Abstract
Introduction:
Depression is one of the under-recognized health problems in adolescents. Emotional instability resulted from childhood to adulthood transition makes adolescents vulnerable to depression.
Aims:
The aim of the study was to explore the prevalence of depression and its associated sociodemographic factors among school-going adolescents.
Materials and Methods:
This cross-sectional study was undertaken from January 2016 to June 2016 in adolescents studying in 9–12th standard from forty schools located in an urban area of Patna, Bihar. The self-administered questionnaire of Beck's Depression Inventory II was utilized to assess the prevalence of depression. Statistical analysis was done with Pearson's Chi-square test using SPSS software version 21.0.
Results:
Among the 1412 selected students, the prevalence of depression was found to be 49.2%, wherein the prevalence of severe depression was 7.7%. The overall prevalence of depression was significantly (P < 0.001) higher among girls (55.1%) than boys (45.8%). The prevalence of depression was found to be higher among students belonging to minorities (Buddhism, Jainism, etc.) (63.3%, P < 0.001). Elder students were found to be more depressed than younger students. Depression was found to be statistically significantly associated with gender and religion (P < 0.005). Guilty feeling (69.48%) was one of the most prominent clinical factors associated with depression followed by pessimism (58.14%), sadness (56.52%), and past failure (55.81%).
Conclusions:
Mental health is one of the most neglected aspects of our society. There is a need to increase awareness about depression among teachers and parents to identify and help depressed adolescents in the school.
Keywords: Adolescents, Beck's Depression Inventory-II, Depression, Prevalence
INTRODUCTION
Depression is one of the most common global mental health problems. In adolescents, it is one of the under-recognized health problems due to the inability to disclose their feelings and reluctant to seek psychiatric help. In the last century, the medical community did not accept the existence of depressive disorders in children. It was believed that children are lacking the mature psychological and cognitive structure needed to experience symptoms related to depressive disorders. However, a growing body of evidence proved that children not only experience the whole spectrum of mood disorders but also suffer from significant morbidity and mortality associated with them.[1] Recent studies have also confirmed the prevalence of depression (10%–60%) in adolescents.[1,2,3,4,5,6]
The transition period from childhood to adulthood is a stage marked by emotional instability that makes adolescents vulnerable to depression. Behavioral changes associated with hormonal changes during this period make depression difficult to diagnose. It is reported that more than 70% of the children with depression do not receive appropriate treatment.[7] The Diagnostic and Statistical Manual of Mental Disorders, Fifth edition has defined symptoms for depression; this includes depressed moods, psychomotor agitation or retardation, diminished interest or pleasure, insomnia, fatigue or loss of energy, diminished ability to concentrate, significant weight loss, feelings of worthlessness or excessive guilt, and recurrent thoughts of death. Individuals exhibiting five or more of those symptoms meet the criteria for major depressive disorders.[8,9]
There is no ideal screening or assessment tool available for depression assessments. However, combinations of optimal diagnostic tools followed by clinical interviews are commonly used for diagnosis and treatment of depression.[10] Exploring the magnitude of depression and associated sociodemographic factors among adolescents can contribute to the development of preventive and control strategies for depression. In the present study, we have attempted to estimate the prevalence of depression and its associated sociodemographic factors among school-going students in the rural and urban areas of Patna, Bihar.
MATERIALS AND METHODS
Study design and settings
A cross-sectional, observational study was undertaken from January 2016 to June 2016 in Patna district of Bihar. Bihar is an Indian state located in the northern region of the country with a population of about 100 million and has recorded a growth rate of 25% which exceeds the national average of about 17%.
Study population
Adolescents studying in 9–12th standard from forty schools located in the rural and urban areas of Patna, Bihar, were included in the study. All the students studying in 9–12th standards were eligible to participate in the study.
Sample size
A sample size of 1485 students was estimated considering 10% prevalence[4,5,6] of depression in adolescents with the 95% confidence interval, 20% acceptable margin of error, 10% of nonresponse rate, and design effect of 1.5.
Participant recruitment
Representative samples of students were selected using a two-stage cluster sampling method. In the first stage, out of 331 schools, forty schools were randomly selected as primary selection unit (PSU). In stage two, from each PSU, any one class was selected randomly among 9–12th standards as a sampling frame. From each sampling frame, a section of 37 students was selected for study participation. If there were more than 37 students in a section, all the students present in a section were included in the study.
Study tool
The Beck's Depression Inventory II (BDI) was utilized in the study which was translated into Hindi, translated back into English, and then piloted extensively by the All India Institute of Medical Sciences (AIIMS) team in Patna. The self-administered questionnaire comprised 21 items with multiple choice answers, and each answer being scored on a scale of values 0–3 with the maximum possible score of 63. A score of 0–13 was considered as normal, 14–19 as mild/borderline depression, 20–28 as moderate depression, and 29–63 as severe depression.
The questionnaire was distributed to the children as a group in their classrooms during a prearranged time. The children were asked to read the questionnaire and answer it to the best of their ability. Researchers were available to answer any of the children's questions or to clarify instructions; if someone was unable to comprehend the questions, an interview was taken to complete the study.
Statistical analysis
Statistical analyses were performed using the SPSS software version 21.0 (IBM). Descriptive analyses were computed in terms of mean and standard deviation for continuous variables and frequency with a percentage for nominal variables. Pearson's Chi-square test was used to compare categorical variables.
Ethical consideration
Written consent was obtained from the principals of each selected school prior to the study by properly explaining them about the purpose of the study. In each class, an informed consent from the students was obtained after being explained about the purpose of the study and that their responses would be kept confidential. Permission to carry out the study was granted by the Institutional Ethics Committee, AIIMS, Patna, and District Education Officer, Patna.
RESULTS
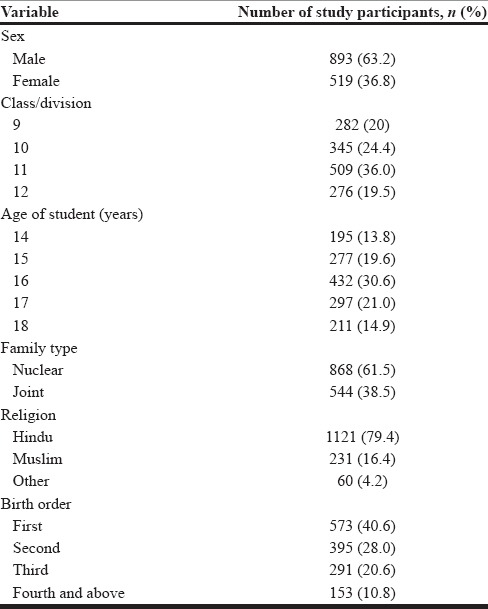
A total of 1485 students studying in Class 9 to Class 12 were enrolled in the study, of which approximately 1412 (response rate: 95.05%) students submitted an answer to all the questions. The mean age of selected students was 16.04 ± 1.24 years (range: 14–18 years). Out of all participating students, 893 (63.2%) were male and 519 (36.8%) were female. A majority of participants were from a nuclear family (61.5%) and belonged to Hindu religion (79.4%). Participating students were divided as per their birth order, in their family, as shown in Table 1.
Table 1.
Sociodemographic profile of selected participants
Overall, the prevalence of depression in selected students was found to be 49.2%, wherein the prevalence of severe depression was 7.7%, followed by moderate depression (18.1%), and mild depression (23.4%) [Figure 1].
Figure 1.
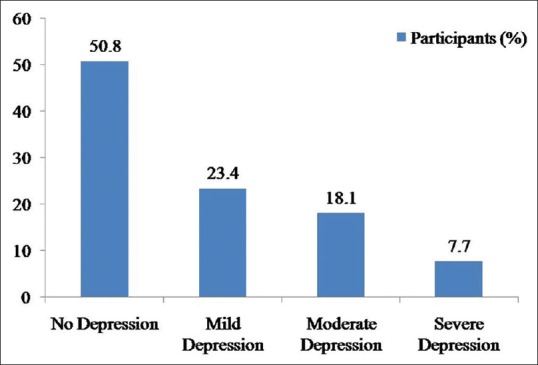
Prevalence of depression as per severity
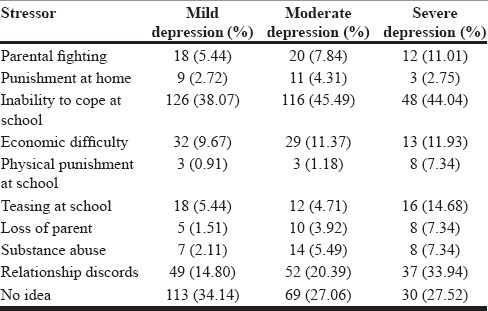
The prevalence of depression was found to be higher in girls (55.1%; P < 0.001) [Table 2]. Students belonging to minority community (Buddhism, Jainism, etc.) (63.3%) had the highest prevalence than students belonging to Hindu and Muslim communities (P < 0.001). The prevalence of depression was lowest among students who was born first in the family, peaked in students who were third, and dipped in students who were fourth and above in the family [Table 2 and Figure 2]. No considerable difference was observed in prevalence among students according to their class/division of study [Figure 3]. Guilty feeling (69.48%) was one of the most prominent clinical factors responsible for depression followed by pessimism (58.14%), sadness (56.52%), and past failure (55.81%) [Table 3]. Inability to cope with academics was one of the leading reasons for the high incidence of depression in the selected population followed by discord in familial relationships and economic difficulties [Table 4].
Table 2.
Prevalence of depression in selected students
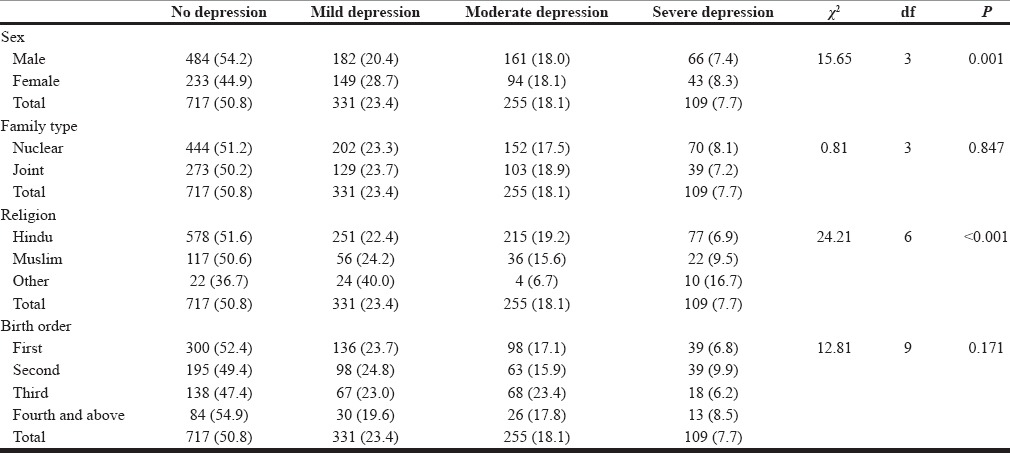
Figure 2.

Prevalence of depression according to age
Figure 3.
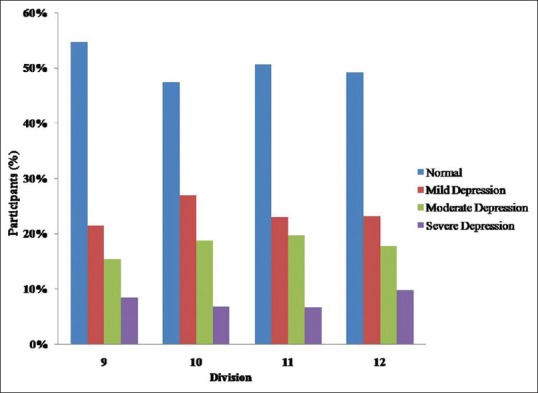
Prevalence of depression according to class/division
Table 3.
Number of participants according to clinical features and severity of depression
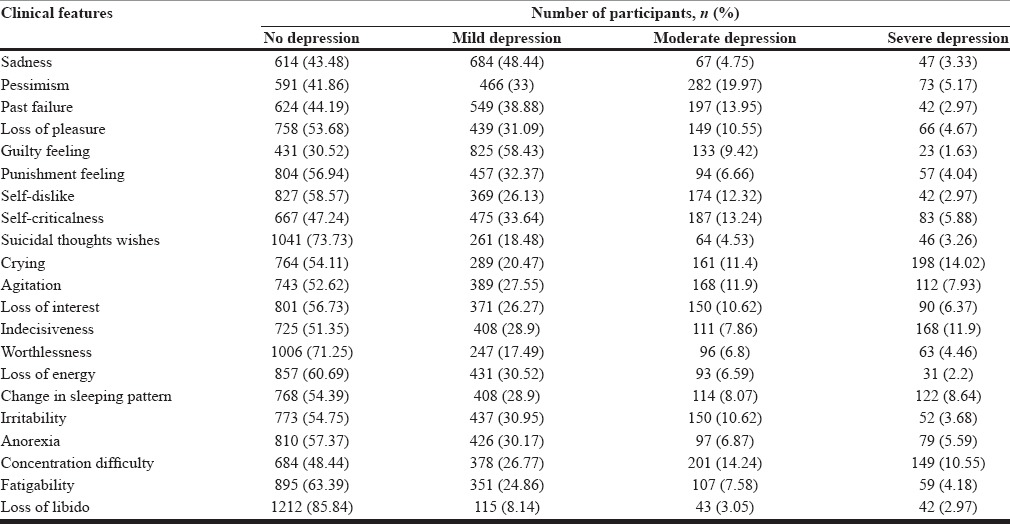
Table 4.
Psychological relationship of depression
DISCUSSION
Prevalence of depression in an adolescent may affect their social as well as personal life with potentially serious long-term consequences. Youth with depression is at high risk of mental disorders such as antisocial behavior and substance abuse disorders.[11] This makes it essential to assess the prevalence of depression in school-going adolescents.
Among the 1412 participants, 695 (49.2%) participants displayed signs of depression. Results of the present study are comparable to previously published study results.[2] In studies conducted by Nagendra et al. and Malik et al., the prevalence of depression was found to be around 50%, which is in line with our study results.[1,3] Several Indian studies conducted in adolescents have found a prevalence of depression ranging from 10% to 27%, which is much lower than our findings.[4,5,6]
The most common severity of depression observed in our study was mild depression (23.4%) followed by moderate depression (18.1%) and severe depression (7.7%). Naushad et al. (39.8%) and Malik et al. (26.6%) observed approximately similar prevalence of mild depression. However, in a study conducted by Malik et al., the prevalence of moderate depression (41.2%) was dominating, wherein the prevalence of severe depression (11.4%) was similar to our observations. On the other hand, the prevalence of severe depression in a study conducted by Naushad et al. was 1.8% which was much lesser than our observations as well as observations by Malik et al.[3,12]
The study results revealed that the prevalence of depression is significantly associated with gender, religion, and birth order of participants (P < 0.005) whereas family structure (P > 0.005) did not have any significant impact on the prevalence of depression [Table 2]. Gender has emerged as a leading factor associated with depression. Prevalence of depression was found to be slightly higher among females than males which are consistent with the results of earlier studies.[13,14] Angold et al. also attributed the preponderance of depression in adolescent females to hormonal changes in puberty.[15] On the contrary, Naushad et al. and Malik et al. reported a higher prevalence of depression among males which might be attributed to diverse culture points, the data collection tools, and settings of survey and timings.[3,12]
The prevalence of depression was also associated with the birth order of students. It was observed that there is an increase in the prevalence of depression with an increase in birth order as reported by Sidana et al.[8] The prevalence of depression was observed to be significantly higher among students belonging minorities. However, these findings cannot be generalized as number of participants belonging to these religions was very small, and there can be many factors associated with it. Our findings of increase in the prevalence with age is comparable with the results of previously reported studies.[1,12] However, there are few studies which did not find an increase in the prevalence of depression with age.[6] Higher prevalence of depression in elder students may be attributed to physical, emotional, and lifestyle changes occurred in their life.
No specific trend was observed in the prevalence of depression according to the division of study. On the contrary, Basin et al. have reported a higher prevalence of depression in 10th and 12th division students due to the pressure of academic performance in the board examinations.[16] We tried to identify factors responsible for the prevalence of depression. Guilty feeling, pessimism, sadness, and past failure were the prominent factors found to be responsible for depression. Inability to cope with academics at the school was another leading reason observed for the higher BDI scores followed by problematic relationships and economic difficulty. Other factors such as parental fighting, punishment at home or school, teasing at school, loss of parents, and substance abuse had a minor effect. The above findings suggest that students should receive mental counseling at school to cope up with studies and to mitigate other factors responsible for depression. Extra coaching by school teachers for students who are especially weak can help in overcoming hurdle.
It is reported that more that 70% of the children with depression do not receive appropriate diagnosis or treatment for depression.[7] It is necessary to create awareness about factors associated with depression among students, parents as well as in their teachers with the help of counselors. Our present study throws light on the magnitude of the problem among students and its associated factors which can be further evaluated by qualitative and quantitative methods.
CONCLUSIONS
We recommend active steps to increase awareness about depression among teachers and parents, with the help of school counselors, to identify and help depressed adolescents in the school. Active, early intervention can help prevent worsening of depression and its impact on life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nagendra K, Sanjay D, Gouli C, Kalappanavar NK, VinodKumar CS. Prevalence and association of depression and suicidal tendency among adolescent students. Int J Biomed Adv Res. 2012;3:714–9. [Google Scholar]
- 2.Mkize LP, Nonkelela NF, Mkize DL. Prevalence of depression in a university population. Curationis. 1998;21:32–7. [PubMed] [Google Scholar]
- 3.Malik M, Khanna P, Rohilla R, Mehta B, Goyal A. Prevalence of depression among school going adolescents in an urban area of Haryana, India. Int J Community Med Public Health. 2015;2:624–6. [Google Scholar]
- 4.Bhatia SK, Bhatia SC. Childhood and adolescent depression. Am Fam Physician. 2007;75:73–80. [PubMed] [Google Scholar]
- 5.Bostanci M, Ozdel O, Oguzhanoglu NK, Ozdel L, Ergin A, Ergin N, et al. Depressive symptomatology among university students in Denizli, Turkey: Prevalence and sociodemographic correlates. Croat Med J. 2005;46:96–100. [PubMed] [Google Scholar]
- 6.Ekundayo OJ, Dodson-Stallworth J, Roofe M, Aban IB, Kempf MC, Ehiri JE, et al. Prevalence and correlates of depressive symptoms among high school students in Hanover, Jamaica. ScientificWorldJournal. 2007;7:567–76. doi: 10.1100/tsw.2007.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Advisory Mental Health Council's Workgroup on Child and Adolescent Mental Health Development and Deployment. Washington, DC: National Institute of Mental Health; 2001. [Google Scholar]
- 8.Sidana S, Kishore J, Ghosh V, Gulati D, Jiloha R, Anand T. Prevalence of depression in students of a medical college in New Delhi: A cross-sectional study. Australas Med J. 2012;5:247–50. doi: 10.4066/AMJ.2012.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 10.Lasa L, Ayuso-Mateos JL, Vázquez-Barquero JL, Díez-Manrique EJ, Dowrick CE. The use of the Beck Depression Inventory to screen for depression in the general population: A preliminary analysis. J Affect Disord. 2000;57:261–5. doi: 10.1016/s0165-0327(99)00088-9. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention National Center for Injury Prevention and Control. Web Based Injury Statistics Query and Reporting System (WISQARS) 2016 [Google Scholar]
- 12.Naushad S, Farooqui W, Sharma S, Rani M, Singh R, Verma S. Study of proportion and determinants of depression among college students in Mangalore city. Niger Med J. 2014;55:156–60. doi: 10.4103/0300-1652.129657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asal AR, Abdel-Fattah MM. Prevalence, symptomatology, and risk factors for depression among high school students in Saudi Arabia. Neurosciences (Riyadh) 2007;12:8–16. [PubMed] [Google Scholar]
- 14.Eskin M, Ertekin K, Harlak H, Dereboy C. Prevalence of and factors related to depression in high school students. Turk Psikiyatri Derg. 2008;19:382–9. [PubMed] [Google Scholar]
- 15.Angold A, Costello EJ, Erkanli A, Worthman CM. Pubertal changes in hormone levels and depression in girls. Psychol Med. 1999;29:1043–53. doi: 10.1017/s0033291799008946. [DOI] [PubMed] [Google Scholar]
- 16.Bhasin SK, Sharma R, Saini NK. Depression, anxiety and stress among adolescent students belonging to affluent families: A school-based study. Indian J Pediatr. 2010;77:161–5. doi: 10.1007/s12098-009-0260-5. [DOI] [PubMed] [Google Scholar]


