Abstract
Background:
Mobile phone technology is being used worldwide to improve follow-ups in health care.
Aim:
Aim of the study is to evaluate whether the use of mobile technology will improve or not the follow-up of Indian patients from a community mental health center.
Materials and Methods:
Patients or caregivers having mobile phones and consenting for study were enrolled, and sociodemographic and clinical details of patients were taken. Participants were randomized into two groups (short message service [SMS] vs. non-SMS group). At first intervention level, a SMS was sent to SMS group (not in non-SMS group) 1 day before their appointment. At second-level intervention (voice call level), patients from both groups who missed their first appointment were given a voice call requesting them to come for follow-up, and the reasons for first missed appointments (MA) were also elicited. The effect of these two intervention levels (first SMS for SMS group and next voice calls for both groups) on follow-up was evaluated.
Results:
A total of 214 patients were enrolled in the study. At first SMS intervention level of SMS group (n = 106), 62.26% of participants reached appointment-on-time (RA), while in the non-SMS/as usual group (n = 108), 45.37% of patients RA. The difference of these groups is statistically significant. At second-level intervention (voice call), 66 of 88 (another 15 were unable to contact) were came for follow-up consultation within 2 days of MA. Distance and diagnosis of alcohol dependence were significantly associated with MA. Social reasons were most common reasons for first MA.
Conclusion:
The use of mobile phone technology in an outpatient community psychiatric clinic improved follow-up significantly.
Keywords: Community mental health clinic, follow-up, mobile phone
INTRODUCTION
Mobile technology has changed lifestyles of citizens globally and studies for its application in health care especially to improve follow-up is been increasing. There are various challenges in continuing care in mental health-care settings, among which missed appointments (MA) are a common occurrence in outpatient care settings,[1,2] yet little is known about the reasons for MA, especially in the Indian population. Follow-up studies from around the world including India[3,4,5,6,7,8,9,10,11,12] show that 16–60% of patients will not follow up in spite of the need for further treatment. About 30–60% of patients miss their appointments while 20–30% discontinue their treatment with subsequent lost to follow-up.[3,4,5,6,7,8,9,10,11,12] Most common reason for MA in the studies is patient errors such as forgetting or oversleeping followed by social stigma, financial reasons, logistics, or getting the date wrong.[1,2,11,12] The use of mobile phones has grown exponentially, especially in India. Mobile phones have been used to improve health outcomes in number of studies but its role to improve follow-up in psychiatry is yet to be established.
To fill this existing knowledge gap, this study evaluates the role of short message service (SMS) and voice calls in improving timely follow-up. We hypothesize that SMS and voice call reminders will improve the follow-up of patients in community mental health settings. The aim of study is to evaluate whether SMS and voice calls of mobile technology will improve the follow-up of patients in community mental health center. This study also aims to evaluate the reasons for MA.
MATERIALS AND METHODS
This study was conducted at the outpatient clinic of “Sakalawara Community Mental Health Centre” of “National Institute of Mental Health and Neurosciences” (NIMHANS), Bengaluru, India. It is a community-based mental health clinic situated (18 km away from the main campus of NIMHANS) in rural areas of Jigani Hobli, Anekal Taluk of Bengaluru district. Data were collected over a period of 6 months from November 2014 to April 2015. It is a randomized control study with stepped-up design. The Ethical Committee of NIMHANS approved this study.
Patients or caregivers (irrespective of clinical diagnosis) having valid mobile number and have competence to manage the English SMS were included in this study. Actively symptomatic patients who are without any caregiver and patients or caregivers who are incompetent to manage either voice call or English SMS were excluded from the study. All patients and/or their caregivers with these inclusion and exclusion criteria were recruited for the study after taking informed consent. All recruited participants received usual treatment, and a specific follow-up appointment date was given at the end of consultation. A person (either patient or caregiver) who will manage the SMS and/or voice call was decided at the time of recruitment. Sociodemographic and clinical data along with valid mobile number were collected in a semi-structured pro forma. The Charleston Psychiatric Outpatient Satisfaction Scale (CPOSS)[13] was administered to the patient.
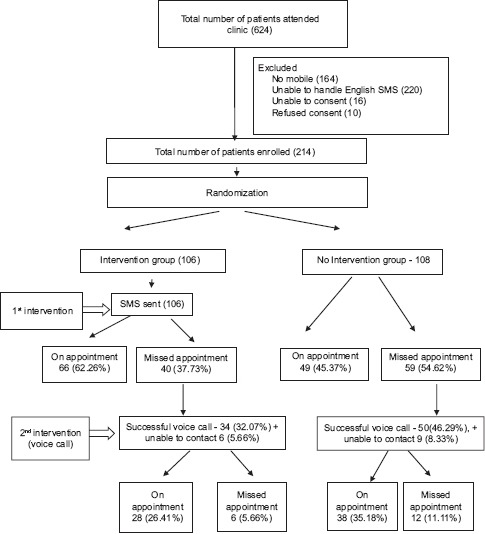
The study design is represented in Flow Diagram 1. Enrolled patients were randomized into two groups (SMS group vs. non-SMS group). All patients were unaware of their group at the time of enrollment. A SMS reminder was sent to SMS group 24–48 h before scheduled appointment day to patients/caregivers. Non-SMS group did not receive any intervention at the first level (as usual follow-up).
Flow Diagram 1.
Results
All patients from both groups who reached appointment-on-time (RA) were given usual treatment. Patients/caregivers who failed to follow-up on the scheduled appointment were contacted on their mobile number voice call. The reason for the MA was elicited through preformed questionnaire during voice call soon (described below), and obtained data were classified in seven broad categories. A new appointment date was fixed within the next 2 days of MA over the phone. For those patients that do not follow up even after a fresh appointment at the second intervention, the procedure as above was carried out for three more times after which the patient was considered lost to follow-up in the study.
Data were analyzed using SPSS Statistics 19.0 version (IBM, USA). Quantitative variables were summarized as mean ± standard deviation for normally distributed data or median (interquartile range) for nonnormal data, whereas categorical variables as number and percentage. Comparison of means of quantitative variables across different intervention groups was done by independent samples t-test for normal data or Mann–Whitney U-test for nonnormal data. Association between categorical variables was checked using Chi-square test. After first SMS versus non-SMS intervention, a bivariate logistic regression analysis was performed first to identify the variables associated with MA status, and those variables showing a Wald test P < 20% were considered for multiple logistic regression analysis. Odds ratio (OR) of MA status and their 95% confidence interval (CI) were estimated.
RESULTS
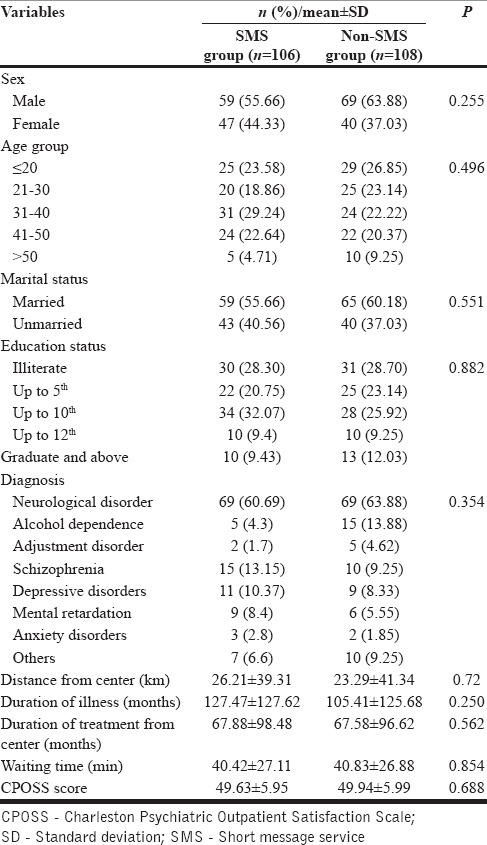
A total of 624 patients were screened for the study. Two hundred and fourteen (n = 214) patients who met inclusion and exclusion criteria were enrolled and randomized into two groups - SMS group (n = 106) and non-SMS group (n = 108). Table 1 shows that there is no statistical significance between two groups with reference to sociodemographic parameters (age, sex, marital status, education, distance from center, and waiting time before consultation), illness parameters (diagnosis, duration of treatment, and duration of treatment from the center), and score of CPOSS between SMS and non-SMS group.
Table 1.
Distribution of sociodemographic/clinical characteristics
Flow Diagram 1 shows that 66 patients in SMS group RA while 40 patients MA; in the non-SMS group consisting of 108 patients, 49 patients RA while 59 patients MA.
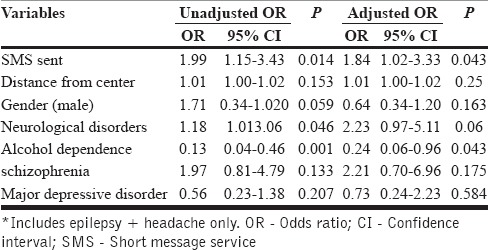
Bivariate analysis found that parameters such as age, education status, duration of illness, time since enrolled at clinic, waiting time before consultation in OPD, and CPOSS scores are not significantly affecting follow-up. Rest of the variables which were significant in the bivariate analysis were subjected to multiple logistic regression.
Multiple logistic regression analysis shows that sending SMS is a significant predictor to RA (OR: 1.84; 95% CI: 1.02–3.33). Diagnosis of alcohol dependence and distance from the center are other significant predictors for MA. Surprisingly, gender is a neutral predictor for MA or RA [Table 2].
Table 2.
Factors affecting missed appointments
Result shows that SMS reminders can help patient follow-up on appointment date significantly more as compared to no intervention (62.26% vs. 45.37%) while using SMS and voice call together can improve follow-up further significantly [Flow Diagram 1].
As the second-line intervention, patients with MA were communicated in voice call. Voice contact in SMS group was established with 34 patients, of which 28 came on new appointment date and in non-SMS group with 50 patients, of which 38 patients came on new appointment date [Flow Diagram 1].
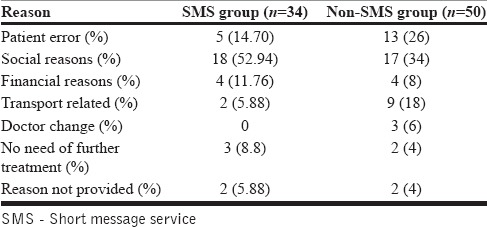
In evaluation of reasons for MA [Table 3] social issues were most common reasons in both SMS and non-SMS groups such as function at home and visit to parents. Patient-related errors such as forgetfulness and misunderstanding were less in the SMS versus non-SMS group (14.7% vs. 26%).
Table 3.
Reasons for missed appointments (n=84)
DISCUSSION
The use of SMS enhanced timely follow-up (SMS vs. non-SMS: % vs. %) which concurs with studies in nonpsychiatric setup.[14,15,16] We used the approach of sending SMS followed by voice call in this study and found highly effective similar to findings in other studies.[14,15,17,18,19,20,21] SMS reminder as the first step is cost-effective and easy to deliver to ensure follow-up, and voice call may be an important second step intervention to ensure follow-up for those who did not respond to SMS reminder.
Longer the distance from center and diagnosis of alcohol dependence was associated with MAs in our study which is similar to other studies[1,2] for them, there is need of innovative mobile technology to ensuring follow-up.
Social reasons were the most common reason for MA in this study in contrast with other studies where the most common reasons were patient-related errors.[1,2] This difference may be attributed to difference in sociocultural background and the difference in awareness of illness. This may need the prior inquiry about anticipated social reasons to ensure follow-up on appointment dates.
This study has some of the limitations such as small sample size and recruiting English SMS competence patients only. Future studies shall involve design with larger sample size with their native languages in view of significant positive result from this pilot study. There is need of more work to understand reasons for MA.
CONCLUSION
This study results conclude that the use of mobile phone technology in an outpatient community psychiatric clinic has improved the follow-up rates.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sparr LF, Moffitt MC, Ward MF. Missed psychiatric appointments: Who returns and who stays away. Am J Psychiatry. 1993;150:801–5. doi: 10.1176/ajp.150.5.801. [DOI] [PubMed] [Google Scholar]
- 2.Neal RD, Hussain-Gambles M, Allgar VL, Lawlor DA, Dempsey O. Reasons for and consequences of missed appointments in general practice in the UK: Questionnaire survey and prospective review of medical records. BMC Fam Pract. 2005;6:47. doi: 10.1186/1471-2296-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Killaspy H, Banerjee S, King M, Lloyd M. Prospective controlled study of psychiatric out-patient non-attendance. Characteristics and outcome. Br J Psychiatry. 2000;176:160–5. doi: 10.1192/bjp.176.2.160. [DOI] [PubMed] [Google Scholar]
- 4.Edlund MJ, Wang PS, Berglund PA, Katz SJ, Lin E, Kessler RC. Dropping out of mental health treatment: Patterns and predictors among epidemiological survey respondents in the United States and Ontario. Am J Psychiatry. 2002;159:845–51. doi: 10.1176/appi.ajp.159.5.845. [DOI] [PubMed] [Google Scholar]
- 5.Percudani M, Belloni G, Contini A, Barbui C. Monitoring community psychiatric services in Italy: Differences between patients who leave care and those who stay in treatment. Br J Psychiatry. 2002;180:254–9. doi: 10.1192/bjp.180.3.254. [DOI] [PubMed] [Google Scholar]
- 6.Rossi A, Amaddeo F, Bisoffi G, Ruggeri M, Thornicroft G, Tansella M. Dropping out of care: Inappropriate terminations of contact with community-based psychiatric services. Br J Psychiatry. 2002;181:331–8. doi: 10.1192/bjp.181.4.331. [DOI] [PubMed] [Google Scholar]
- 7.Tehrani E, Krussel J, Borg L, Munk-Jørgensen P. Dropping out of psychiatric treatment: A prospective study of a first-admission cohort. Acta Psychiatr Scand. 1996;94:266–71. doi: 10.1111/j.1600-0447.1996.tb09859.x. [DOI] [PubMed] [Google Scholar]
- 8.Swett C, Jr, Noones J. Factors associated with premature termination from outpatient treatment. Hosp Community Psychiatry. 1989;40:947–51. doi: 10.1176/ps.40.9.947. [DOI] [PubMed] [Google Scholar]
- 9.Mahneke T, Dragsted V, Jensen PS, Larsen SB, Meidahl B, Rosenbaum B. Ambulatory psychiatry – A follow-up after 1 year. Ugeskr Laeger. 1993;155:1464–8. [PubMed] [Google Scholar]
- 10.Pang AH, Lum FC, Ungvari GS, Wong CK, Leung YS. A prospective outcome study of patients missing regular psychiatric outpatient appointments. Soc Psychiatry Psychiatr Epidemiol. 1996;31:299–302. doi: 10.1007/BF00787924. [DOI] [PubMed] [Google Scholar]
- 11.Kulhara P, Chandiramani K, Mattoo SK, Varma VK. Pattern of follow up visits in a rural psychiatric clinic. Indian J Psychiatry. 1987;29:189–95. [PMC free article] [PubMed] [Google Scholar]
- 12.Gill HP, Singh G, Sharma KC. Study of dropouts from a psychiatric clinic of a general hospital. Indian J Psychiatry. 1990;32:152–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Pellegrin KL, Stuart GW, Maree B, Frueh BC, Ballenger JC. A brief scale for assessing patients’ satisfaction with care in outpatient psychiatric services. Psychiatr Serv. 2001;52:816–9. doi: 10.1176/appi.ps.52.6.816. [DOI] [PubMed] [Google Scholar]
- 14.Liew SM, Tong SF, Lee VK, Ng CJ, Leong KC, Teng CL. Text messaging reminders to reduce non-attendance in chronic disease follow-up: A clinical trial. Br J Gen Pract. 2009;59:916–20. doi: 10.3399/bjgp09X472250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: A systematic review. J Telemed Telecare. 2011;17:358–64. doi: 10.1258/jtt.2011.110707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geraghty M, Glynn F, Amin M, Kinsella J. Patient mobile telephone ‘text’ reminder: A novel way to reduce non-attendance at the ENT out-patient clinic. J Laryngol Otol. 2008;122:296–8. doi: 10.1017/S0022215107007906. [DOI] [PubMed] [Google Scholar]
- 17.Caplan W. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Global Health. 2006;2:9. doi: 10.1186/1744-8603-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, de Walque D, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: A randomized controlled trial of text message reminders. AIDS. 2011;25:825–34. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodrigues R, Shet A, Antony J, Sidney K, Arumugam K, Krishnamurthy S, et al. Supporting adherence to antiretroviral therapy with mobile phone reminders: Results from a cohort in South India. PLoS One. 2012;7:e40723. doi: 10.1371/journal.pone.0040723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sawyer SM, Zalan A, Bond LM. Telephone reminders improve adolescent clinic attendance: A randomized controlled trial. J Paediatr Child Health. 2002;38:79–83. doi: 10.1046/j.1440-1754.2002.00766.x. [DOI] [PubMed] [Google Scholar]
- 21.Junod Perron N, Dao MD, Righini NC, Humair JP, Broers B, Narring F, et al. Text-messaging versus telephone reminders to reduce missed appointments in an academic primary care clinic: A randomized controlled trial. BMC Health Serv Res. 2013;13:125. doi: 10.1186/1472-6963-13-125. [DOI] [PMC free article] [PubMed] [Google Scholar]


