Abstract
Background
The absence of atrial contraction (AC) after the maze procedure has been reported to cause subsequent annular dilatation and to increase the risk of embolic stroke. We hypothesized that the lack of AC could increase the risk of permanent pacemaker (PPM) implantation in patients undergoing the maze procedure.
Methods
In 376 consecutive patients who had undergone a cryo-maze procedure and combined valve operation, recovery of AC was assessed at baseline and at immediate (≤2 weeks), early (≤1 year, 4.6±3.8 months), and late (>1 year, 3.5±1.1 years) postoperative stages.
Results
With a median follow-up of 53 months, 10 patients underwent PPM implantation. Seven PPM implants were for sinus node dysfunction (pauses of 9.6±2.4 seconds), one was for marked sinus bradycardia, and two were for advanced/complete atrioventricular block. The median (interquartile range) time to PPM implantation was 13.8 (0.5–68.2) months. Our time-varying covariate Cox models showed that the absence of AC was a risk factor for PPM implantation (hazard ratio, 11.92; 95% confidence interval, 2.52 to 56.45; p=0.002).
Conclusion
The absence of AC may be associated with a subsequent risk of PPM implantation.
Keywords: Atrial contraction, Atrial fibrillation, Maze procedure, Valve surgery, Permanent pacemaker
Introduction
The Cox maze procedure is widely used for restoring sinus rhythm (SR) in patients with atrial fibrillation (AF) who undergo cardiac valve surgery [1,2]. Despite a high reported success rate of 75% to 95%, a significant proportion of patients fail to recover atrial contraction (AC) after the maze operation [3–7]. The absence of AC could compromise the efficacy of the maze procedure by limiting the atrial contribution to ventricular performance [7]. According to recently published studies, failed AC recovery was associated with an increased risk of subsequent thromboembolic stroke [8] and aggravation of tricuspid regurgitation (TR) [9].
However, the clinical impact of AC recovery on the risk of subsequent permanent pacemaker (PPM) implantation after maze surgery has rarely been evaluated in this patient group. Since AF and valve surgery are associated with sinus node dysfunction (SND) [10,11] and the risk of PPM implantation [12,13], respectively, we hypothesized that AC recovery failure could increase the risk of PPM implantation due to additional adverse effects on the cardiac conduction system.
The objective of the present study was to assess the incidence of PPM implantation and to evaluate the potential association between the absence of AC and the subsequent risk of PPM implantation in patients undergoing a cryo-maze procedure combined with valve surgery for AF and valvular diseases.
Methods
1) Study population
The inclusion criteria for the present study were as follows: (1) a history of AF and valvular heart disease; and (2) having undergone a modified Cox maze III procedure using cryoablation combined with valve surgery at the Samsung Medical Center between January 2003 and December 2009. Patients with the following conditions were excluded: PPM implantation prior to or during the maze procedure, complex congenital heart disease, and the cut-and-sew technique for the Cox maze procedure, microwave, or radiofrequency ablation. Patients who underwent a maze operation without valve surgery were also excluded.
A total of 396 consecutive patients underwent a cryo-maze operation, of whom 20 were excluded for the following reasons: nine for the absence of combined valve surgery (three cases of atrial septal defect closure, two for myxoma resection, one for ventricular septal defect closure, one for patent foramen ovale closure, one for patent ductus arteriosus ligation, and one for left atrial [LA] rupture repair), six for using other methods for the maze procedure (the cut-and-sew technique, microwave, or radiofrequency ablation), two for PPM implantation during the maze procedure, and three for tetralogy of Fallot. Therefore, 376 patients were ultimately enrolled in this analysis. Table 1 lists the demographics, patient characteristics, and combined procedures for all 376 patients. The study protocol was approved by the institutional review board of Samsung Medical Center, and the requirement for written informed consent was waived.
Table 1.
Baseline characteristics
| Characteristic | No PPM (n=366) | PPM (n=10) | p-value |
|---|---|---|---|
| Demographics | |||
| Age (yr) | 57 (47–65) | 63 (51–69) | 0.268 |
| Female | 209 (57) | 8 (80) | 0.199 |
| Thyroid dysfunction | 29 (8) | 2 (20) | 0.269 |
| Hypertension | 99 (27) | 3 (30) | 1.000 |
| Diabetes | 39 (11) | 0 | 0.608 |
| Previous stroke or transient ischemic attack | 59 (16) | 1 (10) | 0.723 |
| Chronic kidney disease | 7 (2) | 0 | 0.931 |
| Coronary artery disease | 24 (7) | 0 | 1.000 |
| AF characteristics | |||
| AF duration (yr) | 24 (6–60) | 55 (19–104) | 0.102 |
| Paroxysmal | 40 (11) | 2 (20) | 0.309 |
| Persistent | 326 (89) | 8 (80) | |
| Operative procedure | |||
| AV replacement | 77 (21) | 4 (40) | 0.231 |
| AV plasty | 11 (3) | 0 (0) | 1.000 |
| MV replacement | 190 (52) | 6 (60) | 0.753 |
| MV plasty/mitral annuloplasty | 106 (29) | 3 (30) | 1.000 |
| TV replacement | 8 (4) | 0 | 1.000 |
| TV plasty/tricuspid annuloplasty | 267 (73) | 10 (100) | 0.069 |
| Multivalve surgerya) | 49 (13) | 3 (70) | 0.148 |
| Coronary artery bypass graft surgery | 11 (3) | 0 | 0.218 |
Values are presented as median (interquartile range) or number (%).
PPM, permanent pacemaker; AF, atrial fibrillation; AV, aortic valve; MV, mitral valve; TV, tricuspid valve.
Indicates operation involving ≥3 sites among the AV, MV, and TV areas.
2) Maze procedure
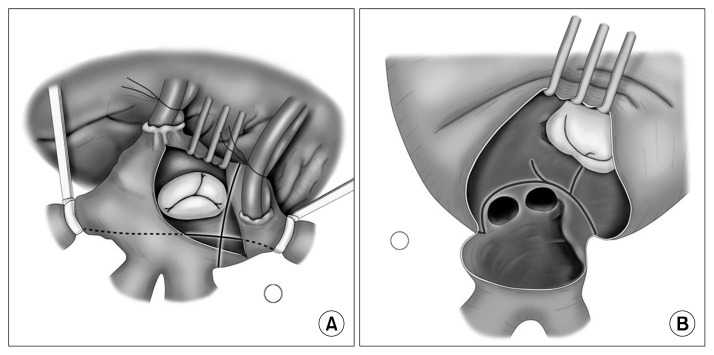
Detailed techniques of the modified Cox maze III procedure were described in our previous report [2]. In brief, cryoablation was performed using a T-shaped cryoprobe (Frigitronics; Cooper Surgical, Shelton, CT, USA) with cryogenerators set at −60° C. To create a transmural lesion, each burst of cryoablation was delivered to the endocardium for 160 seconds, and additional epicardial cryoablation was performed as needed. We isolated the pulmonary veins using linear cryolesions and the incisional atriotomy lines. The cryolesions were then extended to the mitral annulus and to the LA appendage. Suture obliteration of the LA appendage was then performed. Following the right atrial incision parallel to the right atrioventricular (AV) groove, a cryolesion was made from the tricuspid valve (TV) posterior annulus toward the coronary sinus and then to the left atriotomy site. When the right atrium was large, another lesion was made from the right atriotomy site to the anterior annulus of the TV (Fig. 1).
Fig. 1.
Operative technique. (A) Right atrial procedure. (B) Left atrial procedure.
3) Postoperative management and electrocardiographic follow-up
The postoperative rhythm was continuously monitored for 48 hours and electrical cardioversion was performed on patients who remained in AF rhythm after the operation. Warfarin was administered to all patients, whereas antiarrhythmic drugs (40 to 80 mg of sotalol or 100 to 400 mg of amiodarone per day) were only prescribed to patients who showed ongoing AF after electrical cardioversion. During follow-up, serial electrocardiograms (1, 3, 6, 9, and 12 months) and 24-hour Holter monitoring (6 and 12 months) were carried out. If patients complained of symptoms that were suggestive of AF recurrence, electrocardiography and 24-hour Holter monitoring were repeated. The indications for PPM implantation were third-degree AV block, symptomatic sick sinus syndrome, symptomatic bradycardia, a heart rate of less than 40 beats per minute, or intra- or infra-His block on an electrophysiological study, confirmed by a staff cardiologist specializing in electrophysiology.
4) Echocardiographic follow-up and measurement of atrial contraction
Comprehensive transthoracic echocardiography was carried out using 2.5-MHz transducers (Acuson 512; Siemens Medical Solution, Mountain View, CA, USA or Vivid 7; GE Medical System, Milwaukee, WI, USA). We measured AC in patients with normal SR. AC recovery was assessed by measuring the peak velocity of the transmitral A-wave prior to the maze procedure, immediately afterwards (≤2 weeks, 4.2±1.5 days), and before (≤1 year, 4.6±3.8 months) or after (>1 year, 3.5±1.1 years) 1 year of follow-up. We considered AC to have recovered when the peak A-wave velocity was measured at 10 cm/sec or more [4]. The LA volume indexed to body surface area (LAVi) was calculated using the ellipsoid method. Each variable was measured as an average of at least 5 consecutive beats. In the late stage, echocardiographic data were only available in 353 patients because 13 patients died during follow-up (five from a malignancy, four from heart failure, two from pulmonary infection, and two from unknown causes). Additionally, follow-up echocardiographic examinations were not performed in 10 patients.
5) Statistical analysis
Continuous variables were described as the mean±standard deviation or as the median with interquartile range (IQR). The distribution of continuous variables was first analyzed with the Shapiro-Wilk test for normality, and the Student t-test or the Mann-Whitney U-test was used as appropriate. The results for categorical variables were presented as percentages, and the Fisher exact test was performed to compare these results. Risk factors for PPM implantation after the maze operation were evaluated using a univariate Cox proportional hazards model. Freedom from PPM implantation was estimated using Kaplan-Meier analysis, and the time-varying covariate Cox model was used to evaluate the relationship between the lack of AC and PPM implantation. All statistical analyses were performed using PASW Statistics ver. 18.0 software for Windows (SPSS Inc., Chicago, IL, USA). All p-values were 2-sided, and p-values <0.05 were considered to indicate statistical significance.
Results
1) Recovery of sinus rhythm and atrial contraction after the maze operation
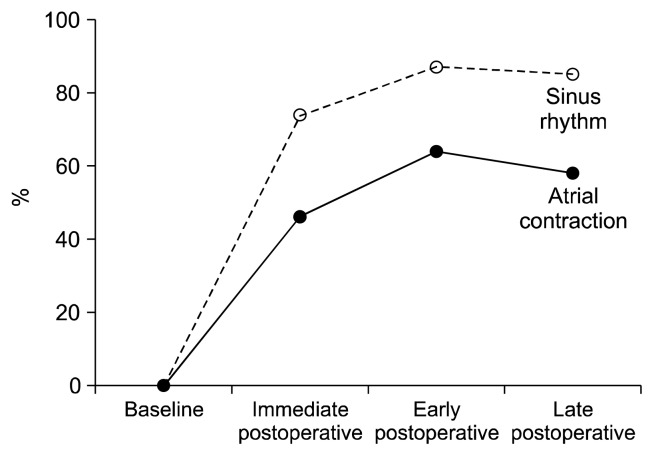
Serial changes in the recovery rates of SR and AC are depicted in Fig. 2. The recovery rates of SR continued to increase in the immediate (≤2 weeks, 4.2±1.5 days) and early postoperative stages (≤1 year, 4.6±3.8 months), with SR recovery rates of 74% (278 of 376) and 87% (327 of 376), respectively. In the late postoperative stage (>1 year, 3.5±1.1 years), SR was noted in 85% (300 of 353) of patients, which was only a 2% reduction in the SR recovery rate when compared to that of the early stage. A similar trend was observed in the AC recovery rate over the follow-up stages. However, the AC recovery rate was at least 20% lower than the SR recovery rate at each stage: 46% (174 of 376), 66% (241 of 376), and 58% (204 of 353), respectively. Approximately one-quarter to one-third of patients with restored SR failed to recover AC in each stage.
Fig. 2.
Serial changes in the recovery rates of sinus rhythm and atrial contraction.
2) Patients with or without permanent pacemaker implantation
Over a median (IQR) follow-up of 53 (28–74) months, 10 of the 376 patients (3%) underwent PPM implantation. The indications for PPM implantation were as follows: SND with prolonged pauses (9.6±2.4 seconds, n=7), marked sinus bradycardia (n=1), and complete or advanced AV block (n=2). The median (IQR) time to PPM implantation was 13.8 (0.5–68.2) months after the maze operation.
The baseline clinical characteristics and the detailed valve operations performed along with the maze procedure are summarized in Table 1. There were no significant differences in the baseline factors between the PPM and non-PPM groups, although the PPM group showed a trend for a longer preoperative AF duration (p=0.102), a higher proportion of females (p=0.199), and a higher frequency of multi-valve (p=0.148) or TV surgery (p=0.069).
The 2 groups also showed no significant differences in the majority of echocardiographic parameters measured in each stage. However, the PPM group exhibited more frequent AC recovery failure than the non-PPM group, especially in the early and late postoperative stages. Additionally, LA volume in the PPM group became significantly greater in the late postoperative stage than in the non-PPM group (p=0.011).
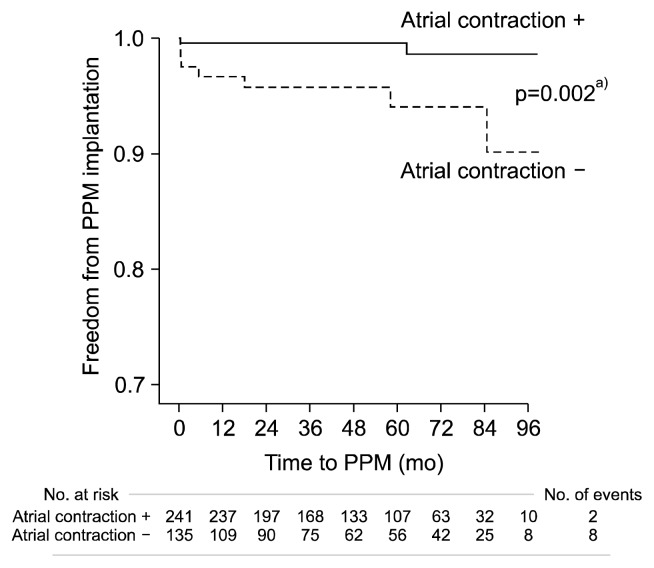
3) Risk factors for permanent pacemaker implantation
To assess the risk factors associated with PPM implantation, Cox proportional hazards models were constructed with risk variables in a univariate analysis (Table 2). Among these variables, risk factors for PPM implantation included the absence of AC in the early stage (hazard ratio [HR], 6.02; 95% confidence interval [CI], 1.21 to 30.08; p=0.029) and in the late stage (HR, 6.59; 95% CI, 1.32 to 32.97; p=0.022). Freedom from PPM implantation is shown in Fig. 3. Our time-varying covariate Cox models showed that the absence of AC (HR, 11.92; 95% CI, 2.52 to 56.45; p=0.002) was a risk factor for PPM implantation.
Table 2.
Risk factors for permanent pacemaker implantation (univariate Cox regression analysis)
| Variable | Hazard ratio (95% confidence interval) | p-value |
|---|---|---|
| Female gender | 2.97 (0.63–13.99) | 0.169 |
| Atrial fibrillation duration (mo) | 1.01 (1.00–1.02) | 0.089 |
| Lack of AC in the early stage | 6.02 (1.21–30.08) | 0.029 |
| Lack of AC in the late stage | 6.59 (1.32–32.97) | 0.022 |
AC, atrial contraction.
Fig. 3.
Comparison of left atrial contraction between groups. “Atrial contraction +” represents patients who recovered atrial contraction, whereas “atrial contraction −” represents those who did not recover atrial contraction. PPM, permanent pacemaker. a)Time-varying covariate Cox models showed that the lack of atrial contraction (hazard ratio, 11.92; 95% confidence interval, 2.52–56.45; p=0.002) was a risk factor for PPM implantation.
Discussion
1) New findings
The present study is the first to demonstrate a significant association between the lack of AC recovery in the early postoperative stage and the subsequent risk of PPM implantation in patients who underwent a maze procedure combined with valve surgery.
Although some studies have evaluated AC recovery after maze operations, only serial changes in AC were described, or several risk factors for the lack of AC recovery were investigated in relatively small patient populations [3–7]. Moreover, the clinical implications of AC recovery failure during long-term follow-up have been evaluated in only a few studies. Buber et al. showed that the absence of AC resulted in a significant increase in the risk for thromboembolic stroke after the maze procedure, even for patients with SR [8]. In another study, restored AC after the maze operation was suggested to be an independent protective factor against TR progression [9]. In contrast, we demonstrated that the lack of AC was associated with a subsequent risk of PPM implantation. This was shown using one of the largest cohorts of patients treated with combined maze and cardiac valve surgery.
2) Lack of atrial contraction and the risk of pacemaker implantation
In our study, the failure rates for AC recovery in the early (4.6±3.8 months) and late (3.5±1.1 years) postoperative stages were 36% and 42%, respectively (Fig. 2). Moreover, approximately one-third of patients, including those with SR, failed to recover AC. These results are in good agreement with data from previous studies [3–8].
Several explanations may account for the significant association between the absence of AC and the increased risk of PPM implantation. First, ongoing AF in patients without AC recovery could induce direct, irreversible impairment of the sinus or AV node. As ongoing AF deteriorates the automaticity of the sinus node, the expression of ion channels that allow for pacemaker current (If) in the sinus node is downregulated [14], and spontaneous sarcoplasmic reticulum Ca2+ release (the Ca2+ clock) becomes defective [15]. Moreover, the absence of AC is known to cause atrial pressure elevation, atrial and annular dilatation, and aggravation of TR [9,16]. Therefore, the AV node and the bundle of His located around the tricuspid annulus could be overstretched and greatly distorted as anatomical remodeling becomes aggravated. This change, along with injury caused by the valve operation, could further reduce the functionality of these structures. Finally, elevated atrial pressure and ongoing AF could induce atrial fibrosis [17,18], especially perinodal fibrosis, which predisposes patients to SND. Recently, using late gadolinium-enhanced magnetic resonance imaging, Akoum et al. [19] demonstrated that fibrosis around the sinus node, right atrium, and LA was more extensive in patients with SND than in those without SND. In our study, 8 of the 10 patients with PPM implantation did not experience AC recovery in the immediate and late postoperative stages (Table 3). Additionally, the increase in LA volume was more prominent in the PPM group than in the non-PPM group during follow-up.
Table 3.
Echocardiographic parameters
| Variable | No PPM | PPM | p-value |
|---|---|---|---|
| Preoperative | |||
| No. of patients | 366 | 10 | |
| LV EDD (mm) | 54 (49–61) | 56 (48–60) | 0.962 |
| LV ejection fraction (%) | 58 (52–63) | 59 (54–64) | 0.748 |
| LAVi (mm3) | 55 (44–71) | 69 (60–72) | 0.567 |
| Atrial contraction (+) | 0 | 0 | 1.000 |
| Immediate postoperative | |||
| No. of patients | 366 | 10 | |
| LV EDD (mm) | 50 (47–56) | 52 (46–56) | 0.862 |
| LV ejection fraction (%) | 56 (50–62) | 55 (47–58) | 0.346 |
| LAVi (mm3) | 54 (43–70) | 62 (45–72) | 0.699 |
| Atrial contraction (+) | 172 (47) | 2 (20) | 0.115 |
| Early postoperative | |||
| No. of patients | 366 | 10 | |
| LV EDD (mm) | 51 (48–55) | 53 (46–57) | 0.752 |
| LV ejection fraction (%) | 58 (53–63) | 55 (46–57) | 0.623 |
| LAVi (mm3) | 53 (43–69) | 65 (47–77) | 0.559 |
| LA activity (+) | 239 (65) | 2 (20) | 0.005 |
| Late postoperative | |||
| No. of patients | 343 | 10 | |
| LV EDD (mm) | 50 (45–54) | 53 (47–58) | 0.692 |
| LV ejection fraction (%) | 60 (56–64) | 54 (46–56) | 0.564 |
| LAVi (mm3) | 50 (39–63) | 72 (53–87) | 0.011 |
| LA activity (+) | 202 (59) | 2 (20) | 0.020 |
Values are presented as median (interquartile range) or number (%), unless otherwise stated.
PPM, permanent pacemaker; LV, left ventricle; EDD, end-diastolic diameter; LAVi, left atrial volume index; LA, left atrial.
3) Clinical implications
Syncope with traumatic complications such as head trauma can be problematic in patients undergoing maze and valve surgeries, as anticoagulation therapy is frequently continued [7,20]. Therefore, based upon the results of the present study, close follow-up might be necessary to prevent bradycardia-related syncope when a persistent absence of AC is observed. This is especially relevant in female patients who undergo combined multivalve surgery.
On the other hand, the baseline fibrotic burden in the atrium before the maze procedure is known to affect the failure rate of AC recovery because extensive fibrotic tissue can cause electromechanical uncoupling between neighboring atrial myocytes [17,21]. Our results show that patients without AC in the early stage exhibited a significantly longer AF duration (59±57 months versus 34±40 months, p<0.001) and a greater baseline LAVi (63±20 mm3 versus 56±20 mm3, p=0.014) than those with AC. This suggests a higher baseline fibrosis burden in the non-AC group. Therefore, further studies might be needed to determine whether earlier maze and valve surgery would lead to better outcomes for AF patients with moderate to severe valve disease.
4) Study limitations
The present study is inherently limited due to its retrospective, observational design. In addition, sinus/AV node function or the extent of atrial/perinodal fibrosis was not compared based on the lack of AC recovery. Therefore, prospective studies are needed to more definitively show the clinical implications of the absence of AC on the risk of PPM implantation.
The low incidence of PPM implantation (n=10, 3%) may be questioned. This might be related to the very strict reimbursement policy in Korea. However, because of the small sample number, we could not con duct multivariable analysis. Therefore, the statistical power of this study is weak and was insufficient to demonstrate an independent relationship between AC and PPM.
However, our patient group made up one of the largest cohorts in which this question has been studied, and was rigorously followed with identical treatment plans (>95%) by a single cardiac surgeon at our institution.
5) Conclusion
The absence of AC might result in additional adverse effects on the cardiac conduction system in patients undergoing the maze procedure combined with valve surgery. Therefore, close follow-up may be needed to prevent bradycardia-related syncope when AC does not recover during follow-up. In addition, further studies are needed to determine the optimal time and extent of surgical interventions to control AF. This would minimize the detrimental effects of AC recovery failure on atrial function in patients with AF and valvular diseases.
Acknowledgments
This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan; Fund no. KTCS04-073).
Footnotes
Conflict of interest
No potential conflicts of interest relevant to this article are reported.
References
- 1.Cox JL, Schuessler RB, Boineau JP. The development of the Maze procedure for the treatment of atrial fibrillation. Semin Thorac Cardiovasc Surg. 2000;12:2–14. doi: 10.1016/S1043-0679(00)70010-4. [DOI] [PubMed] [Google Scholar]
- 2.Kim H, Park PW, Sung K, et al. Mid-term results of the Cox maze III procedure combined with open mitral commissurotomy for the treatment of rheumatic mitral stenosis. Circ J. 2010;74:1332–8. doi: 10.1253/circj.CJ-09-1044. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti M, Costello R, Cardenas C, Piazza A, Iglesias R, Baranchuk A. Persistent atrial fibrillation is associated with inability to recover atrial contractility after MAZE IV surgery in rheumatic disease. Pacing Clin Electrophysiol. 2012;35:999–1004. doi: 10.1111/j.1540-8159.2012.03458.x. [DOI] [PubMed] [Google Scholar]
- 4.Yuda S, Nakatani S, Kosakai Y, Yamagishi M, Miyatake K. Long-term follow-up of atrial contraction after the maze procedure in patients with mitral valve disease. J Am Coll Cardiol. 2001;37:1622–7. doi: 10.1016/S0735-1097(01)01193-7. [DOI] [PubMed] [Google Scholar]
- 5.Jessurun ER, van Hemel NM, Kelder JC, et al. The effect of maze operations on atrial volume. Ann Thorac Surg. 2003;75:51–6. doi: 10.1016/S0003-4975(02)04117-6. [DOI] [PubMed] [Google Scholar]
- 6.Reyes G, Benedicto A, Bustamante J, et al. Restoration of atrial contractility after surgical cryoablation: clinical, electrical and mechanical results. Interact Cardiovasc Thorac Surg. 2009;9:609–12. doi: 10.1510/icvts.2009.208173. [DOI] [PubMed] [Google Scholar]
- 7.Lonnerholm S, Blomstrom P, Nilsson L, Blomstrom-Lundqvist C. Long-term effects of the maze procedure on atrial size and mechanical function. Ann Thorac Surg. 2008;85:916–20. doi: 10.1016/j.athoracsur.2007.10.090. [DOI] [PubMed] [Google Scholar]
- 8.Buber J, Luria D, Sternik L, et al. Left atrial contractile function following a successful modified Maze procedure at surgery and the risk for subsequent thromboembolic stroke. J Am Coll Cardiol. 2011;58:1614–21. doi: 10.1016/j.jacc.2011.05.051. [DOI] [PubMed] [Google Scholar]
- 9.Kim HK, Kim YJ, Kim KI, et al. Impact of the maze operation combined with left-sided valve surgery on the change in tricuspid regurgitation over time. Circulation. 2005;112(9 Suppl):I14–9. doi: 10.1161/CIRCULATIONAHA.104.524496. [DOI] [PubMed] [Google Scholar]
- 10.Lee JM, Kalman JM. Sinus node dysfunction and atrial fibrillation: two sides of the same coin? Europace. 2013;15:161–2. doi: 10.1093/europace/eus223. [DOI] [PubMed] [Google Scholar]
- 11.Barrett TW, Abraham RL, Jenkins CA, Russ S, Storrow AB, Darbar D. Risk factors for bradycardia requiring pacemaker implantation in patients with atrial fibrillation. Am J Cardiol. 2012;110:1315–21. doi: 10.1016/j.amjcard.2012.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dawkins S, Hobson AR, Kalra PR, Tang AT, Monro JL, Dawkins KD. Permanent pacemaker implantation after isolated aortic valve replacement: incidence, indications, and predictors. Ann Thorac Surg. 2008;85:108–12. doi: 10.1016/j.athoracsur.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 13.Jokinen JJ, Turpeinen AK, Pitkanen O, Hippelainen MJ, Hartikainen JE. Pacemaker therapy after tricuspid valve operations: implications on mortality, morbidity, and quality of life. Ann Thorac Surg. 2009;87:1806–14. doi: 10.1016/j.athoracsur.2009.03.048. [DOI] [PubMed] [Google Scholar]
- 14.Yeh YH, Burstein B, Qi XY, et al. Funny current downregulation and sinus node dysfunction associated with atrial tachyarrhythmia: a molecular basis for tachycardia-bradycardia syndrome. Circulation. 2009;119:1576–85. doi: 10.1161/CIRCULATIONAHA.108.789677. [DOI] [PubMed] [Google Scholar]
- 15.Joung B, Lin SF, Chen Z, et al. Mechanisms of sinoatrial node dysfunction in a canine model of pacing-induced atrial fibrillation. Heart Rhythm. 2010;7:88–95. doi: 10.1016/j.hrthm.2009.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Izumi C, Miyake M, Takahashi S, et al. Progression of isolated tricuspid regurgitation late after left-sided valve surgery. Clinical features and mechanisms. Circ J. 2011;75:2902–7. doi: 10.1253/circj.CJ-11-0718. [DOI] [PubMed] [Google Scholar]
- 17.Burstein B, Nattel S. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J Am Coll Cardiol. 2008;51:802–9. doi: 10.1016/j.jacc.2007.09.064. [DOI] [PubMed] [Google Scholar]
- 18.Her AY, Choi EY, Shim CY, et al. Prediction of left atrial fibrosis with speckle tracking echocardiography in mitral valve disease: a comparative study with histopathology. Korean Circ J. 2012;42:311–8. doi: 10.4070/kcj.2012.42.5.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akoum N, McGann C, Vergara G, et al. Atrial fibrosis quantified using late gadolinium enhancement MRI is associated with sinus node dysfunction requiring pacemaker implant. J Cardiovasc Electrophysiol. 2012;23:44–50. doi: 10.1111/j.1540-8167.2011.02140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shin HW, Kim YN, Bae HJ, et al. Trends in oral anticoagulation therapy among Korean patients with atrial fibrillation: the Korean Atrial Fibrillation Investigation. Korean Circ J. 2012;42:113–7. doi: 10.4070/kcj.2012.42.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gramley F, Lorenzen J, Koellensperger E, Kettering K, Weiss C, Munzel T. Atrial fibrosis and atrial fibrillation: the role of the TGF-β1 signaling pathway. Int J Cardiol. 2010;143:405–13. doi: 10.1016/j.ijcard.2009.03.110. [DOI] [PubMed] [Google Scholar]