Abstract
Background
School‐based sexual and reproductive health programmes are widely accepted as an approach to reducing high‐risk sexual behaviour among adolescents. Many studies and systematic reviews have concentrated on measuring effects on knowledge or self‐reported behaviour rather than biological outcomes, such as pregnancy or prevalence of sexually transmitted infections (STIs).
Objectives
To evaluate the effects of school‐based sexual and reproductive health programmes on sexually transmitted infections (such as HIV, herpes simplex virus, and syphilis), and pregnancy among adolescents.
Search methods
We searched MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) for published peer‐reviewed journal articles; and ClinicalTrials.gov and the World Health Organization's (WHO) International Clinical Trials Registry Platform for prospective trials; AIDS Educaton and Global Information System (AEGIS) and National Library of Medicine (NLM) gateway for conference presentations; and the Centers for Disease Control and Prevention (CDC), UNAIDS, the WHO and the National Health Service (NHS) centre for Reviews and Dissemination (CRD) websites from 1990 to 7 April 2016. We handsearched the reference lists of all relevant papers.
Selection criteria
We included randomized controlled trials (RCTs), both individually randomized and cluster‐randomized, that evaluated school‐based programmes aimed at improving the sexual and reproductive health of adolescents.
Data collection and analysis
Two review authors independently assessed trials for inclusion, evaluated risk of bias, and extracted data. When appropriate, we obtained summary measures of treatment effect through a random‐effects meta‐analysis and we reported them using risk ratios (RR) with 95% confidence intervals (CIs). We assessed the certainty of the evidence using the GRADE approach.
Main results
We included eight cluster‐RCTs that enrolled 55,157 participants. Five trials were conducted in sub‐Saharan Africa (Malawi, South Africa, Tanzania, Zimbabwe, and Kenya), one in Latin America (Chile), and two in Europe (England and Scotland).
Sexual and reproductive health educational programmes
Six trials evaluated school‐based educational interventions.
In these trials, the educational programmes evaluated had no demonstrable effect on the prevalence of HIV (RR 1.03, 95% CI 0.80 to 1.32, three trials; 14,163 participants; low certainty evidence), or other STIs (herpes simplex virus prevalence: RR 1.04, 95% CI 0.94 to 1.15; three trials, 17,445 participants; moderate certainty evidence; syphilis prevalence: RR 0.81, 95% CI 0.47 to 1.39; one trial, 6977 participants; low certainty evidence). There was also no apparent effect on the number of young women who were pregnant at the end of the trial (RR 0.99, 95% CI 0.84 to 1.16; three trials, 8280 participants; moderate certainty evidence).
Material or monetary incentive‐based programmes to promote school attendance
Two trials evaluated incentive‐based programmes to promote school attendance.
In these two trials, the incentives used had no demonstrable effect on HIV prevalence (RR 1.23, 95% CI 0.51 to 2.96; two trials, 3805 participants; low certainty evidence). Compared to controls, the prevalence of herpes simplex virus infection was lower in young women receiving a monthly cash incentive to stay in school (RR 0.30, 95% CI 0.11 to 0.85), but not in young people given free school uniforms (Data not pooled, two trials, 7229 participants; very low certainty evidence). One trial evaluated the effects on syphilis and the prevalence was too low to detect or exclude effects confidently (RR 0.41, 95% CI 0.05 to 3.27; one trial, 1291 participants; very low certainty evidence). However, the number of young women who were pregnant at the end of the trial was lower among those who received incentives (RR 0.76, 95% CI 0.58 to 0.99; two trials, 4200 participants; low certainty evidence).
Combined educational and incentive‐based programmes
The single trial that evaluated free school uniforms also included a trial arm in which participants received both uniforms and a programme of sexual and reproductive education. In this trial arm herpes simplex virus infection was reduced (RR 0.82, 95% CI 0.68 to 0.99; one trial, 5899 participants; low certainty evidence), predominantly in young women, but no effect was detected for HIV or pregnancy (low certainty evidence).
Authors' conclusions
There is a continued need to provide health services to adolescents that include contraceptive choices and condoms and that involve them in the design of services. Schools may be a good place in which to provide these services. There is little evidence that educational curriculum‐based programmes alone are effective in improving sexual and reproductive health outcomes for adolescents. Incentive‐based interventions that focus on keeping young people in secondary school may reduce adolescent pregnancy but further trials are needed to confirm this.
15 April 2019
Update pending
Studies awaiting assessment
The CIDG is currently examining a new search conducted in April 2019 for potentially relevant studies. These studies have not yet been incorporated into this Cochrane Review. All eligible published studies found in the last search (7 Apr, 2016) were included and five ongoing studies were identified (see 'Characteristics of ongoing studies' section).
Plain language summary
School‐based interventions for preventing HIV, sexually transmitted infections, and pregnancy in adolescents
Cochrane researchers conducted a review of the effects of school‐based interventions for reducing HIV, sexually transmitted infections (STIs), and pregnancy in adolescents. After searching for relevant trials up to 7 April 2016, they included eight trials that had enrolled 55,157 adolescents.
Why is this important and how might school‐based programmes work?
Sexually active adolescents, particularly young women, are at high risk in many countries of contracting HIV and other STIs. Early unintended pregnancy can also have a detrimental impact on young people's lives.
The school environment plays an important role in the development of children and young people, and curriculum‐based sexuality education programmes have become popular in many regions of the world. While there is some evidence that these programmes improve knowledge and reduce self‐reported risk taking, this review evaluated whether they have any impact on the number of young people that contracted STIs or on the number of adolescent pregnancies.
What the research says
Sexual and reproductive health education programmes
As they are currently configured, educational programmes alone probably have no effect on the number of young people infected with HIV during adolescence (low certainty evidence). They also probably have no effect on the number of young people infected with other STIs (herpes simplex virus: moderate certainty evidence; syphilis: low certainty evidence), or the number of adolescent pregnancies (moderate certainty evidence).
Material or monetary incentive‐based programmes to promote school attendance
Giving monthly cash, or free school uniforms, to encourage students to stay in school may have no effect on the number of young people infected with HIV during adolescence (low certainty evidence). We do not currently know whether monthly cash or free school uniforms will reduce the number of young people infected with other STIs (very low certainty evidence). However, incentives to promote school attendance may reduce the number of adolescent pregnancies (low certainty evidence).
Combined educational and incentive‐based programmes
Based on a single included trial, giving an incentive such as a free school uniform combined with a programme of sexual and reproductive health education may reduce STIs (herpes simplex virus; low certainty evidence) in young women, but no effect was detected for HIV or pregnancy (low certainty evidence).
Authors' conclusions
There is currently little evidence that educational programmes alone are effective at reducing STIs or adolescent pregnancy. Incentive‐based interventions that focus on keeping young people, especially girls, in secondary school may reduce adolescent pregnancy but further high quality trials are needed to confirm this.
Summary of findings
Background
Description of the condition
Adolescents have been recognized as having an important place in the post‐2015 development agenda (United Nations 2015); indeed three of the United Nation's sustainable development goals (SDGs) specifically target adolescent sexual and reproductive health, and access to appropriate health services as a human right. However, adolescents, particularly those under 16 years of age, constitute a high‐risk group who are less likely to use or have access to condoms or contraceptives (Harrison 2005; Mathews 2009; Pettifor 2005; UNAIDS 2012).
Incident HIV infections amongst young people aged 15 to 24 years account for almost half of new infections (UNAIDS 2012). These have increased since 2000, with adolescents within the African region having 90% of the world's HIV‐related adolescent deaths (World Health Organization 2014). Despite a downward trend in adolescent pregnancy worldwide (World Bank 2016), most pregnancies in girls under the age of 18 are unwanted and many are terminated. Restrictive abortion laws and lack of services can result in high levels of maternal mortality (Grimes 2006). If the pregnancy is continued and unwanted, it is associated with adverse outcomes for both the mother's and infant's health (Pallitto 2005). A meta‐analysis that examined risk factors for pregnancy for girls aged between 13 and 19 years, found that sociodemographic indicators, family disruption, and leaving school early were the most consistently associated factors (Imamura 2007).
The effect of intimate partner violence on young women’s ability to control their sexual and reproductive health has also been highlighted as an important issue (Garcia‐Moreno 2013). Poor health‐related outcomes can result from lack of autonomy and difficulty in accessing services. Pregnancy coercion and birth control sabotage has been linked to unintended pregnancy (Miller 2010; Thiel de Bocanegra 2010), and limitations on condom use (Katz 2015), which increases the risk and incidence of sexually transmitted infections (STIs), including HIV (Dhairyawan 2013). It is also associated with poor perinatal and maternal health with increased risk of low birth weight and preterm birth (Shah 2010).
Programmes that promote sexual abstinence and delay of sexual initiation in adolescence have been unsuccessful in reducing self‐reported pregnancy and STIs (Underhill 2008; Oringanje 2016).
Description of the intervention
The school environment plays a pivotal role in the socialization and development of children and young people and has been considered to be an appropriate setting for interventions to promote adolescent sexual and reproductive health (Dick 2006; Mason‐Jones 2012; UNAIDS 1997).
Schools bring together large numbers of young people within an established infrastructure, and can provide systems into which interventions can be incorporated. As many young people spend a substantial amount of time in school, it is also an arena for peer connections and the development of relationships that influence individual and group behaviour within the school, and beyond into local communities; although it is important to recognize that schools are not always supportive or safe social environments for young people (Abrahams 2006; Kaplan 2007; Plummer 2007). It is known that dropping out of school can result in adverse health outcomes for young people (Freudenberg 2007).
Schools have been the setting for many sexual and reproductive health programmes that have been regarded as being successful (Kirby 2006), and curriculum‐based sexuality education programmes have become popular in many regions of the world. Most of these programmes have been based on the theory of social learning (Bandura 1977), the health belief model (Rosenstock 1988), the theory of reasoned action (Fishbein 2010) ‐ or adaptations of these theories ‐ and aim to change attitudes, intentions, behaviours, and social norms through improved knowledge and understanding of the risks of early sexual initiation, and the importance of contraceptive and/or condom use. Many studies have also incorporated the 17 characteristics of programmes that are considered previously to have been successful (Kirby 2009).
Thus, a range of educational interventions has been developed to promote sexual and reproductive health among adolescents, which aims to reduce the incidence of HIV, STIs, and early unwanted pregnancies. Many of these programmes encourage abstinence from sexual activity, the postponement of sexual debut until later years, or encourage secondary delay (that is, those who have their sexual debut delaying further sexual activity). They also encourage increase in condom use among those adolescents who are sexually active. Interventions include programmes delivered by teachers or peer educators that may be supplemented by condom distribution programmes, and others that include targeted health service provision and include drama, role play, and other engagement activities.
Other evidence suggests that simply staying on at school can have positive effects on sexual and reproductive health outcomes, and that encouraging school attendance helps girls in particular to avoid early sexual activity and pregnancy (Black 2008; Monstad 2008).
How the intervention might work
Many sexual and reproductive health education programmes are based on behavioural science theories (Glanz 2010), and aim to improve knowledge, change attitudes, intentions, behaviours, and social norms around sexual and reproductive health. There have been a large number of systematic reviews that evaluated the effectiveness of these programmes (Chin 2012; Dick 2006; DiClemente 2008; Flisher 2008; Gallant 2004; Harrison 2010; Johnson 2003; Johnson, 2011; Kim 2008; Kirby 2007; Lazarus 2010; Magnussen 2004; Medley 2009; Michielsen 2010; Paul 2008; Shepherd 2010; Yankah 2008), including reviews that have focused solely on school‐based interventions (Bennet 2005; Fonner 2014; Kirby 2006; Lopez 2016; Paul 2008), and a review of reviews (Mavedzenge 2013). Many of these reviews have suggested that school‐ and community‐based prevention programmes for adolescents have been effective in delaying self‐reported sexual activity, HIV‐related preventative behaviours, adolescent pregnancy, and STIs (Chin 2012; Fonner 2014; Johnson 2003; Johnson, 2011; Kirby 2009; Laud 2016), although others have reported less, or mixed, success (Bennet 2005; DiCenso 2002; Lopez 2016Oringanje 2016). The logic model for how these programmes might be thought to influence sexual and reproductive health outcomes can be seen in Figure 1.
1.
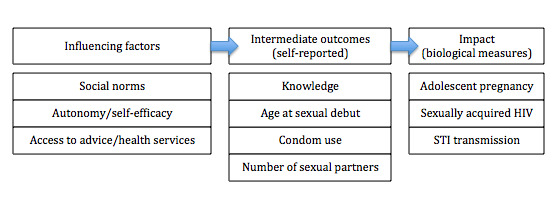
Logic model showing potential causal chain from influencing factors to impact.
As school dropout has negative effects on health outcomes for young people (Freudenberg 2007), researchers have become interested in using cash or other types of transfers (such as free school uniforms or vouchers) as incentives for adolescents to remain at school (Baird 2009; Baird 2010). Conditional and unconditional cash or other transfer programmes have been introduced to take into account the substantial financial barriers to remaining at school or to accessing health services (Pettifor 2012), especially where these are not freely provided on a universal basis. These programmes view staying at school ‐ especially for girls ‐ as a ‘social vaccine’, based on evidence that the longer adolescents stay in education the less likely they are to engage in high risk sexual behaviour, such as transactional sex, or because pregnancy or STI/HIV risks would interrupt their longer‐term aspirations and career plans.
Why it is important to do this review
Most evaluations of school‐ and community‐based programmes, or indeed of any interventions to improve the sexual and reproductive health of young people, have used self‐reported sexual behaviours as their main outcomes. However, self‐report measures have been found to be prone to bias (Langhaug 2011; Plummer 2004), and, as such, may well be an unreliable surrogate measure for effects such as sexually acquired infections and pregnancy (Brown 2015). Therefore, this review focuses on the effect of such interventions on biological outcome measures. Incidence of HIV or other STIs, or pregnancy are the most convincing indicators of the effectiveness of preventative interventions. This systematic review provides a unique contribution to the field because it only included studies if biological outcomes, such as HIV, STIs, or pregnancy, had been measured objectively. There are also varying interpretations of the strength of the evidence regarding school‐based HIV, STIs, and pregnancy prevention programmes for adolescents. This systematic review also provides more detail about the current strength of the evidence by using the GRADE assessment tool.
Objectives
To evaluate the effects of school‐based sexual and reproductive health programmes on sexually transmitted infections (such as HIV, herpes simplex virus, and syphilis), and pregnancy among adolescents.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs) (both individually randomized and cluster‐randomized).
Types of participants
Adolescents (defined as 10 to 19 year olds) attending primary, middle, or high (secondary) school at the time of the intervention.
In countries where children start school at a later age, or where school populations sometimes include young people over the age of 20 years, we included these studies if most of the participants (over 50%) were adolescents.
Types of interventions
We included any intervention that aimed to reduce the risk of HIV or other sexually transmitted infections (STIs) or pregnancy among adolescents, and was primarily conducted in schools or linked to schools or school attendance, with or without a community component. Some were curriculum‐based educational interventions primarily delivered by adults (teachers, or other adults) or peers (peer educators), or included additional features to change the school or community environment (for example, by changing school policies or improving health services). Other interventions focused on encouraging adolescents to stay at school by providing incentives (cash or other material transfers).
Types of outcome measures
Clinical/biological outcomes:
HIV prevalence;
STI prevalence;
Pregnancy prevalence.
Behavioural self‐reported outcomes:
use of male condoms at first sex;
use of male condoms at most recent (last) sex;
incidence of sexual initiation (sexual debut).
Search methods for identification of studies
Electronic searches
We developed the search strategy with the assistance of the HIV/AIDS Review Group Information Specialist and developed a comprehensive search strategy in an attempt to identify all relevant studies regardless of language or publication status (published, unpublished, in press, and in progress). We searched the following bibliographic databases for the years 1990 to 7 April 2016 using the search terms presented in the Appendices: MEDLINE (Appendix 1), Embase (Appendix 2), CENTRAL (the Cochrane Central Register of Controlled Trials) (Appendix 3), the World Health Organization (WHO) International Clinical Trials Registry Platform (apps.who.int/trialsearch; Appendix 4), and ClinicalTrials.gov (clinicaltrials.gov). We also searched the following conference databases: AIDS Education Global Information System (AEGIS) (www.aegis.com), and NLM GATEWAY (gateway.nlm.nih.gov/gw).
Searching other resources
We also searched libraries of relevant organizations and international agencies: the Centers for Disease Control and Prevention (CDC), UNAIDS, the WHO, and the National Health Service (NHS) Centre for Reviews and Dissemination (CRD). We handsearched the reference lists of all relevant papers, including systematic reviews and reviews of reviews. We contacted researchers, research institutions, relevant government departments, and organizations that were known to conduct school‐based HIV intervention research or were known to us to identify further published and unpublished studies. Where we were unable to obtain sufficient data from the published articles, we contacted the study authors to request further information about ongoing trials, raw data, and unpublished work.
Data collection and analysis
Selection of studies
Two review authors (AMJ and either DS, CM, AH, or AK) independently reviewed all titles and abstracts identified in the search for relevant trials for the review. We obtained full‐text articles for all studies that both review authors recorded as potentially relevant for the review. If the two review authors did not agree initially, we obtained the full‐text article and consulted a third review author to make the decision. We listed all full‐text articles that we excluded and their reasons for exclusion in a 'Characteristics of excluded studies' table. Also, we constructed a PRISMA diagram to illustrate the study selection process (Figure 2).
2.
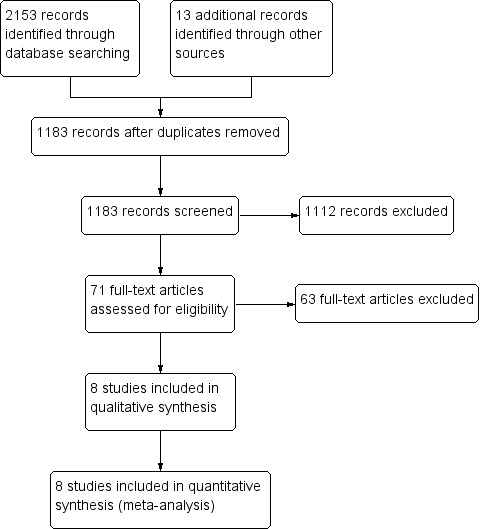
Study flow diagram.
Data extraction and management
Two review authors (AMJ and either DS, CM, AH, or AK) independently extracted data on study design (location, context, theoretical framework, dates, duration of follow‐up), participants (age, gender, language, ethnicity), interventions (type and complexity of the intervention and all the component parts, length of training of teachers or facilitators, content and duration of the intervention, intensity of the intervention), and methodological quality (method of randomization, attrition, sample size, adjustments for assignment bias, appropriateness of analysis for cluster RCTs, potential confounders, and protection against contamination), using a standardized data extraction form designed specifically for the purpose.
For the meta‐analysis of the trials the effect measure we used for inference was the relative risk of the outcome. Some of the included trials reported this measure, but other trials reported odds ratios. To convert the information from these studies into a relative risk framework, we used frequencies of observed outcomes and odds ratio effect estimates and corresponding confidence limits to estimate the design effect (DE) and intraclass correlation (ICC) for each study overall. We did this by estimating the variance of the odds ratio under the assumption of independence from the raw frequencies, extracting the variance of the odds ratio from the confidence limits adjusted for clustering, and then calculating the design effect as the ratio of the variance (clustered) over the variance (independence). We followed the guidelines from the Cochrane Handbook for Systematic Reviews of Interventions to reduce the size of each trial to its 'effective sample size' (Rao 1992). We then solved the corresponding ICC from the standard design effect equation (DE = 1+(m‐1)*ICC, where m is the average cluster size). We used this information to adjust the standard error of the relative risk estimate for clustering (McKenzie 2014). If the ICC or design effect was not reported, we assumed the ICC to be 0.1, as in a previous review of school‐based studies (Walsh 2015).
For Stephenson 2008 GBR, we estimated the DE from the unweighted effect measures and confidence intervals (CIs) reported. We then applied this estimated DE to the weighted estimates and CIs reported.
We managed trials with multiple publications as one study. One trial incorporated three interventions that were meta‐analysed separately (Duflo 2015 KEN). We entered eligible trials into Review Manager (RevMan) 5.3 (Review Manager 5.3). Where methods, data or analyses were unclear, we contacted the trial authors for clarification. We resolved any discrepancies and disagreements by discussion amongst the review author team. There were a few disagreements, generally as a result of differing interpretations of the texts or tables, and we resolved these by going back to the original or supporting papers, or back to the review authors to resolve.
We assessed the quality of evidence using the GRADE approach (GRADEpro 2014).
Assessment of risk of bias in included studies
We independently examined the components of each included trial for risk of bias using the Cochrane 'Risk of bias' assessment tool (Higgins 2011), and incorporated those items specifically related to cluster‐RCTs. This included information on random sequence generation, recruitment bias, baseline imbalance, allocation concealment, blinding (of participants, personnel, and the outcome assessors), incomplete outcome data, selective outcome reporting, and other sources of bias. We assessed the methodological components of the trials and classified them as being at either high, low, or unclear risk of bias. Again, we resolved any differences of opinion by discussion.
Measures of treatment effect
We reported all outcomes using risk ratios (RR) with 95% CIs.
Dealing with missing data
We aimed to conduct a complete‐case analysis so that we included all individuals with a recorded outcome in the analysis. If missing information was a problem, or we needed more details on reported measures, we sought further clarification from study investigators. All included trials reported at least one of the main outcome measures. However, one trial did not include the data in the final published paper and we were unable to get this data for inclusion in the review despite contacting the trial authors (Jemmott 2015 ZAF).
Assessment of heterogeneity
We assessed statistical heterogeneity between trials by inspecting the forest plots to detect overlapping CIs and by calculating the I² statistic using RevMan 5.3 (Higgins 2003). We also conducted a Chi2 test for heterogeneity at the P=0.1 level.
Assessment of reporting biases
When we reported the results of the included trials, we used the intention‐to‐treat results for the meta‐analysis. We did not construct funnel plots to look for evidence of publication bias because there were too few trials included in each analysis.
Data synthesis
Two review authors, AMJ and CL, analysed data using RevMan 5.3 (Review Manager 5.3). Given that the included trials used a variety of interventions, where it was appropriate to combine trials in a meta‐analysis we used a random‐effects model, since this is a conservative approach based on fewer assumptions than the fixed‐effect approach. We stratified the primary analysis by gender and performed a subgroup analysis by type of intervention (primarily curriculum‐based versus incentive‐based, and incentive‐based plus curriculum) where this was possible. Where trials reported incidence rates (for example, Ross 2007 TZA), we estimated the total number of infections reported and added this to the baseline infections to get an overall prevalence of infections at the endpoint of the trial. Where trials reported the inverse outcome we inverted the reported numbers. For Henderson 2007 GBR we estimated the number of respondents who were evaluated for using a condom at last sex and we then used this as the number of sexually active participants in the trial.
Subgroup analysis and investigation of heterogeneity
We conducted subgroup analyses for young women and young men separately. We also conducted subgroup analyses for type of intervention (for example, education‐based interventions and incentives to stay at school).
'Summary of findings' tables
We used a 'Summary of findings' table to interpret the results and to provide key information about the certainty of evidence for included trials in the comparison, magnitude of effect of the interventions examined, and included available data on the main outcomes. We used the GRADE profiler, GRADEpro 2014, to import data from RevMan 5.3 (Review Manager 5.3). We based the display on a recent trial of what review users prefer (Carrasco‐Labra 2015).
Results
Description of studies
Results of the search
The search identified 1183 unique references after we removed duplicates. After screening the abstracts, we excluded 1112 articles, and we assessed the remaining 71 full‐text articles formally for eligibility against the inclusion criteria (see Figure 2).
Included studies
We included eight cluster‐randomized trials in this review; 281 communities and 55,157 participants were enrolled. The cluster size ranged from 18 to 461 participants. One trial was conducted in Latin America (Chile, Cabezón 2005 CHL), two trials in Europe (England (Stephenson 2008 GBR), and Scotland (Henderson 2007 GBR)), and five in sub‐Saharan Africa (Malawi (Baird 2012 MWI), Zimbabwe (Cowan 2010 ZWE), Kenya (Duflo 2015 KEN), South Africa (Jemmott 2015 ZAF), and Tanzania (Ross 2007 TZA). Of those conducted in Africa, two were in rural areas (Cowan 2010 ZWE; Ross 2007 TZA), and three were in both rural and urban areas (Baird 2012 MWI; Duflo 2015 KEN; Jemmott 2015 ZAF).
All included trials were published between 2005 and 2015, with reported follow‐ups ranging from 18 months (Baird 2012 MWI), to seven years (Duflo 2015 KEN; Stephenson 2008 GBR).
Seven of the eight trials included a specific sexual and reproductive health educational component in the intervention and were based on a range of theoretical frameworks (Cabezón 2005 CHL; Cowan 2010 ZWE; Duflo 2015 KEN; Henderson 2007 GBR; Jemmott 2015 ZAF; Ross 2007 TZA; Stephenson 2008 GBR). These interventions focused specifically on changing knowledge, attitudes, behaviours, and norms related to sexual and reproductive health. The educational component ranged in intensity from three, one‐hour sessions in one school year (Stephenson 2008 GBR), to 36 sessions of 40 minutes over three school years (Ross 2007 TZA). Three trials incorporated trained peer educators into their intervention (Cowan 2010 ZWE; Ross 2007 TZA; Stephenson 2008 GBR), two incorporated nurse or health worker training to encourage 'youth friendly services' (Cowan 2010 ZWE; Ross 2007 TZA), and one included a parental training component (Cowan 2010 ZWE). Drama (including video dramas), games, or role play were incorporated into five of the intervention programmes (Cowan 2010 ZWE; Henderson 2007 GBR; Jemmott 2015 ZAF; Ross 2007 TZA; Stephenson 2008 GBR). Four of the seven trials reported some mention of gender roles (Cowan 2010 ZWE; Henderson 2007 GBR; Ross 2007 TZA; Stephenson 2008 GBR). Condoms were not given freely to participants in any of the trials, but were demonstrated to students in two trials (Henderson 2007 GBR; Stephenson 2008 GBR), and sold and marketed to young people in one trial (Ross 2007 TZA) (see Table 4: Description of educational interventions).
1. Description of educational interventions.
| Study (Country) | Target group | Target group education | Other components | Outcome measurement | |||
| Duration of intervention | Number of sessions | Delivered by | Content1 | ||||
| Cabezón 2005 CHL (Chile) | Girls (age 15 to 16 years) attending an all girls' high school | 1 year | 14 | Teachers | TeenSTAR programme focusing on abstinence, fertility awareness, and psychological and personal aspects of sexuality. | N/A | 3 years |
| Cowan 2010 ZWE (Zimbabwe) | Form 2 pupils (median age 15 years) | 3 years | Unclear 'both in‐and‐out of school' |
A school leaver (peer) who received training and supervision | A focus on developing knowledge and skills around sexual health issues. | A 22‐session community‐based programme for parents and community stakeholders aimed at improving communication with and community support of teenagers. A strand aimed at nurses and rural clinic workers aiming to improve accessibility of clinics to young people. |
4 years |
| Duflo 2015 KEN (Kenya) | 6th grade students (median age 13.5 years) | No details given | No details given | Teachers | Kenyan government's UNICEF/HIV/AIDS curriculum focusing on abstinence until marriage. | Health clubs to deliver HIV information outside the classroom. | 2 years 7 years |
| Henderson 2007 GBR (Great Britain) | 13‐15 year olds | 2 years | 20 | Teachers | Aimed to reduce unwanted pregnancies, reduce unsafe sex, and improve the quality of sexual relationships. | 5‐day training for teachers | 4.5 years |
| Jemmott 2015 ZAF (South Africa) | Grade 6 pupils (age range 9 to 18 years) |
6 days | 12 | Adult facilitators with 8 days of training | Mixed‐sex sessions involved games, brainstorming, role‐playing, group discussions, and comic workbooks with a series of characters and storylines. | Participants were given assignments to take home and to complete with parents. | 4.5 years |
| Ross 2007 TZA (Tanzania) | Primary school students (age range 14 to > 18 years) | 3 years | 36 | Teachers with peer assistants | Aimed to provide knowledge and skills to delay sexual debut, reduce sexual risk‐taking, and increase appropriate use of health services. | Health workers were trained for 1 week in the provision of youth‐friendly sexual and reproductive health services and supervised quarterly. Community mobilization activities including annual youth health weeks, interschool competitions and performances, and quarterly video shows. |
3 years |
| Stephenson 2008 GBR (Great Britain) | Year 9 pupils (age 13 to 14 years) | 4 months | 3 | Peers | Aimed at improving skills in sexual communication and condom use and knowledge of pregnancy, STIs, contraception, and local health services. | N/A | 7 years |
1None of the interventions included free distribution of condoms.
Abbreviations: N/A: not applicable ; STI: sexually transmitted infection.
One trial, and a trial within one of the studies, had no specific educational component, and used only a conditional or unconditional cash transfer as the intervention (Baird 2012 MWI), or two free school uniforms over a period of 18 months (Duflo 2015 KEN). These interventions were an attempt to influence the 'upstream factors' that affect reproductive health outcomes, such school attendance, poverty, and inequality (see Table 5: Description of incentive interventions).
2. Description of incentive‐based interventions.
| Study ID (Country) | Target group | Incentive‐based components | Outcome measurement | |||
| Type | Size | Conditional | Frequency | |||
| Baird 2012 MWI(Malawi) | Never married girls (age 13 to 22 years) |
Cash | USD 1 to 5 to the participant and USD 4 to 10 to her family |
Yes | Monthly | 1.5 years |
| Duflo 2015 KEN(Kenya) | 6th grade students (median age 13.5 years) | School uniform | — | No | At start of school year and 18 months later | 2 years 7 years |
Biological outcomes such as HIV, herpes simplex virus 2 (HSV2) (and other sexually transmitted infections (STIs)), were measured by dried blood spots and laboratory tests (Baird 2012 MWI; Cowan 2010 ZWE; Duflo 2015 KEN; Ross 2007 TZA), or blood sera and urine tests (Jemmott 2015 ZAF), and participants were provided treatment, counselling, and follow‐up as necessary. Current pregnancy was measured by urine sample (Ross 2007 TZA), or school reports with follow‐up home visits (Duflo 2015 KEN), whilst pregnancy at follow‐up was measured by linkage to health service records (Henderson 2007 GBR; Stephenson 2008 GBR), or school reports (Cabezón 2005 CHL; Duflo 2015 KEN), with follow‐up home visits (Duflo 2015 KEN).
Excluded studies
We excluded 63 studies (see the 'Characteristics of excluded studies' table); a further five trials are ongoing, or have been completed, but have not reported their results in peer‐reviewed publications (see the 'Characteristics of ongoing studies' table).
Risk of bias in included studies
We have summarized the 'Risk of bias' assessments in Figure 3.
3.
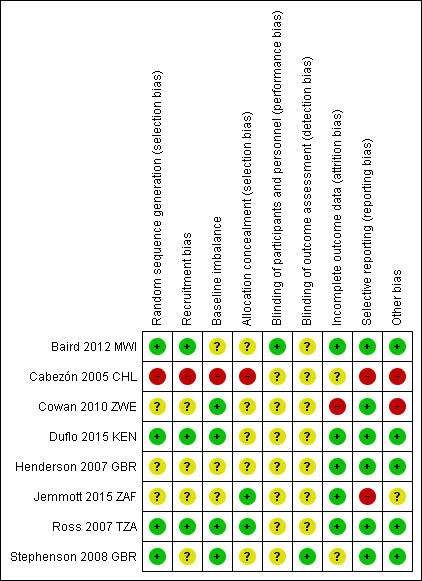
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.
Allocation
Random sequence generation
Baird 2012 MWI, Duflo 2015 KEN, Ross 2007 TZA, and Stephenson 2008 GBR utilized a computer‐generated random sequence and we deemed them to be at low risk of bias. We judged Cabezón 2005 CHL to be at high risk of bias, as classes were alternately selected by choosing a letter of the class from a bag, and the remaining trials were at unclear risk due to inadequate description of methods (Cowan 2010 ZWE; Henderson 2007 GBR; Jemmott 2015 ZAF).
Recruitment bias
We considered Baird 2012 MWI, Duflo 2015 KEN and Ross 2007 TZA to be at low risk of recruitment bias as individuals were recruited and baseline surveys were completed before the randomization of enumeration areas. We judged Cowan 2010 ZWE, Henderson 2007 GBR, Jemmott 2015 ZAF and Stephenson 2008 GBR to be at unclear risk of recruitment bias, as clusters were randomized first and then individuals were recruited from those clusters. Cabezón 2005 CHL only requested informed consent from parents of girls in the intervention group, and we therefore deemed it to be at high risk of recruitment bias.
Baseline imbalance
Cowan 2010 ZWE, Duflo 2015 KEN, Ross 2007 TZA, and Stephenson 2008 GBR all reported baseline measurements of outcomes between intervention and control participants and there were no baseline imbalances reported, therefore we judged them to be at low risk of bias. We deemed Baird 2012 MWI, Henderson 2007 GBR and Jemmott 2015 ZAF to be at unclear risk of bias for baseline imbalance. Baird 2012 MWI reported that, at baseline, schoolgirls in the intervention group were more likely to report unprotected sexual intercourse than those in the control group. Furthermore, the main outcome measures, HIV and HSV2, were not measured at baseline. Henderson 2007 GBR reported a slight gender imbalance at baseline and also an imbalance in those who reported sexual activity between the intervention and control groups. Jemmott 2015 ZAF reported 'some imbalance' at baseline, but provided no further details. We deemed Cabezón 2005 CHL to be at high risk of bias as there was baseline imbalance in the incidence of pregnancy between the intervention and control groups in the 1997 cohort, with no pregnancies in the intervention group and six in the control group.
Allocation concealment
We judged both Jemmott 2015 ZAF and Ross 2007 TZA to be at low risk of bias for allocation concealment as they reported concealing allocation up to the point of assignment. We judged Baird 2012 MWI, Cowan 2010 ZWE, Duflo 2015 KEN, Henderson 2007 GBR, and Stephenson 2008 GBR to be at an unclear risk of bias for allocation concealment, as the trial authors did not describe this in any detail. We judged one trial to be at a high risk of bias for allocation concealment (Cabezón 2005 CHL), as classes were chosen alternately and therefore assignment was unlikely to have been concealed adequately.
Blinding
Baird 2012 MWI and colleagues mentioned that they did not mask students to their assignment, and it became apparent that some participants had friends or acquaintances in other groups. However as it was not an educational intervention but rather a cash transfer incentive‐based programme there was no chance of 'contamination'. Furthermore, although participants were aware of whether they were receiving cash, how much, and whether it was conditional or not, they were not aware that the primary outcomes were related to HIV/STI prevalence. Baird 2012 MWI did not mask the investigators that conducted statistical analyses and did not describe blinding of the assessors who gathered samples. Overall, we deemed the trial as at an unclear risk of bias for performance and detection bias. Only Stephenson 2008 GBR described the process of blind matching of participants to routine National Health Service (NHS) data, and therefore we judged it to be at low risk of bias for the purposes of this Cochrane Review for detection bias, but unclear for performance bias. It is often difficult to blind participants and personnel in cluster‐RCTs within schools and communities, as a number of trial authors noted (Henderson 2007 GBR; Jemmott 2015 ZAF; Stephenson 2008 GBR). Trial authors did not report blinding of participants or personnel (Cabezón 2005 CHL; Cowan 2010 ZWE; Henderson 2007 GBR; Jemmott 2015 ZAF; Ross 2007 TZA), or said that it was not possible to blind teachers who attended a training course to deliver the intervention (Duflo 2015 KEN; Henderson 2007 GBR). Therefore, we judged these trials to be at an unclear risk of bias (Cabezón 2005 CHL; Cowan 2010 ZWE; Duflo 2015 KEN; Henderson 2007 GBR; Jemmott 2015 ZAF; Ross 2007 TZA).
Incomplete outcome data
We judged Baird 2012 MWI, Duflo 2015 KEN, Henderson 2007 GBR, Jemmott 2015 ZAF and Ross 2007 TZA to be at low risk of bias for this domain, as loss to follow‐up was similar in both intervention and control groups amongst those selected for follow‐up, and these trials performed intention‐to‐treat analyses. We deemed Henderson 2007 GBR to be at low risk of bias for objective outcomes, as follow‐up was equal across both trial arms (99.6% intervention, 99.5% control). A small level of attrition may have occurred due to women attending private clinics (less than 2% terminations) or having terminations in England or Wales (2.7%). There is no reason to expect this would differ across trial arms. However, we deemed Henderson 2007 GBR to be at high risk of bias for self‐reported outcomes due to a very low rate of response (41% control, 38% intervention). A systematic under‐representation of school leavers may have biased the result towards the null hypothesis. We deemed Ross 2007 TZA to be at low risk of bias due to similar attrition rates across control (72%) and intervention (74%) arms. Stephenson 2008 GBR conducted an intention‐to‐treat analysis. Missing data for objective measures meant that 28% of the control girls and 21% of the trial girls (P value 0.21) could not be matched with abortion data. It is possible that this may have biased the result towards the null hypothesis, but this risk appears to be small. Cabezón 2005 CHL reported that loss to follow‐up was 'similar' across intervention and control groups, but provided no data to support this, so we judged the trial to be at an unclear risk of bias. Cowan 2010 ZWE reported that interim survey results revealed a high rate of outmigration (46%) from the original cohort, so the design of the trial was altered and resulted in a cross‐sectional study. As a result, the proportion of the original cohort members included in the final survey was unlikely to have been more than 7%. This very high loss to follow‐up left all outcome measures and the study prone to a high risk of bias.
Selective reporting
We judged six trials to be at low risk of bias (Baird 2012 MWI; Cowan 2010 ZWE; Duflo 2015 KEN, Henderson 2007 GBR; Ross 2007 TZA; Stephenson 2008 GBR), as the trial authors reported all of the outcomes stated in their methods section. We judged Cabezón 2005 CHL to be at high risk of bias as the measurement of pregnancy rates was obtained from school records, and it is unlikely that all pregnancies were reported. Jemmott 2015 ZAF did not include complete details of the outcome data related to the biological outcomes measured (HIV, HSV2 and other STIs) in the published paper and so we judged it to be at high risk of bias.
Other potential sources of bias
We considered Baird 2012 MWI, Duflo 2015 KEN, Henderson 2007 GBR, Ross 2007 TZA, and Stephenson 2008 GBR to have a low risk of bias for this domain, as we found no other potential sources of bias. Jemmott 2015 ZAF did not describe their method of choosing schools that were eligible in sufficient detail, so we deemed the trial to be at an unclear risk of bias. We judged Cabezón 2005 CHL to be at high risk of bias. As abortion in Chile is illegal, it is unlikely that pregnancy and abortion would be reported fully to schools. Cowan 2010 ZWE reported that it became difficult to implement the programme in schools for political reasons, and that this coincided with a fall in school attendance for economic reasons and substantial outmigration from the country. Therefore we judged this trial as having a high risk of bias.
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings for the main comparison. Educational interventions versus no intervention.
| Educational programmes to reduce HIV, STIs, and pregnancy in adolescents | |||||
| Patient or population: adolescents Settings: schools and communities Intervention: sexual and reproductive health educational interventions delivered through schools Control: no intervention Outcomes: confirmed biologically by blood or urine test | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (trials) | Certainty of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Control | Sexual and reproductive health education | ||||
|
HIV prevalence Follow‐up: 18 months to 3 years |
10 per 1000 |
10 per 1000 (8 to 13) |
RR 1.03 (0.80 to 1.32) |
14,163 (3 trials) | ⊕⊕⊝⊝ low1,2,3,4 |
|
HSV2 prevalence Follow‐up: 18 months to 3 years |
110 per 1000 |
114 per 1000 (103 to 127) |
RR 1.04 (0.94 to 1.15) |
17,445 (3 trials) | ⊕⊕⊕⊝ moderate1,2,3,5 |
| Syphillis prevalence Follow‐up: 18 months to 3 years | 30 per 1000 |
24 per 1000 (14 to 42) |
RR 0.81 (0.47 to 1.39) |
6977 (1 trial) | ⊕⊕⊝⊝ low1,6,7 |
| Pregnant at end of trial Follow‐up: mean 3 years | 90 per 1000 |
89 per 1000 (77 to 104) |
RR 0.99 (0.85 to 1.16) |
8280 (3 trials) | ⊕⊕⊕⊝ moderate1,2,3,5 |
| The assumed risk is taken from the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Abbreviations: CI: confidence interval; HIV: human immunodeficiency virus; HSV2: herpes simplex virus‐2; RR: risk ratio; STI: sexually transmitted infection. | |||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | |||||
1No serious risk of bias: none of the trials described blinding of outcome assessors but this deficiency was not considered serious enough to downgrade. 2No serious inconsistency: none of these trials found a statistically significant effect. Statistical heterogeneity was low. 3Downgraded by 1 level for serious indirectness: these trials were conducted in schools in low‐income countries, and had extensive programmes of sexuality education including peers, teachers, and communities. However, the findings are not easily generalized to other programmes or settings. 4Downgraded by 1 level for imprecision: due to the low prevalence of HIV in these trials, both the trials and the meta‐analysis remain underpowered to allow confident exclusion of small but clinically important effects. 5No serious imprecision: the meta‐analysis is adequately powered to look for a 25% relative reduction, and the 95% CI is narrow and probably excludes clinically important effects. 6Downgraded by 1 level for serious indirectness: only a single trial from Tanzania evaluated this outcome. This does not exclude effects with different programmes in different settings. 7Downgraded by 1 level for serious imprecision: the 95% CI is wide and includes both clinically important effects and no effect.
Summary of findings 2. Incentive‐based programmes versus no intervention.
| School‐based incentive programmes to reduce HIV, STIs, and pregnancy in adolescents | |||||
|
Patient or population: adolescents
Settings: school and communities
Intervention: incentive‐based programmes delivered through schools which aim to reduce HIV and STI among adolescents
Control: no intervention Outcomes: confirmed biologically by blood or urine test | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Control | Incentive programmes | ||||
|
HIV prevalence Follow‐up: 18 months to 3 years |
10 per 1000 |
12 per 1000 (5 to 30) |
RR 1.23 (0.51 to 2.96) |
3805 (2 trials) | ⊕⊕⊝⊝ low1,2,3,4 |
| HSV2 prevalence Follow‐up: 18 months to 3 years | Not calculated | Not calculated | Not calculated | 7229 (2 trials) | ⊕⊝⊝⊝ very low1,3,5 |
| Syphillis prevalence Follow‐up: 18 months to 3 years | 30 per 1000 |
12 per 1000 (2 to 98) |
RR 0.41 (0.05 to 3.27) |
1291 (1 trial) | ⊕⊝⊝⊝ very low1,6,7 |
| Pregnant at end of trial Follow‐up: mean 3 years | 90 per 1000 |
68 per 1000 (52 to 89) |
RR 0.76 (0.58 to 0.99) |
4200 (2 trials) | ⊕⊕⊝⊝ low1,2,3,8 |
| The assumed risk is taken from the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Abbreviations: CI: confidence interval; HIV: human immunodeficiency virus; HSV2: herpes simplex virus‐2; RR: risk ratio; STI: sexually transmitted infection. | |||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | |||||
1No serious risk of bias: neither of these trials described blinding of outcome assessors. However, this deficiency was not serious enough to downgrade. 2No serious inconsistency: statistical heterogeneity was low. 3Downgraded by 1 level for serious indirectness: these two trials were conducted in Malawi and Kenya, and used very different interventions. Baird 2012 MWI gave a monthly cash transfer while Duflo 2015 KEN provided free school uniforms. It is difficult to extrapolate these result to different settings. 4Downgraded by 1 level for imprecision: due to the low prevalence of HIV in these trials, both the trials and the meta‐analysis remain underpowered to allow confident exclusion of small but clinically important effects. 5Downgraded by 2 levels for serious inconsistency: Baird 2012 MWI reported a statistically significant reduction in HSV2 in young women, whereas Duflo 2015 KEN found no effect in either males or females alone or combined into one mixed gender group. 6Downgraded by 1 level for serious indirectness: only a single trial assessed this outcome. The lack of effect does not exclude the possibility of effects in other settings. 7Downgraded by 2 levels for serious imprecision: the prevalence of syphilis was very low and consequently the trial is underpowered to confidently exclude small but clinically important effects. 8Downgraded by 1 level for serious imprecision: the 95% CI is wide and includes both important effects and negligible effects.
Summary of findings 3. Combined incentive‐based and educational interventions versus no intervention.
| School‐based combined incentive and educational programmes to reduce HIV, STIs, and pregnancy in adolescents | |||||
|
Patient or population: adolescents
Settings: school and communities
Intervention: incentives to promote school attendance plus sexual and reproductive health education
Control: no intervention Outcomes: confirmed biologically by blood or urine test | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Control | Incentive programmes | ||||
|
HIV prevalence Follow‐up: 18 months to 3 years |
10 per 1000 |
15 per 1000 (5 to 51) |
RR 1.53 (0.45 to 5.13) |
2506 (1 trial) | ⊕⊕⊝⊝ low1,2,3 |
| HSV2 prevalence Follow‐up: 18 months to 3 years | 110 per 1000 |
90 per 1000 (75 to 109) |
RR 0.82 (0.68 to 0.99) |
5899 (1 trial) | ⊕⊕⊝⊝ low1,2,3 |
| Syphillis prevalence Follow‐up: 18 months to 3 years | — | — | — | — (0 trials) | — |
| Pregnant at end of trial Follow‐up: mean 3 years | 90 per 1000 |
81 per 1000 (60 to 107) |
RR 0.90 (0.67 to 1.19) |
2782 (1 trial) | ⊕⊕⊝⊝ low1,2,3 |
| The assumed risk is taken from the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Abbreviations: CI: confidence interval; HIV: Human Immunodeficiency Virus; HSV2: herpes simplex virus‐2; RR: risk ratio; STI: sexually transmitted infection. | |||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | |||||
1No serious risk of bias: this trial did not describe blinding of outcome assessors. However, this deficiency was not serious enough to downgrade. 2Downgraded by 1 level for serious indirectness: only a single trial assessed this outcome and consequently the results are difficult to extrapolate to different settings or alternative incentives or educational programmes. 3Downgraded by 1 level for serious imprecision: the 95% CI is wide and includes both important effects and negligible or no effect.
Comparison 1: School‐based educational interventions versus no intervention
Six trials evaluated school‐based educational interventions and reported biologically confirmed outcomes (Cabezón 2005 CHL; Cowan 2010 ZWE; Duflo 2015 KEN; Henderson 2007 GBR; Ross 2007 TZA; Stephenson 2008 GBR). One additional trial reported that these outcomes were measured, but did not report the data (Jemmott 2015 ZAF). We have requested the data from the trial authors but have received no response. Duflo 2015 KEN was a four‐arm trial in which one trial arm received an educational intervention that we included in Comparison 1. This trial also included an incentive programme, the results of which we have reported in Comparison 2, as well as a combined incentive and educational programme that is reported in Comparison 3.
HIV incidence and prevalence
Only Ross 2007 TZA measured HIV incidence. The incidence of HIV was low with no statistically significant differences between intervention and control groups in young women (16/1448 intervention group versus 24/1492 control group), or young men (3/2076 intervention group versus 2/2024 control group).
Three trials measured HIV prevalence at the end of follow‐up (Cowan 2010 ZWE; Duflo 2015 KEN; Ross 2007 TZA). In these trials, there were no demonstrable effects on the prevalence of HIV in young women or young men, or both sexes combined (RR 1.03, 95% CI 0.80 to 1.32; three trials, 14,163 participants; Analysis 1.1). Although the effect estimate is close to no effect, the 95% confidence interval (CI) is wide, and larger studies may be necessary to fully exclude the possibility of small effects.
1.1. Analysis.

Comparison 1 Educational interventions versus no intervention, Outcome 1 HIV prevalence.
Note that although Ross 2007 TZA did not measure HIV prevalence, we were able to calculate prevalence based on the reported baseline prevalence and the incidence rate. This is based on the assumption that those who had HIV at baseline (or subsequently developed HIV during the study) were still living with HIV at the end of the study.
Other sexually transmitted infections
Three trials measured and reported HSV2 prevalence at the end of follow‐up. Across all three trials there were no demonstrable effects in either young women, young men, or both sexes combined (RR 1.04, 95% CI 0.94 to 1.15; three trials, 17,445 participants; Analysis 1.2).
1.2. Analysis.

Comparison 1 Educational interventions versus no intervention, Outcome 2 HSV2 prevalence.
Only Ross 2007 TZA measured and reported the prevalence of syphilis at the end of follow‐up. Although the prevalence was lower in the intervention group, the 95% CI is wide and includes the possibility of no effect for young women, young men, and both sexes combined (RR 0.81, 95% CI 0.47 to 1.39; one trial, 6977 participants; Analysis 1.3).
1.3. Analysis.
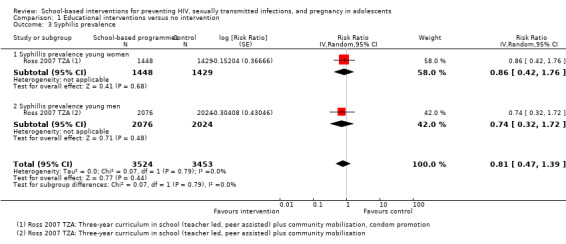
Comparison 1 Educational interventions versus no intervention, Outcome 3 Syphilis prevalence.
Pregnancy
Three trials measured short‐term pregnancy prevalence through either urine testing (Cowan 2010 ZWE; Ross 2007 TZA), or school reports and home visits (Duflo 2015 KEN) of female participants within the trial. There were no apparent effects in individual trials or all trials combined (RR 0.99, 95% CI 0.85 to 1.16; three trials, 8280 participants; Analysis 1.4).
1.4. Analysis.
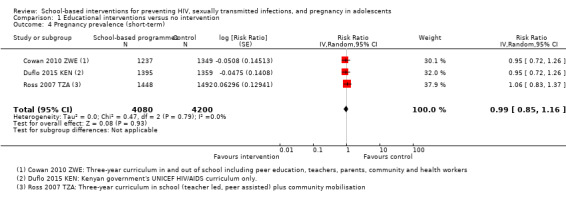
Comparison 1 Educational interventions versus no intervention, Outcome 4 Pregnancy prevalence (short‐term).
Four trials measured long‐term pregnancy prevalence. Two trials measured this outcome using health service data with biologically confirmed pregnancies (Henderson 2007 GBR; Stephenson 2008 GBR), while the other two trials relied on school reports and records (Cabezón 2005 CHL; Duflo 2015 KEN). There was an apparent reduction in long‐term pregnancy prevalence (RR 0.55, 95% CI 0.34 to 0.91; Analysis 1.5). Of these trials, only Cabezón 2005 CHL reported an effect that reached standard levels of statistical significance, and this effect was consistent for both cohorts, (RR 0.20, 95% CI 0.11 to 0.35 and RR 0.18, 95% CI 0.08 to 0.39). However, we deemed this trial to be at a high risk of bias and when this study was excluded there was no effect on long‐term pregnancy prevalence for the remaining trials (RR 0.93, 95% CI 0.81 to 1.08; three trials, 11, 612 participants).
1.5. Analysis.
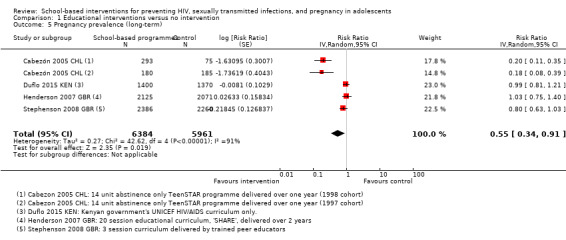
Comparison 1 Educational interventions versus no intervention, Outcome 5 Pregnancy prevalence (long‐term).
Self‐reported measures of behaviour change
Six trials also collected data on secondary measures of self‐reported behaviour change (Cowan 2010 ZWE; Duflo 2015 KEN; Henderson 2007 GBR; Jemmott 2015 ZAF; Ross 2007 TZA; Stephenson 2008 GBR). Across these trials there was no demonstrable effect on the number of young people reporting their first sexual encounter during the trial period (RR 0.96, 95% CI 0.91 to 1.01; four trials, 22,623 participants; Analysis 1.6). There was also no evidence of an effect on the proportion of young people using a condom during their first sexual encounter (RR 1.00, 95% CI 0.98 to 1.01; two trials, 8015 participants; Analysis 1.7), or using a condom during their most recent sexual encounter (RR 1.00, 95% CI 0.97 to 1.03; six trials, 18,795 participants; Analysis 1.8). Although the exact outcome measurement varied between trials, statistical heterogeneity between trials was low.
1.6. Analysis.
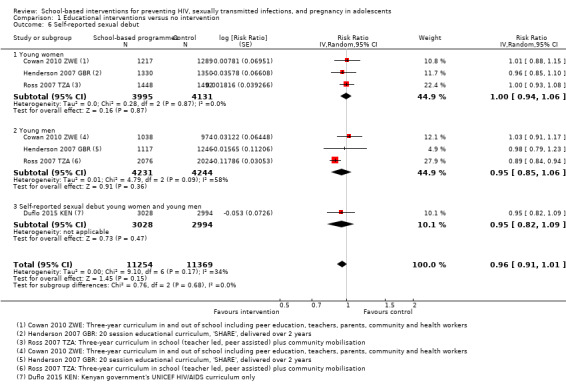
Comparison 1 Educational interventions versus no intervention, Outcome 6 Self‐reported sexual debut.
1.7. Analysis.
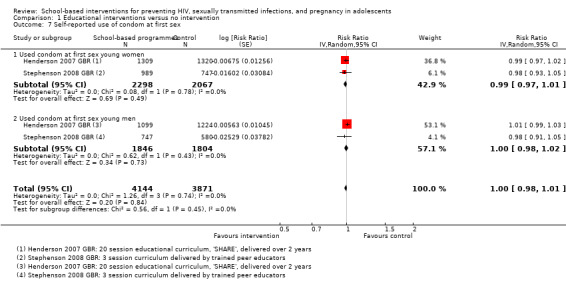
Comparison 1 Educational interventions versus no intervention, Outcome 7 Self‐reported use of condom at first sex.
1.8. Analysis.

Comparison 1 Educational interventions versus no intervention, Outcome 8 Self‐reported use of condom at last sex.
Comparison 2: Incentive programmes versus no intervention
Two trials evaluated incentive‐based programmes to encourage school attendance (Baird 2012 MWI; Duflo 2015 KEN).
HIV prevalence
There were no demonstrable effects on the prevalence of HIV in young women or men in either trial, or in the trials combined (RR 1.23, 95% CI 0.51 to 2.96; two trials, 3805 participants; Analysis 2.1). However, the prevalence of HIV was low, and consequently the trials are underpowered to exclude clinically important effects with confidence.
2.1. Analysis.
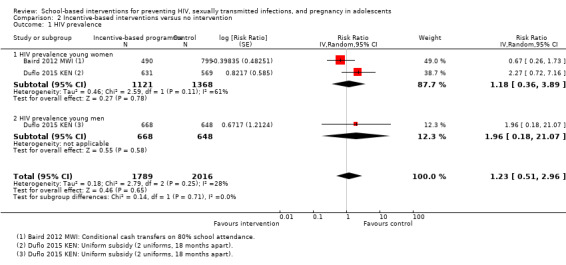
Comparison 2 Incentive‐based interventions versus no intervention, Outcome 1 HIV prevalence.
Baird 2012 MWI measured HIV prevalence amongst girls attending school, and those who had dropped out. However, the trial was not powered to detect effects in school dropouts, and because our analysis was aimed primarily at school‐based interventions, we have only included the schoolgirl cohort in all of our analyses. In the published paper Baird reported that the effect of HIV prevalence was statistically significant (HIV tests were positive in 7/490 intervention schoolgirls and 17/799 control schoolgirls at follow‐up).
Other sexually transmitted diseases
Both trials reported HSV2 prevalence at the end of the trial. Of these, Baird 2012 MWI reported a reduction in HSV2 prevalence in young women (RR 0.30, 95% CI 0.11 to 0.85), based on 5/488 intervention schoolgirls testing positive compared to 27/796 control schoolgirls. However, it is important to note that Baird did not measure, or report HSV2 prevalence at baseline. No effect was apparent in young women or young men in the other trial (Duflo 2015 KEN), or when we combined the two trials (RR 0.98, 95% CI 0.72 to 1.36; two trials, 7229 participants; Analysis 2.2).
2.2. Analysis.
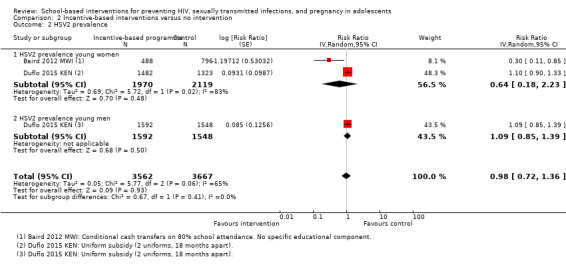
Comparison 2 Incentive‐based interventions versus no intervention, Outcome 2 HSV2 prevalence.
Only Baird 2012 MWI assessed the prevalence of syphilis, and the prevalence was too low to demonstrate effects (1/491 intervention schoolgirls versus 4/800 control schoolgirls; Analysis 2.3).
2.3. Analysis.
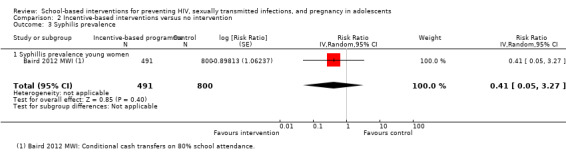
Comparison 2 Incentive‐based interventions versus no intervention, Outcome 3 Syphilis prevalence.
Pregnancy
Both trials measured short‐term pregnancy prevalence. Overall, pregnancy was reduced by around a quarter in those who received incentives (116/2014 intervention versus 151/2186 control; RR 0.76, 95% CI 0.58 to 0.99; two trials, 4200 participants; Analysis 2.4). The effect size was consistent across trials, but with wide CIs which include no effect.
2.4. Analysis.
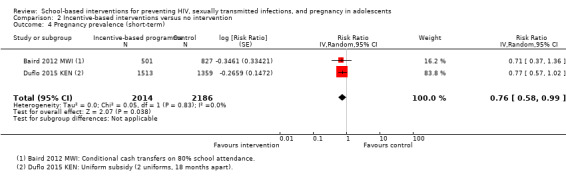
Comparison 2 Incentive‐based interventions versus no intervention, Outcome 4 Pregnancy prevalence (short‐term).
Only Duflo 2015 KEN measured the incidence of pregnancy throughout the long‐term follow‐up period up to seven years, and did not demonstrate an effect (604/1521 intervention versus 583/1370 control; RR 0.89, 95% CI 0.73 to 1.08; one trial, 2891 participants; Analysis 2.5).
2.5. Analysis.
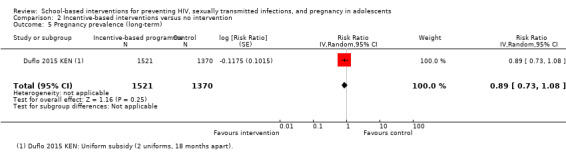
Comparison 2 Incentive‐based interventions versus no intervention, Outcome 5 Pregnancy prevalence (long‐term).
Self‐reported measures of behaviour change
Both trials collected data on secondary measures of self‐reported behaviour change. There was a reduction in the proportion of young people reporting their first sexual encounter (sexual debut) during the trial period (RR 0.83, 95% CI 0.73 to 0.95; two trials, 7177 participants; Analysis 2.6). Only Duflo 2015 KEN, reported on the proportion using a condom during their most recent sexual encounter and demonstrated no reduction (RR 0.98, 95% CI 0.85 to 1.12; one trial, 4265 participants, Analysis 2.7).
2.6. Analysis.
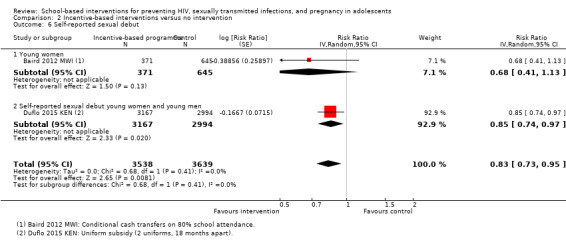
Comparison 2 Incentive‐based interventions versus no intervention, Outcome 6 Self‐reported sexual debut.
2.7. Analysis.
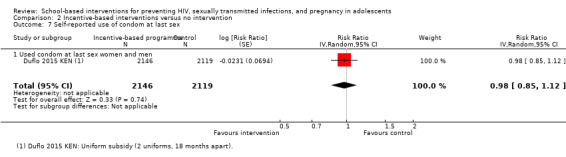
Comparison 2 Incentive‐based interventions versus no intervention, Outcome 7 Self‐reported use of condom at last sex.
Comparison 3: Combined incentive and educational programmes
Duflo 2015 KEN was a four‐arm trial that also included a trial arm in which participants received both free school uniforms and a programme of sexual and reproductive health education.
HIV prevalence
There were no demonstrable effects on HIV prevalence (RR 1.53, 95% CI 0.45 to 5.13; 1 trial, 2506 participants; Analysis 3.1).
3.1. Analysis.

Comparison 3 Combined incentive‐based and educational interventions versus no intervention, Outcome 1 HIV prevalence.
Other sexually transmitted diseases
The prevalence of herpes simplex virus infection was lower in those receiving an incentive and educational programme combined compared to controls (RR 0.82, 95% CI 0.68 to 0.99; one trial, 5899 participants, Analysis 3.2), and this reduction was mainly in young women (RR 0.76, 95% CI 0.62 to 0.93).
3.2. Analysis.

Comparison 3 Combined incentive‐based and educational interventions versus no intervention, Outcome 2 HSV2 prevalence.
Pregnancy
No effect was demonstrated either on the proportion of young women pregnant in the short‐term (RR 0.90, 95% CI 0.67 to 1.19; one trial, 2782 participants; Analysis 3.3), or the incidence of pregnancy at the long‐term follow up (RR 0.90, 95% CI 0.73 to 1.12; one trial, 2801 participants; Analysis 3.4).
3.3. Analysis.
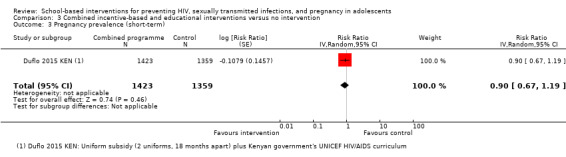
Comparison 3 Combined incentive‐based and educational interventions versus no intervention, Outcome 3 Pregnancy prevalence (short‐term).
3.4. Analysis.
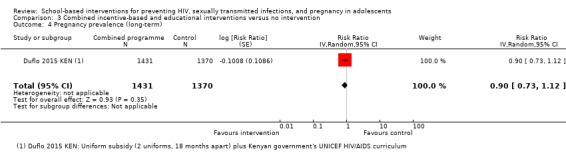
Comparison 3 Combined incentive‐based and educational interventions versus no intervention, Outcome 4 Pregnancy prevalence (long‐term).
Self‐reported measures of behaviour change
The proportion of young people reporting their sexual debut during the trial was lower in those receiving the intervention (RR 0.84, 95% CI 0.73 to 0.97; one trial, 6102 participants; Analysis 3.5), but there was no effect demonstrated on the proportion of adolescents using a condom during their most recent sexual encounter (RR 1.02, 95% CI 0.89 to 1.17; one trial, 4193 participants; Analysis 3.6).
3.5. Analysis.
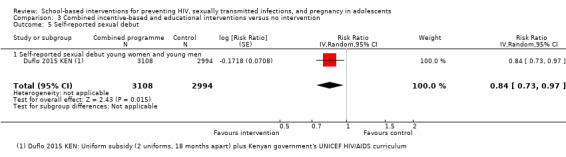
Comparison 3 Combined incentive‐based and educational interventions versus no intervention, Outcome 5 Self‐reported sexual debut.
3.6. Analysis.
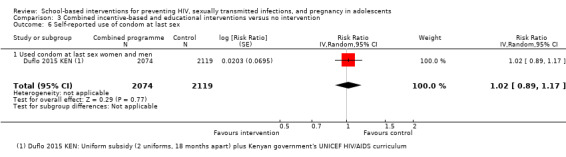
Comparison 3 Combined incentive‐based and educational interventions versus no intervention, Outcome 6 Self‐reported use of condom at last sex.
Discussion
Summary of main results
Sexual and reproductive health educational programmes
In these trials, the educational programmes evaluated had no demonstrable effect on the prevalence of HIV (low certainty evidence), or other sexually transmitted infections (Herpes Simplex virus prevalence: moderate certainty evidence; Syphilis prevalence: low certainty evidence). There was also no apparent effect on the number of young women who were pregnant at the end of the trial (moderate certainty evidence).
Material or monetary incentive‐based programmes to promote school attendance
In these two trials, the incentives used had no demonstrable effect on the prevalence of HIV (low certainty evidence). Compared to controls, the prevalence of Herpes Simplex virus infection was lower in young women receiving a monthly cash incentive to stay in school, but not in young people given free school uniforms (very low certainty evidence). Only one trial evaluated the effects on syphilis and the prevalence was too low to confidently detect or exclude effects (very low certainty evidence). However, the number of young women who were pregnant at the end of the trial was lower among those who received incentives (low certainty evidence).
Combined material or monetary incentive‐based and educational programmes
One trial used a combined approach; this showed there was no demonstrable effect on the prevalence of HIV (low certainty evidence). Compared to controls, the prevalence of HSV infection was lower for those receiving free school uniforms to stay in school and an educational programme (low certainty evidence). The provision of a combined programme had no demonstrable effect on the number of young women who were pregnant at both short‐ and long‐term follow‐up (low certainty evidence).
Overall completeness and applicability of evidence
The trials included in this review evaluated educational programmes that incorporated many of the specific characteristics that have previously been recommended for well‐designed adolescent sexual and reproductive health interventions (Kirby 2006). However, despite this, they failed to demonstrate any reduction in the prevalence of STIs or adolescent pregnancy. It is only possible to theorize about the potential reasons for this, but three factors may be important.
Firstly, the trials could simply be underpowered for the detection of small but clinically important effects. This could certainly be true for the lack of effect on HIV. Even in geographical settings where HIV is more common than elsewhere, the incidence during adolescence is relatively low and very large trials would be required to exclude small effects with confidence (see Table 6). For more common outcomes though, such as HSV2 and pregnancy, the trials are adequately powered to detect effects, and the effect estimate is close to zero with narrow 95% confidence intervals (CIs). Importantly, if the interventions are not reducing these more common outcomes, they are unlikely to be having an impact on HIV.
3. Optimal information size calculations.
| Outcome | Assumed risk1 | Clinically important relative reduction | Sample size required2,3 |
| HIV prevalence | 10/1000 (1%) | 25% | 43,576 |
| HIV prevalence | 10/1000 (1%) | 50% | 9344 |
| HSV2 prevalence | 110/1000 (11%) | 25% | 3606 |
| Syphilis prevalence | 30/1000 (3%) | 25% | 14,264 |
| Pregnancy | 90/1000 (9%) | 25% | 4494 |
1The assumed risk is the median control group risk from the included studies. 2We based all calculations on 2‐sided tests, with a ratio of 1:1, power of 0.8, and confidence level of 0.05. 3We performed all calculations using www.sealedenvelope.com/power/binary‐superiority.
Secondly, despite the effort that went in to designing these educational programmes, they may still have failed to address some areas critical to effecting change. For instance, it is unclear to what extent the programmes incorporated discussion of exploitation or violence, or whether the messages were adapted appropriately for both the male and female students. Furthermore, none gave condoms freely to participants. It is therefore not possible to say that educational programmes would never work, only that these programmes did not, despite extensive efforts to develop multifaceted approaches through formative consultation with young people themselves (Henderson 2007 GBR; Ross 2007 TZA; Stephenson 2008 GBR).
The third possible explanation is that educational programmes alone do not address the wider structural issues that influence sexual health outcomes, sexual behaviour and risk taking; the availability and affordability of schools and health services, contraceptive choice and condoms, poverty, and cultural gender norms. Indeed it is this third factor which has led some to develop and promote interventions which prioritize school attendance and educational achievement.
This review included two trials that promoted school attendance through cash transfers, and free school uniforms respectively (Baird 2012 MWI; Duflo 2015 KEN). Further trials are currently ongoing (Pettifor 2016), or have not yet reported their results (NCT01187979; NCT01233531). The two early trials have had some positive, but conflicting findings, which should temper enthusiasm for this approach until the results of these additional trials have been published. Baird 2012 MWI found a reduction in HSV2 prevalence in girls given monthly cash incentives, while Duflo 2015 KEN did not reproduce this effect with free school uniforms. Similarly, while both cash incentives and free school uniforms were associated with a reduction in adolescent pregnancies, a third trial arm in Duflo 2015 KEN, which received both free school uniforms and an educational intervention, did not have a lower incidence of pregnancy. This is counter‐intuitive and further trials will help us to understand why.
Quality of the evidence
We assessed the quality or certainty in the evidence using the GRADE approach, which we have presented in the 'Summary of findings' tables (Table 1; Table 2).
For educational programmes we have moderate certainty that these programmes do not have an impact on either STIs or pregnancy. As described above, we downgraded the certainty for indirectness, as we are unable to extrapolate the findings of these few trials in specific settings confidently to all educational programmes everywhere. For the finding of no effect on HIV prevalence we further downgraded the evidence to low certainty under 'imprecision', as the prevalence of HIV was generally low in these trials and very large trials would be needed to exclude fully the possibility of small but clinically important effects.
For incentive‐based programmes, our level of certainty is low or very low due to the limited number of trials available (which affects both precision and directness) and the inconsistencies in the findings of the two available trials. There are currently several more trials of incentive‐based programmes underway, and we would expect that certainty about the presence or absence of effects will be increased in future editions of this review.
Potential biases in the review process
We used only peer‐reviewed trials in this review. It is unlikely that we missed papers that were unpublished that included biological outcomes, as this is a relatively new innovation in adolescent sexual and reproductive health research and it is likely that they would be published. Most intervention studies of this kind use self‐reported measures only.
The missing data from Jemmott 2015 ZAF are unlikely to have affected the overall findings, however, the findings on pregnancy at long‐term follow‐up were sensitive to the exclusion of Cabezón 2005 CHL. The potential for a high risk of bias in this study suggests that the study authors' conclusions should be treated with caution.
All eight of the cluster‐randomized controlled trials (cluster‐RCTs) reported that they took account of the cluster randomization. However, not all of them included the intraclass correlation (ICC) or design effect. Therefore, we recalculated the standard errors reported and use these in our meta‐analyses.
We have only included RCTs. Before‐and‐after studies are often used for public health interventions, but when we deemed that there were enough RCTs for this analysis, we decided that the inclusion of studies with less robust designs was unlikely to add anything further.
Agreements and disagreements with other studies or reviews
The conclusions of this Cochrane Review are consistent with previous published reviews of curriculum‐based educational programmes. The Health Technology Assessment Centre’s systematic review of school‐based interventions to prevent STIs including HIV included RCTs and assessed sexual risk behaviour outcomes (Shepherd 2010). The review authors identified few statistically significant effects on behaviour in the included studies. Where there were significant effects, they often only applied to a subgroup of the participants (boys only or girls only, or only the subgroup who became sexually active during the study period). This led them to conclude that “school‐based behavioural interventions for the prevention of STIs in young people can bring about improvements in knowledge and increased self‐efficacy, but the interventions did not significantly influence sexual risk‐taking behaviour or infection rates”. The recent suggestion that the UK Govenment's Teenage Pregnancy Strategy which incorporated school‐based programmes and health service interventions has been effective in reducing adolescent pregnancy (Hadley 2016) is promising but needs further evidence from controlled studies, preferably with randomized designs, as temporal trends can confuse and mislead.
There now seems to be consensus that in sub‐Saharan Africa few curriculum‐based educational programmes have been shown to be effective, and many of the evaluations have a high risk of bias (Michielsen 2010; Paul 2008). The most recent systematic review of programmes for adolescents and young people based in schools and other settings, found 28 experimental studies, only 11 of which were RCTs, and many of which were judged to be of sub optimal quality (Michielsen 2010). This paucity of strong evidence regarding the effects of educational programmes in sub‐Saharan Africa on adolescent HIV, STI and pregnancy prevention is also consistent with the assessments of earlier reviews (Flisher 2008; Gallant 2004; Kirby 2007; Magnussen 2004; Michielsen 2010; Paul 2008), in that programmes that aimed at delaying sexual debut among adolescents and young people have been shown to have limited effectiveness. Our current knowledge of what works remains limited, especially for marginalized adolescents (Chandra‐Mouli 2015).
The finding that incentive‐based programmes that encourage school attendance may reduce pregnancy in adolescents confirms the results of a previous study which suggests that leaving school early was associated with early pregnancy (Imamura 2007).
Authors' conclusions
Implications for practice.
There is a continued need to provide health services that cater for the sexual and reproductive health needs of adolescents by providing a range of contraceptive choices and condoms and to include them in decision‐making around services that can most fully meet their needs. Schools may be a good place in which to provide sexual and reproductive health services, but there is little evidence that curriculum‐based educational programmes alone, as they are currently configured and without the provision of contraception and condoms, are effective in reducing risk behaviours for adolescents and improving their health outcomes. It is likely that the wider role of health service provision and availability, gender norms, sexual exploitation and intimate partner violence, poverty and inequality also need to be acknowledged and addressed and that programmes for girls and boys might need to be configured differently.
Incentive‐based interventions that focus on keeping young people in secondary school have had some promising — though conflicting — early results, and further trials are ongoing to investigate this.
Implications for research.
Some of the trials included in this review were large, complex, well‐designed, and well‐conducted trials whose participants were followed up on a medium‐ to long‐term basis. The cost of these trials has been significant, yet they have not been able to show effectiveness for educational curriculum‐based interventions on biologically measured adolescent sexual and reproductive health outcomes. The implications for research are significant. The only trial that showed promise in reducing the prevalence of herpes simplex virus 2 (HSV2) was the conditional cash transfer intervention (Baird 2012 MWI); while the only two trial interventions that reduced pregnancy were the incentive‐based interventions to maintain school attendance (Baird 2012 MWI; Duflo 2015 KEN).
Increasingly it is being realized that structural determinants of health, such as the provision of continuing secondary education or training, are important issues to address for improving adolescent sexual and reproductive outcomes, especially for girls. We need to begin to acknowledge this fully in our work when designing high quality interventions.
History
Protocol first published: Issue 1, 2007 Review first published: Issue 11, 2016
| Date | Event | Description |
|---|---|---|
| 24 August 2011 | Feedback has been incorporated | Feedback from peer‐review incorporated into the protocol |
| 29 November 2010 | Amended | Revised the protocol |
| 12 November 2008 | Amended | Converted to RevMan 5 and re‐published without new citation. |
Acknowledgements
The University of York, UK; the Cochrane Infectious Diseases Group at the Liverpool School of Tropical Medicine, UK; the South African Medical Research Council; and Stellenbosch University). David Sinclair was supported by the Effective Health Care Research Consortium. This Consortium and the editorial base of the Cochrane Infectious Diseases Group is funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242). The views expressed in this review do not necessarily reflect UK government policy.
Professor Alan Flisher, who sadly died in 2010, had the original idea for the review and registered the original title. Dr Wanjirũ Mũkoma worked on the initial protocol for the review with Professor Flisher. Following a presentation and discussion at the South African Cochrane Centre, Professor Jimmy Volmink suggested changing the review to include only studies with biological endpoints. Joy Oliver at the South African Cochrane Centre designed the search strategy and conducted all searches and the updates of searches. Hasci Horvath from the former HIV/AIDS Collaborative review group at University of California, San Francisco provided support up to 2015 and Professor Paul Garner and Anne‐Marie Stephani from the Cochrane Infectious Diseases Group at the Liverpool School of Tropical Medicine, provided support from 1 February 2015. We acknowledge and thank all of these people who have supported this review.
Appendices
Appendix 1. PubMed search strategy
| Search | Query |
| #10 | Search (((#7 AND #8))) AND (“"[Date ‐ Publication] : ""[Date ‐ Publication]) |
| #9 | Search (#7 AND #8) |
| #8 | Search (youth[tiab] OR youths[tiab] OR youngster[tiab] OR teenager[tiab] OR teenagers[tiab] OR teen[tiab] OR teens[tiab] OR adolescent[mh] OR adolescent[tiab] OR adolescents[tiab] OR adolescence[tiab] OR child[mh] OR child[tiab] OR children[tiab] OR young person*[tiab] OR young people[tiab]) |
| #7 | Search (#3 AND #4 AND #5 AND #6) |
| #6 | Search (randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized [tiab] OR placebo [tiab] OR "clinical trials as topic"[mesh: noexp] OR randomly [tiab] OR trial [ti]) NOT (animals [mh] NOT humans [mh]) |
| #5 | Search (Schools[mh] OR schools[tiab] OR school[tiab] OR community[tiab] OR communities[tiab] OR community networks[mh] OR teacher[tiab] OR teachers[tiab] OR classroom[tiab] OR classrooms[tiab] OR educator[tiab] OR educators[tiab] OR peer[tiab] OR peers[tiab]) |
| #4 | Search (sexual behavior[mh] OR sexual behavior[tiab] OR sexual behaviour[tiab] OR sex behavior[tiab] OR sex behaviour[tiab] OR sex education[mh] OR sex education[tiab] OR sex counseling[mh] OR sex counseling[tiab] OR sex counselling[tiab] OR health education/methods[mh] OR health education[tiab] OR health knowledge, attitudes, practice[mh])) |
| #3 | Search (#1 OR #2) |
| #2 | Search (sexually transmitted diseases[mh] OR sexually transmitted disease*[tiab] OR sexually transmissible disease*[tiab] OR sexually transmitted infection*[tiab] OR sexually transmissible infection*[tiab] OR sexually transmitted infectious disease*[tiab] OR sexually transmissible infectious disease*[tiab] OR sexually transmitted disorder*[tiab] OR sexually transmissible disorder*[tiab] OR STI[tiab] OR STIs[tiab] OR STD[tiab] OR STDs[tiab]) |
| #1 | Search (HIV Infections[MeSH] OR HIV[MeSH] OR hiv[tiab] OR hiv‐1*[tiab] OR hiv‐2*[tiab] OR hiv1[tiab] OR hiv2[tiab] OR hiv infect*[tiab] OR human immunodeficiency virus[tiab] OR human immunedeficiency virus[tiab] OR human immuno‐deficiency virus[tiab] OR human immune‐deficiency virus[tiab] OR ((human immun*[tiab]) AND (deficiency virus[tiab])) OR acquired immunodeficiency syndrome[tiab] OR acquired immunedeficiency syndrome[tiab] OR acquired immuno‐deficiency syndrome[tiab] OR acquired immune‐deficiency syndrome[tiab] OR ((acquired immun*[tiab]) AND (deficiency syndrome[tiab])) OR "sexually transmitted diseases, Viral"[MeSH:NoExp]) |
Appendix 2. Embase search strategy
| No | Query | Results |
| #15 | #12 AND #13 AND [27‐3‐2015]/sd NOT [7‐4‐2016]/sd | 81 |
| #14 | #12 AND #13 | 912 |
| #13 | 'adolescent'/de OR adolescent:ab,ti OR adolescents:ab,ti OR 'adolescence'/de OR adolescence:ab,ti OR 'youth'/de OR youth:ab,ti OR youths:ab,ti OR 'teenager'/de OR teenager:ab,ti OR teenagers:ab,ti OR teens:ab,ti OR 'child'/de OR child:ab,ti OR 'children'/de OR children:ab,ti OR 'minor'/de OR minor:ab,ti OR 'minors'/de OR minors:ab,ti OR 'student'/de OR student:ab,ti OR 'students'/de OR students:ab,ti OR 'young person':ab,ti OR 'young persons':ab,ti OR 'young people':ab,ti | 3103461 |
| #12 | #3 AND #9 AND #10 AND #11 | 1691 |
| #11 | 'school'/de OR school:ab,ti OR 'schools'/de OR schools:ab,ti OR 'community'/de OR community:ab,ti OR communities:ab,ti OR 'teacher'/de OR teacher:ab,ti OR teachers:ab,ti OR classroom:ab,ti OR classrooms:ab,ti OR educator:ab,ti OR educators:ab,ti OR peer:ab,ti OR peers:ab,ti | 808453 |
| #10 | 'sexual behavior'/de OR 'sexual behavior':ab,ti OR 'sexual behaviour'/de OR 'sexual behaviour':ab,ti OR 'sex behavior'/de OR 'sex behavior':ab,ti OR 'sex':ab,ti OR 'sex'/de OR (sex:ab,ti AND behaviour:ab,ti) OR 'sex education'/de OR 'sex education':ab,ti OR 'sex counseling'/de OR 'sex counseling':ab,ti OR 'sex counselling':ab,ti OR 'sexual health'/de OR 'sexual health':ab,ti OR 'sexual education'/de OR 'sexual education':ab,ti OR 'school health education'/de OR 'school health education':ab,ti OR 'attitudes to health':ab,ti OR 'health knowledge, attitudes, practice'/de OR 'health knowledge, attitudes, practice':ab,ti | 662610 |
| #9 | #4 NOT #8 | 1598799 |
| #8 | #5 NOT #7 | 5322811 |
| #7 | #5 AND #6 | 1455470 |
| #6 | 'human'/de OR 'normal human'/de OR 'human cell'/de | 17012217 |
| #5 | 'animal'/de OR 'animal experiment'/de OR 'invertebrate'/de OR 'animal tissue'/de OR 'animal cell'/de OR 'nonhuman'/de | 6778281 |
| #4 | 'randomized controlled trial'/de OR 'randomized controlled trial' OR random*:ab,ti OR trial:ti OR allocat*:ab,ti OR factorial*:ab,ti OR placebo*:ab,ti OR assign*:ab,ti OR volunteer*:ab,ti OR 'crossover procedure'/de OR 'crossover procedure' OR 'double‐blind procedure'/de OR 'double‐blind procedure' OR 'single‐blind procedure'/de OR 'single‐blind procedure' OR (doubl* NEAR/3 blind*):ab,ti OR (singl*:ab,ti AND blind*:ab,ti) OR crossover*:ab,ti OR cross+over*:ab,ti OR (cross NEXT/1 over*):ab,ti | 1792524 |
| #3 | #1 OR #2 | 517510 |
| #2 | 'sexually transmitted diseases'/exp OR 'sexually transmitted diseases':ab,ti OR 'sexually transmitted diseases, bacterial'/exp OR 'sexually transmitted diseases, viral'/exp OR (sexually:ab,ti AND transmitted:ab,ti AND disease*:ab,ti) OR (sexually:ab,ti AND transmissible:ab,ti AND disease*:ab,ti) OR (sexually:ab,ti AND transmitted:ab,ti AND infection*:ab,ti) OR (sexually:ab,ti AND transmissible:ab,ti AND infection*:ab,ti) OR (sexually:ab,ti AND transmitted:ab,ti AND infectious:ab,ti AND disease*:ab,ti) OR (sexually:ab,ti AND transmissible:ab,ti AND infectious:ab,ti AND disease*:ab,ti) OR (sexually:ab,ti AND transmitted:ab,ti AND disorder*:ab,ti) OR (sexually:ab,ti AND transmissible:ab,ti AND disorder*:ab,ti) OR sti:ab,ti OR std:ab,ti | 105559 |
| #1 | 'human immunodeficiency virus infection'/exp OR 'human immunodeficiency virus infection':ab,ti OR 'human immunodeficiency virus'/exp OR 'human immunodeficiency virus':ab,ti OR 'human immunedeficiency virus':ab,ti OR 'human immune‐deficiency virus':ab,ti OR 'human immuno‐deficiency virus':ab,ti OR hiv:ab,ti OR 'hiv+1':ab,ti OR 'hiv+2':ab,ti OR 'acquired immunodeficiency syndrome':ab,ti OR 'acquired immuno+deficiency syndrome':ab,ti OR 'acquired immune+deficiency syndrome':ab,ti OR 'acquired immunedeficiency syndrome':ab,ti | 440747 |
Appendix 3. CENTRAL search strategy
| ID | Search |
| #1 | MeSH descriptor: [HIV Infections] explode all trees |
| #2 | MeSH descriptor: [HIV] explode all trees |
| #3 | hiv or hiv‐1* or hiv‐2* or hiv1 or hiv2 or HIV INFECT* or HUMAN IMMUNODEFICIENCY VIRUS or HUMAN IMMUNEDEFICIENCY VIRUS or HUMAN IMMUNE‐DEFICIENCY VIRUS or HUMAN IMMUNO‐DEFICIENCY VIRUS or HUMAN IMMUN* DEFICIENCY VIRUS or ACQUIRED IMMUNODEFICIENCY SYNDROME or ACQUIRED IMMUNEDEFICIENCY SYNDROME or ACQUIRED IMMUNO‐DEFICIENCY SYNDROME or ACQUIRED IMMUNE‐DEFICIENCY SYNDROME or ACQUIRED IMMUN* DEFICIENCY SYNDROME |
| #4 | MeSH descriptor: [Lymphoma, AIDS‐Related] this term only |
| #5 | MeSH descriptor: [Sexually Transmitted Diseases, Viral] this term only |
| #6 | #1 or #2 or #3 or #4 or #5 |
| #7 | sexually transmitted disease*:ti,ab,kw or sexually transmissible disease*:ti,ab,kw or sexually transmitted infection*:ti,ab,kw or sexually transmissible infection*:ti,ab,kw or sexually transmitted infectious disease*:ti,ab,kw or sexually transmissible infectious disease*:ti,ab,kw or sexually transmitted disorder*:ti,ab,kw or sexually transmissible disorder*:ti,ab,kw or STI:ti,ab,kw or STIs:ti,ab,kw or STD:ti,ab,kw or STDs:ti,ab,kw |
| #8 | MeSH descriptor: [Sexually Transmitted Diseases] explode all trees |
| #9 | #7 or #8 |
| #10 | #6 or #9 |
| #11 | MeSH descriptor: [Sexual Behavior] explode all trees |
| #12 | MeSH descriptor: [Sex Education] this term only |
| #13 | MeSH descriptor: [Sex Counseling] this term only |
| #14 | MeSH descriptor: [Health Education] this term only |
| #15 | MeSH descriptor: [Attitude to Health] 1 tree(s) exploded |
| #16 | sexual behavior:ti,ab,kw or sexual behaviour:ti,ab,kw or sex behavior:ti,ab,kw or sex behaviour:ti,ab,kw or sex education:ti,ab,kw or sex counseling:ti,ab,kw or sex counselling:ti,ab,kw |
| #17 | #11 or #12 or #13 or #14 or #15 or #16 |
| #18 | MeSH descriptor: [Schools] this term only |
| #19 | MeSH descriptor: [Community Networks] explode all trees |
| #20 | school*:ti,ab,kw or community:ti,ab,kw or communities:ti,ab,kw or teacher*:ti,ab,kw or classroom*:ti,ab,kw or educator*:ti,ab,kw or peer*:ti,ab,kw |
| #21 | #18 or #19 or #20 |
| #22 | MeSH descriptor: [Adolescent] this term only |
| #23 | MeSH descriptor: [Child] this term only |
| #24 | youth*:ti,ab,kw or teenager*:ti,ab,kw or teen:ti,ab,kw or teens:ti,ab,kw adolescen*:ti,ab,kw or child:ti,ab,kw or children:ti,ab,kw or youngster:ti,ab,kw or young person:ti,ab,kw or young people:ti,ab,kw |
| #25 | #22 or #23 or #24 |
| #26 | #10 and #17 and #21 and #25 Publication Year from YEAR to YEAR, in Trials |
Appendix 4. WHO ICTRP search strategy
sexually transmitted disease AND sexual behavior AND school OR sexually transmitted disease AND sexual behaviour AND school OR sexually transmitted disease AND sexual behavior AND community OR sexually transmitted disease AND sexual behaviour AND community OR hiv AND sexual behavior AND school OR hiv AND sexual behaviour AND school OR hiv AND sexual behavior AND community OR hiv AND sexual behaviour AND community
Data and analyses
Comparison 1. Educational interventions versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HIV prevalence | 3 | 14163 | Risk Ratio (Random, 95% CI) | 1.03 [0.80, 1.32] |
| 1.1 HIV prevalence young women | 3 | 6680 | Risk Ratio (Random, 95% CI) | 0.96 [0.67, 1.39] |
| 1.2 HIV prevalence young men | 3 | 7483 | Risk Ratio (Random, 95% CI) | 1.28 [0.71, 2.28] |
| 2 HSV2 prevalence | 3 | 17508 | Risk Ratio (Random, 95% CI) | 1.04 [0.94, 1.15] |
| 2.1 HSV2 prevalence young women | 3 | 8211 | Risk Ratio (Random, 95% CI) | 1.05 [0.92, 1.20] |
| 2.2 HSV2 prevalence young men | 3 | 9297 | Risk Ratio (Random, 95% CI) | 1.02 [0.88, 1.19] |
| 3 Syphilis prevalence | 1 | 6977 | Risk Ratio (Random, 95% CI) | 0.81 [0.47, 1.39] |
| 3.1 Syphillis prevalence young women | 1 | 2877 | Risk Ratio (Random, 95% CI) | 0.86 [0.42, 1.76] |
| 3.2 Syphillis prevalence young men | 1 | 4100 | Risk Ratio (Random, 95% CI) | 0.74 [0.32, 1.72] |
| 4 Pregnancy prevalence (short‐term) | 3 | 8280 | Risk Ratio (Random, 95% CI) | 0.99 [0.85, 1.16] |
| 5 Pregnancy prevalence (long‐term) | 4 | 12345 | Risk Ratio (Random, 95% CI) | 0.55 [0.34, 0.91] |
| 6 Self‐reported sexual debut | 4 | 22623 | Risk Ratio (Random, 95% CI) | 0.96 [0.91, 1.01] |
| 6.1 Young women | 3 | 8126 | Risk Ratio (Random, 95% CI) | 1.00 [0.94, 1.06] |
| 6.2 Young men | 3 | 8475 | Risk Ratio (Random, 95% CI) | 0.95 [0.85, 1.06] |
| 6.3 Self‐reported sexual debut young women and young men | 1 | 6022 | Risk Ratio (Random, 95% CI) | 0.95 [0.82, 1.09] |
| 7 Self‐reported use of condom at first sex | 2 | 8015 | Risk Ratio (Random, 95% CI) | 1.00 [0.98, 1.01] |
| 7.1 Used condom at first sex young women | 2 | 4365 | Risk Ratio (Random, 95% CI) | 0.99 [0.97, 1.01] |
| 7.2 Used condom at first sex young men | 2 | 3650 | Risk Ratio (Random, 95% CI) | 1.00 [0.98, 1.02] |
| 8 Self‐reported use of condom at last sex | 6 | 18795 | Risk Ratio (Random, 95% CI) | 1.00 [0.97, 1.03] |
| 8.1 Used condom last sex young women | 4 | 7444 | Risk Ratio (Random, 95% CI) | 1.01 [0.95, 1.07] |
| 8.2 Used condom at last sex young men | 4 | 6412 | Risk Ratio (Random, 95% CI) | 1.00 [0.93, 1.07] |
| 8.3 Used condom at last sex women and men | 2 | 4939 | Risk Ratio (Random, 95% CI) | 1.01 [0.91, 1.12] |
Comparison 2. Incentive‐based interventions versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HIV prevalence | 2 | 3805 | Risk Ratio (Random, 95% CI) | 1.23 [0.51, 2.96] |
| 1.1 HIV prevalence young women | 2 | 2489 | Risk Ratio (Random, 95% CI) | 1.18 [0.36, 3.89] |
| 1.2 HIV prevalence young men | 1 | 1316 | Risk Ratio (Random, 95% CI) | 1.96 [0.18, 21.07] |
| 2 HSV2 prevalence | 2 | 7229 | Risk Ratio (Random, 95% CI) | 0.98 [0.72, 1.36] |
| 2.1 HSV2 prevalence young women | 2 | 4089 | Risk Ratio (Random, 95% CI) | 0.64 [0.18, 2.23] |
| 2.2 HSV2 prevalence young men | 1 | 3140 | Risk Ratio (Random, 95% CI) | 1.09 [0.85, 1.39] |
| 3 Syphilis prevalence | 1 | 1291 | Risk Ratio (Random, 95% CI) | 0.41 [0.05, 3.27] |
| 3.1 Syphillis prevalence young women | 1 | 1291 | Risk Ratio (Random, 95% CI) | 0.41 [0.05, 3.27] |
| 4 Pregnancy prevalence (short‐term) | 2 | 4200 | Risk Ratio (Random, 95% CI) | 0.76 [0.58, 0.99] |
| 5 Pregnancy prevalence (long‐term) | 1 | 2891 | Risk Ratio (Random, 95% CI) | 0.89 [0.73, 1.08] |
| 6 Self‐reported sexual debut | 2 | 7177 | Risk Ratio (Random, 95% CI) | 0.83 [0.73, 0.95] |
| 6.1 Young women | 1 | 1016 | Risk Ratio (Random, 95% CI) | 0.68 [0.41, 1.13] |
| 6.2 Self‐reported sexual debut young women and young men | 1 | 6161 | Risk Ratio (Random, 95% CI) | 0.85 [0.74, 0.97] |
| 7 Self‐reported use of condom at last sex | 1 | 4265 | Risk Ratio (Random, 95% CI) | 0.98 [0.85, 1.12] |
| 7.1 Used condom at last sex women and men | 1 | 4265 | Risk Ratio (Random, 95% CI) | 0.98 [0.85, 1.12] |
Comparison 3. Combined incentive‐based and educational interventions versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HIV prevalence | 1 | 2506 | Risk Ratio (Random, 95% CI) | 1.53 [0.45, 5.13] |
| 1.1 HIV prevalence young women | 1 | 1174 | Risk Ratio (Random, 95% CI) | 1.41 [0.35, 5.78] |
| 1.2 HIV prevalence young men | 1 | 1332 | Risk Ratio (Random, 95% CI) | 1.90 [0.17, 20.60] |
| 2 HSV2 prevalence | 1 | 5899 | Risk Ratio (Random, 95% CI) | 0.82 [0.68, 0.99] |
| 2.1 HSV2 prevalence young women | 1 | 2717 | Risk Ratio (Random, 95% CI) | 0.76 [0.62, 0.93] |
| 2.2 HSV2 prevalence young men | 1 | 3182 | Risk Ratio (Random, 95% CI) | 0.92 [0.71, 1.19] |
| 3 Pregnancy prevalence (short‐term) | 1 | 2782 | Risk Ratio (Random, 95% CI) | 0.90 [0.67, 1.19] |
| 4 Pregnancy prevalence (long‐term) | 1 | 2801 | Risk Ratio (Random, 95% CI) | 0.90 [0.73, 1.12] |
| 5 Self‐reported sexual debut | 1 | 6102 | Risk Ratio (Random, 95% CI) | 0.84 [0.73, 0.97] |
| 5.1 Self‐reported sexual debut young women and young men | 1 | 6102 | Risk Ratio (Random, 95% CI) | 0.84 [0.73, 0.97] |
| 6 Self‐reported use of condom at last sex | 1 | 4193 | Risk Ratio (Random, 95% CI) | 1.02 [0.89, 1.17] |
| 6.1 Used condom at last sex women and men | 1 | 4193 | Risk Ratio (Random, 95% CI) | 1.02 [0.89, 1.17] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Baird 2012 MWI.
| Methods | Trial design: cluster‐randomized controlled trial (cluster‐RCT) Unit of randomization: enumeration areas Number of clusters: 176 Data collection: the primary outcomes were collected by home‐based voluntary counselling and testing (VCT) Length of follow‐up: impact assessed at 12 months, and biological outcomes measured at 18 months Adjustment for clustering: yes |
|
| Participants | Target group: 'never married' girls aged 13 to 22 years (schoolgirls and those who had dropped out of school) Sample size: 3796 Exclusions: none stated |
|
| Interventions | Intervention group:
Control group: no intervention |
|
| Outcomes | Included in this review:
Not included in this review:
|
|
| Notes | Country: Malawi Setting: Zomba district (rural) Study dates: 2007 to 2009 Study sponsors: Global Development Network, Bill and Melinda Gates Foundation, National Bureau of Economic Research Africa Project, World Bank's Research Support Budget, and several World Bank trust funds (Gender Action Plan, Knowledge for Change Program, and Spanish Impact Evaluation fund) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “the 176 geographic enumeration areas were randomly assigned (1:1) to intervention (cash transfer programme) or control groups (no programme)." p.1322 Quote: "the intervention group were further randomly assigned with computer‐generated random numbers to one of two groups: one received conditional cash transfer offers and the other unconditional cash transfer offers." p. 1322 Comment: stratified random sampling was described. Method of stratification described. |
| Recruitment bias | Low risk | Comment: a stratified random sample of 176 enumeration areas was chosen from 550 enumeration areas in the district. Individuals were recruited and baseline surveys completed before randomization of enumeration areas. |
| Baseline imbalance | Unclear risk | Quote: "Baseline characteristics in the intervention and control groups were similar." p. 1325 Comment: the intervention group were more likely to have unprotected sexual intercourse at baseline (16% intervention schoolgirls vs 11% control schoolgirls and 61% vs 57% of those dropped out of school). Biological outcomes (HIV, HSV2 and syphilis prevalence) were not reported at baseline. Authors report that this is because HIV testing was rare in Malawi at the start of the study and that it would constitute a separate intervention. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not reported sufficiently. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Study participants were not masked to their assignment but did not know what the comparison groups were because they were assigned at the enumeration area level.” p.1322, and “Study participants could not think that cash transfers were intended to reduce risky sexual behaviour and HIV or that they were tied to good behaviour in terms of sexual activity.”p.1323 Comment: participants were aware of whether they were receiving cash, how much, and whether it was conditional or not. They were not, however, aware that the primary outcomes were in fact related to STI prevalence, although some students had friends and acquaintances in the other groups. Source: p.1322, p.1323 Procedures. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "Trained counsellors who did home‐based counselling and rapid testing for HIV, HSV‐2 and syphilis were masked to the participant's group. Statistical analyses were done by the investigators who were not masked to the treatment status of the participants." p.1322 |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: “The percentage of study participants lost to follow up did not differ between control, conditional, and unconditional groups, and was lower than that reported for similar studies” and “133 (7%) baseline schoolgirls and 86 (10%) baseline dropouts were lost to follow up at 12 months" and that "none of the enumeration areas had complete loss to follow up rates were similar for 18 month visit (figure 2). Of the 1777 individuals selected for biological testing, 71 (4%) were lost to follow up because of either refusal to get tested (n = 51) or not being located by the data collection teams." Loss to follow up was similar amongst all groups. There was successful follow up of: 255/265 (96%) selected (90% of 283 total) CCT schoolgirls offered cash arm, 235/236 (99.6%) selected (46% of 506 total) UCT schoolgirls offered cash arm, 210/226 (96%) selected (48% of 436 total) dropouts offered cash arm. 799/827 (97%) selected (53% of 1495 total) control schoolgirls. 207/223 (93%) selected (46% of 453 total) schoolgirl controls. Source: p.1324 'Statistical analysis paragraph 2 p.1327 Discussion paragraph 2 p.1325 Results paragraph 2 p.1324 figure 2 |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes stated in methods were reported. |
| Other bias | Low risk | Comment: no other source of bias identified. |
Cabezón 2005 CHL.
| Methods | Trial design: cluster‐RCT Unit of randomization: classes in secondary schools Number of clusters: 13 Data collection: pregnancies that were term, preterm or miscarried were registered by the school administration Length of follow‐up: 3 years Adjustment for clustering: no |
|
| Participants | Target group: girls aged 15 to 16 years attending an all‐girls' high school Sample size: 1259 Exclusions: none stated |
|
| Interventions | The intervention
Control group: no intervention |
|
| Outcomes | Outcomes included in this review:
Not included in this review:
|
|
| Notes | Country: Chile Setting: one school in a suburban area. Study dates: 1997 to 2000 Study sponsors: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Among 10 classes five were alternatively selected". p.65. Quote: "These 8 classes were chosen blindly, taking the letter of the class from a bag to be intervention group in the 1998 cohort, thus leaving 2 classes as control group in this cohort." p.65. |
| Recruitment bias | High risk | Comment: only intervention group parents were asked to sign a consent form. |
| Baseline imbalance | High risk | Comment: there was baseline imbalance in pregnancy incidence between the groups in 1997, with none in the intervention group and 6 in the control group. p.66 Table 3. |
| Allocation concealment (selection bias) | High risk | Comment: unlikely as classes were chosen alternately. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: blinding not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: blinding not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "During the 4‐year follow up period the dropout rates from school were similar in the three studied cohorts." p. 67. |
| Selective reporting (reporting bias) | High risk | Quote: "Measurement of pregnancy rates is difficult because it is not possible to know if there were any induced abortions in the control or study groups." p. 68. |
| Other bias | High risk | Comment: as abortion in Chile is illegal it is unlikely that pregnancy and abortion was fully reported to schools. |
Cowan 2010 ZWE.
| Methods | Trial design: cluster‐RCT Unit of randomization: a 'community' comprising a health clinic, its catchment population and its secondary schools Number of clusters: 30 Data collection: a representative survey of 18‐22 year olds in study communities 4 years after the intervention. This included a questionnaire, HIV‐1, HSV2, and a pregnancy test Length of follow‐up: 4 years Adjustment for clustering: yes |
|
| Participants | Target group: Form 2 pupils (median age 15 years) Sample size: 6791 Exclusions: none stated |
|
| Interventions | The intervention
Control group: no intervention (delayed intervention until 2007) |
|
| Outcomes | Outcomes included in this review:
Outcomes not included in this review:
|
|
| Notes | Country: Zimbabwe Setting: rural districts Study dates: 2003 to 2007 Study sponsors: National Institute of Mental Health, DfID Zimbabwe |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Restricted randomisation was used to ensure balance between arms of the study.” Source: p1237 (Cowan 2008). Comment: random allocation, stratification criteria detailed, but method of randomization was not explained. |
| Recruitment bias | Unclear risk | Comment: clusters were randomized first and then individuals were recruited from those clusters. |
| Baseline imbalance | Low risk | Quote: "There was excellent balance between early and deferred intervention [author's note: i.e. between intervention and control] arms in terms of rates of HIV‐1 infection and other behavioural and socio‐demographic variables." Source: p.1240 (Cowan 2008). |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no blinding described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no blinding described. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: “During our interim survey in 2006, we found there had been considerable outmigration (46%).Those who remained were of lower risk than those who had left” p. 2542 “The age of the [original] cohort spanned 11 years, the age of participants surveyed at the end of the trial spanned 5 years.” “The proportion of original cohort members being included in the final survey was unlikely to be more than 7%.” p.2543. Comment: there was a very low follow‐up rate of the original cohort. Cross‐sectional analysis of clusters was completed, but with few of original participants. As a result any effect of the intervention is likely to be diluted by following up members of the cluster who did not receive the intervention. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes stated in the Methods were reported. |
| Other bias | High risk | Quote: "It became difficult to implement the programme in schools for political reasons. This coincided with a fall in school attendance for economic reasons." p.2551. A reported decline in HIV incidence in Zimbabwe resulted in a change in study design in order to increase the power of the study. As a result, the final cross‐sectional survey included six enumeration areas from each community (each community contained approximately 50 enumeration areas), so approximately 12% of eligible 18‐22 year olds were sampled. As a result of outmigration the proportion of the original cohort members being included was unlikely to be more than 7%. |
Duflo 2015 KEN.
| Methods | Trial design: cluster‐RCT Unit of randomization: schools Number of clusters: 328 Data collection: unannounced 'roll call' visits were made over 5 years. Biomarker data (HIV and HSV2) were measured at 7 years. Length of follow‐up: 7 years Adjustment for clustering: yes |
|
| Participants | Target group: 6th grade students (13 to 14 years old) Sample size: 19,289 students in 6th grade in 2003, enrolled in primary schools Exclusions: none stated |
|
| Interventions | The intervention (3 intervention groups: 1. Stand‐alone education subsidy, 2. Stand‐alone education, 3. a joint programme of subsidy plus education).
Control group: no intervention. |
|
| Outcomes | Included in this review:
Not included in this review:
|
|
| Notes | Country: Kenya Setting: Butere‐Mumias and Bungoma Study dates: 2003 to 2010 Study sponsors:the Hewlett Foundation, the MacArthur Foundation, the National Institutes of Health, the Nike Foundation, the Partnership for Child Development, and the World Bank |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "Schools were stratified and assigned to one of four arms using a random number generator." p.2673. |
| Recruitment bias | Low risk | Comment: all schools in the geographical area were included and agreed to participate. Clusters were randomized first and then individuals were included from those clusters. However students were enrolled before the announcement of the educational subsidy programme and only those on the original baseline enrolment group were eligible for free uniforms. |
| Baseline imbalance | Low risk | Quote: "Differences across treatment groups are small in magnitude and only 4 of 65 p‐values estimated are smaller than 0.10, suggesting that the randomization was effective at creating balance between the groups." |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment was not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: blinding of students not described. Blinding of teachers was not possible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: 'roll calls' were used for the pregnancy outcomes. It was unclear if the assessors were blinded to allocation of the schools and therefore the individuals attending them. The HIV and HSV2 testing was completed by a mobile clinic and later, for those who had not responded, 'field officers' and 'lab technicians'. Again it was unclear if these assessors were blinded to allocation of the individuals/schools. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: there was no loss of clusters in the trial. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes stated in the methods were reported. |
| Other bias | Low risk | Comment: no other source of bias was identified. |
Henderson 2007 GBR.
| Methods | Trial design: cluster‐RCT Unit of randomization: schools Number of clusters: 25 Data collection: Data collection was via linkage of individual participants' details to NHS conception and termination data, aggregated by school. Length of follow‐up: 4.5 years. Adjustment for clustering: yes Cluster‐RCT to assess the impact of a theoretically‐based sexuality education programme in 25 (13 intervention, 12 control) secondary schools in the east of Scotland. The approach taken was stated as 'harm reduction' so that those already sexually active would be encouraged to use condoms. Incentives were offered to schools including teacher training, supply cover, or, for schools in the control arm, an equivalent cash amount that could be spent on personal and social education but not sexuality education. |
|
| Participants | Target group: 3rd year secondary school students aged 13‐15 years Sample size: 4196 Exclusions: Roman Catholic schools |
|
| Interventions | The intervention
Control group: usual practice. |
|
| Outcomes | Included in this review:
Not included in this review:
|
|
| Notes | Country: Scotland Setting: state schools in east Scotland Study dates: 1993 to 1996 Study sponsors: UK Medical Research Council and Health Education Board for Scotland |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “A balanced randomisation took into account socioeconomic characteristics of the school populations…” Comment: stratification of random sampling described. Method of random generation not described. Source: p.2 Recruitment and randomisation of schools |
| Recruitment bias | Unclear risk | Comment: clusters were randomized first and then individuals were recruited from those clusters. |
| Baseline imbalance | Unclear risk | Comment: slight imbalance in gender reported by authors. Also there was a difference in those students who had reported sexual intercourse at baseline. Source: p.3 online (Wight 2002) |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment was not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: blinding of students was not described. Blinding of teachers was not possible, as teachers were sent on a SHARE training course. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: “We submitted records of surname, forename, date of birth, and postcode(s) for women in the trial (excluding withdrawals) for linkage to the NHS data. Comment: biological outcome data from NHS databases, gathered independently of trial personnel, but blinding of study assessors not described. Source: p.2 Follow up and statistical analysis |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Biological outcomes: Quote: “There may have been a small level of attrition across both arms because of women attending private health care (less than 2% of terminations), moving from Scotland during the study period (1% average annual migration out of Scotland), or having their terminations in England or Wales (2.7% of all terminations performed on Scottish residents). On balance, the comparison between this study and national rates suggests that the linkage was broadly effective.” Comment: 99.6% participants in intervention arm analysed, 99.5% participants in control arm analysed (flow diagram p.2). Very high follow‐up rate, loss to follow‐up not significantly different across trial arms (9/2071 intervention arm vs 10/2135 control arm). Intention‐to‐treat analysis performed. Source: p.3 Discussion first paragraph, and p.2 flow diagram. Outcome group: self‐reported outcomes Quote: “One school considered the baseline survey to be too explicit for pupils aged 13‐14 years but took part in all other aspects of the study” “a new work experience scheme increased this [leaving school] to 27%. The response rate was lower for school leavers (41% control, 38% intervention). Non‐response among those still in school was primarily among persistent absentees, but a small proportion refused to participate (2%). The response rates were similar in each arm of the trial.” Comment: follow‐up data available for 2987/4233 (71%) control pupils, and 2867/4197 (68%) intervention pupils. High loss to follow‐up, spread approximately equally across both groups. Systematic under‐representation of school leavers could possibly have introduced bias towards the null as data is missing regarding long‐term effects. Source: p.3 Participant follow up, p.2 flow chart |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes stated in methods were reported. |
| Other bias | Low risk | Comment: no other source of bias identified. |
Jemmott 2015 ZAF.
| Methods | Trial design: cluster‐RCT Unit of randomization: schools Number of clusters: 18 (9 matched pairs) Data collection: questionnaire surveys at 3, 6, 12, 42, and 54 months. Blood test and urine sample for STIs at 54 months Length of follow‐up: 54 months Adjustment for clustering: yes |
|
| Participants | Target group: Grade 6 pupils (median age not stated but range 9 to 18 years) Sample size: 1057 Exclusions: none stated |
|
| Interventions | The intervention
Control group: no intervention. |
|
| Outcomes | Outcomes included in this review:
Outcomes not included in this review:
|
|
| Notes | Country: South Africa Setting: urban/semi‐rural areas of Eastern Cape Study dates: 2004 to 2010 Study sponsors: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were randomized firstly from 35 eligible schools but the method for this was not described. It was not clear how the matching was done for the18 schools chosen. The authors did say that randomization was done using a computer‐generated random number sequence within pairs where one of the pair would be allocated to the HIV/STI risk reduction intervention and one to the control group. p. 611. |
| Recruitment bias | Unclear risk | Comment: clusters were randomized first and then individuals were recruited from those clusters. |
| Baseline imbalance | Unclear risk | Comment: there was some imbalance at baseline. |
| Allocation concealment (selection bias) | Low risk | Quote: "School personnel, potential participants and recruiters were masked to the schools' randomized intervention assignment." p.611. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "The nature of the intervention precluded masking the facilitators and participants to the group assignment during the interventions." p.611. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: blinding was not described. Source: Measures: p.615. No description of blinding of laboratory technicians to the allocation status of the samples |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | It appears that the authors had a very high follow‐up rate. The participant flow diagram (p.616) suggests that the study had a 99.2% follow‐up at 54 months (1049/1057). |
| Selective reporting (reporting bias) | High risk | Data for the biological outcomes was not included in table 2 (p.617) so could not be included in the meta‐analysis. The authors were contacted directly and asked for the data but this has not been sent to date. |
| Other bias | Unclear risk | Method of choosing schools that were eligible was not sufficiently described. |
Ross 2007 TZA.
| Methods | Trial design: cluster‐RCT Unit of randomization: communities Number of clusters: 20 Data collection: survey at 1 and 3 years after enrolment. HIV/HSV2 and pregnancy test at 3 years Length of follow‐up: 3 years Adjustment for clustering: yes |
|
| Participants | Target group: Year 5 to 7 primary school pupils (14 to 18 years old) Sample size: 9645 Exclusions: none stated |
|
| Interventions | The intervention:
Control group: no intervention. |
|
| Outcomes | Outcomes included in this review:
Outcomes not included in this review:
|
|
| Notes | Country: Tanzania Setting: rural areas of Mwanza region Study dates: 1998 to 2002 Study sponsors: The European Commission, Development Cooperation Ireland, UK Medical Research Council, Department for International Development (DFID) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Restricted randomisation was used to balance HIV and chlamydia prevalence between the two trial arms” Comment: stratified randomization of communities described; stratification explained. Source: p.1944 Methods (Ross 2007 TZA). |
| Recruitment bias | Low risk | Comment: individuals were recruited first and then randomized to clusters. |
| Baseline imbalance | Low risk | Quote: "The baseline characteristics of the intervention and comparison groups were generally similar (Table 2). Slight baseline imbalances in ethnic group and lifetime number of partners were adjusted for in all analyses of trial outcomes. There were substantial differences between male and female participants, so outcomes were analyzed separately for sex." p.1947. |
| Allocation concealment (selection bias) | Low risk | Quote: "A system of constrained randomisation was used to allocate communities to the two study arms,ensuring adequate balance on important factors. There were 28,000 ways of allocating half the communities in each stratum to the intervention arm. A computer program tested whether each of these allocations satisfied balance criteria, including: (i) mean HIV prevalence in each study arm within 0.075% of overall mean; (ii) mean prevalence of Chlamydia trachomatis (CT) in each arm within 0.1% of overall mean; (iii) one of two communities neighbouring gold mines allocated to each arm; (iv) even distribution of intervention communities over the four project districts. A total of 953 allocations satisfied these criteria, and one was randomly chosen at a meeting attended by senior government officials" Source: p.436 (Hayes 2005). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no blinding described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: blinding was not described. Source: p.1946 Impact evaluation final paragraph. There is no description of the authors blinding the laboratory technicians to the allocation status of the samples. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: “7040 (73%) of the 9645 eligible cohort members were seen at the final survey. Follow up rates were similar in the intervention (72%) and comparison (74%) communities, higher among male (77%) than female (69%) participants (P<0.001)” “HIV incidence was much lower than predicted based on a previous survey of 15‐19 year olds in the same communities… those who were lost to follow up may have been at a higher risk than those followed up.” Comment: similar attrition across intervention and comparison groups Source: p.1497 Completeness of follow up p.1949 Table 2 p.1951 Discussion |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes stated in Methods were reported. |
| Other bias | Low risk | Comment: no other source of bias identified. |
Stephenson 2008 GBR.
| Methods | Trial design: cluster‐RCT Unit of randomization: schools Number of clusters: 27 Data collection: survey questionnaires were completed in the classroom at baseline, and after 6 and 18 months. Those who were still in school also completed a questionnaire at 54 months after baseline. Those who had left school were provided with a questionnaire by post, by home visit or by GP. Primary outcome measures were abortion and live births age 20 as determined by linkage to routine NHS data. Length of follow‐up: 7 years Adjustment for clustering: yes |
|
| Participants | Target group: Year 9 pupils, (13 to 14 years old) Sample size: 9508 (eligible and followed up for biological outcomes), 8766 for other outcomes Exclusions: 8 schools were excluded due to distance from London where the research team was located. |
|
| Interventions | The intervention
Control group: usual teacher‐led sexual and relationships education (SRE). |
|
| Outcomes | Outcomes included in this review:
Outcomes not included in this review:
|
|
| Notes | Country: England. Setting: rural and urban schools in central and southern England Study dates: 1998‐2005 Study sponsors: UK Medical Research Council |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Schools were ranked and divided into three risk strata of approximately equal size. Randomisation of schools occurred within strata, using a computer‐generated sequence of allocation of block size ten for each”. Comment: randomization method adequately described, criteria for stratification given. Source: p.1581 Randomisation |
| Recruitment bias | Unclear risk | Comment: clusters were randomized first and then individuals were recruited from those clusters. |
| Baseline imbalance | Low risk | Quote: "The two groups were well balanced with respect to demographic data and proportion reporting sexual intercourse at baseline (table 1)." Source: p.342 (Stephenson 2004). |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: “blinding of participants to type of sex education was not possible”. Comment: blinding of participants was not possible. Source: p.1585 Discussion. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome group: biological outcome measures. Quote: “Following list‐cleaning of the trial register through National Health Register (NHS) central register, girls were matched to routine data on live births from two sources: (1) registration of births (2) registration of maternities. Girls were matched to routine data derived from statutory abortion notification…” “Matching to routine sources was blinded”. Comment: biological outcomes were measured independently of trial co‐ordinators. Source: p.1580 Outcomes p.1585 Discussion |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome group: biological outcomes. Quote: “Primary analysis was by intention to treat.” There was “more missing data in the trial register for abortion matching (postcode and date of birth) than for live birth matching (NHS number only). Any bias from under matching of abortions is likely to be toward underestimation of abortion data in the control arm, since the control arm had more missing data than the intervention arm”. “missing postcode for 25% of girls (28% control, 21% intervention, p=0.21)”. Comment: 100% of all eligible girls were followed up, and an intention‐to‐treat analysis performed. Missing data for abortions was higher in the control group but the P value was 0.21. It is possible that this might have biased the results towards the null hypothesis, but this appears to be a small risk. Source: p.1581 Statistical methods p.1583 CONSORT diagram. p.1585 Discussion p1584 Evaluation of outcomes Outcome group: self reported measures. Quote: "Parents did not provide consent for 183 (1·9%) of year 9 pupils (1·5% from control, 2·3% from intervention schools) to take part in the research. Two schools (one from each arm) withdrew because of staff changes without knowing their random allocation. One school was unable to implement the intervention, but contributed to follow‐up. Differential loss to follow‐up between intervention and control schools was largely attributable to loss of one large school after a parent's objection to the questionnaire, although completion rates differed significantly at first follow‐up. Source: p.342 (Stephenson 2004). Quote: “Questionnaires at age 18y were completed by significantly more (p=0.001) intervention pupils (52.3% overall: 61.3% girls, 43.7% boys) than control pupils (38.1% overall: 45.4% girls, 31.4% boys).” “pupils at higher risk of pregnancy are likely to be harder to follow up”. Comment: high rate of loss to follow‐up, different between control and intervention arm. Source: p.1584 Evaluation of outcomes paragraph 2, CONSORT diagram p.1583, p.1585 Discussion. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes stated in Methods were reported. |
| Other bias | Low risk | Comment: no other source of bias identified. |
Abbreviations: HIV: human immunodeficiency virus, HIV‐1: human immunodeficiency virus‐1, HSV2: herpes simplex virus‐2, N/A: not applicable, STD: sexually transmitted disease; STI: sexually transmitted infection.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aninanya 2015 | No biological outcomes |
| Bauermeister 2015 | No biological outcomes |
| Beattie 2015 | Protocol/early report |
| Borawski 2015 | No biological outcomes |
| Chhabra 2007 | Not an RCT |
| Coyle 2004 | No biological outcomes |
| Cupp 2013 | No biological outcomes |
| de Walque 2012 | Not school‐based |
| Dente 2005 | Not an RCT |
| Di Noia 2007 | No biological outcomes |
| DiClemente 2004 | No biological outcomes |
| DiIorio 2007 | Not school‐based |
| Dittus 2014 | No biological outcomes |
| Espada 2015 | No biological outcomes |
| Estrada 2015 | No biological outcomes |
| Gaydos 2008 | No biological outcomes |
| Gray 2007 | Not an RCT |
| Grossman 2013 | Not an RCT |
| Guse 2012 | Systematic review |
| Hawk 2013 | Not school‐based |
| Hidalgo 2015 | No biological outcomes |
| Hill 2014 | Not RCT |
| Jemmott 2010 | No biological outcomes |
| Jewkes 2008 | Not school‐based. |
| Kennedy 2014 | Not school‐based |
| Kirby 1997 | No biological outcomes |
| Langley 2015 | No biological outcomes |
| Li 2008 | Not an RCT |
| Markham 2012 | No biological outcomes |
| Marsch 2015 | No biological outcomes |
| Mathews 2015 | No biological outcomes |
| Mavedzenge 2011 | Systematic review |
| Mellanby 2000 | Not an RCT |
| Michielsen 2010 | Systematic review |
| Morales 2016 | No biological outcomes |
| Morrison 2007 | Not an RCT |
| Namisi 2013 | No biological outcomes |
| Newby 2013 | Protocol/early report |
| Oringanje 2016 | Systematic review |
| Paul‐Ebhohimhen 2008 | Systematic review |
| Pedlow 2003 | Systematic review |
| Peskin 2015 | No biological outcomes |
| Pettifor 2015 | Protocol/early report |
| Picot 2012 | Systematic review |
| Prado 2007 | Not school‐based |
| Raiford 2014 | Not school‐based |
| Reyna 2014 | No biological outcomes |
| Rohrbach 2015 | No biological outcomes |
| Ross 2010 | Systematic review |
| Sanci 2015 | Not school‐based |
| Shahmanesh 2008 | Systematic review |
| Shepherd 2010 | Systematic review |
| Simmons 2015 | Not school‐based |
| Spoth 2014 | Not school‐based |
| Stanton 2015 | No biological outcomes |
| Stephenson 1998 | Not an RCT |
| Tingey 2015 | Protocol/early report |
| Tortolero 2010 | No biological outcomes |
| Underhill 2007 | Systematic review |
| Wang 2014 | No biological outcomes |
| Weiss 2008 | Not an RCT |
| Zhang 2015 | Not an RCT |
| Zimmerman 2008 | Not an RCT |
Abbreviations: RCT: randomized controlled trial.
Characteristics of ongoing studies [ordered by study ID]
ISRCTN56270821.
| Trial name or title | Preventing sexual risk behavior and partner violence among adolescents in Cape Town |
| Methods | Cluster‐RCT in 42 participating high schools in Western Cape Province |
| Participants | Males and females in Grade 8 attending public high schools in the Western Cape Province (between 3000 and 4000 adolescents). |
| Interventions | The intervention consists of 4 components:
|
| Outcomes | The primary outcomes are: 1. sexual debut; 2. number of partners; 3. consistent use of condoms Secondary outcomes are 1. live births and terminations of pregnancy among female participants, as counts per school, over a 3‐year time period; 2. intimate partner violence perpetration and victimization |
| Starting date | January 2013 |
| Contact information | Catherine Mathews, South African Medical Research Council |
| Notes | www.controlled‐trials.com/ISRCTN56270821 |
NCT01187979.
| Trial name or title | Reducing HIV in adolescents (RHIVA): a proof of concept cluster randomized controlled trial to evaluate the impact of a cash incentivised prevention intervention to reduce HIV infection in high school learners in rural KwaZulu‐Natal, South Africa |
| Methods | The impact of the cash incentivised intervention will be assessed using a matched pair, cluster‐RCT design. The 14 selected high schools in the Vulindlela School Circuit will be matched in pairs. The matched pairs of schools will be the unit of randomization. Baseline measurements, using a standardized tool (structured questionnaire and biological specimens) will be undertaken simultaneously in each matched pair and will include all eligibly enrolled and consenting learners in the respective schools. On completion of baseline measurements in each matched pair of schools, the randomization code for the pair will be revealed and the intervention will be implemented in the intervention school. All schools will receive the same prevention intervention but only the intervention school will receive the cash incentives. Follow‐up measurements will be undertaken approximately 12 and 24 months after implementation of the intervention using a similar standardized assessment tool to that used at baseline. |
| Participants | 4000 Grade 9 and 10 male and female students (aged 13+ years) in 14 schools |
| Interventions | Behavioural: cash incentives paid to learners for reaching predetermined milestones Behavioural: standard department of education life skills curriculum |
| Outcomes | Primary: HIV incidence Secondary: academic performance, substance use patterns, pregnancy, contraceptive use, participation in extra‐curricular activities, HIV risk‐reduction behaviour. Linked HIV and substance use testing will be undertaken in all learners and pregnancy testing in female learners. Other secondary endpoints will be assessed using a structured questionnaire. |
| Starting date | September 2010 |
| Contact information | Dr Quarraisha Abdool Karim, Centre for the AIDS Programme of Research in South Africa |
| Notes | www.clinicaltrials.gov/ct2/show/NCT01187979?term=abdool+karim&rank=4 |
NCT01233531.
| Trial name or title | Effects of cash transfer for the prevention of HIV in young South African women |
| Methods | Individually randomized, parallel controlled trial. The overall purpose of this study is to determine whether providing cash transfers to young women and their household, conditional on school attendance, reduces young women's risk of acquiring HIV. The overall goal of the Conditional Cash Transfer (CCT) intervention is to reduce structural barriers to education, with the goal of increasing school attendance of young women, thereby decreasing their HIV risk. |
| Participants | Females 13 to 20 years enrolled in grades 8, 9, 10, or 11 at the beginning of the study at schools at the study site |
| Interventions | Monthly cash transfer payments for attending school In the intervention, young women and their households will be randomized in 1:1 ratio to receive monthly cash transfer payments, conditional on the young woman attending school, or to the control arm. Young women will be recruited at the beginning of grades 8 through 11 in the first year of the study. |
| Outcomes | Primary: HIV incidence Secondary: HSV2 incidence, HSV incidence |
| Starting date | March 2011 |
| Contact information | Audrey Pettifor, University of North Carolina |
| Notes | www.clinicaltrials.gov/ct2/show/NCT01233531?term=hptn+068&rank=1 |
NCT02455583.
| Trial name or title | An assessment of an HIV prevention intervention (Project AIM) on youth sexual intentions, sexual behaviours and HSV‐2 incidence and prevalence in junior secondary schools in Eastern Botswana |
| Methods | Stratified, cluster‐RCT |
| Participants | Males and females enrolled in Form 1 in one of 50 selected schools who are fluent and literate in English or Setswana |
| Interventions | Form 1 learners at 25 intervention schools will receive the Project AIM intervention (14 sessions of 40 minutes delivered twice a week) and LIVING (standard of care)). |
| Outcomes | Primary: difference in HSV2 incidence between the intervention and control arm at 24 months Secondary: self‐reported sexual and sexual‐risk related behaviour measured by sexual initiation, number of sexual partners and frequency of alcohol use, sexual intercourse, and condom use; sexual thoughts measured by frequency of thoughts about engaging in sexual activity, attitudes towards education and frequency of thoughts and feelings about the future and hopelessness; attitudes towards partner concurrency, transactional sex and sexual risk communication with a partner; intention to engage in sexual activity |
| Starting date | September 2014 |
| Contact information | Kim S Miller, Centers for Disease Control and Prevention Nontobeko S Tau, Botswana Ministry of Education and Skills Development |
| Notes | clinicaltrials.gov/ct2/show/NCT02455583 |
NCT02665091.
| Trial name or title | Impact of peer education program on HIV/AIDS related sexual behaviours of secondary school students in rural communities, India: a quasi‐experimental study |
| Methods | Individually RCT |
| Participants | Young people 14 to 18 years old |
| Interventions | Peer education programme |
| Outcomes | Primary: knowledge score of HIV Secondary: willingness to have HIV testing, willingness to participate in HIV counselling services and frequency of use of condoms |
| Starting date | February 2015 |
| Contact information | Hitesh Nayak, NMP Medical Research Institute |
| Notes | clinicaltrials.gov/ct2/show/record/NCT02665091 |
Abbreviations: HIV: human immunodeficiency virus; HSV: herpes simplex virus; HSV2: herpes simplex virus‐2.
Differences between protocol and review
The only major deviation from the protocol and the review was a change in the title in line with recent guidance from Cochrane, which suggested that a more explanatory title be used. The original registered title was 'School‐based interventions to postpone sexual intercourse and promote condom use among adolescents'
Contributions of authors
AMJ and either DS, CM, AK, or AH conducted the searches, independently assessed all papers for inclusion, and extracted the data. AMJ and CL conducted the analyses and CL provided overall statistical advice. AMJ wrote the review and DS, CM, AK, AH, and CL commented on the review drafts and approved the final submission.
Sources of support
Internal sources
-
University of York, UK.
Support for AMJ from October 2012 to date, and AH from January to March 2014.
Liverpool School of Tropical Medicine, UK.
External sources
-
South African Medical Research Council, South Africa.
Funded the time of AMJ to September 2012 and time of CM and CL.
-
Stellenbosch University, South Africa.
Funded the time of AK.
-
South African Cochrane Centre, South Africa.
Provided academic training for AMJ and CM and support for the review authors, assisted with the searches and procured some of the full‐text articles.
-
Department for International Development (DFID), UK.
Grant: 5242
Declarations of interest
Two review authors (AMJ and CM) are investigators in an ongoing study evaluating the effects of school‐based HIV and intimate partner violence prevention intervention programme on biologically measured pregnancy outcome for adolescents. DS has no known conflicts of interest. AK has no known conflicts of interest. AH has no known conflicts of interest. CL has no known conflicts of interest.
Unchanged
References
References to studies included in this review
Baird 2012 MWI {published data only}
- Baird SJ, Garfein S, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet 2012;379(9823):1320‐9. [DOI] [PubMed] [Google Scholar]
Cabezón 2005 CHL {published data only}
- Cabezón C, Vigil P, Rojas I, Leiva E, Riquelme R, Aranda W, et al. Adolescent pregnancy prevention: an abstinence‐centered randomized controlled intervention in a Chilean public high school. Journal of Adolescent Health 2005;36(1):64‐9. [DOI] [PubMed] [Google Scholar]
Cowan 2010 ZWE {published data only}
- Cowan FM, Pascoe SJ, Langhaug LF, Mavhu W, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri project: results of a randomized trial of an HIV prevention intervention for youth. AIDS 2010;24(16):2541‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duflo 2015 KEN {published data only}
- Duflo E, Dupas P, Kremer M. Education, HIV and early fertility: experimental evidence from Kenya. American Economic Review 2015;105(9):2757‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Henderson 2007 GBR {published data only}
- Henderson M, Wight D, Raab GM, Abraham C, Parkes A, Scott S, et al. Impact of a theoretically based sex education programme (SHARE) delivered by teachers on NHS registered conceptions and terminations: final result of cluster randomised trial. BMJ 2007;334(7585):133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jemmott 2015 ZAF {published data only}
- Jemmott JB 3rd, Jemmott LS, Ngwane Z, Bellaby SL, Carty CC, Heeren GA, et al. HIV/STI risk‐reduction intervention efficacy with South African adolescents over 54 months. Health Psychology 2015;34(6):610‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ross 2007 TZA {published data only}
- Ross DA, Changalucha J, Obasi AIN, Todd J, Plummer ML, Cleophas‐Mazige B, et al. Biological and behavioural impact of an adolescent sexual health intervention in Tanzania: a community‐randomized trial. AIDS 2007;21(14):1943‐55. [DOI] [PubMed] [Google Scholar]
Stephenson 2008 GBR {published data only}
- Stephenson J, Strange V, Allen E, Copas A, Johnson A, Bonell C, et al. the RIPPLE Study Team. The long‐term effects of a peer‐led sex education programme (RIPPLE): a cluster randomised trial in schools in England. PLoS Medicine 2008;5(11):e224. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Aninanya 2015 {published data only}
- Aninanya GA, Debpuur CY, Awine T, Williams JE, Hodgson A, Howard N. Effects of an adolescent sexual and reproductive health intervention on health service usage by young people in northern Ghana: a community‐randomised trial. PLoS One 2015;10(4):e0125267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bauermeister 2015 {published data only}
- Bauermeister JA, Pingel ES, Jadwin‐Cakmak J, Harper GW, Horvath K, Weiss G, et al. Acceptability and preliminary efficacy of a tailored online HIV/STI testing intervention for young men who have sex with men: the Get Connected! program. AIDS and Behavior 2015;19(10):1860‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beattie 2015 {published data only}
- Beattie TS, Bhattacharjee P, Isac S, Davey C, Javalkar P, Nair S, et al. Supporting adolescent girls to stay in school, reduce child marriage and reduce entry into sex work as HIV risk prevention in north Karnataka, India: protocol for a cluster randomised controlled trial. BMC Public Health 2015;15:292. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borawski 2015 {published data only}
- Borawski EA, Tufts KA, Trapl ES, Hayman LL, Yoder LD, Lovegreen LD. Effectiveness of health education teachers and school nurses teaching sexually transmitted infections/human immunodeficiency virus prevention knowledge and skills in high school. Journal of School Health 2015;85(3):189‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chhabra 2007 {published data only}
- Chhabra R, Springer C, Rapkin B, Merchant Y. Differences among male/female adolescents participating in a School‐based Teenage Education Program (STEP) focusing on HIV prevention in India. Ethnicity & Disease 2007;18(2 Suppl 2):S2‐123‐7. [PubMed] [Google Scholar]
Coyle 2004 {published data only}
- Coyle KK, Kirby DB, Marín BV, Gómez CA, Gregorich SE. Draw the line/respect the line: a randomized trial of a middle school intervention to reduce sexual risk behaviors. American Journal of Public Health 2004;94(5):843‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cupp 2013 {published data only}
- Cupp PK, Atwood KA, Byrnes HF, Miller BA, Fongkaew W, Chamratrithirong A, et al. The impact of Thai family matters on parent‐adolescent sexual risk communication attitudes and behaviors. Journal of Health Communication 2013;18(11):1384‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dente 2005 {published data only}
- Dente MG, Fabiani M, Okwey R, Conestà N, Opira C, Declich S. Impact of voluntary counselling and testing and health education on HIV prevention among secondary school students in northern Uganda. Health Policy and Development 2005;3(1):1‐11. [Google Scholar]
de Walque 2012 {published data only}
- Walque D, Dow WH, Nathan R, Abdul R, Abilahi F, Gong E, et al. Incentivising safe sex: a randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open 2012;2:e000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
DiClemente 2004 {published data only}
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW 3rd, et al. Efficacy of an HIV prevention intervention for African American adolescent girls: a randomized controlled trial. JAMA 2004;292(2):171‐9. [DOI] [PubMed] [Google Scholar]
DiIorio 2007 {published data only}
- DiIorio C, McCarty F, Resnicow K, Lehr S, Denzmore P. REAL men: a group‐randomized trial of an HIV prevention intervention for adolescent boys. American Journal of Public Health 2007;97(6):1084‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Di Noia 2007 {published data only}
- Noia J, Schinke SP. Gender–specific HIV prevention with urban early‐adolescent girls: outcomes of the keepin’it safe program. AIDS Education and Prevention 2007;19(6):479. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dittus 2014 {published data only}
- Dittus PJ, Rosa CJ, Jeffries RA, Afifi AA, Cumberland WG, Chung EQ, et al. The project connect health systems intervention: linking sexually experienced youth to sexual and reproductive health care. Journal of Adolescent Health 2014;55(4):528‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Espada 2015 {published data only}
- Espada JP, Morales A, Orgilés M, Jemmott JB, Jemmott LS. Short‐term evaluation of a skill‐development sexual education program for Spanish adolescents compared with a well‐established program. Journal of Adolescent Health 2015;56(1):30‐7. [DOI] [PubMed] [Google Scholar]
Estrada 2015 {published data only}
- Estrada Y, Rosen A, Huang S, Tapia M, Sutton M, Willis L, et al. Efficacy of a brief intervention to reduce substance use and human immunodeficiency virus infection risk among Latino youth. Journal of Adolescent Health 2015;57(6):651‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gaydos 2008 {published data only}
- Gaydos C, Hsieh Y, Galbraith J, Barnes M, Waterfield G, Stanton B. Focus‐on‐Teens, sexual risk‐reduction intervention for high‐school adolescents: impact on knowledge, change of risk‐behaviours, and prevalence of sexually transmitted diseases. International Journal of STD & AIDS 2008;19(10):704‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gray 2007 {published data only}
- Gray RH, Wawer MJ. Randomised trials of HIV prevention. Lancet 2007;370(9583):200‐1. [DOI] [PubMed] [Google Scholar]
Grossman 2013 {published data only}
- Grossman JM, Frye A, Charmaraman L, Erkut S. Family homework and school‐based sex education: delaying early adolescents' sexual behavior. Journal of School Health 2013;83(11):810‐7. [DOI] [PubMed] [Google Scholar]
Guse 2012 {published data only}
- Guse K, Levine D, Martins S, Lira A, Gaarde J, Westmorland W, et al. Interventions using new digital media to improve adolescent sexual health: a systematic review. Journal of Adolescent Health 2012;51(6):535‐43. [DOI] [PubMed] [Google Scholar]
Hawk 2013 {published data only}
- Hawk M. The Girlfriends Project: results of a pilot study assessing feasibility of an HIV testing and risk reduction intervention developed, implemented, and evaluated in community settings. AIDS Education and Prevention 2013;25(6):519‐34. [DOI] [PubMed] [Google Scholar]
Hidalgo 2015 {published data only}
- Hidalgo MA, Kuhns LM, Hotton AL, Johnson AK, Mustanski B, Garofalo R. The MyPEEPS randomized controlled trial: a pilot of preliminary efficacy, feasibility, and acceptability of a group‐level, HIV risk reduction intervention for young men who have sex with men. Archives of Sexual Behavior 2015;44(2):475‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hill 2014 {published data only}
- Hill KG, Bailey JA, Hawkins JD, Catalano RF, Kosterman R, Oesterle S, et al. The onset of STI diagnosis through age 30: results from the Seattle Social Development Project intervention. Prevention Science 2014;15(1):19‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jemmott 2010 {published data only}
- Jemmott JB 3rd, Jemmott LS, Fong GT. Efficacy of a theory‐based abstinence‐only intervention over 24 months: a randomized controlled trial with young adolescents. JAMA Pediatrics 2010;164(2):152‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jewkes 2008 {published data only}
- Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, et al. Impact of stepping stones on incidence of HIV and HSV‐2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ 2008;337:a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kennedy 2014 {published data only}
- Kennedy CE, Brahmbhatt H, Likindikoki S, Beckham SW, Mbwambo JK, Kerrigan D. Exploring the potential of a conditional cash transfer intervention to reduce HIV risk among young women in Iringa, Tanzania. AIDS Care 2014;26(3):275‐81. [DOI] [PubMed] [Google Scholar]
Kirby 1997 {published data only}
- Kirby D, Korpi M, Barth RP, Cagampang HH. The impact of the Postponing Sexual Involvement Curriculum among youths in California. Family Planning Perspectives 2007;29(3):100‐8. [PubMed] [Google Scholar]
Langley 2015 {published data only}
- Langley C, Barbee AP, Antle B, Christensen D, Archuleta A, Bibhuti KS, et al. Enhancement of reducing the risk for the 21st century: improvement to a curriculum developed to prevent teen pregnancy and STI transmission. American Journal of Sexuality Education 2015;10(1):40‐69. [Google Scholar]
Li 2008 {published data only}
- Li X, Stanton B, Wang B, Mao R, Zhang H, Qu M, et al. Cultural adaptation of the focus on kids program for college students in China. AIDS Education and Prevention 2008;20(1):1‐14. [DOI] [PubMed] [Google Scholar]
Markham 2012 {published data only}
- Markham CM, Tortolero SR, Peskin MF, Shegog R, Thiel M, Baumler ER, et al. Sexual risk avoidance and sexual risk reduction interventions for middle school youth: a randomized controlled trial. Journal of Adolescent Health 2012;50(3):279‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marsch 2015 {published data only}
- Marsch LA, Guarino H, Grabinski MJ, Syckes MA, Dillingham ET, Xie H, et cal. Comparative effectiveness of web‐based vs. educator‐delivered HIV prevention for adolescent substance users: a randomized, controlled trial. Journal of Substance Abuse Treatment 2015;59:30‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mathews 2015 {published data only}
- Mathews C, Eggers SM, Vries PJ, Mason‐Jones AJ, Townsend L, Aaro LE, et al. Reaching the hard to reach: longitudinal investigation of adolescents' attendance at an after‐school sexual and reproductive health programme in Western Cape, South Africa. BMC Public Health 2015;15:608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mavedzenge 2011 {published data only}
- Mavedzenge SMN, Doyle AM, Ross DA. HIV prevention in young people in sub‐Saharan Africa: a systematic review. Journal of Adolescent Health 2011;49(6):568‐586. [DOI] [PubMed] [Google Scholar]
Mellanby 2000 {published data only}
- Mellanby AR, Rees JB, Tripp JH. Peer‐led and adult‐led school health education: a critical review of available comparative research. Health Education Research 2000;15(5):533‐45. [DOI] [PubMed] [Google Scholar]
Michielsen 2010 {published data only}
- Michielsen K, Chersich MF, Luchters S, Koker P, Rossem R, Temmerman M. Effectiveness of HIV prevention for youth in sub‐Saharan Africa: systematic review and meta‐analysis of randomized and nonrandomized trials. AIDS 2010;24(8):1193‐202. [DOI] [PubMed] [Google Scholar]
Morales 2016 {published data only}
- Morales A, Espada JP, Orgiles M. A 1‐year follow‐up evaluation of a sexual‐health education program for Spanish adolescents compared with a well‐established program. European Journal of Public Health 2016;26(1):35‐41. [DOI] [PubMed] [Google Scholar]
Morrison 2007 {published data only}
- Morrison DM, Casey EA, Beadnell BA, Hoppe MJ, Gillmore MR, Wilsdon A, et al. Effects of friendship closeness in an adolescent group HIV prevention intervention. Prevention Science 2007;8(4):274‐84. [DOI] [PubMed] [Google Scholar]
Namisi 2013 {published data only}
- Namisi FS, Aarø LE, Kaaya S, Onya HE, Wubs A, Mathews C. Condom use and sexuality communication with adults: a study among high school students in South Africa and Tanzania. BMC Public Health 2013;13:874. [DOI] [PMC free article] [PubMed] [Google Scholar]
Newby 2013 {published data only}
- Newby KV, French DP, Brown KE, Lecky DM. Increasing young adults' condom use intentions and behaviour through changing chlamydia risk and coping appraisals: study protocol for a cluster randomised controlled trial of efficacy. BMC Public Health 2013;13:528. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oringanje 2016 {published data only}
- Oringanje C, Meremikwu MM, Eko E, Meremikwu A, Ehiri JE. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database of Systematic Reviews 2016, Issue 2. [DOI: 10.1002/14651858.CD005215.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Paul‐Ebhohimhen 2008 {published data only}
- Paul‐Ebhohimhen VA, Poobalan A, Teijlingen ER. A systematic review of school‐based sexual health interventions to prevent STI/HIV in sub‐Saharan Africa. BMC Public Health 2008;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pedlow 2003 {published data only}
- Pedlow CT, Carey MP. HIV sexual risk‐reduction interventions for youth: a review and methodological critique of randomized controlled trials. Behavior Modification 2003;27(2):135‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peskin 2015 {published data only}
- Peskin MF, Shegog R, Markham CM, Thiel M, Baumler ER, Addy RC, et al. Efficacy of It's Your Game‐Tech: a computer‐based sexual health education program for middle school youth. Journal of Adolescent Health 2015;56(5):515‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pettifor 2015 {published data only}
- Pettifor A, MacPhail C, Selin A, Gomez‐Olive X, Hughes J, Wagner R, et al. HPTN 068 conditional cash transfer to prevent HIV infection among young women in South Africa: results of a randomized controlled trial. Journal of the International AIDS Society 2015;18:45‐6. [Google Scholar]
Picot 2012 {published data only}
- Picot J, Shepherd J, Kavanagh J, Cooper K, Harden A, Barnett‐Page E, et al. Behavioural Interventions for the prevention of sexually transmitted infections in young people aged 13‐19 years: a systematic review. Health Education Research 2012;27(3):495‐512. [DOI] [PubMed] [Google Scholar]
Prado 2007 {published data only}
- Prado G, Pantin H, Briones E, Schwartz SJ, Feaster D, Huang S, et al. A randomized controlled trial of a parent‐centered intervention in preventing substance use and HIV risk behaviors in Hispanic adolescents. Journal of Consulting and Clinical Psychology 2007;75(6):914. [DOI] [PMC free article] [PubMed] [Google Scholar]
Raiford 2014 {published data only}
- Raiford JL, Herbst JH, Carry M, Browne FA, Doherty I, Wechsberg WM. Low prospects and high risk: structural determinants of health associated with sexual risk among young African American women residing in resource‐poor communities in the south. American Journal of Community Psychology 2014;54(3‐4):243‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reyna 2014 {published data only}
- Reyna VF, Mills BA. Theoretically motivated interventions for reducing sexual risk taking in adolescence: a randomized controlled experiment applying fuzzy‐trace theory. Journal of Experimental Psychology. General 2014;143(4):1627‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rohrbach 2015 {published data only}
- Rohrbach LA, Berglas NF, Jerman P, Angulo‐Olaiz F, Chou CP, Constantine NA. A rights‐based sexuality education curriculum for adolescents: 1‐year outcomes from a cluster‐randomized trial. Journal of Adolescent Health 2015;57(4):399‐406. [DOI] [PubMed] [Google Scholar]
Ross 2010 {published data only}
- Ross DA. Behavioural interventions to reduce HIV risk: what works?. AIDS 2010;24(Suppl 4):S4‐14. [DOI] [PubMed] [Google Scholar]
Sanci 2015 {published data only}
- Sanci L, Chondros P, Sawyer S, Pirkis J, Ozer E, Hegarty K, et al. Responding to young people's health risks in primary care: a cluster randomised trial of training clinicians in screening and motivational interviewing. PLoS ONE 2015;10(9):e0137581. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shahmanesh 2008 {published data only}
- Shahmanesh M, Patel V, Mabey D, Cowan F. Effectiveness of interventions for the prevention of HIV and other sexually transmitted infections in female sex workers in resource poor setting: a systematic review. Tropical Medicine & International Health 2008;13(5):659‐79. [DOI] [PubMed] [Google Scholar]
Shepherd 2010 {published data only}
- Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett‐Page E, et al. The effectiveness and cost‐effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13‐19: a systematic review and economic evaluation. Health Technology Assessment 2010;14(7):1‐230. [DOI] [PubMed] [Google Scholar]
Simmons 2015 {published data only}
- Simmons N, Donnell D, Ou SS, Celentano DD, Aramrattana A, Davis‐Vogel A, et al. Assessment of contamination and misclassification biases in a randomized controlled trial of a social network peer education intervention to reduce HIV risk behaviors among drug users and risk partners in Philadelphia, PA and Chiang Mai, Thailand. AIDS and Behavior 2015;19(10):1818‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spoth 2014 {published data only}
- Spoth R, Clair S, Trudeau L. Universal family‐focused intervention with young adolescents: effects on health‐risking sexual behaviors and STDs among young adults. Prevention Science 2014;15(1):47‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stanton 2015 {published data only}
- Stanton B, Wang B, Deveaux L, Lunn S, Rolle G, Li X, et al. Assessing the effects of a complementary parent intervention and prior exposure to a preadolescent program of HIV risk reduction for mid‐adolescents. American Journal of Public Health 2015;57(4):399‐406. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stephenson 1998 {published data only}
- Stephenson JM, Oakley A, Charleston S, Brodala A, Fenton K, Petruckevitch A, et al. Behavioural intervention trials for HIV/STD prevention in schools: are they feasible?. Sexually Transmitted Infections 1998;74(6):405‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tingey 2015 {published data only}
- Tingey L, Mullany B, Chambers R, Hastings R, Barlow A, Rompalo A. The Respecting the Circle of Life trial for American Indian adolescents: rationale, design, methods, and baseline characteristics. AIDS Care 2015;27(7):885‐91. [DOI] [PubMed] [Google Scholar]
Tortolero 2010 {published data only}
- Tortolero SR, Markham CM, Peskin MF, Shegog R, Addy RC, Escobar‐Chaves LE, et al. It's Your Game: Keep It Real: delaying sexual behavior with an effective middle school program. Journal of Adolescent Health 2010;46(2):169‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Underhill 2007 {published data only}
- Underhill K, Operario D, Montgomery P. Systematic review of abstinence‐plus HIV prevention programs in high‐income countries. PLoS Medicine 2007;4(9):e275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2014 {published data only}
- Wang B, Stanton B, Deveaux L, Li X, Koci V, Lunn S. The impact of parent involvement in an effective adolescent risk reduction intervention on sexual risk communication and adolescent outcomes. AIDS Education and Prevention 2014;26(6):500‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weiss 2008 {published data only}
- Weiss HA, Wasserheit JN, Barnabas RV, Hayes RJ, Abu‐Raddad LJ. Persisting with prevention: the importance of adherence for HIV prevention. Emerging Themes in Epidemiology 2008;5(8):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2015 {published data only}
- Zhang J, Jemmott JB, Jemmott LS. Mediation and moderation of an efficacious theory‐based abstinence‐only intervention for African American adolescents. Health Psychology 2015;34(12):1175‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zimmerman 2008 {published data only}
- Zimmerman RS, Cupp PK, Donohew L, Kristin Sionéan C, Feist‐Price S, Helme D. Effects of a school‐based, theory‐driven HIV and pregnancy prevention curriculum. Perspectives on Sexual and Reproductive Health 2008;40(1):42‐51. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN56270821 {published data only}
- ISRCTN56270821. Preventing sexual risk behavior and partner violence among adolescents in Cape Town. isrctn.com/ISRCTN56270821 (first received 7 January 2013).
NCT01187979 {published data only}
- NCT01187979. Reducing HIV in adolescents (RHIVA) [A proof of concept cluster randomised controlled trial to evaluate the impact of a cash incentivised prevention intervention to reduce HIV infection in high school learners in rural KwaZulu‐Natal, South Africa]. clinicaltrials.gov/ct2/show/NCT01187979?term=abdool+karim&rank=4 (first received 12 August 2010).
NCT01233531 {published data only}
- NCT01233531. Effects of cash transfer for the prevention of HIV in young South African women. clinicaltrials.gov/ct2/show/NCT01233531?term=hptn+068&rank=1 (first received 1 November 2010).
NCT02455583 {published data only}
- NCT02455583. An assessment of an HIV prevention intervention (Project AIM) on youth sexual intentions, sexual behaviors and HSV‐2 incidence and prevalence in junior secondary schools in Eastern Botswana. clinicaltrials.gov/ct2/show/NCT02455583 (first received 6 January 2015).
NCT02665091 {published data only}
- NCT02665091. Peer education program for HIV/AIDS related sexual behaviors of secondary school students [Impact of peer education program on HIV/AIDS related sexual behaviors of secondary school students in rural communities, India: a quasi‐experimental study.]. clinicaltrials.gov/ct2/show/record/NCT02665091 (first received 22 January 2016).
Additional references
Abrahams 2006
- Abrahams N, Mathews S, Ramela P. Intersections of 'sanitation, sexual coercion and girls' safety' in schools. Tropical Medicine and International Health 2006;11(5):751‐6. [DOI] [PubMed] [Google Scholar]
Baird 2009
- Baird S, Chirwa E, McIntosh C, Ozler B. The short‐term impacts of a schooling conditional cash transfer program on the sexual behavior of young women. Health Economics 2010;19 Suppl:55‐68. [DOI] [PubMed] [Google Scholar]
Baird 2010
- Baird S, McIntosh G, Ozler B. Cash or Condition? Evidence from a Cash Transfer Experiment. Policy Research Working Paper 5259. The World Bank Development Research Group Poverty and Inequality Team 2010:1‐42.
Bandura 1977
- Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hill, 1977. [Google Scholar]
Bennet 2005
- Bennett SE, Assefi NP. School‐based teenage pregnancy prevention programs: a systematic review of randomized controlled trials. Journal of Adolescent Health 2005;36(1):72‐81. [DOI] [PubMed] [Google Scholar]
Black 2008
- Black SE, Devereux PJ, Salvanes KG. Staying in the classroom and out of the maternity ward? The effect of compulsory schooling laws on teenage births. Economic Journal 2008;118(530):1025‐54. [Google Scholar]
Brown 2015
- Brown JL, DiClemente RJ. The need for biological outcomes to complement self‐report in adolescent research. Pediatrics 2015;136(3):e551‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carrasco‐Labra 2015
- Carrasco‐Labra A, Brignardello‐Peetersen R, Santesso N, Neumann I, Mustafa RA, Mbuagbaw L, et al. Comparison between the standard and a new alternative format of the Summary‐of‐Findings tables in Cochrane review users: study protocol for a randomized controlled trial. Trials 2015;16:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chandra‐Mouli 2015
- Chandra‐Mouli V, Lane C, Wong S. What does not work in adolescent sexual and reproductive health: a review of evidence on interventions commonly accepted as best practices. Global Health: Science and Practice 2015;3(3):333‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chin 2012
- Chin HB, Sipe TA, Elder R, Mercer SL, Chattopadhyay SK, Jacob V, et al. The effectiveness of group‐based comprehensive risk reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus and sexually transmitted infections. Two systematic reviews for the guide to community preventive services. American Journal of Preventive Medicine 2012;42(3):272‐94. [DOI] [PubMed] [Google Scholar]
Cowan 2008
- Cowan FM, Pascoe SJS, Langhaug LF, Dirawo J, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri Project: a cluster randomised controlled trial to determine the effectiveness of a multi‐component community‐based HIV prevention intervention for rural youth in Zimbabwe ‐ study design and baseline results. Tropical Medicine and International Health 2008;13(10):1235‐44. [DOI] [PubMed] [Google Scholar]
Dhairyawan 2013
- Dhairyawan R, Tariq S, Scourse R, Coyne KM. Intimate partner violence in women living with HIV attending an inner city clinic in the UK: prevalence and associated factors. HIV Medicine 2013;14(5):303‐10. [DOI] [PubMed] [Google Scholar]
DiCenso 2002
- DiCenso A, Guyatt G, Willan A, Griffith L. Interventions to reduce unintended pregnancies among adolescents: systematic review of randomised controlled trials. BMJ 2002;324(7351):1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dick 2006
- Dick B, Ferguson J, Ross DA. Preventing HIV/AIDS in young people. A systematic review of the evidence from developing countries. Introduction and rationale. World Health Organization Technical Report Series 2006;938:1‐13, 317‐41. [PubMed] [Google Scholar]
DiClemente 2008
- DiClemente RJ, Crittenden CP, Rose E, Sales JM, Wingood GM, Crosby RA, et al. Psychosocial predictors of HIV‐related sexual behaviours and the efficacy of prevention interventions in adolescents at‐risk for HIV infection: what works and what doesn't work?. Psychosomatic Medicine 2008;70:598‐605. [DOI] [PubMed] [Google Scholar]
Fishbein 2010
- Fishbein M, Asjen I. Predicting and changing behavior. The reasoned action approach. New York (NY): Taylor & Francis, 2010. [Google Scholar]
Flisher 2008
- Flisher AJ, Mukoma W, Louw J. Evaluating adolescent sexual and reproductive health interventions in Southern and Eastern Africa. In: Klepp KI, Flisher AJ, Kaaya SF editor(s). Promoting adolescent sexual and reproductive health in east and southern Africa. The Nordic Africa Institute, 2008:249‐66. [Google Scholar]
Fonner 2014
- Fonner VA, Armstrong KS, Kennedy CE, O'Reilly KR, Sweat M. School‐based sex education and HIV prevention in low‐ and middle‐income countries: a systematic review and meta‐analysis. PLoS ONE 2014;9(3):e89692. [DOI] [PMC free article] [PubMed] [Google Scholar]
Freudenberg 2007
- Freudenberg N, Ruglis J. Reframing school dropout as a public health issue. Preventing chronic disease. Public health research, practice and policy 2007;4(4):1‐11. [PMC free article] [PubMed] [Google Scholar]
Gallant 2004
- Gallant M, Maticka‐Tyndale E. School‐based HIV prevention programmes for African youth. Social Science and Medicine 2004;58(7):1337‐51. [DOI] [PubMed] [Google Scholar]
Garcia‐Moreno 2013
- Garcia‐Moreno C, Palitto C, Devries K, Stockl H, Watts C, Abrahams N. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non‐partner sexual violence. Geneva: Word Health Organization, 2013. [Google Scholar]
Glanz 2010
- Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health 2010;31(1):399‐418. [DOI] [PubMed] [Google Scholar]
GRADEpro 2014 [Computer program]
- GRADE Working Group, McMaster University. GRADEpro GDT. Version accessed July 2015. Hamilton (ON): GRADE Working Group, McMaster University, 2014.
Grimes 2006
- Grimes DA, Benson J, Singh S, Romero M, Ganatra B, Okonofua FE, et al. Unsafe abortion: the preventable pandemic. Lancet 2006;368(9550):1908‐19. [DOI] [PubMed] [Google Scholar]
Hadley 2016
- Hadley A, Chandra‐Mouli V, Ingham G. Implementing the United Kingdom Government's 10‐year teenage pregnancy strategy for England (1999‐2010): applicable lessons for other countries. Journal of Adolescent Health 2016;59(1):68‐74. [DOI] [PubMed] [Google Scholar]
Harrison 2005
- Harrison A, Cleland J, Gouws E, Frohlich J. Early sexual debut among young men in rural South Africa: heightened vulnerability to sexual risk?. Sexually Transmitted Infections 2005;81(3):259‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harrison 2010
- Harrison A, Newell M‐L, Imrie J, Hoddinott G. HIV prevention for South African youth: which interventions work? A systematic review of current evidence. BMC Public Health 2010;10:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayes 2005
- Hayes RJ, Changalucha J, Ross DA, Gavyole A, Todd J, Obasi AI, et al. The MEMA kwa Vijana project: design of a community randomised trial of an innovative adolescent sexual health intervention in rural Tanzania. Contemporary Clinical Trials 2005;26(4):430‐42. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Imamura 2007
- Imamura M, Tucker J, Hannaford P, Oliveira da Silva M, Astin M, Wyness L, et al. Factors associated with teenage pregnancy in the European Union countries: a systematic review. European Journal of Public Health 2007;17(6):630‐6. [DOI] [PubMed] [Google Scholar]
Johnson 2003
- Johnson BT, Carey MP, Marsh KL, Levin KD, Scott‐Sheldon LA. Interventions to reduce sexual risk for the human immunodeficiency virus in adolescents. Archives of Pediatric and Adolescent Medicine 2003;157(4):381‐8. [DOI] [PubMed] [Google Scholar]
Johnson, 2011
- Johnson BT, Scott‐Sheldon LA, Huedo‐Medina TB, Carey MP. Interventions to reduce sexual risk for human immunodeficiency virus in adolescents: a meta‐analysis of trials, 1985‐2008. Archives of Pediatric and Adolescent Medicine 2011;165(1):77‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaplan 2007
- Kaplan I, Lewis I, Mumba P. Picturing global educational inclusion? Looking and thinking across students photographs from the UK, Zambia and Indonesia. Journal of Research in Special Educational Needs 2007;7:23‐35. [Google Scholar]
Katz 2015
- Katz J, Poleshuck EL, Beach B, Olin R. Reproductive coercion by male sexual partners associations with partner violence and college women’s sexual health. Journal of Interpersonal Violence 2015 Aug 5 [Epub ahead of print]. [DOI: 10.1177/0886260515597441] [DOI] [PMC free article] [PubMed]
Kim 2008
- Kim CR, Free C. Recent evaluations of the peer‐led approach In adolescent sexual health education: a systematic review. International Family Planning Perspectives 2008;34(2):89‐96. [DOI] [PubMed] [Google Scholar]
Kirby 2006
- Kirby D, Obasi A, Laris BA. The effectiveness of sex education and HIV education interventions in schools in developing countries. In: Ross D, Dick B, Ferguson J editor(s). Preventing HIV/AIDS in young people : a systematic review of the evidence from developing countries : UNAIDS interagency task team on HIV and young people. World Health Organization, 2006. [PubMed] [Google Scholar]
Kirby 2007
- Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: their impact on sexual behaviors of young people throughout the world. Journal of Adolescent Health 2007;40(3):206‐17. [DOI] [PubMed] [Google Scholar]
Kirby 2009
- Kirby D, Laris BA. Effective curriculum‐based sex and STD/HIV education programs for adolescents. Child Development Perspectives 2009;2:210‐9. [Google Scholar]
Langhaug 2011
- Langhaug LF, Cheung YB, Pascoe SJ, Chirawu P, Woelk G, Hayes RJ, et al. How you ask really matters: randomised comparison of four sexual behaviour questionnaire delivery modes in Zimbabwean youth. Sexually Transmitted Infections 2011;87(2):165‐73. [DOI] [PubMed] [Google Scholar]
Laud 2016
- Laud AD. The efficacy of HIV and sex education interventions among youths in developing countries: a review. Public Health Research 2016;6(1):1‐17. [Google Scholar]
Lazarus 2010
- Lazarus JV, Sihvonen‐Riemenschneider H, Laukamm‐Josten U, Wong F, Liljestrand J. Systematic review of interventions to prevent the spread of sexually transmitted infections, including HIV, among young people in Europe. Croatian Medical Journal 2010;51(1):74‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lopez 2016
- Lopez LM, Bernholc A, Chen M, Tolley EE. School‐based interventions for improving contraceptive use in adolescents. Cochrane Database of Systematic Reviews 2016, Issue 6. [DOI: 10.1002/14651858.CD012249] [DOI] [PMC free article] [PubMed] [Google Scholar]
Magnussen 2004
- Magnussen L, Ehiri JE, Jolly PE. Interventions to prevent HIV/AIDS among adolescents in less developed countries: are they effective?. International Journal of Adolescent Medicine and Health 2004;16(4):303‐23. [DOI] [PubMed] [Google Scholar]
Mason‐Jones 2012
- Mason‐Jones AJ, Crisp C, Momberg M, Koech J, Koker P, Mathews C. A systematic review of the role of school‐based healthcare in adolescent sexual, reproductive, and mental health. Systematic Reviews 2012;1:49. [DOI: 10.1186/2046-4053-1-49] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mathews 2009
- Mathews C, Aaro LE, Flisher AJ, Mukoma W, Wubs AG, Schaalma H. Predictors of early first sexual intercourse among adolescents in Cape Town, South Africa. Health Education Research 2009;24(1):1‐10. [DOI] [PubMed] [Google Scholar]
Mavedzenge 2013
- Mavedzenge SN, Luecke E, Ross DA. Technical brief. Effectiveness of HIV Prevention, Treatment and Care Interventions Among Adolescents: A Systematic Review of Systematic Reviews. September 2013. http://dutblogs.dut.ac.za/hivaids/wp‐content/uploads/2013/10/Systematic‐Review‐Effective‐HIV‐Response‐in‐Adolescents‐2013.pdf (accessed 10 March 2015).
McKenzie 2014
- McKenzie J, Ryan R, Tanna GL. Cochrane Consumers and Communication Review Group: cluster randomised controlled trials. March 2014. https://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/uploads/ClusterRCTs.pdf (accessed 30 June 2016).
Medley 2009
- Medley A, Kennedy C, O'Reilly K, Sweat M. Effectiveness of peer education interventions for HIV prevention in developing countries: a systematic review and meta‐analysis. AIDS Education and Prevention 2009;21(3):181‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2010
- Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception 2010;81(4):316‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Monstad 2008
- Monstad K, Propper C, Salvanes KG. Education and fertility: evidence from a natural experiment. Scandinavian Journal of Economics 2008;110(4):827‐52. [Google Scholar]
Pallitto 2005
- Pallitto CC, Campbell JC, O’Campo P. Is intimate partner violence associated with unintended pregnancy? A review of the literature. Trauma, Violence & Abuse 2005;6(3):217‐35. [DOI] [PubMed] [Google Scholar]
Paul 2008
- Paul‐Ebhohimhen VA, Poobalan A, Teijlingen ER. A systematic review of school‐based sexual health interventions to prevent STI/HIV in sub‐Saharan Africa. BMC Public Health 2008;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pettifor 2005
- Pettifor AE, Rees HV, Kleinschmidt I, Steffenson AE, MacPhail C, Hlongwa‐Madikizela L, et al. Young people's sexual health in South Africa: HIV prevalence and sexual behaviours from a nationally representative household survey. AIDS 2005;19(14):1525‐34. [DOI] [PubMed] [Google Scholar]
Pettifor 2012
- Pettifor A, MacPhail C, Nguyen N, Rosenberg M. Can money prevent the spread of HIV? A review of cash payments for HIV prevention. AIDS and Behavior 2012;16(7):1729‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pettifor 2016
- Pettifor A, MacPhail C, Selin A, Xavier Gomez‐Olive F, Rosenburg M, Wagner RG, the HPTN 068 protocol team. HPTN 068: a randomized control trial of a conditional cash transfer to reduce HIV infection in young women in South Africa ‐ study design and baseline results. AIDS and Behavior 2016;20(9):1863‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Plummer 2004
- Plummer ML, Ross DA, Wight D, Changalucha J, Mshana G, Wamoyi J, et al. A bit more truthful: the validity of adolescent sexual behaviour data collected in rural northern Tanzania using five methods. Sexually Transmitted Infections 2004;80 Suppl 2:ii49‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Plummer 2007
- Plummer ML, Wight D, Wamoyi J, Nyalali K, Ingall T, Mshana G, et al. Are schools a good setting for adolescent sexual health promotion in rural Africa? A qualitative assessment from Tanzania. Health Education Research 2007;22(4):483‐99. [DOI] [PubMed] [Google Scholar]
Rao 1992
- Rao JN, Scott AJ. A simple method for the analysis of clustered binary data. Biometrics 1992;48(2):577‐85. [PubMed] [Google Scholar]
Review Manager 5.3 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rosenstock 1988
- Rosenstock IM, Strecher VJ, Becker MH. Social Learning Theory and the Health Belief Model. Health Education & Behavior 1988;15(2):175‐83. [DOI] [PubMed] [Google Scholar]
Shah 2010
- Shah PS, Shah J. Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta‐analyses. Journal of Women's Health 2010;19(11):2017‐31. [DOI] [PubMed] [Google Scholar]
Stephenson 2004
- Stephenson JM, Strange V, Forrest S, Oakley A, Copas A, Allen E, et al. and the RIPPLE study team. Pupil‐led sex education in England (RIPPLE study): cluster‐randomised intervention trial. Lancet 2004;364(9431):338‐46. [DOI] [PubMed] [Google Scholar]
Thiel de Bocanegra 2010
- Thiel de Bocanegra H, Rostovtseva DP, Khera S, Godhwani N. Birth control sabotage and forced sex: experiences reported by women in domestic violence shelters. Violence Against Women 2010;16(5):601‐12. [DOI] [PubMed] [Google Scholar]
UNAIDS 1997
- UNAIDS. Impact of HIV and sexual health education on the sexual behaviour of young people: a review update. Geneva: UNAIDS, 1997. [Google Scholar]
UNAIDS 2012
- UNAIDS. Report on the global AIDS epidemic. Geneva: UNAIDS, 2012. [Google Scholar]
Underhill 2008
- Underhill K, Operario D, Montgomery P. Abstinence‐only programs for HIV infection prevention in high‐income countries. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD007006] [DOI] [PubMed] [Google Scholar]
United Nations 2015
- United Nations. Sustainable Development Goals 2015. https://sustainabledevelopment.un.org/ (accessed 10 October 2015).
Walsh 2015
- Walsh K, Zwi K, Woolfenden S, Shlonksy A. School‐based education programmes for the prevention of child sexual abuse. Cochrane Database of Systematic Reviews 2015, Issue 4. [DOI: 10.1002/14651858.CD004380.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wight 2002
- Wight D, Raab GM, Henderson M, Abraham C, Buston K, Hart G, et al. Limits of teacher delivered sex education: interim behavioural outcomes from randomised trial. BMJ 2002;324(7351):1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
World Bank 2016
- World Bank. Adolescent fertility rate (births per 1000 women ages 15‐19). http://data.worldbank.org/indicator/SP.ADO.TFRT (accessed 3 August 2016).
World Health Organization 2014
- WHO. Global Health Estimates 2013 Summary tables: DALYs, YLLs and YLDs by cause, age and sex by HWO regional group and World Bank income classification, 2000‐2012. http://www.who.int/healthinfo/global_burden_disease/en/. Geneva, (accessed 10 October 2014).
Yankah 2008
- Yankah E, Aggleton P. Effects and effectiveness of life skills education for HIV prevention in young people. AIDS Education and Prevention 2008;20(6):465‐85. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Mason‐Jones 2011
- Mason‐Jones AJ, Mathews C, Kagee A, Lombard C. Clinical effectiveness of school and mixed school and community based interventions for STI and HIV prevention in adolescents. Cochrane Database of Systematic Reviews 2011, Issue 11. [DOI: 10.1002/14651858.CD006417.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mukoma 2007
- Mukoma W, Kagee A, Flisher AJ, Mathews C. School‐based interventions to postpone sexual intercourse and promote condom use among adolescents. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD006417] [DOI] [Google Scholar]


