Abstract
Background
College students are a worldwide increasing group of young people at risk for suicidal thoughts and behaviours (STB). However, no previous studies have prospectively investigated the first onset of STB during the college period.
Methods
Using longitudinal data from the Leuven College Surveys, 2,337 (response rate [RR]=66.6%) incoming freshmen provided baseline data on STB, parental psychopathology, childhood-adolescent traumatic experiences, 12-month risk for mental disorders, and 12-month stressful experiences. A total of 1,253 baseline respondents provided data on 12-month STB in a two-year annual follow-up survey (conditional RR=53.6%; college dropout adjusted conditional RR=70.2%).
Results
One-year incidence of first-onset STB was 4.6–6.4%. Effect sizes of the included risk factors varied considerably whether viewed from individual-level (ORs 1.91–17.58) or population-level perspective (PARPs 3.4–34.3%). Dating violence prior to the age of 17, physical abuse prior to the age of 17, and 12-month betrayal by someone else than the partner were most strong predictors for first-onset suicidal ideation (ORs=4.23–12.25; PARPs=8.7–27.1%) and plans (ORs=6.57–17.58; PARPs=15.2–34.3%). Multivariate prediction (AUC=.84–.91) revealed that 50.7–65.7% of first-onset STB cases were concentrated in the 10% at highest predicted risk.
Limitations
As this is a first investigation of STB onset in college, future studies should use validation samples to test the accuracy of our multivariate prediction model.
Conclusions
The first onset of STB in college appears to be higher than in the general population. Screening at college entrance is a promising strategy to identify those students at highest prospective risk, enabling the cost-efficient clinical assessment of young adults in college.
Keywords: college student, suicidal ideation, suicide plan, prediction model, population-level risk, individual-level risk
INTRODUCTION
Suicide is the second leading worldwide cause of death for individuals between 15–29 years old (WHO, 2016). A growing subpopulation of these young people consists of college students (OECD, 2012). Suicidal thoughts and behaviours (STB) are common among college students, with 12-month suicidal ideation estimates (either defined as broad ideation or as seriously considering suicide) in the 5–35% range (Robins and Fiske, 2009; Wong et al., 2011), and 12-month suicide attempts ranging between 0.6–11% (Chou et al., 2013; Eisenberg et al., 2013). In response to these alarming statistics, a broad array of prevention interventions have been developed and implemented in colleges worldwide. However, a recent Cochrane review (Harrod et al., 2014) found little evidence that these programs lead to reductions in suicidality.
One explanation for this finding may be that STB risk factors are generally derived from cross-sectional studies that do not distinguish between those students with an onset of STB prior to or after matriculation. College entrance marks the transition from adolescence to “emerging adulthood”, a distinct developmental period characterized by increased autonomy, new social and academic challenges, and continued exploration of possible life directions (Arnett, 2015; Cleary et al., 2011). Interestingly, previous research has found different trajectories of STB in early life (Boeninger et al., 2010; Musci et al., 2015; Rueter et al., 2008), suggesting that risk for STB not only differs by age (Nock et al., 2012) but also as a function of developmental stage (Nkansah-Amankra, 2013). Therefore, an important but unexplored issue in college STB research may be the identification of true risk factors (as opposed to correlates) for a first onset of STB during the college period. As defined by Kraemer et al. (1997) risk factors should effectively split non-suicidal students at college entrance into high and low risk groups, and should be significantly associated with a subsequent first lifetime occurrence of STB during the college years. Identifying such reliable prospective predictors of first-onset STB would facilitate the implementation of targeted evidence-based interventions.
Two additional shortcomings relate to the way risk for STB has been studied. First, previous studies have exclusively provided individual-level effect sizes for risk factors. This does not account for a population-level perspective (Christensen et al., 2016; Drum and Denmark, 2012), which finds that high-prevalence risk factors carrying low individual risk for STB may be equally or even more important to consider as low-prevalence risk factors carrying high risk for the affected individuals (Bruffaerts et al., 2015). This can be evaluated by calculating population attributable risk proportions (PARP; Krysinska and Martin, 2009), thus allowing the risk factors that potentially contribute most to the onset of STB in student populations to be identified. This is important, as it is the combination of both individual- and population-level interventions (Rose, 2008) that has shown to be successful in reducing adverse outcomes with complex multicausal aetiologies such as cardiovascular disease (Taylor et al., 2006), and even STB among the active duty US Air force population (Knox, 2014). Second, most previous studies have failed to evaluate multivariate prediction models based on longitudinal approaches. As has recently been shown for post-traumatic stress disorder (Kessler et al., 2014) and suicide among US Army Soldiers (Kessler et al., 2016), accurate prediction models for the onset of STB could enable the successful targeting of students at highest risk for STB, improving the cost-effectiveness of current interventions. As STB are determined by a large number of distal and proximal risk factors (Knox, 2014) - a number that increases with more severe suicidal outcomes (Van Orden et al., 2010) - it is important to take into account a broad array of risk factors when developing prospective prediction models (Nock, 2016).
In the present study, we address each of these limitations by investigating a broad range of risk factors at college entrance as predictors for subsequent first-onset STB (i.e., a first lifetime occurrence of STB) during the first two college years. Longitudinal data were obtained from the Leuven College Surveys (LCS, 2015), which is part of the WHO World Mental Health Surveys International College Student project (WMH-ICS, 2015). Predictors included in this study are well-established risk factors for STB (Nock et al., 2012) that have also shown to be related to college STB: parental psychopathology (Abramson et al., 1998; Wilcox et al., 2010), early traumatic experiences (Gibb et al., 2001; Zhang and Tao, 2013), mental disorders (Paul et al., 2015; Whitlock et al., 2013), and recent stressful experiences (Chou et al., 2013; You et al., 2014). We build on earlier LCS studies that found self-injurious behaviours to be widespread among incoming freshmen (Kiekens et al., 2016; Mortier et al., 2015). The current study’s objectives are to: (1) estimate one-year incidence proportions of first-onset STB during college, (2) evaluate individual-level and population-level risk for first-onset STB, and (3) test a multivariate model for first-onset STB in terms of prediction accuracy.
METHODS
Procedures
The LCS consists of a series of ongoing web-based self-report surveys of KU Leuven students. Representing Belgium’s largest university, the KU Leuven has an enrolment of over 40,000 students. In the academic year 2012, a total of 3,510 Dutch-speaking incoming freshmen aged 18 years or older were eligible for the baseline survey. The sample was recruited in three stages. In the first stage, the baseline survey was included in a routine psychomedical check-up organized by the university. All incoming freshmen (i.e., census sampling) were sent a standard invitation letter for the check-up. Participants completed the survey on a desktop computer in the waiting room of the student health centre. In a second stage, non-respondents to the first stage were personally contacted using customized emails containing unique electronic links to the survey. The third stage was identical to the second stage, but additionally, included an incentive to complete the survey (i.e., a raffle for 20 euro store credit coupons). Each stage used reminder emails, setting the maximum amount of contacts at eight. The study’s protocol was approved by the University Hospital Leuven Biomedical Ethical Board (B322201215611). Informed consent was obtained from all subjects who participated in the study. Students who reported any past year STB or non-suicidal self-injury were presented with links to local mental health resources.
A total of 2,337 students completed the baseline survey, equivalent to a baseline response rate (RR) of 66.6% (76.7% when adjusting for non-participation due to college dropout). Students were contacted for the follow-up survey 12 and 24 months after the baseline assessment, using a similar sampling design to the one used at baseline. Personalized emails with unique electronic links to the survey were sent, including up to seven reminder emails. Beginning with the fifth reminder email, emphasis was put on a 20 euro store credit coupon raffle. A total of 1,253 of the original baseline respondents responded to at least one follow-up survey, equivalent to a conditional follow-up rate of 53.6% (70.2% when adjusting for non-participation due to college dropout). Reporting STB in a previous wave was not predictive for nonresponse in a subsequent wave (follow-up 1 vs. baseline: χ21=0.59, p=.44; follow-up 2 vs. follow-up 1: χ21=2.41, p=.12), suggesting attrition rates of the STB cases were equivalent to the full sample.
Measures
The WMH-ICS survey instrument was developed by the World Mental Health Survey Consortium to include multiple screening instruments measuring a wide range of mental health outcomes. Each of the included areas of assessment for this study is briefly reviewed in the remainder of this section.
Socio-demographic variables
Information about freshman socio-demographic characteristics was obtained from the KU Leuven students’ administration office and included gender, age, nationality, parents’ financial situation, parental education, parental familial composition, university group membership, and secondary school educational type. Survey items assessed sexual orientation and living situation at college.
Suicidal thoughts and behaviours (STB)
STB items were taken from the Self-Injurious Thoughts and Behaviours Interview (SITBI; Nock et al., 2007). STB was conceptualized as a continuum (Nock et al., 2012), starting with suicidal ideation (“Did you ever in your life have thoughts of killing yourself?”), possibly accompanied by a suicide plan (“Did you ever think about how you might kill yourself [e.g., taking pills, shooting yourself] or work out a plan of how to kill yourself?”), and then leading in some cases to a suicide attempt (“Have you ever made a suicide attempt [i.e., purposefully hurt yourself with at least some intent to die]?”). Suicidal ideation was clearly differentiated from a mere death wish (“Did you ever wish you were dead or would go to sleep and never wake up?”). Past year occurrence of the separate STB outcomes was derived from additional items that assessed age of onset and offset. Construct validity of the SITBI is good to excellent compared with the Schedule for Affective Disorders and Schizophrenia for School Aged Children (K–SADS–PL; κ=0.48–0.65), and the Beck Scale for Suicide Ideation (BSI; κ=0.59). Inter-rater reliability and test-retest reliability after 6-month follow-up are good to excellent (κ=0.7–1.0; Nock et al., 2007).
Parental psychopathology and traumatic experiences in childhood-adolescence
Parental psychopathology and traumatic experiences in childhood-adolescence (i.e. prior to the age of 17) were assessed using 19 items adapted from the CIDI-3.0 childhood section (Kessler and Ustun, 2004), the Adverse Childhood Experience Scale (Felitti et al., 1998), and the Bully Survey (Swearer and Cary, 2003). Items assessed parental psychopathology (e.g., “One of your parents had a serious emotional or mental health problem”), physical abuse (e.g., “Someone in your family hit you so hard that it left bruises or marks”), emotional abuse (e.g., “Someone in your family repeatedly said hurtful or insulting things to you”), sexual abuse (e.g., “Someone in your family touched you or made you touch them in a sexual way against your will”), neglect (e.g., “Nobody took care of you or protected you or made sure you had the things you needed”), bully victimization (e.g., “Someone at school purposefully ignored you, excluded you, or spread rumours about you behind your back”), and dating violence (e.g., “You were in a romantic relationship where your partner repeatedly hit you or hurt you”). Response options consisted of five-point Likert-type items (“never”, “rarely”, “sometimes”, “often”, and “very often”). Confirmatory factor analysis using our data showed excellent validity of the internal screener structure (Comparative Fit Index=0.991; Tucker-Lewis Index=0.988; Root Mean Square Error of Approximation=0.019). To obtain dichotomously coded variables, cut-off values consisted of “rarely” for all items, except bully victimization which had a cut-off of “sometimes” (Nansel et al., 2001).
Risk for 12-month mental disorder
Risk for 12-month mental disorder was assessed with the Global Appraisal of Individual Needs Short Screener (GAIN-SS; Dennis et al., 2006) including: internalizing disorders (depression, anxiety, sleep problems, post-traumatic stress, and suicidal ideation), externalizing disorders (attention deficit, hyperactivity/impulsivity, and conduct problems), substance disorders (abuse and dependence symptoms), and crime/violence related disorders (drug-related, property, and interpersonal crime). The GAIN-SS sub-screeners are very strongly correlated with the original corresponding subscales of the 60–120 minute DSM-IV-TR based GAIN structured interview (Pearson r=0.84–0.93; Dennis et al., 2006). Confirmatory factor analysis using our data showed a very good validity of the internal GAIN-SS structure (Comparative Fit Index=0.956; Tucker-Lewis Index=0.950; Root Mean Square Error of Approximation=0.032). For each screener, the recommended cut-off score for the highest probability of a 12-month diagnosis was used, i.e., three or more positive past year symptoms. The GAIN-internalizing sub-screener was adapted by eliminating the fifth item (i.e., suicidal ideation or attempt) due to overlap with the study’s outcome variables. We also assessed risk for other mental disorders or symptoms. Episodes of (hypo)mania and of intermittent explosive disorder were assessed using two items from the screener section of the Composite International Diagnostic Interview, third version (CIDI-3.0; Kessler and Ustun, 2004). Past year eating disorder symptoms (i.e., binge eating and purging behaviour) were assessed with two items taken from the Mini International Neuropsychiatric Interview Screen (Sheehan et al., 1998). Past year psychotic symptoms (i.e., hallucinations and delusions) included two items taken from the CIDI-3.0 Psychosis Screener (Haro et al., 2006). Non-suicidal self-injury was assessed with the corresponding item from the SITBI (cf. above; Nock et al., 2007) that asked students “Did you ever do something to hurt yourself on purpose, without wanting to die (e.g., cutting yourself, hitting yourself, or burning yourself)?” The SITBI construct validity for NSSI is good (κ=0.74), with excellent inter-rater reliability and test-retest reliability after 6-month follow-up (Nock et al., 2007).
Stressful events experienced in the past 12-months
Stressful events experienced in the past 12-months were assessed using 12 items taken from well-validated screeners, i.e., the Life Events Questionnaire (Brugha and Cragg, 1990), the Deployment Risk and Resilience Inventory (Vogt et al., 2008), and the Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel (Bray and Hourani, 2007). Items selected assessed relevant stressful experiences among young adults, including life-threatening illness or injury of a family member or close friend (Stoeckel and Weissbrod, 2015), accidents or death of a family member or close friend (Rostila et al., 2016), interpersonal events (e.g., break-up with a romantic partner, serious betrayal by someone other than one’s partner; Buitron et al., 2016), physical or sexual assault (Trotman et al., 2015; Viswanathan et al., 2014), and legal problems (e.g., time spent in jail; Salekin, 2008).
Analyses
All analyses were performed with R (version 0.98.1103), and SAS (version 9.4). Due to unit- and item-nonresponse, appropriate missing data handling strategies were implemented. First, nonresponse propensity weights (Rosenbaum and Rubin, 1983) were used to adjust for possible bias caused by final nonresponse, using the extensive sociodemographic information available for the original sampling frame. Second, multiple imputation by chained equations (van Buuren, 2007) was used to adjust for survey attrition and within-survey item nonresponse. The mice() package (van Buuren, 2012) available for R was used for that purpose, which allows for the extensive testing and specification of imputation models. The final data consisted of 200 imputed datasets with 2,337 cases in each dataset, obtained after 100 iterations of the mice algorithm. This approach enabled us to obtain estimates representative of the full student population, and to make appropriate estimates of standard errors that took into consideration the increased uncertainty introduced by imputing missing values.
Prevalence and incidence are reported as weighted proportions (%) and associated standard errors (SE). One-year STB incidence proportions were calculated by using first-onset STB follow-up cases as the numerator, and cases in which respondents never experienced STB in the previous wave as the denominator. Logistic regression parameters were used to test the individual-level strength of the associations between baseline risk factors and the different STB outcomes. To ensure that only associations with first-onset cases of STB were estimated, cases with any STB at baseline were eliminated from these analyses. Association measures are reported as odds ratios (OR) and associated 95% confidence intervals (95% CI). To estimate the population-level impact of baseline risk factors on subsequent onset of STB, PARPs (Krysinska and Martin, 2009) were calculated using as a summary predictor the predicted probabilities resulting from the logistic regression equations (Nock et al., 2012). Theoretically, PARPs provide estimates of the proportion of cases that are preventable if causal risk factors in the population under study were not present. Given the complex multifactorial aetiology of STB, PARPs in this study are best interpreted as the amount of cases that are potentially attributable to a particular risk factor.
Finally, a multivariate model including all risk factors was estimated. Nagelkerke pseudo-R2 was used as a measure of total effect size. Individual-level predicted STB probabilities based on the multivariate equation were created, receiver operating characteristic (ROC) curves generated, and area under the curve (AUC) values calculated to evaluate prediction accuracy. Predicted probabilities were then discretized into deciles (10 groups of equal size ordered by percentiles) and cross-classified with observed STB outcomes to visualize the concentration of risk associated with high composite predicted probabilities.
Results
Incidence proportions of first-onset STB during college
The first-onset of suicidal ideation - among those 2,042 students without any history of STB at baseline (87.4% [SE=0.5] of the total sample) - was estimated at 3.7% (SE=0.6) in year 1, and 3.9% (SE=0.6) in year 2. Suicide plans were estimated at 0.9% (SE=0.2) in year 1, and 2.2% (SE=0.5) in year 2, and suicide attempts were estimated at 0.2% (SE=0.1) in both year 1 and 2. Aggregated one-year incidence proportions for any form of first-onset STB (i.e., at least suicidal ideation) were 4.8% (SE=0.7) in year 1, and 6.4% (SE=0.9) in year 2. Due to the very low incidence of first-onset suicide attempts, the following analyses focus on the onset of suicidal ideation and plans.
Bivariate models for first-onset STB during college
Socio-demographic variables found to predict first-onset STB in college were non-heterosexual orientation, low parental educational level, and difficult parental financial situation (see Table 1). Effect sizes from the included risk factor domains (see Tables 2–4) varied considerably whether viewed from individual-level (ORs 1.9–17.6) or population-level perspective (PARPs 3–34%). When considering both individual- and population-level effects, the three most important risk factors (i.e. those with an OR>5 and PARP>15%) were: physical abuse prior to the age of 17, dating violence prior to the age of 17, and 12-month betrayal by someone other than one’s partner. Non-suicidal self-injury also was an important predictor of first-onset ideation, but only on the individual level (i.e., not on the population level because of low prevalence). In contrast, parental psychopathology, emotional abuse prior to the age of 17, internalizing and externalizing disorders, episodes of (hypo)mania, and recent ongoing arguments with friends or family were important predictors on the population level only (i.e., due to the combination of high prevalence and weakly elevated individual-level associations).
Table 1.
Sociodemographic variables as bivariate predictors for first-onset STB.
| Prevalencea | Suicidal ideationb | Suicide planb | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n(w) | %(w) | (SE) | OR | 95% CI | PARP(%) | OR | 95% CI | PARP(%) | |
| Socio-demographics | |||||||||
| Being male | 927 | 45.4 | 0.8 | 1.37 | (0.77–2.44) | 12.6 | 1.71 | (0.91–3.23) | 21.8 |
| Age > 18 years | 572 | 28.0 | 0.7 | 1.48 | (0.88–2.49) | 10.1 | 1.66 | (0.88–3.12) | 13.6 |
| Non-Belgian nationality | 165 | 8.1 | 0.5 | 1.49 | (0.53–4.21) | 3.6 | 2.02 | (0.72–5.61) | 6.8 |
| Parents’ financial situation difficult | 327 | 16.0 | 0.7 | 2.55 | (1.36–4.77) | 17.5 | 2.43 | (1.15–5.11) | 17.2 |
| Parental educationc | |||||||||
| - both parents high | 1178 | 57.7 | 0.9 | (ref) | – | – | (ref) | – | – |
| - only one parent high | 493 | 24.2 | 0.8 | 1.38 | (0.72–2.66) | −0.5 | 1.51 | (0.70–3.25) | 0.5 |
| - none of parents high | 371 | 18.2 | 0.8 | 2.98 | (1.57–5.67) | 20.3 | 3.29 | (1.44–7.50) | 22.7 |
| Non-intact familial compositiond | 421 | 20.6 | 0.7 | 1.47 | (0.81–2.64) | 8.0 | 1.49 | (0.71–3.10) | 8.7 |
| Non-heterosexual orientation | 82 | 4.0 | 0.4 | 2.71 | (0.91–8.08) | 5.8 | 3.92 | (1.32–11.62) | 9.3 |
| College-related socio-demographics | |||||||||
| University Group membership | |||||||||
| - Human Sciences | 838 | 41.0 | 0.8 | (ref) | – | – | (ref) | – | – |
| - Science & Technology | 668 | 32.7 | 0.7 | 1.15 | (0.66–2.01) | 4.7 | 0.98 | (0.50–1.94) | 1.8 |
| - Biomedical Sciences | 536 | 26.2 | 0.7 | 0.97 | (0.49–1.94) | −2.0 | 0.82 | (0.36–1.83) | −4.4 |
| Non-GSE pre-educational level | 150 | 7.4 | 0.5 | 1.06 | (0.28–4.05) | 1.0 | 0.82 | (0.01–62.53) | 1.5 |
| Living with parents | 540 | 26.4 | 1.1 | 1.17 | (0.64–2.13) | 4.3 | 0.97 | (0.44–2.18) | 0.1 |
prevalence estimate of risk factor among those that never experienced any STB at baseline (n = 2,042).
STB outcomes are mutually exclusive.
high degree of parental education defined as holding a college bachelor degree or more.
non-intact familial composition defined as parents being divorced or separated.
Note: significant odds ratios/PARPs are shown in bold (α = 0.05); OR = Odds ratio; PARP = population attributable risk proportion; GSE = general secondary education
Table 2.
Parental psychopathology, and childhood-adolescent traumatic experiences as bivariate predictors for first-onset STB.
| Prevalencea | Suicidal ideationb | Suicide planb | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n(w) | %(w) | (SE) | OR | 95% CI | PARP(%) | OR | 95% CI | PARP(%) | |
| Parental psychopathology | 553 | 27.1 | 0.8 | 1.91 | (1.11–3.28) | 18.1 | 2.40 | (1.25–4.62) | 25.8 |
| Traumatic experiences (< age 17) | |||||||||
| physical abuse | 78 | 3.8 | 0.4 | 4.23 | (1.51–11.86) | 8.7 | 7.19 | (2.58–20.08) | 15.2 |
| emotional abuse | 262 | 12.9 | 0.6 | 2.34 | (1.25–4.36) | 13.2 | 2.57 | (1.21–5.46) | 15.7 |
| sexual abuse | 11 | 0.5 | 0.1 | / | / | / | / | / | / |
| neglect | 101 | 5.0 | 0.4 | 2.79 | (1.17–6.62) | 7.1 | 2.93 | (0.96–8.92) | 8.2 |
| bully victimization | 609 | 29.8 | 0.9 | 1.38 | (0.80–2.38) | 9.5 | 1.71 | (0.98–2.99) | 16.7 |
| dating violence | 88 | 4.3 | 0.4 | 12.25 | (5.00–29.98) | 21.8 | 17.58 | (6.55–47.18) | 30.2 |
| Any traumatic experience | 1070 | 52.4 | 0.9 | 2.50 | (1.41–4.45) | 41.1 | 3.98 | (1.64–9.65) | 57.7 |
| Number of traumatic experiences | |||||||||
| 0 | 972 | 47.6 | 0.9 | (ref) | – | – | (ref) | – | – |
| 1 | 656 | 32.1 | 0.9 | 1.63 | (0.88–3.05) | −2.9 | 2.15 | (0.85–5.48) | −6.0 |
| 2 | 278 | 13.6 | 0.6 | 3.30 | (1.66–6.57) | 12.2 | 5.74 | (2.20–14.98) | 18.2 |
| 3+ | 136 | 6.7 | 0.5 | 5.72 | (2.39–13.70) | 12.7 | 10.58 | (3.43–32.61) | 18.4 |
| χ2 (p-value)c | 13.8 (<0.01) | 18.1 (<0.01) | |||||||
prevalence estimate of risk factor among those that never experienced any STB at baseline (n = 2,042).
STB outcomes are mutually exclusive.
Cochran-Armitage trend test.
Note: significant ORs/PARPs are shown in bold (α = 0.05); OR = odds ratio; PARP = population attributable risk proportion; / = could not be estimated
Table 4.
Past year stressful experiences as bivariate predictors for first-onset STB.
| Prevalencea | Suicidal ideationb | Suicide planb | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n(w) | %(w) | (SE) | OR | 95% CI | PARP(%) | OR | 95% CI | PARP(%) | |
| 12-month stressful experiences | |||||||||
| life-threatening illness or injury of a friend or family member | 399 | 19.5 | 0.8 | 1.02 | (0.50–2.06) | 0.8 | 1.02 | (0.45–2.32) | 1.0 |
| death of a friend or family member | 376 | 18.4 | 0.8 | 0.90 | (0.43–1.89) | −1.2 | 0.87 | (0.34–2.24) | −1.4 |
| break-up with a romantic partner | 372 | 18.2 | 0.9 | 1.71 | (0.88–3.34) | 10.8 | 1.83 | (0.86–3.91) | 12.6 |
| romantic partner cheated | 99 | 4.8 | 0.5 | 3.39 | (1.17–9.81) | 9.0 | 3.97 | (1.05–15.03) | 11.7 |
| serious betrayal someone else than partner | 232 | 11.4 | 0.7 | 5.13 | (2.35–11.22) | 27.1 | 6.57 | (2.65–16.29) | 34.3 |
| serious ongoing arguments or break-up with friend or family member | 234 | 11.4 | 0.7 | 2.75 | (1.35–5.62) | 14.9 | 3.48 | (1.66–7.33) | 20.2 |
| life-threatening accident | 19 | 1.0 | 0.2 | / | / | / | / | / | / |
| seriously physically assaulted | 39 | 1.9 | 0.3 | 2.91 | (0.70–12.04) | 3.3 | 3.67 | (0.86–15.63) | 4.6 |
| sexually assaulted or raped | 5 | 0.2 | 0.1 | / | / | / | / | / | / |
| trouble with the police | 38 | 1.9 | 0.3 | / | / | / | / | / | / |
| time in jail | 0 | 0.1 | 0.1 | / | / | / | / | / | / |
| other serious legal problem | 9 | 0.4 | 0.2 | / | / | / | / | / | / |
| Any stressful event | 956 | 46.8 | 1.0 | 1.75 | (0.97–3.18) | 24.1 | 2.16 | (1.04–4.52) | 33.2 |
| Number of stressful experiences | |||||||||
| 0 | 1087 | 53.2 | 1.0 | (ref) | – | – | (ref) | – | – |
| 1 | 555 | 27.2 | 0.9 | 1.30 | (0.70–2.39) | −1.1 | 1.54 | (0.72–3.31) | 0.6 |
| 2 | 271 | 13.2 | 0.7 | 1.73 | (0.79–3.80) | 4.3 | 2.30 | (0.90–5.90) | 7.5 |
| 3+ | 130 | 6.4 | 0.5 | 3.96 | (1.57–9.98) | 10.9 | 4.61 | (1.42–14.98) | 12.1 |
| χ2 (p-value)c | 5.1 (0.02) | 5.1 (0.02) | |||||||
prevalence estimate of risk factor among those that never experienced any STB at baseline (n = 2,042).
STB outcomes are mutually exclusive.
Cochran-Armitage trend test.
Note: significant ORs/PARPs are shown in bold (α = 0.05); OR = odds ratio; PARP = population attributable risk proportion; / = could not be estimated
Overall, large proportions of first-onset STB were associated with any trauma prior to the age of 17 (PARPs=41.1–57.7%; see Table 2) or being at risk for any 12-month mental disorder (PARPs=42.4–51.5%; see Table 3). We also consistently found a dose-response relationship between the number of risk factors within each domain and first-onset STB. Here too, risk was important on both the individual- and population-level, with ORs in the range 3.96–10.58 and PARPs in the range 10.9–18.4% for those with three or more risk factors (in each domain).
Table 3.
Risk for 12-month mental disorders as bivariate predictors for first-onset STB.
| Prevalencea | Suicidal ideationb | Suicide planb | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n(w) | %(w) | (SE) | OR | 95% CI | PARP(%) | OR | 95% CI | PARP(%) | |
| Risk for 12-month mental disorders | |||||||||
| risk for internalizing disorder | 397 | 19.5 | 0.8 | 2.72 | (1.54–4.80) | 23.1 | 3.11 | (1.58–6.16) | 27.6 |
| risk for externalizing disorder | 377 | 18.5 | 0.8 | 2.43 | (1.30–4.56) | 18.5 | 3.17 | (1.51–6.67) | 26.0 |
| risk for substance use | 105 | 5.2 | 0.4 | 2.48 | (0.65–9.51) | 6.8 | 2.39 | (0.06–96.89) | 8.9 |
| risk for crime/violence disorder | 4 | 0.2 | 0.1 | / | / | / | / | / | / |
| IED item positive | 94 | 4.6 | 0.5 | 2.52 | (0.87–7.31) | 6.1 | 3.05 | (0.84–11.11) | 8.5 |
| (hypo)mania item positive | 124 | 6.1 | 0.5 | 3.63 | (1.54–8.56) | 11.6 | 4.63 | (1.61–13.36) | 16.0 |
| any eating disorder item positive | 122 | 6.0 | 0.5 | 1.40 | (0.44–4.44) | 2.7 | 1.74 | (0.52–5.86) | 4.7 |
| any psychotic item positive | 35 | 1.7 | 0.3 | 2.43 | (0.02–272.97) | 3.6 | 4.60 | (0.76–27.87) | 5.5 |
| non-suicidal self-injury | 20 | 1.0 | 0.2 | 5.22 | (1.07–25.41) | 3.4 | 1.72 | (0.00–3602.26) | 3.5 |
| Any positive screen | 793 | 38.8 | 1.0 | 3.17 | (1.83–5.50) | 42.4 | 4.09 | (1.99–8.41) | 51.5 |
| Number of positive screens | |||||||||
| 0 | 1249 | 61.2 | 1.0 | (ref) | – | – | (ref) | – | – |
| 1 | 494 | 24.2 | 0.8 | 2.30 | (1.32–4.00) | 8.6 | 2.60 | (1.22–5.54) | 7.1 |
| 2 | 185 | 9.1 | 0.5 | 3.72 | (1.68–8.26) | 9.8 | 5.45 | (2.25–13.22) | 14.2 |
| 3+ | 114 | 5.6 | 0.5 | 6.59 | (2.71–16.00) | 12.2 | 9.14 | (3.06–27.30) | 15.7 |
| χ2 (p-value)c | 14.0 (<0.01) | 13.5 (<0.01) | |||||||
prevalence estimate of risk factor among those that never experienced any STB at baseline (n = 2,042).
STB outcomes are mutually exclusive.
Cochran-Armitage trend test.
Note: significant ORs/PARPs are shown in bold (α = 0.05); OR = odds ratio; PARP = population attributable risk proportion; / = could not be estimated
Multivariate model for first-onset STB during college
We then constructed a multivariate prediction model for first-onset STB based on the longitudinal data. The total effect size (Nagelkerke pseudo-R2) of the included risk factors was .30 for suicidal ideation, and .40 for suicide plan. AUC-values were .84 for suicidal ideation and .91 for suicide plan (see Figure 1). Importantly, 50.7% (SE=6.9) of all first-onset suicidal ideation cases occurred among respondents in the highest decile of predicted risk; for suicide plan this was 65.7% (SE=8.8; see Figure 2). After adjusting for socio-demographic and all other risk factors, the strongest predictors were (data reported as odds ratio [95% CI], and PARP) dating violence before the age of 17 (12.59 [3.21–49.43], 18.7% for suicidal ideation; 23.90 [4.19–136.21], 26.1% for suicide plans), and 12-month serious betrayal (3.71 [1.21–11.43], 19.4% for suicidal ideation; 4.71 [1.12–19.79], 24.1% for suicide plans). A full overview of all multivariate estimates is presented in the supplementary materials.
Figure 1.
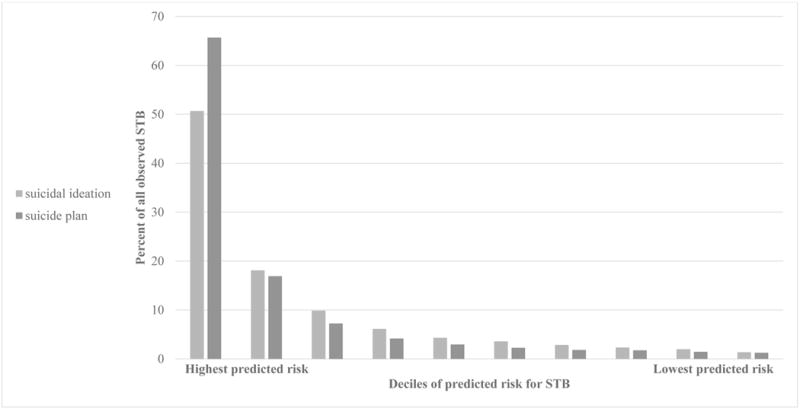
Concentration of risk for first-onset STB based on all risk factors under study.
Figure 2.
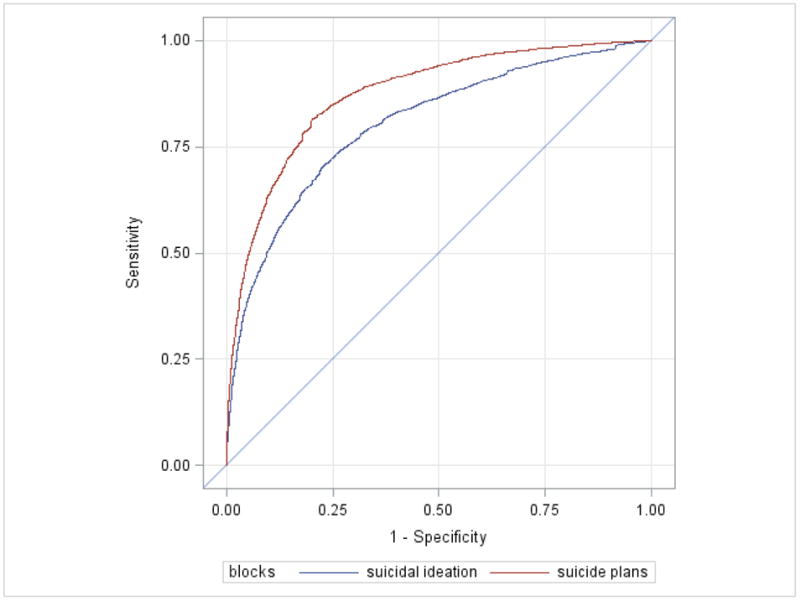
Receiver Operating Characteristic (ROC) curves for predicted probability of first-onset STB based on all risk factors under study.
DISCUSSION
Main findings
This prospective study investigated the first onset of STB in a large representative sample of college students. One-year incidence estimates for first-onset STB were 3.7–3.9% for suicidal ideation, 0.9–2.2% for suicidal plans, and 0.2% for suicide attempts. Approximately 51–66% of students with STB onset during early college were among the 10% of students with highest predicted risk based on our model. Of all risk factors under study, dating violence prior to the age of 17 and 12-month betrayal experiences were most strongly associated with the first-onset of STB.
Limitations
Several limitations of this study deserve attention. First, RR of 66.5% (baseline), and 53.6% (follow-up) are moderate. However, when we correct the RR for non-participation due to college dropout, RRs increased to 76.7% (baseline data) and 70.2% (follow-up data). These RRs are substantially higher than the mean RR in cross-sectional web-based surveys (i.e. around 40%; Cook et al., 2000) or RRs in recent large-scale college student surveys (39–44%; Eisenberg et al., 2013; Paul et al., 2015). We also systematically used state-of-the-art missing data handling techniques to increase the representativeness of our findings. Second, we identified baseline risk for mental disorders by using self-report measures applying a categorical cut-off scoring system. For college students, it is unknown to what extent this effectively corresponds to mental disorders diagnosed by face-to-face clinical interviews. We addressed this limitation by using well-validated measures used in large surveys of the general population. Third, we were not able to calculate risk estimates for suicide attempts due to the very low prevalence of this outcome. This may reflect a genuinely low rate of suicide attempts during college (in line with Wilcox et al., 2010) and points to the need for larger sample sizes to study this particular outcome. Fourth, data for this study were collected in one Belgian university with predominantly Dutch-speaking students in their early college years. It is therefore unknown to what extent these findings generalize to college students from other universities in other countries or cultures, or to the first-onset of STB later in college. Finally, as this is the first study that used a prospective design to test a wide range of risk factors for first-onset STB, our approach should be considered explorative (i.e., hypothesis-generating), rather than conclusive (i.e., hypothesis-testing). Further study may therefore focus on statistical interactions between different risk factors, including protective factors, and may use validation samples to further test the accuracy of our multivariate predictive model.
Significance of our findings
To the best of our knowledge, this is the first study that estimated one-year incidence proportions for separate STB outcomes during college. In general, the proportion of first-onset STB appears to be higher than previously reported data from the general population (Gunnell et al., 2004; Hintikka et al., 2001; Zhang et al., 2015) but comparable with estimates from young adults samples aged 16–24 years (Gunnell et al., 2004; ten Have et al., 2009). One previous study among general university students (Whitlock et al., 2013) reported incidence proportions for any STB of 1–2% annually, which is lower than our estimates. Possible explanations include methodological differences (e.g., higher level of representativeness in our study) or sociodemographic differences (e.g., younger age in our sample). Taken together, findings suggest that the college years are an important risk period for the first onset of STB, and may constitute an important window of opportunity to detect young people at risk for suicide.
Our study provides substantial evidence for a baseline screening instrument to accurately (AUC≥.84) predict the subsequent onset of STB during college. For comparison, Borges et al. (2010) found AUC values of .74–.80 when identifying 12-month suicide attempt cases in cross-sectional general population data. Among college students, suicide screening projects have been limited to referral for treatment of highly symptomatic individuals, depending to a considerable extent on the presence of already ongoing suicidality (King et al., 2015; Moutier et al., 2012). Using a prospective design among non-suicidal students at baseline, we estimate that approximately 51–66% of first-onset STB cases could be reached by interventions targeting the 10% of students at highest predicted risk. This is a promising result given that the proportion of students with severe psychopathology is possibly increasing (Hunt and Eisenberg, 2010), and colleges are in urgent need of powerful tools to support clinical decision-making and resource allocation. To that extent, it also is interesting that we found the predictive accuracy to be higher for suicide plans than for ideation. Help-seeking behaviour decreases with more severe suicidality (Hom et al., 2015), suggesting that risk screening at college entrance is a powerful and timely strategy to address an unmet need for help. Future research should incorporate additional variables (e.g., short-term risk factors, protective factors, biological measures, etc.), test for significant interaction of effects, and/or apply machine learning techniques (Nock, 2016) to develop more accurate baseline screening algorithms.
Our findings contribute substantially to the existing literature on the relationship between trauma, interpersonal stress, and STB (Buitron et al., 2016; King and Merchant, 2008; Pettit et al., 2011; Whitlock et al., 2014), as we found that 19–26% of STB onset cases were independently associated with a history of prior dating violence or recent experiences of serious betrayal. Earlier evidence suggests that both of these factors may function as proximal markers for a more broad history of trauma: early traumatic experiences were found to predict dating violence in adolescence (Chiodo et al., 2012; Crawford and Wright, 2007; Kaukinen, 2014; Widom et al., 2014), and exposure to high-betrayal trauma in early life (e.g., traumatization by an important caregiver) is related to experiences of serious betrayal in adolescence or adulthood (Freyd, 1996; Hocking et al., 2016). The importance of broad trauma in early life is also supported by our findings for abuse and neglect, and by the very strong population-effect of traumatic experiences in general. How childhood-adolescent traumatic experiences, including dating violence, eventually lead to the onset of STB during college can be considered in light of current theories of suicidal behaviour. For example, poor relationship quality characterized by interpersonal violence or experiences of betrayal may lead to feelings of thwarted belongingness and/or an increase in perceived burdensomeness. According to the Interpersonal Theory of Suicide (Joiner TE, 2005; Van Orden et al., 2010) these factors are key in the onset of suicidal ideation. Alternatively, Stress-Diathesis Models of Suicidal Behaviour (Kazan et al., 2016; Mann et al., 1999; van Heeringen, 2012) posit that recent interpersonal stress leads to STB in the presence of a history of early-life adversity, which, in turn, has resulted in biologically or environmentally determined personality traits such as impulsive aggression or disturbed attachment patterns, both known risk factors for STB (Lopez-Castroman et al., 2014; Sheftall et al., 2014). This underscores the importance of providing a careful trauma assessment when screening incoming freshmen, a strategy lacking in currently implemented suicide screening projects (King et al., 2015; Moutier et al., 2012).
Our population-level estimates also offer some unique insights into the potential effectiveness of future interventions. For example, targeting dating violence could have a beneficiary effect for a maximum of about one third (29%) of subsequent STB onset. In contrast, targeting the wider range of traumatic experiences could reach twice the amount of cases (59%), pointing to the potential of a population-based approach when designing interventions (Brownson et al., 2016). As trauma is so closely related to suicidal behaviour, particularly in younger people, providing more attention to the prevention of these adversities may have key positive downstream effects. Public health strategies for childhood maltreatment prevention, such as increasing parenting support (Prinz, 2016; Sanders et al., 2014), or school-based interventions (Stanley et al., 2015) are promising, and may be combined with campus-specific interventions targeting dating violence such as bystander programs (Peterson et al., 2016; Storer et al., 2016) or the use of safety apps (Glass et al., 2015). Ultimately, this may lead to a more developmental approach to prevent STB during adolescence and college (Wyman, 2014). Nevertheless, universal or selective prevention of trauma is rather difficult because this requires changes at the family and household level. However, identifying those families – or students – at risk may be more practical and ultimately, may decrease the onset of STB in college. Evidently, as our study is among the first ones that address the potential reduction of onset of STB during college when targeting specific risk factors, further research is needed to determine causality (Kraemer et al., 1997), for instance in terms of intervention trials, that could guide us towards more targeted treatments in college. Additional research also is needed to focus on those students with pre-existing STB at college entrance, as risk factors for the continuation for STB in this group may be different from those predicting a first onset of STB; thus, warranting a different, yet more fine-grained approach with regard to campus suicide prevention interventions.
Supplementary Material
Glossary
- PARP
population attributable risk proportion
- STB
suicidal thoughts and behaviours
Contributor Information
Philippe Mortier, Research Group Psychiatry, Department of Neurosciences, KU Leuven University, Leuven, Belgium.
Koen Demyttenaere, Research Group Psychiatry, Department of Neurosciences, KU Leuven University, Leuven, Belgium.
Randy P. Auerbach, Department of Psychiatry, Harvard Medical School, Boston MA, USA; Center for Depression, Anxiety and Stress Research, McLean Hospital, Belmont, MA, USA.
Pim Cuijpers, Department of Clinical, Neuro and Developmental Psychology, Vrije Universiteit Amsterdam, the Netherlands.
Jennifer G. Green, School of Education, Boston University, Boston, MA, USA.
Glenn Kiekens, Research Group Psychiatry, Department of Neurosciences, KU Leuven University, Leuven, Belgium.
Ronald C. Kessler, Harvard Medical School, Department of Health Care Policy, Harvard University, Boston, MA, USA.
Matthew K. Nock, Department of Psychology, Harvard University, Boston, MA, USA.
Alan M. Zaslavsky, Harvard Medical School, Department of Health Care Policy, Harvard University, Boston, MA, USA.
Ronny Bruffaerts, Research Group Psychiatry, Department of Neurosciences, KU Leuven University, Leuven, Belgium.
References
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Cornette M, Akhavan S, Chiara A. Suicidality and cognitive vulnerability to depression among college students: a prospective study. J Adolesc. 1998;21:473–487. doi: 10.1006/jado.1998.0167. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging Adulthood The winding road from the late teens through the twenties. Second. Oxford University Press; New York: 2015. [Google Scholar]
- Boeninger DK, Masyn KE, Feldman BJ, Conger RD. Sex differences in developmental trends of suicide ideation, plans, and attempts among European American adolescents. Suicide Life Threat Behav. 2010;40:451–464. doi: 10.1521/suli.2010.40.5.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Nock MK, Haro Abad JM, Hwang I, Sampson NA, Alonso J, Andrade LH, Angermeyer MC, Beautrais A, Bromet E, Bruffaerts R, de Girolamo G, Florescu S, Gureje O, Hu C, Karam EG, Kovess-Masfety V, Lee S, Levinson D, Medina-Mora ME, Ormel J, Posada-Villa J, Sagar R, Tomov T, Uda H, Williams DR, Kessler RC. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry. 2010;71:1617–1628. doi: 10.4088/JCP.08m04967blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray RM, Hourani LL. Substance use trends among active duty military personnel: findings from the United States Department of Defense Health Related Behavior Surveys, 1980–2005. Addiction. 2007;102:1092–1101. doi: 10.1111/j.1360-0443.2007.01841.x. [DOI] [PubMed] [Google Scholar]
- Brownson C, Drum D, Becker MS, Saathoff AK, Hentschel E. Distress and suicidality in higher education: implications for population-oriented prevention paradigms. J College Stud Psychother. 2016;30:98–113. [Google Scholar]
- Bruffaerts R, Kessler RC, Demyttenaere K, Bonnewyn A, Nock MK. Examination of the population attributable risk of different risk factor domains for suicidal thoughts and behaviors. J Affect Disord. 2015;187:66–72. doi: 10.1016/j.jad.2015.07.042. [DOI] [PubMed] [Google Scholar]
- Brugha TS, Cragg D. The List of Threatening Experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand. 1990;82:77–81. doi: 10.1111/j.1600-0447.1990.tb01360.x. [DOI] [PubMed] [Google Scholar]
- Buitron V, Hill RM, Pettit JW, Green KL, Hatkevich C, Sharp C. Interpersonal stress and suicidal ideation in adolescence: An indirect association through perceived burdensomeness toward others. J Affect Disord. 2016;190:143–149. doi: 10.1016/j.jad.2015.09.077. [DOI] [PubMed] [Google Scholar]
- Chiodo D, Crooks CV, Wolfe DA, McIsaac C, Hughes R, Jaffe PG. Longitudinal prediction and concurrent functioning of adolescent girls demonstrating various profiles of dating violence and victimization. Prev Sci. 2012;13:350–359. doi: 10.1007/s11121-011-0236-3. [DOI] [PubMed] [Google Scholar]
- Chou CH, Ko HC, Wu JY, Cheng CP. The prevalence of and psychosocial risks for suicide attempts in male and female college students in Taiwan. Suicide Life Threat Behav. 2013;43:185–197. doi: 10.1111/sltb.12007. [DOI] [PubMed] [Google Scholar]
- Christensen H, Cuijpers P, Reynolds CF., 3rd Changing the Direction of Suicide Prevention Research: A Necessity for True Population Impact. JAMA Psychiatry. 2016;73:435–436. doi: 10.1001/jamapsychiatry.2016.0001. [DOI] [PubMed] [Google Scholar]
- Cleary M, Walter G, Jackson D. “Not always smooth sailing”: mental health issues associated with the transition from high school to college. Issues Ment Health Nurs. 2011;32:250–254. doi: 10.3109/01612840.2010.548906. [DOI] [PubMed] [Google Scholar]
- Cook C, Heath F, Thompson RL. A meta-analysis of response rates in Web- or internet-based surveys. Educ Psychol Meas. 2000;60:821–836. [Google Scholar]
- Crawford E, Wright MO. The impact of childhood psychological maltreatment on interpersonal schemas and subsequent experiences of relationship aggression. Journal of Emotional Abuse. 2007;7:93–116. [Google Scholar]
- Dennis ML, Chan YF, Funk RR. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. Am J Addict. 2006;15(Suppl 1):80–91. doi: 10.1080/10550490601006055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drum DJ, Denmark AB. Campus suicide prevention: bridging paradigms and forging partnerships. Harv Rev Psychiatry. 2012;20:209–221. doi: 10.3109/10673229.2012.712841. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Hunt J, Speer N. Mental health in American colleges and universities: variation across student subgroups and across campuses. J Nerv Ment Dis. 2013;201:60–67. doi: 10.1097/NMD.0b013e31827ab077. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Freyd JJ. Betrayal Trauma: The logic of forgetting childhood abuse. Harvard University Press; Cambridge, MA: 1996. [Google Scholar]
- Gibb BE, Alloy LB, Abramson LY, Rose DT, Whitehouse WG, Hogan ME. Childhood maltreatment and college students’ current suicidal ideation: a test of the hopelessness theory. Suicide Life Threat Behav. 2001;31:405–415. doi: 10.1521/suli.31.4.405.22042. [DOI] [PubMed] [Google Scholar]
- Glass N, Clough A, Case J, Hanson G, Barnes-Hoyt J, Waterbury A, Alhusen J, Ehrensaft M, Grace KT, Perrin N. A safety app to respond to dating violence for college women and their friends: the MyPlan study randomized controlled trial protocol. BMC Public Health. 2015;15:871. doi: 10.1186/s12889-015-2191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D, Harbord R, Singleton N, Jenkins R, Lewis G. Factors influencing the development and amelioration of suicidal thoughts in the general population. Cohort study. Br J Psychiatry. 2004;185:385–393. doi: 10.1192/bjp.185.5.385. [DOI] [PubMed] [Google Scholar]
- Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, Sampson NA, Kessler RC. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15:167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrod CS, Goss CW, Stallones L, DiGuiseppi C. Interventions for primary prevention of suicide in university and other post-secondary educational settings. Cochrane Database Syst Rev. 2014;10:Cd009439. doi: 10.1002/14651858.CD009439.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hintikka J, Pesonen T, Saarinen P, Tanskanen A, Lehtonen J, Viinamaki H. Suicidal ideation in the Finnish general population. A 12-month follow-up study. Soc Psychiatry Psychiatr Epidemiol. 2001;36:590–594. doi: 10.1007/s127-001-8198-x. [DOI] [PubMed] [Google Scholar]
- Hocking EC, Simons RM, Surette RJ. Attachment style as a mediator between childhood maltreatment and the experience of betrayal trauma as an adult. Child Abuse Negl. 2016;52:94–101. doi: 10.1016/j.chiabu.2016.01.001. [DOI] [PubMed] [Google Scholar]
- Hom MA, Stanley IH, Joiner TE., Jr Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: A review of the literature. Clin Psychol Rev. 2015;40:28–39. doi: 10.1016/j.cpr.2015.05.006. [DOI] [PubMed] [Google Scholar]
- Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2010;46:3–10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Kaukinen C. Dating violence among college students: the risk and protective factors. Trauma Violence Abuse. 2014;15:283–296. doi: 10.1177/1524838014521321. [DOI] [PubMed] [Google Scholar]
- Kazan D, Calear AL, Batterham PJ. The impact of intimate partner relationships on suicidal thoughts and behaviours: A systematic review. J Affect Disord. 2016;190:585–598. doi: 10.1016/j.jad.2015.11.003. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Rose S, Koenen KC, Karam EG, Stang PE, Stein DJ, Heeringa SG, Hill ED, Liberzon I, McLaughlin KA, McLean SA, Pennell BE, Petukhova M, Rosellini AJ, Ruscio AM, Shahly V, Shalev AY, Silove D, Zaslavsky AM, Angermeyer MC, Bromet EJ, de Almeida JM, de Girolamo G, de Jonge P, Demyttenaere K, Florescu SE, Gureje O, Haro JM, Hinkov H, Kawakami N, Kovess-Masfety V, Lee S, Medina-Mora ME, Murphy SD, Navarro-Mateu F, Piazza M, Posada-Villa J, Scott K, Torres Y, Carmen Viana M. How well can post-traumatic stress disorder be predicted from pre-trauma risk factors? An exploratory study in the WHO World Mental Health Surveys. World Psychiatry. 2014;13:265–274. doi: 10.1002/wps.20150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Stein MB, Petukhova MV, Bliese P, Bossarte RM, Bromet EJ, Fullerton CS, Gilman SE, Ivany C, Lewandowski-Romps L, Millikan Bell A, Naifeh JA, Nock MK, Reis BY, Rosellini AJ, Sampson NA, Zaslavsky AM, Ursano RJ. Predicting suicides after outpatient mental health visits in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Mol Psychiatry. 2016 doi: 10.1038/mp.2016.110. (published online July 19, 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiekens G, Claes L, Demyttenaere K, Auerbach RP, Green JG, Kessler RC, Mortier P, Nock MK, Bruffaerts R. Lifetime and 12-Month Nonsuicidal Self-Injury and Academic Performance in College Freshmen. Suicide Life Threat Behav. 2016 doi: 10.1111/sltb.12237. (published online March 8, 2016) [DOI] [PubMed] [Google Scholar]
- King CA, Eisenberg D, Zheng K, Czyz E, Kramer A, Horwitz A, Chermack S. Online suicide risk screening and intervention with college students: a pilot randomized controlled trial. J Consult Clin Psychol. 2015;83:630–636. doi: 10.1037/a0038805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Merchant CR. Social and interpersonal factors relating to adolescent suicidality: a review of the literature. Arch Suicide Res. 2008;12:181–196. doi: 10.1080/13811110802101203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox K. Approaching suicide as a public health issue. Ann Intern Med. 2014;161:151–152. doi: 10.7326/M14-0914. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Arch Gen Psychiatry. 1997;54:337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- Krysinska K, Martin G. The struggle to prevent and evaluate: application of population attributable risk and preventive fraction to suicide prevention research. Suicide Life Threat Behav. 2009;39:548–557. doi: 10.1521/suli.2009.39.5.548. [DOI] [PubMed] [Google Scholar]
- Lopez-Castroman J, Jaussent I, Beziat S, Guillaume S, Baca-Garcia E, Genty C, Olie E, Courtet P. Increased severity of suicidal behavior in impulsive aggressive patients exposed to familial adversities. Psychol Med. 2014;44:3059–3068. doi: 10.1017/S0033291714000646. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- Mortier P, Demyttenaere K, Auerbach RP, Green JG, Kessler RC, Kiekens G, Nock MK, Bruffaerts R. The impact of lifetime suicidality on academic performance in college freshmen. J Affect Disord. 2015;186:254–260. doi: 10.1016/j.jad.2015.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moutier C, Norcross W, Jong P, Norman M, Kirby B, McGuire T, Zisook S. The suicide prevention and depression awareness program at the University of California, San Diego School of Medicine. Acad Med. 2012;87:320–326. doi: 10.1097/ACM.0b013e31824451ad. [DOI] [PubMed] [Google Scholar]
- Musci RJ, Hart SR, Ballard ED, Newcomer A, Van Eck K, Ialongo N, Wilcox H. Trajectories of Suicidal Ideation from Sixth through Tenth Grades in Predicting Suicide Attempts in Young Adulthood in an Urban African American Cohort. Suicide Life Threat Behav. 2015;46:255–265. doi: 10.1111/sltb.12191. [DOI] [PubMed] [Google Scholar]
- Nansel TR, Overpeck M, Pilla RS, Ruan WJ, Simons-Morton B, Scheidt P. Bullying behaviors among US youth: prevalence and association with psychosocial adjustment. JAMA. 2001;285:2094–2100. doi: 10.1001/jama.285.16.2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkansah-Amankra S. Adolescent suicidal trajectories through young adulthood: prospective assessment of religiosity and psychosocial factors among a population-based sample in the United States. Suicide Life Threat Behav. 2013;43:439–459. doi: 10.1111/sltb.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M, Borges G, Ono Y. Suicide : global perspectives from the WHO World Mental Health Surveys. Cambridge University Press; Cambridge: 2012. [Google Scholar]
- Nock MK. Recent and needed advances in the understanding, prediction, and prevention of suicidal behavior. Depress Anxiety. 2016;33:460–463. doi: 10.1002/da.22528. [DOI] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, Michel BD. Self-Injurious Thoughts and Behaviors Interview: development, reliability, and validity in an adolescent sample. Psychol Assess. 2007;19:309–317. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development (OECD) Education at a Glance 2012: OECD Indicators. OECD; 2012. http://www.oecd.org/edu/EAG%202012_ebook_EN_200912.pdf (accessed 08.06.16) [Google Scholar]
- Paul E, Tsypes A, Eidlitz L, Ernhout C, Whitlock J. Frequency and functions of non-suicidal self-injury: associations with suicidal thoughts and behaviors. Psychiatry Res. 2015;225:276–282. doi: 10.1016/j.psychres.2014.12.026. [DOI] [PubMed] [Google Scholar]
- Peterson K, Sharps P, Banyard V, Powers RA, Kaukinen C, Gross D, Decker MR, Baatz C, Campbell J. An Evaluation of Two Dating Violence Prevention Programs on a College Campus. J Interpers Violence. 2016 doi: 10.1177/0886260516636069. (published online March 13, 2016) [DOI] [PubMed] [Google Scholar]
- Pettit JW, Green KL, Grover KE, Schatte DJ, Morgan ST. Domains of chronic stress and suicidal behaviors among inpatient adolescents. J Clin Child Adolesc Psychol. 2011;40:494–499. doi: 10.1080/15374416.2011.563466. [DOI] [PubMed] [Google Scholar]
- Prinz RJ. Parenting and family support within a broad child abuse prevention strategy: Child maltreatment prevention can benefit from public health strategies. Child Abuse Negl. 2016;51:400–406. doi: 10.1016/j.chiabu.2015.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins A, Fiske A. Explaining the Relation between Religiousness and Reduced Suicidal Behavior: Social Support Rather Than Specific Beliefs. Suicide Life Threat Behav. 2009;39:386–395. doi: 10.1521/suli.2009.39.4.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose G. Rose’s strategy of preventive medicine. University Press; Oxford: 2008. [Google Scholar]
- Rosenbaum PR, Rubin DB. The Central Role of the Propensity Score in Observational Studies of Causal Effects. Biometrica. 1983;70:41–55. [Google Scholar]
- Rostila M, Berg L, Arat A, Vinnerljung B, Hjern A. Parental death in childhood and self-inflicted injuries in young adults-a national cohort study from Sweden. Eur Child Adolesc Psychiatry. 2016 doi: 10.1007/s00787-016-0833-6. (published online March 1, 2016) [DOI] [PubMed] [Google Scholar]
- Rueter MA, Holm KE, McGeorge CR, Conger RD. Adolescent suicidal ideation subgroups and their association with suicidal plans and attempts in young adulthood. Suicide Life Threat Behav. 2008;38:564–575. doi: 10.1521/suli.2008.38.5.564. [DOI] [PubMed] [Google Scholar]
- Salekin RT. Psychopathy and recidivism from mid-adolescence to young adulthood: cumulating legal problems and limiting life opportunities. J Abnorm Psychol. 2008;117:386–395. doi: 10.1037/0021-843X.117.2.386. [DOI] [PubMed] [Google Scholar]
- Sanders MR, Kirby JN, Tellegen CL, Day JJ. The Triple P-Positive Parenting Program: a systematic review and meta-analysis of a multi-level system of parenting support. Clin Psychol Rev. 2014;34:337–357. doi: 10.1016/j.cpr.2014.04.003. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Sheftall AH, Schoppe-Sullivan SJ, Bridge JA. Insecure attachment and suicidal behavior in adolescents. Crisis. 2014;35:426–430. doi: 10.1027/0227-5910/a000273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley N, Ellis J, Farrelly N, Hollinghurst S, Downe S. Preventing domestic abuse for children and young people: A review of school-based interventions. Child Youth Serv Rev. 2015;59:120–131. doi: 10.1016/j.childyouth.2015.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoeckel M, Weissbrod C. Growing up with an ill parent: An examination of family characteristics and parental illness features. Fam Syst Health. 2015;33:356–362. doi: 10.1037/fsh0000140. [DOI] [PubMed] [Google Scholar]
- Storer HL, Casey E, Herrenkohl T. Efficacy of Bystander Programs to Prevent Dating Abuse Among Youth and Young Adults: A Review of the Literature. Trauma Violence Abuse. 2016;17:256–269. doi: 10.1177/1524838015584361. [DOI] [PubMed] [Google Scholar]
- Swearer S, Cary P. Perceptions and Attitudes Toward Bullying in Middle School Youth. Journal of Applied School Psychology. 2003;19:63–79. [Google Scholar]
- Taylor R, Dobson A, Mirzaei M. Contribution of changes in risk factors to the decline of coronary heart disease mortality in Australia over three decades. Eur J Cardiovasc Prev Rehabil. 2006;13:760–768. doi: 10.1097/01.hjr.0000220581.42387.d4. [DOI] [PubMed] [Google Scholar]
- ten Have M, de Graaf R, van Dorsselaer S, Verdurmen J, van’;t Land H, Vollebergh W, Beekman A. Incidence and course of suicidal ideation and suicide attempts in the general population. Can J Psychiatry. 2009;54:824–833. doi: 10.1177/070674370905401205. [DOI] [PubMed] [Google Scholar]
- The Leuven College Surveys (LCS) 2015 http://www.mindmates.be/page.php?id=28 (accessed 08.06.16)
- The WHO World Mental Health Surveys International College Student Project (WMH-ICS) 2015 http://www.hcp.med.harvard.edu/wmh/college_student_survey.php (accessed 08.06.16)
- Trotman GE, Young-Anderson C, Deye KP. Acute Sexual Assault in the Pediatric and Adolescent Population. J Pediatr Adolesc Gynecol. 2015 doi: 10.1016/j.jpag.2015.05.001. (published online May 16, 2016) [DOI] [PubMed] [Google Scholar]
- van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16:219–242. doi: 10.1177/0962280206074463. [DOI] [PubMed] [Google Scholar]
- van Buuren S. Flexible Imputation of Missing Data. CRC Press (Taylor & Francis Group); Boca Raton London New York: 2012. [Google Scholar]
- van Heeringen K. Stress-Diathesis Model of Suicidal Behavior. In: Dwivedi Y, editor. The Neurobiological Basis of Suicide. Boca Raton (FL): 2012. [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanathan S, Datta S, Sheridan P, Lax-Pericall T. “Too Young to be Worried!” Psychiatric Assessment and Follow-up of Young People After Severe Physical Assault in an Inner City Hospital of South London. Ann Med Health Sci Res. 2014;4:85–89. doi: 10.4103/2141-9248.126607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment. 2008;15:391–403. doi: 10.1177/1073191108316030. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Muehlenkamp J, Eckenrode J, Purington A, Baral Abrams G, Barreira P, Kress V. Nonsuicidal self-injury as a gateway to suicide in young adults. J Adolesc Health. 2013;52:486–492. doi: 10.1016/j.jadohealth.2012.09.010. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Wyman PA, Moore SR. Connectedness and suicide prevention in adolescents: pathways and implications. Suicide Life Threat Behav. 2014;44:246–272. doi: 10.1111/sltb.12071. [DOI] [PubMed] [Google Scholar]
- Widom CS, Czaja S, Dutton MA. Child abuse and neglect and intimate partner violence victimization and perpetration: a prospective investigation. Child Abuse Negl. 2014;38:650–663. doi: 10.1016/j.chiabu.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Arria AM, Caldeira KM, Vincent KB, Pinchevsky GM, O’Grady KE. Prevalence and predictors of persistent suicide ideation, plans, and attempts during college. J Affect Disord. 2010;127:287–294. doi: 10.1016/j.jad.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong YJ, Brownson C, Schwing AE. Risk and Protective Factors Associated With Asian American Students’ Suicidal Ideation: A Multicampus, National Study. J Coll Student Dev. 2011;52:396–408. [Google Scholar]
- World Health Organization (WHO) Suicide data. WHO; p. 2016. http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/ (accessed 08.06.16) [Google Scholar]
- Wyman PA. Developmental approach to prevent adolescent suicides: research pathways to effective upstream preventive interventions. Am J Prev Med. 2014;47:S251–256. doi: 10.1016/j.amepre.2014.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You Z, Chen M, Yang S, Zhou Z, Qin P. Childhood adversity, recent life stressors and suicidal behavior in Chinese college students. PloS One. 2014;9:e86672. doi: 10.1371/journal.pone.0086672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Tao M. Relative deprivation and psychopathology of Chinese college students. J Affect Disord. 2013;150:903–907. doi: 10.1016/j.jad.2013.05.013. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Yip PS, Chang SS, Wong PW, Law FY. Association Between Changes in Risk Factor Status and Suicidal Ideation Incidence and Recovery. Crisis. 2015;36:390–398. doi: 10.1027/0227-5910/a000343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


