Abstract
Esophageal stents have been used to palliate patients with dysphagia caused by esophageal cancer. Early rigid plastic prostheses have been associated with a high risk of complications. However, with the development of self-expanding stents, it has developed into a widely accepted method for treating malignant esophageal strictures and esophagorespiratory fistulas (ERFs). The present review covers various aspects of self-expanding metallic stent placement for palliating esophageal cancer, including its types, placement procedures, indications, contraindications, complications, and some of innovations that will become available in the future.
Keywords: Esophageal Cancer, Self-Expandable Metallic Stents, Esophageal Stenosis
Graphical Abstract
INTRODUCTION
Esophageal cancer is one of the most common malignancies and a major cause of cancer-related deaths worldwide (1). Over 50% esophageal cancers are found to be incurable at the time of diagnosis because of metastases (2). Dysphagia is the most common symptom of incurable esophageal cancer. The aim of esophageal stenting is to restore luminal patency and thereby maintain oral intake and improve quality of life. However, this procedure carries a risk of major complications such as bleeding and perforation (3). Since the first reports of esophageal stents in the late 1970s, these devices have rapidly evolved from rigid plastic tubes to flexible, self-expanding metallic stents (SEMS) (4). SEMS are cylindrical metallic frames that exert self-expansive forces until they reach their maximum fixed diameter (5). Palliation of esophageal cancer with SEMS was first reported by Domschke et al. (6) in 1990. Since then, SEMS placement has developed into a widely accepted method for treating malignant esophageal strictures and esophagorespiratory fistulas (ERFs) (3).
TYPES OF SEMS
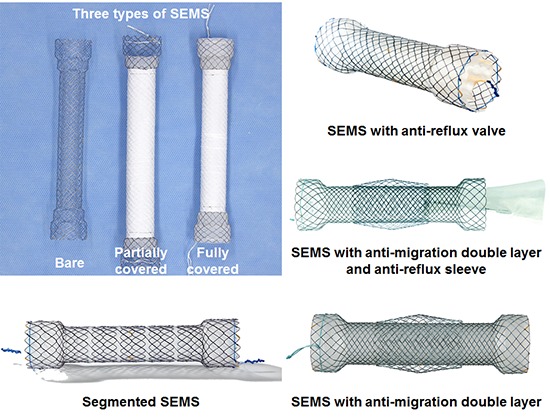
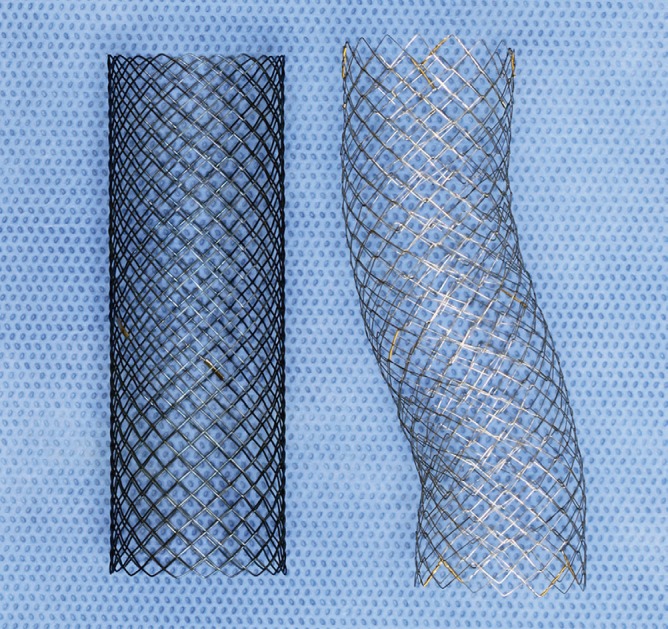
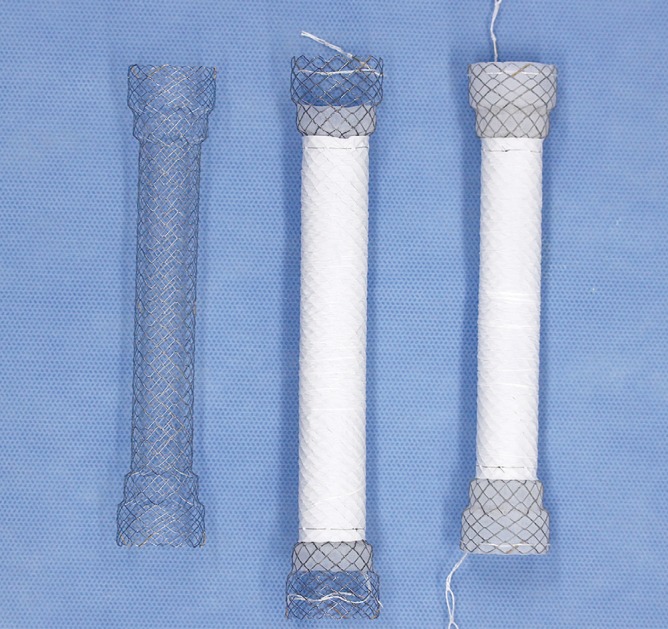
A wide range of SEMS for esophageal cancer are available in Korea (Table 1), and even more are available internationally. Knowledge of the advantages and disadvantages associated with different designs aids physicians in selecting the optimal SEMS for a given condition. Early SEMS were woven from stainless steel wires. At present, all available SEMS are woven from wires made of nitinol, a nickel and titanium alloy known for its shape-memory and superelastic properties. Nitinol SEMS are a major breakthrough because of their greater conformability and smaller profile compared with those of stainless steel SEMS. Two different methods are used to weave SEMS: braiding and knitting (Fig. 1). Braided SEMS are composed of crisscrossed wires that are easily displaced against each other. These SEMS are highly flexible but retain a high axial force. In knitted SEMS, the wire junctions are looped around each other. These SEMS not only are highly flexible but also a have a low axial force and minimal foreshortening. Segmented SEMS consist of several individual SEMS units connected in tandem (Fig. 2). This type of SEMS has high flexibility, but because of the rigidity of the individual SEMS units, it tends to buckle rather than bend. SEMS can be exposed or fully or partially covered with a membrane made of various materials (e.g., silicone and expanded-polytetrafluoroethylene [ePTFE]) to prevent tumor ingrowth (Fig. 3). Most SEMS have antimigration features (e.g., shouldered ends and double-layer design) to decrease stent migration (Fig. 4). To decrease gastroesophageal reflux, some manufacturers offer variants of SEMS with antireflux features such as sleeves and valves (Fig. 5). For insertion, SEMS is compressed and loaded into a distal-release or proximal-release delivery system (Fig. 6). Depending on the profile of the delivery system (> 10.5 Fr or ≤ 10.5 Fr), SEMS is deployed either over the guidewire (over-the-wire technique) or through the working channel of the endoscope (through-the-scope [TTS] technique).
Table 1. Commercially available SEMS for esophageal cancer in Korea.
| Manufacturer and product name | Composition | Delivery system | SEMS | Special features | ||
|---|---|---|---|---|---|---|
| Diameter | Length | Diameter | Length | |||
| S & G Biotech | ||||||
| EGIS (fully covered/uncovered) | Nitinol, silicone, ePTFE | 18 Fr (covered, distal release), 15 Fr (uncovered, distal release) | 70 cm | 16/18/20 mm (proximal shoulders, 20, 24/22, 26/24, and 28 mm; distal shoulders, 20, 24/22, 26/24, and 28 mm) | 4/6/8/10/12 cm (proximal shoulders, 13 mm; distal shoulders, 7 and 13 mm) | Anti-reflux sleeve variant available; double-step shoulders design for decreasing stent migration |
| Taewoong Medical | ||||||
| Niti-S (fully covered/partially covered) | Nitinol, silicone | 16/20/22 Fr (distal and proximal release) | 70 cm | 16/20/24 mm (proximal shoulder, 18/22/28 mm; distal shoulder, 18/22/28 mm) | 6/8/10/12/14/15 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | - |
| Niti-S TTS (fully covered/partially covered) | Nitinol, silicone | 10.5 Fr (distal release) | 160/180 cm | 18/20 mm (proximal shoulder, 20/22 mm; distal shoulder, 20/22 mm) | 6/8/10/12/14/15 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | - |
| Niti-S Double (fully covered) | Nitinol, silicone | 18/20/22 Fr (distal and proximal release) | 70 cm | 16/18/20/22/24/28 mm (proximal shoulder, 18/20/22/24/28/30 mm; distal shoulder, 18/20/22/24/28/30 mm) | 6/8/10/12/14/15 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | Double-layer design for decreasing stent migration |
| Niti-S Double Antireflux (fully covered) | Nitinol, silicone | 18/20/22 Fr (distal release) | 70 cm | 16/18/20/22/24/28 mm (proximal shoulder, 18/20/22/24/28/30 mm; distal shoulder, 18/20/22/24/28/30 mm) | 6/8/10/12/14/15 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | Anti-reflux sleeve; double-layer design for decreasing migration |
| Conoi (fully covered) | Nitinol, silicone | 12/14/16 Fr (distal release), 14/16 Fr (proximal release) | 70 cm | 10/12/14/16 mm (proximal shoulder, 12/14/16/18) | 6/8/10/12/14/15 cm (proximal shoulder, 10 mm) | Smaller diameters for hypopharyngeal strictures |
| CERVICAL (fully covered) | Nitinol, silicone | 18/20 Fr (distal release), 16/20/22 Fr (proximal release) | 70 cm | 16/18/20/22/24 mm (proximal shoulder, 18/20/22/24/28 mm; distal shoulder, 18/20/22/24/28 mm) | 6/8/10/12/14/15 cm (proximal shoulder, 10 mm; distal shoulder, 5 mm) | - |
| M.I. Tech | ||||||
| Choostent (fully covered) | Nitinol, silicone | 18/24 Fr (symmetrical; distal release), 18 Fr (asymmetrical; distal release) | 70 cm | 18/22 mm (proximal shoulder, 24/28 mm; distal shoulder, 24/28 mm) | 4/7/10/13 cm (symmetrical; proximal shoulder, 20 mm; distal shoulder, 20 mm), 3/6/8/10 cm (asymmetrical; proximal shoulder, 20 mm; distal shoulder, 20 mm) | Anti-reflux valve variant available; segmented body design for better conformability |
| Choostent Cervical (fully covered) | Nitinol, silicone | 18 Fr (distal release) | 70 cm | 18 mm (proximal shoulder, 24 mm; distal shoulder, 26 mm) | 3/5/7/9/12 cm (proximal shoulder, 20 mm; distal flare, 7 mm) | Segmented body design for better conformability; |
| Hanarostent (fully covered) | Nitinol, silicone | 18/24 Fr (distal release) | 70 cm | 18/22 mm (proximal shoulder, 24/28 mm; distal shoulder, 24/28 mm) | 4/7/10/13 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | Anti-reflux valve variant available |
| Hanarostent TTS (fully covered/partially covered) | Nitinol, silicone | 10.5 Fr (distal release) | 180 cm | 18 mm (proximal and distal shoulders, 24 mm) | 3/5/7/9 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | - |
| Hanarostent Skidproof (fully covered) | Nitinol, silicone | 18 Fr (distal release) | 70 cm | 20 mm (proximal and distal shoulders, 24 mm) | 2/4/6/8/10/12/14/16/18 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | Skidproof design for decreasing stent migration |
| Hanarostent Bone Shape (partially covered) | Nitinol, silicone | 18/24 Fr (distal release) | 70 cm | 20/22 mm (proximal shoulder, 26/28 mm; distal shoulder, 26/28 mm) | 6/8/11 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | Anti-reflux valve variant available; bone shape proximal end to decrease tissue overgrowth |
| Standard SciTech | ||||||
| Bonastent (fully covered) | Nitinol, silicone | 15/18 Fr (distal release) | 70 cm | 18 mm (proximal shoulder, 24 mm; distal shoulder, 24 mm) | 20/40/60/80/100/120 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | - |
| Bonastent Shim Antireflux (fully covered) | Nitinol, silicone | 21 Fr (distal release) | 70 cm | 22 mm (proximal shoulder, 28 mm; distal shoulder, 28 mm) | 50/70/90/110 cm (proximal shoulder, 20 mm; distal shoulder, 20 mm) | Anti-reflux valve |
SEMS = self-expanding metallic stents, ePTFE = expanded-polytetrafluoroethylene, TTS = through-the-scope.
Fig. 1.
Photograph shows a braided SEMS (right) (constructed in-house) and a knitted SEMS (left) (constructed in-house).
SEMS = self-expanding metallic stents.
Fig. 2.

Photograph shows a segmented SEMS (Choostent; M.I. Tech, Pyeongtaek, Korea).
SEMS = self-expanding metallic stents.
Fig. 3.
Photograph shows an uncovered SEMS (right) (EGIS; S & G Biotech, Seongnam, Korea), PCSEMS (middle) (EGIS; S & G Biotech), and FCSEMS (left) (EGIS; S & G Biotech).
SEMS = self-expanding metallic stents, PCSEMS = partially covered self-expanding metallic stents, FCSEMS = fully covered self-expanding metallic stents.
Fig. 4.

Photograph shows a SEMS with shouldered ends and a double-layer design (Niti-S Double; Taewoong Medical, Gimpo, Korea).
SEMS = self-expanding metallic stents.
Fig. 5.
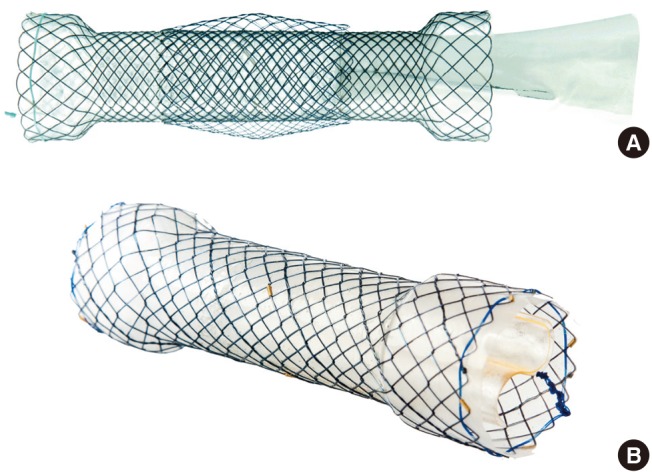
Photograph shows (A) a SEMS with antireflux sleeves (Niti-S Double Anti-reflux; Taewoong Medical, Gimpo, Korea); (B) a SEMS with antireflux valves (Hanarostent; M.I. Tech, Pyeongtaek, Korea).
SEMS = self-expanding metallic stents.
Fig. 6.
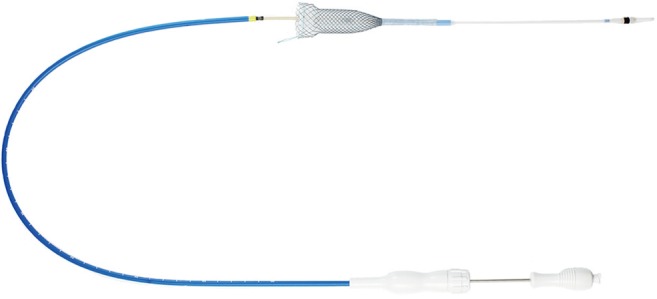
Photograph shows a SEMS deployed using a proximal-release delivery system (Niti-S; Taewoong Medical, Gimpo, Korea).
SEMS = self-expanding metallic stents.
Uncovered vs. covered SEMS
The currently available SEMS for esophageal cancer include uncovered and covered SEMS. Uncovered SEMS are prone to tumor ingrowth, which can lead to recurrent dysphagia. For this reason, these stents are seldom used today. Instead, covered SEMS have become the mainstay for esophageal cancer because the covering membrane of these stents can prevent recurrent dysphagia caused by tumor ingrowth; however, these stents are much more prone to migration than are uncovered SEMS (3). Covered SEMS are either fully covered (FCSEMS) along the entire length of the stent or partially covered (PCSEMS), in which the proximal and distal ends of the stent are devoid of a covering membrane. Because FCSEMS can prevent tumor embedding entirely, they are usually easily removable under endoscopic and/or fluoroscopic guidance. In contrast, PCSEMS do not prevent tumor embedding within the uncovered portions; therefore, these stents may be less prone to migration and more difficult to remove under endoscopic and/or fluoroscopic guidance than are FCSEMS. In a case series by Seven et al. (7), the migration rate was significantly higher with FCSEMS than with PCSEMS (38% vs. 9%; P < 0.001). However, the tumor overgrowth rate was significantly higher with PCSEMS than with FCSEMS (53% vs. 29%; P = 0.004). As no randomized controlled trials have compared FCSEMS and PCSEMS, future studies are needed to determine the optimal type of covered SEMS.
Anti-migration features
Early-model SEMS often used outer fixation barbs to prevent migration; however, these stents appeared to be associated with an increased risk of intractable pain and fatal bleeding (8,9). Larger-diameter SEMS have also been investigated. One study showed that 22–25-mm diameter SEMS are associated with a migration rate of only 3% (10). However, several prospective studies have revealed a major complication rate of > 20% and mortality rate of > 6% (8,9,11,12). Several newly-developed SEMS have antimigration features that take both efficacy and safety into consideration. These SEMS are of 2 types: SEMS with additional components and SEMS with modified shapes. The former includes those with a double layer (Niti-S Double; Taewoong Medical, Gimpo, Korea) and a skidproof design (Hanarostent® Esophagus Skidproof; M.I. Tech, Pyeongtaek, Korea); the latter includes SEMS with a shouldered design. The Niti-S Double SEMS (Taewoong Medical) has an outer uncovered layer and an inner covered layer. Although this stent has a very low migration rate (only 2%–3%), it is much more difficult to remove under endoscopic and/or fluoroscopic guidance compared to conventional FCSEMS because its outer uncovered layer does not prevent tumor embedding (12,13). The skidproof SEMS, which has multiple skidproof flaps, has a migration rate of 15%, suggesting that the skidproof flaps are of only limited value for preventing migration (14). The efficacy and safety of the shouldered design for preventing migration is not very well documented in the literature. However, all available SEMS used in Korea for esophageal cancer have adopted this design, with the exception of a few intended for placement in the cervical esophagus. One SEMS with a double-stepped shoulder design (EGIS; S & G Biotech, Seongnam, Korea) is equipped with outer shoulders and relatively small inner shoulders. However, randomized controlled trials are needed to determine whether this stent has a lower migration rate than those with a conventional shoulder design.
Anti-reflux features
Placement of SEMS across the gastroesophageal junction leads to an increased risk of gastroesophageal reflux because the stent can bypass the lower esophageal sphincter. SEMS with antireflux features such as sleeves or valves have been developed to remedy this problem. These SEMS decrease transprosthetic reflux compared to those without antireflux features. Dua et al. (15) reported in their in vitro study that the proportion of daily esophageal acid exposure time was significantly less after placement of SEMS with antireflux sleeve than that without (1% vs. 49%; P = 0.03). Shim et al. (16) reported in their study that the proportion of time during which esophageal pH was < 4 was significantly less in patients who received a SEMS with antireflux valve, compared to those who received a conventional SEMS without antireflux valve (3% vs. 29%; P < 0.001). Laasch et al. (17) reported in their randomized controlled trial that reflux was seen in only 12% patients who received a SEMS with antireflux sleeve, compared to 96% patients who received a conventional SEMS. However, Blomberg et al. (18) reported no significant difference in health-related quality of life between patients who received a SEMS with an antireflux sleeve and those who received a conventional SEMS. Sabharwal et al. (19) reported no significant difference in reflux rate between SEMS with an antireflux sleeve and conventional SEMS used in conjunction with a high-dose proton pump inhibitor (14% vs. 8%; P = 0.650). Coron et al. (20) reported that SEMS with an antireflux valve was effective in preventing reflux, but at the cost of an increased likelihood of minor adverse events such as migration and/or obstruction of SEMS (55% vs. 18%; P = 0.020). On the basis of these results, the routine use of SEMS with antireflux features could not be recommended. However, previous studies were limited by small sample size and variability in antireflux features. Further studies are needed to determine if antireflux features could reduce the risk of gastroesophageal reflux.
Proximal vs. distal-release delivery systems
The majority of available SEMS use a distal-release delivery system. This type of delivery system deploys SEMS by proximally retracting the outer sheath relative to the inner pusher catheter. However, accurate positioning of the proximal end of a SEMS that is distally released may not be possible in certain situations. For example, when there is a need to deploy a SEMS at a more proximal region within the esophageal, the proximal end of SEMS ideally should be deployed above the stricture but below the cricopharyngeal region to avoid irritating the nerves that control the coughing response. Under such circumstances, a proximal-release delivery system that deploys SEMS by distally extending the outer sheath relative to the inner pusher catheter can aid in more accurate placement of the proximal portion of SEMS. However, this type of delivery system only is offered by a few manufacturers.
SEMS PLACEMENT PROCEDURE
SEMS can be placed under endoscopic and/or fluoroscopic guidance. The outcomes of these procedures are the same, regardless of which guidance method is used. Fluoroscopic SEMS placement is usually well-tolerated under local anesthesia, whereas endoscopic SEMS placement usually requires sedation. The authors are radiologists and typically perform SEMS placement under fluoroscopic guidance alone. There are a variety of guidewires and catheters available for SEMS placement. The authors routinely use the 0.035-inch stiff-angled hydrophilic guidewire (Radiofocus M; Terumo, Tokyo, Japan) and the 5.4-Fr multifunctional coil catheter (Song-Lim; S & G Biotech). Once the guidewire and the catheter have been negotiated through the stricture, a limited amount of diluted water-soluble contrast medium is injected through the catheter to delineate the stricture. The location and length of the stricture is radiopaque-marked on the patient's skin, and the catheter is removed with the guidewire left in place. The delivery system is advanced through the stricture over the guidewire, and SEMS is deployed under continuous fluoroscopic monitoring. Balloon dilation of the stricture before SEMS placement is generally discouraged to avoid perforation but can be useful to allow advancement of the delivery system through the stricture. It is important to “overstent” the stricture by at least 1 cm on each end to prevent tumor overgrowth. If the placed SEMS does not expand to at least half of its fully expanded diameter, balloon dilation of SEMS should be performed. After the procedure, patients are allowed oral intake of liquids within 24 hours. Because of the risk of food impaction, they should not be permitted any food until an upper gastrointestinal series after 1–3 days show full expansion of SEMS.
INDICATIONS
Palliative treatment for malignant esophageal strictures
In several randomized controlled trials, SEMS placement has been shown to provide superior efficacy to photodynamic therapy, laser therapy, and surgical bypass for the palliation of malignant esophageal strictures (21,22,23,24,25,26). Systematic review and meta-analysis studies have demonstrated a technical success rate of virtually 100% and improvements in dysphagia scores by at least 2 points within 1–2 days of the procedure in > 95% patients (3,27,28,29,30). Self-expandable plastic stents (SEPS) are similar to SEMS with regard to relief of dysphagia in the short term, but adverse events such as migration occur more often with SEPS (31), making SEMS preferable over SEPS for palliating malignant esophageal strictures. Brachytherapy has also been widely used for the palliation of malignant esophageal strictures. According to multicenter randomized control trials, this treatment provides a survival advantage and better quality of life than does SEMS placement for palliating malignant esophageal strictures (32,33). However, brachytherapy requires more time to relieve dysphagia than does SEMS placement (33). In addition, brachytherapy has several important limitations, including limited availability, technical difficulty, and the need for dedicated expertise.
Concomitant palliative treatment with SEMS and brachytherapy
Because brachytherapy usually takes 4–6 weeks to relieve dysphagia (34), concomitant palliative treatment with SEMS and brachytherapy has been proposed for palliating malignant esophageal strictures. Several studies have shown that this regimen provides quicker relieve of dysphagia, survival advantages, and possibly a better quality of life than SEMS placement alone (32,33,35,36). However, Shin et al. (35) reported a significantly higher risk of complications (i.e., migration, ERF, and bleeding) in patients who underwent concomitant palliative treatment with SEMS and brachytherapy than those who underwent SEMS placement alone (65% vs. 33%; P = 0.040). Several other investigators have also found a high risk of major complications (16%–35%), including bleeding and ERF, in patients who underwent concomitant palliative treatment with SEMS and brachytherapy (37,38,39,40). Park et al. (36) showed that the rate of ERF was significantly lower in patients who underwent SEMS removal within 6 weeks as compared to after 6 weeks of starting radiation therapy (6% vs. 30%; P = 0.030). However, randomized controlled trials are needed to confirm this finding.
SEMS placement as a bridge to surgery
In patients with stage IIA or IIB esophageal cancer (localized resectable disease), neoadjuvant chemotherapy or chemoradiotherapy before surgery is recommended (41). However, a substantial period of time is required to relieve dysphagia by neoadjuvant chemotherapy or chemoradiotherapy. SEMS placement has been increasingly used as a “bridging therapy” to surgery, improving dysphagia and allowing for oral nutrition during neoadjuvant therapy (29). However, according to recent studies, the use of SEMS placement as bridging therapy has a negative impact on oncological outcomes (42,43,44). Mariette et al. (43) reported in their cohort of 2,944 patients that those who underwent SEMS placement as bridging therapy had a lower median time to recurrence (7 vs. 9 months; P = 0.040) and a lower 3-year overall survival rate (25% vs. 44%; P = 0.023). The following reasons have been suggested in an attempt to explain the negative outcomes associated with SEMS placement as a bridge therapy: First, mechanical injury caused by SEMS results in fibrosis that compromises the resectability of the tumor; Second, SEMS placement increases the levels of circulating neoplastic cells; Third chemotherapy increases the incidence of SEMS-related complications, such as migration and ERF; and Fourth, accurate restaging of the tumor after SEMS placement is technically difficult (45,46,47). Therefore, some investigators argue that the placement of a feeding tube or percutaneous gastrostomy may be preferable over SEMS placement as a bridging therapy (48,49). It should be noted, however, that in the study of Mariette et al. (43), SEMS was not removed until just before surgery; this factor may be the main reason for the negative outcomes. Several authors have reported that SEMS removal 4–6 weeks after starting neoadjuvant chemotherapy or chemoradiotherapy seems to decrease fibrosis and SEMS-related complications (35,36,50). However, randomized controlled trials are needed to confirm this result.
Palliative treatment for malignant ERF
ERF (i.e., tracheoesophageal and bronchoesophageal fistula) are common complications of esophageal cancer, with incidence rates of 5%–26% (51,52,53). This condition is caused by direct tumor invasion or as an adverse event of cancer therapies and can lead to malnutrition and respiratory failure. Therefore, prompt palliative treatment to seal off the fistula is considered a key priority in patients with this condition. Several studies have shown that covered SEMS are highly efficacious in their ability to seal off fistulas, with a success rate of 67%–100% (51,54,55,56,57,58,59,60,61,62,63,64,65,66,67). In addition, some studies report that patients with fistulas experience improved quality of life after covered SEMS placement (63,64). However, in some cases in which covered SEMS placement in the esophagus alone cannot not seal off the fistula, covered SEMS placement in both the esophagus and airway may be required (68). The clinical outcomes of SEMS placement for malignant ERF in the literature are summarized in Table 2.
Table 2. Clinical outcomes of SEMS placement for malignant ERF in the literature.
| Author (reference) | Year | Country | No. of patients | Mean age, yr | Sex (M/F) | SEMS type | SEMS placement location | Treatment success | Complications | Median survival, day | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Esophagus | Airway | Both | Major | Minor | |||||||||
| Saxon et al. (54) | 1995 | USA | 12 | 61.0 | 9/3 | FC | 12 (100.0) | 0 | 0 | 8 (66.7) | 3 (16.0) | 0 | 117.0 |
| Morgan et al. (55) | 1997 | England | 20 | 60.3 | 12/8 | - | 20 (100.0) | 0 | 0 | 18 (90.0) | - | - | 65.3 |
| Low et al. (56) | 1998 | USA | 12 | 59.8 | 7/5 | FC | 12 (100.0) | 0 | 0 | 11 (91.7) | - | - | 93.0 |
| May and Ell (57) | 1998 | Germany | 11 | 58.0 | 10/1 | FC | 11 (100.0) | 0 | 0 | 10 (90.9) | 0 | 6 (54.5) | 121.0 |
| Siersema et al. (58) | 2001 | Netherlands | 16 | 66.4 | 12/4 | FC, PC | 16 (100.0) | 0 | 0 | 14 (87.5) | 4 (25.0) | 5 (31.3) | 58.0 |
| Wang et al. (59) | 2001 | USA | 33 | - | - | - | 33 (100.0) | 0 | 0 | 31 (93.9) | - | - | 134.0 |
| Sarper et al. (60) | 2003 | Turkey | 14 | - | - | PC | 14 (100.0) | 0 | 0 | 12 (85.7) | 0 | 0 | 49.0 |
| Shin et al. (51) | 2004 | Korea | 61 | 59.3 | 58/3 | FC | 55 (90.2) | 5 (8.2) | 1 (1.6) | 49 (80.3) | 14 (23.0) | 12 (19.7) | 94.0 |
| Murthy et al. (61) | 2007 | USA | 12 | 64.0 | 9/3 | FC, PC | 5 (41.7) | 4 (33.3) | 3 (25.0) | 12 (100.0) | 1 (8.3) | 0 | - |
| Ross et al. (62) | 2007 | USA | 21 | - | - | FC | 21 (100.0) | 0 | 0 | 19 (90.5) | - | - | 72.0 |
| Hu (63) | 2009 | China | 17 | 56.8 | 15/2 | FC | 17 (100.0) | 0 | 0 | 16 (94.1) | 2 (11.8) | 6 (35.3) | 93.0 |
| Herth et al. (64) | 2010 | Germany | 112 | 54.3 | 98/14 | PC | 37 (33.0) | 65 (58.0) | 10 (8.9) | 112 (100.0) | 7 (6.3) | 0 | 261.0 |
| Van Heel et al. (65) | 2010 | Netherlands | 15 | - | - | FC, PC | 15 (100.0) | 0 | 0 | 14 (93.3) | 5 (33.3) | 0 | 73.0 |
| Chen et al. (66) | 2012 | China | 30 | 51.2 | - | PC | 25 (83.3) | 0 | 5 (16.7) | 26 (86.7) | 0 | 14 (46.7) | 125.0 |
| Zori et al. (67) | 2014 | USA | 10 | - | - | FC | 6 (60.0) | 1 (10.0) | 3 (30.0) | 7 (70.0) | - | - | - |
| Total | - | - | 396 | 57.2 | 230/43 | - | 299 (75.5) | 75 (18.9) | 22 (5.6) | 359 (90.7) | 36 (12.0) | 43 (14.3) | 144.6 |
SEMS = self-expanding metallic stents, ERF = esophagorespiratory fistula, FC = fully covered, PC = partially covered.
CONTRAINDICATIONS
In the early days of SEMS placement, several conditions were considered to be contraindications, including cervical esophageal strictures < 2 cm from the upper esophageal sphincter and malignant esophageal strictures lacking a proximal “shelf” to prevent migration (69,70). However, advancements in SEMS have made a great contribution to the management of malignant esophageal strictures in patients for whom treatment has traditionally proved technically difficult (71). Currently, there is no consensus on absolute contraindications for SEMS placement, but careful patient selection is important. SEMS placement is commonly considered contraindicated in terminally ill patients with a life expectancy of < 4 weeks, distal obstruction, perforation, bowel ischemia, sepsis, or uncorrectable coagulopathy (72).
COMPLICATIONS
Complications of SEMS placement can be classified as early or delayed. Early complications occur immediately or within 2–4 weeks after SEMS placement and include foreign body sensation, pain, gastroesophageal reflux, migration, bleeding, and perforation. Prolonged chest pain has been reported in up to 14% cases after SEMS placement, and is more common in the cervical esophagus (53,73). For this reason, SEMS with small diameters have been developed for placement in the cervical esophagus (71). Small amounts of bleeding during and 1–2 days after SEMS placement occurs in 5% patients; however, major bleeding requiring intervention occurs in < 1% patients (53). Several studies reported that perforation during or soon after SEMS placement occurred in < 1% patients (27,53,74). Perforations appear to occur more frequently in patients who were previously treated with chemo and/or radiation therapy; “full-thickness” perforation, which requires surgical intervention, is very rare (74). Delayed complications are more common than early ones and are defined as complications that occur at least 2–4 weeks after SEMS placement, including migration, tumor ingrowth and overgrowth, food impaction, and ERF. Although early complications are decreasing because of recent advances in SEMS and delivery systems, delayed complications still occur in up to 65% patients, with a re-intervention rate as high as 50% (3). Among both early and delayed complications, migration is the most common complication, occurring at a rate of 7%–75% (27). Tumor ingrowth is very rare nowadays because of the widespread use of FCSEMS but can still occur if the covering membrane is degraded or detached from the stent (53). In contrast, tumor overgrowth is still a common delayed complication, occurring in about 5% patients following SEMS placement (53). Food impaction also occurs in about 5% patients (53). In contrast, only a few cases of SEMS-related ERF have been reported in the literature, suggesting that this delayed complication is very rare (75,76,77,78). Complications of SEMS placement can also be classified as major and minor. Major complications are life-threatening conditions such as ERF, bleeding, and perforation; minor complications are those that are not life-threatening, including migration, tumor ingrowth and overgrowth, and food impaction (3,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68).
FUTURE OF SEMS
Since the patients with incurable esophageal cancer have a very poor prognosis, the ideal palliative treatment for malignant esophageal strictures should provide rapid and durable relief of symptoms, result in few complications, require minimal hospital stay, and prolong survival. However, patients who underwent SEMS placement often failed to achieve long-term relief of symptoms due to stent malfunction and have to be admitted again for reintervention. In addition, palliation with SEMS only provides symptoms relief but does not prolong survival. Radioactive SEMS has recently been described to combine the advantages of SEMS placement (i.e., quicker relieve of dysphagia) and brachytherapy (i.e., survival advantage and better quality of life) (79,80,81). Zhu et al. (79) showed in their recent multicenter randomized control trial that placement of SEMS loaded with radioactive seeds could result in a modest prolongation of survival in patients with incurable esophageal cancer (177 vs. 147 days; P = 0.005). Several drug-eluting SEMSs are also under development and have shown the potential to inhibit tumor growth in animals (80,81,82).
SUMMARY
SEMS placement is a widely accepted method for treating malignant esophageal strictures and ERFs. A wide range of SEMS for esophageal cancer is available in Korea, and even more are available internationally. Knowledge of the advantages and disadvantages associated with different designs will aid physicians in selecting the optimal SEMS for a given condition. The outcomes of SEMS placement do not differ with respect to the guidance method used (endoscopic and/or fluoroscopic). Brachytherapy provides a survival advantage and a better quality of life than does SEMS placement for palliating malignant esophageal strictures but requires more time to relieve dysphagia. SEMS removal within 6 weeks of starting radiation therapy may decrease complications. If SEMS is not removed 4–6 weeks after starting neoadjuvant chemotherapy or chemoradiotherapy, it may have a negative impact on oncological outcomes. Radioactive and drug-eluting SEMSs may potentially be the future of palliative treatment for malignant esophageal strictures.
ACKNOWLEDGMENT
The authors thank Mr. Dong Ho Shin (Taewoong Medical, Gimpo, Korea), Mr. Seung Hwan Jegal (S & G Biotech, Seongnam, Korea), and Sung Yun (M.I. Tech, Pyeongtaek, Korea) for providing their high-quality stent pictures for this article.
Footnotes
Funding: This study was supported by a grant of the Korean Health Technology R & D Project, Ministry of Health and Welfare, Republic of Korea (Grant No. HI15C0484 to H.Y.S.).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Kim KY, Tsauo J, Song HY. Data curation: Kim KY, Tsauo J, Kim PH, Park JH. Formal analysis: Kim KY, Tsauo J.
References
- 1.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374–1403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 2.Sihvo EI, Luostarinen ME, Salo JA. Fate of patients with adenocarcinoma of the esophagus and the esophagogastric junction: a population-based analysis. Am J Gastroenterol. 2004;99:419–424. doi: 10.1111/j.1572-0241.2004.04094.x. [DOI] [PubMed] [Google Scholar]
- 3.Spaander MC, Baron TH, Siersema PD, Fuccio L, Schumacher B, Escorsell À, Garcia-Pagán JC, Dumonceau JM, Conio M, de Ceglie A, et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:939–948. doi: 10.1055/s-0042-114210. [DOI] [PubMed] [Google Scholar]
- 4.Hill JL, Norberg HP, Smith MD, Young JA, Reyes HM. Clinical technique and success of the esophageal stent to prevent corrosive strictures. J Pediatr Surg. 1976;11:443–450. doi: 10.1016/s0022-3468(76)80201-1. [DOI] [PubMed] [Google Scholar]
- 5.Varadarajulu S, Banerjee S, Barth B, Desilets D, Kaul V, Kethu S, Pedrosa M, Pfau P, Tokar J, Wang A, et al. Enteral stents. Gastrointest Endosc. 2011;74:455–464. doi: 10.1016/j.gie.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 6.Domschke W, Foerster EC, Matek W, Rödl W. Self-expanding mesh stent for esophageal cancer stenosis. Endoscopy. 1990;22:134–136. doi: 10.1055/s-2007-1012818. [DOI] [PubMed] [Google Scholar]
- 7.Seven G, Irani S, Ross AS, Gan SI, Gluck M, Low D, Kozarek RA. Partially versus fully covered self-expanding metal stents for benign and malignant esophageal conditions: a single center experience. Surg Endosc. 2013;27:2185–2192. doi: 10.1007/s00464-012-2738-x. [DOI] [PubMed] [Google Scholar]
- 8.Uitdehaag MJ, Siersema PD, Spaander MC, Vleggaar FP, Verschuur EM, Steyerberg EW, Kuipers EJ. A new fully covered stent with antimigration properties for the palliation of malignant dysphagia: a prospective cohort study. Gastrointest Endosc. 2010;71:600–605. doi: 10.1016/j.gie.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 9.Uitdehaag MJ, van Hooft JE, Verschuur EM, Repici A, Steyerberg EW, Fockens P, Kuipers EJ, Siersema PD. A fully-covered stent (Alimaxx-E) for the palliation of malignant dysphagia: a prospective follow-up study. Gastrointest Endosc. 2009;70:1082–1089. doi: 10.1016/j.gie.2009.05.032. [DOI] [PubMed] [Google Scholar]
- 10.Verschuur EM, Steyerberg EW, Kuipers EJ, Siersema PD. Effect of stent size on complications and recurrent dysphagia in patients with esophageal or gastric cardia cancer. Gastrointest Endosc. 2007;65:592–601. doi: 10.1016/j.gie.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 11.Kozarek RA, Raltz S, Brugge WR, Schapiro RH, Waxman I, Boyce HW, Baillie J, Branch MS, Stevens PD, Lightdale CJ, et al. Prospective multicenter trial of esophageal Z-stent placement for malignant dysphagia and tracheoesophageal fistula. Gastrointest Endosc. 1996;44:562–567. doi: 10.1016/s0016-5107(96)70009-3. [DOI] [PubMed] [Google Scholar]
- 12.Verschuur EM, Repici A, Kuipers EJ, Steyerberg EW, Siersema PD. New design esophageal stents for the palliation of dysphagia from esophageal or gastric cardia cancer: a randomized trial. Am J Gastroenterol. 2008;103:304–312. doi: 10.1111/j.1572-0241.2007.01542.x. [DOI] [PubMed] [Google Scholar]
- 13.Verschuur EM, Homs MY, Steyerberg EW, Haringsma J, Wahab PJ, Kuipers EJ, Siersema PD. A new esophageal stent design (Niti-S stent) for the prevention of migration: a prospective study in 42 patients. Gastrointest Endosc. 2006;63:134–140. doi: 10.1016/j.gie.2005.07.051. [DOI] [PubMed] [Google Scholar]
- 14.Walter D, van den Berg MW, van Hooft JE, Boot H, Scheffer RC, Vleggaar FP, Siersema PD. A new fully covered metal stent with anti-migration features for the treatment of malignant dysphagia. Endoscopy. 2014;46:1101–1105. doi: 10.1055/s-0034-1377632. [DOI] [PubMed] [Google Scholar]
- 15.Dua KS, Kozarek R, Kim J, Evans J, Medda BK, Lang I, Hogan WJ, Shaker R. Self-expanding metal esophageal stent with anti-reflux mechanism. Gastrointest Endosc. 2001;53:603–613. doi: 10.1067/mge.2001.114054. [DOI] [PubMed] [Google Scholar]
- 16.Shim CS, Jung IS, Cheon YK, Ryu CB, Hong SJ, Kim JO, Cho JY, Lee JS, Lee MS, Kim BS. Management of malignant stricture of the esophagogastric junction with a newly designed self-expanding metal stent with an antireflux mechanism. Endoscopy. 2005;37:335–339. doi: 10.1055/s-2005-861113. [DOI] [PubMed] [Google Scholar]
- 17.Laasch HU, Marriott A, Wilbraham L, Tunnah S, England RE, Martin DF. Effectiveness of open versus antireflux stents for palliation of distal esophageal carcinoma and prevention of symptomatic gastroesophageal reflux. Radiology. 2002;225:359–365. doi: 10.1148/radiol.2252011763. [DOI] [PubMed] [Google Scholar]
- 18.Blomberg J, Wenger U, Lagergren J, Arnelo U, Agustsson T, Johnsson E, Toth E, Lagergren P. Antireflux stent versus conventional stent in the palliation of distal esophageal cancer. A randomized, multicenter clinical trial. Scand J Gastroenterol. 2010;45:208–216. doi: 10.3109/00365520903443860. [DOI] [PubMed] [Google Scholar]
- 19.Sabharwal T, Gulati MS, Fotiadis N, Dourado R, Botha A, Mason R, Adam A. Randomised comparison of the FerX Ella antireflux stent and the ultraflex stent: proton pump inhibitor combination for prevention of post-stent reflux in patients with esophageal carcinoma involving the esophago-gastric junction. J Gastroenterol Hepatol. 2008;23:723–728. doi: 10.1111/j.1440-1746.2008.05396.x. [DOI] [PubMed] [Google Scholar]
- 20.Coron E, David G, Lecleire S, Jacques J, Le Sidaner A, Barrioz T, Coumaros D, Volteau C, Vedrenne B, Bichard P, et al. Antireflux versus conventional self-expanding metallic stents (SEMS) for distal esophageal cancer: results of a multicenter randomized trial. Endosc Int Open. 2016;4:E730–6. doi: 10.1055/s-0042-106960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adam A, Ellul J, Watkinson AF, Tan BS, Morgan RA, Saunders MP, Mason RC. Palliation of inoperable esophageal carcinoma: a prospective randomized trial of laser therapy and stent placement. Radiology. 1997;202:344–348. doi: 10.1148/radiology.202.2.9015054. [DOI] [PubMed] [Google Scholar]
- 22.Alderson D, Wright PD. Laser recanalization versus endoscopic intubation in the palliation of malignant dysphagia. Br J Surg. 1990;77:1151–1153. doi: 10.1002/bjs.1800771023. [DOI] [PubMed] [Google Scholar]
- 23.Aoki T, Osaka Y, Takagi Y, Okada R, Shinohara M, Tsuchida A, Sato S, Koyanagi Y. Comparative study of self-expandable metallic stent and bypass surgery for inoperable esophageal cancer. Dis Esophagus. 2001;14:208–211. doi: 10.1046/j.1442-2050.2001.00186.x. [DOI] [PubMed] [Google Scholar]
- 24.Carter R, Smith JS, Anderson JR. Laser recanalization versus endoscopic intubation in the palliation of malignant dysphagia: a randomized prospective study. Br J Surg. 1992;79:1167–1170. doi: 10.1002/bjs.1800791120. [DOI] [PubMed] [Google Scholar]
- 25.Dallal HJ, Smith GD, Grieve DC, Ghosh S, Penman ID, Palmer KR. A randomized trial of thermal ablative therapy versus expandable metal stents in the palliative treatment of patients with esophageal carcinoma. Gastrointest Endosc. 2001;54:549–557. doi: 10.1067/mge.2001.118947. [DOI] [PubMed] [Google Scholar]
- 26.Fuchs KH, Freys SM, Schaube H, Eckstein AK, Selch A, Hamelmann H. Randomized comparison of endoscopic palliation of malignant esophageal stenoses. Surg Endosc. 1991;5:63–67. doi: 10.1007/BF00316838. [DOI] [PubMed] [Google Scholar]
- 27.Sharma P, Kozarek R, Practice Parameters Committee of American College of Gastroenterology Role of esophageal stents in benign and malignant diseases. Am J Gastroenterol. 2010;105:258–273. doi: 10.1038/ajg.2009.684. [DOI] [PubMed] [Google Scholar]
- 28.Hindy P, Hong J, Lam-Tsai Y, Gress F. A comprehensive review of esophageal stents. Gastroenterol Hepatol (N Y) 2012;8:526–534. [PMC free article] [PubMed] [Google Scholar]
- 29.Nagaraja V, Cox MR, Eslick GD. Safety and efficacy of esophageal stents preceding or during neoadjuvant chemotherapy for esophageal cancer: a systematic review and meta-analysis. J Gastrointest Oncol. 2014;5:119–126. doi: 10.3978/j.issn.2078-6891.2014.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hussain Z, Diamantopoulos A, Krokidis M, Katsanos K. Double-layered covered stent for the treatment of malignant oesophageal obstructions: systematic review and meta-analysis. World J Gastroenterol. 2016;22:7841–7850. doi: 10.3748/wjg.v22.i34.7841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Conio M, Repici A, Battaglia G, De Pretis G, Ghezzo L, Bittinger M, Messmann H, Demarquay JF, Blanchi S, Togni M, et al. A randomized prospective comparison of self-expandable plastic stents and partially covered self-expandable metal stents in the palliation of malignant esophageal dysphagia. Am J Gastroenterol. 2007;102:2667–2677. doi: 10.1111/j.1572-0241.2007.01565.x. [DOI] [PubMed] [Google Scholar]
- 32.Bergquist H, Wenger U, Johnsson E, Nyman J, Ejnell H, Hammerlid E, Lundell L, Ruth M. Stent insertion or endoluminal brachytherapy as palliation of patients with advanced cancer of the esophagus and gastroesophageal junction. Results of a randomized, controlled clinical trial. Dis Esophagus. 2005;18:131–139. doi: 10.1111/j.1442-2050.2005.00467.x. [DOI] [PubMed] [Google Scholar]
- 33.Homs MY, Steyerberg EW, Eijkenboom WM, Tilanus HW, Stalpers LJ, Bartelsman JF, van Lanschot JJ, Wijrdeman HK, Mulder CJ, Reinders JG, et al. Single-dose brachytherapy versus metal stent placement for the palliation of dysphagia from oesophageal cancer: multicentre randomised trial. Lancet. 2004;364:1497–1504. doi: 10.1016/S0140-6736(04)17272-3. [DOI] [PubMed] [Google Scholar]
- 34.Welsch J, Kup PG, Nieder C, Khosrawipour V, Bühler H, Adamietz IA, Fakhrian K. Survival and symptom relief after palliative radiotherapy for esophageal cancer. J Cancer. 2016;7:125–130. doi: 10.7150/jca.13655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shin JH, Song HY, Kim JH, Kim SB, Lee GH, Park SI, Han YM, Kang W. Comparison of temporary and permanent stent placement with concurrent radiation therapy in patients with esophageal carcinoma. J Vasc Interv Radiol. 2005;16:67–74. doi: 10.1097/01.rvi.0000142585.90055.74. [DOI] [PubMed] [Google Scholar]
- 36.Park JH, Song HY, Park JY, Kim JH, Kim YH, Kim JH, Kim SB. Temporary stent placement with concurrent chemoradiation therapy in patients with unresectable oesophageal carcinoma: is there an optimal time for stent removal? Eur Radiol. 2013;23:1940–1945. doi: 10.1007/s00330-013-2786-1. [DOI] [PubMed] [Google Scholar]
- 37.Javed A, Pal S, Dash NR, Ahuja V, Mohanti BK, Vishnubhatla S, Sahni P, Chattopadhyay TK. Palliative stenting with or without radiotherapy for inoperable esophageal carcinoma: a randomized trial. J Gastrointest Cancer. 2012;43:63–69. doi: 10.1007/s12029-010-9206-4. [DOI] [PubMed] [Google Scholar]
- 38.Langer FB, Schoppmann SF, Prager G, Tomaselli F, Pluschnig U, Hejna M, Schmid R, Zacherl J. Temporary placement of self-expanding oesophageal stents as bridging for neo-adjuvant therapy. Ann Surg Oncol. 2010;17:470–475. doi: 10.1245/s10434-009-0760-6. [DOI] [PubMed] [Google Scholar]
- 39.Nishimura Y, Nagata K, Katano S, Hirota S, Nakamura K, Higuchi F, Soejima T, Sai H, Japanese Society for Esophageal Diseases Severe complications in advanced esophageal cancer treated with radiotherapy after intubation of esophageal stents: a questionnaire survey of the Japanese Society for Esophageal Diseases. Int J Radiat Oncol Biol Phys. 2003;56:1327–1332. doi: 10.1016/s0360-3016(03)00198-6. [DOI] [PubMed] [Google Scholar]
- 40.Zhong J, Wu Y, Xu Z, Liu X, Xu B, Zhai Z. Treatment of medium and late stage esophageal carcinoma with combined endoscopic metal stenting and radiotherapy. Chin Med J (Engl) 2003;116:24–28. [PubMed] [Google Scholar]
- 41.Walsh TN. Oesophageal cancer: who needs neoadjuvant therapy? Lancet Oncol. 2011;12:615–616. doi: 10.1016/S1470-2045(11)70158-9. [DOI] [PubMed] [Google Scholar]
- 42.Vleggaar FP. Stent placement in esophageal cancer as a bridge to surgery. Gastrointest Endosc. 2009;70:620–622. doi: 10.1016/j.gie.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 43.Mariette C, Gronnier C, Duhamel A, Mabrut JY, Bail JP, Carrere N, Lefevre JH, Meunier B, Collet D, Piessen G, et al. Self-expanding covered metallic stent as a bridge to surgery in esophageal cancer: impact on oncologic outcomes. J Am Coll Surg. 2015;220:287–296. doi: 10.1016/j.jamcollsurg.2014.11.028. [DOI] [PubMed] [Google Scholar]
- 44.Kjaer DW, Nassar M, Jensen LS, Svendsen LB, Mortensen FV. A bridging stent to surgery in patients with esophageal and gastroesophageal junction cancer has a dramatic negative impact on patient survival: a retrospective cohort study through data acquired from a prospectively maintained national database. Dis Esophagus. 2017;30:1–7. doi: 10.1111/dote.12474. [DOI] [PubMed] [Google Scholar]
- 45.Hirdes MM, Vleggaar FP, de Beule M, Siersema PD. In vitro evaluation of the radial and axial force of self-expanding esophageal stents. Endoscopy. 2013;45:997–1005. doi: 10.1055/s-0033-1344985. [DOI] [PubMed] [Google Scholar]
- 46.Maruthachalam K, Lash GE, Shenton BK, Horgan AF. Tumour cell dissemination following endoscopic stent insertion. Br J Surg. 2007;94:1151–1154. doi: 10.1002/bjs.5790. [DOI] [PubMed] [Google Scholar]
- 47.Lecleire S, Di Fiore F, Ben-Soussan E, Antonietti M, Hellot MF, Paillot B, Lerebours E, Ducrotté P, Michel P. Prior chemoradiotherapy is associated with a higher life-threatening complication rate after palliative insertion of metal stents in patients with oesophageal cancer. Aliment Pharmacol Ther. 2006;23:1693–1702. doi: 10.1111/j.1365-2036.2006.02946.x. [DOI] [PubMed] [Google Scholar]
- 48.Löser C, Aschl G, Hébuterne X, Mathus-Vliegen EM, Muscaritoli M, Niv Y, Rollins H, Singer P, Skelly RH. ESPEN guidelines on artificial enteral nutrition--percutaneous endoscopic gastrostomy (PEG) Clin Nutr. 2005;24:848–861. doi: 10.1016/j.clnu.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 49.Toussaint E, Van Gossum A, Ballarin A, Arvanitakis M. Enteral access in adults. Clin Nutr. 2015;34:350–358. doi: 10.1016/j.clnu.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 50.Park JH, Song HY, Shin JH, Kim JH, Kim YH, Kim SB, Kim JH. Preliminary results of temporary placement of retrievable expandable metallic stents during preoperative neoadjuvant chemoradiotherapy in patients with resectable esophageal cancer. J Vasc Interv Radiol. 2015;26:883–888. doi: 10.1016/j.jvir.2014.12.622. [DOI] [PubMed] [Google Scholar]
- 51.Shin JH, Song HY, Ko GY, Lim JO, Yoon HK, Sung KB. Esophagorespiratory fistula: long-term results of palliative treatment with covered expandable metallic stents in 61 patients. Radiology. 2004;232:252–259. doi: 10.1148/radiol.2321030733. [DOI] [PubMed] [Google Scholar]
- 52.Balazs A, Kupcsulik PK, Galambos Z. Esophagorespiratory fistulas of tumorous origin. Non-operative management of 264 cases in a 20-year period. Eur J Cardiothorac Surg. 2008;34:1103–1107. doi: 10.1016/j.ejcts.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 53.Na HK, Song HY, Kim JH, Park JH, Kang MK, Lee J, Oh SJ. How to design the optimal self-expandable oesophageal metallic stents: 22 years of experience in 645 patients with malignant strictures. Eur Radiol. 2013;23:786–796. doi: 10.1007/s00330-012-2661-5. [DOI] [PubMed] [Google Scholar]
- 54.Saxon RR, Barton RE, Katon RM, Lakin PC, Timmermans HA, Uchida BT, Keller FS, Rösch J. Treatment of malignant esophagorespiratory fistulas with silicone-covered metallic Z stents. J Vasc Interv Radiol. 1995;6:237–242. doi: 10.1016/s1051-0443(95)71104-6. [DOI] [PubMed] [Google Scholar]
- 55.Morgan RA, Ellul JP, Denton ER, Glynos M, Mason RC, Adam A. Malignant esophageal fistulas and perforations: management with plastic-covered metallic endoprostheses. Radiology. 1997;204:527–532. doi: 10.1148/radiology.204.2.9240548. [DOI] [PubMed] [Google Scholar]
- 56.Low DE, Kozarek RA. Comparison of conventional and wire mesh expandable prostheses and surgical bypass in patients with malignant esophagorespiratory fistulas. Ann Thorac Surg. 1998;65:919–923. doi: 10.1016/s0003-4975(98)00081-2. [DOI] [PubMed] [Google Scholar]
- 57.May A, Ell C. Palliative treatment of malignant esophagorespiratory fistulas with Gianturco-Z stents. A prospective clinical trial and review of the literature on covered metal stents. Am J Gastroenterol. 1998;93:532–535. doi: 10.1111/j.1572-0241.1998.160_b.x. [DOI] [PubMed] [Google Scholar]
- 58.Siersema PD, Schrauwen SL, van Blankenstein M, Steyerberg EW, van der Gaast A, Tilanus HW, Dees J, Rotterdam Esophageal Tumor Study Group Self-expanding metal stents for complicated and recurrent esophagogastric cancer. Gastrointest Endosc. 2001;54:579–586. doi: 10.1067/mge.2001.118716. [DOI] [PubMed] [Google Scholar]
- 59.Wang MQ, Sze DY, Wang ZP, Wang ZQ, Gao YA, Dake MD. Delayed complications after esophageal stent placement for treatment of malignant esophageal obstructions and esophagorespiratory fistulas. J Vasc Interv Radiol. 2001;12:465–474. doi: 10.1016/s1051-0443(07)61886-7. [DOI] [PubMed] [Google Scholar]
- 60.Sarper A, Oz N, Cihangir C, Demircan A, Isin E. The efficacy of self-expanding metal stents for palliation of malignant esophageal strictures and fistulas. Eur J Cardiothorac Surg. 2003;23:794–798. doi: 10.1016/s1010-7940(03)00091-5. [DOI] [PubMed] [Google Scholar]
- 61.Murthy S, Gonzalez-Stawinski GV, Rozas MS, Gildea TR, Dumot JA. Palliation of malignant aerodigestive fistulae with self-expanding metallic stents. Dis Esophagus. 2007;20:386–389. doi: 10.1111/j.1442-2050.2007.00689.x. [DOI] [PubMed] [Google Scholar]
- 62.Ross WA, Alkassab F, Lynch PM, Ayers GD, Ajani J, Lee JH, Bismar M. Evolving role of self-expanding metal stents in the treatment of malignant dysphagia and fistulas. Gastrointest Endosc. 2007;65:70–76. doi: 10.1016/j.gie.2006.04.040. [DOI] [PubMed] [Google Scholar]
- 63.Hu Y, Zhao YF, Chen LQ, Zhu ZJ, Liu LX, Wang Y, Kou YL. Comparative study of different treatments for malignant tracheoesophageal/bronchoesophageal fistulae. Dis Esophagus. 2009;22:526–531. doi: 10.1111/j.1442-2050.2009.00950.x. [DOI] [PubMed] [Google Scholar]
- 64.Herth FJ, Peter S, Baty F, Eberhardt R, Leuppi JD, Chhajed PN. Combined airway and oesophageal stenting in malignant airway-oesophageal fistulas: a prospective study. Eur Respir J. 2010;36:1370–1374. doi: 10.1183/09031936.00049809. [DOI] [PubMed] [Google Scholar]
- 65.Van Heel NC, Haringsma J, Spaander MC, Didden P, Bruno MJ, Kuipers EJ. Esophageal stents for the palliation of malignant dysphagia and fistula recurrence after esophagectomy. Gastrointest Endosc. 2010;72:249–254. doi: 10.1016/j.gie.2010.01.070. [DOI] [PubMed] [Google Scholar]
- 66.Chen YH, Li SH, Chiu YC, Lu HI, Huang CH, Rau KM, Liu CT. Comparative study of esophageal stent and feeding gastrostomy/jejunostomy for tracheoesophageal fistula caused by esophageal squamous cell carcinoma. PLoS One. 2012;7:e42766. doi: 10.1371/journal.pone.0042766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zori AG, Jantz MA, Forsmark CE, Wagh MS. Simultaneous dual scope endotherapy of esophago-airway fistulas and obstructions. Dis Esophagus. 2014;27:428–434. doi: 10.1111/dote.12120. [DOI] [PubMed] [Google Scholar]
- 68.Shin JH, Kim JH, Song HY. Interventional management of esophagorespiratory fistula. Korean J Radiol. 2010;11:133–140. doi: 10.3348/kjr.2010.11.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Verschuur EM, Kuipers EJ, Siersema PD. Esophageal stents for malignant strictures close to the upper esophageal sphincter. Gastrointest Endosc. 2007;66:1082–1090. doi: 10.1016/j.gie.2007.03.1087. [DOI] [PubMed] [Google Scholar]
- 70.Katsanos K, Sabharwal T, Adam A. Stenting of the upper gastrointestinal tract: current status. Cardiovasc Intervent Radiol. 2010;33:690–705. doi: 10.1007/s00270-010-9862-6. [DOI] [PubMed] [Google Scholar]
- 71.Conigliaro R, Battaglia G, Repici A, De Pretis G, Ghezzo L, Bittinger M, Messmann H, Demarquay JF, Togni M, Blanchi S, et al. Polyflex stents for malignant oesophageal and oesophagogastric stricture: a prospective, multicentric study. Eur J Gastroenterol Hepatol. 2007;19:195–203. doi: 10.1097/MEG.0b013e328013a418. [DOI] [PubMed] [Google Scholar]
- 72.Yakami M, Mitsumori M, Sai H, Nagata Y, Hiraoka M, Nishimura Y. Development of severe complications caused by stent placement followed by definitive radiation therapy for T4 esophageal cancer. Int J Clin Oncol. 2003;8:395–398. doi: 10.1007/s10147-003-0356-2. [DOI] [PubMed] [Google Scholar]
- 73.Schowengerdt CG. Tracheoesophageal fistula caused by a self-expanding esophageal stent. Ann Thorac Surg. 1999;67:830–831. doi: 10.1016/s0003-4975(98)01341-1. [DOI] [PubMed] [Google Scholar]
- 74.Nagahama T, Maruyama M, Kato K, Shinoura H, Hasegawa K, Takashima I, Ebuchi M. Complication after self expandable metallic stent for esophageal cancer. Gan To Kagaku Ryoho. 2003;30:1750–1753. [PubMed] [Google Scholar]
- 75.Saito Y, Tanaka T, Andoh A, Minematsu H, Hata K, Tsujikawa T, Nitta N, Murata K, Fujiyama Y. Novel biodegradable stents for benign esophageal strictures following endoscopic submucosal dissection. Dig Dis Sci. 2008;53:330–333. doi: 10.1007/s10620-007-9873-6. [DOI] [PubMed] [Google Scholar]
- 76.Jung GE, Sauer P, Schaible A. Tracheoesophageal fistula following implantation of a biodegradable stent for a refractory benign esophageal stricture. Endoscopy. 2010;42(Suppl 2):E338–9. doi: 10.1055/s-0030-1256005. [DOI] [PubMed] [Google Scholar]
- 77.Guo JH, Teng GJ, Zhu GY, He SC, Deng G, He J. Self-expandable stent loaded with 125I seeds: feasibility and safety in a rabbit model. Eur J Radiol. 2007;61:356–361. doi: 10.1016/j.ejrad.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 78.Guo JH, Teng GJ, Zhu GY, He SC, Fang W, Deng G, Li GZ. Self-expandable esophageal stent loaded with 125I seeds: initial experience in patients with advanced esophageal cancer. Radiology. 2008;247:574–581. doi: 10.1148/radiol.2472070999. [DOI] [PubMed] [Google Scholar]
- 79.Zhu HD, Guo JH, Mao AW, Lv WF, Ji JS, Wang WH, Lv B, Yang RM, Wu W, Ni CF, et al. Conventional stents versus stents loaded with (125)iodine seeds for the treatment of unresectable oesophageal cancer: a multicentre, randomised phase 3 trial. Lancet Oncol. 2014;15:612–619. doi: 10.1016/S1470-2045(14)70131-7. [DOI] [PubMed] [Google Scholar]
- 80.Moon S, Yang SG, Na K. An acetylated polysaccharide-PTFE membrane-covered stent for the delivery of gemcitabine for treatment of gastrointestinal cancer and related stenosis. Biomaterials. 2011;32:3603–3610. doi: 10.1016/j.biomaterials.2011.01.070. [DOI] [PubMed] [Google Scholar]
- 81.Kim SY, Kim M, Kim MK, Lee H, Lee DK, Lee DH, Yang SG. Paclitaxel-eluting nanofiber-covered self-expanding nonvascular stent for palliative chemotherapy of gastrointestinal cancer and its related stenosis. Biomed Microdevices. 2014;16:897–904. doi: 10.1007/s10544-014-9894-9. [DOI] [PubMed] [Google Scholar]
- 82.Lei L, Liu X, Guo S, Tang M, Cheng L, Tian L. 5-Fluorouracil-loaded multilayered films for drug controlled releasing stent application: Drug release, microstructure, and ex vivo permeation behaviors. J Control Release. 2010;146:45–53. doi: 10.1016/j.jconrel.2010.05.017. [DOI] [PubMed] [Google Scholar]


