The “female athlete triad” has long been recognised as a syndrome that has the potential to affect female athletes and consists of three inter-related disorders:
Osteoporosis
Disordered eating
Menstrual disorders.
The potential impact of each of, and the combination of, these disorders is detrimental to performance and to health. Certainly, the increased risk of infertility, stress fractures, eating disorders, and osteoporosis in later life is a high price to pay for involvement in an essentially healthy activity. This is especially true, as many of these factors can be prevented with careful management.
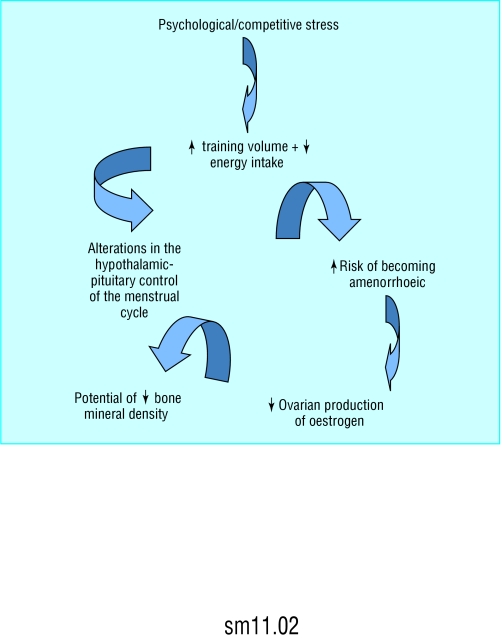
Figure 1.

The female athlete triad can affect performance and health but can be prevented with good management
Why are the three corners of the triad inter-related?
The three corners of the triad are inter-related through psychological and physiological mechanisms. The psychological pressures to perform to an optimal standard, and thus often a perceived requirement to maintain a low body mass, result in a high volume of training. The high volume of training and low energy intake, in addition to stress hormones produced by psychological stress, may lead to a physiological alteration in the endocrinological control of the menstrual cycle, which may ultimately lead to the athlete becoming amenorrhoeic (loss of cycle after menarche). The consequence of being amenorrhoeic through dysfunction of the hypothalamus and pituitary is a decreased production of oestrogen. This hormone has a huge role in maintaining adequate bone mineral density, and a hypo-oestrogenic state (low oestrogen) thus is associated with low bone mineral density and an increased risk of osteoporosis.
Menstrual disorders
The normal regular, healthy menstrual cycle (eumenorrhoea) is about 26-35 days, is controlled by the hypothalamus and pituitary glands, and is divided simplistically into two phases by the occurrence mid-cycle of ovulation. The first half of the cycle is the follicular phase and the second half the luteal phase. The follicular phase is characterised by gradually increasing levels of oestrogen produced primarily by the ovaries, while the luteal phase is characterised by high concentrations of oestrogen and progesterone. Loss of oestrogen is associated with an increased risk of osteoporosis and coronary artery disease.
Figure 2.
The corners of the female athlete triad (osteoporosis, disordered eating, and menstrual disorders) are inter-related through psychological and physiological mechanisms
Menstrual cycle disturbances can progress from luteal phase defects to anovulation (no ovulation) and then to oligomenorrhoea (irregular cycles) and amenorrhoea. The diagnosis of luteal phase defects is completed with measures such as a luteal phase less than 10 days long, inadequate progesterone concentration, ultrasound measurement of pre-ovulatory follicle diameter, and endometrial biopsy.
Prevalence of amenorrhoea
| • Population—5% |
| • Athletes—1-44% (luteal phase defects 79%) |
Causes in athletes
Causes of menstrual disorders are multiple and not completely understood. Pulsatile release of luteinising hormone is decreased, which leads initially to luteal phase defects. In addition, compared with sedentary women, women with luteal phase defects and amenorrhoea have higher concentrations of growth hormone and cortisol and lower concentrations of leptin, insulin, and triiodothyronine. These hormones are related to metabolism, and thus to nutritional and metabolic status. If energy availability is low over a period of time, as indicated by these hormones, the menstrual cycle is temporarily “switched off” or suppressed to conserve energy.
This article is adapted from the 3rd edition of the ABC of Sports and Exercise Medicine, which will be published later this year.
Luteal phase defects may be less obvious than amenorrhoea in athletes, but the clinical consequences are serious
Eating disorder or disordered eating?
Some female athletes do have a classic eating disorder, potentially driven by a need to maintain a low body mass for performance. Anorexia, however, has specific clinical diagnostic criteria, and not all athletes satisfy the criteria that indicate a disturbance in how they experience body weight or shape.
The term “anorexia athletica” has been used to distinguish between pathological anorexia and eating disorders associated with training and sports performance. The criteria for this include perfectionism, compulsiveness, competitiveness, high self motivation, menstrual disturbances, and at least one unhealthy method of weight control (fasting, vomiting, and use of diet pills, laxatives, or diuretics). In reality, athletes in this category will show signs of disordered eating, as opposed to an eating disorder, and clinical observations indicate a prevalence of 15-60% for disordered eating, with 50% of these women compulsively overexercising. This will obviously lead to a decreased energy intake and thus a negative energy balance.
Figure 3.

Athlete having bone scan
Osteoporosis or osteopenia?
Osteoporosis is defined as a bone mineral density more than 2.5 standard deviations below the average for young adults and is associated with a reduction in bone mass with no alteration in the mineralisation of bone tissue. Bone tissue responds well to mechanical stress, and thus exercise, alongside nutrition, is essential in the teenage years to attain peak bone mass. Women with low energy availability and low oestrogen concentrations, however, have increased risk of becoming osteoporotic.
Oestrogen protects the skeleton from bone resorption, while deficiencies in calcium, vitamin D, and other bone trophic substances from inadequate nutritional intake also lead to increased bone resorption. Long term risk of osteoporosis seems to be reduced by attaining a good peak bone mineral density in early life and by lifelong exposure to oestrogen. Thus, long periods of amenorrhoea may increase the long term risk of osteoporosis.
Ostoeopenia is much more common than osteoporosis in female athletes and associated with decalcification. Researchers have called for osteopenia to replace osteoporosis in the triad.
Effects of menstrual disturbances on bone mineral density
Studies have consistently shown lower bone mineral density in amenorrhoeic athletes than eumenorrhoeic athletes. The bone mineral density of amenorrhoeic runners has been reported to be lower at the spine (-5%), hip (-6 %), and whole body (-3%) than in eumenorrhoeic runners. Furthermore, eumenorrhoeic runners with disordered eating patterns have lower bone mineral density at the spine (-11%), hip (-5%), and whole body (-5%) than eumenorrhoeic runners without disordered eating. Athletes with less severe menstrual disruption have intermediate bone densities. The bone mineral density of the femur in amenorrhoeic athletes is closer to that of sedentary controls than that of the spine. This suggests that regular running (or weight bearing activity) can offset bone loss because of menstrual disturbances.
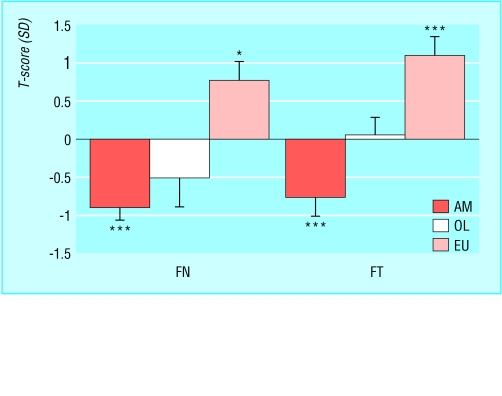
Figure 4.
Bone mineral density of proximal femur of 50 endurance trained female runners compared with the young peak bone mass according to a standard reference range (Hologic Inc). This is known as the T score and is expressed in standard deviations above or below the mean. This chart shows the approximate linear relation between number of menstrual cycles per year and bone density. (AM=amenorrhoeic (0-3 cycles a year), OL=oligomenorrhoeic (4-10 cycles a year), EU=eumenorrhoeic (11-13 cycles a year), FN=neck of femur, FT=trochanteric region of proximal femur. *P<0.02, **P<0.01, ***P<0.001.
Luteal phase defects and amenorrhoea are not caused by low levels of body fat and associated lack of production of peripherally produced oestrogen in female athletes but by decrease in availability of energy
Energy balance = energy in-energy out
A low percentage of body fat is associated with negative energy balance. Thus, a low percentage of body fat should be seen as a signal that disordered eating and menstrual disturbances may be present
Osteopenia is defined as bone mineral density 1-2.5 standard deviations below the average. Both osteopenia and osteoporosis are negative for athletes as they increase the risk of stress fractures
Treatment of female athlete triad
Prevention is better than treatment, but prevention in athletes is made difficult by the nature of the game. Athletes will resist increasing body weight, decreasing training loads, and using the contraceptive pill (because of worries about weight gain, breast tenderness, and mood changes). In addition, athletes will find it difficult to admit to menstrual problems and disordered eating or eating disorders. These points should be kept firmly in mind when consulting with athletes.
Perhaps the first step is for all individuals and agencies involved with female athletes to be made fully aware of the potential causes, mechanisms, and long term risks of the female athlete triad. In addition, women athletes, their parents, and medical staff should be informed about the triad and its pitfalls. The management of the athlete, however, is most imperative.
Eating disorders
The treatment of true eating disorders should be undertaken only by qualified staff on an inpatient or outpatient basis. The treatment plan will vary for each individual on the basis of psychology and environment, but several common sense guidelines exist.
The ultimate goal is to increase the nutritional status of the woman. This will reverse many of the symptoms associated with disordered eating (for example, bloating, constipation, fatigue, lanugo, and dry skin—although not loss of enamel from teeth), reverse menstrual disorders, and help reduce the risk of osteopenia or osteoporosis. Of course, many of these changes will ultimately increase muscle strength, decrease the risk of injury, and thus increase training and sports performance.
Menstrual disturbances
Once disturbances have been established as non-pathological (the athlete should be medically assessed), the treatment is based on training load and nutritional intake. Athletes will benefit from decreasing the intensity or duration of training by 10%; they then should increase energy intake by initially small amounts.
Menstrual disturbances and decreased bone mineral density
Treatment is reliant on oestrogen replacement. Oestrogen replacement can be provided with the contraceptive pill, although progestogen-only pills and the mini pill should be avoided. If the athlete agrees to take the pill, she should understand that it does not correct the underlying problem. If menses (bleeding) is not desired, the practitioner can sometimes provide monophasic pills in which the placebo week is missing. This, however, should only be a short term approach. Hormone replacement therapy, as provided for postmenopausal women, has been successful in only a few studies. Hormone replacement therapy with unopposed oestrogens should be avoided and should not be used for long periods.
Useful organisations
| • American College of Sports Medicine, 401 West Michigan Street, Indianapolis, IN, USA 46202-3233 (www.ACSM.org) |
| • National Osteoporosis Society, PO Box 10, Radstock, Bath BA3 3YB (www.nos.org.uk) |
Other treatments recommended for bone loss are specific oestrogen receptor modulators, intranasal calcitonin, and bisphosphonates. These products are used primarily in older women, and little is known about their effects on bone mineral density in amenorrhoeic women. Calcium intake should be increased to 1500-2000 mg a day, and calcium should be taken alongside vitamin D. Calcium does not increase bone mineral density but may aid in preventing further decreases.
When energy intake matches expenditure, body weight will not increase but maintenance of muscle mass will increase performance
Athletes with menstrual disturbances can increase bone mineral density with weight bearing exercise or treatment on reversal of the menstrual disturbance. Bone mineral density, however, will never return to what it may have been if the athlete had remained eumenorrhoeic. If trabecular bone is lost during long term amenorrhoea, reversal of bone mineral density may be impossible
Competing interests: None declared.
The ABC of Sports and Exercise Medicine is edited by Gregory P Whyte, director of science and research, Olympic Medical Institute, Northwick Park Hospital, Middlesex; Mark Harries, consultant physician, Olympic Medical Institute; and Clyde Williams, professor of sport and exercise medicine, University of Loughborough.
The graph of bone mineral density in a female athlete is adapted from Gibson JH, Mitchell A, Harries M, Reeve J. Nutritional and exercise related determinants of bone density in elite female runners. Osteoporosis Int 2004;15: 611-8. The photograph of a gymnast is with permission of Getty Images.
References
- • American College of Sports Medicine. Position stand on the female athlete triad. Med Sci Sports Exercise 1997;29: 1-9 [DOI] [PubMed] [Google Scholar]
- • Drinkwater B. Women in sport. The encyclopaedia of sports medicine. Blackwell Science, Oxford, 2000
- • De Souza MJ. Menstrual disturbances in athletes: A focus on luteal phase defects. Med Sci Sports Exercise 2003;35: 1553-63 [DOI] [PubMed] [Google Scholar]
- • Loucks A, Vurdun M, Heath E. Low energy availability, not stress of exercise, alters LH pulsatility in exercising women. J App Physiol 1998;84: 37-46 [DOI] [PubMed] [Google Scholar]
- • Rutherford O. Spine and total body mineral density in amenorrheic endurance athletes. J App Physiol 1993;74: 2904-8 [DOI] [PubMed] [Google Scholar]