Abstract
Few studies have assessed the overall effects of multi-centered, complicated mental health support on the grief process. This study investigated the broader influence of mental health support provided practically to the bereaved family on the severity of complicated grief. Ninety-three bereaved family members of the Sewol ferry accident were recruited. Severity of complicated grief, post-traumatic stress disorder (PTSD) and depressive disorder was assessed through self-reporting questionnaire, inventory of complicated grief (ICG), PTSD Check List-5 (PCL-5) and Patient Health Questionnaire-9 (PHQ-9). We also included demographic, socioeconomic, health-related variables, and Functional Social Support Questionnaire (FSSQ), which affect the ICG score. Participants were divided into 4 groups based on the experience of psychotherapy or psychiatry clinic service before the accident and mental health support after the disaster. In univariate analysis, these 4 groups showed a significant difference in the mean ICG score (P = 0.020). Participants who received mental health support only after the Sewol ferry accident (group 2) showed a lower mean ICG score than those who received neither psychotherapy or psychiatry clinic service before the disaster nor mental health support after the accident (group 4). There was no significant correlation between the ICG score and other variables except for subjective health status measured 1 month after the disaster (P = 0.005). There was no significant difference in PCL-5 (P = 0.140) and PHQ-9 scores (P = 0.603) among groups, respectively. In conclusion, mental health support significantly reduced the severity of grief only in those participants who had not received any psychotherapy or psychiatry clinic service before the accident.
Keywords: Grief, Bereavement, Sewol Ferry, Disasters, Mental Health Services, Social Support
Graphical Abstract
INTRODUCTION
The Sewol ferry accident in April 2014 was one of the most tragic disasters in Korean history. Among the 476 people on board, 325 were high school students, 14 were teachers, and a total of 304 people died or are still missing after the disaster. This accident is surely the most traumatic loss to the family. After the Sewol ferry accident, there was increased nationwide interest in disaster mental health support. The majority of mental health support services focused on the post-traumatic stress disorder (PTSD) and acute stress disorder in the bereaved family members. The intervention and evaluation focused on acute stress disorder within one month after the disaster and PTSD in the following period (1). Even though the Sewol ferry accident is fundamentally a bereavement and grief experience after the loss of their family members, few attempts were made to understand their grief process (2). After the Sewol ferry accident, the bereaved family members showed symptoms of PTSD, post-traumatic embitterment disorder, depressive disorder, anxiety disorder, and insomnia disorder. However, most of the bereaved families belong to the general population which consists of those who do not have a history of psychiatric pathologies before the accident. And all of them are essentially undergoing the process of grief after the loss of their family member and most of them are having complicated grief disorder. The prevalence of complicated grief is higher in individuals who lost their child as the bereaved parents of victims of the Sewol ferry accident (3). The loss, which is sudden, unexpected, and caused by intentional power led to violent death is also associated with a high prevalence of complicated grief (4,5). The Sewol ferry accident is a representative example of sudden, unexpected, and violent events. Therefore, it is critical to evaluate the effectiveness of disaster mental health support services offered after the accident in mitigating grief of the bereaved family members.
There are different types of grief support services according to the types of bereaved people, provider, time, settings, and types. Approaches for helping the bereaved family vary from the support provided by their friends or families to a structured grief intervention provided by mental health professionals (6,7). Previous studies on grief support focused on the effects of a specific structured intervention in a clinical setting, where the support services were designed for specific bereaved individuals, support providers, intervention timing, and methods. However, the intervention offered to the family bereaved by a sudden disaster is much more complicated than a specific structured intervention for an individual as in the case of the Sewol ferry accident. For example, various professional organizations or non-professionals provide a range of supported programs over the course of time. And even multiple support approaches by professionals and non-professionals were offered simultaneously. Until now, few studies have investigated the overall effects of multi-centered and complicated mental health support on the grief process in a disaster. In the case of the Sewol ferry accident, various national institutions and agencies, hospitals, professionals, and non-professionals voluntarily involved themselves in the support programs to help the bereaved family members. In particular, immediately after the accident, lack of a control tower prevented the application of systematic mental health support (8). As many as 561 voluntary mental health professionals from 34 supporting organizations participated in these support programs (9). In addition, various religious organizations and personal friends and relatives, which could also be considered as an intervention in a wider sense, visited the bereaved family members. In response to the Sewol ferry accident, the government established the Ansan Mental Health Trauma Center to lead and organize disaster mental health support. However, some of the bereaved family members still hold on to their anger against the government and continue to seek support and counseling from religious organizations or counseling agencies (1).
In this study, we investigated the broader influence of mental health support provided to the bereaved family members in mitigating the grief process. To this end, the severity of complicated grief was determined among those who received some form of support and those who did not receive any form of support. The study also considered the influence of history of psychiatric pathologies before a disaster on the bereaved family members (10). Furthermore, the association of the mental health support and PTSD, depressive disorder was investigated since PTSD and depressive disorder are known to be comorbidities in complicated grief. If mental health support is associated with other psychopathology, the effect of mental health support on grief should be differentiated from the effects of other psychopathological factors. We also examined whether the level of social support, which is known to be related to grief, differs according to whether or not they receive mental health support.
MATERIALS AND METHODS
Participants
We contacted the representatives of the council of bereaved families in Asan, Korea to explain them the purpose of the study that is part of a longitudinal cohort study. The cohort study performed to identify the risk and prognostic factors that have an influence on mental health of individuals who have experienced a disaster. After the representatives of the council of bereaved families agreed, 93 bereaved family members were recruited. Before the survey was carried out, informed consent was obtained from all participants. Psychiatrists who are disaster mental health professionals interviewed the participants. Data were collected through self-reporting questionnaire, including psychiatric scales, socio-demographic variables and items for psychiatric symptoms. Out of the 93 bereaved family members, 87 participants completed the questionnaire, and only data from the completed questionnaires were used for analysis.
History of psychiatric pathologies before a disaster is a risk factor for psychiatric problems after the disaster, such as complicated grief (10). Therefore, the participants were divided into 4 groups based on the experience of psychotherapy or psychiatry clinic service before the accident and mental health support after the disaster. In this study, mental health support services for the Sewol ferry accident included the Ansan Mental Health Trauma Center service, psychiatric clinic service by a psychiatrist, counseling center service, mental health support by religious organizations, and ventilation to friends (support by friends). Group 1 received psychotherapy or psychiatry clinic service before the disaster and mental health support after the Sewol ferry accident. Group 2 consisted of those who received mental health support only after the Sewol ferry accident. Participants included in group 4 received neither psychotherapy or psychiatry clinic service before the disaster nor mental health support after the Sewol ferry accident. Because only one participant was classified into group 3, which consisted of individuals who received psychotherapy or psychiatry clinic service only before the disaster, group 3 was excluded from univariate and multivariate analyses, and only its frequency and descriptive statistics were presented.
Measures
We included the variables that affect the inventory of complicated grief (ICG) score (11). We categorized the variables based on 3 characteristics: demographic, socioeconomic, and health-related characteristics. Demographic variables included sex, age, marital status, having a child/children other than the deceased child, family generations, and religion. Socioeconomic variables included economic status, unemployment after the disaster, type of residence, type of medical insurance, and insurance coverage for the accident. Lastly, health-related variables included receipt of psychiatry clinic service or psychotherapy before and after the disaster, hospitalization after the disaster, use of pharmaceutical medicine without prescription, outpatient visit, use of sleeping pills, digestive medicine and pain reliever, subjective health status 1 month after the disaster, diagnosis of severe and chronic diseases, family history of psychiatric illness, alcohol drinking, smoking, and physical activity.
ICG
ICG (11) is a self-rated inventory which was developed to evaluate the symptoms of grief to predict functional mental disorders. This instrument was designed to measure functional mental symptoms that have been termed as complicated grief. The rating score of ICG ranges from 0 to 76, and a score of 25 or higher is considered as a high-risk group requiring therapeutic intervention.
PTSD Check List-5 (PCL-5)
The PCL-5 (12) is a self-rated inventory which was developed for screening PTSD symptoms based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). The score of the PCL-5 scale ranges from 0 to 80, and a score of 38 is used as the cut-off score for PTSD diagnosis.
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 (13) is an inventory for screening, diagnosing, monitoring, and measuring the severity of depression. The PHQ-9 has 9 questions, and each question rates the frequency of symptoms according to the scoring severity index from 0 to 3. The PHQ-9 score ranges from 0 to 27, and a score of 8–11 is used as the cut-off score for the diagnosis of major depressive disorder (14).
Functional Social Support Questionnaire (FSSQ)
The FSSQ (14,15) is a self-rated FSSQ consisting of 14 items, and the FSSQ score ranges from 14 to 70. The lower the total score, the higher the degree of social support.
Data analysis
We conducted a frequency and descriptive statistical analysis to calculate the frequency, mean, standard deviation (SD), median, interquartile range (IQR), and minimum and maximum values. For univariate analysis, we performed t-test, one-way analysis of variance (ANOVA) and correlation analysis to identify the mean difference among groups and to determine the relationship between continuous variables and ICG, PCL-5, and PHQ-9 scores. To control for potential confounding factors, multiple linear regression analysis was carried out. It identified the association of variables with ICG, PCL-5, and PHQ-9 scores. All statistical analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Seoul St. Mary's Hospital at The Catholic University of Korea (registration No. KC15OIMI0261). Informed consent was submitted by all subjects when they were enrolled.
RESULTS
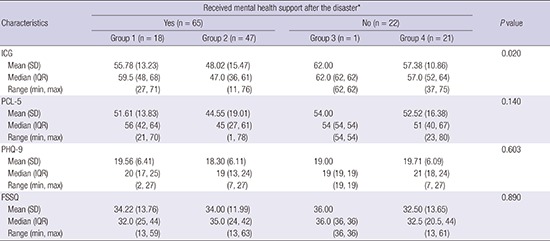
Eighty-seven bereaved family members, who completed the questionnaires, included 75 parents, 1 wife, 2 grandparents, 8 siblings, and 1 aunt of the victims. The mean ICG score of 87 bereaved family members was 54.05 (SD, 14.49; ranging from 11 to 76). Of the 87 participants, 84 scored 25 or above on the ICG scale and showed symptoms of complicated grief. Table 1 shows the demographic, socioeconomic, health-related variables of the study population and the univariate analysis results of the ICG score for each intervention group. Groups 1, 2, 3, and 4 comprised of 18, 47, 1, and 21 people, respectively. In univariate analysis, groups showed a significant difference in the mean ICG score (P = 0.020). There was no significant correlation between the ICG score and other variables except for subjective health status measured 1 month after the disaster (P = 0.005). Furthermore, the association of variables with PCL-5 and PHQ-9 scores was analyzed. In univariate analysis, there was no significant difference in the PCL-5 (P = 0.140) and PHQ-9 scores (P = 0.603) among groups, respectively. Subjective health status 1 month after the disaster also showed a significant difference in the mean PCL-5 (P < 0.001) and PHQ-9 scores (P < 0.001), respectively. Otherwise no significant correlation was found between the PCL-5 and PHQ-9 scores and other variables except for alcohol drinking status in the PCL-5 (P = 0.038).
Table 1. Baseline characteristics of the study population (n = 87).
| Characteristics | Received mental health support after the disaster* | P value | |||
|---|---|---|---|---|---|
| Yes (n = 65) | No (n = 22) | ||||
| Group 1 (n = 18) | Group 2 (n = 47) | Group 3 (n = 1) | Group 4 (n = 21) | ||
| Age, yr | 0.122‡ | ||||
| No. | 18 | 47 | 1 | 21 | |
| Mean (SD) | 47.6 (8.56) | 43.7 (9.44) | 42.0 | 45.1 (6.66) | |
| Median (IQR) | 50 (43, 53) | 46 (43, 49) | 42 (42, 42) | 45 (42, 47) | |
| Range (min, max) | (21, 60) | (15, 61) | (42, 42) | (25, 56) | |
| Sex, No. (%) | 0.565† | ||||
| Male | 8 (21.62) | 19 (51.35) | 0 | 10 (27.03) | |
| Female | 10 (20.00) | 28 (56.00) | 1 (2.00) | 11 (22.00) | |
| Marital status, No. (%) | 0.784† | ||||
| Married | 15 (23.81) | 33 (52.38) | 0 | 15 (23.81) | |
| Single, widowed, divorced | 3 (13.64) | 12 (54.55) | 1 (4.55) | 6 (27.27) | |
| Had children after the disaster, No. (%) | 0.183† | ||||
| No | 6 (24.00) | 13 (52.00) | 0 | 6 (24.00) | |
| Yes | 9 (18.75) | 27 (56.25) | 1 (2.08) | 11 (22.92) | |
| Family generation | 0.292§ | ||||
| 1 generation | 3 (33.33) | 5 (55.56) | 0 | 1 (11.11) | |
| 2 generations | 13 (20.31) | 33 (51.56) | 1 (1.56) | 17 (26.56) | |
| 3 generations | 2 (25.00) | 5 (62.50) | 0 | 1 (12.50) | |
| Religion | 0.929† | ||||
| Yes | 11 (26.83) | 19 (46.34) | 0 | 11 (26.83) | |
| No | 7 (15.56) | 28 (62.22) | 1 (2.22) | 9 (20.00) | |
| Economic activity | 0.697† | ||||
| Yes | 9 (18.37) | 25 (51.02) | 1 (2.04) | 14 (28.57) | |
| No | 9 (24.32) | 21 (56.76) | 0 | 7 (18.92) | |
| Unemployed after the accident | 0.174† | ||||
| No | 11 (20.00) | 27 (49.09) | 1 (1.82) | 16 (29.09) | |
| Yes | 7 (22.58) | 20 (64.52) | 0 | 4 (12.90) | |
| Residence type | 0.780§ | ||||
| Own house | 14 (24.56) | 27 (47.37) | 0 | 16 (28.07) | |
| Lease | 1 (6.67) | 12 (80.00) | 0 | 2 (13.33) | |
| Monthly rent, etc. | 3 (27.27) | 6 (54.55) | 0 | 2 (18.18) | |
| Medical care | 0.583† | ||||
| Medical insurance | 17 (25.37) | 35 (52.24) | 0 | 15 (22.39) | |
| Other medical care | 0 | 6 (50.00) | 0 | 6 (50.00) | |
| Accident-related insurance | 0.282† | ||||
| Received | 8 (25.00) | 17 (53.13) | 0 | 7 (21.88) | |
| Not received | 10 (18.52) | 30 (55.56) | 1 (1.85) | 13 (24.07) | |
| Hospitalization after the accident | 0.348† | ||||
| Yes | 9 (16.36) | 29 (52.73) | 1 (1.82) | 16 (29.09) | |
| No | 9 (28.13) | 18 (56.25) | 0 | 5 (15.63) | |
| Pharmacy visit after the accident | 0.561† | ||||
| Yes | 2 (6.67) | 17 (56.67) | 0 | 11 (36.67) | |
| No | 16 (28.07) | 30 (52.63) | 1 (1.75) | 10 (17.54) | |
| Outpatient visit | 0.354† | ||||
| No | 5 (11.63) | 26 (60.47) | 1 (2.33) | 11 (25.58) | |
| Yes | 13 (29.55) | 21 (47.73) | 0 | 10 (22.73) | |
| Sleeping pills | 0.641† | ||||
| No | 4 (28.57) | 7 (50.00) | 0 | 3 (21.43) | |
| Yes | 14 (19.18) | 40 (54.79) | 1 (1.37) | 18 (24.66) | |
| Digestive medicine | 0.184† | ||||
| No | 7 (21.21) | 16 (48.48) | 1 (3.03) | 9 (27.27) | |
| Yes | 11 (20.37) | 31 (57.41) | 0 | 12 (22.22) | |
| Pain reliever | 0.762† | ||||
| No | 4 (13.33) | 16 (53.33) | 1 (3.33) | 9 (30.00) | |
| Yes | 14 (24.56) | 31 (54.39) | 0 | 12 (21.05) | |
| Subjective health status after the accident | 0.005† | ||||
| No change or improved | 1 (11.11) | 6 (66.67) | 0 | 2 (22.22) | |
| Deteriorated | 17 (21.79) | 41 (52.56) | 1 (1.28) | 19 (24.36) | |
| Diagnosis of a severe and chronic disease | 0.792† | ||||
| No | 11 (17.46) | 34 (53.97) | 1 (1.59) | 17 (26.98) | |
| Yes | 7 (29.17) | 13 (54.17) | 0 | 4 (16.67) | |
| Family psychiatric history | 0.574† | ||||
| No | 15 (19.74) | 42 (55.26) | 1 (1.32) | 18 (23.68) | |
| Yes | 3 (30.00) | 5 (50.00) | 0 | 2 (20.00) | |
| Alcohol consumption | 0.144§ | ||||
| No | 6 (31.58) | 6 (31.58) | 0 | 7 (36.84) | |
| Low-risk | 10 (20.83) | 28 (58.33) | 1 (2.08) | 9 (18.75) | |
| High-risk | 2 (10.53) | 12 (63.16) | 0 | 5 (26.32) | |
| Smoking | 0.843§ | ||||
| No | 8 (17.78) | 27 (60.00) | 1 (2.22) | 9 (20.00) | |
| Previous smoker | 6 (60.00) | 2 (20.00) | 0 | 2 (20.00) | |
| Smoker | 3 (12.50) | 15 (62.50) | 0 | 6 (25.00) | |
| Physical exercise | 0.760† | ||||
| No | 13 (20.63) | 30 (47.62) | 1 (1.59) | 19 (30.16) | |
| Yes | 5 (22.73) | 15 (68.18) | 0 | 2 (9.09) | |
SD = standard deviation, IQR = interquartile range, min = minimum, max = maximum, ANOVA = analysis of variance.
*Participants who received psychotherapy or psychiatry clinic service before the disaster were classified as groups 1 and 3. And participants who did not received were classified as groups 2 and 4. †P value by t-test. ‡P value by Correlation analysis. §P value by one-way ANOVA.
The results of multiple linear regression analysis are summarized in Table 2. We included the variables, which were found to be significant in univariate analysis, in a regression model. And we also included the demographic variables such as age and sex. In multiple linear regression analysis, the ICG score was significantly associated with group 2 (β = 9.07; P = 0.012) and subjective health status 1 month after the disaster (β = 14.18; P = 0.007).
Table 2. Results of multiple linear regression analysis of variables related to ICG score.
| Variables | Coeff. | SE | P value | |
|---|---|---|---|---|
| Groups based on the experience of psychotherapy or psychiatry clinic service before the Sewol Ferry accident and mental health support after the accident | Group 1 | 2.76 | 4.33 | 0.525 |
| Group 2 | 9.07 | 3.53 | 0.012 | |
| Group 4 | Reference | - | - | |
| Sex | Male | 5.7 | 3.17 | 0.075 |
| Female | Reference | - | - | |
| Age | −0.17 | 0.19 | 0.365 | |
| Subjective health status after the accident | No change or improved | 14.18 | 5.13 | 0.007 |
| Deteriorated | Reference | - | - | |
ICG = inventory of complicated grief, Coeff. = coefficient, SE = standard error.
R2 = 20%, Adj R2 = 15%.
Group 2 showed a lower mean ICG score than group 4 (Table 3). Group 2 showed lower mean PCL-5 and PHQ-9 scores than group 4, but the differences were not significant. Also, the improving or remaining subjective health status group showed lower mean ICG, PCL-5, and PHQ-9 scores than the worse subjective health status group. In the PCL-5 scale, non-alcoholic participants (mean ± SD, 49.83 ± 19.22) in group 2 showed a higher PCL-5 score than participants in the low risk (44.96 ± 18.94) and high risk (38.17 ± 17.34) alcohol drinking groups. Alcohol may function as a sedative, counterbalancing the symptoms of PTSD, but it is most likely that persistent alcohol consumption may cause more severe mental health problems later.
Table 3. Differences in ICG, PCL-5, PHQ-9, and FSSQ scores among groups.
| Characteristics | Received mental health support after the disaster* | P value | |||
|---|---|---|---|---|---|
| Yes (n = 65) | No (n = 22) | ||||
| Group 1 (n = 18) | Group 2 (n = 47) | Group 3 (n = 1) | Group 4 (n = 21) | ||
| ICG | 0.020 | ||||
| Mean (SD) | 55.78 (13.23) | 48.02 (15.47) | 62.00 | 57.38 (10.86) | |
| Median (IQR) | 59.5 (48, 68) | 47.0 (36, 61) | 62.0 (62, 62) | 57.0 (52, 64) | |
| Range (min, max) | (27, 71) | (11, 76) | (62, 62) | (37, 75) | |
| PCL-5 | 0.140 | ||||
| Mean (SD) | 51.61 (13.83) | 44.55 (19.01) | 54.00 | 52.52 (16.38) | |
| Median (IQR) | 56 (42, 64) | 45 (27, 61) | 54 (54, 54) | 51 (40, 67) | |
| Range (min, max) | (21, 70) | (1, 78) | (54, 54) | (23, 80) | |
| PHQ-9 | 0.603 | ||||
| Mean (SD) | 19.56 (6.41) | 18.30 (6.11) | 19.00 | 19.71 (6.09) | |
| Median (IQR) | 20 (17, 25) | 19 (13, 24) | 19 (19, 19) | 21 (18, 24) | |
| Range (min, max) | (2, 27) | (7, 27) | (19, 19) | (7, 27) | |
| FSSQ | 0.890 | ||||
| Mean (SD) | 34.22 (13.76) | 34.00 (11.99) | 36.00 | 32.50 (13.65) | |
| Median (IQR) | 32.0 (25, 44) | 35.0 (24, 42) | 36.0 (36, 36) | 32.5 (20.5, 44) | |
| Range (min, max) | (13, 59) | (13, 63) | (36, 36) | (13, 61) | |
ICG = inventory of complicated grief, PTSD = post-traumatic stress disorder, PCL-5 = PTSD Check List-5, PHQ-9 = Patient Health Questionnaire-9, FSSQ = Functional Social Support Questionnaire, SD = standard deviation, IQR = interquartile range, min = minimum, max = maximum.
*Participants who received psychotherapy or psychiatry clinic service before the disaster were classified as groups 1 and 3. And participants who did not received were classified as groups 2 and 4.
Table 3 shows the FSSQ scores for each group. There is a possibility that mental health support could be considered a different aspect of social support, which is known to help mitigate the grief response (16,17). Therefore, we analyzed FSSQ according to the 4 groups. Group 2 showed a higher mean FSSQ score, indicating a low level of subjective functional social support, than group 4, but the difference was not significant. There was no significant correlation between the degree of social support and whether or not they received mental health support.
DISCUSSION
There are many different types of mental health support services according to the types of bereaved people, provider, time, settings, and types and adequate mental health support is needed for bereaved people who experience a traumatic loss (18,19,20,21,22,23,24,25,26). Previous studies have focused on a specific structured intervention. However, the intervention offered to the family bereaved by a sudden disaster is much more complicated than a specific structured intervention for an individual. There are few studies assessing the overall effects of multi-centered and complicated mental health support on the grief process.
This study investigated the broader influence of mental health support provided practically to the bereaved family on the severity of complicated grief. The effects of disaster mental health support on an individual's grief caused by a sudden disaster were evaluated in a broad perspective. We did not focus on a specific structured intervention as in previous studies. Accordingly, comprehensive mental health support services including the Ansan Mental Health Trauma Center service, psychiatry clinic service by a psychiatrist, counseling center service, mental health support by religious organizations and ventilation to friends (support by friends) were considered in this study. The results of this study demonstrated that any form of mental health support reduced the severity of grief. This result is particularly meaningful because it was obtained from the analysis of the 4 groups categorized based on the experience of psychotherapy or psychiatry clinic service before the disaster. Mental health support significantly reduced the severity of grief only in those participants who had not received any psychotherapy or psychiatry clinic service before the traumatic loss. To determine if the disaster mental health support services were associated with other mental health problems, the severity of depressive disorder and PTSD was analyzed. There was no significant difference in PCL-5 and PHQ-9 scores among groups. Since after the Sewol ferry accident, mental health support focused on acute stress disorder and PTSD, it is interesting to note that mental health support after Sewol ferry accident showed a greater association with the severity of grief than with that of other pathologies.
Although currently there is a lack of policies to mitigate the grief of bereaved families, the understanding and empathy of individual mental health support providers for the bereaved family members might have influenced the grief process of families. These qualitative effects could not be represented by the qualitative results of this study. And it is not clear if the effects are common among those who lost their family member in other disasters. These issues should be further investigated in future studies.
The participants' interpretation of receiving an intervention should also be considered. Considering that the concept of mental health support can be a different aspect of social support, we evaluated the degree of social support perceived by the 4 groups using the FSSQ scale. The results showed that there was no significant difference in social support among groups. Wilson et al. (6) reviewed 38 bereavement services and suggested that educational information and emotional support from organizations or support providers who prepared to help a bereaved person were helpful for bereaved individuals. In a report on resilience to loss and chronic grief by Bonanno et al. (17), coping resources were described to play a critical role in moderating adjustment to interpersonal loss. In this study, we propose that the participants' acceptance of any form of disaster mental health support service could be explained by the ‘willingness’ or ‘coping resources’ to seek help from support providers. And further studies are needed on this subject.
An advantage of this study is that it included a number of demographic, socioeconomic and health-related variables which can affect the severity of grief, PTSD and depression. Among the variables considered, the presence of mental health support most significantly influenced the severity of grief. The subgroup with worse subjective health status in each group showed a higher correlation with grief, PTSD and depression, which could be attributed to the association between subjective physical health status and mental health. The association between physical and mental health should be carefully considered when disaster mental health is concerned.
The limitations of this study also merit brief discussion. First, the sample size assessed in this study was not large enough. Second, the participants were limited to family members bereaved by the Sewol ferry accident, and they may not represent the populations dealing with grief caused by a traumatic loss. Based on the ICG scores, 84 of the 87 participants were suffering from complicated grief, and this incidence was higher than that reported in previous studies. This high prevalence may be related to factors such as the scale of the tragic accident, predominant young victims, man-made disaster caused by half-hearted response of the government and unclear explanation provided by the government, which all together aggravate embitterment. Unlike other studies where data were collected from multiple disasters, the scope of this study was limited to a single disaster, eliminating potential disturbance due to the heterogeneous data source. Third, this was a cross-sectional study performed 1 year 6 months after the accident. However, because most of the previous studies measured the effects of intervention on the grief process immediately after disasters, the results of this study could be used to elaborate on the long-term effects of grief intervention on mental health support. Fourth, this study was based on the use of self-rating questionnaires. Only the presence of disaster mental health support service was considered and its frequency was not taken into consideration. Therefore, although the effects of the frequency of disaster mental health support service could not be determined, a simple yes/no answer would have ensured the credibility of the results which were dependent on the presence of intervention.
In future studies, we expect a comprehensive assessment of the effects of mental health support on disaster mental health so that an appropriate intervention can be developed and provided to each individual who has experienced a disaster and is currently experiencing grief.
ACKNOWLEDGMENT
We are thankful for the families, who despite the unbearable physical and mental pain, participated in the study, and for those who have striven to help them. It is impossible for the family members to forget the Sewol ferry accident, but we sincerely hope that our society will become safer as the families' desire and the suffering of the families is relieved.
Footnotes
Funding: This study was supported by a grant of the Korean Mental Health Technology R & D Project, Ministry of Health and Welfare, Republic of Korea (HM15C1054).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Han H, Noh JW, Huh HJ, Huh S, Chae JH. Data curation: Han H, Huh HJ, Huh S, Joo JY. Investigation: Han H, Noh JW, Huh HJ, Joo JY, Hong JH. Writing - original draft: Han H, Noh JW. Writing - review & editing: Han H, Noh JW, Chae JH.
References
- 1.Paik JW, Kim HS, Sim M, Lee HK, Woo YS, Chung C, Lee SH, Seok JH, Jeon HJ, Lee SM, et al. The Sewol Ferry accident and early mental health care response by volunteer activities of Korean Disaster Mental Health Committee and members of Korean Neuropsychiatric Association. J Korean Neuropsychiatr Assoc. 2015;54:1–5. [Google Scholar]
- 2.Han H, Choi W, Huh S, Heo HJ, Chae JH. Understanding of complicated grief. Cognitive Behav Ther Korea. 2016;16:383–401. [Google Scholar]
- 3.Meert KL, Shear K, Newth CJ, Harrison R, Berger J, Zimmerman J, Anand KJ, Carcillo J, Donaldson AE, Dean JM, et al. Follow-up study of complicated grief among parents eighteen months after a child’s death in the pediatric intensive care unit. J Palliat Med. 2011;14:207–214. doi: 10.1089/jpm.2010.0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Currier JM, Holland JM, Neimeyer RA. Sense-making, grief, and the experience of violent loss: toward a mediational model. Death Stud. 2006;30:403–428. doi: 10.1080/07481180600614351. [DOI] [PubMed] [Google Scholar]
- 5.Nakajima S, Ito M, Shirai A, Konishi T. Complicated grief in those bereaved by violent death: the effects of post-traumatic stress disorder on complicated grief. Dialogues Clin Neurosci. 2012;14:210–214. doi: 10.31887/DCNS.2012.14.2/snakajima. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilson DM, Dhanji N, Playfair R, Nayak SS, Puplampu GL, Macleod R. A scoping review of bereavement service outcomes. Palliat Support Care. 2017;15:242–259. doi: 10.1017/S147895151600047X. [DOI] [PubMed] [Google Scholar]
- 7.Wittouck C, Van Autreve S, De Jaegere E, Portzky G, van Heeringen K. The prevention and treatment of complicated grief: a meta-analysis. Clin Psychol Rev. 2011;31:69–78. doi: 10.1016/j.cpr.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Lee N, Sim K, Hahn S, Lee K, Sim M, Chae JH, Ahn H. A qualitative content analysis of reports of mental health service providers after the Sewol Ferry accident in Korea. Ment Health Soc Work. 2015;43:116–144. [Google Scholar]
- 9.Gyeonggi-do Ansan-si Integrated Disaster Metal Health Support Team (KR) Disaster Mental Health Support for 14 Days after the Sewol Ferry Accident. Suwon: Gyeonggi Provincial Mental Health Center; 2014. [Google Scholar]
- 10.Ogrodniczuk JS, Joyce AS, Piper WE. Changes in perceived social support after group therapy for complicated grief. J Nerv Ment Dis. 2003;191:524–530. doi: 10.1097/01.nmd.0000082180.09023.64. [DOI] [PubMed] [Google Scholar]
- 11.Prigerson HG, Maciejewski PK, Reynolds CF, 3rd, Bierhals AJ, Newsom JT, Fasiczka A, Frank E, Doman J, Miller M. Inventory of complicated grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res. 1995;59:65–79. doi: 10.1016/0165-1781(95)02757-2. [DOI] [PubMed] [Google Scholar]
- 12.Hoge CW, Riviere LA, Wilk JE, Herrell RK, Weathers FW. The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: a head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. Lancet Psychiatry. 2014;1:269–277. doi: 10.1016/S2215-0366(14)70235-4. [DOI] [PubMed] [Google Scholar]
- 13.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184:E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC functional social support questionnaire. Measurement of social support in family medicine patients. Med Care. 1988;26:709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Burke LA, Neimeyer RA, McDevitt-Murphy ME. African American homicide bereavement: aspects of social support that predict complicated grief, PTSD, and depression. Omega (Westport) 2010;61:1–24. doi: 10.2190/OM.61.1.a. [DOI] [PubMed] [Google Scholar]
- 17.Bonanno GA, Wortman CB, Lehman DR, Tweed RG, Haring M, Sonnega J, Carr D, Nesse RM. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. J Pers Soc Psychol. 2002;83:1150–1164. doi: 10.1037//0022-3514.83.5.1150. [DOI] [PubMed] [Google Scholar]
- 18.Boelen PA, de Keijser J, van den Hout MA, van den Bout J. Treatment of complicated grief: a comparison between cognitive-behavioral therapy and supportive counseling. J Consult Clin Psychol. 2007;75:277–284. doi: 10.1037/0022-006X.75.2.277. [DOI] [PubMed] [Google Scholar]
- 19.Reynolds CF, 3rd, Miller MD, Pasternak RE, Frank E, Perel JM, Cornes C, Houck PR, Mazumdar S, Dew MA, Kupfer DJ. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatry. 1999;156:202–208. doi: 10.1176/ajp.156.2.202. [DOI] [PubMed] [Google Scholar]
- 20.Rosner R, Bartl H, Pfoh G, Kotoučová M, Hagl M. Efficacy of an integrative CBT for prolonged grief disorder: a long-term follow-up. J Affect Disord. 2015;183:106–112. doi: 10.1016/j.jad.2015.04.051. [DOI] [PubMed] [Google Scholar]
- 21.Shear K, Frank E, Houck PR, Reynolds CF., 3rd Treatment of complicated grief: a randomized controlled trial. JAMA. 2005;293:2601–2608. doi: 10.1001/jama.293.21.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smid GE, Kleber RJ, de la Rie SM, Bos JB, Gersons BP, Boelen PA. Brief eclectic psychotherapy for traumatic grief (BEP-TG): toward integrated treatment of symptoms related to traumatic loss. Eur J Psychotraumatol. 2015;6:27324. doi: 10.3402/ejpt.v6.27324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weissman MM, Markowitz JC, Klerman GL. Comprehensive Guide to Interpersonal Psychotherapy. New York, NY: Basic Books; 2000. [Google Scholar]
- 24.Zygmont M, Prigerson HG, Houck PR, Miller MD, Shear MK, Jacobs S, Reynolds CF., 3rd A post hoc comparison of paroxetine and nortriptyline for symptoms of traumatic grief. J Clin Psychiatry. 1998;59:241–245. doi: 10.4088/jcp.v59n0507. [DOI] [PubMed] [Google Scholar]
- 25.Hensley PL, Slonimski CK, Uhlenhuth EH, Clayton PJ. Escitalopram: an open-label study of bereavement-related depression and grief. J Affect Disord. 2009;113:142–149. doi: 10.1016/j.jad.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 26.Simon NM, Shear MK, Fagiolini A, Frank E, Zalta A, Thompson EH, Reynolds CF, 3rd, Silowash R. Impact of concurrent naturalistic pharmacotherapy on psychotherapy of complicated grief. Psychiatry Res. 2008;159:31–36. doi: 10.1016/j.psychres.2007.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


