Keywords: nerve regeneration, dyspepsia, acupoint combination, acupuncture, traditional Chinese medicine, neuromechanism, functional magnetic resonance imaging, clinical trial, protocol, neural regeneration
Abstract
Acupuncture is widely used to treat functional dyspepsia with satisfactory outcomes. Combination of the He and Mu acupoints is commonly used and has a synergistic effect on functional dyspepsia; however, its underlying mechanisms remain unclear. Therefore, a randomized controlled parallel clinical trial is currently underway at Chengdu University of Traditional Chinese Medicine, China. This trial is designed to explore the efficacy of and central responses to the He-Mu point combination in patients with functional dyspepsia using functional magnetic resonance imaging. A total of 105 patients with functional dyspepsia will be allocated into 3 groups: the low-He point group (puncturing at Zusanli (ST36)), Mu point group (puncturing at Zhongwan (CV12)), and He-Mu point combination group (puncturing at ST36 and CV12). Every participant will receive 20 sessions of manual acupuncture for 4 weeks. The needles will be inserted perpendicularly to a depth of 1 to 2 cun. The angle of rotation and twisting will range from 90 to 180 degrees, while lifting and thrusting will range from 0.3 to 0.5 cm. The various manipulations will be performed 60 to 90 times per minute. The needles will remain in place for 30 minutes, during which manipulation will be applied every 10 minutes. Magnetic resonance imaging will be performed before and after 20 sessions of acupuncture. The primary outcome is symptom improvement according to the Chinese version of the Nepean Dyspepsia Index. Secondary outcomes include the Leeds dyspepsia questionnaire, Self-Rating Anxiety Scale, Self-Rating Depression Scale, Beck Anxiety Inventory, Beck Depression Inventory, and visual analogue scale scores before and after 10 and 20 sessions of acupuncture. Needle sensation and adverse events will be used to assess the therapeutic effects. This study will promote more widespread awareness of the benefits of acupoint combination in the clinical setting and provide a further explanation of the neuromechanism by which acupuncture at the He-Mu point combination for functional dyspepsia. Registration: Chinese Clinical Trial Registry, ChiCTR-IOR-15006402.
Introduction
Functional dyspepsia, one of the most frequently reported functional gastrointestinal disorders, is characterized by abdominal discomfort, pain, early satiety, abdominal distension, belching, and nausea without organic or metabolic pathology (Kumar et al., 2012; Tack and Talley, 2013). Although functional dyspepsia is not life-threatening, it has became an important public health issue worldwide because of its high prevalence (Mahadeva and Goh, 2006), detrimental effects on health-related quality of life (QOL) (Filipović et al., 2013) and work productivity (Sander et al., 2011), and association with high health care costs (Lacy et al., 2013). Epidemiological surveys have shown that the prevalence of functional dyspepsia ranges from 10% to 30% worldwide (Mahadeva and Goh, 2006). Approximately 20.0% to 25.0% of cases occur in Western countries (Voiosu et al., 2013) while 24.4% occur in China (Jiang et al., 2015). Each patient with functional dyspepsia incurs a direct cost of $699 in medical costs each year (Lacy et al., 2013). Medications such as antacids, prokinetics, and antidepressants seem to be the most common choices for treatment of functional dyspepsia. However, their efficacy remains unsatisfactory because of the multifactorial etiology of functional dyspepsia (Camilleri and Stanghellini, 2013; Chen, 2013), and their side effects are problematic (Bielefeldt, 2014). Therefore, both patients and doctors desire more effective and safe therapies.
Acupuncture has been widely accepted for management of gastrointestinal disorders in China for thousands of years and has been gradually recognized as a complementary therapy in non-oriental cultures as well (Takahashi, 2006; Kondo and Kawamoto, 2014; Rafiei et al., 2014; Lee et al., 2015). Evidence from clinical trials has demonstrated that acupuncture treatment can improve the symptoms and QOL of patients with functional dyspepsia, and acupoints related to the stomach are the most effective sites (Ma et al., 2012; Lima et al., 2013; Lan et al., 2014; Li et al., 2014). Clinically, acupoints are not used singly; instead, their combinations are crucial for acupuncture effectiveness because various acupoints trigger synergistic effects when stimulated together. Previous studies on acupoint combinations have demonstrated that the combination of Jueyinshu (BL14) and Danzhong (RN17) is more effective than a single acupoint for coronary arteriosclerotic heart disease (Wang, 2005), and the combination of Feishu (BL13) and Zhongfu (LU1) is more effective than a single acupoint for improving pulmonary function (Kong et al., 2004). Thus, it has been confirmed that synergistic effects can be produced by acupoint combinations. In light of traditional acupuncture theory and clinical experience (Ren et al., 2009; Hu and Wang, 2013), the He-Mu point combination (Zusanli and Zhongwan) is the most frequently used acupoint combination for treatment of functional dyspepsia (Han, 2003; Ji et al., 2008). Zusanli (ST36, the low-He point of the stomach) is the most important point for gastrointestinal problems, and Zhongwan (CV12, the Mu point of the stomach) effectively regulates gastric function. These points are often used in combination rather than singly for better efficacy (Geng et al., 2015). However, the underlying mechanism of their synergistic effect remains unclear and worthy of further study.
With the development of functional neuroimaging techniques, increasing numbers of studies have reported that brain function anomalies and injuries play an important role in the pathophysiology of functional dyspepsia (Huang et al., 2013; Lee et al., 2016). A systematic review showed that functional dyspepsia is associated with functional abnormalities in the sensory and pain modulation, emotion, saliency, and homeostatic processing regions (Lee et al., 2016). Many acupuncture neuroimaging studies have indicated that acupuncture can help to normalize the abnormal brain function and metabolism in patients with functional dyspepsia. For example, one study demonstrated that the relief of gastrointestinal signs and symptoms by acupuncture is likely due to normalization of functional connectivity in the brain (Fang et al., 2015). Another study involving positron emission tomography–computed tomography indicated that acupuncture can produce deactivations in the brain stem, anterior cingulate cortex, insula, thalamus, and hypothalamus, thus relieving symptoms (Zeng et al., 2012). Our previous study showed that key regions (anterior cingulate cortex, insula, thalamus, and hypothalamus) determine the severity of symptoms in patients with functional dyspepsia and that the mechanism of acupuncture involved specific and targeted brain function modulation in these key regions (Zeng et al., 2011, 2012, 2015). Other studies have revealed that the central integration of acupoint combinations does not involve central activity superposition of single acupoints but instead involves the restructuring of brain function (Wang, 2012). Therefore, we hypothesized that compared with the low-He point or Mu point alone, the He-Mu point combination will be more effective because of specific brain function modulation.
This study is designed to investigate the efficacy and central activity of puncturing at the He-Mu point combination versus at single acupoints for treatment of functional dyspepsia.
Design and Methods
Design
This is a clinical neuroimaging study focusing on the central mechanism of puncturing at the He-Mu point combination for treatment of functional dyspepsia.
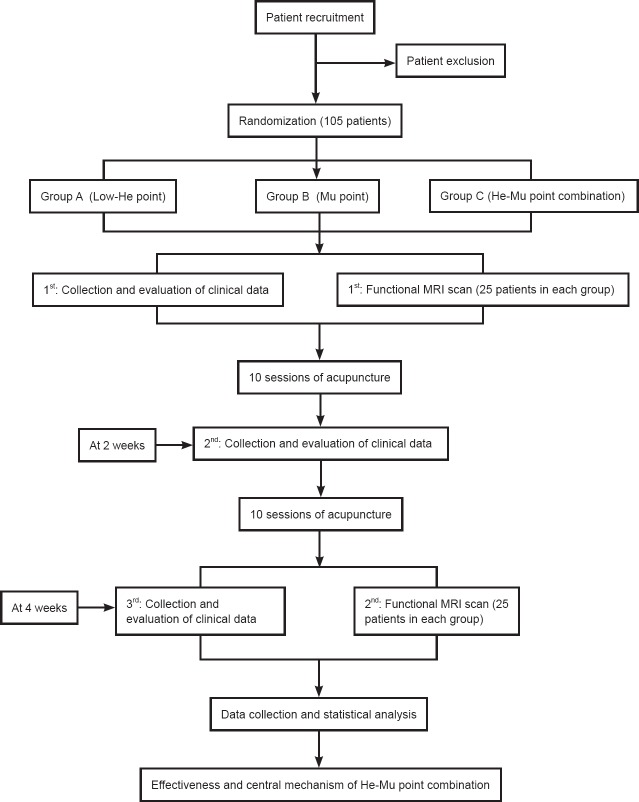
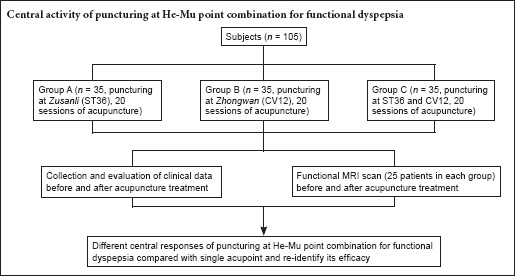
A total of 105 patients diagnosed with postprandial distress syndrome (a subset of functional dyspepsia) in accordance with the Rome III Diagnostic Criteria for Functional Gastrointestinal Disorders will be considered as eligible patients. These 105 participants will be randomly allocated into 3 equal groups of 35 patients each: Group A (puncturing at ST36, low-He point), Group B (puncturing at CV12, Mu point), and Group C (puncturing at ST36 and CV12, He-Mu point combination). All patients will undergo 20 manual acupuncture sessions during a 4-week period; the technique will depend on the treatment group to which they are assigned. Outcome measurements will be assessed at baseline and after 10 and 20 acupuncture sessions. Twenty-five randomly selected patients from each group will undergo functional magnetic resonance imaging (fMRI) scans before and after the acupuncture treatment (Figure 1). The effectiveness and central mechanism of the He-Mu point combination versus the low-He point alone or the Mu point alone for treatment of functional dyspepsia will be analyzed after data collection.
Figure 1.
Flow chart of the trial.
Patients
Patients diagnosed with postprandial distress syndrome (a subset of functional dyspepsia) will be recruited from the First Affiliated Hospital of Chengdu University of Traditional Chinese Medicine and the campus of Chengdu University of Traditional Chinese Medicine, China.
Inclusion criteria
Patients will be included if they (1) are right-handed and aged 18 to 45 years, (2) match the Rome III criteria (Tack and Talley, 2013) for functional dyspepsia and postprandial distress syndrome, (3) have not taken any gastrointestinal dynamic medicine or received acupuncture treatment during the last 15 days, and (4) provide written informed consent.
Exclusion criteria
Patients will be excluded if they (1) are pregnant or lactating, (2) have a history of head trauma with loss of consciousness or gastrointestinal surgery, (3) have diabetes or serious cardiovascular, neurological, psychiatric, renal, or respiratory diseases, (4) have used aspirin, steroids, phenothiazines, nonsteroidal anti-inflammatory drugs, selective serotonin-reuptake inhibitors, medication affecting gastrointestinal motility, or other drugs at least 15 days before enrollment, (5) have any contraindications to acupuncture, such as hemorrhagic disorders or excessive weakness, (6) have any contraindications to fMRI scanning, such as the presence of a cardiac pacemaker, defibrillator, metal stent, or electronic device in the body or an intraocular metal foreign body, claustrophobia, or hyperpyrexia.
This study protocol has been approved by the supervision of the Sichuan Regional Ethics Review Committee on Traditional Chinese Medicine (ethical approval number 2014KL-028). This study will be performed according to the guidance and principles of the Declaration of Helsinki. The authors retain full control of the manuscript content.
Sample size
Because there is no reference on the expected effect size of using acupuncture to treat postprandial distress syndrome, the subtype of functional dyspepsia evaluated in this study, we did not estimate the sample size based on a power calculation. Instead, we enrolled 105 participants with a 15% expected withdrawal rate to provide 30 participants in each group, meeting the requirement for the minimum sample size.
In previous studies of fMRI, 12 to 15 patients per group provided statistical power (Desmond and Glover, 2002; Hayasaka et al., 2007). In our previous study (Qiu et al., 2016), we found that the average sample size in acupuncture neuroimaging studies was 15 patients per group and that the average sample size for patients (16 per group) was slightly greater than that for healthy subjects (14 per group). Considering the principle of nonmaleficence in ethics and our available research funds, we require 16 participants to undergo an fMRI scan in each group to investigate the different central responses of puncturing at different acupoints. Because some participants may be excluded due to excessive head motion during scanning, we must increase the sample size to 20. Finally, considering a 20% dropout rate, the required sample size is 25 participants in each group.
Recruitment
Hospital recruitment
Doctors in the outpatient and inpatient departments of gastroenterology in the First Affiliated Hospital of Chengdu University of Traditional Chinese Medicine will help to recruit patients. Patients with interest in the study will undergo a basic evaluation. Those who decide to participate, satisfy the criteria, and provide written informed consent will undergo further examination and acupuncture treatment.
Campus recruitment
Printed recruitment posters will be posted on the campus of Chengdu University of Traditional Chinese Medicine, and researchers will deliver leaflets to students. Patients with interest will contact the trial personnel. The following steps are the same as the hospital recruitment.
Informed consent
First, we will provide all patients with the details of the trial schedule, potential benefits and adverse events of treatment, and responsibilities of the researchers and participants. Written informed consent will be obtained from all participants prior to randomization in the study. Moreover, before every visit, a researcher will contact the patient to reconfirm the consent. The patients will be free to withdraw from the study at any time without a specific reason and without any penalty or loss of benefits. However, we will attempt to understand the reason for withdrawal and encourage the participant to remain in the study if possible.
Randomization
Randomization will consist of (1) random assignment of the 105 participants into 3 groups and (2) random selection of 25 participants from each group to undergo fMRI scans. The randomization will be carried out using random number lists created in accordance with PROC PLAN of SAS 9.2 (SAS Institute Inc., Cary, NC, USA) by an independent statistician and concealed from the researchers until completion of the statistical analysis. If a patient meets the inclusion criteria, the researcher will use a mobile telephone to send randomization information to the data manager. This randomization information will include the participant's name, sex, and birthdate. A random number and group assignment and information on whether the patient will undergo fMRI will then be sent from the data manager to the researcher via a short message. This procedure will ensure adequate randomization concealment.
Blinding
The acupuncturists, who will be asked to apply the same method of stimulation to each patient, will not be blinded to the treatment allocation for the different locations and number of acupoints in each group. The treatment will be revealed to the acupuncturists before treatment. We will inform the patients that three types of acupuncture treatment used in clinical practice will be provided in this study. They will accept one of them in a separate small room; each patient will know the type of acupuncture that they accepted, but they will not know the other two types. The evaluators and statisticians will be blind to the group allocation during outcome evaluation and data analysis to reduce the risk of bias.
Intervention
The acupuncture treatments will be performed in different small rooms by two licensed acupuncturists with more than 6 years of clinical experience. Manual acupuncture treatment will be administered using disposable sterile stainless steel needles (25–40 × 0.25 mm; Suzhou Hua Tuo Medical Instrument Co., Ltd., China). ST36 will be used in Group A (low-He point group), CV12 will be used in Group B (Mu point group), and both ST36 and CV12 will be used in Group C (He-Mu point combination group). ST36 will be punctured unilaterally, alternating between the left and right. The locations of the acupoints are shown in Figure 2.
Figure 2.
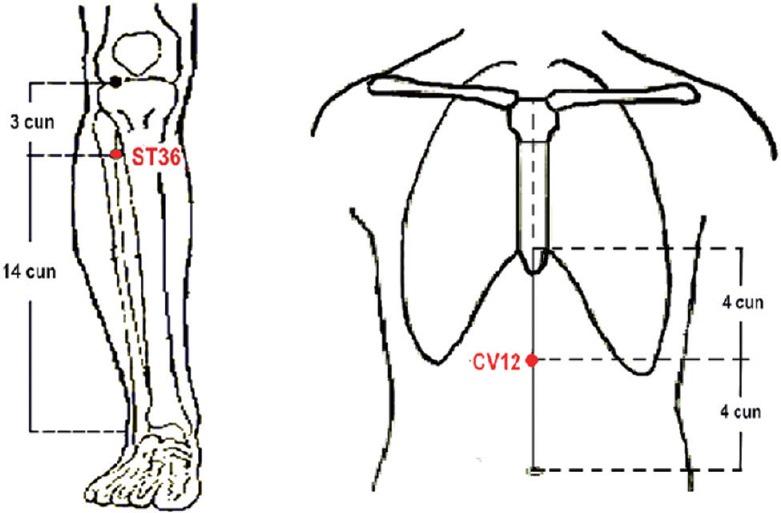
Acupoint locations of He-Mu point combination.
Zusanli (ST36): on the anterior lateral side of the shank, 3 cun below Dubi (ST35), one horizontally placed finger distance lateral to the anterior border of the tibia. Zhongwan (CV12): on the anterior median line of the upper abdomen, 4 cun above the navel.
The needles will be inserted perpendicularly to a depth of 1 to 2 cun (a special length-measuring unit in traditional Chinese medicine) with the patient lying down after skin sterilization; this will be followed by bidirectional rotation and twisting, lifting, and thrusting to induce Deqi sensation (arrival of qi). The angle of rotation and twisting will ranged from 90 to 180 degrees, while lifting and thrusting will range from 0.3 to 0.5 cm. The frequency of rotations and twisting manipulations and of lifting and thrusting manipulations will be 60 to 90 times per minute. The needles will be left in place for 30 minutes, during which manipulation will be applied every 10 minutes. Every patient will receive five treatments per week for 4 weeks.
Before enrollment, we will evaluate the severity of disease to exclude patients with severe symptoms. We will expect all patients to stop any medication being taken for symptomatic relief of functional dyspepsia during the acupuncture treatment and accept the usual care for functional dyspepsia. Nevertheless, the patients will be permitted to treat acute stomach disorders as required, and the type and dosage of all medications used will be recorded in the case report form. If their condition worsens, they will be withdrawn from the study and recommended to undergo evaluation by gastrointestinal disease specialists.
MRI data acquisition
MRI data will be acquired with a 3.0T magnetic resonance scanner (Siemens, Munich, Germany) at the MRI Center, West China Hospital, China before and after treatment. The patients will be instructed to maintain their regular lifestyle and avoid staying up late, alcohol, tobacco, tea, and coffee for 24 hours before the scan; they will also be required to withstand the prolonged duration and high noise of the scan Each patient will have a 30-minute rest period in the waiting room prior to the scan. The patients will be instructed to remove all metal items and place them on the examination table, keep their head fixed with the pressurized pad, close their eyes, stay awake, and think nothing during the scan. A technician of the MR Research Center shall manage the scan conditions, including the temperature (18–22°C), humidity (> 60%), and noise (< 150 decibels). The scan will consisted of two parts: acquisition of a high-resolution structural image using a three-dimensional MRI sequence and acquisition of a blood oxygenation level-dependent resting-state functional image. The three-dimensional structural image parameters will be as follows: repetition time/echo time = 1,900 ms/2.26 ms, slices = 176, data matrix = 256 × 256, field of view = 256 × 256 mm2, and slice thickness = 1 mm. The functional image parameters will be as follows: repetition time/echo time = 2,000 ms/30 ms, flip angle = 90°, slices = 30; data matrix = 64 × 64, field of view = 240 × 240 mm2, slice thickness = 5 mm, total volume = 180, and total scan time = 360 seconds.
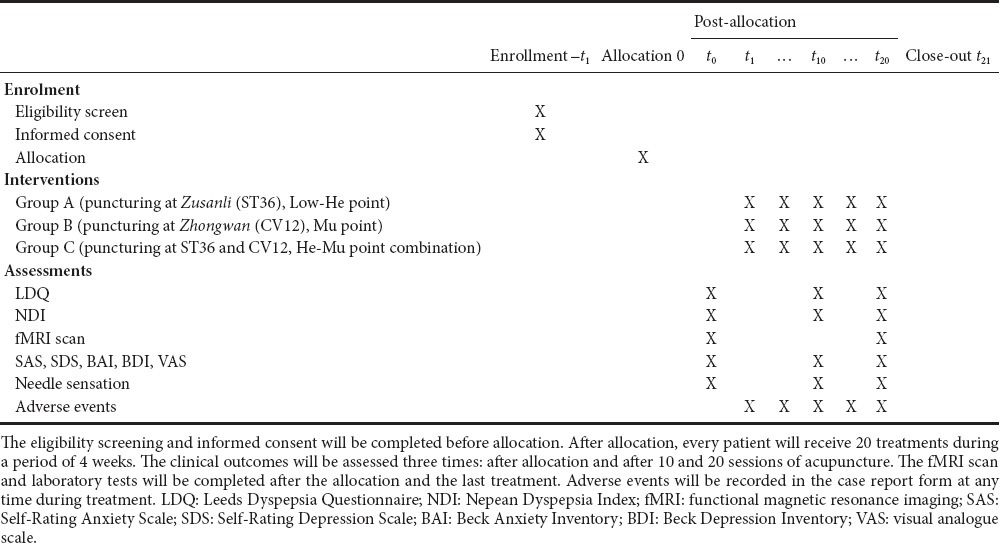
Outcome measurement
The clinical evaluations will comprise four parts: the Leeds Dyspepsia Questionnaire, Nepean Dyspepsia Index, emotion, and needle sensation. All evaluations will be performed three times: after randomization and after 10 and 20 acupuncture sessions. However, the Leeds Dyspepsia Questionnaire will be only administered twice after randomization and treatment. The 25 participants from each group who are randomly selected for fMRI will undergo the scans before and after acupuncture treatment.
Primary outcome
The primary outcome will be the Chinese version of the Nepean Dyspepsia Index (Talley et al., 1999). The Nepean Dyspepsia Index is a dyspepsia-specific index used to measure the impairment of QOL over the prior 14 days. The symptom checklist measures the frequency, intensity, and level of discomfort of 15 upper gastrointestinal symptoms. The QOL checklist includes four aspects: interference (13 items), know/control (7 items), eat/drink (3 items), and sleep/disturb (2 items). Higher scores indicate more severe symptoms and poorer QOL.
Secondary outcomes
The secondary outcomes will be the Leeds Dyspepsia Questionnaire score (Moayyedi et al., 1998), emotion, and needle sensation.
The Leeds Dyspepsia Questionnaire contains eight questions, each with two items, related to the frequency and severity of dyspeptic symptoms over the previous 1 month; the scores range from 0 to 40. It also contains one question regarding the most troublesome symptom for the patient. The higher the score of all symptoms, the more or severe the symptom is.
The patients will be required to complete the following four scales for emotional evaluation: the Self-Rating Anxiety Scale (Zung, 1971), the Self-Rating Depression Scale (Zung, 1965), the Beck Anxiety Inventory (Beck et al., 1988), and the Beck Depression Inventory (Beck et al., 1961). Both the Self-Rating Anxiety Scale and the Self-Rating Depression Scale comprise 20 items. Each item is scored from 1 to 4. According to the Chinese norm (Wang et al., 1986), an index score of the Self-Rating Anxiety Scale (calculated by multiplying the raw score by 1.25) of < 50 or an index score of the Self-Rating Depression Scale (calculated by multiplying the raw score by 1.25) of < 53 falls within the normal range. Both the Beck Anxiety Inventory and Beck Depression Inventory comprise 21 items. Each item of the Beck Anxiety Inventory is scored from 1 to 4, and a total score of < 45 is considered normal. The Beck Depression Inventory is scored from 0 to 3, and a total score of < 13 is considered normal.
The 10-point visual analogue scale (Wewers and Lowe, 1990) will be used to evaluate needle sensation (deqi) after acupuncture stimulation in the study. This is a 10-cm scale containing the anchor words “none,” “mild,” “moderate,” “severe,” and “unbearable” spaced along the continuum. The scale includes five descriptors of typical deqi sensations: soreness, numbness, fullness, heaviness, and aching as well as one blank row for patients to add their own words if the scale does not adequately describe the sensations they experienced. The patients will assess these sensations and their anxiety using this 10-point visual analogue scale.
Patient safety
Adverse events caused by acupuncture, such as pain, bleeding, fainting, or other severe events, will be processed immediately and recorded in detail in the case report form. Table 1 provides a complete overview of the time schedule of the enrollment, interventions, and assessments.
Table 1.
Time schedule of enrollment, interventions, and assessments
Data management
The case report form includes observation time points, scanning time points, outcome measures, adverse events, and safety evaluations. The researchers will be required to follow the requirements of the case report form and fill in the relevant information in a timely and accurate manner.
Data analysis
Before the data analyses, the research group will provide a statistical scheme to the statisticians. The scheme will include the required data and processing method. The data will be processed and analyzed by the statisticians according to the scheme.
For the clinical data, statistical analyses will be performed with SPSS 22.0 statistics software (IBM Corp., Armonk, NY, USA). The data analysis process will be completed by statisticians who are independent from the research team and blinded to the test settings. A t-test will be used to compare the numerical variables in the within-group analyses, including the Leeds Dyspepsia Questionnaire, Nepean Dyspepsia Index, Self-Rating Anxiety Scale, Self-Rating Depression Scale, Beck Anxiety Inventory, and Beck Depression Inventory. Analysis of variance and the Kruskal–Wallis test will be used for numerical variables in the between-group analyses, including age, height, and scores of the Leeds Dyspepsia Questionnaire, Nepean Dyspepsia Index, Self-Rating Anxiety Scale, Self-Rating Depression Scale, Beck Anxiety Inventory, and Beck Depression Inventory. The chi-square test will be used for categorical variables. A two-sided test will be applied for all available data. The accepted level of significance for all analyses will be P < 0.05.
For the fMRI scans, all preprocessing steps will be conducted using the Data Processing Assistant for Resting-State fMRI (Advanced) based on MATLAB. The preprocessing steps will include slice timing correction, head motion correction, spatial normalization, spatial smoothing, and detrending. After data preprocessing, the data analysis will include two parts: (1) whole-brain performance analysis through the amplitude of low-frequency fluctuation method and (2) functional connectivity through seed correlation analysis. Seeds will be defined based on the result of the amplitude of low-frequency fluctuation analysis and will involve different regions in the He-Mu point combination group compared with the two single-acupoint groups. Seeds will also be defined based on the results of our previous study, which showed that the anterior cingulate cortex, insula, thalamus, and hypothalamus are the key regions that determine the severity of functional dyspepsia symptoms (Zeng et al., 2011). Two-sample t-tests will be used to evaluate the cerebral responses to acupuncture in each group by within-group analysis (post-treatment minus pre-treatment). We will compare the difference in cerebral response changes by between-group analysis in the factorial design module of SPM8. We will also apply Pearson correlation between the post-treatment and pre-treatment cerebral response changes and the corresponding clinical data changes in each group. In this study, cerebral responses to acupuncture mainly refer to the change in amplitude of low-frequency fluctuations and functional connectivity before and after treatment. A threshold of a voxel-wise uncorrected P < 0.005 and P < 0.05 familywise error correction at the cluster level will be applied in all analyses.
Trial Status
The trial is currently in the participant recruitment stage.
Discussion
This clinical fMRI trial is designed to focus on the central mechanism of puncturing at the He-Mu point combination for functional dyspepsia.
Acupoint combination is essential for acupuncture efficacy
The theory of acupoint combination can be traced back to Huangdi Neijing (Zhang and Zhang, 1977). With gradual replenishment and development in each generation, acupoint combination is now widely used in the clinical treatment of acupuncture (Feng et al., 1999; Li, 2010). Acupoint combination is based on traditional Chinese medicine theories and is an acupoint selection method that can integrate the specific effects of different acupoints to produce synergistic effects for better clinical efficacy (Zhang et al., 2014). Thus, acupoint combination is thought to be not only the embodiment of syndrome differentiation and treatment administration but also a crucial component of acupuncture prescriptions and the basis of acupuncture manipulation. It is therefore an essential factor for acupuncture efficacy.
In light of the clinical experience in traditional Chinese medicine, the use of acupoint combination rather than single acupoints is often the first treatment choice because of its better curative effect and wider therapeutic range. For example, according to a bibliometrics study, the commonly used acupoint Neiguan (PC6) was singly used in 105 studies for 39 diseases and in combination with other acupoints in 456 studies for 95 diseases (Xing et al., 2013). More importantly, different acupoint combinations have specific synergistic effects that can be applied to relevant diseases (Zhang and Wang, 2006). Different acupoint combinations have varying efficacies for the same disease (Wang et al., 2014; Zhang, 2014). The He-Mu point combination reportedly has a better curative effect than the Shu-Mu point combination for stress ulcers (Wang et al., 2014). Therefore, use of the most appropriate acupoint combination plays a critical role in the therapeutic effects of acupuncture.
As the classic acupoint combination, the He-Mu point combination (ST36 and CV12) has been proven effective for gastrointestinal diseases (Liu, 2014; Su et al., 2015). However, its efficacy should be investigated further in clinical trials. In addition, because it lacks a clear scientific explanation, the underlying mechanism of the He-Mu point combination deserves further study.
Central integration is the key mechanism of the effects of acupuncture
The mechanisms of the effects of acupuncture remain unclear. The effects of acupuncture are known to comprise a complicated biological \process involving multiple factors, targets, and pathways (Long et al., 2015). A study of the peripheral mechanism underlying acupuncture revealed that the effects of acupuncture are associated with a variety of humoral factors and immune pathways (Long et al., 2015). However, none of these factors plays an indispensable role in the effects of acupuncture; thus, whether the peripheral mechanism is the key factor of the effects of acupuncture remains uncertain.
Scientists have gradually realized that a central mechanism plays a vital role in the effects of acupuncture (Bai and Lao, 2013). The acupuncture signal can travel to the central nervous system via afferent nerve pathways and cause various central integrations to achieve the treatment effect. Furthermore, damage to this central integration can reduce or eliminate the acupuncture effect (Han et al., 1980; Zhang and Zhang, 2007; Lin et al., 2014). Previous studies of pain have demonstrated that acupuncture analgesia can be attributed to pain signal modulation involving multiple nuclei and activation by acupuncture signals in the central nervous system (Han et al., 1980). Pain modulation can be affected by damage to the related brain regions (caudate nucleus and periaqueductal gray), thus reducing or eliminating the effects of acupuncture analgesia. It follows that central integration is an indispensable component of the effects of acupuncture.
Some investigators have also suggested that under the same stimulation, the differences in clinical effects among different acupoints are closely related to different central integrations (Yang et al., 2012; Zhou and Ye, 2012; Zhou et al., 2013). For example, electroacupuncturing at different acupoints, such as Shenmen (HT7), PC6, ST36, or Sanyinjiao (SP6), in rats with insomnia can induce different central integration processes; consequently, different amounts of interleukin-1 and tumor necrosis factor alpha can be produced in the central nervous system, resulting in different effects on insomnia (Zhou and Ye, 2012). Therefore, central integration is the key to acupuncture therapy. The present study focuses on the difference in central integration between the He-Mu point combination and single acupoints for functional dyspepsia.
However, researchers have gradually realized that there are some problems associated with research of the central mechanism of acupuncture. First, data obtained from animal experiments cannot eliminate the influence of species-related differences on the study results. Moreover, in vitro experiment results cannot fully reflect the interaction effect between substances throughout the whole body. Likewise, autopsy case analysis can hardly explain the physiological and pathological functions in vivo. Finally, exploration from the viewpoint of the local structure of an acupoint cannot fully reveal the characteristics of integrated regulation of acupuncture. Therefore, elucidation of the central mechanism by obtaining objective and clearly visualized evidence in vivo has become an urgent task in acupuncture research.
fMRI is the most commonly used neuroimaging technique for exploring the central integration mechanism of acupuncture in vivo
During the past decade, researchers have carried out extensive studies of the central mechanism of acupuncture by a variety of neuroimaging techniques and have accumulated rich visual evidence (Napadow et al., 2008). It has been confirmed that the functional neuroimaging technique is an effective noninvasive method with which to study the central mechanism of acupuncture in vivo.
fMRI is one of multiple neuroimaging techniques. The emergence of fMRI methodology is fundamentally based on the fortuitous presence of an endogenous contrast agent, paramagnetic deoxyhemoglobin, circulating in the brain and the tight coupling between neuronal activation and hemodynamic responses. The fMRI signal can be changed by alterations in deoxyhemoglobin through hemodynamic responses at the sites of neuronal activation induced by stimuli to the brain, such as acupuncture. The most important function of fMRI in investigating the central mechanism of acupuncture is to determine the areas associated with specific stimuli because the brain function is spatially segmented and compartmentalized. Since its introduction, fMRI has rapidly become a widely used method in investigating the central mechanism of acupuncture because of its lack of radiation, high-quality spatial and time resolution, quick imaging velocity, and low price (Ogawa et al., 1998; Health Quality Ontario, 2006). fMRI was reportedly used in 779 acupuncture studies before September 2009 (Huang et al., 2012). Therefore, fMRI has been selected as a tool with which to reveal the central mechanism of the synergistic effect of the He-Mu point combination in the present study.
Quality control is the precondition for improving the reliability of results
Because of the diversity of acupuncture manipulations and the complexity of brain function, the results of acupuncture neuroimaging studies can be affected by various factors such as participants’ baseline characteristics, types of acupuncture manipulation, and fMRI scan parameters. Thus, different or even opposite results have been obtained in similar studies. Identification of rational methods with which to upgrade the reproducibility and reliability of results has therefore become a pressing issue in study design.
Considering the particularity of acupuncture neuroimaging studies, specific measures will be conducted to avoid bias in the present trial. Age, race, and handedness have a significant influence on the functional activity and structure of the brain (Rushton and Ankney, 1996). To acquire higher homogeneity at baseline, we have established rigorous inclusion and exclusion criteria including many demographic characteristics such as age, race, and handedness. Moreover, psychological factors have a strong influence on the function and structure of the human brain; thus, a preliminary evaluation of the patients’ psychological states will be conducted with the Self-Rating Anxiety Scale and Self-Rating Depression Scale to exclude severely depressed and anxious patients.
To ensure the stability of MRI data acquisition, only one technician will perform all scans using the same MRI machine according to the related operation standard and design of the study in the fixed condition. Some recent studies have indicated that the cerebral function and structure change during menstruation (Hagemann et al., 2011); therefore, scanning of female patients will be conducted during the same physiological period to avoid possible changes induced by the menstrual cycle. Furthermore, a unified guidebook will be used to standardize the researchers’ speech and behavior.
In summary, acupoint combination is an essential factor for acupuncture efficacy, and elucidation of its underlying mechanisms is vital for improvements in the effect of acupuncture. Thus, this study is designed to investigate the central mechanisms of puncturing at the He-Mu point combination for functional dyspepsia. We expect that our findings will promote more widespread awareness of the benefits of acupoint combination in the clinical setting and provide a baseline for further research on the central mechanisms of acupuncture for gastrointestinal disease. We expect that more related studies of the mechanism of acupuncture will be performed in the future.
Limitations
The main limitation of this study is the small sample size. The clinical sample size should be determined using a more accurate calculation. Although this is a pilot study, demonstration of the central mechanisms involved in acupoint combination could provide a new approach for future studies.
Acknowledgments
We are grateful to Professor Yong Tang, Dr. Lei Lan, Dr. Zheng-jie Li, Dr. Ying Lan and Dr. Shi-rui Cheng, from Acupuncture and Tuina School, Chengdu University of Traditional Chinese Medicine, China, for scientific help.
Footnotes
Funding: The study was financially supported by the National Scientific Foundation Committee in China, No. 81473602; the Education Ministry's New Century Excellent Talents Supporting Plan in China; the Foundation for the Author of National Excellent Doctoral Dissertation of China, No. 201486; the Youth Foundation of Science and Technology Department of Sichuan Province in China, No. 15QNJJ0008; the National Natural Science Foundation—Excellent Youth Foundation in China, No. 81622052; the 2011 Co-Innovation Center of Sichuan Province named Acupoint Effects of Acupuncture Co-Innovation Center.
Declaration of patient consent: The authors certify that they will obtain all appropriate patient consent forms. In the form the patients will give their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest: None declared.
Plagiarism check: This paper was screened twice using CrossCheck to verify originality before publication.
Peer review: This paper was double-blinded and stringently reviewed by international expert reviewers.
Copyedited by Morben A, Haase R, Yu J, Li CH, Qiu Y, Song LP, Zhao M
References
- Bai L, Lao L. Neurobiological foundations of acupuncture: the relevance and future prospect based on neuroimaging evidence. Evid Based Complement Alternat Med 2013. 2013 doi: 10.1155/2013/812568. 812568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bielefeldt K. From ischochymia to gastroparesis: proposed mechanisms and preferred management of dyspepsia over the centuries. Dig Dis Sci. 2014;59:1088–1098. doi: 10.1007/s10620-014-3144-0. [DOI] [PubMed] [Google Scholar]
- Camilleri M, Stanghellini V. Current management strategies and emerging treatments for functional dyspepsia. Nat Rev Gastroenterol Hepatol. 2013;10:187–194. doi: 10.1038/nrgastro.2013.11. [DOI] [PubMed] [Google Scholar]
- Chen SL. A review of drug therapy for functional dyspepsia. J Dig Dis. 2013;14:623–625. doi: 10.1111/1751-2980.12094. [DOI] [PubMed] [Google Scholar]
- Desmond JE, Glover GH. Estimating sample size in functional MRI (fMRI) neuroimaging studies: Statistical power analyses. J Neurosci Methods. 2002;118:115–128. doi: 10.1016/s0165-0270(02)00121-8. [DOI] [PubMed] [Google Scholar]
- Fang J, Wang D, Zhao Q, Hong Y, Jin Y, Liu Z, Zhou K, Jing X, Yu X, Pan R, Chang A, Liu H, Zhu B. Brain-gut axis modulation of acupuncture in functional dyspepsia: a preliminary resting-state fcmri study. Evid Based Complement Alternat Med 2015. 2015 doi: 10.1155/2015/860463. 860463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng QG, Pei JC, Ren L. The law of prescription and acupoints combination in Zhenjiufengyuan. Liaoning Zhongyi Zazhi. 1999;26:79–80. [Google Scholar]
- Filipović BF, Randjelovic T, Ille T, Markovic O, Milovanović B, Kovacevic N, Filipović BR. Anxiety, personality traits and quality of life in functional dyspepsia-suffering patients. Eur J Intern Med. 2013;24:83–86. doi: 10.1016/j.ejim.2012.06.017. [DOI] [PubMed] [Google Scholar]
- Geng D, Hu YP, Li XL, Li JH, Ma TT. Clinical observation of combining lower he-sea and front-mu points for functional dyspepsia. Shanghai Zhenjiu Zazhi. 2015;34:731–733. [Google Scholar]
- Hagemann G, Ugur T, Schleussner E, Mentzel HJ, Fitzek C, Witte OW, Gaser C. Changes in brain size during the menstrual cycle. PLoS One. 2011;6:e14655. doi: 10.1371/journal.pone.0014655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han GW. Research of the basic prescription to treat all gastric diseases with three points Zusanli (ST36), Neiguan (PC6), Zhongwan (CV13)from acient classic. Zhenjiu Linchuang Zazhi. 2003;19:1–2. [Google Scholar]
- Han JS, Tang J, Ren MF, Zhou ZF, Fan SG, Qiu XC. The central nervous medium and the acupuncture analgesia. Beijing Yixueyuan. 1980;Xuebao:11–19. [Google Scholar]
- Hayasaka S, Peiffer AM, Hugenschmidt CE, Laurienti PJ. Power and sample size calculation for neuroimaging studies by non-central random field theory. Neuroimage. 2007;37:721–730. doi: 10.1016/j.neuroimage.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Quality Ontario (2006) Functional brain imaging: an evidence-based analysis. Ont Health Technol Assess Ser. 6:1–79. [PMC free article] [PubMed] [Google Scholar]
- Hu SS, Wang YP. The overview of clinical research of acupuncture on functional dyspepsia. Zhenjiu Linchuang Zazhi. 2013;29:91–94. [Google Scholar]
- Huang J, Liu B, Yang C, Chen H, Eunice D, Yuan Z. Acute hyperglycemia worsens ischemic stroke-induced brain damage via high mobility group box-1 in rats. Brain Res. 2013;1535:148–155. doi: 10.1016/j.brainres.2013.08.057. [DOI] [PubMed] [Google Scholar]
- Huang W, Pach D, Napadow V, Park K, Long X, Neumann J, Maeda Y, Nierhaus T, Liang F, Witt CM. Characterizing acupuncture stimuli using brain imaging with FMRI--a systematic review and meta-analysis of the literature. PLoS One. 2012;7:e32960. doi: 10.1371/journal.pone.0032960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji LX, Yan LP, Wang HJ, Wang B, Zhang XY, Zhang TS, Jin XF. Selection of basic acupoints for composing “gastric-disorder-formula” for electroacupuncture prevention of acute gastric mucosal lesion in rats. Zhen Ci Yan Jiu. 2008;33:296–300. 325. [PubMed] [Google Scholar]
- Jiang SM, Jia L, Lei XG, Xu M, Wang SB, Liu J, Song M, Li WD. Incidence and psychological-behavioral characteristics of refractory functional dyspepsia: a large, multi-center, prospective investigation from China. World J Gastroenterol. 2015;21:1932–1937. doi: 10.3748/wjg.v21.i6.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo T, Kawamoto M. Acupuncture and moxibustion for stress-related disorders. Biopsychosoc Med. 2014;8:7. doi: 10.1186/1751-0759-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong SP, Shan QH, Dong AM. Synergetic and antagonistic effects of shu-points and mupoints of the lung on pulmonary functions. Zhongguo Zhen Jiu. 2004;24:840–842. [Google Scholar]
- Kumar A, Pate J, Sawant P. Epidemiology of functional dyspepsia. J Assoc Physicians India. 2012;60(Suppl):9–12. [PubMed] [Google Scholar]
- Lacy BE, Weiser KT, Kennedy AT, Crowell MD, Talley NJ. Functional dyspepsia: the economic impact to patients. Aliment Pharmacol Ther. 2013;38:170–177. doi: 10.1111/apt.12355. [DOI] [PubMed] [Google Scholar]
- Lan L, Zeng F, Liu GJ, Ying L, Wu X, Liu M, Liang FR. Acupuncture for functional dyspepsia. Cochrane Database Syst Eev. 2014:CD008487. doi: 10.1002/14651858.CD008487.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee IS, Wang H, Chae Y, Preissl H, Enck P. Functional neuroimaging studies in functional dyspepsia patients: a systematic review. Neurogastroenterol Motil. 2016;28:793–805. doi: 10.1111/nmo.12793. [DOI] [PubMed] [Google Scholar]
- Lee LA, Chen J, Yin J. Complementary and alternative medicine for gastroparesis. Gastroenterol Clin North Am. 2015;44:137–150. doi: 10.1016/j.gtc.2014.11.011. [DOI] [PubMed] [Google Scholar]
- Li DD, Yue ZH, Xu LC, Xie T, Hu GZ, Yang J. Clinical evaluation study on long-term effect of acupuncture with pattern/syndrome differentiation on functional dyspepsia. Zhongguo Zhen Jiu. 2014;34:431–434. [PubMed] [Google Scholar]
- Li ZR. Survey of research on acupoints compatibility. Zhongguo Zhen Jiu. 2010;30:437–440. [PubMed] [Google Scholar]
- Lima FA, Ferreira LE, Pace FH. Acupuncture effectiveness as a complementary therapy in functional dyspepsia patients. Arq Gastroenterol. 2013;50:202–207. doi: 10.1590/S0004-28032013000200036. [DOI] [PubMed] [Google Scholar]
- Lin D, De La Pena I, Lin L, Zhou SF, Borlongan CV, Cao C. The neuroprotective role of acupuncture and activation of the BDNF signaling pathway. Int J Mol Sci. 2014;15:3234–3252. doi: 10.3390/ijms15023234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu ZZ. Clinical efficacy of lower He-frone Mu points acupuncture methods for functional diarrhea. Changchun: Changchun University of Traditional Chinese Medicine; 2014. [Google Scholar]
- Long XQ, Jiang HL, Ren XJ, Ji LL, Tu Y. Development of researches on mechanisms of acupoint combination for some disorders in nerve-humoral-immunological modulation. Zhen Ci Yan Jiu. 2015;40:314–318. [PubMed] [Google Scholar]
- Ma TT, Yu SY, Li Y, Liang FR, Tian XP, Zheng H, Yan J, Sun GJ, Chang XR, Zhao L, Wu X, Zeng F. Randomised clinical trial: an assessment of acupuncture on specific meridian or specific acupoint vs. sham acupuncture for treating functional dyspepsia. Aliment Pharmacol Ther. 2012;35:552–561. doi: 10.1111/j.1365-2036.2011.04979.x. [DOI] [PubMed] [Google Scholar]
- Mahadeva S, Goh KL. Epidemiology of functional dyspepsia: a global perspective. World J Gastroenterol. 2006;12:2661–2666. doi: 10.3748/wjg.v12.i17.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moayyedi, Duffett, Braunholtz, Mason, Richards, Dowell, Axon The Leeds Dyspepsia Questionnaire: a valid tool for measuring the presence and severity of dyspepsia. Aliment Pharmacol Ther. 1998;12:1257–1262. doi: 10.1046/j.1365-2036.1998.00404.x. [DOI] [PubMed] [Google Scholar]
- Napadow V, Ahn A, Longhurst J, Lao L, Stener-Victorin E, Harris R, Langevin HM. The Status and Future of Acupuncture Mechanism Research. J Altern Complement Med. 2008;14:861–869. doi: 10.1089/acm.2008.SAR-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogawa S, Menon RS, Kim SG, Ugurbil K. On the characteristics of functional magnetic resonance imaging of the brain. Annu Rev Biophys Biomol Struct. 1998;27:447–474. doi: 10.1146/annurev.biophys.27.1.447. [DOI] [PubMed] [Google Scholar]
- Qiu K, Jing M, Sun R, Yang J, Liu X, He Z, Yin S, Lan Y, Cheng S, Gao F, Liang F, Zeng F. The status of the quality control in acupuncture-neuroimaging studies. Evid Based Complement Alternat Med 2016. 2016 doi: 10.1155/2016/3685785. 3685785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafiei R, Ataie M, Ramezani MA, Etemadi A, Ataei B, Nikyar H, Abdoli S. A new acupuncture method for management of irritable bowel syndrome: A randomized double blind clinical trial. J Res Med Sci. 2014;19:913–917. [PMC free article] [PubMed] [Google Scholar]
- Ren YL, Zhao L, Liu ML, Liang FR. Data mining-based study on characteristics of acupoints selection on ancient acupuncture treatment of functional dyspepsia. Liaoning Zhongyi Zazhi. 2009;36:259–262. [Google Scholar]
- Rushton JP, Ankney CD. Brain size and cognitive ability: Correlations with age, sex, social class, and race. Psychon Bull Rev. 1996;3:21–36. doi: 10.3758/BF03210739. [DOI] [PubMed] [Google Scholar]
- Sander GB, Mazzoleni LE, Francesconi CF, Balbinotto G, Mazzoleni F, Wortmann AC, Cardoso Ide Q, Klamt AL, Milbradt TC. Helicobacter Eradication Relief of Dyspetic Symptoms Trial Investigators (2011) Influence of organic and functional dyspepsia on work productivity: the HEROES-DIP study. Value Health. 14:S126–S129. doi: 10.1016/j.jval.2011.05.021. [DOI] [PubMed] [Google Scholar]
- Su YS, Xin JJ, Yang ZK, He W, Shi H, Wang XY, Hu L, Jing XH, Zhu B. Effects of different local moxibustion-like stimuli at Zusanli (ST36) and Zhongwan (CV12) on gastric motility and its underlying receptor mechanism. Evid Based Complement Alternat Med 2015. 2015 doi: 10.1155/2015/486963. 486963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tack J, Talley NJ. Functional dyspepsia--symptoms, definitions and validity of the Rome III criteria. Nat Rev Gastroenterol Hepatol. 2013;10:134–141. doi: 10.1038/nrgastro.2013.14. [DOI] [PubMed] [Google Scholar]
- Takahashi T. Acupuncture for functional gastrointestinal disorders. J Gastroenterol. 2006;41:408–417. doi: 10.1007/s00535-006-1773-6. [DOI] [PubMed] [Google Scholar]
- Talley NJ, Verlinden M, Jones M. Validity of a new quality of life scale for functional dyspepsia: a United States multicenter trial of the Nepean Dyspepsia Index. Am J Gastroenterol. 1999;94:2390–2397. doi: 10.1111/j.1572-0241.1999.01363.x. [DOI] [PubMed] [Google Scholar]
- Voiosu TA, Giurcan R, Voiosu AM, Voiosu MR. Functional dyspepsia today. Maedica (Buchar) 2013;8:68–74. [PMC free article] [PubMed] [Google Scholar]
- Wang CF, Cai ZH, Xu Q. Self-Rating Depression Scale (SDS): an analysis on 1340 health subjects. Zhongguo Shenjing Jingshen Jibing Zazhi. 1986;12:267–268. [Google Scholar]
- Wang M. Functional MRI studies on puncturing in ‘Siguan’ acupoints for Alzheimer's disease patients. Beijing: Capital Medical University; 2012. [Google Scholar]
- Wang YL. Clinical study on the synergic and antagonistic effects of pericardial back-Shu and front-Mu point compatibility. Shanghai Zhenjiu Zazhi. 2005;24:29–32. [Google Scholar]
- Wang ZH, Zhang JJ, Wang FC. Effect of different acupoint prescriptions on prevention and treatment of stress gastric ulcer. Zhongguo Zhen Jiu. 2014;34:149–151. [PubMed] [Google Scholar]
- Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- Xing JJ, Ren YL, Tang Y, Liang FR. Research on disease spectrums of puncturing PC-6 and its compatibility. Liaoning Zhongyi Zazhi. 2013;40:173–176. [Google Scholar]
- Yang J, Zeng F, Feng Y, Fang L, Qin W, Liu X, Song W, Xie H, Chen J, Liang F. A PET-CT study on the specificity of acupoints through acupuncture treatment in migraine patients. BMC Complement Altern Med. 2012;12:123. doi: 10.1186/1472-6882-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng F, Lan L, Tang Y, Liu M, Liu X, Song W, Li Y, Qin W, Sun J, Yu S, Gao X, Tian J, Liang F. Cerebral responses to puncturing at different acupoints for treating meal-related functional dyspepsia. Neurogastroenterol Motil. 2015;27:559–568. doi: 10.1111/nmo.12532. [DOI] [PubMed] [Google Scholar]
- Zeng F, Qin W, Liang F, Liu J, Tang Y, Liu X, Yuan K, Yu S, Song W, Liu M, Lan L, Gao X, Liu Y, Tian J. Abnormal resting brain activity in patients with functional dyspepsia is related to symptom severity. Gastroenterology. 2011;141:499–506. doi: 10.1053/j.gastro.2011.05.003. [DOI] [PubMed] [Google Scholar]
- Zeng F, Qin W, Ma T, Sun J, Tang Y, Yuan K, Li Y, Liu J, Liu X, Song W, Lan L, Liu M, Yu S, Gao X, Tian J, Liang F. Influence of acupuncture treatment on cerebral activity in functional dyspepsia patients and its relationship with efficacy. Am J Gastroenterol. 2012;107:1236–1247. doi: 10.1038/ajg.2012.53. [DOI] [PubMed] [Google Scholar]
- Zhang BY. The different effect of different acupoints compatibility for functional diarrhea. Beijing: Beijing University of Traditional Chinese Medicine; 2014. [Google Scholar]
- Zhang GX, Liu H, Wang FC. Acupoint combination and acupuncture-moxibustion prescription. Zhongguo Zhen Jiu. 2014;34:987–990. [PubMed] [Google Scholar]
- Zhang HS, Wang FC. Application of combination of he-mu points and combination of shu-yuan in syndrome differentiation of zang- and fu-organs. Zhongguo Zhen Jiu. 2006;26:378–380. [PubMed] [Google Scholar]
- Zhang J, Zhang N. Study on mechanisms of acupuncture analgesia. Zhongguo Zhen Jiu. 2007;27:72–75. [PubMed] [Google Scholar]
- Zhang SC, Zhang DB. The basic law of acupoint selection in Huangdineijing. Shandong Zhongyiyao Daxue. 1977;Xuebao:20–25. [Google Scholar]
- Zhou S, Zeng F, Liu J, Zheng H, Huang W, Liu T, Chen D, Qin W, Gong Q, Tian J, Li Y. Influence of acupuncture stimulation on cerebral network in functional diarrhea. Evid Based Complement Alternat Med 2013. 2013 doi: 10.1155/2013/975769. 975769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou YL, Ye XF. Experimental research on the difference of IL-1 and TNF-α in the brain of rats with insomnia between different acupoints. Zhongguo Zhongyi Jichu Yixue Zazhi. 2012;18:419–420. [Google Scholar]
- Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]