Abstract
Fundamental to cognitive models of addiction is the gradual strengthening of automatic, urge-related responding that develops in tandem with the diminution of self-control-related processes aimed at inhibiting impulses. Recent conceptualizations of addiction also include a third set of cognitive processes related to self-awareness and superordinate regulation of self-control and other higher brain function. This review describes new human research evidence and theoretical developments related to the multicausal strengthening of urge-related responding and failure of self-control in addiction, and the etiology of disrupted self-awareness and rational decision-making associated with continued substance use. Recent progress in the development of therapeutic strategies targeting these mechanisms of addiction is reviewed, including cognitive bias modification, mindfulness training, and neurocognitive rehabilitation.
INTRODUCTION
Addiction is a brain disease characterized by the compulsion to use psychoactive substances despite negative consequences. Although different methods and models have been used to explain addiction, its etiology is generally attributed to neurobehavioral adaptations resulting from a combination of predisposing factors and chronic substance use that gradually strengthen the urge to use substances, weaken willpower and resolve to resist these urges, and diminish critical awareness of the growing strength and range of stimuli that trigger these urges.
Recent conceptualizations of addiction [1–3]• include three disparate but interactive sets of mental processes instrumental to the initiation, progression, and maintenance of addiction1: (1) implicit cognitive processes, which encompass learning and memory; (2) metacognitive processes, including self-awareness, reflective thinking, and superordinate self-regulation; and (3) executive function, which includes other higher order mental processes necessary for the planning, execution, and monitoring of goal-directed behavior. Central to the compulsive nature of addiction is the gradual strengthening of stimulus-driven implicit processes, which overwhelm a progressively weaker executive control system and interfere with awareness and rational thinking about the costs and benefits associated with continued substance use. The purpose of this paper is to provide a concise yet integrative review of the literature since 2014 that has contributed to a greater understanding of these cognitive processes both as mechanisms of addiction and as therapeutic targets.
Implicit Cognitive Processes
Implicit, or automatic, cognition includes classically and operantly conditioned responses, which are controlled respectively by repeated pairings with their antecedents and consequences. Implicit responding is generally measured indirectly as central task disruption or facilitation, or the degree to which drug-or-alcohol-related cue responding impedes or facilitates performance of (i.e., increases or decreases latency to complete) a goal-directed task. The three most common implicit cognition paradigms examined in addiction literature include spontaneous memory association (i.e., memory bias), attentional capture (i.e., attentional bias), and action tendency (i.e., approach-avoidance biases). These are sometimes referred to collectively as measures of cognitive bias. It is, however, important to differentiate cognitive bias paradigms, that vary the type of central task, from the underlying cue-reactivity, or implicit processing, which influences central task performance.
Recent studies provide evidence in support of [4], in partial support of [5] and contrary to [6] the validity and clinical relevance of specific cognitive bias measures. Recent papers have also reviewed the clinical relevance of attentional bias in substance use disorders (SUD) in general [7, 8] and in cocaine use disorder specifically [9].
There is no universal consensus regarding how implicit processes are strengthened over the course of addiction, but the progression appears to be multidetermined. One way implicit processes are regarded to strengthen over time is through incentive sensitization [10], in which chronic substance use is posited to hypersensitize mesocorticolimbic reward pathways resulting in enhanced incentive motivation (i.e., “wanting”). Recent studies provide evidence in support of incentive sensitization theory. For example, repeated exposure to amphetamine in a human laboratory study resulted in increased fMRI BOLD activation in the caudate nucleus during reward anticipation that was correlated with enhanced subjective amphetamine-like responding [11]••. Other clinical studies similarly identify reward pathway hypersensitivity associated with quantity of recent cannabis use [12] and duration and severity of alcohol dependence [13]. Furthermore, across twenty-four neuroimaging studies of cognitive interventions for addiction, the reduction of reward pathway sensitivity was identified as one of two brain changes common to successful treatment outcomes [14].
Another mechanism by which implicitly learned habits become increasingly resistant to extinction is through Pavlovian-to-instrumental transfer (PIT). Closely related to incentive sensitization, PIT represents a shift over the course of addiction in which increasingly stronger incentive motivation in response to predictive cues maintains operantly conditioned habits in the apparent absence of a reinforcement mechanism. A recent study showed PIT associated BOLD activation in the nucleus accumbens that was predictive of subsequent relapse in alcohol dependent individuals [15]. Central to PIT is the maintenance of habit via predictive, or anticipatory, responding. Investigators in another study examined anticipatory cue responding using a modified alcohol approach-avoidance task, and found cue-reactivity to be associated with strength of anticipatory processing as measured by EEG beta-band event-related desynchronization [16].
Although no reinforcement mechanism may be apparent in PIT, hedonic shifting over the course of addiction [17] suggests that drug-and-alcohol-related predictive cues trigger avoidance responding, which is a negatively reinforced behavior. This would provide an additional mechanism for the further strengthening of learned habits. Potential support for this mechanism is provided by a recent study in which reward anticipation was associated with anhedonia in cocaine users, suggesting implicit responding may be driven by “wanting” to alleviate a negative affective state [18].
Another mechanism that contributes to the resistance to extinction of implicitly learned associations is the impaired ability for new learning. Whether a cognitive predisposition or consequence of the neurotoxic effects of prolonged substance use (or both), learning and memory deficits likely play a role in the maintenance of implicitly learned associations. For example, in comparison to healthy control subjects, people with SUDs in one study were more likely to develop habitual responding to stimulus response contingencies that interfered with the learning of new response contingencies [19]. In contrast, Sebold and colleagues [20] found that chronic alcohol use was associated with impaired goal-directed responding, but not increased habitual responding. Lengthier discussion about addiction related learning and memory impairment is beyond the scope of this review, but impairment is likely influenced by the chronicity of substance use, duration of time since last use, and quantity and type of substances used.
Cognitive Bias Modification
Implicit measures of cognitive bias associated with drug-and-alcohol-related stimuli have also been examined as platforms for cue exposure and counter-conditioning methods. Collectively, these approaches are referred to as cognitive bias modification. Primarily, attentional bias and approach-avoidance bias measures have been adapted for this purpose and examined for their effectiveness in reducing cue responding and other clinically relevant outcomes. Recent studies provide evidence in support of [21], in partial support of [22]•, and contrary to [23, 24]• the clinical utility of cognitive bias modification.
One important challenge associated with cognitive bias modification appears to be the increasing complexity of implicit responding over the course of addiction. In other words, addicted individuals develop sophisticated and individualized associative networks that selectively activate information processing (e.g., heuristics, attributions, appraisals, schemata, etc.) and complicate retraining as a therapeutic strategy. For example, Woud and colleagues [25] found that alcohol-dependent patients in their study demonstrated biased interpretation processes, in which alcohol-related contexts were attributed to emotionally relevant but ambiguous scenarios. Findings from these investigators also showed that coping motives were associated with the attribution of negatively valenced scenarios to alcohol-related contexts [26]; which provides additional evidence that predictive cues may trigger negatively reinforced avoidance responding. However, when Woud and colleagues [27] examined the malleability of alcohol interpretation bias using a cognitive bias modification paradigm, they found that biased interpretations could be increased but not decreased via the experimental parameters used in their study.
See the annotated bibliography for descriptions of other studies examining dispositional drinking motives associated with implicit associations [28]•• and heuristic appraisal of alcohol effects [29]••; and for other potential therapeutic strategies for targeting implicit responding, including memory reconsolidation [30]•• and cognitive reappraisal in the context of memory retrieval-destabilization [31]••.
Explicit Cognitive Processes: Metacognition
In contrast to the automatic and stimulus-driven processes associated with the implicit system, the explicit system includes higher order brain functions that are non-automatic and effortful. The compulsion to use substances, or lack of control over substance use, may be regarded as an imbalance between the implicit and explicit systems, in which explicit processes aimed at self-regulation are unable to control urge-related responding. The processes subsumed under the explicit system are neither universally designated nor operationalized, but have been conceptualized as having two subsystems [1, 3, 32] that are referred to here as “metacognition” and “executive function.”
Metacognition involves the critical awareness, knowledge and control of our own cognitive processes, reasoning and decision-making. Recent studies support an association between metacognitive processing deficits and addiction [33, 34]••. Although one recent study reported a relationship between maladaptive metacognitive style and addiction potential in college students [35]•, there is little evidence at present to comment on the comparative influence of predisposing cognitive factors versus acquired deficits on metacognitive functioning.
As opposed to a cognitive deficit or weakness, implicit processes may directly interfere with metacognitive awareness of reasoning and decision-making about drugs and alcohol. The rational mind relies on heuristics and other mental short cuts (e.g., attributions, appraisals, schemata) representing implicitly activated information processing to avoid the need to relearn previously acquired knowledge. However, these automatic processes foster an irrational persistence of belief – e.g., positive expectancies regarding continued substance use – that contributes to the maintenance of addiction. A recent paper provides a detailed review and commentary regarding automatically triggered thoughts in addiction, and how they may, furthermore, interact with explicit cognitive processes to intensify cue-reactive responding based on Elaborated Intrusion Theory [36].
Mindfulness
Several constructs examined in recent addiction literature are conceptually similar to metacognitive processes, including self-reflection and rational decision-making [1], insight and self-awareness [37, 38], and appraisal of affective and motivational significance [37, 39]. In particular, a large amount of recent literature has been devoted to the construct of mindfulness [40], which may be defined as focused awareness on the present moment.
A recent meta-analysis of thirty-nine studies [41] identified a relationship between indices of substance use severity and mindfulness domains based on the Five Facet Mindfulness Questionnaire [42]. In that study, mindfulness domains including acting with awareness, non-judgment, and non-reactivity (but not observing or describing) were negatively associated with problem substance use.
Interventions aimed at increasing mindfulness have also been examined as a therapeutic strategy for the treatment of addiction. A recent meta-analytic review of twenty-four studies provides evidence for the effectiveness of mindfulness-based interventions in reducing substance use [43]. Furthermore, in a recent clinical trial, the integrated delivery of mindfulness-based and relapse-prevention interventions showed added benefit over standard relapse prevention in reducing long-term substance use [44]. These investigators speculate that mindfulness practices may support long-term outcomes by strengthening the ability to monitor and cope with dysphoria associated with negative hedonic processing in addiction. In the context of implicit processes, mindfulness may also increase awareness of automatic thinking that can interfere with thoughtful consideration about continued substance use. Recent papers also discuss other mechanisms through which enhanced mindfulness is theorized to improve SUD treatment outcomes [45, 46].
Explicit Cognitive Processes: Executive Function
Executive function represents the second major sub-division of the explicit system, and broadly includes mental operations necessary for the planning, execution, and monitoring of goal-directed behavior. Whereas metacognition includes subjective processes, the executive system is regarded to include mental operations that are value free, purposeful, and algorithmic [32]. The processes subsumed under executive function are not universally operationalized, but are typically measured using performance based neuropsychological tests or cognitive neuroimaging paradigms. Inventory questionnaires of executive function measure subjective self-appraisal of ability [47]• that, like performance measures, appear to be state dependent [48], but may also be influenced by the reliability of the historian.
Functional organization of the executive system is complex and composed of modular and superordinate processes. Execution of more complex goal-directed activities (e.g., self-control, decision-making, problem solving, and concept formation) requires multiple subordinate executive functions that include purposeful manipulation of core cognitive processes (e.g., working memory and selective attention). For example, executive processes associated with inhibitory control, error detection (or self-monitoring), and error correction (or self-adjustment) appear to comprise a dissociable yet interactive set of elements responsible for self-control [49]. These dissociable elements, furthermore, depend on other parallel and subordinate executive functions (e.g., initiation, scanning, selective attention, working memory, maintenance of set, pattern recognition, response selection, flexibility, switching, etc.). Similar cognitive processes are posited to exist for the control, or regulation, of cognitive, behavioral, and emotional responding.
Although profiles of executive dysfunction vary by substance [50], combinations of substances [51], and duration of abstinence [52], failure of the executive system to override drug-or-alcohol-related impulses is regarded as central to the development of addiction [53]. In other words, fundamental to cognitive conceptualizations of addiction is the dynamic opposition between self-control and urge-related responding. The etiology of executive control failure is commonly examined in three contexts: (1) predisposing cognitive vulnerabilities and personality characteristics (e.g., attention deficit hyperactivity disorder, and other trait-related impulse control deficiencies), (2) neurodevelopmental immaturity of brain areas associated with executive control in adolescents and young adults, and (3) the neurotoxic and neuroadatptive changes associated with chronic substance use. Failure of executive control attributable to multiple etiologies appears to be most strongly associated with addiction [54].
Impulsivity
Among the constructs most commonly associated with executive control failure is impulsivity. Due, in part, to its flexible measurement and multicausal etiology, there is no consensus regarding its dimensionality or the respective clinical relevance of core components or subtypes. Recent papers have contributed to increased knowledge about impulsivity dimensionality through data classification methods [55] and computational modeling [56]; and to the clinical relevance of core components through mediation analysis [57, 58]. In addition to studies examining predominantly data-driven analyses of impulsivity, expert judgment has also played an important role in providing evidence for the content-related validity of critical impulsivity subtypes and dimensions [59, 60].
A significant amount of recent research has also examined the relationship between impulsivity and its many associated constructs, including novelty seeking [57], risk taking [61], delay discounting [51], delay of gratification [62], impulsive choice or decision-making [58] and response inhibition [50, 63]. A recent paper by Bickel and colleagues [64] uniquely integrates many constructs associated with impulsivity through their elaboration of competing neurobehavioral systems theory [65]. Among the benefits of their model is that it meets previously suggested criteria for assessing the utility of impulsivity-related models of addiction [66]. Specifically, Bickel and colleagues [64] propose a theory-driven two-factor model (i.e., based on the dynamic opposition of self-control and urge-related responding in addiction) that is supported by neural evidence and provides a balance of explanatory power, parsimony and integration of evidence.
Relevance of Executive Function in the Treatment of Addiction
The strengthening of the inhibitory control neural network was recently identified as a possible common therapeutic mechanism across addiction treatment modalities, even when control processes are not specifically targeted [14, 67]. Thus, while the remediation of control processes is a valuable therapeutic approach, indirect relationships between self-control and treatment outcome are important to consider in efforts to improve treatment effectiveness. For example, a recent study showed that promoting greater metacognitive level construal of one’s smoking induced greater inhibitory control that mediated a reduction in cigarette consumption [68]. Another recent paper describes self-control strategies relevant to addiction, in which metacognitive processes related to situational awareness and prediction of self-control exertion are enlisted to minimize exposure to drug-and-alcohol-related cues [69].
Important indirect relationships between self-control and treatment outcome may also involve the enlistment of parallel and subordinate processes. One promising therapeutic approach involves working memory training –i.e., neurocognitive rehabilitation aimed at increasing storage capacity for, and ability to, hold, process, and manipulate information in the present. Working memory training has been shown to decrease delay discounting among stimulant addicts [70], and is posited to build self-control capacity [71] and improve efficacy of existing treatments when delivered adjunctive to standard care [72].
The use of neurocognitive rehabilitation strategies in addiction, however, is an area in its relative infancy. Executive and other core cognitive dysfunction in addiction includes deficits that may hinder the learning and effective application of skills and strategies taught in standard addiction treatment. Further research is needed to determine if delivering adjunctive neurocognitive rehabilitation of a broader set of executive and cognitive domains can enhance standard addiction treatment effectiveness.
Conclusions
Cognitive mechanisms of addiction may be broadly conceptualized as three sets of mental processes. The implicit system includes automatic and stimulus-driven processes. Metacognition and executive function are two major subdivisions of the explicit system that respectively represent subjective processes and value-free, purposeful mental operations. Fundamental to cognitive models of addiction is the gradual strengthening of implicitly developed urge-related responding that progressively overwhelms effortful cognitive processes aimed at self-control. Automatic processes can also disrupt substance use-related metacognitive self-awareness. Promising new therapeutic strategies target different cognitive mechanisms of addiction. Evidence suggests that the reduction of reward pathway sensitivity and strengthening of inhibitory control may be common to successful outcomes across treatment modalities. However, indirect relationships between control processes and treatment outcome are important to consider in order to improve treatment effectiveness. Neurocognitive rehabilitation delivered adjunctive to standard addiction treatment has shown some success, but more research is needed to adequately assess its effectiveness.
Figure 1. Visual representation of the cognitive mechanisms of addiction.
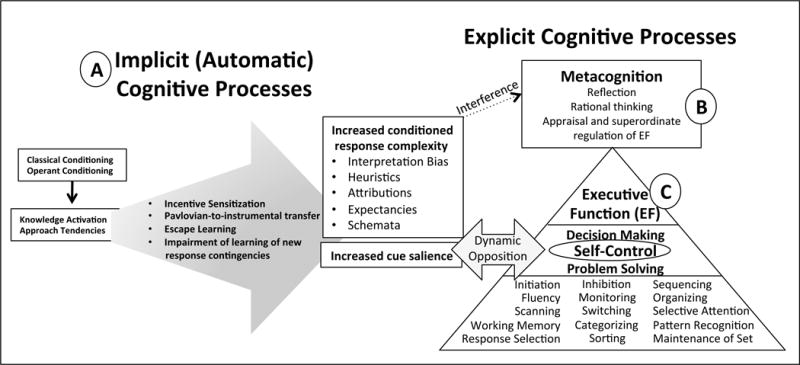
(A) Implicit, or automatic, cognition includes classically and operantly conditioned responses that strengthen over time, resulting in increased cue salience and conditioned response complexity; (B) Metacognition is a subdivision of explicit, or controlled, cognitive processes, and includes subjective, self-reflective and rational thinking, and appraisal and superordinate regulation of executive function. Complex conditioned responses (i.e., automatic information processing) happen outside of metacognitive self-awareness and can bypass reflective thinking. (C) Executive function represents the second sub-division of the explicit system, and includes mental operations that are value free, purposeful, and algorithmic. Fundamental to cognitive conceptualizations of addiction is the dynamic opposition between self-control and implicitly strengthened urge-related responding.
Highlights.
Cognitive mechanisms of addiction include automatic and controlled processes.
Strengthening of automatic and weakening of controlled processes are multicausal.
Automatic processes can disrupt substance use-related self-awareness.
Promising new therapeutic strategies target various mechanisms of addiction.
More research is needed to examine effectiveness of neurocognitive rehabilitation.
Acknowledgments
This work was supported by the National Institutes of Health [grant number K23DA027045], and The Peter and Elizabeth C. Tower Foundation [grant number AGR-1505-02589]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
The author has no conflicts of interest to report.
These authors present cognitive models of addiction whose elements are not necessarily named the same, but include similar characteristics. The labels, implicit, metacognitive, and executive were selected for this review because they appear with greater frequency as PubMed keywords in the context of addiction than do alternative search terms of similar meaning.
References
- 1•.Foxall GR. Metacognitive Control of Categorial Neurobehavioral Decision Systems. Front Psychol. 2016;7:170. doi: 10.3389/fpsyg.2016.00170. As noted elsewhere, the opposition between impulsive responding and impulse control is fundamental to cognitive models of addiction. This presents one of several recent papers dedicated to conceptualizing a framework for the cognitive mechanisms of addiction. The model presented in this paper integrates the competing neurobehavioral decision systems (CNDS) model, defined by Bickel and colleagues (2016), and the tri-process model, defined by Stanovich (2009). In the author’s Metacognitive Control of CNDS model, the CNDS impulsive decision system is sub-divided into state- and trait-dependent impulsive systems; and a superordinate level of reflective, or rational, decision-making regulates the executive decision system. The key oppositional relationship in this model is between the state impulsive and executive systems. This relationship is modified by the reflective/rational system, which “encourages cooperation” between impulsive and control-related decision-making. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2•.Turel O, Bechara A. A Triadic Reflective-Impulsive-Interoceptive Awareness Model of General and Impulsive Information System Use: Behavioral Tests of Neuro-Cognitive Theory. Front Psychol. 2016;7:601. doi: 10.3389/fpsyg.2016.00601. The Triadic Reflective-Impulsive-Interoceptive Awareness Model similarly includes two opposed information-processing brain systems, here named the impulsive and reflective systems. In this model, the reflective system represents processes associated with impulse control, thus maintaining the dual-process conceptualization (i.e., impulsive responding versus self-control) fundamental to cognitive models of addiction. This tri-partite model of “problematic and addictive behavior” includes an interoceptive awareness system that is associated with the awareness of “temptation;” and that modulates the effects of the reflective and impulsive systems on behavior. The model is tested and supported by two studies of social networking site use based on outcomes using structural equation modeling. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3•.Spada MM, et al. Metacognition in addictive behaviors. Addict Behav. 2015;44:9–15. doi: 10.1016/j.addbeh.2014.08.002. This paper describes the Self-Regulatory Executive Function (S-REF) model, for conceptualizing psychological distress and its application to addictive behaviors using a “triphasic metacognitive formulation.” The authors conclude that “The S-REF model provides a conceptual framework for expressing how stored knowledge and beliefs about thinking processes influence the choice of plans and regulation of coping” (p.13) that can be applied to addictive behaviors. [DOI] [PubMed] [Google Scholar]
- 4.Garland EL, Howard MO. Opioid attentional bias and cue-elicited craving predict future risk of prescription opioid misuse among chronic pain patients. Drug Alcohol Depend. 2014;144:283–7. doi: 10.1016/j.drugalcdep.2014.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cousijn J, Luijten M, Wiers RW. Mechanisms underlying alcohol-approach action tendencies: the role of emotional primes and drinking motives. Front Psychiatry. 2014;5:44. doi: 10.3389/fpsyt.2014.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Lemma LC, et al. Priming of conflicting motivational orientations in heavy drinkers: robust effects on self-report but not implicit measures. Front Psychol. 2015;6:1465. doi: 10.3389/fpsyg.2015.01465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christiansen P, Schoenmakers TM, Field M. Less than meets the eye: reappraising the clinical relevance of attentional bias in addiction. Addict Behav. 2015;44:43–50. doi: 10.1016/j.addbeh.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Field M, Marhe R, Franken IH. The clinical relevance of attentional bias in substance use disorders. CNS Spectr. 2014;19(3):225–30. doi: 10.1017/S1092852913000321. [DOI] [PubMed] [Google Scholar]
- 9.Leeman RF, et al. A critical review of the literature on attentional bias in cocaine use disorder and suggestions for future research. Exp Clin Psychopharmacol. 2014;22(6):469–83. doi: 10.1037/a0037806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson TE, Berridge KC. The psychology and neurobiology of addiction: an incentive-sensitization view. Addiction. 2000;95(Suppl 2):S91–117. doi: 10.1080/09652140050111681. [DOI] [PubMed] [Google Scholar]
- 11••.O’Daly OG, et al. Amphetamine sensitization alters reward processing in the human striatum and amygdala. PLoS One. 2014;9(4):e93955. doi: 10.1371/journal.pone.0093955. Historically, incentive sensitization theory has been criticized for reliance on animal models for research evidence. This study adds to a growing body of research evidence demonstrating behavioral and neural incentive sensitization in humans. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filbey FM, et al. fMRI study of neural sensitization to hedonic stimuli in long-term, daily cannabis users. Hum Brain Mapp. 2016 doi: 10.1002/hbm.23250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sjoerds Z, et al. Cue reactivity is associated with duration and severity of alcohol dependence: an FMRI study. PLoS One. 2014;9(1):e84560. doi: 10.1371/journal.pone.0084560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zilverstand A, et al. Cognitive interventions for addiction medicine: Understanding the underlying neurobiological mechanisms. Prog Brain Res. 2016;224:285–304. doi: 10.1016/bs.pbr.2015.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garbusow M, et al. Pavlovian-to-instrumental transfer effects in the nucleus accumbens relate to relapse in alcohol dependence. Addict Biol. 2016;21(3):719–31. doi: 10.1111/adb.12243. [DOI] [PubMed] [Google Scholar]
- 16.Korucuoglu O, Gladwin TE, Wiers RW. Preparing to approach or avoid alcohol: EEG correlates, and acute alcohol effects. Neurosci Lett. 2014;559:199–204. doi: 10.1016/j.neulet.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 17.Koob GFMA, Weiss F, Schulteis G. Opponent process and drug dependence: neurobiological mechanisms. Seminars in the Neurosciences. 1993;5:351–358. [Google Scholar]
- 18.Morie KP, et al. Regulating task-monitoring systems in response to variable reward contingencies and outcomes in cocaine addicts. Psychopharmacology (Berl) 2016;233(6):1105–18. doi: 10.1007/s00213-015-4191-8. [DOI] [PubMed] [Google Scholar]
- 19.McKim TH, Bauer DJ, Boettiger CA. Addiction History Associates with the Propensity to Form Habits. J Cogn Neurosci. 2016;28(7):1024–38. doi: 10.1162/jocn_a_00953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sebold M, et al. Model-based and model-free decisions in alcohol dependence. Neuropsychobiology. 2014;70(2):122–31. doi: 10.1159/000362840. [DOI] [PubMed] [Google Scholar]
- 21.Wiers CE, et al. Effects of cognitive bias modification training on neural alcohol cue reactivity in alcohol dependence. Am J Psychiatry. 2015;172(4):335–43. doi: 10.1176/appi.ajp.2014.13111495. [DOI] [PubMed] [Google Scholar]
- 22•.Kerst WF, Waters AJ. Attentional retraining administered in the field reduces smokers’ attentional bias and craving. Health Psychol. 2014;33(10):1232–40. doi: 10.1037/a0035708. Attentional retraining, in which attention is focused away from drug-related cues, resulted in reduced attentional bias to tobacco-smoking-related cues that was not associated with a change in smoking behavior, but did reduce smoking-related craving. [DOI] [PubMed] [Google Scholar]
- 23•.Ramirez JJ, Monti PM, Colwill RM. Alcohol-cue exposure effects on craving and attentional bias in underage college-student drinkers. Psychol Addict Behav. 2015;29(2):317–22. doi: 10.1037/adb0000028. This study demonstrated that underage college student drinkers express greater subjective craving following in vivo alcohol cue exposure. Exposure to alcohol cues, furthermore, was associated with greater attentional bias to subsequent (i.e., not previously presented) alcohol cues. There was also a positive relationship between craving and attentional bias. It is important to interpret these findings within the context of the subject sample. In other words, study subjects included underage college student drinkers who drank at least one beer on a weekly basis over the past month. Rather than these results being inconsistent with evidence of decreased attentional bias in interventions targeting addicted individuals with well-established learning histories, it may be more appropriate to say these results provide initial evidence for the ineffectiveness of in vivo alcohol cue-exposure as a prevention method. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24•.Ramirez JJ, Monti PM, Colwill RM. Brief and extended alcohol-cue-exposure effects on craving and attentional bias. Exp Clin Psychopharmacol. 2015;23(3):159–67. doi: 10.1037/pha0000018. This study expands on previous work by these authors (see #44) and examined the effect of the “dose” of intervention (i.e., brief versus extended duration in-vivo alcohol cue exposure) on subjective craving and attentional bias in underage college student drinkers. Results indicated no group differences in mean craving or mean attentional bias before or after cue exposure. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woud ML, et al. Alcohol-related interpretation bias in alcohol-dependent patients. Alcohol Clin Exp Res. 2014;38(4):1151–9. doi: 10.1111/acer.12334. [DOI] [PubMed] [Google Scholar]
- 26.Woud ML, et al. The relationship between drinking motives and alcohol-related interpretation biases. J Behav Ther Exp Psychiatry. 2015;47:102–10. doi: 10.1016/j.jbtep.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 27.Woud ML, et al. The manipulation of alcohol-related interpretation biases by means of Cognitive Bias Modification–Interpretation (CBM-I) J Behav Ther Exp Psychiatry. 2015;49(Pt A):61–8. doi: 10.1016/j.jbtep.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 28••.Salemink E, Wiers RW. Alcohol-related memory associations in positive and negative affect situations: drinking motives, working memory capacity, and prospective drinking. Psychol Addict Behav. 2014;28(1):105–13. doi: 10.1037/a0032806. Subjects demonstrated dispositional drinking motives, as measured by the Drinking Motives Questionnaire-Revised (DMQ-R), that were associated with congruent alcohol-related interpretive biases–i.e., enhancement motives (but not coping motives) predicted the tendency to associate alcohol-related words with positive affect situations, whereas coping motives (and not enhancement motives) predicted the tendency to associate alcohol-related words with negative affect situations. Although the alcohol-related interpretive bias in positive affect situations predicted prospective alcohol consumption in individuals with low working memory capacity, this was not observed for alcohol-related interpretive bias in negative affect situations. The reason for the discrepancy is unclear. The authors discuss how treatment optimization efforts may include investigation of therapeutic approaches that combine multiple modalities, such as those discussed in this review paper, including cognitive bias modification (CBM), mindfulness training, and neurocognitive rehabilitation of working memory. The authors also discuss the potential use of neurostimulation techniques (e.g., transcranial direct current stimulation; tDCS) to improve working memory. [DOI] [PubMed] [Google Scholar]
- 29••.Piasecki TM, et al. Dispositional drinking motives: associations with appraised alcohol effects and alcohol consumption in an ecological momentary assessment investigation. Psychol Assess. 2014;26(2):363–9. doi: 10.1037/a0035153. This study examined whether dispositional drinking motives (i.e., enhancement and coping), as measured by the Drinking Motives Questionnaire-Revised (DMQ-R), were associated with perceived consequences of alcohol consumption by drinkers in their natural environments. Based on data collected via ecological momentary assessment, results showed that enhancement motives uniquely predicted real-time reports of enhanced drinking pleasure; and coping motives uniquely predicted real-time reports of increased drinking-contingent relief and punishment. In comparison to coping motives, enhancement motives predicted higher per-episode drink consumption. Findings support that internal/dispositional drinking motives are related to the perceived, or experienced, drinking outcomes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30••.Das RK, Lawn W, Kamboj SK. Rewriting the valuation and salience of alcohol-related stimuli via memory reconsolidation. Transl Psychiatry. 2015;5:e645. doi: 10.1038/tp.2015.132. The implicit development of associations between environmental drug-and-alcohol-related cues and their drug-like effects, rewarding effects, and physical availability are defined in this paper as “maladaptive motivational memory.” These memories are posited to imbue drug-and-alcohol-related cues with enhanced incentive salience that increase their attention-capturing strength; and trigger craving and motivate substance seeking-and-using behavior when the cues are encountered. This paper presents research evidence in support of a novel memory retrieval and intervention procedure for the treatment of substance use disorders. Specifically, this therapeutic approach aims to neutralize maladaptive motivational memories through memory retrieval destabilization (i.e., clinician-guided expectancy violation during memory retrieval) and memory reconsolidation (i.e., counter-conditioning/pairing alcohol cues with aversive visual stimuli). Positive outcomes, including reduction of attentional bias, are reported based on the results of a randomized, controlled clinical trial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31••.Hon T, Das RK, Kamboj SK. The effects of cognitive reappraisal following retrieval-procedures designed to destabilize alcohol memories in high-risk drinkers. Psychopharmacology (Berl) 2016;233(5):851–61. doi: 10.1007/s00213-015-4164-y. This study expands on previous work by these authors (see #51) examining memory modification as a therapeutic approach for treating alcohol use disorder. In this study, the memory destabilization component is maintained, but instead of counter-conditioning, the investigators examined whether reappraisal of maladaptive alcohol cognitions performed during alcohol memory network instability affected subsequent alcohol memory. Put another way, investigators sought to determine if memory destabilization + cognitive reappraisal led to enhanced memory for reappraisals generated to counteract maladaptive appraisals. Results were mixed: memory destabilization conducted through prediction error-generating procedures, but not value prediction error-generating procedures, was associated with significant reductions in verbal fluency for positive alcohol-related words. This study provides partial preliminary support for the idea that reappraisal in the context of memory retrieval destabilization can alter accessibility of alcohol semantic networks. But further research is needed to determine if cognitive reappraisal techniques can enhance retrieval of reappraisals generated to counteract maladaptive appraisals. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stanovich KE. Distinguishing the reflective, algorithmic, and autonomous minds: is it time for a tri-process theory? In: Frankish JSBTEaK., editor. Two Minds: Dual Processes and Beyond. Oxford University Press; Oxford, UK: 2009. pp. 55–88. [Google Scholar]
- 33••.Wasmuth SL, et al. Metacognition in persons with substance abuse: Findings and implications for occupational therapists. Can J Occup Ther. 2015;82(3):150–9. doi: 10.1177/0008417414564865. Investigators in this study used a semi-structured interview to characterize individuals with one or more substance use disorders in comparison to other psychiatric outpatient groups on metacognitive ability. Results showed that addicted individuals were impaired in mastery (i.e., capacity to use knowledge of oneself and others to respond to psychological and social challenges) but not other areas of metacognition including self-reflectivity, understanding others’ thoughts, and decentering in comparison to other psychiatric groups. [DOI] [PubMed] [Google Scholar]
- 34••.Balconi M, Finocchiaro R, Campanella S. Reward sensitivity, decisional bias, and metacognitive deficits in cocaine drug addiction. J Addict Med. 2014;8(6):399–406. doi: 10.1097/ADM.0000000000000065. This study operationalized metacognition as self-knowledge of cognitive strategy used during a decision-making task in four domains (i.e., awareness, application, appraisal, openness to modification). Results indicated that patients with substance use disorders demonstrate less self-knowledge on all four indices in comparison to healthy control subjects, but perceive their approaches to be more flexible and efficacious. [DOI] [PubMed] [Google Scholar]
- 35•.Hajloo N, et al. The Role of Meta-cognition in Students’ Addiction Potential Tendency. Int J High Risk Behav Addict. 2014;3(1):e9355. doi: 10.5812/ijhrba.9355. There is little evidence to comment on the comparative influence of predisposing cognitive factors versus acquired deficits on metacognitive functioning. However, this study examined the correlation between college students’ responses on questionnaires measuring metacognition and “addiction potential tendency.” Results of that study showed student addiction potential tendency was associated with maladaptive metacognitive functioning on three out of five subscales including beliefs about the need for controlling thoughts, positive beliefs about worry, and negative beliefs about riskiness and uncontrollability; but not lack of cognitive self-confidence, or cognitive self-awareness. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.May J, Kavanagh DJ, Andrade J. The Elaborated Intrusion Theory of desire: a 10-year retrospective and implications for addiction treatments. Addict Behav. 2015;44:29–34. doi: 10.1016/j.addbeh.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 37.Moeller SJ, et al. Functional, structural, and emotional correlates of impaired insight in cocaine addiction. JAMA Psychiatry. 2014;71(1):61–70. doi: 10.1001/jamapsychiatry.2013.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moeller SJ, Goldstein RZ. Impaired self-awareness in human addiction: deficient attribution of personal relevance. Trends Cogn Sci. 2014;18(12):635–41. doi: 10.1016/j.tics.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garland EL, Froeliger B, Howard MO. Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Front Psychiatry. 2014;4:173. doi: 10.3389/fpsyt.2013.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Garland EL. Restructuring reward processing with Mindfulness-Oriented Recovery Enhancement: novel therapeutic mechanisms to remediate hedonic dysregulation in addiction, stress, and pain. Ann N Y Acad Sci. 2016;1373(1):25–37. doi: 10.1111/nyas.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karyadi KA, VanderVeen JD, Cyders MA. A meta-analysis of the relationship between trait mindfulness and substance use behaviors. Drug Alcohol Depend. 2014;143:1–10. doi: 10.1016/j.drugalcdep.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baer RA, et al. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 43.Chiesa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Subst Use Misuse. 2014;49(5):492–512. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- 44.Bowen S, et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry. 2014;71(5):547–56. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McConnell PA, Froeliger B. Mindfulness, Mechanisms and Meaning: Perspectives from the Cognitive Neuroscience of Addiction. Psychol Inq. 2015;26(4):349–357. doi: 10.1080/1047840X.2015.1076701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Witkiewitz K, et al. Mindfulness-based treatment to prevent addictive behavior relapse: theoretical models and hypothesized mechanisms of change. Subst Use Misuse. 2014;49(5):513–24. doi: 10.3109/10826084.2014.891845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47•.Hagen E, et al. Assessment of Executive Function in Patients With Substance Use Disorder: A Comparison of Inventory- and Performance-Based Assessment. J Subst Abuse Treat. 2016;66:1–8. doi: 10.1016/j.jsat.2016.02.010. Subjective measures of executive function are gaining in popularity. Their clinical significance, however, isn’t entirely clear. In this paper, patients being treated for a substance use disorder (SUD) performed worse than control subjects on measures of general cognitive ability, word reading, color naming, color naming of congruent color and word combinations, and visual-motor numerical sequencing. Groups did not differ on performance measures of executive function including inhibitory control, letter-number sequencing/shifting, and decision-making. However, the SUD patients reported more executive dysfunction than healthy control subjects on a subjective executive function questionnaire. Test sensitivity is based on the proportion of true positives in comparison to a “gold standard.” Since the questionnaire is the individual’s appraisal of their ability rather than their actual ability, these results indicate that SUD patients are more likely to over-report executive dysfunction on a questionnaire. This may be related to reading or other comprehension difficulties, yea-saying bias, or unknown motivational differences. Given the subjective nature of the inventory measure, however, this may be a more useful indicator of metacognitive self-awareness – i.e., indicating less accurate awareness or appraisal of one’s executive ability. More research is needed to clarify the clinical significance of discrepancies between executive function performance and appraisal of ability. [DOI] [PubMed] [Google Scholar]
- 48.Conroy DA, et al. Impact of marijuana use on self-rated cognition in young adult men and women. Am J Addict. 2015;24(2):160–5. doi: 10.1111/ajad.12157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garavan H, et al. Dissociable executive functions in the dynamic control of behavior: inhibition, error detection, and correction. Neuroimage. 2002;17(4):1820–9. doi: 10.1006/nimg.2002.1326. [DOI] [PubMed] [Google Scholar]
- 50.Smith JL, et al. Deficits in behavioural inhibition in substance abuse and addiction: a meta-analysis. Drug Alcohol Depend. 2014;145:1–33. doi: 10.1016/j.drugalcdep.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 51.Moody L, et al. Impulsivity and polysubstance use: A systematic comparison of delay discounting in mono-, dual-, and trisubstance use. Exp Clin Psychopharmacol. 2016;24(1):30–7. doi: 10.1037/pha0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schulte MH, et al. Recovery of neurocognitive functions following sustained abstinence after substance dependence and implications for treatment. Clin Psychol Rev. 2014;34(7):531–50. doi: 10.1016/j.cpr.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 53.Spechler PA, et al. Response inhibition and addiction medicine: from use to abstinence. Prog Brain Res. 2016;223:143–64. doi: 10.1016/bs.pbr.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 54.Conrod PJ, Nikolaou K. Annual Research Review: On the developmental neuropsychology of substance use disorders. J Child Psychol Psychiatry. 2016;57(3):371–94. doi: 10.1111/jcpp.12516. [DOI] [PubMed] [Google Scholar]
- 55.Albein-Urios N, et al. The value of impulsivity to define subgroups of addicted individuals differing in personality dysfunction, craving, psychosocial adjustment, and wellbeing: a latent class analysis. Arch Clin Neuropsychol. 2014;29(1):38–46. doi: 10.1093/arclin/act072. [DOI] [PubMed] [Google Scholar]
- 56.Ahn WY, et al. Utility of Machine-Learning Approaches to Identify Behavioral Markers for Substance Use Disorders: Impulsivity Dimensions as Predictors of Current Cocaine Dependence. Front Psychiatry. 2016;7:34. doi: 10.3389/fpsyt.2016.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bidwell LC, et al. Novelty Seeking as a Phenotypic Marker of Adolescent Substance Use. Subst Abuse. 2015;9(Suppl 1):1–10. doi: 10.4137/SART.S22440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stevens L, et al. Impulsive choice predicts short-term relapse in substance-dependent individuals attending an in-patient detoxification programme. Psychol Med. 2015;45(10):2083–93. doi: 10.1017/S003329171500001X. [DOI] [PubMed] [Google Scholar]
- 59.Hamilton KR, et al. Choice impulsivity: Definitions, measurement issues, and clinical implications. Personal Disord. 2015;6(2):182–98. doi: 10.1037/per0000099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hamilton KR, et al. Rapid-response impulsivity: definitions, measurement issues, and clinical implications. Personal Disord. 2015;6(2):168–81. doi: 10.1037/per0000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Balogh KN, Mayes LC, Potenza MN. Risk-taking and decision-making in youth: relationships to addiction vulnerability. J Behav Addict. 2013;2(1) doi: 10.1556/JBA.2.2013.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hulka LM, et al. Changes in cocaine consumption are associated with fluctuations in self-reported impulsivity and gambling decision-making. Psychol Med. 2015;45(14):3097–110. doi: 10.1017/S0033291715001063. [DOI] [PubMed] [Google Scholar]
- 63.Stevens L, et al. Impulsivity in cocaine-dependent individuals with and without attention-deficit/hyperactivity disorder. Eur Addict Res. 2015;21(3):131–43. doi: 10.1159/000369008. [DOI] [PubMed] [Google Scholar]
- 64.Bickel WK, et al. Competing neurobehavioral decision systems theory of cocaine addiction: From mechanisms to therapeutic opportunities. Prog Brain Res. 2016;223:269–93. doi: 10.1016/bs.pbr.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.McClure SM, Bickel WK. A dual-systems perspective on addiction: contributions from neuroimaging and cognitive training. Ann N Y Acad Sci. 2014;1327:62–78. doi: 10.1111/nyas.12561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gullo MJ, Loxton NJ, Dawe S. Impulsivity: four ways five factors are not basic to addiction. Addict Behav. 2014;39(11):1547–56. doi: 10.1016/j.addbeh.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 67.Konova AB, Moeller SJ, Goldstein RZ. Common and distinct neural targets of treatment: changing brain function in substance addiction. Neurosci Biobehav Rev. 2013;37(10 Pt 2):2806–17. doi: 10.1016/j.neubiorev.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chiou WB, Wu WH, Chang MH. Think abstractly, smoke less: a brief construal-level intervention can promote self-control, leading to reduced cigarette consumption among current smokers. Addiction. 2013;108(5):985–92. doi: 10.1111/add.12100. [DOI] [PubMed] [Google Scholar]
- 69.Duckworth AL, Gendler TS, Gross JJ. Situational Strategies for Self-Control. Perspect Psychol Sci. 2016;11(1):35–55. doi: 10.1177/1745691615623247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bickel WK, et al. Remember the future: working memory training decreases delay discounting among stimulant addicts. Biol Psychiatry. 2011;69(3):260–5. doi: 10.1016/j.biopsych.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bickel WK, et al. Therapeutic Opportunities for Self-Control Repair in Addiction and Related Disorders: Change and the Limits of Change in Trans-Disease Processes. Clin Psychol Sci. 2015;3(1):140–153. doi: 10.1177/2167702614541260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bickel WK, Moody L, Quisenberry A. Computerized Working-Memory Training as a Candidate Adjunctive Treatment for Addiction. Alcohol Res. 2014;36(1):123–6. [PMC free article] [PubMed] [Google Scholar]


