was 61 points during the preoperative assessment and 83 points at 30 months follow-up. The talocalcaneal angle was 40° during the preoperative assessment and 20° at 30 months follow-up. The Meary angle was 40° during the preoperative assessment and 0° at 30 months follow-up.
Figure 2.
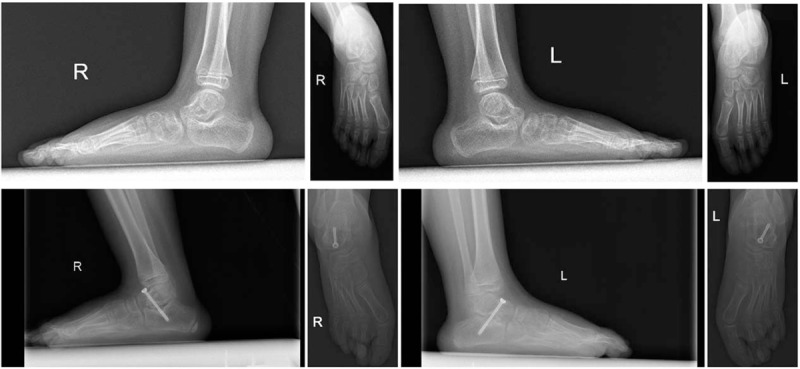
Boy, aged 6, Case No. 2, bilateral spastic flatfoot, Gross Motor Function Classification System grade I in the Dennyson–Fulford subtalar arthrodesis group. Right foot American Orthopedic Foot and Ankle Society-Ankle and Hindfoot (AOFAS-AH) scoring was 61 points during preoperative assessment and 75 points at 48 months follow-up. The talocalcaneal angle was 35° during the preoperative assessment and 15° at 48 months follow-up. The Meary angle was 15° during the preoperative assessment and 2° at 48 months follow-up. Left foot AOFAS-AH scoring was 64 points during the preoperative assessment and 75 points at 48 months follow-up. The talocalcaneal angle was 30° during the preoperative assessment and 20° at 48 months follow-up. The Meary angle was 24° during the preoperative assessment and 0° at 48 months follow-up.
Table 5.
Comparison of the improvement between the preoperative and postoperative indexes in the patients of the 2 groups.

Table 2.
Details of patients in the Dennyson–Fulford subtalar arthrodesis group.

Table 3.
The differences between the preoperative and postoperative indexes in patients of the subtalar joint stabilizer group.

Table 4.
The differences between the preoperative and postoperative indexes in patients of the Dennyson–Fulford subtalar arthrodesis group.

4. Discussion
Hefti et al[13] believed that if the pain of the spastic flatfoot is ignored for a long time, it would cause functional changes of the foot. When the medial weight-bearing area of the foot becomes obviously higher than the lateral side, surgical treatment should be considered.[14–16]
In 1946, Chambers[17] first proposed the idea of using autogenous bone to implant into the tarsal sinus to restrict the range of subtalar joint activity. Grice[18] used extra-articular subtalar arthrodesis combined with tarsal sinus bone graft to treat flatfoot children. LeLievre[19] proposed the method of implanting temporary staple into lateral subtalar joint for retardation. Afterward, Subotnick[20] first described the method of implanting rubber prosthesis into the tarsal sinus for subtalar joint retardation. Smith and Millar[21] used polyethylene screw implant into the tarsal sinus for subtalar joint retardation, and the success rate was 96%. Zaret and Myerson[22] treated 23 cases of flatfoot children using tapered implant for subtalar joint retardation, and the incidence of postoperative tarsal sinus pain was 18%. Vedantam et al[23] reported the application of polyethylene tarsal sinus screw in 78 cases of flatfoot children, and the satisfaction rate was as high as 96%, and no degradation occurred in the implant. Roth et al[24] treated 48 cases of flatfoot children by using screw implantation in tarsal sinus for subtalar joint retardation with an excellent rate of 91.5% at 5 years follow-up.
Although SJS has been widely applied in flatfoot children, the application in spastic flatfoot has rarely been reported. In this study, the Meary angles on the lateral radiographs of children in the SJS group could all be recovered to within 4° during follow-up visits. The anteroposterior radiographs showed that the calcaneal valgus was significantly better than before, and could be recovered to within 30°. This demonstrated that the foot force line was well restored, and the improvement rate of postoperative pain was 95%, reflecting the surgery had a good effect in treating spastic flatfoot. The literature has reported that the most common postoperative complications of SJS surgery were tarsal sinus pain, insufficient or excessive correction caused by inappropriate size of the stabilizer, too much intrusion or protrusion of the implants, related synovitis, vascular/nerve related injury, spontaneous fusion of subtalar joint, and talus neck fracture.[25] Black et al[26] used the implants designed by Viladot to treat flatfoot children, and the incidence of postoperative pain was 73%. But 36% of the children had to have their implants removed due to invalid correction. Afterward the implant was abandoned. Gutierrez and Lara[27] reported that postoperative supine immobilization could solve the problem of pain, but the time taken was long (1–4 months). The general treatment method was to remove the implant. Overcorrection was an important cause of tarsal sinus pain, and the solution was also implant removal.[28] In this study, only 1 patient had tarsal sinus pain, while other patients had no pain. The reasons might be that the appropriate size of the stabilizer, weakening of the valgus strength after the intramuscular lengthening of the peroneus brevis muscle in most patients, long postoperative plaster fixation time, and good healing of soft tissues. The patient who developed pain received bilateral surgery and the postoperative pain occurred only in 1 foot. Pain was not significantly improved after the outpatient use of nonsteroidal anti-inflammatory drugs, and the pain finally disappeared after the removal of the internal fixation. A possible reason might be that the patient did not receive intramuscular lengthening surgery of the peroneus brevis muscle, the sustained muscle spasms and body weight were both exerted to the foot, and the valgus strength was not controlled and eventually caused pain.
The D-FSA is one of the joint fusion surgeries, first used by Grice on the treatment of flatfoot[29] and the satisfactory rate was 78%. In 1977, Bratberg and Scheer[30] got their satisfactory rate up to 74% in 573 pediatric patients. In 1994, Hadley et al[31] reviewed 46 cases of pediatric patients, with a success rate of up to 70%, but with a false joint formation rate of about 6.4%. In 1976, Dennyson and Fulford[32] further proposed the use of a metallic internal fixation screw to reduce the incidence of false joint and the recurrence rate of the deformity. In our study, all patients achieved bony fusion at the last follow-up, and no false joint occurred. Meary angle on the lateral radiographs was found to be recovered from preoperative 20° to postoperative 1.7°, and the calcaneal valgus on the posteroanterior radiographs was found to be recovered from preoperative 33° to postoperative 17°. The foot force line was well restored, and the relief rate of postoperative pain was up to 95%. To avoid false joint formation, we suggest that the activity and flexibility of the subtalar joint should be clarified before surgery. The downward state of the talonavicular joint must be confirmed and maintained during the operation. Under the assistance of the fluoroscopy, the line between the long axis of the talus and navicular bone at the anteroposterior position should be maintained at the position of approximately 5° of the valgus. The position of the screw should be located at the dorsal side of the talus neck and in the gap between the extensor digitorum longus and the anterior tibial neurovascular bundle. The anterior tibial neurovascular bundle should be protected to avoid injury. All fat and soft tissues inside the tarsal sinus should be carefully cleaned before bone graft, and the lower surface of the talus and the nonarticular upper surface of the calcaneus should be roughened by the raspatory. The use of iliac cancellous bone graft for filling could effectively prevent the formation of false joint.
Our study results demonstrated that the SJS group as well as the D-FSA group had good therapeutic effect for the spastic flatfoot. Several aspects of AOFAS-AH scores, ATAs, and lateral Meary angles were significantly improved after operation, and the results were statistically significant. Comparison between the groups suggested that there were no significant difference in the improvement rate of the 2 methods, indicating that both the methods had their own advantages in the treatment of spastic flatfoot and close successful clinical effects. But the procedure of the SJS retained the activity of the talocalcaneal joint. If this method was invalid or caused pain, the patient could receive arthrodesis or other surgical treatment methods after the removal of the stabilizer. The patients who underwent D-FSA were treated with iliac bone graft, and due to more skin incisions compared with the SJS implantation, they had an increased risk of more complications, such as infection of the bone graft area, implant fracture, bone graft fusion failure, etc. In this study, 1 patient in D-FSA group had a screw fracture in 1 foot in the follow-up period (Fig. 3). But the child did not appear to have any symptoms of pain or disability. Thus, the internal fixation was not removed, and the patient is still being monitored for this during follow-up. In addition, we suggest that the contracture of peroneus brevis muscle of flatfoot children should be monitored before and during surgery to determine whether during the D-FSA procedure there was a need of peroneus brevis muscle lengthening in order to balance the force of the inner and outer strength of the foot. The follow-up time in our study was relatively short, and long-term status of the foot line could not be provided. We plan a further follow-up study where we would observe these indicators to get more detailed data.
5. Conclusions
In conclusion, both nonfusion subtalar arthroereisis and D-FSA had good therapeutic effects for spastic flatfoot. Three indicators of the 2 surgical methods before and after the operation were compared: there were no significant differences in the improvement degrees of the AOFAS-AH functional scores, ATAs, and Meary angles, indicating that the 2 methods had close clinical effects for spastic flatfoot.
Footnotes
Abbreviations: AFO = ankle-foot orthosis, AOFAS-AH = American Orthopedic Foot and Ankle Society-Ankle and Hindfoot, ATAs = anteroposterior–talocalcaneal angles, CP = cerebral palsy, D-FSA = Dennyson–Fulford subtalar arthrodesis, SJS = subtalar joint stabilizer.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Miller F. Cerebral Palsy-Section I, Part 11: Knee, Leg and Foot. 2004;New York, NY: Springer, 667–802. [Google Scholar]
- [2].Duffy C, Cosgrove A. The foot in cerebral palsy. Curr Orthop 2002;16:104–13. [Google Scholar]
- [3].Patterson RL, Jr, Parrish FF, Hathaway EN. Stabilizing operations on the foot; a study of the indications, techniques used, and end results. J Bone Joint Surg Am 1950;32A:1–26. [PubMed] [Google Scholar]
- [4].Aiona MD, Sussman MD. Treatment of spastic diplegia in patients with cerebral palsy: part II. J Pediatr Orthop B 2004;13:S13–38. [DOI] [PubMed] [Google Scholar]
- [5].Morrell DS, Pearson JM, Sauser DD. Progressive bone and joint abnormalities of the spine and lower extremities in cerebral palsy. Radiographics 2002;22:257–68. [DOI] [PubMed] [Google Scholar]
- [6].Fulford GE. Surgical management of ankle and foot deformities in cerebral palsy. Clin Orthop Relat Res 1990;55–61. [PubMed] [Google Scholar]
- [7].Kuhn DR, Shibley NJ, Austin WM, et al. Radiographic evaluation of weight-bearing orthotics and their effect on flexible pes planus. J Manipulative Physiol Ther 1999;22:221–6. [DOI] [PubMed] [Google Scholar]
- [8].Westberry DE, Davids JR, Shaver JC, et al. Impact of ankle-foot orthoses on static foot alignment in children with cerebral palsy. J Bone Joint Surg Am 2007;89:806–13. [DOI] [PubMed] [Google Scholar]
- [9].Rathjen KE, Mubarak SJ. Calcaneal-cuboid-cuneiform osteotomy for the correction of valgus foot deformities in children. J Pediatr Orthop 1998;18:775–82. [PubMed] [Google Scholar]
- [10].Alman BA, Craig CL, Zimbler S. Subtalar arthrodesis for stabilization of valgus hindfoot in patients with cerebral palsy. J Pediatr Orthop 1993;13:634–41. [PubMed] [Google Scholar]
- [11].Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot. Results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am 1995;77:500–12. [DOI] [PubMed] [Google Scholar]
- [12].Ireland ML, Hoffer M. Triple arthrodesis for children with spastic cerebral palsy. Dev Med Child Neurol 1985;27:623–7. [DOI] [PubMed] [Google Scholar]
- [13].Hefti F, Brunner R, Hasler CC. Pediatric Orthopedics in Practice. 2007;Berlin: Springer-Verlag, 408–418. [Google Scholar]
- [14].Dollard MD, Marcinko DE, Lazerson A, et al. The Evans calcaneal osteotomy for correction of flexible flatfoot syndrome. J Foot Surg 1984;23:291–301. [PubMed] [Google Scholar]
- [15].Andreacchio A, Orellana CA, Miller F, et al. Lateral column lengthening as treatment for planovalgus foot deformity in ambulatory children with spastic cerebral palsy. J Pediatr Orthop 2000;20:501–5. [PubMed] [Google Scholar]
- [16].Bourelle S, Cottalorda J, Gautheron V, et al. Extra-articular subtalar arthrodesis. A long-term follow-up in patients with cerebral palsy. J Bone Joint Surg Br 2004;86:737–42. [DOI] [PubMed] [Google Scholar]
- [17].Chambers EF. An operation for the correction of flexible flat feet of adolescents. West J Surg Obstet Gynecol 1946;54:77–86. [PubMed] [Google Scholar]
- [18].Grice DS. An extra-articular arthrodesis of the subastragalar joint for correction of paralytic flat feet in children. J Bone Joint Surg Am 1952;34A:927–40. [PubMed] [Google Scholar]
- [19].LeLievre J. Current concepts and correction in the valgus foot. Clin Orthop Relat Res 1970;70:43–55. [PubMed] [Google Scholar]
- [20].Subotnick SI. The subtalar joint lateral extra-articular arthroereisis: a follow-up report. J Am Podiatry Assoc 1977;67:157–71. [DOI] [PubMed] [Google Scholar]
- [21].Smith SD, Millar EA. Arthrorisis by means of a subtalar polyethylene peg implant for correction of hindfoot pronation in children. Clin Orthop Relat Res 1983;15–23. [PubMed] [Google Scholar]
- [22].Zaret DI, Myerson MS. Arthroerisis of the subtalar joint. Foot Ankle Clin 2003;8:605–17. [DOI] [PubMed] [Google Scholar]
- [23].Vedantam R, Capelli AM, Schoenecker PL. Subtalar arthroereisis for the correction of planovalgus foot in children with neuromuscular disorders. J Pediatr Orthop 1998;18:294–8. [PubMed] [Google Scholar]
- [24].Roth S, Sestan B, Tudor A, et al. Minimally invasive calcaneo-stop method for idiopathic, flexible pes planovalgus in children. Foot Ankle Int 2007;28:991–5. [DOI] [PubMed] [Google Scholar]
- [25].Needleman RL. Current topic review: subtalar arthroereisis for the correction of flexible flatfoot. Foot Ankle Int 2005;26:336–46. [DOI] [PubMed] [Google Scholar]
- [26].Black PR, Betts RP, Duckworth T, et al. The Viladot implant in flatfooted children. Foot Ankle Int 2000;21:478–81. [DOI] [PubMed] [Google Scholar]
- [27].Gutierrez PR, Lara MH. Giannini prosthesis for flatfoot. Foot Ankle Int 2005;26:918–26. [DOI] [PubMed] [Google Scholar]
- [28].Soomekh DJ, Baravarian B. Pediatric and adult flatfoot reconstruction: subtalar arthroereisis versus realignment osteotomy surgical options. Clin Podiatr Med Surg 2006;23:695–708. [DOI] [PubMed] [Google Scholar]
- [29].Grice DS. Further experience with extra-articular arthrodesis of the subtalar joint. J Bone Joint Surg Am 1955;37-A:246–59. [PubMed] [Google Scholar]
- [30].Bratberg JJ, Scheer GE. Extra-articular arthrodesis of the subtalar joint: a clinical study and review. Clin Orthop Relat Res 1977;220–4. [PubMed] [Google Scholar]
- [31].Hadley N, Rahm M, Cain TE. Dennyson–Fulford subtalar arthrodesis. J Pediatr Orthop 1994;14:363–8. [DOI] [PubMed] [Google Scholar]
- [32].Dennyson WG, Fulford GE. Subtalar arthrodesis by cancellous grafts and metallic internal fixation. J Bone Joint Surg Br 1976;58-B:507–10. [DOI] [PubMed] [Google Scholar]


