Abstract
Background:
Vertigo Symptom Scale (VSS) is a proper instrument for assessing the patient status, clarifying the symptoms, and examining the relative impact of the vertigo and anxiety on reported handicap. Our aim is the translation and cross-cultural adaptation of the VSS into Persian language (VSS-P) and investigating its validity and reliability in patients with peripheral vestibular disorders.
Materials and Methods:
VSS was translated into Persian. Cross-cultural adaptation was carried out on 101 patients with peripheral vestibular disorders and 34 participants with no history of vertigo. They completed the Persian versions of VSS, dizziness handicap inventory (DHI), and Beck anxiety inventory (BAI). Internal, discriminant, and convergent validities, internal consistency, and test-retest reliability were determined.
Results:
The VSS-P showed good face validity. Internal validity was confirmed and demonstrated the presence of two vertigo (VSS-VER) and autonomic-anxiety (VSS-AA) subscales. Significant difference between the median scores for patient and healthy groups was reported in discriminate validity (P <0.001). Convergent validity revealed high correlation between both BAI and DHI with VSS-P. There was a high test-retest reliability; with intraclass correlation coefficient of 0.89, 0.86, and 0.91 for VSS-AA, VER, and VSS-P, respectively. The internal consistency was good with Cronbach's alpha 0.90 for VER subscale, 0.86 for VSS-AA subscale, and 0.92 for the overall VSS-P.
Conclusion:
The Persian version of the VSS could be used clinically as a valid and reliable tool. Thus, it is a key instrument to focus on the symptoms associated with dizziness.
Keywords: Anxiety, Persian, reliability, validity, vertigo, Vertigo Symptom Scale
INTRODUCTION
Dizziness is among the most common patient complaints. Diagnosing the cause of dizziness can be challenging due to its vague symptoms and broad causes, ranging from vestibular to psychological.[1,2] Dizziness is a general term often used to describe a variety of subjective symptoms, including vertigo, disequilibrium, presyncope, and lightheadedness.[3,4] Vertigo, a perception of motion without any external source of that sensation, is a common type of dizziness due to vestibular causes.[1,5,6]
Substantial and increasing evidence points to a link between vestibular disorders and the activation of certain parts of the brain, notably those related to emotion and the autonomic nervous system.[1,7,8] The patients with vestibular vertigo syndromes usually suffer from anxiety and depression as well.[9] On the other hand, patients with psychiatric disorders can experience subjective unsteadiness, dizziness, or vertigo.[10,11]
As conventional vestibular metric techniques cannot completely evaluate the clinical state of patients with vestibular-balance symptoms,[12,13] self-assessment scales assessing both vestibular-balance and psycho-physiological factors are absolutely necessary to diagnose the patient status and severity of the vertigo.[14] The Vertigo Symptoms Scale (VSS) is one of the most widely used self-assessment scales for evaluating patients with vestibular-balance symptoms. It was developed by Yardley et al. in 1992 from extensive interviews with patients who had had clinical experiences of vertigo. Their aim was to develop a self-reported measure of vertigo severity that was uncontaminated by anxiety-based symptoms.[12,15] This test seeks to categorize the prevalence and severity of dizziness symptoms over a period of 1 year. It contains two subscales: (1) the vertigo scale (VSS-VER) measuring symptoms primarily associated with vestibular system disorders; (2) the anxiety and autonomic symptom scale (VSS-AA) assessing a group of generic symptoms that can be due to autonomic arousal or somatic anxiety symptoms. The VSS has already been translated into different languages such as Spanish, Swedish,[16] German,[17] Turkish,[18] Japanese,[19] Malay,[20] Chinese,[21] Norwegian, Afrikaans[1] and Dutch,[20] without losing validity.
There is no validated VSS available in Persian; therefore, the aim of this study was to develop the VSS into Persian by adapting it cross-culturally after translation it into Persian, and to evaluate its psychometric parameters for the whole test and each subscale, separately.
MATERIALS AND METHODS
Translation and cross-cultural adaptation of the Vertigo Symptom Scale
First of all, permission was obtained from the original authors of VSS to translate the VSS. The translation and cross-cultural adaptation into Persian were performed according to the international guidelines for self-reported measures published by the American Association of Orthopedic Surgeons Outcomes Committee.[21] Then, to examine face validity and cross-cultural adaptation, the prefinal VSS-P was pilot-tested in both PVD patients and healthy groups, 15 people in each group.
Measures
Vertigo Symptom Scale
The VSS consists of 34 items and is a self-reported instrument that addresses the frequency and severity of dizziness symptoms within the last 12 months. Two primary subscales (VER and AA) assess symptoms of balance system dysfunction and symptoms of somatic anxiety and autonomic arousal. The VSS uses a five-point Likert scale: 0 (never), 1 (a few times), 2 (several times), 3 (quite often), and 4 (very often). The total score ranges from 0 to 136, and a higher score indicates a higher frequency of symptoms. Both the internal consistency and test-retest reliability of the original English version of the VSS have been established.[12,15]
Dizziness handicap inventory
The dizziness handicap inventory (DHI) is a 25-item, self-reported questionnaire that evaluates the impact of dizziness and/or vertigo on quality of life. The questionnaire has three subscales: physical (7 items), functional (9 items), and emotional (9 items). The items are responded with “yes” (4 points), “sometimes” (2 points), and “no” (0 points). The total score ranges from zero (no disability) to 100 (severe disability). Good validity, reliability, and internal consistency have been shown in the original version[13] and the Persian translation.[22]
Beck anxiety inventory
This well-validated questionnaire is a 21-question, multiple-choice, self-reported inventory that is used for measuring the severity of anxiety. This measurement asks about common symptoms of anxiety that the subject has had during the past month (such as numbness and tingling, cold sweating, and fear of the worst happening). It has been previously translated and validated in Persian.[23]
Participants and procedure
The study participants had been suffering from peripheral vestibular dysfunction (PVD) for at least a month; to detect abnormalities that would be indicative of PVD, patients attending the Amir Alam Hospital for vestibular evaluation were medically assessed by clinical history and objective tests such as cervical vestibular evoked myogenic potential, video head impulse test, electrocochleography, oculomotor function (smooth pursuit, saccade, and optokinetic), positional, positioning, and caloric irrigation tests. They should have the ability to complete at least 50% of their routine tasks, no blindness, no neurological disorder such as severe paresis and no psychiatric disorders. The exclusion criteria were being reluctant to or unable to continue cooperation.
The participants comprised 101 patients, with a chief complaint of dizziness and vertigo, referred to Amir Alam Hospital in Tehran as PVD group. Thirty-four people from the hospital staff participated in the study as a healthy group; they had no history of vertigo or hearing loss. All participants in both groups gave written informed consent. The study was approved by the Human Research Ethics Committee of Tehran University of Medical Sciences.
Statistical analysis
Statistical analysis was performed by SPSS (Version 17.0, SPSS Inc., Chicago, IL, USA). Cross-cultural adaptation and face validity scores for each item were examined through descriptive statistics. Internal validity was determined to establish that items assessing vertigo and those assessing somatic anxiety formed separate clusters; this was investigated by a principal components analysis with Varimax rotation. Moreover, factor analysis was also carried out with two fixed factors.
To determine discriminate validity, we used Mann–Whitney U-test to compare the median scores of VSS-P, VSS-VER, and VSS-AA between healthy and PVD groups. Furthermore, if the difference between mean scores for two groups was significant, receiver operating characteristic (ROC) curve was calculated. Convergent validity, the degree to which two measures of constructs that theoretically should be related, are in fact related, was investigated using Spearman's orrelations, and it measured the association of VSS-P, VSS-VER, and VSS-AA with Beck anxiety inventory (BAI) and DHI.
Test-retest reliability was calculated by a subsample (n = 30) with 24–48 h interval and reported as an interclass correlation coefficient (ICC). A value >0.7 was considered satisfactory.[24] In addition, the standard error of measurement (SEM) and the smallest detectable of change (SDC) are two reliability measures that assess response stability. SEM and SDC are calculated by standard deviation (SD) ×  and 1.96×
and 1.96×  , respectively. Internal consistency was tested by Cronbach's alpha.[25] Cronbach's alpha values >0.7 were considered good.[26]
, respectively. Internal consistency was tested by Cronbach's alpha.[25] Cronbach's alpha values >0.7 were considered good.[26]
RESULTS
Translation and cross-cultural adaptation
During different phases of translation, there were some differences in definitions, such as flickering, tingling, and disorientation. For “flickering” and “tingling,” the correct definition was selected by an optometrist and a physiotherapist. Regarding another word, some comments mentioned by the specialists in their meeting were chosen as being the most appropriate. Polling resulted in lower scores in items 2, 3, 4, 6, 10, 15, 19, and 22. The expert committee discussed each item and considered comments. Items 3 (”hot or cold spells”) and 4 (unsteadiness so severe that you fall) were adapted to Iranian culture. Items 6 (tension), 10 (fluttering), 19 (numbness), and 22 (about to black out) were revised, and a familiar word was chosen. According to the specialists, the form of items 1 (a–e), 7 (a–e), and 18 (a–e) were changed, and all were written in sentences. The face validity based on pilot study resulted in an acceptable score for each item, so there was no need for further adaptation. However, the most problematic issue in the pilot study was the method of filling in the questionnaire, with patients often asking for assistance. It was therefore attempted to write the initial instructions clearly, highlighting the frequency aspect.
Characteristics of study sample
Participants were included 62 females and 39 males in PVD group and 18 females and 16 males in healthy group. Mean age was 47.76 for the PVD group and 39.41 for the healthy group (SD 13.72 and 8.86, respectively).
Internal validity
A principal-components analysis (exploratory factor analysis) of the 34 items of the VSS identified eight factors with eigenvalues >1, which explained 71.88% of the variance in scores. To compare our results with other studies, we examined factor analysis by two fixed factors (confirmatory). It just covers 43.53 of the total variance. Tables 1 and 2 show the results for loading different items on each factor. Compared to the original subscales of the VSS, 79% (15/19) of the items clearly loaded on factor two. The remaining items, including 1a, 7a, 18a and 5, loaded on factor one, related to the anxiety subscale. Like in the original version, these items had been considered to be in the vertigo subscale because there was an association between the vestibular system and the VSS-AA system. Besides, nausea and a short duration of vertigo are mainly seen in vestibular disorders (especially in benign paroxysmal positional vertigo). This means they have high face validity for the vertigo subscale. Hence, in the VSS-P, the subscale structure was maintained as in the original version.
Table 1.
Factor analyzing with two fixed factors for vertigo subscale
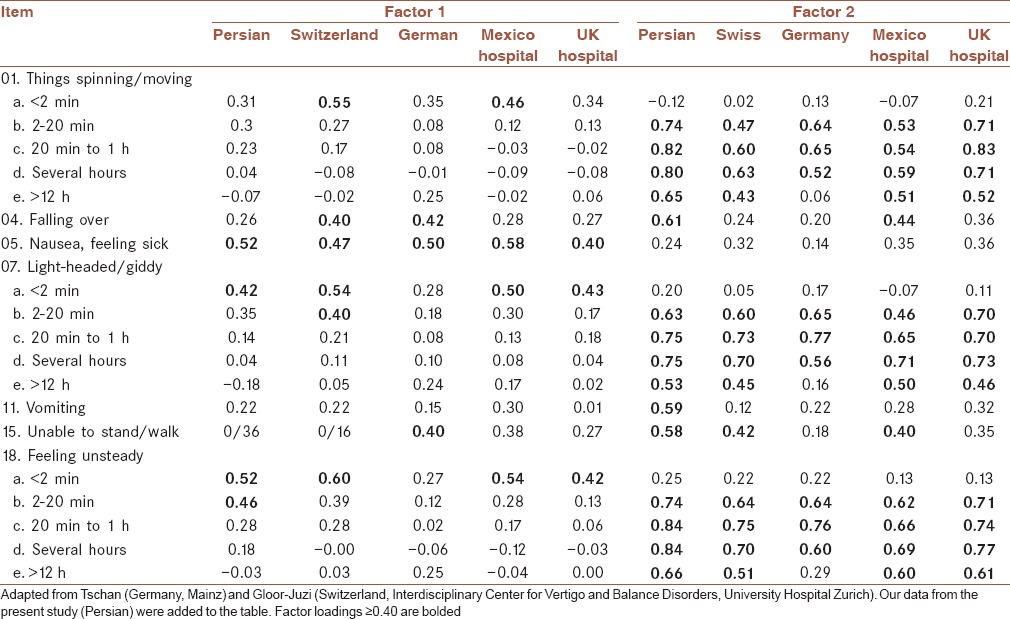
Table 2.
Factor analyzing with two fixed factors for anxiety subscale
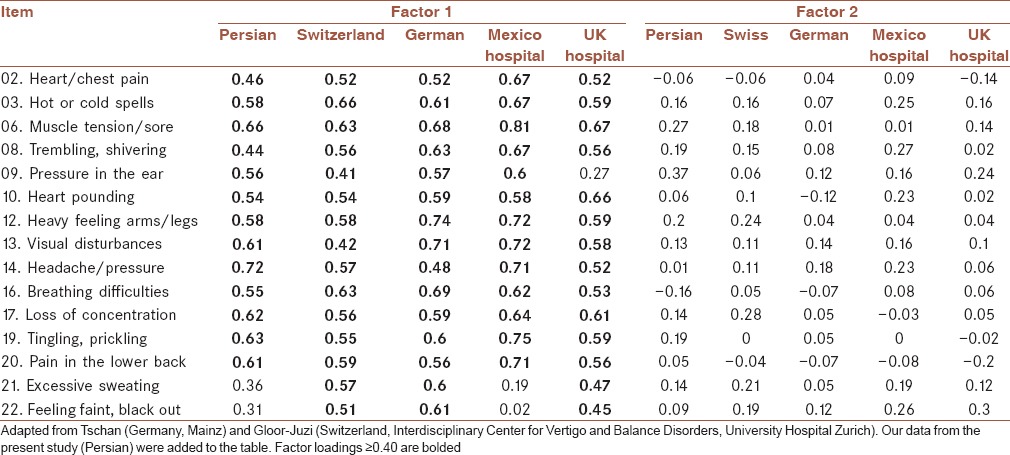
After rotation, most of the elements in the original VSS-AA subscale loaded onto the VSS-AA subscale based on loading > 0.4. Items 21 and 22 also loaded more on the anxiety subscale rather than the VSS-VER. Based on this high face validity and the overlap between vestibular and autonomic/anxiety symptoms, the original subscale structure was kept for the VSS-P.
Discriminate validity
Data statistics is shown in Table 3. The mean total score was 8.23 for the healthy group and 27.62 for the PVD. Statistically, there was a significant difference between the two groups (P < 0.001). For both the VSS-VER and VSS-AA subscales, the Mann–Whitney U-test revealed a significant difference between the two groups; P < 0.001 and P = 0.03, respectively. Apparently, VSS can distinguish between the patient and healthy groups.
Table 3.
Data statistics for both peripheral vestibular dysfunction and healthy groups
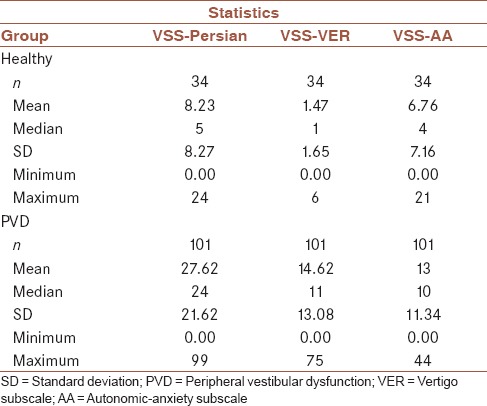
A ROC curve was used to explore the ability to discriminate between the normal and PVD groups as well.
According to the ROC curve [Figure 1], the VSS-P was a good instrument to identify PVD, with a cutoff value of 10.5 (sensitivity: 0.85 and specificity: 0.74). The vertigo subscale was able to distinguish normal from PVD group as well, with a cutoff of 4.5 (sensitivity: 0.88 and specificity: 0.97). However, the anxiety subscale's ability to distinguish was not as great as the others, and the area under the curve was smaller (cutoff value: 5.5, sensitivity: 0.64 and specificity: 0.62).
Figure 1.
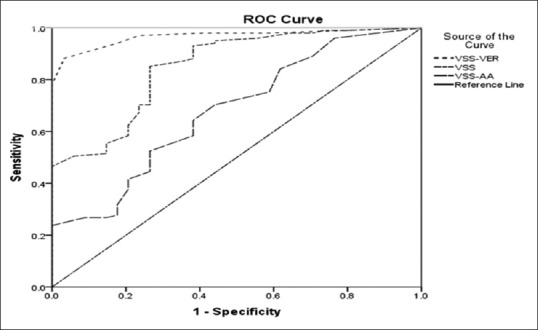
Receiver operating characteristic curve for discrimination between dizzy patients and healthy subjects. VSS = Vertigo Symptom Scale; VSS-VER = Vertigo subscale; VSS-AA = Autonomic-anxiety subscale
Convergent validity
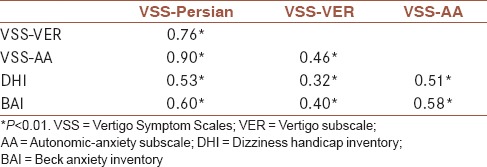
Spearman's orrelations analyzed VSS-P and its subscales to investigate the association with DHI and BAI. The correlation between VSS-P and its subscales with other measurements is shown in Table 4. VSS-P had a moderate relationship with both DHI and BAI (r: 0.53 and 0.60, respectively). Both of the BAI and DHI had a higher correlation with Anxiety subscale than vertigo.
Table 4.
Intercorrelations between Vertigo Symptom Scales-Persian, anxiety and disability in dizzy patients (n=101)
Reliability
Test-retest reliability was determined by thirty patients after an interval of 1–2 days. To assess the reliability, the intraclass correlation coefficient was excellent for both subscales and total single measures; ICC was 0.89, 0.86, and 0.91 for VSS-AA, VSS-VER, and overall VSS, respectively.
The SEM obtained 4.88, 3.76, and 6.48 for vertigo, anxiety subscales and the total score, respectively. SDC was 7.05, 6.12, and 5.37 for the total VSS, vertigo and anxiety subscales, respectively, showing that if an individual patient's ondition has really changed, the total score must change at least 7.05 scores.
Internal consistency
Internal consistency was identified by Cronbach's alpha, which determines how closely related a set of items are as a group, and it was measured as being 0.90 for the VSS-VER, 0.86 for the VSS-AA and 0.92 for the overall VSS in PVD group. Internal consistency was excellent for the total score and each of its individual subscales.
DISCUSSION
VSS was translated and cross-culturally adapted into Persian. The translation had been done without serious problem; the semantic and technical equivalence of items was kept as close as possible to the original version. Our finding shows that the VSS-P has good reliability and validity. In addition, it is able to distinguish between patients and healthy groups.
It is one of the most used questionnaires and translated into different languages.[1,17,18,19,20,21,27] There were different methods for translating questionnaires. Similar to German version of the VSS, we chose the guideline based on the American Association of Orthopedic Surgeons Outcomes Committee.[17]
Internal validity
VSS consists of two dimensions: VER/balance and AA.[12] In factor analysis with Varimax rotation, the pattern of items loading were similar to others samples such as the primary care,[28] UK hospital,[12] Mexico City,[27] and German samples.[17] In Persian version of the VSS, the two-factor structure was supported as well. In our study, nausea and vertigo and dizziness symptoms lasting <2 min loaded on anxiety subscale. The cross-loaded items are not uncommon because of the overlapping between symptomatology related to VER-balance and AA. These items were considered into VSS-VER subscale as they are common complaints among vertiginous patients. In some studies, in addition to short duration vertigo and dizziness, vomiting, falling, and being unable to stand or walk were cross-loaded; however, they tried to keep the original structures as well.[17,28]
Discriminate validity
Determining the cutoff values is useful in identifying the patients from healthy individuals. In our study, the VSS-VER subscale had the highest discriminative quality with cutoff value 4.5, like the Germen version.[17] According to this value, 12 patients misclassified as normal. Although their vertigo severity scores were not very high, they had a confirmed PVD that may affect their lives. Therefore, their limitations and decreased quality of their daily life should be considered in the treatment plan. VSS-AA subscale was not a robust measure to discriminate between vertiginous patients and healthy individuals. This was maybe due to the fact that the healthy group had some degree of somatic expression of anxiety symptoms, such as low back pain and muscular tension/soreness. However, patients with high level of anxiety could be detected by this subscale; further research may be needed to clarify discriminative properties.
Convergent validity
Convergent validity was established by comparison of scale scores with independent measures of anxiety and handicap. BAI and DHI previously were translated into Persian.[22,23] Correlation between VSS-P and DHI revealed the impact of the severity of symptoms on the limitation of daily activities. These findings are comparable to the German and Norwegian version of the VSS.[17] Higher correlation between measures of anxiety and VSS-AA subscale and lower correlation with VSS-VER subscale confirmed that VSS was truly developed as an instrument for measuring vertigo severity that is not affected by anxiety symptoms.[12] Tschan et al. had reported weaker correlation with emotional distress that affects the level of patient's participation in society, for the VSS-VER subscale than for the VSS-AA.[10]
Both VSS-AA and VSS-VER subscales were correlated with dizziness handicap. It shows that symptoms can cause disability and handicap. The model of relationship between vertigo symptoms, anxiety and handicap had been constructed previously, but underlying mechanisms are not very clear.[12,29] The symptoms can affect quality of life as well. Identifying the severity of symptoms can be predictor of the level of handicap. In comparison to vestibular tests, VSS is used to predict the severity of the symptoms of vertigo, because the VSS cumulatively investigates the symptoms experienced over a period up to 12 months, while the objective tests demonstrate the status of the patient only in the time of evaluation. Thus, the VSS is a more sensitive measure indicative of the patient status.
Reliability and internal consistency
Similar to the original version of VSS, high internal consistency and acceptable test-retest reliability were shown for the VSS-P that indicates it is a reliable instrument for clinical use. The alpha values for VSS and its subscales were within recommended limits.[12,26]
CONCLUSION
The Persian version of VSS was developed for clinical use. The VSS-P had good sensitivity and specificity and therefore demonstrates satisfactory discriminative ability in differentiating vertiginous from anxious patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article is emerged from A. Kamalvand's MSc thesis in Audiology submitted to Tehran University of Medical Sciences. The authors appreciated Dr. Nehzat Koohi and Dr. Diego Kaski from London University, UK, for critically revision of the back-translated version of the VSS.
REFERENCES
- 1.Rogers C, de Wet J, Gina A, Louw L, Makhoba M, Tacon L. The translation of the vertigo symptom scale into afrikaans: A pilot study. S Afr J Commun Disord. 2011;58:6–12. doi: 10.4102/sajcd.v58i1.36. [DOI] [PubMed] [Google Scholar]
- 2.Lee AT. Diagnosing the cause of vertigo: A practical approach. Hong Kong Med J. 2012;18:327–32. [PubMed] [Google Scholar]
- 3.Hogue JD. Office evaluation of dizziness. Prim Care. 2015;42:249–58. doi: 10.1016/j.pop.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Susanto M. Dizziness: If not vertigo could it be cardiac disease? Aust Fam Physician. 2014;43:264–9. [PubMed] [Google Scholar]
- 5.Newman-Toker DE, Hsieh YH, Camargo CA, Jr, Pelletier AJ, Butchy GT, Edlow JA. Spectrum of dizziness visits to US emergency departments: Cross-sectional analysis from a nationally representative sample. Mayo Clin Proc. 2008;83:765–75. doi: 10.4065/83.7.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kroenke K, Hoffman RM, Einstadter D. How common are various causes of dizziness? A critical review. South Med J. 2000;93:160–7. [PubMed] [Google Scholar]
- 7.Wiltink J, Tschan R, Michal M, Subic-Wrana C, Eckhardt-Henn A, Dieterich M, et al. Dizziness: Anxiety, health care utilization and health behavior – results from a representative German community survey. J Psychosom Res. 2009;66:417–24. doi: 10.1016/j.jpsychores.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 8.Best C, Eckhardt-Henn A, Diener G, Bense S, Breuer P, Dieterich M. Interaction of somatoform and vestibular disorders. J Neurol Neurosurg Psychiatry. 2006;77:658–64. doi: 10.1136/jnnp.2005.072934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacob RG, Furman JM. Psychiatric consequences of vestibular dysfunction. Curr Opin Neurol. 2001;14:41–6. doi: 10.1097/00019052-200102000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Tschan R, Wiltink J, Best C, Bense S, Dieterich M, Beutel ME, et al. Validation of the German version of the vertigo symptom scale (VSS) in patients with organic or somatoform dizziness and healthy controls. J Neurol. 2008;255:1168–75. doi: 10.1007/s00415-008-0863-1. [DOI] [PubMed] [Google Scholar]
- 11.Best C, Tschan R, Eckhardt-Henn A, Dieterich M. Who is at risk for ongoing dizziness and psychological strain after a vestibular disorder? Neuroscience. 2009;164:1579–87. doi: 10.1016/j.neuroscience.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 12.Yardley L, Masson E, Verschuur C, Haacke N, Luxon L. Symptoms, anxiety and handicap in dizzy patients: Development of the vertigo symptom scale. J Psychosom Res. 1992;36:731–41. doi: 10.1016/0022-3999(92)90131-k. [DOI] [PubMed] [Google Scholar]
- 13.Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990;116:424–7. doi: 10.1001/archotol.1990.01870040046011. [DOI] [PubMed] [Google Scholar]
- 14.Yardley L, Barker F, Muller I, Turner D, Kirby S, Mullee M, et al. Clinical and cost effectiveness of booklet based vestibular rehabilitation for chronic dizziness in primary care: Single blind, parallel group, pragmatic, randomised controlled trial. BMJ. 2012;344:e2237. doi: 10.1136/bmj.e2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yardley L, Todd A, Lacoudraye-Harter M, Ingham R. Psychosocial consequences of recurrent vertigo. Psychol Health. 1992;6:85–96. [Google Scholar]
- 16.Mendel B, Bergenius J, Langius A. Dizziness symptom severity and impact on daily living as perceived by patients suffering from peripheral vestibular disorder. Clin Otolaryngol Allied Sci. 1999;24:286–93. doi: 10.1046/j.1365-2273.1999.00261.x. [DOI] [PubMed] [Google Scholar]
- 17.Gloor-Juzi T, Kurre A, Straumann D, de Bruin ED. Translation and validation of the vertigo symptom scale into German: A cultural adaption to a wider German-speaking population. BMC Ear Nose Throat Disord. 2012;12:7. doi: 10.1186/1472-6815-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yanik B, Külcü DG, Kurtais Y, Boynukalin S, Kurtarah H, Gökmen D. The reliability and validity of the vertigo symptom scale and the Vertigo Dizziness Imbalance Questionnaires in a Turkish patient population with benign paroxysmal positional vertigo. J Vestib Res. 2008;18:159–70. [PubMed] [Google Scholar]
- 19.Kondo M, Kiyomizu K, Goto F, Kitahara T, Imai T, Hashimoto M, et al. Analysis of vestibular-balance symptoms according to symptom duration: Dimensionality of the vertigo symptom scale-short form. Health Qual Life Outcomes. 2015;13:4. doi: 10.1186/s12955-015-0207-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zainun Z, Zakaria MN, Sidek D, Ismail Z. Clinical use of Malay version of vertigo symptom scale (MWSS) in patients with peripheral vestibular disorder (PVD) Med J Malaysia. 2012;67:386–9. [PubMed] [Google Scholar]
- 21.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000;25:3186–91. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 22.Jafarzadeh S, Bahrami E, Pourbakht A, Jalaie S, Daneshi A. Validity and reliability of the Persian version of the dizziness handicap inventory. J Res Med Sci. 2014;19:769–75. [PMC free article] [PubMed] [Google Scholar]
- 23.Kaviani H, Mousavi A. Psychometric properties of the Persian version of Beck Anxiety Inventory (BAI) Tehran Univ Med J. 2008;66:136–40. [Google Scholar]
- 24.Lewsey J. Medical statistics: A guide to data analysis and critical appraisal. Ann R Coll Surg Engl. 2006;88:603. [Google Scholar]
- 25.Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63:737–45. doi: 10.1016/j.jclinepi.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Streiner DL, Norman GR, Cairney J. Health Measurement Scales: A Practical Guide to Their Development and Use. USA: Oxford University Press; 2014. [Google Scholar]
- 27.Yardley L, Medina SM, Jurado CS, Morales TP, Martinez RA, Villegas HE. Relationship between physical and psychosocial dysfunction in Mexican patients with vertigo: A cross-cultural validation of the vertigo symptom scale. J Psychosom Res. 1999;46:63–74. doi: 10.1016/s0022-3999(98)00056-7. [DOI] [PubMed] [Google Scholar]
- 28.Yardley L, Beech S, Zander L, Evans T, Weinman J. A randomized controlled trial of exercise therapy for dizziness and vertigo in primary care. Br J Gen Pract. 1998;48:1136–40. [PMC free article] [PubMed] [Google Scholar]
- 29.Yardley L, Putman J. Quantitative analysis of factors contributing to handicap and distress in vertiginous patients: A questionnaire study. Clin Otolaryngol Allied Sci. 1992;17:231–6. doi: 10.1111/j.1365-2273.1992.tb01833.x. [DOI] [PubMed] [Google Scholar]


