Abstract
Background:
Anxiety and depressive disorders belong to the most common psychiatric disorders worldwide. They are generally seen in individuals who suffer from chronic diseases, such as diabetes mellitus (DM). The prevalence of depression among diabetics ranges from 8.5% to 32.5%, while that for anxiety it is up to 30%. In this study, we try to compare the mental health problems faced by those with Type I and Type II DM.
Materials and Methods:
Fifty patients diagnosed with Type I diabetes (T1D) and Type II diabetes each presenting to Medicine and Endocrinology Department were assessed with Hamilton Depression Rating Scale (HAM-D) for depression and Hamilton Anxiety Rating Scale (HAM-A) for anxiety. Patients were assessed on sociodemographic profile, duration of illness, type of treatment and then the data were analyzed on different domains.
Results:
On the assessment of patients with HAM-D a total of 38% with T1D were found to be depressed, and 42% patients with Type II diabetes had depression. Similarly, on assessment of anxiety with HAM-A, a total of 44% with T1D had anxiety. In patients with Type II diabetes, a total of 34% patients suffer from anxiety.
Conclusion:
The study concludes that Type I and Type II are slightly different in terms of associated psychiatric illnesses. In those with psychiatric illness, they do less well in terms of improving their overall diabetes control. The wider implication is that all the patients with diabetes should be regularly assessed for psychological problems. There needs to be greater psychological/psychiatric support available to intensive diabetes clinics.
Keywords: Anxiety, depression, diabetes
INTRODUCTION
The number of people with diabetes mellitus (DM) in India is increasing across geographic, ethnic, and administrative boundaries.[1,2,3] It is a known fact that DM, as well as psychiatric disorders, are common. These may co-occur with one another, and one may worsen the other. In addition, a variety of psychological distress can occur when DM is first diagnosed: denial, anger, guilt, reactive depression, and finally acceptance.
Acting through the hypothalamo-pituitary-adrenal axis, stress, and anxiety may initiate or worsen hyperglycemia. Depression may be a risk factor for the development of diabetes[4,5] it also commonly occurs in subjects with diabetes. Depression is associated with hyperglycemia and an increased risk for diabetic complications; relief of depression is associated with improved glycemic control.
A recent study has shown that leptin, originally studied in relation to adipose tissue, has receptors in the limbic system and could have a potential role in emotional processes. Increasing the leptin signals in the brain may be a new approach to treat depressive disorders.[6]
A meta-analysis of studies on the prevalence of co-morbid depression in adults with diabetes was published recently. The principal conclusion was that diabetes doubled the odds of depression,[7] i.e. persons with diabetes were twice as likely to have depression compared to those without diabetes. The odds of depression occurring in women were higher than in men. Depression may be related to complexities in the management of diabetes, or to neurohormonal abnormalities.[8]
Physicians caring for people with diabetes must be trained to recognize and manage comorbid psychiatric conditions that commonly occur. There are little published data from the Indian subcontinent on the coexistence of diabetes and psychiatric illness. This study attempts to compare the psychiatric manifestations of Type I and Type II DM.[9]
These investigators found that major depression was present in 14.7% and elevated depression symptoms in 26% of diabetic patients. Thus, as many as one in every three individuals with diabetes (at least in those participating in clinical studies) has depression at a level that impairs functioning and quality of life, adherence to medical treatment, and glycemic control, and increases the risk of diabetes complications.
The associations of depression with hyperglycemia and with increased risk of complications described in recent meta-analytic reviews support the hypothesis that the severity of diabetes and/or functional impairment may increase the risk for depression.[7]
MATERIALS AND METHODS
This study was conducted at a Tertiary Care Hospital in North India. Patients of both the sexes aged more than 18 years at the time of study were taken. Fifty patients diagnosed with Type I and fifty patients with Type II DM presenting to Medicine and Endocrinology Department were assessed on standardized rating scales for anxiety and depression.
Patients with the absence of preexisting depression/anxiety before the diagnosis of DM were considered for the study. However, those with associated drug and alcohol dependence, any serious organic illness, any other major psychiatric illness, like schizophrenia and mental retardation, those already on any psychotropic drug, or any history of psychiatric disorder, severe cognitive impairment were excluded from the study.
Hamilton Depression Rating Scale (HAM-D) was used for assessment of depressive symptoms and Hamilton Anxiety Rating Scale (HAM-A) for assessment of anxiety symptoms. Patients were assessed on sociodemographic profile, duration of illness, type of treatment using a sociodemographic pro forma, and then the data obtained was analyzed on different domains.
No ethical clearance or written consent was required as the study was conducted on outdoor patients. Oral consent, however, was taken.
RESULTS
On analyzing the sociodemographic data, it was found that mean age in those with DM Type I was 34.2 years whereas in Type II it was found to be 47.8 years. Thus, indicating that those with DM I presented at an earlier age as compared to those with Type II.
However, when comparing the educational status, marital status, and sex distribution of the two groups, no significant difference was found.
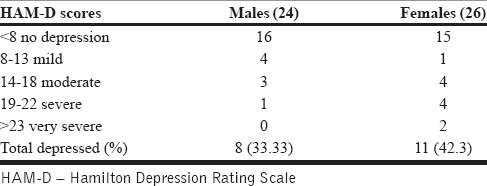
On the assessment of patients with HAM-D in Type I diabetes (T1D) group 33.3% (8) males were found to be depressed whereas 42.3% (11) females had depression. A total of 38% (19) patients with T1D were found to be depressed as shown in Table 1.
Table 1.
Severity of depressive disorder in patients with type I diabetes on the basis of Hamilton Depression Rating Scale
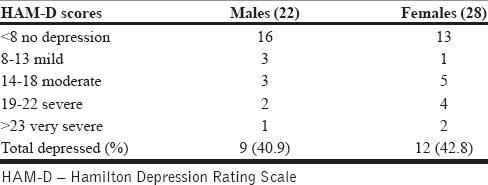
When those with Type II diabetes were assessed, it was found that 40.9% (9) males and 42.8% (12) females were depressed. Overall, 42% (21) patients with Type II diabetes were found to be depressed as in Table 2.
Table 2.
Severity of depressive disorder in patients with type II diabetes on the basis of Hamilton Depression Rating Scale
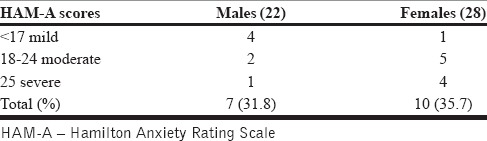
Similarly, on the assessment of anxiety with HAM-A for patients with T1D 37.5% (9) males and 50% (13) females had anxiety, i.e., a total of 44% (22) had anxiety as depicted in Table 3. In patients with Type II diabetes, 31.8% (7) males and 35.7% (10) females had anxiety, with a total of 34% (17) patients suffering from anxiety as shown in Table 4.
Table 3.
Severity of anxiety disorder in patients with type I diabetes on the basis of Hamilton Anxiety Rating Scale
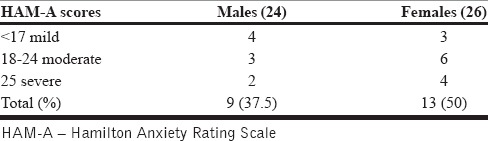
Table 4.
Severity of anxiety disorder in patients with type I diabetes on the basis of Hamilton Anxiety Rating Scale
Overall common symptoms found in patients with diabetes were depressed mood, anxiety, gastrointestinal symptoms, and genital symptoms such as loss of libido and erectile dysfunction.
Depressive symptoms were found to be more prominent in Type II as compared to Type I which had more prevalence of anxiety symptoms as depicted in Table 5 and Chart 1.
Table 5.
Comparison of depression and anxiety in type I versus type II diabetes
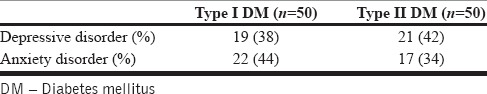
Chart 1.
Comparison of depression and anxiety in Type I versus Type II diabetes mellitus
DISCUSSION
The prevalence of a mental disorder, in general, in patients with DM is regarded to be comparable to the general population; an increased prevalence of depressive disorders and anxiety disorders has been reported in patients with DM. This co-occurrence of depression in diabetes is attributed to a variety of factors, including the psychological and psychosocial impact of the disease, a potential common genetic susceptibility and common pathophysiological abnormalities involving neuroimmunological and neuroendocrinol pathways, as well as microvascular brain lesions due to DM.[9]
It has been seen that individuals with T1D experience greater fatigue and less emotionally stable as compared to healthy individuals.[10] Patients low in emotional stability generally experience more negative affect, report more symptoms, and use dysfunctional coping. Low emotional stability is generally considered an important risk factor for developing anxiety and depressive symptoms.[11]
As expected, anxiety is more prevalent in T1D population than in the general population.[7] A study in the United Kingdom examined, the relationship between generic and diabetes-specific psychological factors and their impact on glycemic control in participants with T1D. Investigators found that anxiety was predictive of glycosylated hemoglobin (HbA1c), even after controlling for relevant demographic and medical covariates.[12] They also found that diabetes-related distress was a significant predictor of HbA1c. Diabetes-related distress attenuated the relationship between anxiety and HbA1c.[12] Another study by quotes the rates for anxiety disorders to be 32% and for the depressive disorder to be 30.04% in patients with T1D.[13]
These findings are similar to those in our study which reiterates the fact that T1D is more significantly associated with anxiety disorders.
The possible reason being that those with T1D have the difficult task of caring for a chronic disease, which requires maintenance multiple times a day, as well as living with the stress and fear of T1D complications. These fears regarding future complications can lead to anxiety spectrum disorders. Furthermore, anxiety in combination with depression and Type A behavior, life events stress, and interpersonal support may play important psychosocial roles in predicting health outcomes in diabetes as well.
In T1D, the physiological changes in the chronic course of the disease: weight gain, pain, hypertension, heart disease, loss of motor skills, or blindness directly affect the emotional state thus predisposing the person to mental disorders like anxiety and depression and vice versa.
There is a high prevalence of psychiatric disorders in T1D patients associated with anxiety-phobia.[14] With regard to anxiety disorders, panic disorder, (symptoms such as subsequent hyperventilation, palpitations, chest pain, nausea, numbness) seems similar to the symptoms of hypoglycemia, frequently observed in T1D, so one has to differentiate between the two to reduce the morbidity.
Furthermore, previous researches have demonstrated that female patients with T1D generally show poorer physical and psychosocial functioning (e.g., lower glycemic control and quality of life), use more maladaptive coping strategies and have a higher incidence of anxiety disorders than their male counterparts. They feel less confident about their body, as evidenced by the relatively high prevalence of eating disorders.[15,16,17]
This is in sync with our study which also shows a greater prevalence of psychiatric comorbidities in female patients as compared to males with T1D.
In addition, a study found that 16% were diagnosed with an ongoing major depressive episode, while 33% met the criteria for previous depressive disorders. Comorbid depression and T1D is also associated with poorer diabetes self-management and metabolic control, decreased quality of life, and higher health-care usage.[18]
Another study prospectively studied whether depression was associated with the risk of developing Type II diabetes, and vice versa and investigators found that during 10 years of follow-up, depressed mood increased the risk of developing Type II diabetes. In addition, those with Type II diabetes were at a significantly increased risk of developing clinical depression, regardless of treatment through oral hypoglycemic agents or insulin.[19]
In Type II diabetics, diabetes doubled the odds of depression.[7] As per our study, 38% in T1D and 42% in Type II diabetics are depressed, much more than that in nondiabetic population.
Depression may be related to neurohormonal abnormalities or complexities in the management of diabetes,[8] such as poor dietary intake, lack of exercise, sedentary lifestyle, hopelessness, poor treatment compliance, and leading to morbidity in diabetes.
Surveys and meta-analyses conducted on DM and depression have shown that the existence of DM doubles the probabilities of depression occurrence and that depressive symptoms were significantly more in women than in men.[20,21] A proclivity of female sex in anxiety and depressive disorders is observed in the general population as well. Women exhibited higher percentages of anxiety symptoms (almost three times higher), as shown in the surveys.[7] While the rates of depressive symptomatology were almost two times higher than those in men.
Our study also leads to similar observations with a greater percentage of women, i.e., 42.8% having depressive symptoms as compared to males (40.9%). The same is also true for anxiety symptoms in patients with Type II diabetes with 35.7% females and 31.8% males suffering from anxiety disorder. However, this difference is not that significant as compared to other studies. This can be because of gender bias that exists in our society and women do not come forward with their complaints till they become disabling.
These findings in the difference between the psychiatric manifestations in Type I versus Type II are in sync with those of our study, also emphasizing the fact that both Type I and Type II are separate entities.
CONCLUSION
The presence of depression and anxiety in patients with DM is of vast importance, as it is usually associated with poor disease control, adverse health outcomes and quality of life impairment. Comorbid psychiatric illness is a matter of great concern in patients with DM. It is not only highly prevalent but also highly persistent and recurrent leading to a significant negative impact on both clinical outcomes and quality of life. A further sensitization of health-care professionals, especially in primary care, is imperative, to enhance timely detection and treatment of depression in DM.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 2.Huizinga MM, Rothman RL. Addressing the diabetes pandemic: A comprehensive approach. Indian J Med Res. 2006;124:481–4. [PubMed] [Google Scholar]
- 3.Sadikot SM, Nigam A, Das S, Bajaj S, Zargar AH, Prasannakumar KM, et al. The burden of diabetes and impaired glucose tolerance in India using the WHO 1999 criteria: Prevalence of diabetes in India study (PODIS) Diabetes Res Clin Pract. 2004;66:301–7. doi: 10.1016/j.diabres.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 4.Eaton WW, Armenian H, Gallo J, Pratt L, Ford DE. Depression and risk for onset of type II diabetes. A prospective population-based study. Diabetes Care. 1996;19:1097–102. doi: 10.2337/diacare.19.10.1097. [DOI] [PubMed] [Google Scholar]
- 5.Freedland KE. Depression is a risk factor for the development of type 2 diabetes. Diabetes Spectr. 2004;17:150–2. [Google Scholar]
- 6.Lu XY, Kim CS, Frazer A, Zhang W. Leptin: A potential novel antidepressant. Proc Natl Acad Sci U S A. 2006;103:1593–8. doi: 10.1073/pnas.0508901103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 8.Sridhar GR, Madhu K. Depression and psychosocial stress in diabetes mellitus. In: Kapur A, Joshi JK, editors. Novo Nordisk Diabetes Update Proc. Mumbai: Business Network Inc; 2002. pp. 87–92. [Google Scholar]
- 9.Sridhar GR. Psychiatric co-morbidity & diabetes. Indian J Med Res. 2007;125:311–20. [PubMed] [Google Scholar]
- 10.Varni JW, Limbers CA, Bryant WP, Wilson DP. The PedsQL multidimensional fatigue scale in type 1 diabetes: Feasibility, reliability, and validity. Pediatr Diabetes. 2009;10:321–8. doi: 10.1111/j.1399-5448.2008.00482.x. [DOI] [PubMed] [Google Scholar]
- 11.Jylhä P, Isometsä E. The relationship of neuroticism and extraversion to symptoms of anxiety and depression in the general population. Depress Anxiety. 2006;23:281–9. doi: 10.1002/da.20167. [DOI] [PubMed] [Google Scholar]
- 12.Shaban C, Fosbury JA, Cavan DA, Kerr D, Skinner TC. The relationship between generic and diabetes specific psychological factors and glycaemic control in adults with type 1 diabetes. Diabetes Res Clin Pract. 2009;85:e26–9. doi: 10.1016/j.diabres.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A. Symptoms of depression and anxiety in youth with type 1 diabetes: A systematic review and meta-analysis. Psychoneuroendocrinology. 2016;70:70–84. doi: 10.1016/j.psyneuen.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 14.Engum A. The role of depression and anxiety in onset of diabetes in a large population-based study. J Psychosom Res. 2007;62:31–8. doi: 10.1016/j.jpsychores.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Enzlin P, Mathieu C, Demyttenaere K. Gender differences in the psychological adjustment to type 1 diabetes mellitus: An explorative study. Patient Educ Couns. 2002;48:139–45. doi: 10.1016/s0738-3991(02)00009-5. [DOI] [PubMed] [Google Scholar]
- 16.Undén AL, Elofsson S, Andréasson A, Hillered E, Eriksson I, Brismar K. Gender differences in self-rated health, quality of life, quality of care, and metabolic control in patients with diabetes. Gend Med. 2008;5:162–80. doi: 10.1016/j.genm.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Daneman D, Rodin G, Jones J, Colton P, Rydall A, Maharaj S, et al. Eating disorders in adolescent girls and young adult women with type 1 diabetes. Diabetes Spectr. 2002;15:83–105. [Google Scholar]
- 18.Egede LE, Ellis C. Diabetes and depression: Global perspectives. Diabetes Res Clin Pract. 2010;87:302–12. doi: 10.1016/j.diabres.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 19.Bloom BS. Prevalence and economic effects of depression. Manag Care. 2004;13(6 Suppl):9–16. [PubMed] [Google Scholar]
- 20.Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diabetes Care. 1993;16:1167–78. doi: 10.2337/diacare.16.8.1167. [DOI] [PubMed] [Google Scholar]
- 21.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with type 2 diabetes: A systematic review and meta-analysis. Diabet Med. 2006;23:1165–73. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]


