Abstract
The implementation of patient-centered care requires an individualized approach to hemodialysis vascular access, on the basis of each patient’s unique balance of risks and benefits. This systematic review aimed to summarize current literature on fistula risks, including rates of complications, to assist with patient-centered decision making. We searched Medline from 2000 to 2014 for English-language studies with prospectively captured data on ≥100 fistulas. We assessed study quality and extracted data on study design, patient characteristics, and outcomes. After screening 2292 citations, 43 articles met our inclusion criteria (61 unique cohorts; n>11,374 fistulas). Median complication rates per 1000 patient days were as follows: 0.04 aneurysms (14 unique cohorts; n=1827 fistulas), 0.11 infections (16 cohorts; n>6439 fistulas), 0.05 steal events (15 cohorts; n>2543 fistulas), 0.24 thrombotic events (26 cohorts; n=4232 fistulas), and 0.03 venous hypertensive events (1 cohort; n=350 fistulas). Risk of bias was high in many studies and event rates were variable, thus we could not present pooled results. Studies generally did not report variables associated with fistula complications, patient comorbidities, vessel characteristics, surgeon experience, or nursing cannulation skill. Overall, we found marked variability in complication rates, partly due to poor quality studies, significant heterogeneity of study populations, and inconsistent definitions. There is an urgent need to standardize reporting of methods and definitions of vascular access complications in future clinical studies to better inform patient and provider decision making.
Keywords: arteriovenous fistula, chronic hemodialysis, epidemiology and outcomes
Current literature suggests the arteriovenous fistula (fistula) to be the preferred type of vascular access for hemodialysis.1–3 Once established, fistulas have longer patency and lower rates of complications compared with arteriovenous grafts and catheters.4,5 However, with the increasing proportion of elderly and frail patients on hemodialysis, the rate of failure to mature has increased with a decrease in patency rates.6 The current focus on patient-centered care requires individualized approaches to therapy, including the choice and use of vascular access, on the basis of each patient’s unique balance of risks and benefits. As such, complications related to vascular access also deserve careful consideration when individualizing the choice of vascular access type, facilitating informed consent, and providing an appropriate implementation plan (creation, monitoring, and use).
Fistula complications are associated with morbidity, mortality, and a high economic burden.7–10 Although there have been systematic reviews and meta-analyses on fistula patency and failure to mature, to our knowledge, no published systematic review has evaluated fistula complication rates related to aneurysm, infection, ischemic steal syndrome, thrombosis, and venous hypertension. We conducted this systematic review to concisely summarize contemporary published information between 2000 and 2014 on the rates for the above-mentioned complications, as well as to identify knowledge gaps in the existing literature.
Results
The literature search yielded 2292 citations. All citations were screened by title and abstract, resulting in 172 articles reviewed in full-text. Thirty-five articles met eligibility criteria. Details of the study selection are shown in Supplemental Figure 1. Twelve additional studies were identified through manual search of bibliographies of selected articles and eight were included in our analyses. Thus, 43 studies (61 unique cohorts; n>11,374 fistulas—not all studies reported number of fistulas included) were included from 19 countries. Most published studies were from the United States (13 studies), Canada (five studies), and Italy (four studies). One study reported outcomes of interest across European countries and another reported on infections internationally.11,12 All studies were published between 2001 and 2014 with patient recruitment beginning between 1986 and 2012. The characteristics of each study are described in Table 1.
Table 1.
Study characteristics
| Author (Yr Published) | Country | Recruitment Start | Type of Study | Cohort Subset | Follow-Up (Mo) | No. of Fistulas | Upper Arm, % | First Fistula, % | Age, yr | Men, % | DM, % | CAD, % | CHD, % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| McCarley et al. (2001)58a,b | United States | 1996 | Retrospective | NM | 11.0 | 39 | . | . | 55.3 | 51 | 36 | . | . |
| McCarley et al. (2001)58a,b | United States | 1996 | Retrospective | DVPM | 12.0 | 41 | . | . | 56.6 | 54 | 36 | . | . |
| McCarley et al. (2001)58a,b | United States | 1997 | Retrospective | VABFM | 10.0 | 43 | . | . | 56.1 | 59 | 34 | . | . |
| Tokars et al. (2001)59 | United States | 1997 | Prospective | Standard | 5.2 | . | . | . | . | . | . | . | . |
| Dixon et al. (2002)60 | United States | 1992 | Retrospective | Lower arm | . | 88 | 0 | . | 50.9 | 81 | 47 | 39 | . |
| Dixon et al. (2002)60 | United States | 1992 | Retrospective | Upper arm | . | 117 | 100 | . | 57.8 | 56 | 56 | 49 | . |
| Ravani et al. (2002)61 | Italy | 1995 | Prospective | Standard | 20.4 | 197 | 19 | 100 | 65.7 | 59 | 22 | . | 14 |
| Saxena et al. (2002)62 | Saudi Arabia | 1996 | Prospective | Diabetic nasal carriers of MRSA/MSSA | 36.0 | . | . | . | . | . | . | . | . |
| Saxena et al. (2002)62 | Saudi Arabia | 1996 | Prospective | Nondiabetic nasal carriers of MRSA/MSSA | 36.0 | . | . | . | . | . | . | . | . |
| Stevenson et al. (2002)63 | United States | 1998 | Retrospective | Standard | . | . | . | . | . | . | . | . | . |
| Taylor et al. (2002)64 | Canada | 1998 | Surveillance | Standard | 6.0 | . | . | . | . | . | . | . | . |
| Tokars et al. (2002)65 | United States | 1999 | Prospective | Standard | . | . | . | . | . | . | . | . | . |
| Elseviers et al. (2003)11b | Europe | 1998 | Prospective | Standard | 12.0 | 1049 | . | . | . | 56 | . | . | . |
| Lok et al. (2003)66a | Canada | 1997 | Prospective | Duplex US Monitoring | 9.2 | 189 | 30 | 96 | 57.5 | 71 | . | . | . |
| Lok et al. (2003)66a | Canada | 1999 | Prospective | Transonic surveillance | 10.4 | 241 | 30 | 96 | 57.5 | 71 | . | . | . |
| Saxena et al. (2003)67b | Saudi Arabia | 1997 | Surveillance | Standard | . | . | . | . | 47.5 | 54 | . | . | . |
| Bonforte et al. (2004)68 | Italy | 1991 | Prospective | Lower arm | 27.0 | 112 | 0 | . | 71 | 50 | 22 | . | . |
| Astor et al. (2005)69 | United States | 1995 | Prospective | Standard | 35.9 | 185 | . | . | 56.8 | 71 | 47 | 42 | . |
| Gilad et al. (2005)70b | Israel | 2002 | Surveillance | Standard | . | . | . | . | 63.5 | 55 | 48 | 44 | 21 |
| Lok et al. (2005)71 | Canada | 1995 | Retrospective | Nonelderly (<65 yr) | 65.0 | 248 | 44 | 100 | 46 | 65 | 29 | 24 | 15 |
| Lok et al. (2005)71 | Canada | 1995 | Retrospective | Elderly (≥65 yr) | 51.7 | 196 | 53 | 100 | 74 | 69 | 30 | 44 | 29 |
| Mallamaci et al. (2005)72 | Italy | . | Prospective | Standard | 32.5 | 205 | 5 | . | 59.4 | 57 | 14 | . | . |
| Shahin et al. (2005)73 | United States | 1992 | Retrospective | Standard | 21.0 | 146 | 51 | 100 | 54.9 | 58 | 49 | 53 | . |
| Shahin et al. (2005)73 | United States | 1999 | Retrospective | Qa surveillance | 19.0 | 76 | 61 | 100 | 57.6 | 59 | 57 | 68 | . |
| Jennings et al. (2006)74 | United States | 2003 | Retrospective | Standard | 11.0 | 134 | 91 | 74 | 61 | 54 | 52 | . | . |
| Polkinghorne et al. (2006)75 | Australia | 2001 | RCT | Standard | 16.2 | 68 | 34 | . | 56.4 | 71 | 28 | 29 | . |
| Polkinghorne et al. (2006)75 | Australia | 2001 | RCT | Qa surveillance | 17.3 | 69 | 36 | . | 60 | 65 | 35 | 28 | . |
| Roozbeh et al. (2006)76a | Iran | . | Prospective | Standard | 23.0 | 171 | 57 | . | 53 | 68 | 27 | . | . |
| Huijbregts et al. (2008)5 | The Netherlands | 2004 | Prospective | Standard | 8.6 | 285 | 40 | . | 64.6 | 62 | 33 | 23 | . |
| Pflederer et al. (2008)77 | United States | 2004 | Retrospective | Standard | 8.0 | 321 | 37 | . | 64.5 | 65 | 43 | . | . |
| Pflederer et al. (2008)77 | United States | 2004 | Retrospective | AVF-T | 8.0 | 161 | 100 | . | 63.3 | 61 | 45 | . | . |
| Qasaimeh et al. (2008)78b | Jordan | 2004 | Retrospective | Standard | 12.0 | 104 | . | . | . | 52 | 32 | . | . |
| Tessitore et al. (2008)79c | Italy | 2002 | Prospective | Standard | 31.0 | 97 | 18 | . | 65.1 | 64 | 19 | 62 | . |
| Tessitore et al. (2008)79c | Italy | 2002 | Prospective | Qa Surveillance | 30.0 | 62 | 21 | . | 63.4 | 52 | 31 | 69 | . |
| Koksoy et al. (2009)80 | Turkey | 2003 | RCT | AVF-T | 43.6 | 50 | 100 | 0 | 54.66 | 52 | 32 | . | . |
| Koksoy et al. (2009)80 | Turkey | 2003 | RCT | Upper arm | 39.5 | 50 | 100 | 0 | 54.78 | 60 | 24 | . | . |
| Papanikolaou et al. (2009)81 | Greece | 1986 | Retrospective | Lower arm | . | . | 100 | . | . | 45 | 8 | . | . |
| Papanikolaou et al. (2009)81 | Greece | 1986 | Retrospective | Upper arm | . | . | . | . | . | 45 | 8 | . | . |
| Korkut et al. (2010)15 | Turkey | 2004 | Retrospective | AVF-T | 48.0 | 350 | 100 | . | 57.8 | 44 | 51 | 15 | . |
| Paul et al. (2010)82 | United States | 2006 | Retrospective | Endo/AVF-T | 14.0 | 98 | 100 | 47 | 60 | 40 | 49 | . | . |
| Paul et al. (2010)82 | United States | 2006 | Retrospective | Open/AVF-T | 18.0 | 78 | 100 | 41 | 62 | 27 | 56 | . | . |
| van Loon et al. (2010)13 | The Netherlands | 2007 | Prospective | Rope ladder | . | 70 | 39 | 84 | 65 | 67 | 21 | 80 | . |
| van Loon et al. (2010)13 | The Netherlands | 2007 | Prospective | Buttonhole | . | 75 | 51 | 68 | 67 | 59 | 27 | 61 | . |
| Jennings et al. (2011)83a | United States | 2003 | Retrospective | Elderly (≥65 yr) | 17.0 | 461 | 38 | 77 | 73 | 49 | 60 | . | . |
| Labriola et al. (2011)84 | Belgium | 2001 | Retrospective | Standard | 35.1 | . | 37 | . | 70.4 | 66 | 33 | . | . |
| Ng et al. (2011)85 | United States | 1996 | Prospective | Standard | 6.0 | 476 | . | . | 61.1 | 73 | 49 | 47 | 34 |
| Ayez et al. (2012)86 | The Netherlands | 2000 | Retrospective | Upper arm | 19.0 | 173 | 100 | 68 | 62.61 | 52 | 46 | 3 | 57 |
| Renaud et al. (2012)87 | Singapore | 2008 | Retrospective | Nonelderly (<65 yr) | 12.0 | 191 | 41 | 100 | 52 | 60 | 70 | 41 | . |
| Renaud et al. (2012)87 | Singapore | 2008 | Retrospective | Elderly (≥65 yr) | 13.0 | 89 | 39 | 100 | 72 | 55 | 71 | 49 | . |
| Kandil et al. (2013)88 | United Kingdom | 2007 | Retrospective | Buttonhole | . | 227 | . | . | 63.8 | 61 | 46 | . | . |
| Lin et al. (2013)14 | Taiwan | 2008 | RCT | Infrared | 12.0 | 60 | 15 | 100 | 63.2 | 53 | 47 | 17 | . |
| Lin et al. (2013)14 | Taiwan | 2008 | RCT | Standard | 12.0 | 62 | 18 | 100 | 63 | 57 | 37 | 12 | . |
| Macrae et al. (2013)19 | Canada | 2006 | RCT | Buttonhole | . | 70 | 84 | 83 | 77.2 | 73 | 49 | 61 | . |
| Macrae et al. (2013)19 | Canada | 2006 | RCT | Standard | . | 69 | 75 | 86 | 66.1 | 67 | 54 | 42 | . |
| Ravani et al. (2013)12 | International | 1996 | RCT | Standard | . | 3352 | . | 100 | 62.2 | 68 | 38 | 36 | 29 |
| de Albuquerque et al. (2013)89 | Brazil | 2010 | Surveillance | Standard | . | . | . | . | . | . | . | . | . |
| Agarwal et al. (2014)90 | United States | 2005 | Retrospective | AVF-T (1-stage) | . | 61 | 100 | . | 59.1 | . | . | . | . |
| Agarwal et al. (2014)90 | United States | 2005 | Retrospective | AVF-T (2-stage) | . | 83 | 100 | . | 61.5 | . | . | . | . |
| Badawy et al. (2014)91b | Kuwait | 2012 | Surveillance | Standard | . | . | . | . | 58.1 | 40 | . | . | . |
| Lok et al. (2014)92 | Canada | 2000 | Retrospective | Rope ladder | 29.6 | 457 | . | . | 58.8 | 58 | 36 | 29 | 16 |
| Olsha et al. (2014)93 | Turkey | 2005 | Retrospective | Elderly (≥80 yr) | 17.6 | 128 | 71 | . | 85 | 66 | 40 | 45 | 24 |
DM, diabetes mellitus; CAD, coronary artery disease; CHD, Congestive Heart Disease; NM, no monitoring; ., data not reported; DVPM, dynamic venous pressure monitoring; VABFM, vascular access blood flow monitoring; standard, all fistula locations; lower arm, a cohort consisting of patients only fistulas located in the lower arm; upper arm, patients with fistulas located in the upper arm, including transposed brachiobasilic fistulas; MRSA, methicillin‐resistant Staphylococcus aureus; MSSA, methicillin‐sensitive Staphylococcus aureus; duplex US, duplex ultrasound; RCT, randomized controlled trial; AVF-T, transposed arteriovenous fifistula; endo/AVF-T, a transposed arteriovenous fistula created using an endoscopic procedure; open/AVF-T, a transposed arteriovenous fistula created using a long open incision technique; rope ladder, rope ladder cannulation; buttonhole, buttonhole cannulation.
Percentage of patients whose diabetes was the cause of kidney failure.
Baseline data reported for fistulas and other accesses grouped together.
CAD was defined as presence of cardiovascular disease.
Patient Population
Patient demographic data, comorbid conditions, and site of fistula creation were not always reported. Three out of the 39 observational studies were prospective surveillance studies and generally did not report baseline characteristics specific to patients using a fistula. However, when the data were reported, the median age was 61 years (ranging from 46 to 85 years; interquartile range [IQR] =7.6 years). The median proportion of men and patients with diabetes was 59% (range 27%–81%; IQR=13%) and 37% (range 8%–71%; IQR=20%), respectively. The median proportion of patients who had an upper arm fistula was 44% (range 0%–100%; IQR=70%). A summary of characteristics is presented in Table 2.
Table 2.
Summary of study characteristics (61 cohorts in total)
| Variable | N (%) | Median | Min | Q1 | Q3 | Max |
|---|---|---|---|---|---|---|
| Proportion of patients with first fistula, % | 23 (38) | 96 | 0 | 68 | 100 | 100 |
| Mean age reported in study, yr | 50 (82) | 61.05 | 46 | 56.8 | 64.6 | 85 |
| Time from fistula creation to use, mo | 15 (25) | 3.49 | 1.11 | 1.73 | 4.87 | 5.92 |
| Body mass index, kg/m2 | 15 (25) | 25.5 | 23.39 | 24.9 | 26.8 | 28 |
| Coronary artery disease, % | 27 (44) | 42 | 3 | 28 | 53 | 80 |
| Congestive heart disease, % | 9 (15) | 24 | 14 | 16 | 29 | 57 |
| Diabetes, % | 47 (77) | 37 | 8 | 29 | 49 | 71 |
| Men, % | 52 (85) | 59 | 27 | 53 | 66 | 81 |
| Peripheral vascular disease, % | 22 (36) | 16 | 0 | 9 | 23 | 53 |
| Patients with a fistula, % | 59 (97) | 100 | 38 | 100 | 100 | 100 |
| White, % | 23 (38) | 74 | 44 | 63 | 90 | 100 |
| Upper arm, % | 41 (67) | 44 | 0 | 30 | 100 | 100 |
There were 61 cohorts in total. N, total number of cohorts that reported the variable of interest; Min/Max, minimum/maximum reported value; Q1 and Q3, the values which 25% and 75% of the data set lie below, respectively.
Study Quality Assessment
Methods were inadequately reported and definitions were inconsistent across studies. Definitions were not reported for five of nine studies reporting aneurysm, seven of 23 studies reporting infections, nine of 12 studies reporting ischemic steal syndrome, 13 of 18 studies reporting thrombosis, and the one study reporting venous hypertension. Loss to follow-up was not reported in 28 out of 38 observational studies and one of the four randomized controlled trials. However, when reported, the median loss to follow-up was <10% for all studies. For observational studies, 38 of 39 studies were at moderate or high risk of bias in at least one domain. For randomized trials, three of four studies were at moderate or high risk of bias in at least one domain. The distribution of the components that described study quality is summarized in Supplemental Tables 2 and 3.
Incidence of Primary Outcomes
All complication rates reported by study are presented in Supplemental Table 4. Below we report summary statistics. When ≥2 event rates were reported for a specific subgroup, we calculated the median event rate for subgroups of nonelderly and elderly patients, lower and upper arm fistulas, as well as buttonhole and rope ladder cannulation (Supplemental Table 5).
Aneurysm
The median rate of aneurysm was 0.04 events per 1000 patient days (ranging from 0 to 3.01; IQR=0.06) among 14 unique cohorts (n=1827 fistulas; Supplemental Figure 2). Van Loon et al.13 reported the highest rate of aneurysm (3.01 per 1000 patient days) among patients using rope ladder cannulation. The next highest rate was reported by the same study for buttonhole cannulation at a rate of 0.13 events per 1000 patient days.13
Infection
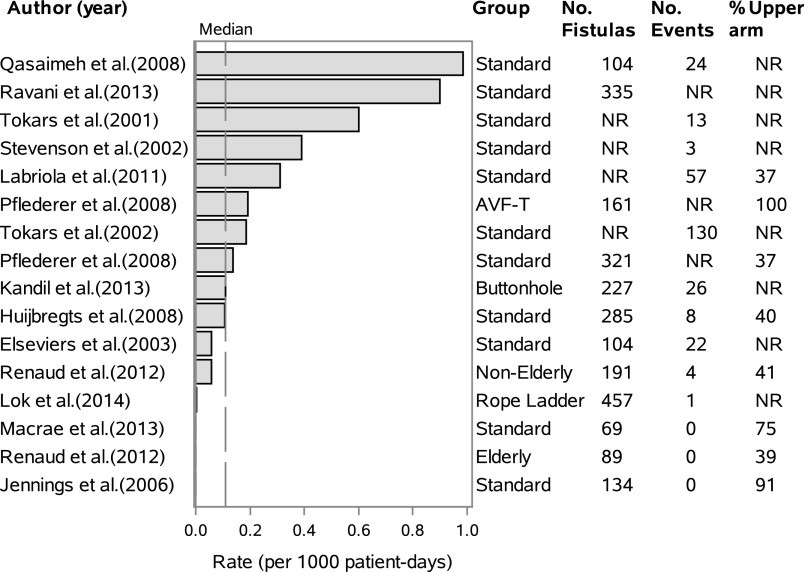
Twenty-three studies reported the incident rate of infection for 28 unique cohorts. The median rate of total infections was 0.11 infections per 1000 patient days (range 0–0.98; IQR=0.29) among 16 unique cohorts (n>6439 fistulas; Figure 1). However, Ravani et al. reported an event rate of 3, 1.7, and 0.9 infections per 1000 patient days in the first 1–3, 3–6, and 6–12 months of starting dialysis, respectively. Only the latter event rate was entered in the overall median rate.
Figure 1.
Studies reporting the incident rate for all types of infections per 1000 patient days. Dashed line refers to the median event rate per 1000 patient days. AVF-T, transposed arteriovenous fistula; buttonhole, all patients cannulated using a buttonhole technique; elderly, ≥65 years; rope ladder, all patients cannulated using a rope ladder technique; standard, no specific cohort followed.
The median rate for bloodstream infection was 0.05 events per 1000 patient days (range 0–0.55; IQR=0.08) among 9 cohorts (n>753 fistulas; Supplemental Figure 3). The median rate for vascular access site infections was 0.03 events per 1000 patient days (range 0–0.26; IQR=0.05) among 14 unique cohorts (n>771 fistulas; Supplemental Figure 4). Using buttonhole cannulation, the median rate of infection was 0.17 (two studies; N fistulas=302) compared with 0.001 (two studies; N fistulas=527) events per 1000 patient days for rope ladder cannulation.
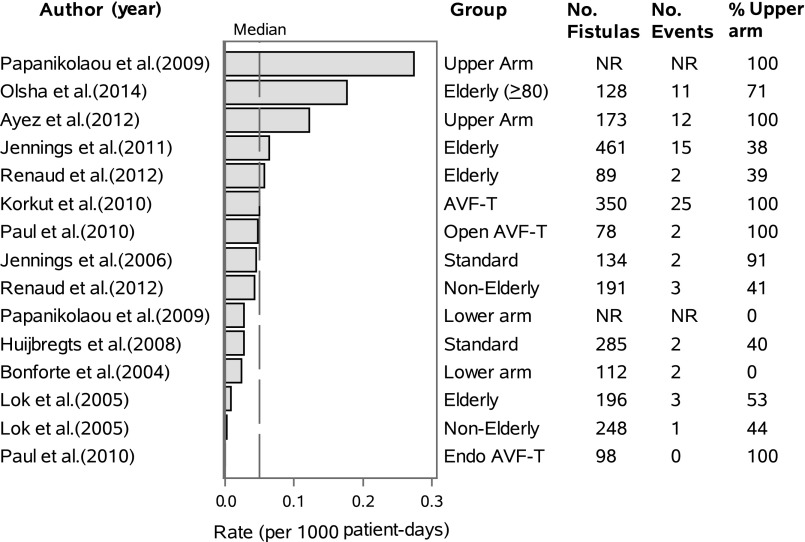
Ischemic Steal Syndrome
Eleven studies reported event rates of ischemic steal syndrome for 15 unique cohorts (n>2543; Figure 2). The median incident rate of ischemic steal syndrome was 0.05 events per 1000 patient days (range 0–0.27; IQR=0.04). The highest rates were 0.18 and 0.27 events per 1000 patient days reported for elderly patients (≥80 years) and those with an upper arm fistula, respectively.
Figure 2.
Studies reporting the incident rate for ischemic steal syndrome per 1000 patient days. Dashed line refers to the median event rate per 1000 patient days. AVF-T, transposed arteriovenous fistula; elderly, ≥65 years unless otherwise specified; endo AVF-T, fistula transposition of a deep vein through endoscopic procedure; lower arm, cohort made up of all lower arm fistulas; open AVF-T, fistula transposition of a deep vein through a long open incision; standard, no specific cohort followed; upper arm, cohort made up of all upper arm fistulas.
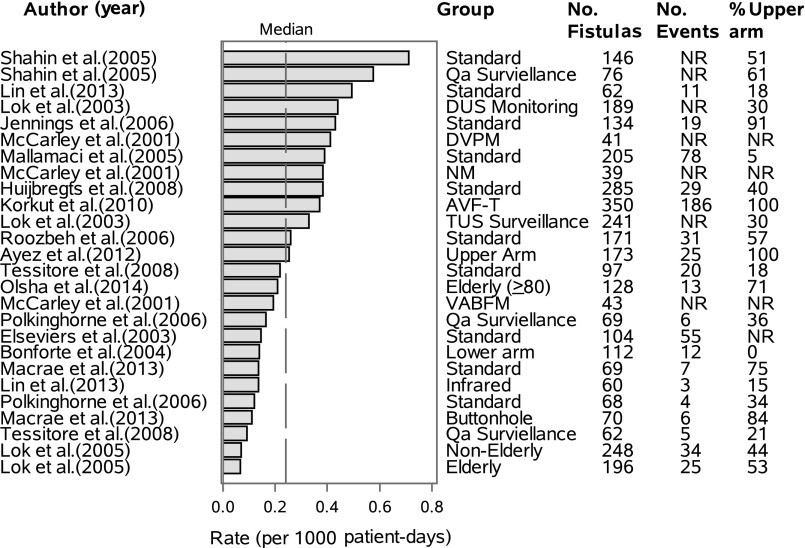
Thrombosis
Fifteen studies reported event rates of thrombosis in 26 unique cohorts (n=4232 fistulas; Figure 3). The median thrombosis rate was 0.24 events per 1000 patient days (range 0.07–0.71; IQR=0.25). Patients undergoing vascular access surveillance (e.g., Qa surveillance) had a median thrombosis rate of 0.33 events per 1000 patient days (seven groups; 721 fistulas). Lin et al.14 reported 1.43 thrombotic events per 1000 patient days rate at 3 months compared with 0.49 events per 1000 patient days at 12 months (only the event rate at 12 months was included in the median calculation above). A number of studies included prevalent patients and thus did not report thrombotic events occurring before or shortly after starting dialysis.
Figure 3.
Studies reporting the incident rate for thrombosis per 1000 patient days. Dashed line refers to the median event rate per 1000 patient days. AVF-T, transposed arteriovenous fistula; buttonhole, all patients cannulated using a buttonhole technique; DUS monitoring, duplex ultrasound monitoring of blood flow; DVPM, dynamic venous pressure monitoring; elderly, ≥65 years unless otherwise specified; infrared, patients received far infrared therapy 3 times weekly for a year; lower arm, cohort made up of all lower arm fistulas; NM, no monitoring (standard care); Qa surveillance, access blood flow monitoring; standard, no specific cohort followed; TUS surveillance, transonic ultrasound monitoring of blood flow; upper arm, cohort made up of all upper arm fistulas; VABFM, vascular access blood flow monitoring.
Venous Hypertension
Only one study reported an event rate of 0.03 venous hypertensive events per 1000 patient days. However, it should be noted that arm edema was included as an event. This cohort consisted of incident patients (n=350 fistulas) with transposed upper arm fistulas with a mean age of 58 years.15
Incidence of Secondary Outcomes
Endovascular interventions (34 unique cohorts; n=3930) and surgical (27 unique cohorts; n=2886) revisions were the most commonly reported secondary outcomes. Endovascular interventions included angioplasty (with or without thrombectomy), stenting, and mechanical thrombolysis. The median event rates were 0.82 (range 0–7.42; IQR=1.39) and 0.19 (range 0–0.77; IQR=0.15) per 1000 patient days for endovascular interventions and surgical revisions, respectively. All-cause mortality (13 unique cohorts; n=1880 fistulas), bleeding (seven unique cohorts; n>1672 fistulas), and total fistula complications (six unique cohorts; n>1666) were reported at a median rate of 0.33 (range 0.09–0.64; IQR=0.11), 0.06 (range 0.02–0.11; IQR=0.05), and 0.56 (range 0.13–1.56; IQR=0.79) per 1000 patient days, respectively. Other outcomes such as catheter insertions, fistula ligation due to high cardiac output, difficult cannulations, hematomas, and hospitalizations were infrequently reported (Supplemental Table 4). No study reported on pulmonary hypertension or heart failure.
Discussion
Our review identified 61 unique cohorts that reported on the fistula event rate of aneurysms, infections, steal syndrome, thrombosis, venous hypertension, and our secondary outcomes among patients using a fistula. We identified three important findings: (1) the contemporary rates of complications in fistulae; (2) the critical need for standardized definitions to report complication rates in order to allow proper evaluation of these outcomes across studies; and (3) a clear need to improve reporting and data quality of observational data in the area of vascular access.
Despite the burden of vascular access complications on patients and the healthcare system, there remains a poor consensus on the incidence risk and factors associated with increased rates of fistula complications. The wide variation in complication event rates across studies is attributed to variation in definitions, inconsistent reporting, and differences in patient populations.
With regard to fistula aneurysmal complications, repeated punctures in a clustered area can weaken the vascular access wall and cause aneurysm formation. Aneurysmal dilatation can occur naturally over time because of the higher blood flow and the process may be accelerated by raising the pressure within the fistula. A previous review documented an aneurysm rate between 5% and 6% (no units were provided), a much higher rate than our median rate of 1.5% per year (0.04 per 1000 patient days).16 Aneurysms generally require surgical repair if there is evidence of loss of skin integrity or ulceration. Left untreated, aneurysms are at risk of rupture and serious hemorrhage, as well as limiting the available sites for cannulation. If inadvertently traumatized, the aneurysm may rupture which can be fatal due to exsanguination.17,18
The clinical practice guidelines for the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF/KDOQI) and the Canadian Society of Nephrology (CSN) recommend that the infection rate should not exceed 0.01 events per patient year (0.027 per 1000 patient days).1,2 On the basis of the evidence from the current literature, the rate of infection was higher for 23 out of 30 cohorts compared with recommended rates proposed by practice guidelines. We also found that patients cannulated using the buttonhole technique had a much higher rate of infection compared with rope ladder cannulation. Similar results were found in a recent randomized controlled trial that found 17% of patients had an infection when using buttonhole compared with 0% using the rope ladder technique.19 Compared with catheters and arteriovenous (AV) grafts, fistulas have lower rates of infection. Previous studies have shown that the rate of catheter infection ranges from 5% to 18% per patient year but this depends on the duration of catheter use.20,21 Similarly, AV-grafts may be at a higher risk for infections.2,22 The rate of local and bacteremic infections for AV-grafts can range between 11% and 20% per patient year.23–26
Ischemic steal syndrome is another important complication of fistulas with significant patient implications including pain and loss of access or extremity function. The NKF/KDOQI and CSN have made no recommendations for target rates of ischemic steal syndrome. Previous studies have reported symptomatic ischemic steal occurrence to range between 1% and 2% for lower arm fistulas and between 5% and 10% among patients using an upper arm fistula.27–32 Indeed, we found that as the proportion of upper arm fistulas increased, the rate of ischemic steal syndrome increased. We found that the rate of ischemic steal syndrome was similar to estimates reported in the NKF/KDOQI guidelines (1%–4% of patients) and other studies.2 Compared with AV-grafts, fistulas have a two-fold lower risk of developing ischemic steal syndrome.2,22,33
Thrombosis is a common early and late fistula complication that can lead to fistula loss. The current NKF/KDOQI and CSN guidelines recommend that center-specific thrombosis rate for the fistula should not exceed 0.25 events per patient year (0.69 per 1000 patient days).34 Among studies included in our review, the thrombosis rates observed were generally lower (with the exception of two studies) than the target rates recommended by practice guidelines. Furthermore, the rates of thrombosis observed in studies before 2000 were also comparable to rates reported in our study.35,36 Compared with AV-grafts, fistulas have lower rates of thrombotic events. Previous reports have reported graft thrombosis to exceeded 0.8 events per patient year (2.2 events per 1000 patient days).37–39
The most common cause of venous hypertension is central stenosis secondary to placement of central venous catheters and devices.40,41 Symptoms of venous hypertension include finger and hand edema that may progress to limit upper extremity mobility. Beyond swelling, extremely advanced stages of this complication can lead to hand and extremity discoloration and even venous gangrene.42 This complication may be under-reported and requires more attention in future studies where they explicitly report its definition, diagnosis, and occurrence.
Studies included in our review varied substantially in quality, outcome definitions, and patient population. Accordingly, the rate of fistula complications varied and may reflect selection bias of study participants, differences in clinical practice, inconsistent levels of vascular access care and monitoring across facilities, and variable case definitions. Despite published recommendations for standardized vascular access reporting,43–45 the majority of studies failed to report definition of outcomes and only a smaller number of studies used published standardized definitions.
In this review, we do not report on fistula nonmaturation or primary failure. We recently published a separate systematic review and meta-analysis, indicating primary failure occurs in approximately 23% (95% confidence interval [95% CI], 18% to 28%) of created fistulas.6 We also found the primary patency rate was 60% (95% CI, 56% to 64%) at 1 year and 51% (95% CI, 44% to 58%) at 2 years. The secondary patency rate was 71% (95% CI, 64% to 78%) at 1 year and 64% (95% CI, 56% to 73%) at 2 years.
Our review has a number of strengths compared with prior narrative reviews on this topic. We conducted a comprehensive search of the literature and systematically identified relevant studies in accordance with published guidelines and a published prespecified protocol. We prespecified a wide range of primary and secondary outcomes that are relevant to patients, physicians, and administrators. To our knowledge, this is the first review that has examined fistula complication in the contemporary dialysis population. Previous narrative reviews have included studies from the 1970s when patient characteristics, clinical focus, and policies differed from the current dialysis environment. Furthermore, previous reviews reported the proportion of patients with an infection, ischemic steal syndrome, and thrombosis events as opposed to the event rate.46–49
Our study does have limitations. Heterogeneity between studies precluded precise estimates of complication incidence rates and precluded the pooling of risk factors; it has been suggested that pooling results when not warranted may lead to misleading conclusions.50 We restricted this review to articles published in English; whether this introduced some bias is controversial.51 We also did not query prospective databases (e.g., Dialysis Outcomes and Practice Patterns Study, Centers for Medicare & Medicaid Services, etc.) without peer-reviewed published data. Finally, when calculating event rates, we assumed a constant hazard ratio; however, it has been shown that hazard ratios of fistula outcomes can vary over time, with higher hazard rates being observed within the first 6 months of dialysis.52
The quality of primary studies inherently limits the conclusions that can be drawn from this review. We were also unable to differentiate complications that occurred in fistulas that were created in the predialysis period and a number of studies reported outcomes for patients already on dialysis. Risk factors for fistula complications which include patient comorbidities, vessel characteristics, surgeons’ experience, and nursing experience with cannulation were generally not reported. Additionally, factors on timing between fistula creation and fistula use, timing of vascular access interventions, and clinical monitoring or surveillance practices were also not reported. These variables may have explained some of the heterogeneity in the literature. The paucity in reporting of risk factors impairs our ability to identify patients at highest risk for complications.
We found that the rates of aneurysm, ischemic steal syndrome, and thrombosis rates were similar or less than previously published reports and those reported in NKF/KDOQI guidelines (update 2006). However, the infection rate was much higher than the range recommended by NKF/KDOQI guidelines, although this varied by cannulation technique. We found marked variability in complications rates in part due to the poor quality of studies, significant heterogeneity of study populations, and inconsistent definitions. This information on complication rates is critical to informing patient-physician decision making and patient consent, and guiding resource allocation for vascular access care. Having accurate information on fistula complications and patients at highest risk for complications is important in making informed decisions and choosing the appropriate vascular access on the basis of the risks.
There is an urgent need to standardize reporting of methods, baseline patient and access characteristics, and complications of vascular access in future clinical studies.
Concise Methods
We conducted and reported this systematic review according to published guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses [PRISMA] checklist: Supplemental Table 1) using a prespecified protocol (CRD42014010444 and Supplemental Item 1).53,55 Description of studies eligible for review, data sources, study selection, data abstraction, and quality assessment used for this review have been reported elsewhere.6,55
Briefly, we included English-language studies indexed in Medline that followed patients prospectively (observational cohort, randomized control trials, or surveillance programs) for a period of at least 3 months. Studies included were published between January 1, 2000 and December 31, 2014 and reported on ≥100 fistulas. Two blinded independent reviewers (A.A.A. and one of A.R.L. or J.C.Z.) selected the studies using a standardized form with a third reviewer adjudicating discrepancies when necessary. We assessed risk of bias using previously reported methods and modified these tools as appropriate,56,57 and abstracted data on study methodology and cohort characteristics. All studies must have reported on at least one of the primary outcomes: (1) aneurysm, (2) infections, (3) ischemic steal syndrome, (4) thrombosis, or (5) venous hypertension among hemodialysis patients using a fistula. When reported, we also captured the following secondary outcomes: (1) difficult cannulation, (2) bleeding, (3) hematoma, (4) catheter insertion, (5) endovascular intervention, (6) surgical revisions, (7) hospitalization (infection-related), (8) hospitalization (VA-related), (9) hospitalizations (all-cause), (10) pulmonary hypertension, (11) high cardiac output, (12) heart failure, (13) all-cause mortality, and (14) total complications.
Study Definitions
We used outcome definitions in accordance with the Society of Vascular Surgery (SVS) and the American Association of Vascular Surgery as well as the North American Vascular Access Consortium (NAVAC) (below).43,44 The SVS and NAVAC did not report a definition for aneurysm. When the study definition was not in accordance with previously published definitions, we noted the differences in our tables. Definitions for infections and venous hypertension were intentionally kept broad to include all variations in the published literature.
Primary Outcome Definitions
(1) Aneurysm: Diffuse and progressive degeneration of the vascular access site. Patient has signs of bleeding, infection, or ulceration.16,45 (2) Infections: Definite or probable local vascular access infections, vascular access–related sepsis, bacteremia, or a composite of these infections. (3) Ischemic steal syndrome (SVS): One or more clinical manifestations of: pain, ischemic neuropathy, ulceration, and gangrene felt to be related to a fistula diverting blood from the distal circulation resulting in a zone of arterial insufficiency in the tissues distal to the fistula.44 (4) Thrombosis (SVS and NAVAC): Absence of bruit or thrill, using auscultation and palpation, throughout systole and diastole at least 8 cm proximal to the arteriovenous anastomosis.43,44 (5) Venous hypertension (SVS): High pressure in veins due to damage to venous system often presenting with arm and hand swelling; dusky, rubber color of the hand; and dilated veins on the arm and/or chest wall.
Summary Statistics
We report the median and range for the event rate (per 1000 patient days) of an outcome. Because of differences in sampled populations, outcome definitions, prevalence of comorbid conditions, and variable sample selection criteria, it was not appropriate to calculate a summary statistic on the basis of the weighted average. When incidence rates were not reported, we calculated the overall follow-up time (denominator) by multiplying the mean follow-up time by the number of patients. We used the overall follow-up time to calculate the event rate per 1000 patient days. Using this method, we assumed that the hazard rate of developing a particular outcome was constant across individuals and over time.
Disclosures
None.
Supplementary Material
Acknowledgments
A.A.A. is supported by the Kidney Foundation of Canada Allied Health Doctoral Fellowship.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2016040412/-/DCSupplemental.
References
- 1.Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, Culleton BF; Canadian Society of Nephrology Committee for Clinical Practice Guidelines : Hemodialysis clinical practice guidelines for the Canadian Society of Nephrology. J Am Soc Nephrol 17[Suppl 1]: S1–S27, 2006 [DOI] [PubMed] [Google Scholar]
- 2.Vascular Access 2006 Work Group : Clinical practice guidelines for vascular access. Am J Kidney Dis 48[Suppl 1]: S176–S247, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Tordoir J, Canaud B, Haage P, Konner K, Basci A, Fouque D, Kooman J, Martin-Malo A, Pedrini L, Pizzarelli F, Tattersall J, Vennegoor M, Wanner C, ter Wee P, Vanholder R: EBPG on vascular access. Nephrol Dial Transplant 22[Suppl 2]: ii88–ii117, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Lok CE, Sontrop JM, Tomlinson G, Rajan D, Cattral M, Oreopoulos G, Harris J, Moist L: Cumulative patency of contemporary fistulas versus grafts (2000-2010). Clin J Am Soc Nephrol 8: 810–818, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huijbregts HJTT, Bots ML, Wittens CHAA, Schrama YC, Moll FL, Blankestijn PJ; CIMINO study group : Hemodialysis arteriovenous fistula patency revisited: Results of a prospective, multicenter initiative. Clin J Am Soc Nephrol 3: 714–719, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Jaishi AA, Oliver MJ, Thomas SM, Lok CE, Zhang JC, Garg AX, Kosa SD, Quinn RR, Moist LM: Patency rates of the arteriovenous fistula for hemodialysis: A systematic review and meta-analysis. Am J Kidney Dis 63: 464–478, 2014 [DOI] [PubMed] [Google Scholar]
- 7.Tonelli M, Klarenbach S, Jindal K, Manns B; Alberta Kidney Disease Network : Economic implications of screening strategies in arteriovenous fistulae. Kidney Int 69: 2219–2226, 2006 [DOI] [PubMed] [Google Scholar]
- 8.Lee H, Manns B, Taub K, Ghali WA, Dean S, Johnson D, Donaldson C: Cost analysis of ongoing care of patients with end-stage renal disease: The impact of dialysis modality and dialysis access. Am J Kidney Dis 40: 611–622, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Manns B, Tonelli M, Yilmaz S, Lee H, Laupland K, Klarenbach S, Radkevich V, Murphy B: Establishment and maintenance of vascular access in incident hemodialysis patients: A prospective cost analysis. J Am Soc Nephrol 16: 201–209, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Ravani P, Palmer SC, Oliver MJ, Quinn RR, MacRae JM, Tai DJ, Pannu NI, Thomas C, Hemmelgarn BR, Craig JC, Manns B, Tonelli M, Strippoli GFM, James MT: Associations between hemodialysis access type and clinical outcomes: A systematic review. J Am Soc Nephrol 24: 465–473, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elseviers MM, Van Waeleghem J-P: Identifying vascular access complications among ESRD patients in Europe. A prospective, multicenter study. Nephrol News Issues 17: 61–4, 66,–8, 99, 2003 [PubMed] [Google Scholar]
- 12.Ravani P, Gillespie BW, Quinn RR, MacRae J, Manns B, Mendelssohn D, Tonelli M, Hemmelgarn B, James M, Pannu N, Robinson BM, Zhang X, Pisoni R: Temporal risk profile for infectious and noninfectious complications of hemodialysis access. J Am Soc Nephrol 24: 1668–1677, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Loon MM, Goovaerts T, Kessels AGH, van der Sande FM, Tordoir JHM: Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrol Dial Transplant 25: 225–230, 2010 [DOI] [PubMed] [Google Scholar]
- 14.Lin C-C, Yang W-C, Chen M-C, Liu W-S, Yang C-Y, Lee P-C: Effect of far infrared therapy on arteriovenous fistula maturation: An open-label randomized controlled trial. Am J Kidney Dis 62: 304–311, 2013 [DOI] [PubMed] [Google Scholar]
- 15.Korkut AK, Kosem M: Superficialization of the basilic vein technique in brachiobasilic arteriovenous fistula: Surgical experience of 350 cases during 4 years period. Ann Vasc Surg 24: 762–767, 2010 [DOI] [PubMed] [Google Scholar]
- 16.Stolic R: Most important chronic complications of arteriovenous fistulas for hemodialysis. Med Princ Pract 22: 220–228, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ellingson KD, Palekar RS, Lucero CA, Kurkjian KM, Chai SJ, Schlossberg DS, Vincenti DM, Fink JC, Davies-Cole JO, Magri JM, Arduino MJ, Patel PR: Vascular access hemorrhages contribute to deaths among hemodialysis patients. Kidney Int 82: 686–692, 2012 [DOI] [PubMed] [Google Scholar]
- 18.Lo H-Y, Tan S-G: Arteriovenous fistula aneurysm--plicate, not ligate. Ann Acad Med Singapore 36: 851–853, 2007 [PubMed] [Google Scholar]
- 19.Macrae JM, Ahmed SB, Hemmelgarn BR; Alberta Kidney Disease Network : Arteriovenous fistula survival and needling technique: Long-term results from a randomized buttonhole trial. Am J Kidney Dis 63: 636–642, 2014 [DOI] [PubMed] [Google Scholar]
- 20.Levin A, Mason AJ, Jindal KK, Fong IW, Goldstein MB: Prevention of hemodialysis subclavian vein catheter infections by topical povidone-iodine. Kidney Int 40: 934–938, 1991 [DOI] [PubMed] [Google Scholar]
- 21.Lund GB, Trerotola SO, Scheel PF Jr, Savader SJ, Mitchell SE, Venbrux AC, Osterman FA Jr: Outcome of tunneled hemodialysis catheters placed by radiologists. Radiology 198: 467–472, 1996 [DOI] [PubMed] [Google Scholar]
- 22.Morsy AH, Kulbaski M, Chen C, Isiklar H, Lumsden AB: Incidence and characteristics of patients with hand ischemia after a hemodialysis access procedure. J Surg Res 74: 8–10, 1998 [DOI] [PubMed] [Google Scholar]
- 23.Bhat DJ, Tellis VA, Kohlberg WI, Driscoll B, Veith FJ: Management of sepsis involving expanded polytetrafluoroethylene grafts for hemodialysis access. Surgery 87: 445–450, 1980 [PubMed] [Google Scholar]
- 24.Raju S: PTFE grafts for hemodialysis access. Techniques for insertion and management of complications. Ann Surg 206: 666–673, 1987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kherlakian GM, Roedersheimer LR, Arbaugh JJ, Newmark KJ, King LR: Comparison of autogenous fistula versus expanded polytetrafluoroethylene graft fistula for angioaccess in hemodialysis. Am J Surg 152: 238–243, 1986 [DOI] [PubMed] [Google Scholar]
- 26.Rizzuti RP, Hale JC, Burkart TE: Extended patency of expanded polytetrafluoroethylene grafts for vascular access using optimal configuration and revisions. Surg Gynecol Obstet 166: 23–27, 1988 [PubMed] [Google Scholar]
- 27.Davidson D, Louridas G, Guzman R, Tanner J, Weighell W, Spelay J, Chateau D: Steal syndrome complicating upper extremity hemoaccess procedures: Incidence and risk factors. Can J Surg 46: 408–412, 2003 [PMC free article] [PubMed] [Google Scholar]
- 28.Berman SS, Gentile AT, Glickman MH, Mills JL, Hurwitz RL, Westerband A, Marek JM, Hunter GC, McEnroe CS, Fogle MA, Stokes GK: Distal revascularization-interval ligation for limb salvage and maintenance of dialysis access in ischemic steal syndrome. J Vasc Surg 26: 393–402, discussion 402–404, 1997 [DOI] [PubMed] [Google Scholar]
- 29.Goff CD, Sato DT, Bloch PH, DeMasi RJ, Gregory RT, Gayle RG, Parent FN, Meier GH, Wheeler JR: Steal syndrome complicating hemodialysis access procedures: Can it be predicted? Ann Vasc Surg 14: 138–144, 2000 [DOI] [PubMed] [Google Scholar]
- 30.Konner K, Hulbert-Shearon TE, Roys EC, Port FK: Tailoring the initial vascular access for dialysis patients. Kidney Int 62: 329–338, 2002 [DOI] [PubMed] [Google Scholar]
- 31.DeCaprio JD, Valentine RJ, Kakish HB, Awad R, Hagino RT, Clagett GP: Steal syndrome complicating hemodialysis access. Cardiovasc Surg 5: 648–653, 1997 [DOI] [PubMed] [Google Scholar]
- 32.Zamani P, Kaufman J, Kinlay S: Ischemic steal syndrome following arm arteriovenous fistula for hemodialysis. Vasc Med 14: 371–376, 2009 [DOI] [PubMed] [Google Scholar]
- 33.Akoh JA: Prosthetic arteriovenous grafts for hemodialysis. J Vasc Access 10: 137–147, 2009 [DOI] [PubMed] [Google Scholar]
- 34.III. NKF-K/DOQI Clinical practice guidelines for vascular access: Update 2000. Am J Kidney Dis 37[Suppl 1]: S137–S181, 2001 [DOI] [PubMed] [Google Scholar]
- 35.Kinnaert P, Vereerstraeten P, Toussaint C, Van Geertruyden J: Nine years’ experience with internal arteriovenous fistulas for haemodialysis: A study of some factors influencing the results. Br J Surg 64: 242–246, 1977 [DOI] [PubMed] [Google Scholar]
- 36.Fan PY, Schwab SJ: Vascular access: Concepts for the 1990s. J Am Soc Nephrol 3: 1–11, 1992 [DOI] [PubMed] [Google Scholar]
- 37.Sands J, Young S, Miranda C: The effect of Doppler flow screening studies and elective revisions on dialysis access failure. ASAIO J 38: M524–M527, 1992 [DOI] [PubMed] [Google Scholar]
- 38.Besarab A, Sullivan KL, Ross RP, Moritz MJ: Utility of intra-access pressure monitoring in detecting and correcting venous outlet stenoses prior to thrombosis. Kidney Int 47: 1364–1373, 1995 [DOI] [PubMed] [Google Scholar]
- 39.Schwab SJ, Raymond JR, Saeed M, Newman GE, Dennis PA, Bollinger RR: Prevention of hemodialysis fistula thrombosis. Early detection of venous stenoses. Kidney Int 36: 707–711, 1989 [DOI] [PubMed] [Google Scholar]
- 40.Agarwal AK, Patel BM, Haddad NJ: Central vein stenosis: A nephrologist’s perspective. Semin Dial 20: 53–62, 2007 [DOI] [PubMed] [Google Scholar]
- 41.Criado E, Marston WA, Jaques PF, Mauro MA, Keagy BA: Proximal venous outflow obstruction in patients with upper extremity arteriovenous dialysis access. Ann Vasc Surg 8: 530–535, 1994 [DOI] [PubMed] [Google Scholar]
- 42.Bachleda P, Kojecký Z, Utíkal P, Drác P, Herman J, Zadrazil J: Peripheral venous hypertension after the creation of arteriovenous fistula for haemodialysis. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 148: 85–87, 2004 [DOI] [PubMed] [Google Scholar]
- 43.Lee T, Mokrzycki M, Moist L, Maya I, Vazquez M, Lok CE; North American Vascular Access Consortium : Standardized definitions for hemodialysis vascular access. Semin Dial 24: 515–524, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sidawy AN, Gray R, Besarab A, Henry M, Ascher E, Silva M Jr, Miller A, Scher L, Trerotola S, Gregory RT, Rutherford RB, Kent KC: Recommended standards for reports dealing with arteriovenous hemodialysis accesses. J Vasc Surg 35: 603–610, 2002 [DOI] [PubMed] [Google Scholar]
- 45.Tordoir JH, Mickley V: European guidelines for vascular access: Clinical algorithms on vascular access for haemodialysis. EDTNA ERCA J 29: 131–136, 2003 [DOI] [PubMed] [Google Scholar]
- 46.Dukkipati R, de Virgilio C, Reynolds T, Dhamija R: Outcomes of brachial artery-basilic vein fistula. Semin Dial 24: 220–230, 2011 [DOI] [PubMed] [Google Scholar]
- 47.Dix FP, Khan Y, Al-Khaffaf H: The brachial artery-basilic vein arterio-venous fistula in vascular access for haemodialysis--a review paper. Eur J Vasc Endovasc Surg 31: 70–79, 2006 [DOI] [PubMed] [Google Scholar]
- 48.Mousa AY, Dearing DD, Aburahma AF: Radiocephalic fistula: Review and update. Ann Vasc Surg 27: 370–378, 2013 [DOI] [PubMed] [Google Scholar]
- 49.Siddiky A, Sarwar K, Ahmad N, Gilbert J: Management of arteriovenous fistulas. BMJ 349: g6262, 2014 [DOI] [PubMed] [Google Scholar]
- 50.Ioannidis JP: Meta-research: The art of getting it wrong. Res Synth Methods 1: 169–184, 2010 [DOI] [PubMed] [Google Scholar]
- 51.Moher D, Pham B, Klassen TP, Schulz KF, Berlin JA, Jadad AR, Liberati A: What contributions do languages other than English make on the results of meta-analyses? J Clin Epidemiol 53: 964–972, 2000 [DOI] [PubMed] [Google Scholar]
- 52.Ravani P, Parfrey P, MacRae J, James M, Quinn R, Malberti F, Brunori G, Mandolfo S, Tonelli M, Hemmelgarn B, Manns B, Barrett B: Modeling survival of arteriovenous accesses for hemodialysis: Semiparametric versus parametric methods. Clin J Am Soc Nephrol 5: 1243–1248, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group : Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol 62: 1006–1012, 2009 [DOI] [PubMed] [Google Scholar]
- 54.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB: Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283: 2008–2012, 2000 [DOI] [PubMed] [Google Scholar]
- 55.Al-Jaishi AA, Oliver MJ, Liu AR, Garg AX, Zhang JC, Thomas SM, Moist LM: Complication rates of the arteriovenous fistula: a systematic review. PROSPERO 2014. Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014010444. Accessed March 31, 2016
- 56.Busse J, Guyatt G: Instrument for assessing risk of bias in cohort studies. Available from: http://www.evidencepartners.com/resources/. Accessed March 31, 2016
- 57.Higgins JPT, Green S, editors: Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from: http://handbook.cochrane.org/front_page.htm. Accessed March 31, 2016
- 58.McCarley P, Wingard RL, Shyr Y, Pettus W, Hakim RM, Ikizler TA: Vascular access blood flow monitoring reduces access morbidity and costs. Kidney Int 60: 1164–1172, 2001 [DOI] [PubMed] [Google Scholar]
- 59.Tokars JII, Light P, Anderson J, Miller ERR, Parrish J, Armistead N, Jarvis WRR, Gehr T: A prospective study of vascular access infections at seven outpatient hemodialysis centers. Am J Kidney Dis 37: 1232–1240, 2001 [DOI] [PubMed] [Google Scholar]
- 60.Dixon BSBS, Novak L, Fangman J: Hemodialysis vascular access survival: Upper-arm native arteriovenous fistula. Am J Kidney Dis 39: 92–101, 2002 [DOI] [PubMed] [Google Scholar]
- 61.Ravani P, Marcelli D, Malberti F: Vascular access surgery managed by renal physicians: The choice of native arteriovenous fistulas for hemodialysis. Am J Kidney Dis 40: 1264–1276, 2002 [DOI] [PubMed] [Google Scholar]
- 62.Saxena AK, Panhotra BR, Venkateshappa CK, Sundaram DS, Naguib M, Uzzaman W, Al Mulhim K: The impact of nasal carriage of methicillin-resistant and methicillin-susceptible Staphylococcus a ureus (MRSA & MSSA) on vascular access-related septicemia among patients with type-II diabetes on dialysis. Ren Fail 24: 763–777, 2002 [DOI] [PubMed] [Google Scholar]
- 63.Stevenson KB, Hannah EL, Lowder CA, Adcox MJ, Davidson RL, Mallea MC, Narasimhan N, Wagnild JP: Epidemiology of hemodialysis vascular access infections from longitudinal infection surveillance data: Predicting the impact of NKF-DOQI clinical practice guidelines for vascular access. Am J Kidney Dis 39: 549–555, 2002 [DOI] [PubMed] [Google Scholar]
- 64.Taylor G, Gravel D, Johnston L, Embil J, Holton D, Paton S; Canadian Hospital Epidemiology Committee. Canadian Nosocomial Infection Surveillance Program : Prospective surveillance for primary bloodstream infections occurring in Canadian hemodialysis units. Am J Infect Control 23: 716–720, 2002 [DOI] [PubMed] [Google Scholar]
- 65.Tokars JI, Miller ER, Stein G: New national surveillance system for hemodialysis-associated infections: Initial results. Am J Infect Control 30: 288–295, 2002 [DOI] [PubMed] [Google Scholar]
- 66.Lok CE, Bhola C, Croxford R, Richardson RM: Reducing vascular access morbidity: A comparative trial of two vascular access monitoring strategies. Nephrol Dial Transplant 18: 1174–1180, 2003 [DOI] [PubMed] [Google Scholar]
- 67.Saxena AK, Panhotra BR: The prevalence of nasal carriage of Staphylococcus aureus and associated vascular access-related septicemia among patients on Hemodialysis in Al-Hasa region of Saudi Arabia. Saudi J Kidney Dis Transpl 14: 30–38, 2003 [PubMed] [Google Scholar]
- 68.Bonforte G, Zerbi S, Surian M: The middle-arm fistula: A new native arteriovenous vascular access for hemodialysis patients. Ann Vasc Surg 18: 448–452, 2004 [DOI] [PubMed] [Google Scholar]
- 69.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J; CHOICE Study : Type of vascular access and survival among incident hemodialysis patients: The Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 16: 1449–1455, 2005 [DOI] [PubMed] [Google Scholar]
- 70.Gilad J, Eskira S, Schlaeffer F, Vorobiov M, Marcovici A, Tovbin D, Zlotnik M, Borer A: Surveillance of chronic haemodialysis-associated infections in southern Israel. Clin Microbiol Infect 11: 547–552, 2005 [DOI] [PubMed] [Google Scholar]
- 71.Lok CE, Oliver MJ, Su J, Bhola C, Hannigan N, Jassal SV: Arteriovenous fistula outcomes in the era of the elderly dialysis population. Kidney Int 67: 2462–2469, 2005 [DOI] [PubMed] [Google Scholar]
- 72.Mallamaci F, Bonanno G, Seminara G, Rapisarda F, Fatuzzo P, Candela V, Scudo P, Spoto B, Testa A, Tripepi G, Tech S, Zoccali C: Hyperhomocysteinemia and arteriovenous fistula thrombosis in hemodialysis patients. Am J Kidney Dis 45: 702–707, 2005 [DOI] [PubMed] [Google Scholar]
- 73.Shahin H, Reddy G, Sharafuddin M, Katz D, Franzwa BS, Dixon BS: Monthly access flow monitoring with increased prophylactic angioplasty did not improve fistula patency. Kidney Int 68: 2352–2361, 2005 [DOI] [PubMed] [Google Scholar]
- 74.Jennings WC: Creating arteriovenous fistulas in 132 consecutive patients: Exploiting the proximal radial artery arteriovenous fistula: Reliable, safe, and simple forearm and upper arm hemodialysis access. Arch Surg 141: 27–32, discussion 32, 2006 [DOI] [PubMed] [Google Scholar]
- 75.Polkinghorne KR, Lau KKP, Saunder A, Atkins RC, Kerr PG: Does monthly native arteriovenous fistula blood-flow surveillance detect significant stenosis--a randomized controlled trial. Nephrol Dial Transplant 21: 2498–2506, 2006 [DOI] [PubMed] [Google Scholar]
- 76.Roozbeh J, Serati A-R, Malekhoseini S-A: Arteriovenous fistula thrombosis in patients on regular hemodialysis: A report of 171 patients. Arch Iran Med 9: 26–32, 2006 [PubMed] [Google Scholar]
- 77.Pflederer TA, Kwok S, Ketel BL, Pilgram T: A comparison of transposed brachiobasilic fistulae with nontransposed fistulae and grafts in the fistula first era. Semin Dial 21: 357–363, 2008 [DOI] [PubMed] [Google Scholar]
- 78.Qasaimeh GRGR, El Qaderi S, Al Omari G, Al Badadweh M: Vascular access infection among hemodialysis patients in Northern Jordan: Incidence and risk factors. South Med J 101: 508–512, 2008 [DOI] [PubMed] [Google Scholar]
- 79.Tessitore N, Bedogna V, Poli A, Mantovani W, Lipari G, Baggio E, Mansueto G, Lupo A: Adding access blood flow surveillance to clinical monitoring reduces thrombosis rates and costs, and improves fistula patency in the short term: A controlled cohort study. Nephrol Dial Transplant 23: 3578–3584, 2008 [DOI] [PubMed] [Google Scholar]
- 80.Koksoy C, Demirci RK, Balci D, Solak T, Köse SK: Brachiobasilic versus brachiocephalic arteriovenous fistula: A prospective randomized study. J Vasc Surg 49: 171–177.e5, 2009 [DOI] [PubMed] [Google Scholar]
- 81.Papanikolaou V, Papagiannis A, Vrochides D, Imvrios G, Gakis D, Fouzas I, Antoniadis N, Takoudas D: The natural history of vascular access for hemodialysis: A single center study of 2,422 patients. Surgery 145: 272–279, 2009 [DOI] [PubMed] [Google Scholar]
- 82.Paul EM, Sideman MJ, Rhoden DH, Jennings WC: Endoscopic basilic vein transposition for hemodialysis access. J Vasc Surg 51: 1451–1456, 2010 [DOI] [PubMed] [Google Scholar]
- 83.Jennings WC, Landis L, Taubman KE, Parker DE: Creating functional autogenous vascular access in older patients. J Vasc Surg 53: 713–719, discussion 719, 2011 [DOI] [PubMed] [Google Scholar]
- 84.Labriola L, Crott R, Desmet C, André G, Jadoul M: Infectious complications following conversion to buttonhole cannulation of native arteriovenous fistulas: A quality improvement report. Am J Kidney Dis 57: 442–448, 2011 [DOI] [PubMed] [Google Scholar]
- 85.Ng LJ, Chen F, Pisoni RL, Krishnan M, Mapes D, Keen M, Bradbury BD: Hospitalization risks related to vascular access type among incident US hemodialysis patients. Nephrol Dial Transplant 26: 3659–3666, 2011 [DOI] [PubMed] [Google Scholar]
- 86.Ayez N, van Houten VA, de Smet AA, van Well AM, Akkersdijk GP, van de Ven PJ, Fioole B: The basilic vein and the cephalic vein perform equally in upper arm arteriovenous fistulae. Eur J Vasc Endovasc Surg 44: 227–231, 2012 [DOI] [PubMed] [Google Scholar]
- 87.Renaud CJ, Pei JH, Lee EJC, Robless PA, Vathsala A: Comparative outcomes of primary autogenous fistulas in elderly, multiethnic Asian hemodialysis patients. J Vasc Surg 56: 433–439, 2012 [DOI] [PubMed] [Google Scholar]
- 88.Kandil H, Collier S, Yewetu E, Cross J, Davenport A: Arteriovenous fistula survival with buttonhole (constant site) cannulation for hemodialysis access [Internet]. ASAIO J 60: 95–98. Available at: http://www.ncbi.nlm.nih.gov/pubmed/?term=24281124. Accessed December 1, 2015 [DOI] [PubMed]
- 89.Albuquerque SE, Cavalcante RS, Ponce D, Fortaleza CMCB: Epidemiology of healthcare-associated infections among patients from a hemodialysis unit in southeastern Brazil. Braz J Infect Dis 18: 327–330, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Agarwal A, Mantell M, Cohen R, Yan Y, Trerotola S, Clark TW: Outcomes of single-stage compared to two-stage basilic vein transposition fistulae. Semin Dial 27: 298–302, 2014 [DOI] [PubMed] [Google Scholar]
- 91.Badawy DA, Mowafi HS, Al-Mousa HH: Surveillance of dialysis events: 12-month experience at five outpatient adult hemodialysis centers in Kuwait. J Infect Public Health 7: 386–391, 2014 [DOI] [PubMed] [Google Scholar]
- 92.Lok CE, Sontrop JM, Faratro R, Chan CT, Zimmerman DL: Frequent hemodialysis fistula infectious complications. Nephron Extra 4: 159–167, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Olsha O, Hijazi J, Goldin I, Shemesh D: Vascular access in hemodialysis patients older than 80 years. J Vasc Surg 61: 177–183, 2015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.