Abstract
A wide discrepancy exists in India between the existing mental healthcare repertoire and the alarmingly high burden of individuals requiring immediate attention from requisite mental healthcare services. Providing equitable mental healthcare across a vast country characterized by profound cultural variations and territorial caveats has remained a major public health concern. Against this gloomy backdrop, the emergence of distant communications technology offers solace and optimism as an ingenious approach to bridge the existing gap between clients and mental health professionals. Using inexpensive equipment and basic technical knowhow, telepsychiatry expands the scope of the discipline to distant and hazy suburbs and villages from its urban centers of excellence. The current academic endeavor intends to perform a systematic review of relevant literature from India as well as from other countries. The various models of telepsychiatry-both asynchronous and synchronous models-in practice have been elaborated on with a focus on effectiveness, feasibility and acceptability of this latest modality. A sincere attempt to chronicle the remarkable journey of telepsychiatry in India, beginning in the dawn of the 21st century to the current Indian scenario, has been made. The legal and ethical issues, along with a few words of caution and contemplation, have been briefly touched on. A set of recommendations has been provided with the hope that policy makers and administrators in the domain of mental health may benefit from them. It is anticipated that telepsychiatry will be adequately utilized in India to tackle the raging menace of inadequate mental healthcare services.
Keywords: India, models, systematic review, telepsychiatry
INTRODUCTION
Since antiquity human ingenuity has perpetually thrived to transcend the limits of sensory experience. The folklore and mythology of diverse dwellings are studded with vivid accounts of extracampine communications such as prophecies and sermons elaborated by symbolism and imagery. The idea of stretching out to those beyond the boundaries of vicinity has spurred intuitive minds for centuries. The ancients used light reflections and smoke signals to communicate crucial information with their distant compatriots and neighbors. With evolution more emphasis was laid on innovative methods of effective communication just as the stream of medicine became more sophisticated and specialized. The advent of information and communication technology coupled with the menace of the inequity of access to healthcare provided the backdrop for the germination of “telemedicine” - a breakthrough that promised to touch countless lives while overcoming geographical barrier in the delivery of healthcare.
According to the United States Food and Drug Administration, “Telemedicine refers to consultative services to individual patients and the transmission of information related to care, over distance, using telecommunications technologies. It incorporates direct clinical, preventive, diagnostic and therapeutic services and treatment; consultative and follow-up services; remote monitoring of patients; rehabilitative services; and patient education.”[1] In simpler terms, it is the use of multimedia technology (voice, video, and data) to deliver healthcare services.
It is noteworthy that throughout history, connectivity has been a central feature of medical care in general and mental healthcare in particular. Telemedicine has had a fascinating journey originating from the humble roots in semaphore to the telegraph to the radio to advanced digital communication technologies of today. Its scope has expanded from a simple tool of connectivity to an agent of versatility as is evident from its increasing role in patient empowerment and clinical decision support. In this article, we look at telemedicine not just as a technological advancement but also will evaluate how it answers to many enduring problems in healthcare delivery such as inequitable access to healthcare at the community level and issues relating to quality and cost of healthcare services. The story of early telemedicine is replete with anecdotes from the lives of legendary discoverers such as Willem Einthoven and Alexander Graham Bell.[2] Anecdotal claims have been made that the first call made by Dr. Bell to his assistant Mr. Watson set the ball rolling for the nascent field of telemedicine when a plea for medical help may have been sought![2] The Dutch genius Einthoven, who won the Nobel Prize in 1924, is credited with pioneering techniques in the domain of telecardiology.[3] A careful analysis of this journey reveals the persistence of conflicting themes of continuity and change in the growth of this discipline. It is characterized by the convergence and syncretization of previous technologies on one hand and the emergence of progressive new approaches on the other. It has endured crests and troughs in its course which has been marked by periods of advancement alternating with those of quiet abandonment. It was in the Netherlands of the early 1900s that pioneering work was done to send heart rhythms via telephone lines. Radio consultations from Norway, France, and Italy for people aboard ships and in distant islands were introduced in the 1920s and continued gaining momentum until the 1950s. The first wave of organized telemedicine programs, with its onset in the late 1950s in the United States and Canada, lasted for two decades before an abrupt halt due to unavailability of funds.[4] The last wave of organized telemedicine began nearly two decades back and with advances in global communication systems, it has penetrated many hitherto uncharted regions of the world.
Today telemedicine lies at the forefront of the advancement of medicine as a scientific discipline. Its goal is not only increased access but also improved quality and effectiveness of healthcare. It also offers promise as an innovative approach to integrate complex health systems. It is indeed a modality with implications in both individual wellbeing and public health systems.
The origins of telepsychiatry may be traced in the use of the closed circuit, two-way television for clinical, academic as well as emergency services during the 1960s in the United States.[5] This has been followed by the Internet era and the age of sophisticated distant communication technologies such as E-mail, instant messaging, online forums, and websites and blogs dedicated to address the mental health needs of the users. Community-based initiatives intended to utilize the advances in communication technology have been attempted in various parts of the world. With the passage of time, telepsychiatry has expanded in its scope whereby psychiatrists can reach out to clients in far-flung areas and also educate primary care givers in the rural areas. There is a wealth of literature pointing out the effectiveness of telepsychiatry in diverse mental illnesses including depression, panic disorder, eating disorders, and schizophrenia.[6] It has been proven to be an effective modality in special subgroups such as adolescents, veterans, victims of abuse, and the elderly. It holds enormous potential for providing consultation-liaison service in primary healthcare. In addition to accurate assessment and diagnosis, it is an effective tool for imparting individual and group psychotherapy.[7] It is also a novel approach toward compiling medical data in an electronic format which may be readily utilized for the purposes of research.[8]
In this particular review, we intend to perform a systematic review of literatures available in India and in abroad and also intend to give a comprehensive comparative view of the various models that had been or currently are in use across the world and that in India, thereby finding out the relevant scopes, for improvement of telepsychiatry in India.
Method of literature search for articles on telepsychiatry from countries other than India:
We carried out an electronic title search in PubMed, PsyINFO, Directory of Open Access Journals (DOAJ), and Google Scholar without any timeline using the following keywords: “telepsychiatry” OR “tele-psychiatry” AND “systematic review” OR “model.” Our search led to 281 articles in total. Another title search was conducted using the keywords: “videoconferencing (VC)” AND “psychiatry,” which yielded 79 results. These articles were then reviewed by each author separately. After removal of duplicates, full texts were read to resolve any conflict and to reach to a common consensus. We included only (1) articles written in English (2) only peer reviewed articles (3) studies that addressed the use of telepsychiatry in all countries except India.
RESULTS
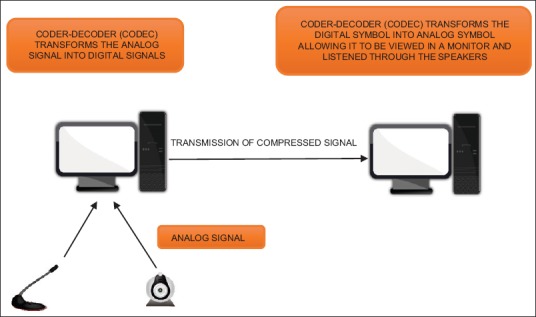
Out of the 360 articles obtained after database search, we finally identified 32 relevant articles[9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] and those were included in our review. The details of the study types, designs, and outcomes are described in Table 1.
Table 1.
The study designs and major findings of the included studies
Technological models for telepsychiatry practice
Literature on telemedicine has described numerous models as they came into vogue. Broadly, however, all these models can be classified as either synchronous or asynchronous. It was Allely et al.[41] (1995) who first described these two models of delivering telemedicine to the patients.
Synchronous telemedicine
Synchronous telemedicine “provides live, two-way interactive transmission between patient and provider at distant locations via telephony, online communication (e.g., chat forums) and video-conferencing.”[42]
Features
Asynchronous telemedicine
Asynchronous telemedicine “involves acquiring medical data and then transmitting this clinical information in the form of data, audio, video clips, or recordings via E-mail or Web applications for later review by a specialist.”[42]
Features
No need of synchronized communication between both sides
Advantage– Its cheap, less hardware requirements.[44]
Literature[45] mentions about various technological models that are used in providing telepsychiatry services. Those are real-time VC alone, combining VC with other systems, store-and-forward only systems, and telephone-only systems. Among all the studies, we reviewed, VC was the most used mode of communication between the patient and the specialist.
A typical videoconferencing system
The setup and equipment
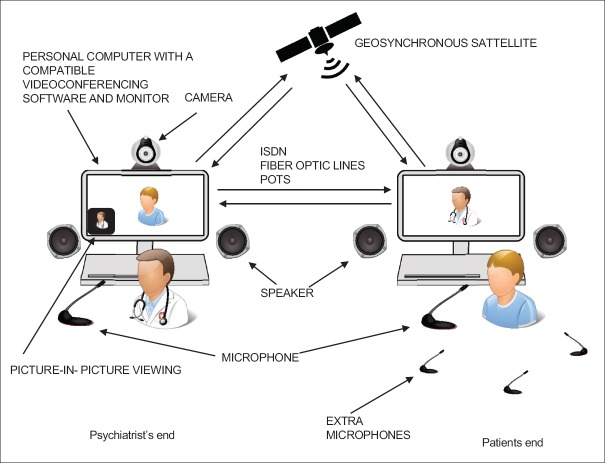
Hyler et al.'s (2002)[14] paper from Colombia, US gave a holistic description of a typical VC setup which involves a “host” site that can connect to one or more “remote” locations. According to their model, which is almost intact from its inception with minor modifications, each site generally has certain basic hardware:
Capturing device – (a) a video camera (b) microphone
Viewing device – (a) computer with a good processor (b) monitor (personal computer display/high resolution television monitor) (c) speakers
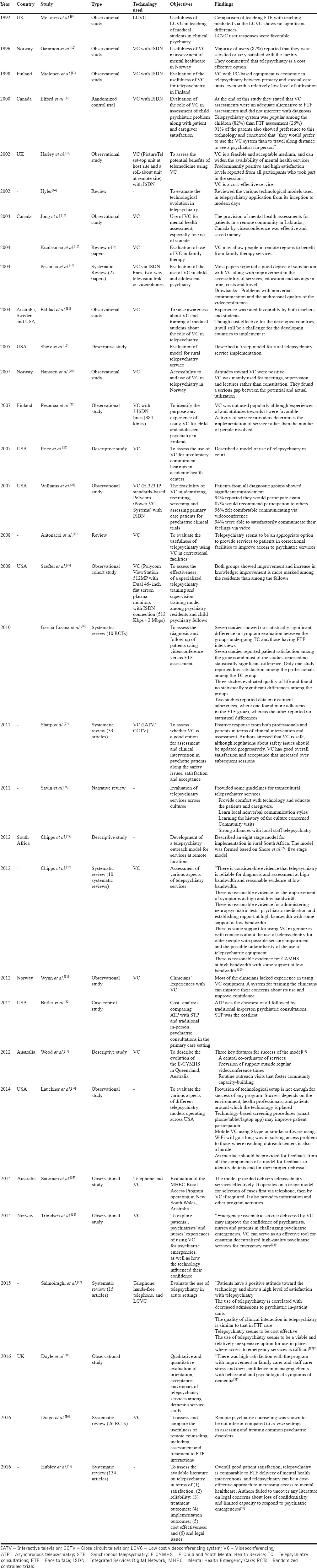
Figure 1 describes the process of information processing and signaling in a typical videoconference system. The capturing devices, that is, the video camera and the microphone receive the analog signals and transmit them to the computer. The coder-decoder (CODEC) software present in the computer converts the analog signals to digital signals, compresses them and send them to the remote site. The computer present at the receiving end transforms the analog signals back to digital signals using another set of CODEC and transmits the signal to the viewing and listening devices, that is, the monitor and speakers. Elford et al. (2000)[12] from Canada used a computer-based VC system to conduct child psychiatry assessments and compared it to face-to-face (FTF) consultation. The model is almost similar to that described before with some modifications. Common setup at both sites consists of a personal computer with a compatible VC software, a monitor, remotely controlled camera, with pan, tilt and zoom functions and microphone. The monitor at the psychiatrist's end supports a picture in picture view (this enables the psychiatrist to view and control their own image as well as that of their patient), whereas at the patient's end, the system allows only full screen video of that of psychiatrist only. Extra microphones were set up at the patient's end to pick up sounds throughout the room. Data transfer between the host and the remote sites is done through various routes which includes:
Geosynchronous satellite transmission
Fiber optic lines (the largest bandwidth of terrestrial technologies)
Integrated Services Digital Network (ISDN) (bandwidth – 128 kilobytes/s is most commonly used)
Plain-Old Telephone System (bandwidth 56–64 kilobytes/s; good for only voice communication).
Figure 1.
The basic mechanism of signal transmission in videoconferencing
High bandwidth transmission is desirable for clear transmission and good resolution. However, lately with the development in compression technology, it has been observed that quality of transmission can be preserved in low bandwidth also. The model is described in Figure 2.
Figure 2.
A typical videoconferencing setup used for telepsychiatry consultation. POTS - Plain old telephone service, ISDN - Integrated Services Digital Network
At the end of Elford et al.'s (2000)[12] study, they stated that VC assessments were an adequate alternative to FTF assessments and did not interfere with diagnosis. Telepsychiatry system was popular among the children (82%) than FTF assessment (26%). Nearly, 91% of the parents also showed preference to this technology and concurred that “they would prefer to use the VC system than to travel a long distance to see a psychiatrist in person.”[12] Disadvantages of VC as described by them are poor technical support, lack of training, and poor audio-visual quality leading to difficulty in perceiving emotional cues.[17]
Shore et al.'s model
A developmental model for rural telepsychiatry.
The American Indian and Alaska Native Programs started a number of telepsychiatric clinic to provide services among the American Indian war veterans suffering from posttraumatic stress disorder. Shore et al.[19] in their paper published in 2005 described the model that was implemented. Implementation of the model went through six different stages.
Stage 1: Identification - The implementation started with the identification of the at-risk and underserved population. This was followed by a discussion with the community about the services provided and feasibility.
Stage 2: Infrastructure survey - This survey was conducted at the same time as that of stage 1. Here, the possible areas of service delivery are scrutinized for available resources and documented. It helps in integrating the new resources in the infrastructure in a cost-effective way.
Stage 3: Partnership Organization - In stage 3, the local organizations were evaluated for their involvement and possible roles. The aim was a holistic community development by combined approach.
Stage 4: Structure configuration - This involves recruitment of staffs, giving them education about their roles and responsibilities along with a creation of the clinic structure.
Stage 5: Pilot implementation - For six months (pilot period), the clinic was started and feedback was received from both patients and staffs. Areas of deficits were identified and corrected as much as possible.
Stage 6: Solidification - The service was integrated more in the community and among the organizations and routine was set.
Chipps et al.'s model
Telepsychiatry consultation (TC) in South Africa.
This model[29] was an improvement of Shore et al.'s[19] model as described before. Based on local and international researches, the Departments of Psychiatry and TeleHealth at the University of KwaZulu-Nata, South Africa formulated a model to establish a telepsychiatry outreach model.
Stage 1: Situational Analysis and Needs Assessment - This is the earliest form of assessment aimed at identifying the treatment gaps and the reasons contributing to it.
Stage 2: Adoption of a Telepsychiatry Solution - An assessment of the feasibility, sustainability, advantages and disadvantages of telepsychiatry in addressing the needs is required.
Stage 3: Planning to implement the model - Once telepsychiatry is established to be a feasible plan for implementation, assessment of infrastructure and costs for implementation of desired setup, consultants and local assets has to be done.
Stage 4: Infrastructure Assessment - An understanding of the existing technological, organizational, and programmatic infrastructure required for telepsychiatry is essential to determine whether the infrastructure is adequate.[19] Local available resources and services have to be reviewed to see whether the adequate infrastructure is present to follow the consultants recommendations.
Stage 5: Consultant and Referring Telepsychiatry Services Configuration - “This process should ensure that the type of referral telepsychiatry services are determined, the roles and responsibilities of the stakeholders are delineated, organizational roles and responsibilities are identified, new healthcare processes and clinician roles designed and duty statements are adapted.
Stage 6: Local protocols should be adapted from the National Guidelines for Telepsychiatry and where appropriate, adaptation of local policies for registrar deployment and training, and referral should be done.”[29]
Stage 7: Training to support the model - Appropriate training of the coordinators, the technical support personnel as well as the users of the services should be ensured for the smooth functioning of the model.
Stage 8: Monitoring and Evaluation Planning - For proper quality control, regular monitoring, and evaluation for scopes of improvement should be done for integration and solidification of the service.
E-child and youth mental health service model (Wood et al.)
This particular model[33] was proposed to extend child and youth mental health services in Queensland, Australia. It is a centralized model controlled by metropolitan based staffs and allows to understand the intricacies of rural service delivery which is then conveyed to the strategic wing of the model who works on them to provide more integrative and elaborative services. This model provides three important keystones for success of Telepsychiatry services:
The coordinator - The role of the coordinator is to organize service delivery to rural and remote areas, collection of data, analysis, support service development, to negotiate between central site and rural/remote site, establish a system for sustained evaluation, safety and quality reviews, and establishment of a management system for administration of staff
Provision of support outside VC - Appropriate support should be provided to both the clinicians and local staffs and their requests should be addressed promptly. This improves quality of service and builds confidence among the service providers
Routine outreach visits that foster community capacity-building - Specialists visit at the outreach sites, helps in FTF services to complex cases, building peer support, improving knowledge among the support staffs and helps the clinicians understand the rural constraints.
Telepsychiatry in emergency mental health: The Mental Health Emergency Care-Rural Access Programme of New South wales, Australia (Saurman et al.).
Saurman et al.[35] described an emergency mental healthcare model that has been employed in New South Wales, Australia. This model employs ‘no wrong door’ philosophy, that is, “no caller is refused assistance.” Figure 3 provides a pictorial version of the service delivery which includes provision and information as well as clinical care. The clinical care is based on telephone triage which determines the necessity of a video assessment.
Figure 3.
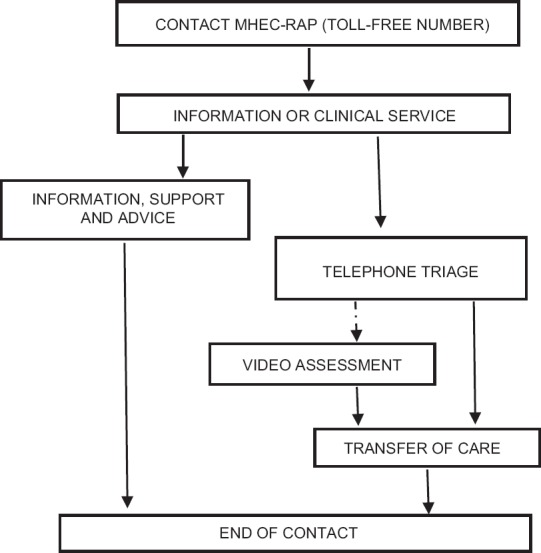
The emergency telepsychiatry model used under MHEC-RAP (Mental Health Emergency Care-Rural Access Programme)
Telecourt: Telepsychiatry in legal system
Price et al.[22] in their paper published in 2007, described a telepsychiatry model to aid legal proceedings. This model described two setups. One at the courtroom and another at the conference room of the psychiatry inpatient unit. A standard VC setup with all equipment is present at both sites. Personnels usually present at the courtroom are Honorable judge himself, prosecuting attorney, court personnels, witnesses, and family members. Whereas at the conference room of in-patient unit, the personnels usually allowed are the patient, attorney of the patient, testifying physician, nurse, and any security personnels, if required.
The experience described by the authors outlines certain advantages and disadvantages. The advantages being (a) significant savings in staff time and productivity (b) patient safety (c) decreased hospital's liability risk (d) savings of transport cost and time. The disadvantages being (a) disapproval of attorneys to participate. (b) Patient may face problem to face this form of hearing. In conclusion, they have commented “The experience of the University of Michigan Health System and the Washtenaw Probate Court with tele-court hearings for involuntary commitment has proven to benefit the safety and dignity of patients as well as the financial health of the medical center.”
Telepsychiatry for psychotic patients
Whether telepsychiatry is a good option for assessment and treatment of psychotic patients has been a topic of debate. In 2011, Sharp et al.[27] published a systematic analysis of 33 different types of articles to address this issue. Their objectives were to assess whether VC is a good option for assessment and clinical intervention in psychotic patients alongside the safety issues, satisfaction and acceptance. The studies in the review that discussed clinical intervention through VC, reported that most of the doctors/residents reported positive experiences and considered VC to be safe and effective way of reaching out to patients, especially those in rural and challenging settings. Many believe that many of the skills useful in the assessment of psychotic patients will be rendered useless by the process. Author of one of the included studies commented, “I was delightfully surprised to discover that this was not true.”[46] Patients showed better attendance and follow-up rates and considered VC as an easier way of communication (this was particularly true for patients with schizophrenia). Authors of one of the studies commented, “even schizophrenics with ideas of reference including TV (e.g., being talked about on public programs) accepted the CCTV interaction very well and no exacerbation of their delusions was observed.”[47] Sharp et al.[27] commented, “based on the studies reviewed, patients with psychosis can be reliably interviewed and evaluated via VC, including using symptom severity scales (e.g., BPRS) and diagnostic, clinical, and psychiatric interviews.”[27] The reviewers while talking about safety issues commented that the regulations and rules for the management of patients with telepsychiatry should always be evolved toward providing best services to the patients. One important finding was highlighted, which was “the physical distance afforded by telepsychiatry has allowed patients to express strong affects that may have led to premature termination of in person sessions.”[48] Satisfaction and acceptance as reported by the reviewer were quite high among both the professionals and patients, often rating VC higher than FTF sessions, especially among children.[49] It was observed that acceptance and satisfaction increased over time.[50]
Transcultural telepsychiatry model
Culture's influence on the mental health of people is undeniable. Hence, understanding and acclimatizing to a particular culture is very much essential to understand symptoms and formulate diagnosis. Savin et al.[28] in their article provided some basic guidelines to model the telepsychiatry services for proper implementation.
Provision of comfort and training: Before any teleconsultation, the psychiatrist should inquire about the comfort level of the patient and their caregivers about it and simultaneously should provide adequate information to make the process comfortable. This is essential for the process of establishment of proper rapport
Learn local nonverbal communication styles: A professional who provides telepsychiatry services across cultures is expected to get himself familiar with the colloquial style of language and nonverbal communications and should understand those aspects of technology that may affect this form of communication
Learn local history: History is a rich source of knowledge for any given culture, which can be used to understand the patient or to provide psychoeducation using metaphors
Community visits: The authors commented that it is almost impossible to understand a patient's psychosocial environment without actually interacting with it. Hence, community visits on and off should be done, which provides the necessary information
Incorporation of local resources: A functional therapeutic team should be created utilizing local resources. Local staffs are far more acquainted with a patient's current condition and helps in establishment of quick rapport and trust.
Store and forward model
Transmission of medical information stored in the form of digital images, documents, prerecorded videos and secure E-mail transmission is referred to as store and forward model. Figure 4 gives us a rough outline of the concept.
Figure 4.
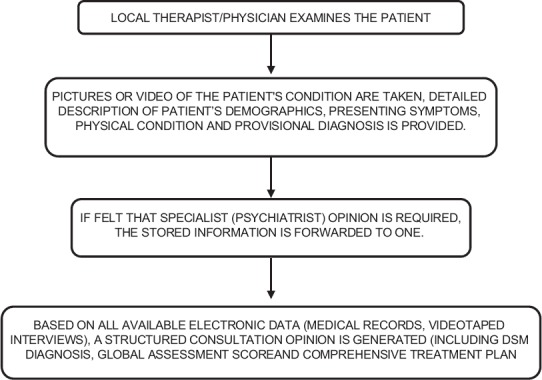
The outlines of the “store and forward” model
Advantages of “store and forward” model
More time efficient for providers
Consultation can be done regardless of time and place without any administrative difficulties of scheduling an in-person consultation[43]
Consultations are cost-effective[24]
Can be used to provide culturally sensitive multilingual psychiatric services[44]
This model integrates the services of primary healthcare provider in managing mild to moderate mental health illnesses in the community
Provides improved communication between a primary healthcare provider and a specialist with increased information and knowledge sharing.
Effectiveness of telepsychiatry
Since the inception of telepsychiatry the concern that has been repeatedly expressed by both the patients and the service providers is, “Is Telepsychiatry effective?” Available literature shows, yes, Telepsychiatry is definitely effective. Garcia-Lizana et al.[26] in 2010 published a systematic review of literature of 10 randomized controlled trials (RCT), all of which asked the same question. They found that seven of the included studies showed no statistically significant difference in symptom evaluation between the groups undergoing TCs and those having FTF interviews. Chipps et al. (2012)[30] performed a systematic review of 10 systematic reviews on Telepsychiatry, results showed that Telepsychiatry is indeed reliable for diagnosis and assessment and there are reasonable evidences of patient improvement. Evidences also show that telepsychiatry through VC is effective for administering neuropsychiatric tests, psychiatric medication and for establishment of rapport. Another systematic review of 26 RCTs by Drago et al. (2016)[39] commented that, “Remote psychiatric counseling was shown to be not inferior compared to in vivo settings in assessing and treating common psychiatric disorders.” Hubley et al.'s[40] review (2016) of 134 articles also concluded that telepsychiatry is comparable to FTF delivery of mental health interventions.
Feasibility and acceptability
When the question comes to feasibility and acceptability, studies report that Telepsychiatry is very much feasible and has been accepted as an effective alternative to traditional FTF consultations. Harley et al.[13] (2002) conducted an observational study in the UK in 2002 to assess the potential benefits of Telepsychiatry, he remarked that VC is a feasible and acceptable medium, and can widen the availability of mental health services. Pesämaa et al.[21] in 2007, conducted an observational study to identify the purpose and experience of VC among children and adolescents. He concluded that VC was not used popularly although experiences of and attitudes toward it were favorable and it is the activity of service providers which determines the implementation of service rather than the number of people involved in the service.
Satisfaction, attitude and cost effectiveness
Most of the studies included in the review have accepted telepsychiatry as a cost effective alternative treatment modality with high satisfaction among the service providers and the patients. The oldest included study that set out to assess its usefulness from Norway[10] reported 87% satisfaction rate among its users, most of whom reported the service as “satisfied” or “very satisfied” with the facility. In another Canadian study,[12] 91% of the patients also showed preference to this technology and concurred that “they would prefer to use the VC system than to travel a long distance to see a psychiatrist in person.” Numerous studies and systematic reviews[13,15,18,27,38,40] carried out subsequently solidified the idea that telepsychiatry through VC delivers a satisfactory level of treatment in a cost effective manner and may be a preferred modality in the near future over others.
Videoconferencing in psychiatry education
It has been suggested that VC can be an important tool in imparting psychiatry education. The earliest study that could be found among the included articles of this review dates back to 1992, when Mclaren et al.[9] compared education through VC with FTF teaching. They found no significant difference in improvement among the two groups. On the contrary, the responses toward VC were favorable. A transcontinental educational program (Sweden, USA and Australia) utilizing VC was reported in 2004 by Ekblad et al.;[18] favorable outcome was reported by both the students and teachers. The authors commented that although it is a cost-effective way of imparting education, it would be a challenge for the developing countries to adopt it. In 2008, Szeftel et al.[25] tried to assess the effectiveness of a specialized telepsychiatry training and supervision training model among psychiatry residents and child psychiatry fellows using VC. Both groups in this study showed improvement and increase in knowledge; however, improvement was much more marked among the residents than among the fellows. Thus, from the available literature, it turns out that, contrary to popular belief, VC can successfully provide psychiatry training and is a cost effective way of doing so.
Telepsychiatry in India
It was at the turn of the 21st century that India embarked on its tryst with telemedicine when Aragonda, a remote village in Andhra Pradesh, was linked via distant communications technology with a tertiary center 200 km away in the South Indian metropolis of Chennai. It necessitated the coming together of such diverse agencies as the Ministry of Health and Family Welfare, the Department of Space and the Indian Space Research Organisation to materialize this ambitious venture. On March 30th 2000, Mr. Bill Clinton the then president of the United States of America, during his India tour, formally launched telemedicine in India and commissioned the first telemedicine unit in the village of Aragonda. The advancement in communications technology has henceforth served to the benefit of various medical disciplines, psychiatry being no exception. The Schizophrenia Research Foundation (SCARF), which is a nongovernmental organization (NGO) providing mental healthcare services from its center in Chennai, holds the distinction of pioneering telepsychiatry services in India. Their novel initiative of rendering telepsychiatry services to reach out to the victims of the devastating tsunami of December, 2004 in the coastal districts of Tamil Nadu has been acclaimed worldwide. This has led to a spring of optimism about the possibility of delivering quality mental healthcare via telepsychiatry, provided a clearly outlined process is laid out and realistic goals are set.
There are numerous literatures which points towards the inadequacy of quality mental healthcare services in India.[51,52,53] A careful scrutiny of the information in this context available in the public domain reveals that there are two psychiatrist available for every ten lakh population.[54] It is estimated that 7% of the total population suffers from mental illnesses,[55] with close to 90% remaining untreated.[55] The problem is compounded by the equally alarming acute dearth of trained mental health professionals in the fields of psychiatric nursing, psychiatric social work, and clinical psychology.[54] The Government of India launched initiatives such as the National Mental Health Programme[56] and the District Mental Health Programme[56] to tackle this public health menace. However, the results of these ventures have been far from satisfactory as the burden of individuals with mental illnesses continues to accrue. Despite an on-going spate of migration from the villages to cities, a defining feature of India's demographics remains that about 74% of India's vast populace is rural.[54] Although urban India has seen a multitude of innovations and institutions targeting the need for quality mental healthcare, replicating the same has proved tiresome in agrarian rural India where prejudices and misconceptions regarding mental health are deep-seated and difficult to overcome. The stigma associated with mental illness is widespread in the Indian society and it tends to have woeful implications on all aspects of life-personal, social as well as vocational. It is indeed heart-wrenching that a huge proportion of those with serious mental illnesses are abandoned by their families and are compelled to lead a despicable life with little, if at all any, dignity and security.
It is in this context that telepsychiatry appears as a ray of light at the end of the deplorable tunnel. One heartening fact remains that telepsychiatry utilizes only the rudiments of distant communications technology that is required for VC as compared to the advanced technological knowhow required for other medical disciplines. Using the Digital Imaging and Communications in Medicine platform 3.0 standards and a simple bandwidth of 128 kbps, urban practitioners can effectively communicate with rural clients. Studies comparing the accuracy of diagnosis and the level of satisfaction in consultations through telepsychiatry and that during FTF consultations advocate the effectiveness of this modality.[57] The invigorating SCARF experience makes us dream of a promising future for telepsychiatry in India.
Method for literature search for Indian articles on telepsychiatry
Search methodology for articles reporting telepsychiatric advancement and models in India was more elaborate and relaxed. Here, we decided to search and include all types of articles we could find in the reputed databases. A literature search was conducted in PubMed, PsyINFO, Medline, DOAJ and Google Scholar databases with the keywords “telepsychiatry” OR “tele-psychiatry” (Title search) and “India” (Title/Abstract search). The search yielded eight articles (excluding duplicates). Indian Journal of Psychiatry and Indian Journal of Psychological Medicine website were separately searched next with keywords “Telepsychiatry” OR “Tele-psychiatry,” which yielded one and three articles, respectively. Search criteria were further extended to include any literature on “telepsychiatry in India.” No time period filter was applied in any searches. After excluding the duplicates, we decided to include eleven articles in total, for the review. Those are: Balasinorwala et al., 2014;[42] Malhotra et al., 2015;[58] Malhotra et al., 2013;[8] Thara et al., 2008;[59] Thara and Sujit, 2013;[60] Math et al., 2015;[61] Thara, 2012;[62] Parekh, 2016;[63] Malhotra 2013;[64] Malhotra 2014;[65] Gogia 2015.[66] Apart from these studies, we also included information regarding the available tele-mentoring programs running in India currently and also addressed the long standing issue regarding laws and ethics regarding telepsychiatry practice in India.
Synchronous telepsychiatry models
Models provided by Schizophrenia research foundation
The first of the studies included was published in 2008, by Thara et al.[59] which described the experience of the implementation of telepsychiatry services in India by SCARF. SCARF is a reputed NGO operating from Chennai, India and provides mental health services countrywide. After the disaster struck by tsunami on December 26, 2004 in coastal India, while providing the much needed psychological support and training to volunteers, SCARF authorities understood the usefulness of telepsychiatry services and later decided to take it to the next level. Initially funded by Oxfam trust of India, SCARF set out to model its telepsychiatry services after the template they used in their community outreach program.
Model 1 - SCARF tele-psychiatry in Puddukottai (STEP) model [Figure 5]:
Figure 5.
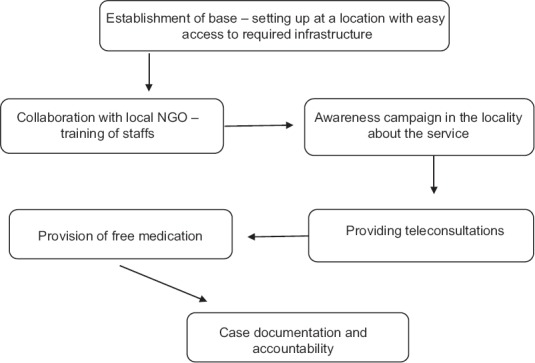
Schizophrenia Research Foundation model of telepsychiatry services
Establishment of base - A peripheral base location is established at a place with limited psychiatric services so that people might benefit from it and also, from where, easy accessibility of required infrastructures and technology is possible
Collaboration with NGO - A collaboration is established with a local NGO to utilize and train the local manpower who are knowledgeable about the terrain, language, and customs of the area
Awareness campaigns - Campaigns in forms of street theater, folk songs, film screening, etc., have to be done in the catchment area, to raise awareness about mental illnesses and the availability of this new facility
Providing teleconsultations - Teleconsultation timings has to be fixed which includes consultation to new patients and review of old cases [Figure 6]. SCARF recommends consultation time of 30 min to 1 h for new patients and 10–40 min for review cases. Peripheral units are advised to directly contact psychiatrist in case of relapse or adverse drug reactions. Teleconsultation was initially provided through ISDN[60] lines of minimum 128 kbps connection[59], which later was shifted to broadband[60]
Provision of free medication: Since, the idea is to provide psychiatric services at the remote areas via teleconsultation, it is obvious that people availing the services will be from the lower socioeconomic strata of the country. Hence, provision of free medications will serve as a big motivation for the population to access the services and this must be provided at the peripheral base by field staffs or local coordinators
Case documentation and accountability - Maintenance of a patient dossier on patient demographics, history of illness, mental state examination, and level of functioning and prescription should be done. This gives important information about mental illness burden in the area, creates scopes for research and provides information for areas of improvement.
Figure 6.

A live telepsychiatry consultation organized by Schizophrenia Research Foundation (Source: Schizophrenia Research Foundation, India)
Model 2 - Schizophrenia Research Foundation model for mobile telepsychiatry services (Thara and Sujit, 2013):[60]
SCARF pioneered in implementation of mobile telepsychiatric services in India too. After the success of the initial nonmobile model, mobile telepsychiatry unit was implemented for the first time in 2010, in the District of Pudukkottai, Tamil Nadu, India [Figures 7–9].
Figure 7.

A schizophrenia research foundation mobile telepsychiatry unit (Source: Schizophrenia Research Foundation, India)
Figure 9.

A mobile Telepsychiatry unit pharmacy (Source: Schizophrenia Research Foundation, India)
Figure 8.

The patient's end during a live teleconsultation (Source: Schizophrenia Research Foundation, India)
Components
-
Mobile unit - The mobile unit is usually a custom-built bus with a consultation room and a pharmacy
- Consultation room - The room has a flat screen television with a state of the art camera. Patients and caregivers communicate with a psychiatrist using a wireless internet connection
- Pharmacy: On board pharmacy provides medication as prescribed
Teleconsultations - Consultations are provided by a psychiatrist after interacting with the patient and caregivers in the consultation room. The prescription is issued and medications are dispensed free of cost. Patients are provided with a record slip that mentions the provisional diagnosis, prescription, investigations that have to be done by patient independently and a follow-up date
-
Psychosocial interventions - Apart from teleconsultations, SCARF also provides various psychosocial interventions through their mobile unit like:
- Psychoeducation to caregivers
- Removal of stigma about mental illnesses
- Provisions of jobs to patients through the various available government schemes or in voluntary sectors
Awareness Programs - Numerous programs are carried out by health workers such as street play, screening of films, etc., which are broadcasted in a television screen on the back of the mobile unit. Posters and pamphlets containing information about mental illnesses and services provided are also distributed.
Thara and Sujit, 2013[60] reported that the project has been immensely successful and recommended its incorporation in the district mental health program.
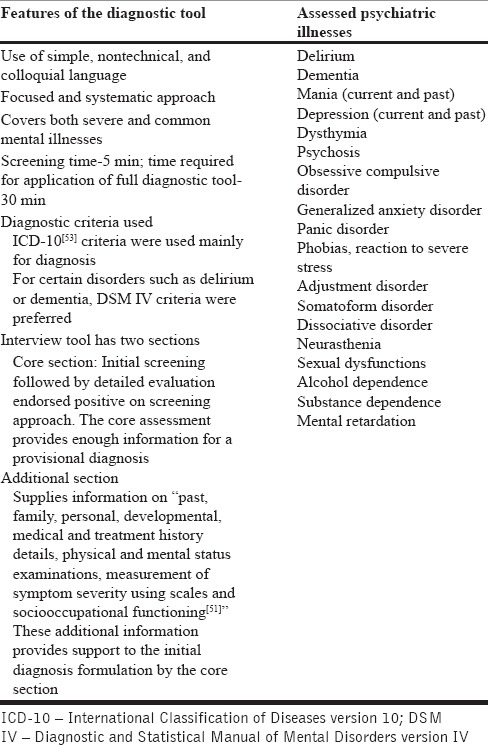
Models provided by Postgraduate Institute of Medical Education and Research, Chandigarh psychiatristonweb application
Due to a deficit of mental health professionals in India, which remains ever growing owing to the population boom, the vision to provide telepsychiatry services in the remotest corners of the country may lead to overburdening of the specialists. Hence for effective implementation of the services, the nonpsychiatrist medical professionals have to be included (general practitioners, para-professionals) for the effectiveness of the services and distribution of workload. An innovative new approach to service provision through telepsychiatry was suggested by the Department of Psychiatry, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. Malhotra et al.[65] suggested the development of a net based software package with “codified medical knowledge and logical decision support system.”[58] The application was named “psychiatristonweb.”
Model 1 - Adult Version: The pilot study to create and test the adult version of this software package was published in 2014. A new indigenous diagnostic tool was formulated for the purpose. Detail of the model and its features are described in Figure 10 and Table 2. The model showed high feasibility and acceptable sensitivity and specificity for most of the disorders except few
Model 2 - Child and adolescent version: Created as a joint venture of Department of Psychiatry, PGIMER and Tata Consultancy Services. Published in 2015 by Malhotra et al.[58] this model used the same format as that of the adult version. It was estimated that for a full diagnostic interview the tool would take a maximum of 30 min. However, this diagnostic tool assessed nineteen different disorders of childhood onset, different from its adult version. Those being “mental retardation, specific learning disability, attention deficit hyperactivity disorder, oppositional defiant disorder and conduct disorder, autism, depression, mania, psychosis, obsessive-compulsive disorder, generalized anxiety disorder, specific phobias, social anxiety disorder, separation anxiety disorder, somatoform disorder, dissociative disorder, alcohol dependence, substance use disorders and enuresis.[58]” They found that the diagnostic tool was comparable to most of the reputed structured interviews such as Mini International Neuropsychiatric Interview for Children and Adolescents, Diagnostic Interview Schedule for Children, etc., and has high specificity and sensitivity for most disorders. Not only the time consumed for the interview was much less than any of the standardized tools, but also, the tool was easy to administer as reported by the interviewers and interviewees.
Figure 10.
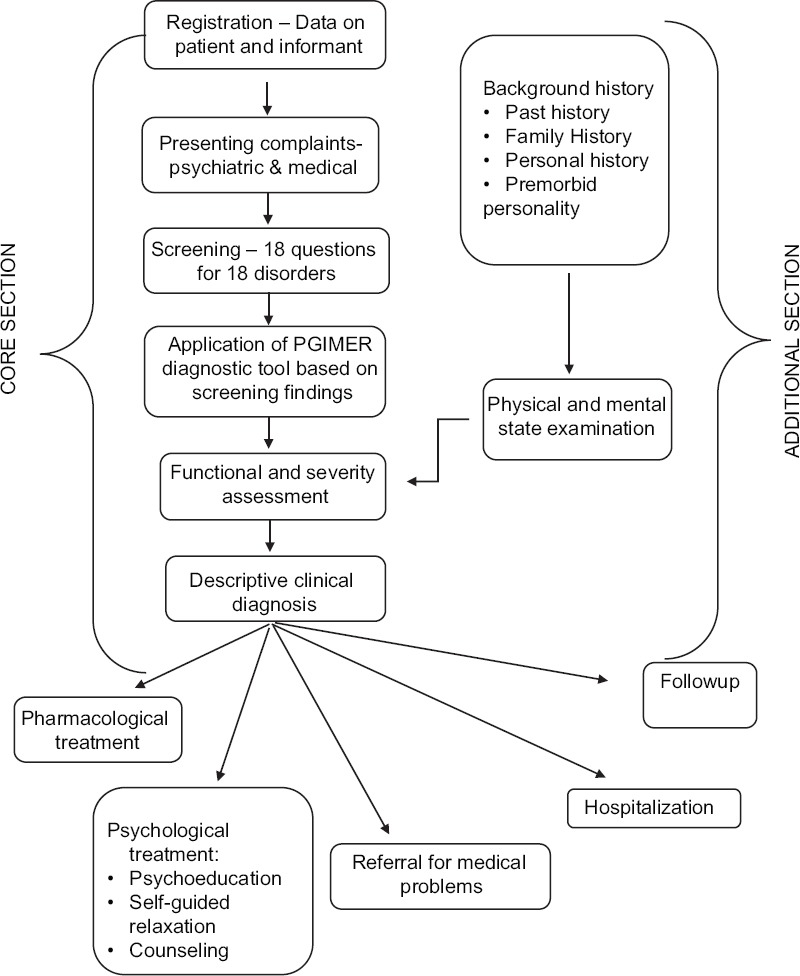
Functioning of PGIMER telepsychiatry delivery software package
Table 2.
Describing the features of Postgraduate Institute of Medical Education and Research telepsychiatry diagnostic tool
Both the models have options to suggest both pharmacological management and psychological management.
Pharmacological management
Drugs are chosen according to the diagnosis provided and those listed in the application. The application also provides “explicit guidelines on need for hospitalization, details of drugs, their dosing and side effects, alteration in dose/drugs on follow up, etc.”[67]
Psychological management
Psychoeducation modules: Aim of this module is provide psychoeducation to patient (child and adult) and caregivers about the illness. Sessions of 30-minute duration were conducted over 3–4 weeks
Self-guided relaxation (SGR) module:[64] The SGR module was developed based autogenic training. Each session is of 25–35 min. The SGR technique divides the body into 10 different muscle groups. The idea is to produce relaxation of those muscle groups through suggestion. Suggestion is provided by an audio-visual tape that also describes the procedure or by a trainer
Counseling module: Counseling modules are available for both patient/caregiver and counselors
Guide to parenting (only for model 2): This model includes parenting guidelines required for management of various child psychiatric problems such as attention deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, autism, etc.
Alongside this, the program also included training of the staffs working at the remote centers which was mainly done by VC software's like Skype. The PGIMER project has been awarded “the Skoch Order of Merit” as India's best Governance Project 2014; and also conferred award of excellence for Highest Independent Honour in India the 37th Skoch Summit on “Minimum Government, Maximum Governance” in New Delhi on September 19–20, 2014.”[68]
The Ganiyari model
Under the Jan Swasthya Sahyog[69] community health program, a telepsychiatry model was prepared to serve the tribal and rural areas of Bilaspur and surrounding areas of Chhattisgarh in central India.[57] First established in April 2012, the model has been running effectively for the past 4 years, providing both out-patient consultation and occasional emergency services. The consultation is provided via Skype (a video conferencing software),[70] using a high speed (2 Mbps) internet connection. The patient end is manned by a resident doctor or a paramedic, who facilitate the conversation and maintain logistics. A computer program called Team Viewer[71] allows simultaneous viewing of electronic medical records of the patient on the screen. Diagnosis is made and prescription is dispensed with a date for follow-up. Psychiatrist visits the peripheral center every 6 months to train referring physicians and spread awareness.
Hub and spokes model of National Institute of Mental Health and Neurosciences, Bengaluru, India
The model followed by the National Institute of Mental Health and Neurosciences (NIMHANS) is a typical hub and spokes model; where, NIMHANS acts as the hub and extends its services to its’ various spokes which being various districts, taluks, prisons and relief and rehabilitation centers. The initial contact with the hub is made by any mental health professional serving at the spokes. The details of the patient including demographics, clinical presentation, history of illness, etc., are sent to the hub and a consultation date is fixed. On the fixed date, a consultation takes place between the specialist (psychiatrist) present at the hub and the mental health worker present at the spokes via VC. Interaction with patients only takes place if only the specialist feels the need for it. Each consultation is of 10–15 min duration.
Asynchronous telepsychiatry models
Balasinorwala et al.[42] in 2014 studied the feasibility of asynchronous telepsychiatry in Maharashtra, India. The Maharashtra State Telemedicine project, which is operational from 2007, provides infrastructure for both synchronous and asynchronous telemedicine [Figure 11]. In this particular project, the authors involved 94 referrals that were made to their centers between 2007 and 2013. The model they used is described in Figure 11. Of the 94 referrals, 89 patients (95%) received a definitive psychiatric diagnosis, thus proving asynchronous telepsychiatry is both feasible and often helpful in the face of instantaneous workforce shortage.
Figure 11.
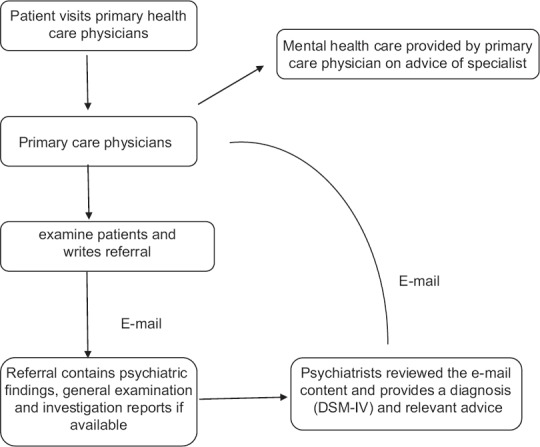
Asynchronous telepsychiatry project
Effectiveness of telepsychiatry in India
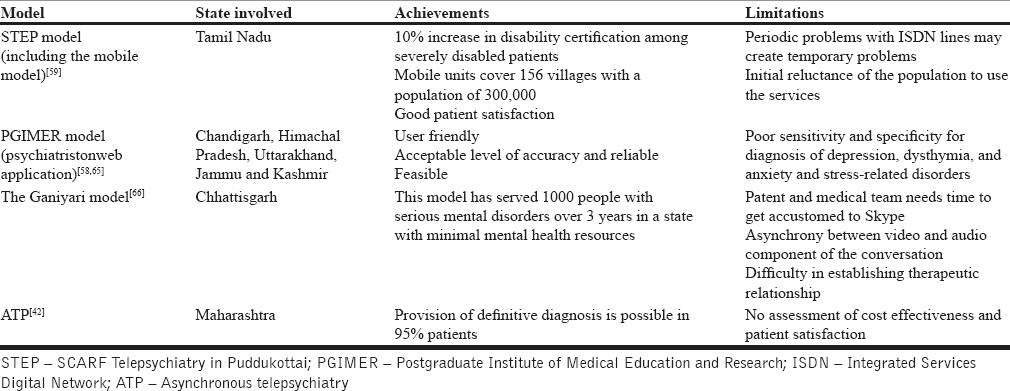
All the models discussed before, are successful despite some limitations as reported by the researchers. Those are discussed in Table 3.
Table 3.
A brief overview of achievements and limitations of the discussed models in India
E-learning
Virtual Knowledge Network (NIMHANS Extension for Community Healthcare Outcomes [ECHO]), Center for Addiction Medicine, NIMHANS:[72]
The Centre for Addiction Medicine, Department of Psychiatry, NIMHANS, Bengaluru, India, has started an innovative program which provides a platform for discussion, learning and active participation for the mental healthcare professionals all over the country. The NIMHANS ECHO is a part of a greater program called “project ECHO”[73] which was initially started by the University of New Mexico, USA. The idea is to distribute knowledge to the frontline community physicians through the specialist for management of “chronic, common, and complex diseases” through a series of presentations and case discussions. Weekly VC is carried out through multipoint VC, which is led by experts in the field.
Law and medical ethics in telepsychiatry practice: The long standing dilemma
Is practicing telepsychiatry legal? Is it even ethical to diagnose and propose interventions to a patient whom the doctor hasn’t seen FTF? This is a question which must have been asked by every one of us. The American Telemedicine Association and The American Psychiatric Association (APA) however, encourage the growth of telepsychiatry in USA and have recognized it as a validated form of treatment. According to APA “Telemedicine in psychiatry, using video conferencing, is a validated and effective practice of medicine that increases access to care. The APA supports the use of telemedicine as a legitimate component of a mental health delivery system to the extent that its use is in the best interest of the patient and is in compliance with the APA policies on medical ethics and confidentiality.”[74] Till now, existing Indian law does not adequately address concerns relating to telemedicine practice.[75] Indian Government has not rolled out any clear guidelines of telemedicine practice yet. However, the Ministry of Health and Family welfare has proposed setting up a National e-Health Authority (NeHA) which will be responsible for enforcing the laws and regulations related to telepsychiatry.[76]
Scopes of improvement for India – recommendations:
India is at the forefront of Information Technology globally. It gives us an added advantage regarding knowhow and expertise in this sector which may be tapered for promoting telepsychiatry in our vast country. Integration of technology with relevant social sciences is essential for maximum outreach of telepsychiatry. An interdisciplinary approach involving multiple agencies is a requisite for a positive outcome
As we have insufficient funding in mental health compared to other disciplines, it appears a feasible solution modality as per preliminary evidence, the cost of setting up infrastructure and supporting staff must be evaluated and proposed for the benefits of the policy makers
There are important legal and ethical issues involved in telepsychiatry such as confidentiality, role in emergency situations and security of data. This can be addressed if the consultant does not assume direct responsibility but provides support to the primary care physician
The National Mental Health programme and the District Mental Health programme have been both welcome steps taken by the Central Government to tackle the ever-increasing burden of mental health in our country. Telepsychiatry should be incorporated in principle by both these public health initiatives to render not only clinical services but also training to primary care providers to ensure quality affordable mental healthcare
Psychiatry is deeply rooted in human interaction and empathy. Hence, a combination of distance consultation by experts and a support framework provided by mental health professionals at the grassroots level is the way forward in the Indian context
Out of the various models practiced, a combination of mobile telepsychiatry unit with basic technology such as video-conferencing seems feasible for maximum penetration of effective mental healthcare
With the recent revolution in tele-technology and adequate network coverage, there are many in this country who has a basic knowledge in telecommunication. India currently has a number of vertical programs and a huge network of NGO. By using these networks, on one hand proper psychiatric services can be spread easily and effectively to the remotest corner of the country in a very cost effective manner and on the other, it can provide employment opportunities to a huge number of youth, simultaneously generating the much needed awareness about mental health in this country.
CONCLUSION
The foremost challenge faced by Psychiatry as a discipline in India is to overcome the various inadequacies that exist in the delivery of equitable mental health services. Telepsychiatry offers promise as an innovative modality to reach out to the vast majority of Indians in dire need of psychiatric attention and care. It is heartening that as a global leader in Information Technology India has the technological acumen and know-how to materialize the ambitious dream of connecting those in need of psychiatric help with trained mental health professionals via distant communications technology. Telepsychiatry has been proven to be an effective modality as is evident from the varied literature enumerated in this current study. A sincere attempt has been made to explain the technicalities involved across various models of telepsychiatry as they currently stand. Mention has been made of the two predominant approaches in vogue-asynchronous and synchronous models. A set of recommendations have been made for the benefit of policymakers to efficiently incorporate telepsychiatry in the existing scheme of mental healthcare. Telepsychiatry is indeed a boon at our disposal in our march against the ever-growing burden of mental illness in our country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.White LA, Krousel-Wood MA, Mather F. Technology meets healthcare: Distance learning and telehealth. Ochsner J. 2001;3:22–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Bashshur RL, Shannon GW. History of telemedicine: evolution, context, and transformation. New Rochelle, NY: Mary Ann Liebert, Inc, publishers; 2009. [Last cited on 2016 Oct 24]. Available from: http://www.d×.doi.org/10.1089/9781934854112.131 . [Google Scholar]
- 3.Alexander Graham Bell and the Birth of Telemedicine – TELEMEDICINE. [Last cited on 2016 Oct 24]. Available from: http://www.telemedmag.com/content-pages/2016/2/19/saved-by-a-bell .
- 4.Luiz Ribeiro AP, Beatriz Alkmim M, Silva Cardoso C, Galeno Carvalho GR, Teixeira Caiaffa W, Viegas Andrade M, et al. Implementation of a Telecardiology System in the State of Minas Gerais: The Minas Telecardio Project. 2010 doi: 10.1590/s0066-782x2010005000060. [DOI] [PubMed] [Google Scholar]
- 5.What You Didn’t Know About The History of Telemedicine | SightCall. [Last cited on 2016 Oct 24]. Available from: http://www.sightcall.com/history-telemedicine/
- 6.Telemedicine I of M (US) C on ECA of, Field MJ. Evolution and Current Applications of Telemedicine. US: National Academies Press; 1996. [Google Scholar]
- 7.Deslich S, Stec B, Tomblin S, Coustasse A. Telepsychiatry in the 21st century: Transforming healthcare with technology. Perspect Health Inf Manag. 2013;10:1f. [PMC free article] [PubMed] [Google Scholar]
- 8.Malhotra S, Chakrabarti S, Shah R. Telepsychiatry: Promise, potential, and challenges. Indian J Psychiatry. 2013;55:3–11. doi: 10.4103/0019-5545.105499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McLaren PM, Ball CJ, Summerfield AB, Lipsedge M, Watson JP. Preliminary evaluation of a low cost videoconferencing system for teaching in clinical psychiatry. Med Teach. 1992;14:43–7. doi: 10.3109/01421599209044014. [DOI] [PubMed] [Google Scholar]
- 10.Gammon D, Bergvik S, Bergmo T, Pedersen S. Videoconferencing in psychiatry: A survey of use in Northern Norway. J Telemed Telecare. 1996;2:192–8. doi: 10.1258/1357633961930068. [DOI] [PubMed] [Google Scholar]
- 11.Mielonen ML, Ohinmaa A, Moring J, Isohanni M. The use of videoconferencing for telepsychiatry in Finland. J Telemed Telecare. 1998;4:125–31. doi: 10.1258/1357633981932073. [DOI] [PubMed] [Google Scholar]
- 12.Elford R, White H, Bowering R, Ghandi A, Maddiggan B, St John K, et al. A randomized, controlled trial of child psychiatric assessments conducted using videoconferencing. J Telemed Telecare. 2000;6:73–82. doi: 10.1258/1357633001935086. [DOI] [PubMed] [Google Scholar]
- 13.Harley J, McLaren P, Blackwood G, Tierney K, Everett M. The use of videoconferencing to enhance tertiary mental health service provision to the Island of Jersey. J Telemed Telecare. 2002;8(Suppl 2):36–8. doi: 10.1177/1357633X020080S216. [DOI] [PubMed] [Google Scholar]
- 14.Hyler SE. Technological advances in telepsychiatry. Prim Psychiatry. 2002;9:24–8. [Google Scholar]
- 15.Jong M. Managing suicides via videoconferencing in a remote Northern community in Canada. Int J Circumpolar Health. 2004;63:422–8. doi: 10.3402/ijch.v63i4.17759. [DOI] [PubMed] [Google Scholar]
- 16.Kuulasmaa A, Wahlberg KE, Kuusimäki ML. Videoconferencing in family therapy: A review. J Telemed Telecare. 2004;10:125–9. doi: 10.1258/135763304323070742. [DOI] [PubMed] [Google Scholar]
- 17.Pesämaa L, Ebeling H, Kuusimäki ML, Winblad I, Isohanni M, Moilanen I. Videoconferencing in child and adolescent telepsychiatry: A systematic review of the literature. J Telemed Telecare. 2004;10:187–92. doi: 10.1258/1357633041424458. [DOI] [PubMed] [Google Scholar]
- 18.Ekblad S, Manicavasagar V, Silove D, Bäärnhielm S, Reczycki M, Mollica R, et al. The use of international videoconferencing as a strategy for teaching medical students about transcultural psychiatry. Transcult Psychiatry. 2004;41:120–9. doi: 10.1177/1363461504041357. [DOI] [PubMed] [Google Scholar]
- 19.Shore JH, Manson SM. A developmental model for rural telepsychiatry. Psychiatr Serv. 2005;56:976–80. doi: 10.1176/appi.ps.56.8.976. [DOI] [PubMed] [Google Scholar]
- 20.Hanssen B, Wangberg SC, Gammon D. Use of videoconferencing in Norwegian psychiatry. J Telemed Telecare. 2007;13:130–5. doi: 10.1258/135763307780677587. [DOI] [PubMed] [Google Scholar]
- 21.Pesämaa L, Ebeling H, Kuusimäki ML, Winblad I, Isohanni M, Moilanen I. Videoconferencing in child and adolescent psychiatry in Finland – an inadequately exploited resource. J Telemed Telecare. 2007;13:125–9. doi: 10.1258/135763307780677631. [DOI] [PubMed] [Google Scholar]
- 22.Price J, Sapci H. Law and psychiatry: Telecourt: The use of videoconferencing for involuntary commitment hearings in academic health centers. Psychiatr Serv. 2007;58:17–8. doi: 10.1176/ps.2007.58.1.19. [DOI] [PubMed] [Google Scholar]
- 23.Williams JB, Ellis A, Middleton A, Kobak KA. Primary care patients in psychiatric clinical trials: A pilot study using videoconferencing. Ann Gen Psychiatry. 2007;6:24. doi: 10.1186/1744-859X-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Antonacci DJ, Bloch RM, Saeed SA, Yildirim Y, Talley J. Empirical evidence on the use and effectiveness of telepsychiatry via videoconferencing: Implications for forensic and correctional psychiatry. Behav Sci Law. 2008;26:253–69. doi: 10.1002/bsl.812. [DOI] [PubMed] [Google Scholar]
- 25.Szeftel R, Hakak R, Meyer S, Naqvi S, Sulman-Smith H, Delrahim K, et al. Training psychiatric residents and fellows in a telepsychiatry clinic: A supervision model. Acad Psychiatry. 2008;32:393–9. doi: 10.1176/appi.ap.32.5.393. [DOI] [PubMed] [Google Scholar]
- 26.García-Lizana F, Muñoz-Mayorga I. What about telepsychiatry? A systematic review. Prim Care Companion J Clin Psychiatry. 2010;12 doi: 10.4088/PCC.09m00831whi. pii: PCC.09m00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharp IR, Kobak KA, Osman DA. The use of videoconferencing with patients with psychosis: A review of the literature. Ann Gen Psychiatry. 2011;10:14. doi: 10.1186/1744-859X-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Savin D, Glueck DA, Chardavoyne J, Yager J, Novins DK. Bridging cultures: Child psychiatry via videoconferencing. Child Adolesc Psychiatr Clin N Am. 2011;20:125–34. doi: 10.1016/j.chc.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Chipps J, Ramlall S, Mars M. A telepsychiatry model to support psychiatric outreach in the public sector in South Africa. Afr J Psychiatry (Johannesbg) 2012;15:264–70. doi: 10.4314/ajpsy.v15i4.34. [DOI] [PubMed] [Google Scholar]
- 30.Chipps J, Brysiewicz P, Mars M. Effectiveness and feasibility of telepsychiatry in resource constrained environments? A systematic review of the evidence. Afr J Psychiatry (Johannesbg) 2012;15:235–43. doi: 10.4314/ajpsy.v15i4.30. [DOI] [PubMed] [Google Scholar]
- 31.Wynn R, Bergvik S, Pettersen G, Fossum S. Clinicians’ experiences with videoconferencing in psychiatry. Stud Health Technol Inform. 2012;180:1218–20. [PubMed] [Google Scholar]
- 32.Butler TN, Yellowlees P. Cost analysis of store-and-forward telepsychiatry as a consultation model for primary care. Telemed J E Health. 2012;18:74–7. doi: 10.1089/tmj.2011.0086. [DOI] [PubMed] [Google Scholar]
- 33.Wood J, Stathis S, Smith A, Krause J. E-CYMHS: An expansion of a child and youth telepsychiatry model in Queensland. Australas Psychiatry. 2012;20:333–7. doi: 10.1177/1039856212450756. [DOI] [PubMed] [Google Scholar]
- 34.Lauckner C, Whitten P, Holtz B. 2014 International Conference on Collaboration Technologies and Systems (CTS) IEEE; 2014. [Last cited on 2016 Jul 20]. When technology alone is not enough: A discussion of a struggling telepsychiatry project and lessons from model programs; pp. 441–8. Available from: http://www.ieeexplore.ieee.org/lpdocs/epic03/wrapper.htm?arnumber=6867602 . [Google Scholar]
- 35.Saurman E, Johnston J, Hindman J, Kirby S, Lyle D. A transferable telepsychiatry model for improving access to emergency mental health care. J Telemed Telecare. 2014;20:391–9. doi: 10.1177/1357633X14552372. [DOI] [PubMed] [Google Scholar]
- 36.Trondsen MV, Bolle SR, Stensland GØ, Tjora A. Video-confidence: A qualitative exploration of videoconferencing for psychiatric emergencies. BMC Health Serv Res. 2014;14:544. doi: 10.1186/s12913-014-0544-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Salmoiraghi A, Hussain S. A systematic review of the use of telepsychiatry in acute settings. J Psychiatr Pract. 2015;21:389–93. doi: 10.1097/PRA.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 38.Doyle C, Jackson D, Loi S, Malta S, Moore K. Videoconferencing and telementoring about dementia care: Evaluation of a pilot model for sharing scarce old age psychiatry resources. Int Psychogeriatr. 2016;28:1567–74. doi: 10.1017/S1041610216000740. [DOI] [PubMed] [Google Scholar]
- 39.Drago A, Winding TN, Antypa N. Videoconferencing in psychiatry, a meta-analysis of assessment and treatment. Eur Psychiatry. 2016;36:29–37. doi: 10.1016/j.eurpsy.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 40.Hubley S, Lynch SB, Schneck C, Thomas M, Shore J. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6:269–82. doi: 10.5498/wjp.v6.i2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allely EB. Synchronous and asynchronous telemedicine. J Med Syst. 1995;19:207–12. doi: 10.1007/BF02257174. [DOI] [PubMed] [Google Scholar]
- 42.Balasinorwala VP, Shah NB, Chatterjee SD, Kale VP, Matcheswalla YA. Asynchronous telepsychiatry in Maharashtra, India: Study of feasibility and referral pattern. Indian J Psychol Med. 2014;36:299–301. doi: 10.4103/0253-7176.135384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Principles of Data Communications: Basic Concepts and Terminology [Internet] [Last cited on 2016 Oct 24]. Available from: http://www.sqa.org.uk/e-learning/NetTechDC01BCD/page_40htm#SynchronousTransmission .
- 44.Asynchronous telemedicine can improve healthcare delivery in rural areas. [Internet] [Last cited on 2016 Oct 24]. Available from: http://www.news-medical.net/news/20111222/Asynchronous-telemedicine-can-improve-healthcare-delivery-in-rural-areas.aspx .
- 45.Williams TL, May CR, Esmail A. Limitations of patient satisfaction studies in telehealthcare: A systematic review of the literature. Telemed J E Health. 2001;7:293–316. doi: 10.1089/15305620152814700. [DOI] [PubMed] [Google Scholar]
- 46.Dwyer TF. Telepsychiatry: Psychiatric consultation by interactive television. Am J Psychiatry. 1973;130:865–9. doi: 10.1176/ajp.130.8.865. [DOI] [PubMed] [Google Scholar]
- 47.Dongier M, Tempier R, Lalinec-Michaud M, Meunier D. Telepsychiatry: Psychiatric consultation through two-way television. A controlled study. Can J Psychiatry. 1986;31:32–4. doi: 10.1177/070674378603100107. [DOI] [PubMed] [Google Scholar]
- 48.Shore JH, Hilty DM, Yellowlees P. Emergency management guidelines for telepsychiatry. Gen Hosp Psychiatry. 2007;29:199–206. doi: 10.1016/j.genhosppsych.2007.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pakyurek M, Yellowlees P, Hilty D. The child and adolescent telepsychiatry consultation: Can it be a more effective clinical process for certain patients than conventional practice? [Last cited on 2016 Oct 26];Telemed J E Health [Internet] 2010 16:289–92. doi: 10.1089/tmj.2009.0130. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20406115 . [DOI] [PubMed] [Google Scholar]
- 50.Magaletta PR, Fagan TJ, Peyrot MF. Telehealth in the Federal Bureau of Prisons: Inmates’ perceptions? Prof Psychol Res Pract [Internet] 2000;31:497–502. Available from: http://doi.apa.org/getdoi.cfm?doi=10.1037/0735-7028.31.5.497 . [Google Scholar]
- 51.Math SB, Srinivasaraju R. Indian Psychiatric epidemiological studies: Learning from the past. Indian J Psychiatry. 2010;52(Suppl 1):S95–103. doi: 10.4103/0019-5545.69220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ganguli HC. Epidemiological findings on prevalence of mental disorders in India. Indian J Psychiatry. 2000;42:14–20. [PMC free article] [PubMed] [Google Scholar]
- 53.Malhotra S, Patra BN. Prevalence of child and adolescent psychiatric disorders in India: A systematic review and meta-analysis. Child Adolesc Psychiatry Ment Health. 2014;8:22. doi: 10.1186/1753-2000-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mohandas E. Roadmap to Indian psychiatry. Indian J Psychiatry. 2009;51:173–9. doi: 10.4103/0019-5545.55083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Government of India Planning Commission. Report of the Working Group on Disease Burden for 12th Five Year Plan: WG– 3(2)- Non Communicable Diseases [Internet] 2011. [Last cited on 2016 Oct 24]. Available from: http://planningcommission.nic.in/aboutus/committee/wrkgrp12/health/WG_3_2non_communicable.pdf .
- 56.Sinha SK, Kaur J. National mental health programme: Manpower development scheme of eleventh five-year plan. Indian J Psychiatry. 2011;53:261–5. doi: 10.4103/0019-5545.86821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hyler SE, Gangure DP, Batchelder ST. Can telepsychiatry replace in-person psychiatric assessments? A review and meta-analysis of comparison studies. CNS Spectr. 2005;10:403–13. doi: 10.1017/s109285290002277x. [DOI] [PubMed] [Google Scholar]
- 58.Malhotra S, Chakrabarti S, Shah R, Mehta A, Gupta A, Sharma M. A novel screening and diagnostic tool for child and adolescent psychiatric disorders for telepsychiatry. Indian J Psychol Med. 2015;37:288–98. doi: 10.4103/0253-7176.162921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thara R, John S, Rao K. Telepsychiatry in Chennai, India: The SCARF experience. Behav Sci Law. 2008;26:315–22. doi: 10.1002/bsl.816. [DOI] [PubMed] [Google Scholar]
- 60.Thara R, Sujit J. Mobile telepsychiatry in India. World Psychiatry. 2013;12:84. doi: 10.1002/wps.20025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Math SB, Moirangthem S, Kumar NC. Tele-psychiatry: After mars, can we reach the unreached? Indian J Psychol Med. 2015;37:120–1. doi: 10.4103/0253-7176.155606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thara R. Using mobile telepsychiatry to close the mental health gap. Curr Psychiatry Rep. 2012;14:167–8. doi: 10.1007/s11920-012-0267-x. [DOI] [PubMed] [Google Scholar]
- 63.Parekh A. Reaching the Unreachable: The Promise of Telepsychiatry in India. Columbia Soc Work Rev [Internet] 2015. [Last cited on 2016 Jul 14]. Available from: http://cswr.columbia.edu/article/reaching-the-unreachable-the-promise-of-telepsychiatry-in-india/
- 64.Malhotra S, Chakrabarti S, Gupta A, Mehta A, Shah R, Kumar V, et al. A self-guided relaxation module for telepsychiatric services: Development, usefulness, and feasibility. Int J Psychiatry Med. 2013;46:325–37. doi: 10.2190/PM.46.4.a. [DOI] [PubMed] [Google Scholar]
- 65.Malhotra S, Chakrabarti S, Shah R, Gupta A, Mehta A, Nithya B, et al. Development of a novel diagnostic system for a telepsychiatric application: A pilot validation study. BMC Res Notes. 2014;7:508. doi: 10.1186/1756-0500-7-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gogia P. Letter from Ganiyari. Natl Med J India. 2015;28:153–4. [PubMed] [Google Scholar]
- 67.Malhotra S, Chakrabarti S. Telepsychiatry Software Application – “Psychiatristonweb” Mental Healthcare at Your Doorstep. [Last cited on 2016 Oct 24]. Available from: http://www.14.139.56.217/
- 68.Government of India; Department of Science and Technology. Development and Implementation of a Model Telepsychiatry Application for Delivering Mental Healthcare in Remote Areas. [Last cited on 2016 Oct 24]. Available from: http://www.dst.gov.in/technology-systems-development-programme-tsdp .
- 69.Sahyog JS. [Last cited on 2016 Jul 17]. Available from: http://www.jssbilaspur.org/
- 70.Skype. [Last cited on 2016 Oct 24]. Available from: https://www.skype.com/en/download-skype/skype-for-computer/
- 71.Team Viewer. [Last cited on 2016 Oct 24]. Available from: https://www.teamviewer.com/en/download/windows/
- 72.National Institute of Mental Health and Neurosciences (NIMHANS) Bengaluru India. Virtual Knowledge Network (NIMHANS ECHO) [Last cited on 2016 Jul 17]. Available from: http://www.vlc.nimhans.ac.in/
- 73.The University of New Mexico. Project ECHO. [Last cited on 2016 Oct 24]. Available from: http://www.echounm.edu/
- 74.American Psychiatric Association. APA Committee on Telepsychiatry. [Last cited on 2016 Jul 30]. Available from: https://www.psychiatry.org/psychiatrists/practice/telepsychiatry .
- 75.Gorea RK. Legal aspects of telemedicine: Telemedical jurisprudence. [Last cited on 2016 Oct 24];J Punjab Acad Forensic Med Toxicol. 2005 5:3–5. Available from: http://www.medind.nic.in/jbc/t05/i1/jbct05i1p2.pdf . [Google Scholar]
- 76.Govt of India. National eHealth Authority (NeHA) 2015. [Last cited on 2016 Oct 24]. Available from: http://www.nhp.gov.in/UploadFiles/microsite/635689249545690829_1.pdf .