Abstract
Objective
Studies of aging usually focus on trajectories of physical and cognitive function, with far less emphasis on overall mental health, despite its impact on general health and mortality. This study examined linear and non-linear trends of physical, cognitive, and mental health over the entire adult lifespan.
Method
Cross-sectional data were obtained from 1,546 individuals aged 21 to 100 years, selected using random digit dialing for the Successful AGing Evaluation (SAGE) study, a structured multi-cohort investigation, that included telephone interviews and in-home surveys of community-based adults without dementia. Data were collected from 1/26/2010 to 10/07/2011 targeting participants aged 50 to 100 years, and 6/25/2012 to 7/15/2013 targeting participants aged 21 to 50 years. Data included self-report measures of physical health, measures of both positive and negative attributes of mental health, and a phone interview-based measure of cognition.
Results
Comparison of age cohorts using polynomial regression suggested a possible accelerated deterioration in physical and cognitive functioning, averaging one-and-a-half to two standard deviations over the adult lifespan. In contrast, there appeared to be a linear improvement of about one standard deviation in various attributes of mental health over the same life period.
Conclusion
These cross-sectional findings suggest the possibility of a linear improvement in mental health beginning in young adulthood rather than a U-shaped curve reported in some prior studies. Lifespan research combining psychosocial and biological markers may improve our understanding of resilience to mental disability in older age, and lead to broad-based interventions promoting mental health in all age groups.
INTRODUCTION
Traditionally, aging has been conceptualized as an ongoing process of physical and cognitive decline, with far less emphasis on mental health. Yet, in a recent national poll, 89% of American adults reported that mental health was as important as physical health.1. Impaired mental health can adversely impact self-care and is a leading cause of disability.2 Furthermore, untreated mental health problems often have a deleterious effect on physical health.3
Although mental health of older people might be assumed to follow a deteriorating course in step with worsening physical and cognitive function, findings regarding subjective well-being have been mixed.4,5 Some investigators find a U-shaped curve of well-being across the lifespan, with declines from early adulthood to middle age followed by improvement during later adulthood.6–8 Other studies report contradictory findings,9–11 including increase, decline, or flat trajectory of psychological well-being across early adulthood. Charles et al.10 showed declines in negative affect while positive affect remained stable. Vaillant and Blazer have described successful cognitive and emotional aging in specific groups of older adults.12–16 The reasons for differences in results are not obvious. Springer et al. suggest changes in well-being with ages may be due to measurement variation across studies,17 with many studies focusing on single domains of physical18,19 or cognitive health20 or on single indicators of mental health such as psychological well-being.
Psychological well-being21 should be distinguished from the multidimensional construct of mental health, which also includes perceived stress and absence of anxiety and depressive symptoms. The effects of age may vary depending on the specific domain(s) assessed. In one study,7 happiness, enjoyment, and the inverse of sadness were all U-shaped, while stress, worry, and anger showed apparent improvements with aging.7 Thus, the empirical literature is inconsistent regarding the pattern of change in mental health across the adult lifespan.
Epidemiologic studies have reported lower prevalence of all mental illnesses, except for neurocognitive disorders, in older adults.22–25 The reasons remain unclear. Common explanations include inappropriate diagnostic criteria for geriatric mental disorders, older patients’ reluctance or inability (due to memory difficulties) to report mental problems, and mis-attribution of psychological symptoms to physical illnesses.26 However, survivor effects also may play a role – i.e., the adults who survive into older age may have better mental health than younger counterparts. Additional studies of aging, using validated measures of broadly defined mental health along with physical and cognitive functioning across the adult lifespan, are needed.
We simultaneously examined physical health, cognitive function, and several measures of mental health across the adult lifespan (age 21–100 years) in a community sample. Unlike many studies using samples of convenience, we obtained a sample in San Diego County, California, using random digit dialing, with nearly equal numbers of men and women, stratified by age decade, and an oversampling of adults over age 75. We hypothesized that while physical and cognitive function would be lower among successively older age cohorts, mental health would follow a non-linear, U-shaped trend, with middle-aged cohorts evidencing the worst mental health relative to younger and older cohorts.
METHODS
Participants
Participants included 1,546 community-dwelling adults from the University of California (UC) San Diego Successful AGing Evaluation (SAGE) study.27 A structured multi-cohort design was used to recruit residents of San Diego County. The study originally targeted adults aged 50–100 years, but subsequently we added participants aged 21–50 years. Partial data in adults age 50+ have been reported previously27,28 in regard to self-perceived successful aging, but this report represents our first examination of the life-span trajectory of physical, cognitive, and mental health in the entire age range. Exclusion criteria were: 1) residence in a nursing home or need for daily skilled nursing care, 2) self-reported prior diagnosis of dementia, 3) terminal illness or need for hospice care, and 4) inability to understand written or spoken English. Participants who completed a 25-minute structured telephone interview, that included cognitive assessment, were subsequently mailed a survey questionnaire that asked for detailed demographic and clinical information and included a number of rating scales and other measures. The enrollment sequence is depicted in Supplemental (on-line only) Figure 1. Participants were compensated $10 for their participation in the phone interview and $15 for the completion of their baseline SAGE Survey. The study was approved by UC San Diego, Human Research Protections Program.
Measures
Physical health
This construct was operationally defined as a composite of self-reported Physical Functioning, Role-Physical, Bodily Pain, and General Health subscale total scores from the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36).29,30 Subjects rated themselves on both the presence of good (or poor) health and its functional consequences. To create the composite, we standardized scores from each subscale, computed the average value, and then standardized the outcome (z-scores). Unlike the manual-based scoring method for the SF-36 - which includes both physical and mental health subscale scores to determine the physical health composite, our composite was composed of physical health subscales only, in order to operationalize physical health independently of mental health. The internal consistency of the modified physical composite was high (α=0.81) and variance was dominated by a general factor (ωh=0.75).
Cognitive function
This was assessed by total scores on the Telephone Interview of Cognitive Status - Modified (TICS-M).31 TICS-M scores are documented as having good convergent31 and discriminant32 validity.
Mental health
This construct was operationally defined as a composite of 3 measures reflecting positive and 3 reflecting negative attributes. Measures reflecting positive attributes included total scores on the Happiness Subscale33 of the Center for Epidemiological Studies – Depression scale (CES-D); the Satisfaction with Life Scale;34 and a composite of Vitality, Social Functioning, Role-Emotional, and Mental Health subscale total scores from the SF-36.29 Negative attributes were assessed with total scores on the Brief Symptom Inventory Anxiety Scale;35 Patient Health Questionnaire Depression Module (PHQ-9);36 and Perceived Stress Scale.37,38 We created the mental health composite by standardizing the scores reflecting 3 positive and 3 negative psychological attributes, calculating the average value (with negative attributes weighted by −1), and then standardizing the outcome. The internal consistency of the composite was high (α=0.87) and variance was dominated by a general factor (ωh=0.82).
Analyses
To evaluate aging-associated trends in physical, cognitive, and mental health, we fitted power polynomial regression models to each construct.39 These models sought to determine whether, and how, the relationship between age and each construct was linear or nonlinear. We hierarchically compared models that included linear, linear and quadratic, or linear, quadratic, and cubic effects of (centered) age. Polynomial terms allow nonlinear curves or bends in the relationship between variables. Models with linear terms allow zero bends, models with linear and a single nonlinear (quadratic) term allow one bend, and models with linear and two nonlinear (quadratic and cubic) terms allow two bends. The linear term indicates whether the relationship between variables generally rises or falls; the nonlinear (quadratic and cubic) terms indicate whether the bends are concave upward or downward. All models also included gender and marital status (contrast coded), and education (linear trend coded).40 Additionally, we assessed age effects for each scale contributing to the mental health composite. Models were compared using likelihood ratio tests. Effect size was quantified in terms of increment in variance accounted for (ΔR2) comparing nested models. All analyses were conducted using R.41
RESULTS
Participant Characteristics
Mean age was 66 years (SD=21; range=21–99), and 51% were men. Highest level of education completed was ≤12 years for 20%, 13–16 years (Bachelor’s degree) for 60%, and post-graduate education for 21% of the sample. Seventy-six percent identified as non-Latino Caucasian, 14% as Hispanic/Latino, 7% Asian-American, 1% African American, and 2% other ethnic or racial backgrounds.
Age-associated Trends in Physical Health, Cognitive Function, and Mental Health
Tables 1, 2, and 3 show results of regression analyses for physical, cognitive, and mental health variables, respectively. For ease of communication, results are described in terms of age-associated deterioration or improvement in health; however, within-subject changes can only be inferred from longitudinal data. Interpretive limitations of the cross-sectional design are discussed below.
Table 1.
Results of Nested Regression Models for Physical Health (N =1,491)
| Predictor | Model 1
|
Model 2
|
Model 3
|
Model 4
|
||||
|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | b | SE | |
| Intercept | 0.0037 | 0.0252 | −0.0004 | 0.0236 | 0.0638 | 0.0365 | 0.0769* | 0.0380 |
| Gender (Male) | −0.0234 | 0.0534 | 0.0690 | 0.0503 | 0.0767 | 0.0504 | 0.0747 | 0.0504 |
| Education | 0.2398*** | 0.0406 | 0.1745*** | 0.0382 | 0.1682*** | 0.0383 | 0.1713*** | 0.0383 |
| Marital Status (Married) | 0.2816*** | 0.0539 | 0.2201*** | 0.0506 | 0.1831*** | 0.0531 | 0.1877*** | 0.0532 |
| Age (linear) | -- | -- | −0.0166*** | 0.0011 | −0.0182*** | 0.0013 | −0.0155*** | 0.0025 |
| Age (quadratic) | -- | -- | -- | -- | −0.0001* | 0.0001 | −0.0002* | 0.0001 |
| Age (cubic) | -- | -- | -- | -- | -- | -- | <.0001 | <.0001 |
| LRT p value | -- | < .001 | .021 | .219 | ||||
| R2 | .051 | .170 | .173 | .174 | ||||
Note: b = beta coefficient, SE = standard error, LRT = likelihood ratio test; R2 = variance accounted for;
p < .05
p < .01
p < .001.
Table 2.
Results of Nested Regression Models for Cognitive Function (N =1,491)
| Predictor | Model 1
|
Model 2
|
Model 3
|
Model 4
|
||||
|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | b | SE | |
| Intercept | 0.0118 | 0.0244 | 0.0069 | 0.0219 | 0.1893*** | 0.0333 | 0.2114*** | 0.0347 |
| Gender (Male) | −0.3633*** | 0.0517 | −0.2509*** | 0.0467 | −0.2290*** | 0.0460 | −0.2324*** | 0.0460 |
| Education | 0.3933*** | 0.0393 | 0.3138*** | 0.0355 | 0.2960*** | 0.0350 | 0.3011*** | 0.0350 |
| Marital Status (Married) | 0.2245*** | 0.0522 | 0.1498** | 0.0470 | 0.0445 | 0.0485 | 0.0522 | 0.0485 |
| Age (linear) | -- | -- | −0.0202*** | 0.0011 | −0.0246*** | 0.0012 | −0.0202*** | 0.0023 |
| Age (quadratic) | -- | -- | -- | -- | −0.0004*** | 0.0001 | −0.0005*** | 0.0001 |
| Age (cubic) | -- | -- | -- | -- | -- | -- | <.0001* | <.0001 |
| LRT p value | -- | < .001 | < .001 | .024 | ||||
| R2 | .094 | .273 | .297 | .299 | ||||
Note: b = beta coefficient, SE = standard error, LRT = likelihood ratio test; R2 = variance accounted for
p < .05
p < .01
p < .001.
Table 3.
Results of Nested Regression Models for Mental Health (N =1,491)
| Predictor | Model 1
|
Model 2
|
Model 3
|
Model 4
|
||||
|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | b | SE | |
| Intercept | −0.0003 | 0.0255 | 0.0022 | 0.0249 | 0.0483 | 0.0386 | 0.0651 | 0.0402 |
| Gender (Male) | 0.0920 | 0.0540 | 0.0354 | 0.0532 | 0.0409 | 0.0533 | 0.0384 | 0.0533 |
| Education | 0.1859*** | 0.0411 | 0.2258*** | 0.0404 | 0.2213*** | 0.0405 | 0.2252*** | 0.0406 |
| Marital Status (Married) | 0.2038*** | 0.0546 | 0.2414*** | 0.0535 | 0.2149*** | 0.0562 | 0.2208*** | 0.0563 |
| Age (linear) | -- | -- | 0.0102*** | 0.0012 | 0.0090*** | 0.0014 | 0.0124*** | 0.0027 |
| Age (quadratic) | -- | -- | -- | -- | −0.0001 | 0.0001 | −0.0002* | 0.0001 |
| Age (cubic) | -- | -- | -- | -- | -- | -- | <.0001 | <.0001 |
| LRT p value | -- | < .001 | .119 | .138 | ||||
| R2 | .036 | .080 | .082 | .083 | ||||
Note: b = beta coefficient, SE = standard error, LRT = likelihood ratio test; R2 = variance accounted for
p < .05
p < .01
p < .001.
While physical and cognitive function showed nonlinear (accelerating) worsening with age, mental health showed linear improvement. Specifically, the physical health model with gender, education, and marital status was improved by adding a linear effect of age (ΔR2=.125) as well as a nonlinear (quadratic) effect (ΔR2=.004), but not a second nonlinear (cubic) effect. The cognitive function model was improved by adding a linear effect of age (ΔR2=.197) as well as a nonlinear (quadratic) effect (ΔR2=.033) and a second nonlinear (cubic) effect (ΔR2=.003). The mental health model was improved by adding a linear effect of age (ΔR2 = .046) but not by adding nonlinear (quadratic and cubic) effects.
Predicted values for the best fitting regression models are plotted in Figure 1 (corresponding observed data are reported in Supplemental Figure 2). Successively older cohorts had better mental health despite having successively worse physical and cognitive function than younger cohorts. Across the 80 cross-sectional years of data, participants reported, on average, approximately a 1.5 standard deviation (SD) drop in self-reported physical health and a 2 SD decline in cognitive function. Cognitive function appeared very non-linear, with accelerating decline beginning in the 60s. The apparent improvement in mental health with age was linear with participants reporting nearly 1 SD of change, on average.
Figure 1.
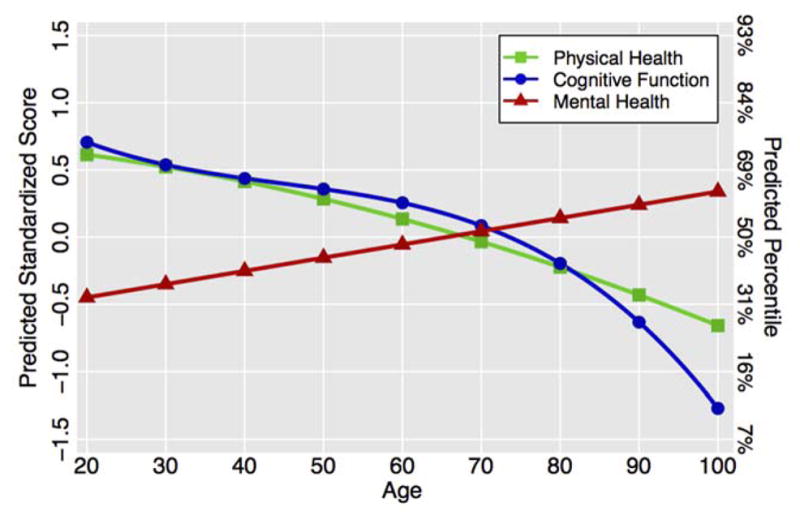
Predicted Values of Each Health Domain by Age
It has been argued that the U-shaped curve frequently seen in studies of well-being is an artifact of inappropriately controlling for marital status and education, as these variables are possibly influenced by well-being42. In the present data, results without these covariates were similar except for a few minor differences – i.e., the nonlinear (quadratic) effect of age on mental health was additionally significant and the second nonlinear (cubic) effect of age on cognitive function was non-significant. Interpretively, mental health showed slight inverted U-shaped trend with age that peaked in late life and cognitive function showed an inverted U-shaped trend that peaked in early life.
Figure 2 shows predicted age-related trends in the individual mental health scores that contributed to the composite. Scores on the Happiness Subscale, and reverse-coded Anxiety Scale and Depression Scale all improved with age (linear terms of b=0.0108, SE=0.0013, p<.001; b=0.0068, SE=0.0013, p<.001; and b=0.0085, SE=0.0013, p<.001, respectively). Both the SF-36 mental health composite and the reverse-coded Perceived Stress Scale score demonstrated inverted U-shaped effects (linear terms of b=0.0011, SE=0.0015, p=.486; and b=0.0075, SE=0.0015, p<.001, respectively, and quadratic terms of b=−0.0002, SE=0.0001, p=.005; and b=−0.0001, SE=0.0001, p=.037, respectively). The Satisfaction with Life Scale score demonstrated a U-shaped effect (linear term of b=0.0155, SE=0.0014, p<.001 and quadratic term of b=0.0001, SE=0.0001, p<.029).
Figure 2. Predicted Values for Individual Measures of Mental Health.
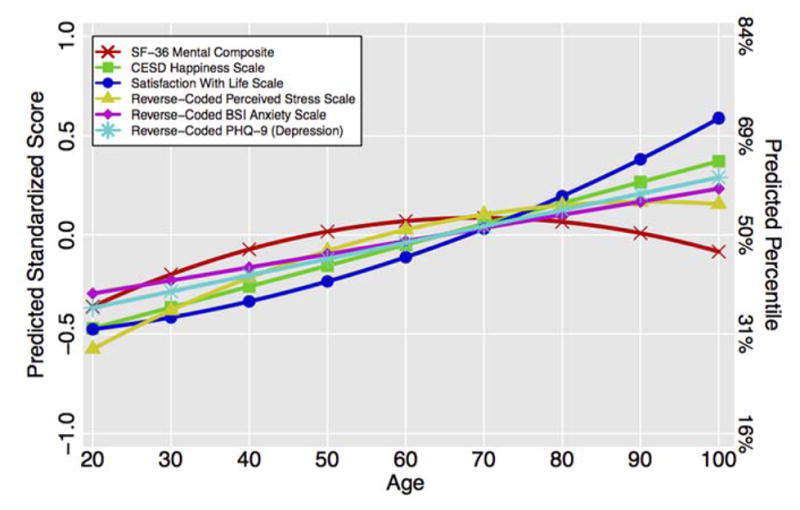
Abbreviations. BSI = Brief Symptom Inventory; CESD = Center for Epidemiological Studies – Depression scale; PHQ-9 = Patient Health Questionnaire Depression Module.
DISCUSSION
Our findings support the existence of a “paradox” in which aging is associated with better mental health among older adults at the population level despite loss of physical and cognitive function. Consistent with prior research, relative to successively younger cohorts, older cohorts had worse physical and cognitive function,43–45 but better mental health. This pattern was observed in each successive age cohort from 20s through 90s. The magnitude of this change was substantial, with the oldest cohort having mental health scores 1 SD higher than the youngest cohort’s, in sharp contrast to the 1.5 and 2 SD differences (suggesting declines) in physical and cognitive function, respectively. The age effects on the composite mental health measure did not conform to a “U-shaped” curve, rather a linear increase from the 20s to the 90s provided the best fitting model.
Study strengths include the structured multi-cohort design, subject selection using random digit dialing, oversampling of older adults (due to increased risk of drop-outs), and use of published, validated measures of various constructs simultaneously. However, our study also has limitations. First, data were cross-sectional; therefore, we cannot make longitudinal or causal inferences about changes in these domains for individual participants. The apparent changes might reflect birth cohort differences (e.g., baby boomers have a higher incidence of mental illnesses including depression, anxiety disorders, and substance use disorders compared to the people born before the World War II)46 and/or survivor bias (i.e., less healthy younger adults are less likely to survive into old age). However, the negative trajectory of physical and cognitive health across age groups with expected magnitudes of decline argues against the older participants being super-healthy. While longitudinal studies to examine aging trajectories require many resources, are expensive, and require more than a decade of follow-up, employment of innovative study designs such as the multi-cohort longitudinal design that we used, can make such research more feasible. Second, self-report measures of physical and mental health could be less accurate than objective measures. However, investigations have shown self-reports of subjective functioning correlate significantly with objective measures of health (e.g., mortality)47 and of local community wellness,48 suggesting that subjective measures do have objective value. Third, representativeness of the sample might have varied across age groups. While we used random digit dialing to reduce bias in convenience sampling, our study protocol required participants be selected/contacted using a landline. Many younger adults use cell phones as their main form of communication;49 we might not have achieved a fully representative sample among younger age groups. However, cell phone numbers do not correspond to the local area code of residence and thus, do not help ascertain if the participant is located in San Diego county. Similarly, measurement floor or ceiling effects could have impacted the analyses. Furthermore, we did not use a comprehensive neuropsychological evaluation to measure cognition, but rather a telephone-based screening tool (TICS-M). Although dementia was screened out by self-report, our sample likely included some individuals with previously undiagnosed dementia.32 Some of the observed cognitive decline beginning around age 65 may reflect such pathological cognitive aging. Finally, our sample was based in San Diego, and further studies of this type are needed in other regions to generalize our findings to communities with different population characteristics.
Notwithstanding these limitations, an intriguing question is whether the observed positive mental health in old age reflects favorable brain changes,50 or is the result of diminished risk factors for mental distress. One possibility is that older adults become more adept at coping with stressful changes.12,13,51–53 Similar to the literature on cognitive reserve in which passive versus active processes converge in maintaining cognitive function,54 active emotional reserve may enable older adults to counter threats to mental health such as diminishing physical health. Carstensen and colleagues have attributed such changes to socioemotional selectivity in later life, resulting from narrower horizon of life in view of the acknowledgement of mortality.14 Another possible explanation for greater life satisfaction among older adults is what Linda George described 30 years ago as “lowering [of] aspirations to meet realities.”55
An important explanation for improved mental health in later life is increase in wisdom with aging, as suggested by several (but not all) studies.8,13,56 Researchers have reported that, compared to younger adults, older individuals tend to be more skilled at emotional regulation and complex social decision making, and to exhibit more positively valenced information processing.12–16 Others have found that as people age they experience fewer negative emotions, regulate their emotions more effectively, and show positive biases in their memory.57 One study reported older adults used accumulated lifetime experience in decision making to determine long-term utility rather than immediate gains.16 In one investigation, Gooding and colleagues reported older adults were more resilient than younger ones with respect to emotional regulation and problem solving.58 These behavioral changes parallel functional imaging studies showing diminished responsiveness of amygdala to negative or stressful images in older compared to younger adults.59 Such positivity may lead to higher levels of subjective well-being in later life.
Our results are consistent with epidemiological studies finding the prevalence of non-dementing mental disorders decline incrementally from younger to older age groups.22–25 Our results suggest that surviving older adults may be more resilient to common physical and social stresses compared to younger counterparts. A similar phenomenon may underlie the lower prevalence of mental illnesses in older adults, although there are alternative explanations such as under-diagnosis or mis-diagnosis of psychiatric conditions in later life.
At the same time, old age is often associated with serious physical, psychological, and social stresses. One must not underestimate the need for high quality mental and physical healthcare for older adults. Nonetheless, our study raises important questions about traditional conceptualization of models of aging, including biological ones, which focus on functional (physical and cognitive) declines with usual aging or employ longevity as the primary marker of successful aging. These models need revising to account for what may be “normative” improvement in mental health that may accompany population aging. Even among people with serious mental illnesses such as schizophrenia, aging tends to be associated with improvement in mental health.60,61
Another notable finding relates to high levels of subjective (perceived) stress along with symptoms of depression and anxiety among those in their 20s and 30s. This “fountain of youth” is associated with far worse level of psychological well-being than during any other period of adulthood. There are many pressures rather unique to this life phase – e.g., establishing careers, finding life partners, and navigating financial issues.62 Whereas adolescence has long been an area of social and scientific concern, relatively little attention has been paid to issues that continue or get exacerbated post-adolescence. Of note, the rate of mental illness and treatment seeking in younger persons has been increasing sharply,63 whereas rates of self-reported depressive symptoms in later life have declined.64
When treating younger adults, we should consider how to leverage positive mental health factors to augment their psychosocial functioning, whereas in older adults these factors may help with physical and cognitive functioning. There is a critical need for lifespan research combining psychosocial and biological sciences to improve our understanding of the processes that underlie increased well-being in later life and to help develop interventions to promote wellness in all age groups.
Supplementary Material
CLINICAL POINTS.
Studies show declining physical and cognitive health during later phases of the lifespan; yet, few have examined trajectories of mental health in the context of these declines.
Our results point to a progressive improvement in mental health (i.e., higher levels of life satisfaction, happiness, and well-being, and lower levels of anxiety, depression, and perceived stress) from age 21 through the 90s.
When treating younger adults, consider how to leverage positive mental health factors in augmenting their psychosocial functioning, whereas in older adults these factors may help with physical and cognitive functioning.
Acknowledgments
We wish to thank Rebecca Daly, AA, from the Department of Psychiatry and Sam and Rose Stein Institute for Research on Aging at University of California, San Diego, for her invaluable contributions in database management. She has no conflicts of interest to report.
Sources of financial and material support: This work was supported, in part, by NIMH grants T32 MH019934, R01 MH099987, R01 MH094151, and K23 MH102420 and by the Sam and Rose Stein Institute for Research on Aging at the University of California, San Diego. The donors to the Stein Institute had no role in the design and conduct of this study.
Footnotes
Previous presentations: None.
Disclaimer: None to declare.
References
- 1.National Alliance for Suicide Prevention. [Accessed September 3, 2015];Executive summary: a survey about mental health and suicide in the United States. http://www.afsp.org/news-events/in-the-news/surveyresults.
- 2.WHO. Mental disorders. WHO; [Accessed August 21, 2015]. http://www.who.int/mediacentre/factsheets/fs396/en/ [Google Scholar]
- 3.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 4.Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–648. doi: 10.1016/S0140-6736(13)61489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeste DV, Depp CA, Vahia IV. Successful cognitive and emotional aging. World Psychiatry. 2010;9(2):78–84. doi: 10.1002/j.2051-5545.2010.tb00277.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blanchflower DG, Oswald AJ. Is well-being U-shaped over the life cycle? Soc Sci Med. 2008;66(8):1733–1749. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 7.Stone AA, Schwartz JE, Broderick JE, Deaton A. A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci USA. 2010;107(22):9985–9990. doi: 10.1073/pnas.1003744107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jeste DV, Oswald AJ. Individual and societal wisdom: explaining the paradox of human aging and high well-being. Psychiatry. 2014;77(4):317–330. doi: 10.1521/psyc.2014.77.4.317. [DOI] [PubMed] [Google Scholar]
- 9.López Ulloa BF, Møller V, Sousa-Poza A. How does subjective well-being evolve with age? A literature review. Population Ageing. 2013;6(3):227–246. doi: 10.1007/s12062-013-9085-0. [DOI] [Google Scholar]
- 10.Charles ST, Reynolds CA, Gatz M. Age-related differences and change in positive and negative affect over 23 years. J Pers Soc Psychol. 2001;80(1):136–151. [PubMed] [Google Scholar]
- 11.Mroczek DK, Kolarz CM. The effect of age on positive and negative affect: a developmental perspective on happiness. J Pers Soc Psychol. 1998;75(5):1333–1349. doi: 10.1037//0022-3514.75.5.1333. [DOI] [PubMed] [Google Scholar]
- 12.Blazer DG. Successful aging. Am J Geriatr Psychiatry. 2006;14(1):2–5. doi: 10.1097/01.JGP.0000195222.93655.d1. [DOI] [PubMed] [Google Scholar]
- 13.Vaillant GE. Aging Well: Surprising Guideposts to a Happier Life From the Landmark Harvard Study of Adult Development. Boston: Little, Brown & Company; 2002. [Google Scholar]
- 14.Carstensen LL, Mikels JA, Mather M. Handbook of the Psychology of Aging. Elsevier; 2006. Aging and the Intersection of Cognition, Motivation, and Emotion; pp. 343–362. [DOI] [Google Scholar]
- 15.Grossmann I, Na J, Varnum MEW, Park DC, Kitayama S, Nisbett RE. Reasoning about social conflicts improves into old age. Proc Natl Acad Sci USA. 2010;107(16):7246–7250. doi: 10.1073/pnas.1001715107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Worthy DA, Gorlick MA, Pacheco JL, Schnyer DM, Maddox WT. With age comes wisdom: decision making in younger and older adults. Psychol Sci. 2011;22(11):1375–1380. doi: 10.1177/0956797611420301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Springer KW, Pudrovska T, Hauser RM. Does Psychological Well-Being Change with Age?: Longitudinal Tests of Age Variations and Further Exploration of the Multidimensionality of Ryff’s Model of Psychological Well-Being. Soc Sci Res. 2011;40(1):392–398. doi: 10.1016/j.ssresearch.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 19.Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol. 1993;22(4 Suppl A):6A–13A. doi: 10.1016/0735-1097(93)90455-a. [DOI] [PubMed] [Google Scholar]
- 20.Craik FIM, Salthouse TA. The Handbook of Aging and Cognition. Mahwah, N.J: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 21.Andrews FM, Withey SB. Social Indicators of Well-Being: Americans’ Perceptions of Life Quality. New York and London: Plenum Press; 1976. [Google Scholar]
- 22.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 23.de Graaf R, Have ten M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):203–213. doi: 10.1007/s00127-010-0334-8. [DOI] [PubMed] [Google Scholar]
- 24.Regier DA, Farmer ME, Rae DS, et al. One-month prevalence of mental disorders in the United States and sociodemographic characteristics: the Epidemiologic Catchment Area study. Acta Psychiatr Scand. 1993;88(1):35–47. doi: 10.1111/j.1600-0447.1993.tb03411.x. [DOI] [PubMed] [Google Scholar]
- 25.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 26.Palmer BW, Jeste DV, Sheikh JI. Anxiety disorders in the elderly: DSM-IV and other barriers to diagnosis and treatment. J Affect Disord. 1997;46(3):183–190. doi: 10.1016/S0165-0327(97)00146-8. [DOI] [PubMed] [Google Scholar]
- 27.Jeste DV, Savla GN, Thompson WK, et al. Association between older age and more successful aging: critical role of resilience and depression. Am J Psychiatry. 2013;170(2):188–196. doi: 10.1176/appi.ajp.2012.12030386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martin AS, Palmer BW, Rock D, Gelston CV, Jeste DV. Associations of self-perceived successful aging in young-old versus old-old adults. Int Psychogeriatr. 2015;27(4):601–609. doi: 10.1017/S104161021400221X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ware JE, Kosinski M, Keller S. SF-36 Physical and Mental Health Summary Scales: a User’s Manual. 1994. [Google Scholar]
- 30.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 31.de Jager CA, Budge MM, Clarke R. Utility of TICS-M for the assessment of cognitive function in older adults. Int J Geriatr Psychiatry. 2003;18(4):318–324. doi: 10.1002/gps.830. [DOI] [PubMed] [Google Scholar]
- 32.Zlatar ZZ, Moore RC, Palmer BW, Thompson WK, Jeste DV. Cognitive complaints correlate with depression rather than concurrent objective cognitive impairment in the successful aging evaluation baseline sample. J Geriatr Psychiatry Neurol. 2014;27(3):181–187. doi: 10.1177/0891988714524628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fowler JH, Christakis NA. Dynamic spread of happiness in a large social network: longitudinal analysis over 20 years in the Framingham Heart Study. BMJ. 2008;337:a2338. doi: 10.1136/bmj.a2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985;49(1):71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 35.Derogatis LR. BSI, Brief Symptom Inventory: Administration, Scoring, and Procedures Manual. 4. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cohen S, Williamson G. The Social Psychology of Health. SAGE Publications; 1988. Perceived stress in a probability sample of the United States; pp. 31–67. Incorporated. [Google Scholar]
- 38.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 39.Cohen J, Cohen P, West SG, Aiken LS. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Mahwah, N.J: Lawrence Erlbaum Associates Publishers; 2003. [Google Scholar]
- 40.Serlin RC, Levin JR. Teaching how to derive directly interpretable coding schemes for multiple regression analysis. Journal of Educational and Behavioral Statistics. 1985;10(3):223–238. doi: 10.3102/10769986010003223. [DOI] [Google Scholar]
- 41.Team R. R: a Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. http://www.R-project.org/ [Google Scholar]
- 42.Glenn N. Is the apparent U-shape of well-being over the life course a result of inappropriate use of control variables? A commentary on Blanchflower and Oswald (66: 8, 2008, 1733–1749) Soc Sci Med. 2009;69(4):481–5. doi: 10.1016/j.socscimed.2009.05.038. discussion486–88. [DOI] [PubMed] [Google Scholar]
- 43.Nair KS. Aging muscle. Am J Clin Nutr. 2005;81(5):953–963. doi: 10.1093/ajcn/81.5.953. [DOI] [PubMed] [Google Scholar]
- 44.Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289(18):2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 45.Fleg JL, Morrell CH, Bos AG, et al. Accelerated longitudinal decline of aerobic capacity in healthy older adults. Circulation. 2005;112(5):674–682. doi: 10.1161/CIRCULATIONAHA.105.545459. [DOI] [PubMed] [Google Scholar]
- 46.Jeste DV, Alexopoulos GS, Bartels SJ, et al. Consensus statement on the upcoming crisis in geriatric mental health: research agenda for the next 2 decades. Arch Gen Psychiatry. 1999;56(9):848–853. doi: 10.1001/archpsyc.56.9.848. [DOI] [PubMed] [Google Scholar]
- 47.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oswald AJ, Wu S. Objective confirmation of subjective measures of human well-being: evidence from the U.S.A. Science. 2010;327(5965):576–579. doi: 10.1126/science.1180606. [DOI] [PubMed] [Google Scholar]
- 49.Lee S, Brick JM, Brown ER, Grant D. Growing cell-phone population and noncoverage bias in traditional random digit dial telephone health surveys. Health Serv Res. 2010;45(4):1121–1139. doi: 10.1111/j.1475-6773.2010.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Charles ST, Carstensen LL. Social and emotional aging. Annu Rev Psychol. 2010;61(1):383–409. doi: 10.1146/annurev.psych.093008.100448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jeste DV, Palmer BW. Positive Psychiatry—a Clinical Handbook. Washington, DC: American Psychiatric Publishing; 2015. [Google Scholar]
- 52.Jeste DV, Palmer BW, Rettew DC, Boardman S. Positive psychiatry: Its time has come. J Clin Psychiatry. 2015 doi: 10.4088/JCP.14nr09599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Reynolds CF. Preventing depression in old age: it’s time. Am J Geriatr Psychiatry. 2008;16(6):433–434. doi: 10.1097/JGP.0b013e31816c7b67. [DOI] [PubMed] [Google Scholar]
- 54.Stern Y. Cognitive reserve. Neuropsychologia. 2009;47(10):2015–2028. doi: 10.1016/j.neuropsychologia.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.George LK. Life satisfaction in later life. Generations: Journal of the American Society on Aging. 1986 [Google Scholar]
- 56.Mickler C, Staudinger UM. Personal wisdom: validation and age-related differences of a performance measure. Psychol Aging. 2008;23(4):787–799. doi: 10.1037/a0013928. [DOI] [PubMed] [Google Scholar]
- 57.Reed AE, Carstensen LL. The theory behind the age-related positivity effect. Front Psychol. 2012;3:339. doi: 10.3389/fpsyg.2012.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gooding PA, Hurst A, Johnson J, Tarrier N. Psychological resilience in young and older adults. Int J Geriatr Psychiatry. 2012;27(3):262–270. doi: 10.1002/gps.2712. [DOI] [PubMed] [Google Scholar]
- 59.Mather M, Canli T, English T, et al. Amygdala responses to emotionally valenced stimuli in older and younger adults. Psychol Sci. 2004;15(4):259–263. doi: 10.1111/j.0956-7976.2004.00662.x. [DOI] [PubMed] [Google Scholar]
- 60.Jeste DV, Wolkowitz OM, Palmer BW. Divergent trajectories of physical, cognitive, and psychosocial aging in schizophrenia. Schizophr Bull. 2011;37(3):451–455. doi: 10.1093/schbul/sbr026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Folsom DP, Depp C, Palmer BW, et al. Physical and mental health-related quality of life among older people with schizophrenia. Schizophr Res. 2009;108(1–3):207–213. doi: 10.1016/j.schres.2008.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schwartz B. The Paradox of Choice. New York: Harper Collins; 2009. [Google Scholar]
- 63.Collishaw S. Annual research review: Secular trends in child and adolescent mental health. J Child Psychol Psychiatry. 2015;56(3):370–393. doi: 10.1111/jcpp.12372. [DOI] [PubMed] [Google Scholar]
- 64.Zivin K, Pirraglia PA, McCammon RJ, Langa KM, Vijan S. Trends in depressive symptom burden among older adults in the United States from 1998 to 2008. J Gen Intern Med. 2013;28(12):1611–1619. doi: 10.1007/s11606-013-2533-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


