Abstract
Endoscopic third ventriculostomy (ETV) is an alternative to ventriculoperitoneal shunting for treatment of hydrocephalus. Studies have reported favorable outcomes for up to three-quarters of adult patients. We performed the first ETV outcomes study using an administrative claims database, examining current practice for adult patients in the United States. We queried the Truven Health MarketScan® database for Current Procedural Terminology codes corresponding to ETV and ventriculoperitoneal shunt from 2003 to 2011, including patients over 18 years and data from initial and subsequent hospitalizations. ETV failure was defined as any subsequent ETV or shunt procedure. Five hundred twenty-five patients underwent ETV with 6 months’ minimum follow-up. Mean age was 45.9 years (range 18–86 years). Mean follow-up was 2.2 years (SD: 1.6 years, range 0.5–8.4 years). Etiology of hydrocephalus was 21.3% tumor, 9.0% congenital/aqueductal stenosis, 15.8% hemorrhage, and 53.9% others. ETV was successful in 74.7% of patients. Of 133 who failed, 25 had repeat ETV; 108 had shunt placement. Longer length of stay for index surgery was associated with higher risk of failure (HR: 1.03, p = <0.001), as was history of previous shunt (HR: 2.45, p < 0.001). Among patients with repeat surgeries, median time to failure was 25 days. This study represents a longitudinal analysis of nationwide ETV practice over 9 years. Success rate in this large cohort is similar to that published by other single-center retrospective studies. Age and geographic variation may be associated with surgeon choice of ETV or shunt placement after failure of the initial ETV.
Keywords: Endoscopic third ventriculostomy, Hydrocephalus, Ventriculoperitoneal shunt, Administrative database, Outcomes
INTRODUCTION
Endoscopic third ventriculostomy (ETV) has been shown to be a safe and effective treatment for hydrocephalus of various etiologies [1–5]. Among children, there is evidence supporting that younger age is predictive of a worse outcome after ETV [1, 2], and some evidence on the role of hydrocephalus etiology in outcomes after ETV [1, 2, 4, 6, 7]. The role of ETV in the management of hydrocephalus in adults is less extensively studied. Given the different physiology of cranial development, intracranial compliance, and cerebrospinal fluid (CSF) production and absorption, findings from pediatric studies may not be applicable to adults [8–10]. Woodworth et al. reported on a single-institution series of 124 adult ETV patients with 55% success [11], while Dusick et al. reported on another single-institution series of 108 adult patients with 77% success with shunt independence [10].
The purpose of this study was to use a large, nationally representative administrative database to examine national practice, correlates, and effectiveness of ETV in adult patients with hydrocephalus in the United States.
METHODS
Data Source
The Truven Health MarketScan database is a collection of health insurance claims for working adults and early retirees with employer-sponsored health insurance and their dependents. For the current project, we used the MarketScan Commercial Claims and Encounters database, constructed from paid claims for employee-sponsored health insurance between 2003 and 2011, representing 17 million enrollees in 2003 and up to 52 million enrollees in 2011. We utilized inpatient admission, inpatient service, outpatient service, and enrollment data tables. Within these tables, records from January 1, 2003, to December 31, 2011, were analyzed. The study received exempt status from the University of Chicago and Baylor College of Medicine Institutional Review Boards.
Patient Selection
For the initial procedure hospitalization, we queried inpatient service tables for all hospitalizations for patients 18 years and older from the following Current Procedural Terminology (CPT) procedure codes: (1) ETV codes 62200, 62201 or (2) shunt placement codes 62220, 62223. These codes and associated dates of procedures were used to determine the type and timing of index and follow-up surgeries. For each patient, the first occurrence of ETV in the database while aged 18 years or older was considered the index procedure.
Follow-up Data
Patients with a minimum 6 months’ follow-up were included in the cohort. For these patients, we examined details of any subsequent hospitalization in the inpatient service and inpatient admission tables from the date of the index procedure until the end of the records in 2011. Analysis was then based on initial and subsequent hospitalizations for ETV or shunt.
ETV failure was defined as subsequent surgery for hydrocephalus after primary surgery (i.e., repeat ETV or placement of ventriculoperitoneal shunt [VP shunt]) [12]. Temporary CSF diversion measures, such as ventricular puncture, lumbar puncture, and external ventricular drain placement, were not included. Inpatient deaths were noted, but deaths in general were not included as ETV failure since outpatient deaths are not captured reliably in MarketScan.
To determine duration of postoperative follow-up, we used the enrollment table to obtain the final month of insurance enrollment for each patient. End of follow-up was defined as 1) the last day of the final month of enrollment, 2) the date of discharge with deceased status, or 3) the last date of data collection, December 31, 2011. Postoperative follow-up time was measured from the date of initial ETV to either ETV failure or end of follow-up.
Covariates
Age in years on the date of index admission was available in the inpatient admission tables. We retrieved from the inpatient admission tables and analyzed International Classification of Diseases-9 (ICD-9) diagnosis codes associated with the index hospitalization. Indication for ETV surgery was determined based on previously published methodology using administrative data to examine pediatric hydrocephalus and CSF shunts [13]. We reviewed these codes, focusing on those that occurred at a frequency of ≥ 1% of the study population. We assigned etiology at the time of ETV with the concurrent assignment of the following diagnosis codes: subarachnoid hemorrhage (430), intracerebral hemorrhage (432), central nervous system (CNS) tumor (191–194, 198.3–198.4, 225.0–2 and 225.8–9, 227.4, 237.0–1 and 237.5–7, 239.6, 239.7), meningitis (320–322, 326), trauma (767.4, 851.xx–854.xx, 995.55), cerebral cyst (348), normal pressure hydrocephalus (331.5), and congenital hydrocephalus (742.3 [coding for aqueductal stenosis]). Due to limitations in ICD-9 coding, the indications were not mutually exclusive and did not describe the entire study population. Those with no indications or multiple indications were classified as other etiology.
History of previous CSF shunt was determined from diagnosis codes of inpatient and outpatient encounters from initial enrollment until the day prior to index ETV surgery. Codes considered to indicate history of CSF shunt include ICD-9-CM procedure codes of shunt surgery (02.32–35, 02.42, 02.43); ICD-9-CM codes indicating the presence of or complications of shunt device (V45.2, V53.01, 996.2, 996.63); and CPT codes for shunt surgery (62190, 62192, 62194, 62220, 62223, 62225, 62230, 62180, 62256, 62258). Patients were classified either as having a history of prior shunt or no history of prior shunt.
Statistical Analysis
We summarized the distribution of patient demographics and surgery-related characteristics using descriptive analyses. We performed chi-squared tests for univariate analyses of categorical variables and the Mann-Whitney U test for continuous variables. Kaplan-Meier plots were used to estimate time to being ETV failure-free and 1-, 2-, and 5-year success rates. The association of age, gender region, payer type, etiology, length of stay associated with index procedures (index length of stay [iLOS]), and history of prior shunt with being ETV failure-free were quantified using hazard ratios (HRs) estimated from multivariate Cox proportional hazards models. Multivariate logistic regression was used to examine factors associated with second ETV versus VP shunt placement among ETV failures. We conducted a sensitivity analysis to examine the effects of mortality and changes in insurance coverage before the end of the study period. We used two-sided tests, with p values < 0.05 considered to be statistically significant. Statistical analyses were performed with Stata 12 (StataCorp, College Station, Texas).
RESULTS
730 patients aged 18 years and older were identified who had a primary ETV procedure between 2003 and 2011, inclusive. The sample represents rates of 2.1 (95% confidence interval [CI]: 1.3–2.9) index ETV procedures per million enrollees and dependents of enrollees aged 18 and older in 2003 to 3.0 (95% CI: 2.5–3.6) per million in 2011. Among this group, 525 patients were identified as the study sample. Patients without a minimum 6 months’ follow-up or whose residential region were unknown (n = 4) were excluded.
Table 1 describes the demographic characteristics of this study cohort.
Table 1.
Characteristics of the study sample (n = 525)
| Characteristic | Overall (n = 525) n (%) |
Success (n = 392) n (%) |
Failure (n = 133) n (%) |
p value |
|---|---|---|---|---|
| Median age (range) | 47 (18–86) | 48 (18–86) | 45 (18–85) | |
| Mean age [SD] | 45.9 (16.3) | 46.9 (16.3) | 43.2 (16.3) | 0.03 |
| Age (years) | ||||
| 18–39 | 174 (33.1) | 126 (72.4) | 48 (27.6) | 0.40 |
| 40+ | 351 (66.9) | 266 (75.8) | 85 (24.2) | |
| Gender | ||||
| Male | 234 (44.6) | 176 (75.2) | 58 (24.8) | 0.80 |
| Female | 291 (55.4) | 216 (74.2) | 75 (25.8) | |
| Region | ||||
| Northeast | 76 (14.5) | 55 (72.4) | 21 (27.6) | 0.89 |
| Midwest | 143 (27.2) | 105 (73.4) | 38 (26.6) | |
| South | 219 (41.7) | 167 (76.3) | 52 (23.7) | |
| West | 87 (16.6) | 65 (74.7) | 22 (25.3) | |
| Payer type | ||||
| PPO/Comprehensive | 365 (69.5) | 272 (74.5) | 93 (25.5) | 0.91 |
| HMO/Other | 160 (30.5) | 120 (75.0) | 40 (25.0) | |
| Etiology | ||||
| Congenital | 47 (9.0) | 33 (70.2) | 14 (29.8) | 0.78 |
| Tumor | 112 (21.3) | 87 (77.7) | 25 (22.3) | |
| Hemorrhage | 83 (15.8) | 61 (73.5) | 22 (26.5) | |
| Other | 283 (53.9) | 211 (74.6) | 72 (25.4) | |
| History of prior shunt | ||||
| No prior shunt | 433 (82.5) | 340 (78.5) | 93 (21.5) | <0.001 |
| Prior shunt | 92 (17.5) | 52 (56.5) | 40 (43.5) | |
| Index length of stay, mean [SD] | 9.9 [12.5] | 8.5 [10.9] | 14.2 [15.6] | <0.001 |
HMO = health maintenance organization, PPO = preferred provider organization, SD = standard deviation
In this cohort, the most common ICD-9 diagnosis pertaining to hydrocephalus etiology was tumor (21.3%), subarachnoid/intracranial hemorrhage (15.8%), congenital (9.0%), trauma (5.5%), normal pressure hydrocephalus (NPH) (3.4%), and meningitis (1.5%). Other etiology encompassed 43.4% of the group. Due to the small number, patients with trauma, NPH, or meningitis were included in the “other” category.
ETV Failure
Table 1 compares the subjects with failed primary ETVs (n = 133) to those with successful ETV procedures (n = 392). A majority (74.7%) had successful treatment of hydrocephalus with ETV: that is, they did not receive any subsequent hydrocephalus surgery (shunt or revision ETV). Median postoperative follow-up time was 1.2 years (range 0–7.9 years). Of the 25.3% whose ETV failed (133 patients), 18.8% (25/133 patients) received a repeat ETV; 81.2% (108/133 patients) received a VP shunt.
A statistically significant difference in age was seen between these two groups: those with failed ETVs had a mean age 3.7 years younger (p = 0.03). The difference in mean iLOS was also statistically significant, with patients with ETV success having a mean 8.5 (SD 10.9) days in the hospital, while those with ETV failure spent a mean 14.2 (SD 15.6) days in the hospital (p < 0.001).
Inpatient mortality did not differ between the groups. Eight inpatient deaths (1.5%) were associated with this ETV cohort. Median (interquartile range [IQR]) years to death was 2.1 (0.9–2.4), range 0.6–3.4, years following the index surgery. Three had one to two subsequent surgeries or admissions between the index procedure and death. Two died during an admission for ETV-related surgery at ages 60 and 85. Two of the eight deaths occurred in patients with hemorrhage diagnoses. The other cases included two in the tumor category and four in the “other” category.
In the multivariate Cox proportional hazards model, history of prior shunt and iLOS were associated with an increased risk of ETV failure (Table 2).
Table 2.
Multivariate Cox regression of factors associated with ETV failures (n = 525)
| Characteristic | HR | 95% CI | p Value | |
|---|---|---|---|---|
| Age (years) | ||||
| 18 to 39 | 1.00 | REF | REF | |
| 40+ | 1.00 | 0.69 | 1.46 | 1.00 |
| Gender | ||||
| Male | 1.00 | REF | REF | |
| Female | 1.10 | 0.78 | 1.56 | 0.58 |
| Region | ||||
| Northeast | 1.00 | REF | REF | |
| Midwest | 0.91 | 0.52 | 1.57 | 0.73 |
| South | 0.77 | 0.46 | 1.29 | 0.31 |
| West | 0.82 | 0.45 | 1.51 | 0.53 |
| Payer type | ||||
| PPO/Comprehensive | 1.00 | REF | REF | |
| HMO/Other | 1.10 | 0.75 | 1.62 | 0.63 |
| Etiology | ||||
| Tumor | 1.00 | REF | REF | |
| Congenital | 1.01 | 0.51 | 2.00 | 0.98 |
| Hemorrhage | 0.77 | 0.42 | 1.42 | 0.40 |
| Other | 0.92 | 0.57 | 1.46 | 0.71 |
| Prior shunt | ||||
| No | 1.00 | REF | REF | |
| Yes | 2.45 | 1.64 | 3.65 | <0.001 |
| Index length of stay | 1.03 | 1.02 | 1.04 | <0.001 |
CI = confidence interval, ETV = endoscopic third ventriculostomy, HR = hazard ratio
Figure 1 shows a Kaplan-Meier curve of those who were ETV failure-free over time (“ETV survival”). Success rates at 1, 2, and 5 years were 76.2%, 74.0%, and 70.7%, respectively. Figures 2 and 3 show Kaplan-Meier estimates of those who were ETV failure-free divided by age group and hydrocephalus etiology, respectively. Log-rank analysis showed no significant difference in ETV success based on age (p = 0.32) or etiology (p = 0.78). Figure 4 shows Kaplan-Meier estimates of those who were ETV failure-free among patient groups with a history of prior shunt or no prior shunt. Consistent with the multivariate analysis, those with a history of prior shunt showed a lower proportion of ETV success (log-rank test, p < 0.001). Moreover, among those who failed (i.e. they required subsequent surgery for treatment of hydrocephalus in the form of repeat ETV or VP shunt placement), failure occurred at a median of 25 days after ETV surgery; 54% occurred in the first 30 days after the index ETV surgery.
Fig. 1.
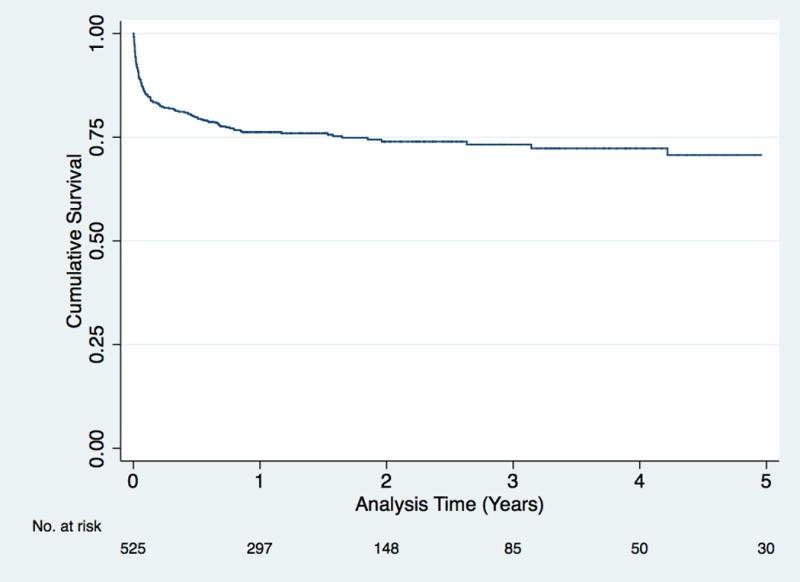
Kaplan-Meier estimate of proportion ETV failure-free (“ETV survival”).
Fig. 2.
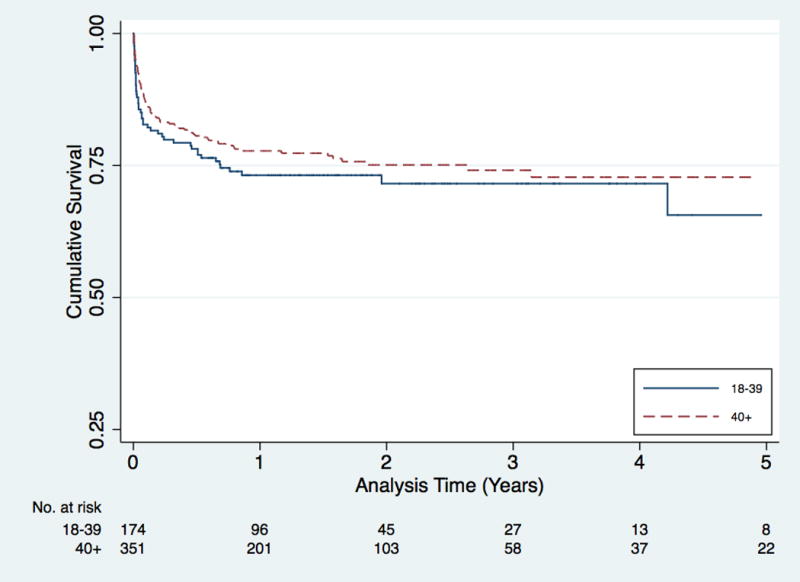
Kaplan-Meier estimate of proportion ETV failure-free (“ETV survival”) by age. Log-rank analysis shows no significant difference between the curves for these age groups (p = 0.32).
Fig. 3.
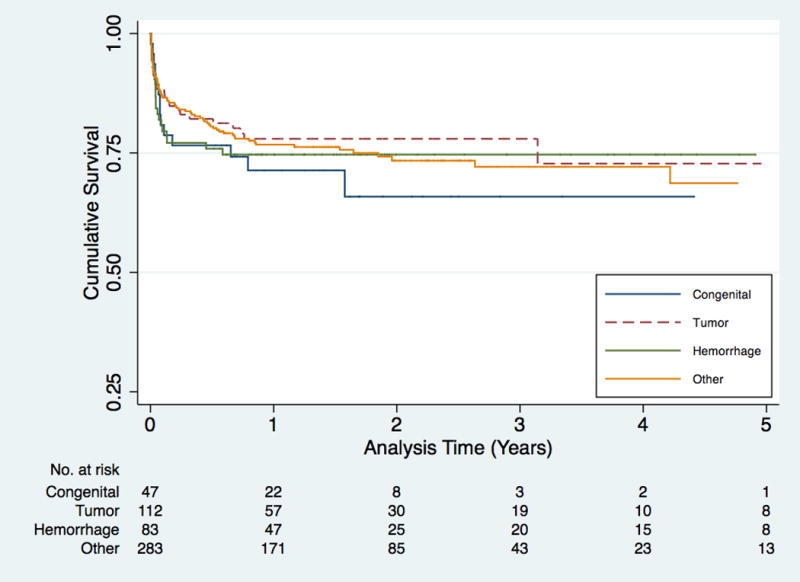
Kaplan-Meier estimate of proportion ETV failure-free (“ETV survival”) by etiology of hydrocephalus. Log-rank analysis shows no significant difference between the curves for these etiologies (p = 0.78).
Fig. 4.
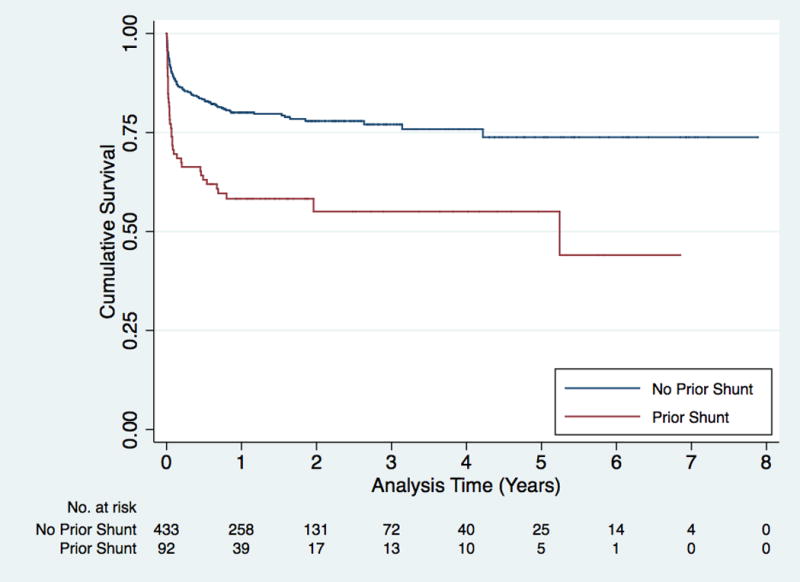
Kaplan-Meier estimate of proportion ETV failure-free (“ETV survival”) by history of shunt prior to ETV. Log-rank analysis shows a significant difference between the curves for the group with a prior shunt and the group without history of prior shunt (p < 0.001).
Revision Surgery After ETV Failure
Among subjects whose primary ETV failed (n = 133), most received a VP shunt (n = 108, 81.2% of 133), while a smaller proportion underwent a revision ETV procedure (n = 25). A statistically significant difference in age was found between these two groups: those who received a shunt had a mean age that was 12 years older than those who received a revision ETV (Table 3). In the multivariate logistic regression, the association between older age and receiving VP shunt instead of revision ETV was statistically significant (Table 4). The association between region and revision ETV was also statistically significant. Patients residing in the South or West were less likely to receive revision ETV compared to patients in the Northeast. Due to very low numbers of revision ETVs, the South and West regions were combined for this analysis.
Table 3.
Characteristics of patients with ETV failure, by second treatment (n = 133)
| Characteristic | Shunt (n = 108) n (%) |
ETV (n = 25) n (%) |
p Value |
|---|---|---|---|
| Median age | 47 | 27 | |
| Mean age [SD] | 45.4 [16.2] | 33.6 [13.6] | 0.00 |
| Age (years) | |||
| 18–39 | 33 (68.8) | 15 (31.2) | 0.01 |
| 40+ | 75 (88.2) | 10 (11.8) | |
| Gender | |||
| Male | 49 (84.5) | 9 (15.5) | 0.40 |
| Female | 59 (78.7) | 16 (21.3) | |
| Region | |||
| Northeast | 13 (61.9) | 8 (38.1) | 0.01 |
| Midwest | 28 (73.7) | 10 (26.3) | |
| South/West | 67 (90.5) | 7 (9.5) | |
| Payer type | |||
| PPO/Comprehensive | 74 (79.6) | 19 (20.4) | 0.46 |
| HMO/Other | 34 (85.0) | 6 (15.0) | |
| Etiology | |||
| Congenital | 11 (78.6) | 3 (21.4) | 0.08 |
| Tumor | 16 (64.0) | 9 (36.0) | |
| Hemorrhage | 18 (81.8) | 4 (18.2) | |
| Other | 63 (87.5) | 9 (12.5) | |
| Mean index LOS | 15.4 [16.5] | 9.1 [9.2] | 0.08 |
| Prior shunt | 33 (82.5) | 7 (17.5) | 0.80 |
LOS = length of stay (at initial ETV surgery)
Table 4.
Multivariate logistic regression for second ETV after failure (n = 133)
| Characteristic | ORa | 95% CI | p Value | |
|---|---|---|---|---|
| Age (years) | ||||
| 18–39 | 1.00 | REF | REF | |
| 40+ | 0.24 | 0.08 | 0.72 | 0.011 |
| Gender | ||||
| Male | 1.00 | REF | REF | |
| Female | 1.64 | 0.57 | 4.70 | 0.36 |
| Region | ||||
| Northeast | 1.00 | REF | REF | |
| Midwest | 0.69 | 0.19 | 2.48 | 0.57 |
| South/West | 0.20 | 0.06 | 0.72 | 0.01 |
| Payer Type | ||||
| PPO/Comprehensive | 1.00 | REF | REF | |
| HMO/Other | 1.10 | 0.75 | 1.62 | 0.63 |
| Etiology | ||||
| Tumor | 1.00 | REF | REF | |
| Congenital | 0.65 | 0.11 | 3.83 | 0.64 |
| Hemorrhage | 1.10 | 0.20 | 6.10 | 0.91 |
| Other | 0.47 | 0.14 | 1.61 | 0.23 |
| Prior shunt | ||||
| No | 1.00 | REF | REF | |
| Yes | 0.73 | 0.22 | 2.41 | 0.61 |
| Index length of stay | 0.96 | 0.91 | 1.01 | 0.13 |
| Constant | 2.23 | 0.51 | 9.69 | 0.28 |
OR > 1 favors ETV, OR < 1 favors shunt
OR = odds ratio
DISCUSSION
This administrative claims database study of ETV procedures in adults from 2003 to 2011 is the largest study to date of ETV in the adult neurosurgical literature. The overall success rate was 74.7%, with a median follow-up of 1.6 years. The median time to failure was 25 days, with 54.1% of failures occurring in the first 30 days of surgery. Success rates at 1, 2, and 5 years were 76.2%, 74.0%, and 70.7%, respectively. Among those who failed, 18.8% received another ETV, while 81.2% received a shunt. History of prior shunt and iLOS were associated with risk of ETV failure.
ETV Failure
The ETV success rate found in this study (74.7%), which is defined as the absence of follow-up ETV or shunt procedure, is on par with reported rates [3, 10–12, 14–17] among studies reporting on adult patients (55–88%). Our finding that most failures occur within the first month after surgery is also consistent with previous reports [1, 4, 10, 18, 19]. Variation in success rates may be associated with numerous factors, from patient factors, such as age and etiology of hydrocephalus, to provider factors such as surgeon/center experience and volume. In this study, age, gender, payer type, region, and etiology of hydrocephalus were not associated with ETV failure.
Our study found no association between age and ETV outcomes. Few studies have examined the association between age and outcomes after ETV in purely adult populations; those that did, such as studies by Dusick et al. (n = 108) and Woodworth et al. (n = 124), did not find an association between age and ETV outcomes among adult patients [10, 11].
Patients had a median 1.25 years (ranging from 0 days to 7.9 years) of postoperative follow-up time. Most failures were within 6 months of the index ETV. The ETV success and failure groups did not differ in duration of follow-up.
The role of hydrocephalus etiology on ETV outcomes is not entirely delineated. No significant association was found between diagnosis and outcomes in this study. The clinical impact of this is unclear, though there is incomplete understanding in the literature predicting ETV success based on hydrocephalus etiology. For instance, while Fukuhara et al. (n = 89) have found that a history of intracerebral infection was associated with failure after ETV [18], both Dusick et al. (n = 108) and Siomin et al. (n = 101) reported no significant difference in ETV failure rates between subjects with a history of infection and those with hydrocephalus of obstructive etiologies [10, 20]. In a large, multicenter study, Drake et al. did not find an association between hydrocephalus etiology and outcome after ETV in a pediatric population [1], though his colleagues later reported a significant role of hydrocephalus etiology on ETV outcomes [21].
History of prior shunt was significantly correlated with an increased risk of ETV failure (HR: 2.45, 95% CI: 1.64–3.65, p < 0.001), a finding consistent with most other reports in adult populations, such as those by Woodworth et al. and Amini and Schmidt [11, 22], as well as in large pediatric cohorts [21]. Length of index hospital stay of the initial ETV also correlated with the risk of ETV failure, with increasing length of stay corresponding to increasing risk of ETV failure (HR: 1.03, 95% CI: 1.02–1.04, p < 0.001). This may suggest the presence of comorbidities, continuing hydrocephalus symptoms, or perioperative adverse events complicating the ETV hospital course.
ETV is a procedure with a steep learning curve; many studies have reported better outcomes toward the end of single-surgeon series [10, 12, 17, 23]. By contrast, Drake did not find an association between surgeon or hospital volume and outcomes in the Canadian multicenter pediatric ETV study (n = 368) [1]. In this study, there was no association between the year of ETV procedure and outcome (data not shown); in this nationwide setting, our data does not give information about individual surgeon experience.
Revision Surgery After ETV Failure
In our study, a majority of subjects who required revision surgery after primary ETV failure received VP shunts (81.2%) rather than another ETV (18.8%). Geographical variation and age were associated with the type of revision surgery received after ETV failure. This is observational and descriptive of surgeons’ choice of surgery at ETV failure. Practice variation and clinical factors may account for some of these choices, though lack of further detail in the data set limits the ability to draw conclusions. To our knowledge, no studies have been published that directly compare repeat ETV to VP shunt after primary ETV failure in adult patients. In two papers in the pediatric literature describing failed ETV, Mohanty et al. (primary ETV failure n = 13) and Cinalli et al. (primary ETV failure n = 15), the decision of ETV versus VP shunt after ETV failure was based on the patency of the original ETV stoma, ascertained by endoscopic re-exploration and/or magnetic resonance imaging. In cases of patent stoma, VP shunt was placed, and in cases of closed stoma, repeat ETV was performed. Siomin et al. exclusively examined repeat ETV (n = 20) after primary ETV failure; all cases were found to have closed stoma. In these three studies, the success rate of repeat ETV was similar to that of the primary ETV [6, 19, 24]. An area of future study may be an evaluation of the success rate of repeat ETV in the adult population.
Strengths and Limitations
Strengths of this study include the large sample size, the nationally representative database, and the longitudinal follow-up. Since the data represent a variety of geographic and hospital settings, including academic and community hospitals, these results are more generalizable than those reported in single-institution series in the literature.
Limitations are mainly related to the nature of administrative insurance claims database inquiry, as well as those inherent to the MarketScan database. This proprietary national claims database is comprised of enrollees who are employees of major U.S. employers or those enrolled in other commercial health plans. This patient sample may represent a group with different access to neurologic and neurosurgical care and/or different health outcomes than that with public insurance.
All clinical conditions and events identified from the database are based on healthcare claims. Standard claims coding practices limit the level of clinical detail that can be obtained. Claims are generated for financial reasons; while they are audited within the insurance systems, they cannot be validated by medical chart review for this study. Conditions not captured in the claims database (such as outpatient death) would not be recognized in this study. One of the main limitations of using a large administrative database is dependence on coding. While procedure codes are directly linked to billing, thus are likely to be reliable and correct in the database, diagnosis codes may not be as reliable. We attempted to extract information regarding etiology of hydrocephalus using diagnosis codes according to methodology published by the Hydrocephalus Clinical Research Network, though the limitations of ICD-9 codes are well recognized [13]. We used caution in drawing conclusions regarding hydrocephalus etiology from this type of database.
Additional limitations include those known to retrospective claims-based studies: absence of complete treatment data and demographic data such as race, ethnicity, income, and educational level. As with retrospective database studies, no conclusions about causal relationships can be drawn.
CONCLUSIONS
The overall success rate of primary ETV in adult patients was 74.7%, with a median postoperative follow-up of 1.25 years. Success rates at 1, 2, and 5 years were 76.2%, 74.0%, and 70.7%, respectively. Among those with ETV failure, 18.8% received repeated ETV, while 81.2% had VP shunt placement. Younger age and geographic variation were associated with choice of surgery at ETV failure.
Footnotes
CONFLICTS OF INTEREST/DISCLOSURES
The authors declare that they have no financial or other conflicts of interest in relation to this research and its publication.
References
- 1.Drake JM, Canadian Pediatric Neurosurgery Study Group Endoscopic third ventriculostomy in pediatric patients: the Canadian experience. Neurosurgery. 2007;60:881–6. doi: 10.1227/01.NEU.0000255420.78431.E7. discussion -6. [DOI] [PubMed] [Google Scholar]
- 2.Warf BC. Hydrocephalus in Uganda: the predominance of infectious origin and primary management with endoscopic third ventriculostomy. J Neurosurg. 2005;102:1–15. doi: 10.3171/ped.2005.102.1.0001. [DOI] [PubMed] [Google Scholar]
- 3.Kadrian D, van Gelder J, Florida D, Jones R, Vonau M, Teo C, et al. Long-term reliability of endoscopic third ventriculostomy. Neurosurgery. 2008;62(Suppl 2):614–21. doi: 10.1227/01.neu.0000316265.59596.8c. [DOI] [PubMed] [Google Scholar]
- 4.Feng H, Huang G, Liao X, Fu K, Tan H, Pu H, et al. Endoscopic third ventriculostomy in the management of obstructive hydrocephalus: an outcome analysis. J Neurosurg. 2004;100:626–33. doi: 10.3171/jns.2004.100.4.0626. [DOI] [PubMed] [Google Scholar]
- 5.Baldauf J, Oertel J, Gaab MR, Schroeder HW. Endoscopic third ventriculostomy in children younger than 2 years of age. Childs Nerv Syst. 2007;23:623–6. doi: 10.1007/s00381-007-0335-4. [DOI] [PubMed] [Google Scholar]
- 6.Cinalli G, Sainte-Rose C, Chumas P, Zerah M, Brunelle F, Lot G, et al. Failure of third ventriculostomy in the treatment of aqueductal stenosis in children. J Neurosurg. 1999;90:448–54. doi: 10.3171/jns.1999.90.3.0448. [DOI] [PubMed] [Google Scholar]
- 7.Koch D, Wagner W. Endoscopic third ventriculostomy in infants of less than 1 year of age: which factors influence the outcome? Childs Nerv Syst. 2004;20:405–11. doi: 10.1007/s00381-004-0958-7. [DOI] [PubMed] [Google Scholar]
- 8.Albeck MJ, Skak C, Nielsen PR, Olsen KS, Borgesen SE, Gjerris F. Age dependency of resistance to cerebrospinal fluid outflow. J Neurosurg. 1998;89:275–8. doi: 10.3171/jns.1998.89.2.0275. [DOI] [PubMed] [Google Scholar]
- 9.Czosnyka M, Czosnyka ZH, Whitfield PC, Donovan T, Pickard JD. Age dependence of cerebrospinal pressure-volume compensation in patients with hydrocephalus. J Neurosurg. 2001;94:482–6. doi: 10.3171/jns.2001.94.3.0482. [DOI] [PubMed] [Google Scholar]
- 10.Dusick JR, McArthur DL, Bergsneider M. Success and complication rates of endoscopic third ventriculostomy for adult hydrocephalus: a series of 108 patients. Surg Neurol. 2008;69:5–15. doi: 10.1016/j.surneu.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 11.Woodworth GF, See A, Bettegowda C, Batra S, Jallo GI, Rigamonti D. Predictors of surgery-free outcome in adult endoscopic third ventriculostomy. World Neurosurg. 2012;78:312–7. doi: 10.1016/j.wneu.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 12.Buxton N, Ho KJ, Macarthur D, Vloeberghs M, Punt J, Robertson I. Neuroendoscopic third ventriculostomy for hydrocephalus in adults: report of a single unit’s experience with 63 cases. Surg Neurol. 2001;55:74–8. doi: 10.1016/s0090-3019(01)00352-4. [DOI] [PubMed] [Google Scholar]
- 13.Simon TD, Hall M, Riva-Cambrin J, Albert JE, Jeffries HE, Lafleur B, et al. Infection rates following initial cerebrospinal fluid shunt placement across pediatric hospitals in the United States. Clinical article. J Neurosurg Pediatr. 2009;4:156–65. doi: 10.3171/2009.3.PEDS08215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bognar L, Markia B, Novak L. Retrospective analysis of 400 neuroendoscopic interventions: the Hungarian experience. Neurosurg Focus. 2005;19:E10. doi: 10.3171/foc.2005.19.6.11. [DOI] [PubMed] [Google Scholar]
- 15.Grunert P, Charalampaki P, Hopf N, Filippi R. The role of third ventriculostomy in the management of obstructive hydrocephalus. Minim Invasive Neurosurg. 2003;46:16–21. doi: 10.1055/s-2003-37957. [DOI] [PubMed] [Google Scholar]
- 16.Santamarta D, Diaz Alvarez A, Goncalves JM, Hernandez J. Outcome of endoscopic third ventriculostomy. Results from an unselected series with noncommunicating hydrocephalus. Acta Neurochir (Wien) 2005;147:377–82. doi: 10.1007/s00701-005-0484-8. discussion 82. [DOI] [PubMed] [Google Scholar]
- 17.Schroeder HW, Niendorf WR, Gaab MR. Complications of endoscopic third ventriculostomy. J Neurosurg. 2002;96:1032–40. doi: 10.3171/jns.2002.96.6.1032. [DOI] [PubMed] [Google Scholar]
- 18.Fukuhara T, Vorster SJ, Luciano MG. Risk factors for failure of endoscopic third ventriculostomy for obstructive hydrocephalus. Neurosurgery. 2000;46:1100–9. doi: 10.1097/00006123-200005000-00015. discussion 9–11. [DOI] [PubMed] [Google Scholar]
- 19.Mohanty A, Vasudev MK, Sampath S, Radhesh S, Sastry Kolluri VR. Failed endoscopic third ventriculostomy in children: management options. Pediatr Neurosurg. 2002;37:304–9. doi: 10.1159/000066310. [DOI] [PubMed] [Google Scholar]
- 20.Siomin V, Cinalli G, Grotenhuis A, Golash A, Oi S, Kothbauer K, et al. Endoscopic third ventriculostomy in patients with cerebrospinal fluid infection and/or hemorrhage. J Neurosurg. 2002;97:519–24. doi: 10.3171/jns.2002.97.3.0519. [DOI] [PubMed] [Google Scholar]
- 21.Kulkarni AV, Drake JM, Kestle JR, Mallucci CL, Sgouros S, Constantini S, et al. Predicting who will benefit from endoscopic third ventriculostomy compared with shunt insertion in childhood hydrocephalus using the ETV Success Score. J Neurosurg Pediatr. 2010;6:310–5. doi: 10.3171/2010.8.PEDS103. [DOI] [PubMed] [Google Scholar]
- 22.Amini A, Schmidt RH. Endoscopic third ventriculostomy in a series of 36 adult patients. Neurosurg Focus. 2005;19:E9. [PubMed] [Google Scholar]
- 23.Ersahin Y, Arslan D. Complications of endoscopic third ventriculostomy. Childs Nerv Syst. 2008;24:943–8. doi: 10.1007/s00381-008-0589-5. [DOI] [PubMed] [Google Scholar]
- 24.Siomin V, Weiner H, Wisoff J, Cinalli G, Pierre-Kahn A, Saint-Rose C, et al. Repeat endoscopic third ventriculostomy: is it worth trying? Childs Nerv Syst. 2001;17:551–5. doi: 10.1007/s003810100475. [DOI] [PubMed] [Google Scholar]


