Abstract
Aim:
In a resource-poor country such as India, telepsychiatry could be an economical method to expand health-care services. This study was planned to compare the costing and feasibility of three different service delivery models. The end user was a state-funded long-stay Rehabilitation Center (RC) for the homeless.
Methodology:
Model A comprised patients going to a tertiary care center for clinical care, Model B was community outreach service, and Model C comprised telepsychiatry services. The costing included expenses incurred by the health system to complete a single consultation for a patient on an outpatient basis. It specifically excluded the cost borne by the care-receiver. No patients were interviewed for the study.
Results:
The RC had 736 inmates, of which 341 had mental illness of very long duration. On comparing the costing, Model A costed 6047.5 INR (100$), Model B costed 577.1 INR (9.1$), and Model C costed 137.2 INR (2.2$). Model C was found fifty times more economical when compared to Model A and four times more economical when compared to Model B.
Conclusion:
Telepsychiatry services connecting tertiary center and a primary health-care center have potential to be an economical model of service delivery compared to other traditional ones. This resource needs to be tapped in a better fashion to reach the unreached.
Keywords: Costing, reaching the unreached, telepsychiatry
INTRODUCTION
Telemedicine is defined as the practice of medical care using interactive or one-way audio, visual, and data communications. Worldwide, in both developed and developing economies, various programs for health-care delivery and education have used telemedicine.[1] Even in mental health-care delivery, several studies have demonstrated high reliability and patients’ acceptance of telepsychiatry.[2,3]
Many studies and reviews have tried to evaluate the cost-effectiveness of telepsychiatry using different methods such as Monte Carlo simulation and Markov's analysis.[4] However, uniform and reproducible techniques have not been developed so far which can be applied in all economic scenarios. Most studies examine the cost-using methods such as cost-feasibility, cost surveys, direct comparison of costs of telepsychiatry and in-person psychiatry. Some have reported the break-even number of consultations, the number that makes telepsychiatry comparable in cost to in-person psychiatry.[5,6] In all, telepsychiatry was found to be cost-effective and comparable in clinical outcomes compared to the usual care.[7,8]
The models of contemporary telemedicine in India link a tertiary care center, either with a district hospital or a nodal center[9,10,11] or a specialist unit which provides mobile telemedicine services,[12] or uses a smartphone-based web application,[9] or in some center uses an asynchronous method.[9,12,13,14] These systems have largely been underutilized and have failed to become an integral part of the health-care delivery system even after more than a decade of telepsychiatry in India. However, the felt need is a direct communication between a tertiary care center and a primary care center or a primary health center (PHC). In this background, we compared the costing of three different types of service delivery models.
METHODOLOGY
Setting
Rehabilitation Center (RC) for the homeless is a home run by the Social Welfare Department of the Government of Karnataka, India. The facility has 736 (however, this number is dynamic on a day-to-day basis) multi-ethnic inmates, of which 341 have mental illness of very long duration. On an average day, there are approximately 5–15 admissions to and discharges from this facility. A PHC is located inside the premises.
Mental health service delivery models for the inmates of Rehabilitation Center
In Model A, National Institute of Mental Health and Neurosciences (NIMHANS) receives inmates from a state-funded long-stay RC for the homeless. A three-member team consisting of a nurse, an attender, and a driver from RC brings the inmates to NIMHANS for consultation.
In Model B, the community psychiatry team of NIMHANS visits the RC for providing clinical care monthly. The team has 14 members, consisting of two senior consultant psychiatrists, two junior consultant psychiatrists, two psychiatry resident trainees, a junior consultant of clinical psychology, a trainee in clinical psychology, a consultant in psychiatric social work, two trainees in psychiatric social work, a nurse, a nursing trainee, and the driver. At each visit, the NIMHANS team could serve only 60–80 patients/visit.
Model C consisted of providing services on a weekly basis through telepsychiatry to make up for the gap in services at the RC. The service was started at RC from October 2013 on a pilot basis.
The treating team of RC, including doctors and nurses, were trained using synchronous mode telemedicine using Skype videoconferencing. They were also oriented toward clinical features of mental illness and identifying signs of early relapse. Telepsychiatry was utilized as a secondary consult. Telephonic consultation was used when there was nonavailability of internet.
Telemedicine
The internet service provider for RC and NIMHANS is the state-run Bharat Sanchar Nigam Limited and the bandwidth is about 1 Mbps though it ranges from 512 Kbps to 3 Mbps. The data subscription at both places was made on an annual basis, and no extra financial burden was imposed to start the telepsychiatry service. NIMHANS uses an Intel i-3 processor-based desktop computer system with a 17” monitor with an 8 MP Logitech video camera and Logitech speaker system and runs on Windows platform. RC used a similar desktop computer.
This retrospective report focused on comparing the costing/feasibility of the above-mentioned service delivery models (Models A, B, and C).
RESULTS
Table 1 gives the demographic and clinical details. Nearly half of the patients (49.5%) were from outside the state of Karnataka. Most of them reached Bengaluru by boarding a train (randomly as wandering mentally ill). Medical comorbidities detected included diabetes, hypertension, nutritional anemia, worm infestation, and dental caries. The medications used were the following - risperidone, olanzapine, aripiprazole, clozapine, trihexyphenydyl, haloperidol, chlorpromazine (CPZ), phenytoin, phenobarbitone, sodium valproate in addition to the regular drugs used for other medical conditions.
Table 1.
Demographic and clinical characteristics (n=341)
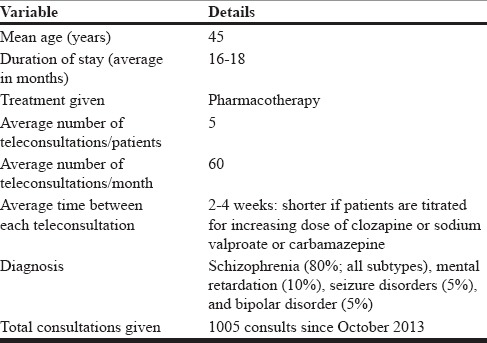
The average number of teleconsultations/patients from the initiation of services was about five. The average time between each teleconsultation was about 2–4 weeks. The total number of consultations from October 2013 to March 2015 was 1005, at an average of 60 patients/month or 20 patients weekly. A psychiatrist at NIMHANS and a doctor at RC conducted a teleconsultation. Until date, all teleconsultations were limited to psychopharmacology (follow-up care and prescription renewal). No psychological interventions have been provided through this portal.
Costing
The approximate salary per day of each team member is shown in Table 2. These data were based on the salary earned in the month of March 2015 by each member at NIMHANS and at RC. At the time of writing this manuscript, one US dollar (1 $) was selling at 64.12 INR. The total monthly estimated costs of each model are itemized [Table 3]. The calculation is based solely on the monthly salary of the health-care providers assuming they work 30 days a month and calculating the cost of a single day (including food).
Table 2.
Approximate salary of the treating team
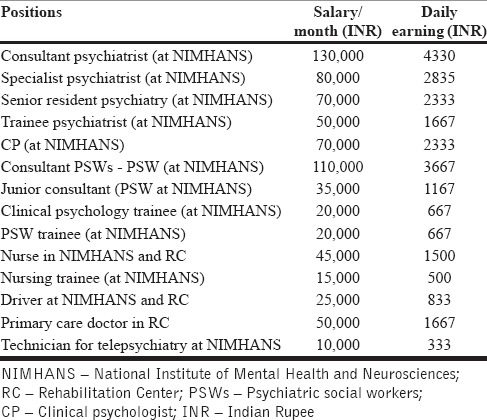
Table 3.
Comparison of costing of the three service delivery models
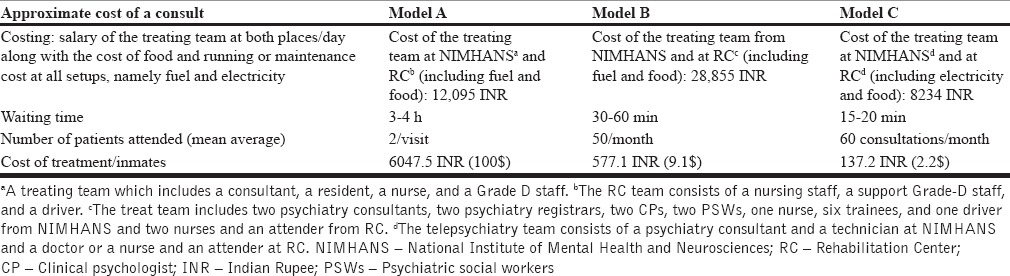
The cost of in-patient care at NIMHANS was excluded as the cost will be the same in all the three models. Equipment lifecycle replacement planning, maintenance, and communication costs are also excluded as they were covered in the maintenance schedule of NIMHANS and RC and were not limited to telepsychiatry alone. As both places are government-funded organizations, the maintenance is done by the technical team at no added cost.
Model A was the most expensive (6047.5 INR) and the least expensive was the one provided by telepsychiatry (137.2 INR). In calculating the costing, fixed items (nonrecurring expenses) were not taken into consideration as most of them were one-time expenses and do not add up to the operational cost significantly. Internet connectivity was already present in RC and a telemedicine service was already operational in NIMHANS for more than a decade. It has been argued that the turnover time for a computer and its operating system is <4 years but in a developing economy such as India with limited resources, the turnover time is longer, and the apparently dated system works as far as the line speed is not altered or decreased. In operating a telemedicine unit, technical specifications such as processor type/speed and operating system are not a hindrance to service delivery.
Indicators of improved outcomes
The rate of referrals had decreased. Hospitalization and readmission were reduced along with decreased travel time and expenditure to provide care. Since the initiation of service, only 5 patients were referred for inpatient treatment and 15 patients were set for outpatient care in 1 year. This translates into <2 patients/month. There was an increased access to health care, faster treatment, reduced waiting and consultation time, and increased medication adherence. Most investigations were completed within a week of a session of telepsychiatry, and titration of medicines no longer poses a challenge.
For the recipient (primary care team), there was increased availability of time in RC to attend other inmates. Travel expenditure was curtailed, and there was increased knowledge transfer from the telepsychiatry service provider (NIMHANS). The community psychiatry teams can give more service within the same time slot without added cost or additional workforce.
The above benefits are not quantified in measurable variables such as “quality-adjusted life-years” as the model was tested as a pilot to assess the effectiveness and sustainability. Until date, our model continues to function and deliver mental health services.
DISCUSSION
Our study has shown that the introduction of telepsychiatry services brought in a radical positive change in patient care in this facility without the need for additional workforce or resources. The services proved to be more economical than the traditional services.
Studies regarding the acceptance of telepsychiatry have found positive results for both patients and psychiatrists (cost-effective, accepted, sustainable, and reproducible) although some authors argue that better controlled studies are needed.[7,15,16,17,18,19,20] We believe that our model worked in this setting and is a successful one. It is simple and easily reproducible. The acceptance could be high from both the treating team and the inmates. The services have been continuing until date. However, the need for more systematic and controlled studies is the need of the hour.
Although there are guidelines on calculating cost, there is no universally accepted method to calculate cost-effectiveness. Most studies used models adapted to their local needs.[7,21,22,23] In some countries, the health insurance is mandatory and the insurance covers the cost of any form of treatment (usual care or telemedicine). However, many countries, particularly the underdeveloped and developing economies, do not have this coverage. In some developed economies, health care is a state subject and the state bears the expenses. In addition, different models are used to calculate cost of telemedicine consultation – insurance model, mathematical models, etc.,[4,24] but reproducibility in a setup like ours with lot of logistic limitations is difficult. It was a challenge to arrive at a result using the earlier models. Hence, we calculated the costing based on a day's cost of service or cost for session of consultation by the way of each of the three models.
How is this model different from some of the existing models in India?
As far as we know, this is the first of such studies, which has assessed the costing of telepsychiatry in the Indian subcontinent. This model is unique in many ways. The end users are the primary care team and their patients/inmates. The model does not operate on tertiary care-to-tertiary care centers where both the service provider and the recipient are specialists (Meher et al., 2012).[9,12,13,14] The model also does not operate where a tertiary care team goes out in the community, interacts with the patients, or takes their complaints and then communicates with the specialist back at their tertiary center.[12] It is not a web-based smartphone application where the underserved population has less to no access.[9] It provides a direct interaction with the patients through a primary care physician or a nurse. The mode is a synchronous system, which provides live interaction between a doctor and his/her patient. There is always a back-up system of a telephonic conversation when the internet connectivity becomes an issue to deliver service. The logistic difficulty of a primary care physician having to travel to a nodal center to take a telemedicine consult was eliminated. The acceptance rate by the primary care team is high. It works very well in the absence of a doctor whereby a trained nurse can present the patient's complaints to the tertiary center as shown by earlier studies.[25] Finally, it empowers a primary care team to handle simple and sometimes complex situations with the knowledge that the specialist is available for teleconsultation.
Our model also has its own challenges and problems. Availability of workforce remains a concern. The thinly staffed RC nurses sometimes have to prioritize the medically ill over the mentally ill. Teleconsultation on such occasions had to be shifted to a later slot in the week or month. Connectivity can be a hindrance to service delivery. The internet connectivity sometimes becomes unavailable or the speed of the connection slows down. It affects the detection of symptoms such as affect alteration and movement problems. Unavailability of medicine is the single most important factor for relapse and poor response to treatment by either telepsychiatry or the usual care. There have been many instances wherein a time gap existed between the availability of medications and the patients’ needs.
Limitations of the study
As it is a retrospective report, randomization could not be done and the actual effectiveness may be more or less than what is reported in this paper. However, the simple calculation made has at least shown that the model is effective, economical, and feasible. No structured instruments were used in assessing the acceptance of the service, clinical outcome, and service providers’ professional satisfaction.
CONCLUSION
Telepsychiatry services connecting tertiary center and a primary health-care center have potential to be an economical model of service delivery compared to the other traditional ones. This resource needs to be tapped in a better fashion to reach the unreached. In addition, studies with better methods of assessing cost-effectiveness need to be done.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would gratefully acknowledge the staff of the Rehabilitation Center for having extended their co-operation throughout this endeavor by providing logistic support and assistance.
REFERENCES
- 1.Siminerio L, Ruppert K, Huber K, Toledo FG. Telemedicine for Reach, Education, Access, and Treatment (TREAT): Linking telemedicine with diabetes self-management education to improve care in rural communities. Diabetes Educ. 2014;40:797–805. doi: 10.1177/0145721714551993. [DOI] [PubMed] [Google Scholar]
- 2.Bishop JE, O’Reilly RL, Maddox K, Hutchinson LJ. Client satisfaction in a feasibility study comparing face-to-face interviews with telepsychiatry. J Telemed Telecare. 2002;8:217–21. doi: 10.1258/135763302320272185. [DOI] [PubMed] [Google Scholar]
- 3.Morland LA, Raab M, Mackintosh MA, Rosen CS, Dismuke CE, Greene CJ, et al. Telemedicine: A cost-reducing means of delivering psychotherapy to rural combat veterans with PTSD. Telemed J E Health. 2013;19:754–9. doi: 10.1089/tmj.2012.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xin S. Markov modelling in healthcare economic evaluations. Chin J Evid Based Med. 2007;7:750–6. [Google Scholar]
- 5.Hyler SE, Gangure DP, Batchelder ST. Can telepsychiatry replace in-person psychiatric assessments? A review and meta-analysis of comparison studies. CNS Spectr. 2005;10:403–13. doi: 10.1017/s109285290002277x. [DOI] [PubMed] [Google Scholar]
- 6.O’Reilly R, Bishop J, Maddox K, Hutchinson L, Fisman M, Takhar J. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr Serv. 2007;58:836–43. doi: 10.1176/ps.2007.58.6.836. [DOI] [PubMed] [Google Scholar]
- 7.Modai I, Jabarin M, Kurs R, Barak P, Hanan I, Kitain L. Cost effectiveness, safety, and satisfaction with video telepsychiatry versus face-to-face care in ambulatory settings. Telemed J E Health. 2006;12:515–20. doi: 10.1089/tmj.2006.12.515. [DOI] [PubMed] [Google Scholar]
- 8.Mucic D. International telepsychiatry: A study of patient acceptability. J Telemed Telecare. 2008;14:241–3. doi: 10.1258/jtt.2008.080301. [DOI] [PubMed] [Google Scholar]
- 9.Malhotra S, Chakrabarti S, Shah R, Gupta A, Mehta A, Nithya B, et al. Development of a novel diagnostic system for a telepsychiatric application: A pilot validation study. BMC Res Notes. 2014;7:508. doi: 10.1186/1756-0500-7-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holla B, Viswanath B, Neelaveni S, Harish T, Kumar CN, Math SB. Karnataka state telemedicine project: Utilization pattern, current, and future challenges. Indian J Psychol Med. 2013;35:278–83. doi: 10.4103/0253-7176.119492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Math SB, Moirangthem S, Kumar NC. Tele-psychiatry: After mars, can we reach the unreached? Indian J Psychol Med. 2015;37:120–1. doi: 10.4103/0253-7176.155606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thara R, Sujit J. Mobile telepsychiatry in India. World Psychiatry. 2013;12:84. doi: 10.1002/wps.20025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balasinorwala VP, Shah NB, Chatterjee SD, Kale VP, Matcheswalla YA. Asynchronous telepsychiatry in maharashtra, India: Study of feasibility and referral pattern. Indian J Psychol Med. 2014;36:299–301. doi: 10.4103/0253-7176.135384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meher SK, Biswas A, Ratha BK. Legal issues among doctors in the implementation of teleconsultation: A study at AIIMS, New Delhi, India. Stud Health Technol Inform. 2013;192:1107. [PubMed] [Google Scholar]
- 15.Chung-Do J, Helm S, Fukuda M, Alicata D, Nishimura S, Else I. Rural mental health: Implications for telepsychiatry in clinical service, workforce development, and organizational capacity. Telemed J E Health. 2012;18:244–6. doi: 10.1089/tmj.2011.0107. [DOI] [PubMed] [Google Scholar]
- 16.Hyler SE, Gangure DP. A review of the costs of telepsychiatry. Psychiatr Serv. 2003;54:976–80. doi: 10.1176/appi.ps.54.7.976. [DOI] [PubMed] [Google Scholar]
- 17.Meglic M, Furlan M, Kuzmanic M, Kozel D, Baraga D, Kuhar I, et al. Feasibility of an eHealth service to support collaborative depression care: Results of a pilot study. J Med Internet Res. 2010;12:e63. doi: 10.2196/jmir.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Naveršnik K, Mrhar A. Cost-effectiveness of a novel e-health depression service. Telemed J E Health. 2013;19:110–6. doi: 10.1089/tmj.2012.0081. [DOI] [PubMed] [Google Scholar]
- 19.Pyne JM, Fortney JC, Mouden S, Lu L, Hudson TJ, Mittal D. Cost-effectiveness of on-site versus off-site collaborative care for depression in rural FQHCs. Psychiatr Serv. 2015;66:491–9. doi: 10.1176/appi.ps.201400186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rabinowitz T, Murphy KM, Amour JL, Ricci MA, Caputo MP, Newhouse PA. Benefits of a telepsychiatry consultation service for rural nursing home residents. Telemed J E Health. 2010;16:34–40. doi: 10.1089/tmj.2009.0088. [DOI] [PubMed] [Google Scholar]
- 21.Butler TN, Yellowlees P. Cost analysis of store-and-forward telepsychiatry as a consultation model for primary care. Telemed J E Health. 2012;18:74–7. doi: 10.1089/tmj.2011.0086. [DOI] [PubMed] [Google Scholar]
- 22.Naveršnik K, Mrhar A. Routine real-time cost-effectiveness monitoring of a web-based depression intervention: A risk-sharing proposal. J Med Internet Res. 2014;16:e67. doi: 10.2196/jmir.2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richter KP, Shireman TI, Ellerbeck EF, Cupertino AP, Catley D, Cox LS, et al. Comparative and cost effectiveness of telemedicine versus telephone counseling for smoking cessation. J Med Internet Res. 2015;17:e113. doi: 10.2196/jmir.3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dávalos ME, French MT, Burdick AE, Simmons SC. Economic evaluation of telemedicine: Review of the literature and research guidelines for benefit-cost analysis. Telemed J E Health. 2009;15:933–48. doi: 10.1089/tmj.2009.0067. [DOI] [PubMed] [Google Scholar]
- 25.Leahy M, Krishnasamy M, Herschtal A, Bressel M, Dryden T, Tai KH, et al. Satisfaction with nurse-led telephone follow up for low to intermediate risk prostate cancer patients treated with radical radiotherapy. A comparative study. Eur J Oncol Nurs. 2013;17:162–9. doi: 10.1016/j.ejon.2012.04.003. [DOI] [PubMed] [Google Scholar]


