Abstract
This study aimed to assess whether night shift work is associated with the risk of depression by using a meta-analysis of observational studies. We searched PubMed and EMBASE in August, 2016 to locate eligible studies and investigated the association between night shift work and the risk of depression, reporting outcome measures with adjusted odds ratios (ORs) or relative risks (RRs) and 95% confidence intervals (CIs). In the meta-analysis of a total of 11 observational studies with 9 cross-sectional study, 1 longitudinal study, and 1 cohort study, night shift work was significantly associated with an increased risk of depression (OR/RR, 1.43; 95% CI, 1.24–1.64; I2 = 78.0%). Also, subgroup meta-analyses by gender, night shift work duration, type of occupation, continent, and type of publication showed that night shift work was consistently associated with the increased risk of depression. The current meta-analysis suggests that night shift work is associated with the increased risk of depression. However, further large prospective cohort studies are needed to confirm this association.
Keywords: Night Shift Work, Depression, Observational Study, Meta-analysis
Graphical Abstract
INTRODUCTION
Shift work refers to work schedules that extend beyond a typical 9-to-5 work day (1). The full spectrum of shift work includes regular evening or night schedules, rotating shifts, on-call, 24-hour shifts, and irregular schedules (2). According to the 5th European Working Conditions Survey, 17% of workers carry out shift work across the EU (3). Shift work is known to be associated with an increased risk of physical health problems of the workers such as metabolic syndrome, diabetes mellitus, cancer, and cardiovascular disease (4,5,6). Moreover, several observational studies have reported the association between night shift work and the risk of mental illnesses such as depression and anxiety (7,8,9,10,11,12,13,14,15,16,17). Among the mental illnesses, depression is considered a predictor of sickness absence and work disability among the working population (18). One of the possible mechanisms on the association between night shift work and depression is circadian rhythm, which is a fundamental mechanism of a large number of medical conditions such as adrenal insufficiency, nocturia, peptic ulcer diseases, and asthma (19). Circadian rhythm disorder could affect the imbalance of cortisol levels and accordingly cause depression (20).
However, other observational studies have reported that there was no significant association between night shift work and depression (21,22). So far, there is no meta-analysis on the association between them. The current study aimed to investigate the association between night shift work and the risk of depression by using a meta-analysis of observational epidemiological studies such as cross-sectional studies, case-control studies, and cohort studies.
MATERIALS AND METHODS
Literature search
We searched PubMed (1970 to August 2016) and EMBASE (1987 to August 2016) for eligible studies using common keywords related to night shift work and the risk of depression. The keywords for literature search were as follows: ‘shift work,’ ‘night shift,’ ‘night work,’ ‘work at night,’ ‘depressive disorder,’ ‘depression,’ and ‘major depressive disorder.’
Selection criteria
We included observational studies such as case-control studies, cross-sectional studies, and prospective or retrospective cohort studies that investigated the association between night shift work and the risk of depression, reporting outcome measures with adjusted odds ratios (ORs) or relative risks (RRs) and 95% confidence intervals (CIs). If data were duplicated or shared in more than one study, the first published study or most comprehensive study was included in the analysis. The language of publication was restricted to English.
Selection of relevant studies
Three of the authors (Aeyoung Lee, Yu-Jin Jung, and Seung-Kwon Myung) independently evaluated the eligibility of all studies retrieved from the databases based on the pre-determined selection criteria. Disagreements between evaluators were resolved by discussion. We extracted the following data from studies included in the final analysis: study name (along with the name of the first author and year of publication), type of study design, country, years enrolled, population (gender and age), screening tool for depression, adjusted OR/RR with 95% CI, and adjusted variables.
Main and subgroup analyses
We investigated the association between night shift work and the risk of depression by using adjusted OR/RR with 95% CI for the main analysis. Driesen's prospective cohort study (11) reported the results from both prospective analyses and retrospective analyses. In their study, the findings from the prospective analyses unusually showed a non-significantly opposite direction (a decreased risk of depression) to those (an increased risk of depression) from the remaining 9 studies included in the current study. Thus, for all the subgroup meta-analysis, we decided to use the retrospective data from Driesen's study, although we presented both results using either prospective or retrospective data from Driesen's study in the main analyses. We also performed subgroup analyses by gender, night shift work duration, type of occupation, continent, and type of publication.
Statistical analysis
To calculate a pooled OR/RR with 95% CI, we used an adjusted OR/RR and its 95% CI reported in individual articles whenever possible. We evaluated heterogeneity in results across studies using Higgins, which measures the percentage of total variation across studies (23). I2 was calculated as follows:
| I2 = 100% × (Q − df)/Q |
where Q is Cochran's heterogeneity statistic, and df is the degrees of freedom. Negative values of I2 are set at zero; I2 lies between 0% (no observed heterogeneity) and 100% (maximal heterogeneity). An I2 value greater than 50% was considered to indicate substantial heterogeneity. All the analyses were performed by using a random-effect model meta-analysis.
We also examined publication bias regarding the studies included in the final analysis using the Begg's funnel plot and Egger's test. If publication bias exists, the Begg's funnel plot is asymmetrical or the P value is less than 0.05 by the Egger's test. If there is a discrepancy in results between the funnel plot (asymmetrical) and Egger's test (P value ≥ 0.05), we preferred the results from Egger's test for the interpretation because the visual inspection of a funnel plot might be misleading (24). Statistical analyses were conducted using the Stata SE version 12.1 software package (StataCorp., College Station, TX, USA).
RESULTS
Identification of relevant studies
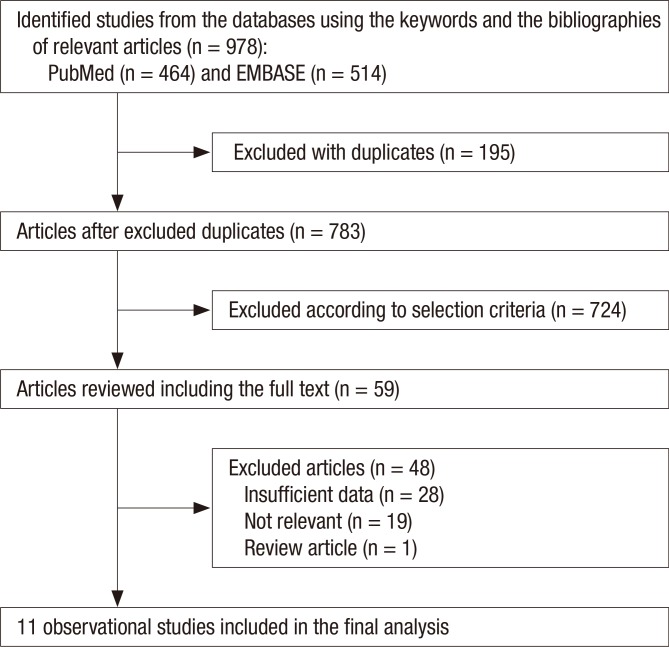
Fig. 1 shows a flow diagram of how we identified relevant studies. A total of 978 articles were identified by searching PubMed and EMBASE. We excluded 195 duplicated articles and an additional 724 articles that did not satisfy the selection criteria. The full texts of the remaining 59 articles were reviewed, and 48 additional articles were excluded for the reasons shown in Fig. 1. The remaining 11 articles were included in the final analysis.
Fig. 1.
Flow diagram of identification of relevant studies.
General characteristics of studies
We identified a total of 11 observational studies with 9 cross-sectional studies, 1 longitudinal study, and 1 cohort study. Table 1 shows the general characteristics of the studies in the final analysis. The included studies were performed in Korea (n = 5), United Kingdom (n = 1), The Netherlands (n = 1), Norway (n = 1), Sweden (n = 1), China (n = 1), and Brazil (n = 1). The age range of the study participants in 7 studies (7,8,9,10,13,16,17) was from 15 to 90 years, and the mean age in 4 studies (10,11,13,14) was from 25 to 39.76 years. The year of enrollment for participants across studies ranged between 1995 and 2009. Three studies (10,13,16) involved nursing workers such as nurses, nursing technicians, and nursing auxiliaries, and the remaining studies included other types of workers such as employees from various companies, white collar workers, physicians, and police officers. Screening tools for depression used in each study were Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition, Revised (DSM-III-R), Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV), General Health Questionnaire, Beck Depression Inventory (BDI), World Health Organization (WHO)'s health and work performance questionnaire, Hospital Anxiety and Depression Scale, Zung Self Rating Depression Scale, Patient Health Questionnaire-9 (PHQ-9), and WHO-5 wellbeing index.
Table 1. General characteristics of the studies included in the final analysis.
| Study (Reference No.) | Type of study | Country | Years enrolled | Population (gender, age) | Screening tool for depression: category of depression | OR/RR (95% CI) | Adjusted variables |
|---|---|---|---|---|---|---|---|
| Bildt and Michélsen (7) | Longitudinal study | Sweden | 1993 | 186 non-institutionalized individuals (women, 100%; 46–63 yr) | DSM-III-R: sub-clinical depression (at least 2 depressive symptoms at any time during the past year) | 2.40 (1.00–5.80) | Job strain and poor quality of social contacts |
| Ohayon and Hong (8) | Cross-sectional study | Korea | 2001 | 3,719 non-institutionalized individuals (women, 50.5%; 15–90 yr) | DSM-IV: major depressive disorders | 1.89 (0.99–3.61) | Gender, occupation, number of cigarettes per day, levels of stress, health status, number of medical consultations last year, physical activities, and BMI |
| Bara and Arber (9) | Cross-sectional study | United Kingdom | 1995–2005 | A household panel comprising 8,711 men and women (women, 54%; 21–73 yr) | GHQ: anxiety/depression | 3.12 (1.48–6.59) | Age, education, marital status, number of working in occupational categories, and anxiety/depression at baseline |
| de Vargas and Dias (10) | Cross-sectional study | Brazil | 2011 | 67 nursing workers (women, 55%; 21–30 yr) | BDI: depression (BDI score ≥ 20) | 1.46 (1.42–1.78) | Marital status and number of jobs |
| Driesen et al. (11) | Prospective cohort study | The Netherlands | 1998–2008 | 8,178 employees from various companies and organizations (women, 16%; 37.5 years for shift workers) | WHO's health and work performance questionnaire: depressive disorder | 1.33 (1.00–1.75)* | Age and education |
| Kim et al. (12) | Cross-sectional study | Korea | NA | 1,438 white collar workers in the public sector (NA, NA) | BDI: depressive symptoms (BDI score > 24) | 3.18 (1.43–7.09) | Gender, age, company type, employment type, satisfaction for income, smoking, and drinking |
| Øyane et al. (13) | Cross-sectional study | Norway | 2008–2009 | 2,035 nurses (women, 91%; 21–63 yr) | Hospital Anxiety and Depression Scale: depression (cut-off point ≥ 8) | 1.35 (0.75–2.42) | Age, gender, years of work experience, marital status, and children living at home |
| Gong et al. (14) | Cross-sectional study | China | 2009 | 2,646 physicians (women, 46%; mean 39.76 yr) | Zung Self Rating Depression Scale: depressive symptoms (score ≥ 53) | 1.40 (1.02–1.93) | Demographic variables, life styles, work-related characteristic, and self-perceived physical health |
| Lee et al. (15) | Cross-sectional study | Korea | NA | 7,476 police officers (NA, NA) | Depressive symptoms continuously lasting for more than 2 weeks within the last one year | 1.20 (1.02–1.41) | NA |
| Lee et al. (16) | Cross-sectional study | Korea | 2013 | 9,789 female nurses (women, 100%; < 29 yr [42.6%] and 30–39 yr [42.9%]) | PHQ-9: depressive symptoms | 1.52 (1.38–1.67) | Age, education, annual income, marital status, smoking, alcohol consumption, and BMI |
| Park et al. (17) | Cross-sectional study | Korea | 2011 | 50,032 employees (women, 41.8%; > 15 yr) | WHO-5 wellbeing index: depressive symptoms (a raw score ≤ 12) | 1.12 (1.04–1.20) | Gender, age, education, monthly income, smoking status, drinking frequency, self-rated health, weekly work hours, type of occupation, duration of career, working to tight deadlines, exposure to stress at work, and hazard exposure |
NA = not available, OR = odds ratio, RR = relative risk, CI = confidence interval, DSM-III-R = Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition, Revised, DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, GHQ = General Health Questionnaire, BMI = body mass index, BDI = Beck Depression Inventory, WHO = World Health Organization, PHQ-9 = Patient Health Questionnaire-9.
*The OR with 95% CI of Driesen et al's study (11) was calculated by combining the values for depressive disorder in men and women.
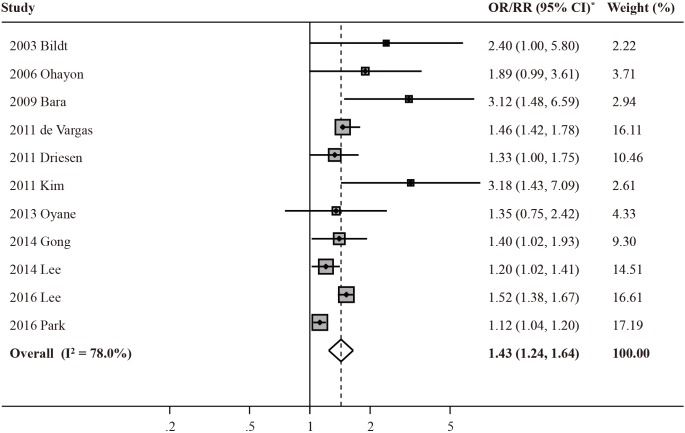
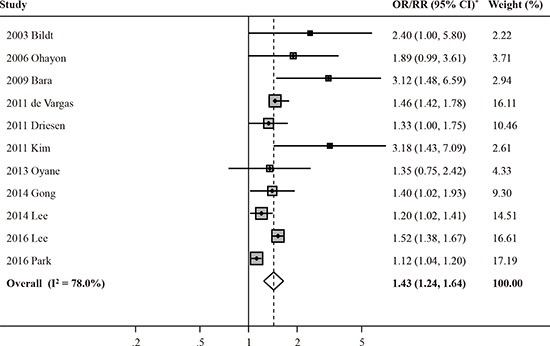
Night shift work and risk of depression
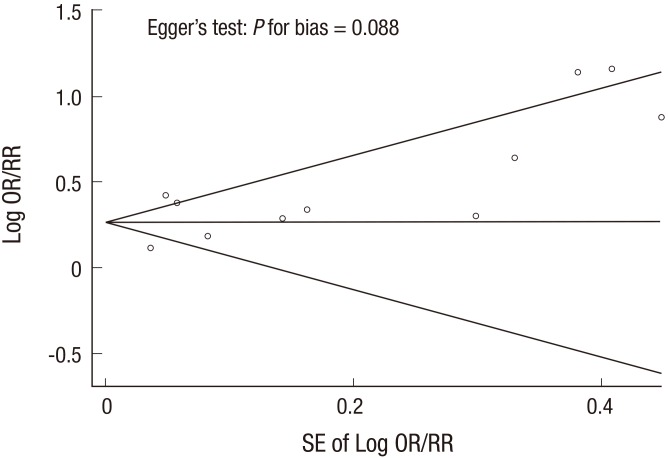
Fig. 2 shows the effect of night shift work on the risk of depression in the meta-analysis of all 11 studies. Night shift work was associated with an increased risk of depression in a random-effects model meta-analysis (OR/RR, 1.43; 95% CI, 1.24–1.64; I2 = 78.0%). P for bias from the Egger's test was 0.088 (Fig. 3), whereas Begg's funnel plot was asymmetric base on the visual inspection. Therefore, no publication bias was found.
Fig. 2.
Association between night shift work and the risk of depression in a random-effects model meta-analysis of observational studies (n = 11).
OR = odds ratio, RR = relative risk, CI = confidence interval.
*Random-Effects Model.
Fig. 3.
Begg's funnel plots and Egger's test for identifying publication bias in the meta-analysis of observational studies (n = 11).
OR = odds ratio, RR = relative risk, SE = standard error.
Subgroup meta-analyses
Table 2 summarizes the findings from the subgroup meta-analyses by gender, night shift work duration, type of occupation, continent, and type of publication. When using prospective data from Driesen's study (11), night shift work was consistently associated with an increased risk of depression (OR/RR, 1.37; 95% CI, 1.17–1.60; I2 = 84.8%). In the subgroup meta-analysis by gender, there was a significant association in women (OR/RR, 1.43; 95% CI, 1.16–1.76; I2 = 68.2%), but not in men (OR/RR, 1.42; 95% CI, 0.88–2.28; I2 = 79.4%). There was an increased trend of the risk of depression with an increased duration of night shift work. Also, the subgroup meta-analyses by type of occupation and continent consistently showed a positive association between night shift work and the risk of depression. In the subgroup meta-analysis by type of publication, no significant association was observed in 2 studies published in conference proceedings (i.e., poster presentation).
Table 2. Association between night shift work and the risk of depression in the subgroup meta-analyses by various factors* .
| Factor (Reference No.) | No. of studies | Summary OR/RR (95% CI) | Heterogeneity, I2 (%) |
|---|---|---|---|
| All (7,8,9,10,11,12,13,14,15,16,17)† | 11 | 1.43 (1.24–1.64) | 78.0 |
| All (7,8,9,10,11,12,13,14,15,16,17)† | 11 | 1.37 (1.17–1.60) | 83.7 |
| Gender | |||
| Men (9,11,17) | 3 | 1.42 (0.88–2.28) | 79.4 |
| Women (7,9,11,16,17) | 5 | 1.43 (1.16–1.76) | 68.2 |
| Night shift work duration, yr | |||
| 1 (9) | 1 | 1.23 (0.69–2.19) | NA |
| 2–3 (9) | 1 | 1.73 (0.95–3.17) | NA |
| 4–10 (9,13) | 2 | 1.99 (0.88–4.50) | 66.6 |
| Type of occupation | |||
| Nursing workers (10,13,16) | 3 | 1.49 (1.39–1.60) | 0 |
| Others (7,8,9,11,12,14,15,17) | 8 | 1.42 (1.18–1.71) | 66.4 |
| Continent | |||
| Europe: UK, The Netherlands, Norway, and Sweden (7,9,11,13) | 4 | 1.70 (1.15–2.51) | 46.7 |
| South America: Brazil (10) | 1 | 1.46 (1.42–1.78) | NA |
| Asia: Korea and China (8,12,14,15,16,17) | 6 | 1.38 (1.14–1.66) | 84.7 |
| Type of publication | |||
| Peer-reviewed journals (7,8,9,10,11,13,14,16,17) | 9 | 1.44 (1.23–1.68) | 79.9 |
| Conference proceedings (12,15) | 2 | 1.80 (0.70–4.61) | 81.7 |
NA = not applicable, OR = odds ratio, RR = relative risk, CI = confidence interval.
*In Driesen's study (11), the findings from the prospective analyses unusually showed a non-significantly opposite direction to those from the remaining 9 studies included in the current study. Thus, the retrospective data from Driesen's study were used in the subgroup meta-analyses by various factors; †Retrospective data from reference No. 11.
DISCUSSION
In this meta-analysis, we found that overall night shift work was associated with an increased risk of depression. Also, subgroup meta-analyses by gender, night shift work duration, type of occupation, continent, and type of publication showed that night shift work was consistently associated with the increased risk of depression.
There are several biological mechanisms that may explain a positive association between night shift work and the risk of depression observed in our meta-analysis. First, the effect of environmental stress on serotonin transporter gene (SLC6A4) promoter methylation would be one of the possible mechanisms. The protein encoded by SLC6A4 transports serotonin from synaptic spaces into pre-synaptic neurons and serves to regulate emotional aspects of behavior (25). A recent nurse cohort study showed significantly lower promoter methylation levels in the high stress group (26). The environmental stress might cause decreased methylation of the SLC6A4 promoter and decrease the amount of extracellular serotonin in the synaptic cleft and consequently increase a risk of functional disturbance such as depressive mood (26).
Second, the effect of night shift work on the increased risk of depression might be associated with disruption of circadian glucocorticoid oscillations. It has been reported that circadian glucocorticoid oscillations act to balance synapse formation and pruning after learning and during development (27). Chronic stress such as night shift disrupts this balance: it reduces the survival of newly formed synapses, while at the same time it increases the elimination of pre-existing synapses (27). Also, this disruption of glucocorticoid hormone interacts with signaling pathways in neurons and may contribute to the development of stress-related psychiatric disorders such as depression to vulnerable individuals (27). In the meantime, it is suggested that impaired corticosteroid receptor signaling is a key mechanism in the pathogenesis of depression based on the clinical and preclinical data (28).
To the best of our knowledge, this study is the first meta-analysis of observational studies on the association between night shift work and the risk of depression. Several observational epidemiological studies have reported this association. In 2010, a small cross-sectional study reported that night shift work was not correlated with depressive symptoms (29). Also, a relatively large cross-sectional study with 2,059 nurses indicated that night shift work was not associated with the risk of depression (13). Similarly, Driesen's prospective study indicated that depressed mood among shift workers non-significantly increased when adjusting for potential confounding factors, whereas retrospective analyses in their study found that former or current male shift workers had a statistically significant increased risk of depressed mood and depressive disorder (11). However, the remaining studies included in our analysis consistently revealed that night shift work was associated with the increased risk of depression (7,9,10,12,14,15,16,17). In the current meta-analysis, we were able to quantitatively suggest that night shift workers had an increased risk of depression by about 40%, compared with those without night shift.
Our study has several limitations. First, our study included a small number of observational studies to draw definite conclusions because of a paucity of data. Further larger prospective cohort studies are warranted to confirm our findings. Second, most of the included studies used self-reported assessment tools in order to screen depression or depressive symptoms. Thus, we were unable to evaluate whether night shift work increases the risk of depressive disorder clinically confirmed by physicians. Third, the included studies consisted of heterogeneous populations such as nursing workers, physicians, and other employees from various companies. Although we performed subgroup meta-analyses by type of occupation, we were unable to evaluate whether there are any differences in the effect of night shift work on the risk of depression according to type of occupation due to insufficient data. Last, we had a limitation to investigate the difference in findings between men and women. The subgroup meta-analysis in men showed there was no significant association between night shift work and the risk of depression. However, only 3 studies were included in this subgroup met-analysis because several studies included in this study did not separately present findings in each gender. Similarly, we were unable to confirm the association between the duration of night shift work and the risk of depression because of a paucity of data.
In summary, we found that night shift work was significantly associated with the increased risk of depression in the meta-analysis of observational epidemiological studies, even though there have been a small number of studies published so far to draw a confirmative relationship between them. Further well-conducted case-control studies and large prospective cohort studies are warranted to confirm the association between night shift work and the risk of depression.
Footnotes
Funding: This study was supported by a grant of the Korean Health Technology R & D Projects, Ministry of Health and Welfare, Republic of Korea (HI13C1461).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Myung SK, Cho JJ. Data curation: Lee A, Myung SK, Jung YJ. Formal analysis: Lee A, Myung SK. Writing - original draft: Lee A, Myung SK.– Writing - review & editing: Myung SK, Cho JJ, Yoon JL, Kim MY.
References
- 1.Boivin DB, Boudreau P. Impacts of shift work on sleep and circadian rhythms. Pathol Biol (Paris) 2014;62:292–301. doi: 10.1016/j.patbio.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Vyas MV, Garg AX, Iansavichus AV, Costella J, Donner A, Laugsand LE, Janszky I, Mrkobrada M, Parraga G, Hackam DG. Shift work and vascular events: systematic review and meta-analysis. BMJ. 2012;345:e4800. doi: 10.1136/bmj.e4800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agnès PT, Greet V, Gijs VH, Maija LY, Isabella B, Jorge C. Fifth European working conditions survey [Internet] [accessed on 5 June 2012]. Available at http://www.eurofound.europa.eu/publications/report/2012/working-conditions/fifth-european-working-conditions-survey-overview-report.
- 4.Szosland D. Shift work and metabolic syndrome, diabetes mellitus and ischaemic heart disease. Int J Occup Med Environ Health. 2010;23:287–291. doi: 10.2478/v10001-010-0032-5. [DOI] [PubMed] [Google Scholar]
- 5.Ye HH, Jeong JU, Jeon MJ, Sakong J. The association between shift work and the metabolic syndrome in female workers. Ann Occup Environ Med. 2013;25:33. doi: 10.1186/2052-4374-25-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Puttonen S, Kivimäki M, Elovainio M, Pulkki-Råback L, Hintsanen M, Vahtera J, Telama R, Juonala M, Viikari JS, Raitakari OT, et al. Shift work in young adults and carotid artery intima-media thickness: the Cardiovascular Risk in Young Finns study. Atherosclerosis. 2009;205:608–613. doi: 10.1016/j.atherosclerosis.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Bildt C, Michélsen H. Gender differences in the effects from working conditions on mental health: a 4-year follow-up. Int Arch Occup Environ Health. 2002;75:252–258. doi: 10.1007/s00420-001-0299-8. [DOI] [PubMed] [Google Scholar]
- 8.Ohayon MM, Hong SC. Prevalence of major depressive disorder in the general population of South Korea. J Psychiatr Res. 2006;40:30–36. doi: 10.1016/j.jpsychires.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Bara AC, Arber S. Working shifts and mental health--findings from the British Household Panel Survey (1995–2005) Scand J Work Environ Health. 2009;35:361–367. doi: 10.5271/sjweh.1344. [DOI] [PubMed] [Google Scholar]
- 10.de Vargas D, Dias AP. Depression prevalence in intensive care unit nursing workers: a study at hospitals in a northwestern city of São Paulo State. Rev Lat Am Enfermagem. 2011;19:1114–1121. doi: 10.1590/s0104-11692011000500008. [DOI] [PubMed] [Google Scholar]
- 11.Driesen K, Jansen NW, van Amelsvoort LG, Kant I. The mutual relationship between shift work and depressive complaints--a prospective cohort study. Scand J Work Environ Health. 2011;37:402–410. doi: 10.5271/sjweh.3158. [DOI] [PubMed] [Google Scholar]
- 12.Kim I, Heo HT, Kim S, Jang S. Night duty and depressive symptoms of white collar workers in the public sector. Occup Environ Med. 2011;68:A100–A101. [Google Scholar]
- 13.Øyane NM, Pallesen S, Moen BE, Akerstedt T, Bjorvatn B. Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One. 2013;8:e70228. doi: 10.1371/journal.pone.0070228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gong Y, Han T, Chen W, Dib HH, Yang G, Zhuang R, Chen Y, Tong X, Yin X, Lu Z. Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: a cross-sectional study. PLoS One. 2014;9:e103242. doi: 10.1371/journal.pone.0103242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SG, Kim I, Kim D. Workplace violence and depressive symptomatology among police officer. Occup Environ Med. 2014;71:A76. [Google Scholar]
- 16.Lee HY, Kim MS, Kim O, Lee IH, Kim HK. Association between shift work and severity of depressive symptoms among female nurses: the Korea Nurses’ Health Study. J Nurs Manag. 2016;24:192–200. doi: 10.1111/jonm.12298. [DOI] [PubMed] [Google Scholar]
- 17.Park JN, Han MA, Park J, Ryu SY. Prevalence of depressive symptoms and related factors in Korean employees: the Third Korean Working Conditions Survey (2011) Int J Environ Res Public Health. 2016;13:424. doi: 10.3390/ijerph13040424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lexis MA, Jansen NW, van Amelsvoort LG, van den Brandt PA, Kant I. Depressive complaints as a predictor of sickness absence among the working population. J Occup Environ Med. 2009;51:887–895. doi: 10.1097/JOM.0b013e3181aa012a. [DOI] [PubMed] [Google Scholar]
- 19.Smolensky MH, Hermida RC, Reinberg A, Sackett-Lundeen L, Portaluppi F. Circadian disruption: new clinical perspective of disease pathology and basis for chronotherapeutic intervention. Chronobiol Int. 2016;33:1101–1119. doi: 10.1080/07420528.2016.1184678. [DOI] [PubMed] [Google Scholar]
- 20.Baba M, Ohkura M, Koga K, Nishiuchi K, Herrera LR, Matsuse R, Inoue T. Analysis of salivary cortisol levels to determine the association between depression level and differences in circadian rhythms of shift-working nurses. J Occup Health. 2015;57:237–244. doi: 10.1539/joh.14-0079-OA. [DOI] [PubMed] [Google Scholar]
- 21.Berthelsen M, Pallesen S, Magerøy N, Tyssen R, Bjorvatn B, Moen BE, Knardahl S. Effects of psychological and social factors in shiftwork on symptoms of anxiety and depression in nurses: a 1-year follow-up. J Occup Environ Med. 2015;57:1127–1137. doi: 10.1097/JOM.0000000000000532. [DOI] [PubMed] [Google Scholar]
- 22.Maghsoudipour M, Saberi H. Sleep disorders and depression in shift workers in comparison with day workers. Sleep. 2011;34 Abstr Suppl:A165. [Google Scholar]
- 23.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 24.Simmonds M. Quantifying the risk of error when interpreting funnel plots. Syst Rev. 2015;4:24. doi: 10.1186/s13643-015-0004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meyer-Lindenberg A. Neural connectivity as an intermediate phenotype: brain networks under genetic control. Hum Brain Mapp. 2009;30:1938–1946. doi: 10.1002/hbm.20639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alasaari JS, Lagus M, Ollila HM, Toivola A, Kivimäki M, Vahtera J, Kronholm E, Härmä M, Puttonen S, Paunio T. Environmental stress affects DNA methylation of a CpG rich promoter region of serotonin transporter gene in a nurse cohort. PLoS One. 2012;7:e45813. doi: 10.1371/journal.pone.0045813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hall BS, Moda RN, Liston C. Glucocorticoid mechanisms of functional connectivity changes in stress-related neuropsychiatric disorders. Neurobiol Stress. 2015;1:174–183. doi: 10.1016/j.ynstr.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000;23:477–501. doi: 10.1016/S0893-133X(00)00159-7. [DOI] [PubMed] [Google Scholar]
- 29.Antunes LC, Jornada MN, Ramalho L, Hidalgo MP. Correlation of shift work and waist circumference, body mass index, chronotype and depressive symptoms. Arq Bras Endocrinol Metabol. 2010;54:652–656. doi: 10.1590/s0004-27302010000700010. [DOI] [PubMed] [Google Scholar]