Abstract
Three of ten teenagers in Korea are addicted to mobile phones. The aim of this study was to examine the relationship between mobile phone addiction and the incidence of poor sleep quality and short sleep duration in adolescents. We used longitudinal data from the Korean Children & Youth Panel Survey conducted by the National Youth Policy Institute in Korea (2011–2013). A total of 1,125 students at baseline were included in this study after excluding those who already had poor sleep quality or short sleep duration in the previous year. A generalized estimating equation was used to analyze the data. High mobile phone addiction (mobile phone addiction score > 20) increased the risk of poor sleep quality but not short sleep duration. We suggest that consistent monitoring and effective intervention programs are required to prevent mobile phone addiction and improve adolescents' sleep quality.
Keywords: Mobile Phone Addiction, Sleep Quality, Sleep Duration, Adolescents, Sleep Problems
Graphical Abstract
INTRODUCTION
Mobile phones are now an integral part of people's everyday life, especially young people. Mobile phone overuse and addiction is a critical social issue in many societies. Korea has one of the world's highest mobile phone distribution rates. Approximately 90% of 13-year-old Korean adolescents own their own mobile phone according to a 2010 international comparison report from the Groupe Speciale Mobile Association (1). This rate is higher than those in other Asian countries, China, Japan, and India (from 40% to 60%). Along with the high rate of mobile phone ownership, excessive or uncontrollable use of mobile phones has become a serious social concern for Korean adolescents. Three out of ten teenagers are addicted to their mobile phone according to the Ministry of Science, ICT and Future Planning of Korea. Compared with adults (11.3%), adolescents have a higher mobile phone addiction rate (29.2%) (2). Because teenagers have lower level of self-control, they may be vulnerable to mobile phone addiction (3).
Mobile phone addiction is a rapidly increasing factor that impacts physical and psychological health. Poor sleep quality and insufficient sleep duration are internationally recognized crucial health concerns. In adolescents, sleep is regarded as especially important, as poor or insufficient sleep may cause poor academic performance or negatively impact growth and development (4,5,6,7). Nevertheless, sleep problems are increasingly reported in school-aged children and tend to become worse with age (8). It is well known that there is an inverse relationship between sleep duration and age (9,10). In East Asian cultures, many adolescents have insufficient sleep durations because of a competitive academic environment that forces them to study. Along with insufficient sleep duration, problems related to poor sleep quality have also increased in adolescents (11,12). Furthermore, sleep problems established in childhood tend to continue into adulthood (13).
Many factors impact quality and duration of sleep in adolescents, and one rapidly emerging factor may be the increased use of technology, more specifically mobile phone addiction. There are various reasons why mobile phone addiction may lead to shorter sleep duration or poor sleep (14). Mobile phones are now used not only for calling but also for text messaging, surfing the Internet, playing mobile games, or using social network services. These behaviors may cause short night sleep and disturbed sleep among adolescents who are addicted to mobile phones.
Mobile phone addiction may lead to less and poorer sleep. Several studies show that the use of mobile phones is associated with insufficient sleep duration (14,15). A more recent study, however, shows no significant association between mobile phone addiction and sleep duration (16). Some researchers found that mobile phone overuse or use in the dark is associated with poor sleep (17,18). On the other hand, other researchers found no significant relationship between mobile phone use and sleep disturbances (19). Most studies have examined hours or frequency of mobile phone use and sleep problems but not mobile phone addiction (18,20,21). Furthermore, few studies, especially longitudinal epidemiologic studies based on nationwide representative samples, have been conducted to examine the relationship between mobile phone addiction and sleep quantity and quality in adolescents. Due to the controversy about the relationship between mobile phone addiction and sleep quantity and quality, more longitudinal studies using a representative sample are required.
Therefore, we performed a longitudinal study using a representative sample of Korean adolescents to examine the relationship between mobile phone addiction and sleep quality and duration. Furthermore, to clarify the nature of the relationship between mobile phone addiction and sleep problems, we examined the incidence of poor sleep quality and short sleep duration and performed subgroup analysis according to mobile phone addiction in the past year.
MATERIALS AND METHODS
Participants
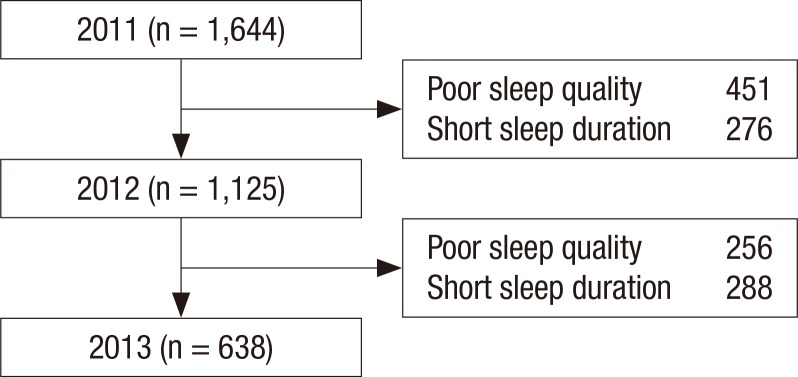
For this study, data from the 3 waves of the Korean Children & Youth Panel Survey (KCYPS) (2011–2013) were analyzed. The National Youth Policy Institute has conducted the KCYPS since 2010. The sample for the KCYPS was selected using stratified multi-stage clustering and was a nationally representative sample of Korean youth. First-year middle school students were stratified into 16 administrative districts relative to the number of students in middle schools in each administrative district. Random sampling was performed using random integers. Expecting that sample attrition would be very slight due to the student study population, we performed a single-subject research design without panel substitution. The panel survey was administered to middle school students and their parents. Group interviews were performed at school for students, and questionnaires were administered to their parents. In total, 2,351 students and their parents were selected as the final sample in the first wave (2010). The sleep quality questionnaire was administered in the second wave (2011). The subjects were 15 years old in 2011 and were followed up until 17 years old. Only 1,125 subjects who did not experience poor sleep quality or short sleep duration in 2011 were analyzed in 2012 as a baseline. We excluded 256 students who had poor sleep quality in the prior year (2012) in the 2013 sleep quality analysis and 288 students who had short sleep duration in the prior year (2012) in the 2013 sleep duration analysis (Fig. 1).
Fig. 1.
Flow chart of study participants.
Outcome variables
The outcome variables were the incidence of poor sleep quality and short sleep duration. Subjects were asked to rate how well they sleep, with poor quality sleep defined as follows: “You cannot fall asleep deeply and wake up often during the night.” Possible responses were: very well, well, poorly, or very poorly. If the answer was “poorly” or “very poorly,” the response was considered to indicate poor sleep quality. Incidence of poor sleep quality was defined as the number of students reporting poor sleep quality in the current year but not in the prior year. Short sleep duration was measured by the inquiry “What time did you go to sleep and get up on average on a weekday (Monday to Friday) this semester?” The number of sleep hours reported by subjects in this study were consistent with those reported in previous studies, which show that a minority of adolescents sleep 8–10 hours (22,23). Only 29.1% of subjects in 2011 slept 8 hours or longer, which is recommended for adolescents (24). As a result, the short sleep duration cutoff was defined as less than 7 hours of sleep in this study.
Mobile phone addiction
Mobile phone addiction was measured by inquiries composed through discussion with a specialist and systematic review: “The amount of time using my cell phone is increasing,” “I feel nervous without my cell phone,” “I feel nervous when I have not received any message or call in some time,” “I'm easily unaware of the passing of time when I'm using my cell phone,” “I feel isolated when I don't have my cell phone with me,” and “I feel too uncomfortable to live even a day when I don't have my cell phone with me.” Answers ranged from 1 to 4 on a 4-point Likert-type scale. Mobile phone addiction level was categorized into 3 groups: low (mobile phone addiction score ≤ 15), middle (mobile phone addiction score > 15 and ≤ 20), and high (mobile phone addiction score > 20).
Covariates
The survey was composed of questions for adolescents and their parents. Questions for children included computer use time (< 2 hours or ≥ 2 hours), television viewing (< 2 hours or ≥ 2 hours), studying outside school hours (low, < 2.5 hours; middle, < 4.5 hours; or high, ≥ 4.5 hours), gender (male or female), year of school (3rd year in middle school or 1st year in high school), health status (good or bad), and academic record (high, middle, or low). Questions for parents included residency area (capital city, metropolitan area, or other), household income (very low, low, high, or very high), father's education level (high school/lower or college/higher), and mother's education level (high school/lower or college/higher).
Statistical analysis
Chi-square tests were used to analyze baseline characteristics according to the occurrence poor sleep quality and short sleep duration. A generalized estimating equation (GEE) model was used to examine the relationship between mobile phone addiction and the incidence of poor sleep quality and short sleep duration. We performed subgroup analysis stratifying the subjects by gender, household income, and mobile phone addiction in the past year.
Ethics statement
The data source used in this study was anonymized prior to public release. Therefore, this study was exempted review by the International Review Board of Yonsei University College of Medicine.
RESULTS
Descriptive statistics of characteristics of the baseline sample according to the occurrence of poor sleep quality and short sleep duration are shown in Table 1. In total, there were 1,125 subjects at baseline after excluding those who had experienced poor sleep quality or short sleep duration in the prior year. At baseline, the number of students who had poor sleep quality was 256 (22.8%), and the number of students who had short sleep duration was 288 (25.6%). Considering mobile phone addiction, students with greater mobile phone addiction showed a significantly higher probability of poor sleep quality (19.0% for mobile phone addiction score ≤ 15, 22.7% for mobile phone addiction score > 15 and ≤ 20, and 31.2% for mobile phone addiction score > 20). When analyzed by study outside school hours, those in the high category had a higher probability of short sleep duration than those in the low or middle categories (14.5% for low, 26.9% for middle, and 32.4% for high).
Table 1. Baseline subject characteristics according to new onset of poor sleep quality and short sleep duration.
| Variables | Total | Poor sleep quality | Short sleep duration | ||
|---|---|---|---|---|---|
| No. (%) | P value | No. (%) | P value | ||
| Mobile phone addiction score | 0.002 | 0.207 | |||
| Low (≤ 15) | 489 | 93 (19.0) | 113 (23.1) | ||
| Middle (>15 and ≤ 20) | 418 | 95 (22.7) | 112 (26.8) | ||
| High (> 20) | 218 | 68 (31.2) | 63 (28.9) | ||
| Computer use time, hr | 0.001 | 0.126 | |||
| < 2 | 786 | 157 (20.0) | 212 (27.0) | ||
| ≥ 2 | 339 | 99 (29.2) | 76 (22.4) | ||
| Television viewing, hr | 0.006 | 0.137 | |||
| < 2 | 751 | 152 (20.2) | 203 (27.0) | ||
| ≥ 2 | 374 | 104 (27.8) | 85 (22.7) | ||
| Study outside school, hr | 0.114 | < 0.001 | |||
| Low (< 2.5) | 303 | 81 (26.7) | 44 (14.5) | ||
| Middle (≥ 2.5 and < 4.5) | 412 | 83 (20.2) | 111 (26.9) | ||
| High (≥ 4.5) | 410 | 92 (22.4) | 133 (32.4) | ||
| Gender | 0.705 | < 0.001 | |||
| Male | 572 | 127 (22.2) | 113 (19.8) | ||
| Female | 553 | 129 (23.3) | 175 (31.7) | ||
| Health status | 0.010 | 0.786 | |||
| Good | 1,045 | 228 (21.8) | 266 (25.5) | ||
| Bad | 80 | 28 (35.0) | 22 (27.5) | ||
| Academic record | 0.098 | < 0.001 | |||
| Low | 236 | 65 (27.5) | 53 (22.5) | ||
| Middle | 624 | 139 (22.3) | 142 (22.8) | ||
| High | 265 | 52 (19.6) | 93 (35.1) | ||
| Residency region | 0.981 | 0.697 | |||
| Capital city (Seoul or Gyeonggi) | 244 | 56 (23.0) | 65 (26.6) | ||
| Metropolitan area | 396 | 91 (23.0) | 105 (26.5) | ||
| Other | 485 | 109 (22.5) | 118 (24.3) | ||
| Household income | 0.764 | < 0.001 | |||
| Very low | 136 | 32 (23.5) | 27 (19.9) | ||
| Low | 227 | 54 (23.8) | 44 (19.4) | ||
| High | 424 | 100 (23.6) | 103 (24.3) | ||
| Very high | 338 | 70 (20.7) | 114 (33.7) | ||
| Father's education | 0.152 | 0.001 | |||
| High school/lower | 490 | 122 (24.9) | 101 (20.6) | ||
| College/higher | 635 | 134 (21.1) | 187 (29.5) | ||
| Mother's education | 0.069 | 0.001 | |||
| High school/lower | 623 | 155 (24.9) | 135 (21.7) | ||
| College/higher | 502 | 101 (20.1) | 153 (30.5) | ||
| Total | 1,125 | 256 (22.8) | 288 (25.6) | ||
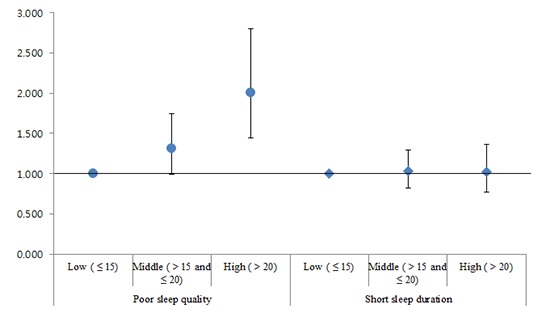
Results of a GEE model for incidence of poor sleep quality and short sleep duration are shown in Table 2. The incidence of poor sleep quality was significantly higher for children with high mobile phone addiction (mobile phone addiction score > 20) than for those with low mobile phone addiction (mobile phone addiction score ≤ 15) after adjusting for possible confounders (odds ratio [OR], 2.009; 95% confidence interval [CI], 1.443–2.796). For sleep duration, students who studied ≥ 4.5 hours outside of class had a higher risk of short sleep duration than those who studied < 2.5 hours (OR, 2.243; 95% CI, 1.683–2.990). When subjects became high school students, they were likely to have better sleep quality but shorter sleep duration than when they were middle school students (OR, 0.387; 95% CI, 0.283–0.504 for poor sleep quality; OR, 10.621; 95% CI, 8.573–13.156 for short sleep duration).
Table 2. Generalized linear model with new onset of poor sleep quality and short sleep duration in 2012–2013.
| Variables | Poor sleep quality | Short sleep duration | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Mobile phone addiction score | ||||
| Low (≤ 15) | 1.000 | - | 1.000 | - |
| Middle (> 15 and ≤ 20) | 1.313 | 0.991–1.740 | 1.030 | 0.819–1.295 |
| High (> 20) | 2.009 | 1.443–2.796 | 1.021 | 0.767–1.360 |
| Computer use time, hr | ||||
| < 2 | 1.000 | - | 1.000 | - |
| ≥ 2 | 1.393 | 0.897–2.164 | 0.866 | 0.594–1.263 |
| Television viewing, hr | ||||
| < 2 | 1.000 | - | 1.000 | - |
| ≥ 2 | 1.034 | 0.668–1.599 | 0.737 | 0.514–1.057 |
| Study outside school, hr | ||||
| Low (< 2.5) | 1.000 | - | 1.000 | - |
| Middle (≥ 2.5 and < 4.5) | 0.644 | 0.467–0.888 | 1.903 | 1.465–2.472 |
| High (≥ 4.5) | 0.890 | 0.635–1.247 | 2.243 | 1.683–2.990 |
| Gender | ||||
| Male | 1.000 | - | 1.000 | - |
| Female | 0.995 | 0.771–1.284 | 1.551 | 1.257–1.915 |
| Year of school | ||||
| 3rd year of middle school | 1.000 | - | 1.000 | - |
| 1st year of high school | 0.378 | 0.283–0.504 | 10.621 | 8.573–13.156 |
| Health status | ||||
| Good | 1.000 | - | 1.000 | - |
| Bad | 1.568 | 1.005–2.447 | 1.061 | 0.725–1.552 |
| Academic record | ||||
| Low | 1.317 | 0.877–1.975 | 0.907 | 0.647–1.273 |
| Middle | 1.094 | 0.786–1.522 | 0.755 | 0.576–0.989 |
| High | 1.000 | - | 1.000 | - |
| Residency region | ||||
| Capital city (Seoul or Gyeonggi) | 1.000 | - | 1.000 | - |
| Metropolitan area | 1.089 | 0.772–1.538 | 1.047 | 0.781–1.404 |
| Other | 1.001 | 0.712–1.408 | 0.910 | 0.684–1.212 |
| Household income | ||||
| Very low | 0.950 | 0.599–1.505 | 0.605 | 0.407–0.900 |
| Low | 1.128 | 0.776–1.639 | 0.664 | 0.484–0.912 |
| High | 1.187 | 0.863–1.633 | 0.794 | 0.615–1.024 |
| Very high | 1.000 | - | 1.000 | - |
| Father's education | ||||
| High school/lower | 1.000 | - | 1.000 | - |
| College/higher | 0.897 | 0.642–1.252 | 1.135 | 0.858–1.502 |
| Mother's education | ||||
| High school/lower | 1.000 | - | 1.000 | - |
| College/higher | 0.937 | 0.669–1.312 | 0.958 | 0.731–1.257 |
OR = odds ratio, CI = confidence interval.
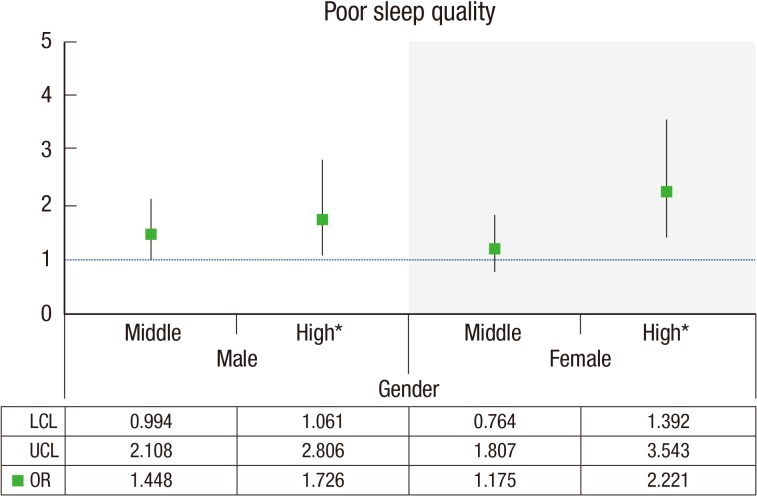
Fig. 2 shows data for mobile phone addiction and sleep quality according to gender. Using the low mobile phone addiction group as the reference group, we found that high mobile phone addiction was significantly associated with poor sleep quality for both genders. Female students with high mobile phone addiction were more likely to have poor sleep than male students with high mobile phone addiction (OR, 1.726; 95% CI, 1.061–2.806 for males; OR, 2.221; 95% CI, 1.392–3.543 for females).
Fig. 2.
Association between mobile phone addiction and new onset of poor sleep quality according to gender. Reference category: low mobile phone addiction score.
LCL = lower confidence limit, UCL = upper confidence limit, OR = odds ratio.
*P value < 0.05.
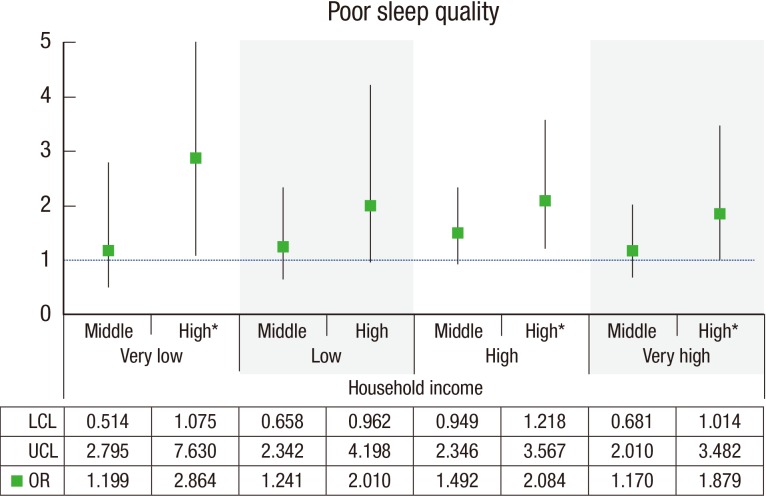
Results of a GEE model stratified by household income are shown in Fig. 3. Among students with high mobile phone addiction, those in a lower household income group had a higher risk of poor sleep quality than those in a higher household income group (OR, 2.864; 95% CI, 1.705–7.630 for very low group; OR, 2.010; 95% CI, 0.962–4.198 for low group; OR, 2.084; 95% CI, 1.218–3.567 for high group; OR, 1.879; 95% CI, 1.014–3.482 for very high group).
Fig. 3.
Association between mobile phone addiction and new onset of poor sleep quality according to household income. Reference category: low mobile phone addiction score.
LCL = lower confidence limit, UCL = upper confidence limit, OR = odds ratio.
*P value < 0.05.
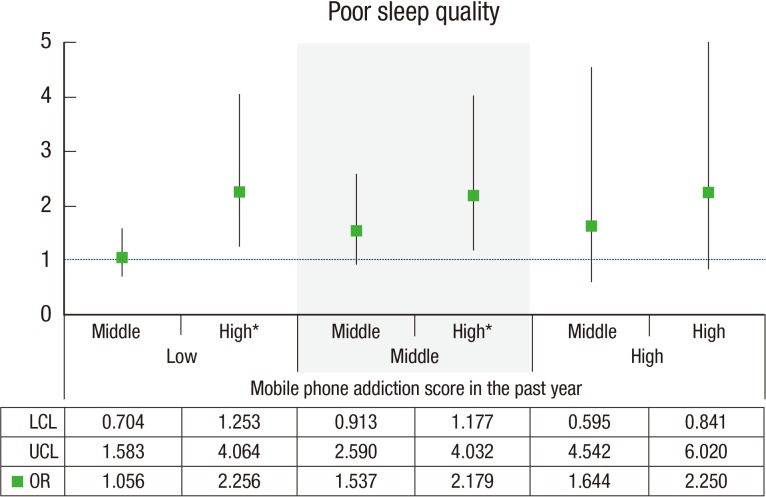
Fig. 4 shows the association between mobile phone addiction and sleep quality according to mobile phone addiction score in the past year. Students with a worsening mobile phone addiction were more likely to have poor sleep quality than those with a consistent low mobile phone addiction or improving mobile phone addiction (OR, 2.256; 95% CI, 1.253–4.064 for low mobile phone addiction score in the past year and high mobile phone addiction score in the current year; OR, 2.179; 95% CI, 1.177–4.032 for middle mobile phone addiction score in the past year and high mobile phone addiction score in the current year).
Fig. 4.
Association between mobile phone addiction and new onset of poor sleep quality according to mobile phone addiction score in the past year. Reference category: low mobile phone addiction score.
LCL = lower confidence limit, UCL = upper confidence limit, OR = odds ratio.
*P value < 0.05.
DISCUSSION
The importance of sleep for health is well known. Unfortunately, a considerable number of people have insufficient or poor sleep. More than just recognizing the importance of sleep, it is necessary to identify and improve the factors disturbing sleep. There are many factors that interrupt good sleep, and one of these may be mobile phone addiction, especially among adolescents. One possible explanation for this is that individuals who are obsessed with their mobile phone do not want to miss any text messages or social network posts, and this might disturb their deep sleep. Also, mobile phone overuse might reduce physical activities leading to good sleep.
Using longitudinal data, the current study examined whether mobile phone addiction is related to the incidence of poor sleep quality and insufficient sleep duration in adolescents. We found that adolescents who were highly addicted to mobile phones had a higher risk of poor sleep quality but not a significantly shorter sleep duration after excluding those with poor sleep quality or short sleep duration in the prior year. It is well known that media use differs by gender (25,26,27). We also found gender differences in the magnitude of the relationship between mobile phone addiction and sleep quality. When students with high mobile phone addiction were stratified by household income, those in the lower household income group were more likely to have poor sleep quality than those in the higher household income group. Considering mobile phone addiction in the past year, students with a worsening mobile phone addiction had a higher risk of poor sleep quality than those with a consistently low mobile phone addiction or improving mobile phone addiction.
The results of this study are accordance with those of previous studies, which show a relationship between mobile phone use and sleep quality in college students (28,29). However, we did not find a significant relationship between mobile phone addiction and sleep duration. Therefore, these results are consistent with those of other studies suggesting that mobile phone addiction has no direct effect on sleep duration in adolescents (16,30). The majority of research on the relationship between mobile phone use and sleep characteristics has been performed using cross-sectional data or studies with small sample sizes in spite of large variability at this age. It is possible that adolescents are addicted to their mobile phone because they cannot sleep well in their sleep environment or because they already have poor sleep. Thus, we aimed to overcome the limitations of previous research by conducting a longitudinal study using a representative Korean youth sample to examine the relationship between mobile phone addiction and sleep quality and duration among middle school students. Furthermore, as the associations between mobile phone addiction and sleep characteristics are complex and bidirectional, we assessed the incidence of poor sleep quality and insufficient sleep duration to examine whether mobile phone addiction is associated with decreased sleep quality and sleep duration.
There are several limitations of this study. First, mobile phone addiction was measured by items developed in Korea. Therefore, a comparative analysis of Korea and other countries is limited. Second, as the data used in this study did not include information on the type of mobile phones, we could not consider differences between smartphones and feature phones. However, we assume that most youths used smartphones, as the survey was conducted in 2011–2013. Third, sleep-related variables in this study were assessed by self-reported measurements and not by objective measurements such as polysomnogram or actigraphy. However, previous studies suggest that self-reported features of sleep are highly associated with electrophysiological measures of sleep (31). Fourth, sleep quality was measured by a single question. More thorough approaches such as the Pittsburgh Sleep Quality Index are a more appropriate method of measuring the quality of sleep. Fifth, a comparison between Korea and other countries might provide more useful insights into the association between mobile phone addiction and sleep problems and strategies for reducing the adverse effects of mobile phone use on sleep in youth. Finally, residual confounders were not investigated in this study, such as depression, anxiety, parents' sleep patterns or sleep circumstances, because of lack of information in the data used in this study.
Despite these limitations, this study has several strengths. First, stratified, randomly sampled, national data were used in this study. Using this community-based large-scale sample increases the external validity of this study and provides more representative results than prior studies with small sample sizes. This large-scale sample also made it possible to conduct well-polished analyses and control potential confounders. Second, this study used longitudinal data instead of cross-sectional data. As most studies of mobile phone addiction and sleep quality in school-aged children are cross-sectional, longitudinal studies in this area are relatively rare. Third, we investigated both adolescents and their parents. Surveying both types of individuals enabled us to obtain more precise information and consider family background. Finally, we excluded students who had sleep problems in the prior year and analyzed the incidence of sleep problems. We found that high mobile phone addiction was a risk factor for poor sleep in school-aged children, even though a bidirectional and more complex relationship may exist between mobile phone addiction and sleep problems.
The current study shows the longitudinal relationship between mobile phone addiction and sleep quality in adolescents. Adolescents tend to be more easily addicted to mobile phones than adults, and this addiction may persist and influence sleep disorders in adulthood. Although teenagers at risk of mobile phone addiction report that family or friends' support is the most helpful factor for decreasing their mobile phone use (2), Korean parents do not care much about their children's use of mobile phones (1). Therefore, we should raise awareness of mobile phone addiction and associated sleep problem among adolescents and their parents. Monitoring mobile phone addiction in adolescents is important, and parents should pay attention to whether their children's mobile phone addiction leads to sleep problem, which in turn may cause physical and psychological health problems. For teenagers, education programs concerning the suitable use of mobile phones and ways of controlling mobile phone use time and counseling programs for those who are already addicted to their mobile phone are required. The findings of this research provide good information to improve youth's sleep quality, which is a crucial worldwide issue.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Lee JE, Jang SI, Park EC. Formal analysis: Lee JE, Lee HJ. Investigation: Lee JE, Kim W. Writing - original draft: Lee JE. Writing - review & editing: Jang SI, Park EC.
References
- 1.Groupe Speciale Mobile Association (JP) Children's use of mobile phones and personal relationships: an international comparison 2011 [Internet] [accessed on 8 May 2017]. Available at http://www.gsma.com/publicpolicy/wp-content/uploads/2012/03/Childrensuseofmobilephones2011.pdf.
- 2.Ministry of Science, ICT and Future Planning (KR) Internet addiction survey 2014 [Internet] [accessed on 8 May 2017]. Available at http://msip.go.kr/SYNAP/skin/doc.html?fn=7d3b3733d68811084a78cc79d78a38bd&rs=/SYNAP/sn3hcv/result/201704/
- 3.Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, Nugent TF, 3rd, Herman DH, Clasen LS, Toga AW, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA. 2004;101:8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10:323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021:276–291. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 6.Kwon JA, Lee M, Yoo KB, Park EC. Does the duration and time of sleep increase the risk of allergic rhinitis? Results of the 6-year nationwide Korea youth risk behavior web-based survey. PLoS One. 2013;8:e72507. doi: 10.1371/journal.pone.0072507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JH, Park EC, Lee SG, Yoo KB. Associations between time in bed and suicidal thoughts, plans and attempts in Korean adolescents. BMJ Open. 2015;5:e008766. doi: 10.1136/bmjopen-2015-008766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12:110–118. doi: 10.1016/j.sleep.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Dollman J, Ridley K, Olds T, Lowe E. Trends in the duration of school-day sleep among 10- to 15-year-old South Australians between 1985 and 2004. Acta Paediatr. 2007;96:1011–1014. doi: 10.1111/j.1651-2227.2007.00278.x. [DOI] [PubMed] [Google Scholar]
- 10.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–307. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt AT, Li X, Hanten GR, McCauley SR, Faber J, Levin HS. A longitudinal investigation of sleep quality in adolescents and young adults after mild traumatic brain injury. Cogn Behav Neurol. 2015;28:53–62. doi: 10.1097/WNN.0000000000000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kronholm E, Puusniekka R, Jokela J, Villberg J, Urrila AS, Paunio T, Välimaa R, Tynjälä J. Trends in self-reported sleep problems, tiredness and related school performance among Finnish adolescents from 1984 to 2011. J Sleep Res. 2015;24:3–10. doi: 10.1111/jsr.12258. [DOI] [PubMed] [Google Scholar]
- 13.Jenni OG, Molinari L, Caflisch JA, Largo RH. Sleep duration from ages 1 to 10 years: variability and stability in comparison with growth. Pediatrics. 2007;120:e769–e776. doi: 10.1542/peds.2006-3300. [DOI] [PubMed] [Google Scholar]
- 14.Punamäki RL, Wallenius M, Nygård CH, Saarni L, Rimpelä A. Use of information and communication technology (ICT) and perceived health in adolescence: the role of sleeping habits and waking-time tiredness. J Adolesc. 2007;30:569–585. doi: 10.1016/j.adolescence.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Harada T, Morikuni M, Yoshii S, Yamashita Y, Takeuchi H. Usage of mobile phone in the evening or at night makes Japanese students evening-typed and night sleep uncomfortable. Sleep Hypn. 2002;4:149–153. [Google Scholar]
- 16.Yen CF, Ko CH, Yen JY, Cheng CP. The multidimensional correlates associated with short nocturnal sleep duration and subjective insomnia among Taiwanese adolescents. Sleep. 2008;31:1515–1525. doi: 10.1093/sleep/31.11.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomée S, Härenstam A, Hagberg M. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults--a prospective cohort study. BMC Public Health. 2011;11:66. doi: 10.1186/1471-2458-11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arora T, Broglia E, Thomas GN, Taheri S. Associations between specific technologies and adolescent sleep quantity, sleep quality, and parasomnias. Sleep Med. 2014;15:240–247. doi: 10.1016/j.sleep.2013.08.799. [DOI] [PubMed] [Google Scholar]
- 19.Söderqvist F, Carlberg M, Hardell L. Use of wireless telephones and self-reported health symptoms: a population-based study among Swedish adolescents aged 15–19 years. Environ Health. 2008;7:18. doi: 10.1186/1476-069X-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents' electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc. 2015;44:405–418. doi: 10.1007/s10964-014-0176-x. [DOI] [PubMed] [Google Scholar]
- 21.Murdock KK. Texting while stressed: implications for students' burnout, sleep, and well-being. Psychol Pop Media Cult. 2013;2:207–221. [Google Scholar]
- 22.Maslowsky J, Ozer EJ. Developmental trends in sleep duration in adolescence and young adulthood: evidence from a national United States sample. J Adolesc Health. 2014;54:691–697. doi: 10.1016/j.jadohealth.2013.10.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tagaya H, Uchiyama M, Ohida T, Kamei Y, Shibui K, Ozaki A, Tan X, Suzuki H, Aritake S, Li L, et al. Sleep habits and factors associated with short sleep duration among Japanese high-school students: a community study. Sleep Biol Rhythms. 2004;2:57–64. [Google Scholar]
- 24.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Hillard PJ, Katz ES, et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Health. 2015;1:233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Van den Bulck J, Van den Bergh B. The influence of perceived parental guidance patterns on children's media use: gender differences and media displacement. J Broadcast Electron Media. 2000;44:329–348. [Google Scholar]
- 26.Igarashi T, Takai J, Yoshida T. Gender differences in social network development via mobile phone text messages: a longitudinal study. J Soc Pers Relat. 2005;22:691–713. [Google Scholar]
- 27.Lee SY, Park EC, Han KT, Kim SJ, Chun SY, Park S. The association of level of internet use with suicidal ideation and suicide attempts in South Korean adolescents: a focus on family structure and household economic status. Can J Psychiatry. 2016;61:243–251. doi: 10.1177/0706743716635550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White AG, Buboltz W, Igou F. Mobile phone use and sleep quality and length in college students. Int J Humanit Soc Sci. 2011;1:51–58. [Google Scholar]
- 29.Li J, Lepp A, Barkley JE. Locus of control and cell phone use: implications for sleep quality, academic performance, and subjective well-being. Comput Human Behav. 2015;52:450–457. [Google Scholar]
- 30.Gaina A, Sekine M, Kanayama H, Sengoku K, Yamagami T, Kagamimori S. Short–long sleep latency and associated factors in Japanese junior high school children. Sleep Biol Rhythms. 2005;3:162–165. [Google Scholar]
- 31.Bertocci MA, Dahl RE, Williamson DE, Iosif AM, Birmaher B, Axelson D, Ryan ND. Subjective sleep complaints in pediatric depression: a controlled study and comparison with EEG measures of sleep and waking. J Am Acad Child Adolesc Psychiatry. 2005;44:1158–1166. doi: 10.1097/01.chi.0000179057.54419.17. [DOI] [PubMed] [Google Scholar]