Abstract
The conflict in Syria has created the largest humanitarian emergency of the twenty-first century. The 4-year Syrian conflict has destroyed hospitals and severely reduced the capacity of intensive care units (ICUs) and on-site intensivists. The crisis has triggered attempts from abroad to support the medical care of severely injured and acutely ill civilians inside Syria, including application of telemedicine. Within the United States, tele-ICU programs have been operating for more than a decade, albeit with high start-up costs and generally long development times. With the benefit of lessons drawn from those domestic models, the Syria Tele-ICU program was launched in December 2012 to manage the care of ICU patients in parts of Syria by using inexpensive, off-the-shelf video cameras, free social media applications, and a volunteer network of Arabic-speaking intensivists in North America and Europe. Within 1 year, 90 patients per month in three ICUs were receiving tele-ICU services. At the end of 2015, a network of approximately 20 participating intensivists was providing clinical decision support 24 hours per day to five civilian ICUs in Syria. The volunteer clinicians manage patients at a distance of more than 6,000 miles, separated by seven or eight time zones between North America and Syria. The program is implementing a cloud-based electronic medical record for physician documentation and a medication administration record for nurses. There are virtual chat rooms for patient rounds, radiology review, and trainee teaching. The early success of the program shows how a small number of committed physicians can use inexpensive equipment spawned by the Internet revolution to support from afar civilian health care delivery in a high-conflict country.
Keywords: telemedicine, health services, civil disorder
There is a long tradition of physicians providing medical care in conflict areas. At present, physicians with Médecins Sans Frontières, the Red Cross or Red Crescent, or several national Armed Forces care for patients in dangerous environments (1, 2). But some conflict areas are too risky for direct engagement of even the most dedicated humanitarian organizations. In less risky areas, access to patients and hospital facilities is sometimes denied by government or irregular forces. People then die of otherwise survivable illness or trauma.
Intensive care physicians have traditionally provided care only at the bedside, but there is a growing tele–intensive care unit (tele-ICU) movement, which can leapfrog distance, time zone differences, and physical barriers to link providers to on-site caregivers and their patients. Although potentially cost-effective in appropriate settings, tele-ICU programs often take years of planning, capital investment, legal contracting, medical licensing, and medical staff approval before implementation in U.S. hospitals (3). The prevailing models for domestic tele-ICU programs require considerable modification for application in high-conflict areas where civil society may be severely degraded and rapid deployment is needed to address acute health care crises.
Here, we describe how a tele-ICU program can, in fact, be rapidly deployed, with minimal cost, to bridge 6,000 miles of distance and provide critical care to civilians suffering severe injuries or an acute illness in an active war zone (4). A description of the Syria Tele-ICU program, which is the focus of this report, has been previously described in the form of an abstract (5).
Background
The Syrian Republic has operated modern medical facilities, especially in the large cities, for many years. Hospitals had sophisticated cardiac, trauma and neurosurgery programs, large intensive care units equipped with modern technology, medical schools, and postgraduate training programs (6). However, since 2011, conflict has destroyed much of the country’s acute care infrastructure. Thousands of physicians have become refugees or have been killed (7, 8). For instance, by 2012, only 35 physicians remained in one-half of the city of Aleppo, the largest city in Syria, to care for 2.5 million people (9). Although some hospitals have been destroyed, even physically intact ICUs have operated at low capacity because there are no physicians to supervise nurses and manage critically ill patients after they are initially stabilized by emergency and trauma services.
Initial Idea and Needs Assessment
The impetus for development of the Syria tele-ICU project arose on September 2012 when one of the authors (A.M.) viewed a YouTube video of a street scene in Homs, Syria. The video showed an injured civilian receiving cardiopulmonary resuscitation. It was obvious that resuscitation was being performed poorly. The patient died. The initial idea was to create a training curriculum to improve emergency medical service and bystander trauma stabilization for civilians caught in the conflict. But further investigation revealed that even if people survived transport to a hospital, they could not receive adequate care because much of the critical care infrastructure, especially medical staff, had been severely degraded by the conflict. The focus changed to providing remote, around-the-clock care to patients who need ICU services and to stabilizing patients to transfer them to neighboring countries.
A rudimentary needs assessment determined that equipment, nurse training, and remote-access medical advice were most needed in hospitals near conflict areas that were outside of Syrian government control and that had a severe shortage of trained critical care physicians. Funds were raised from the Syrian-American Medical Society (SAMS) ($15,000) and personal resources ($15,000) to purchase equipment and airfare to Turkey.
Program Preparation and Early Development
One month after viewing the YouTube video, A.M. held a 1-week training course in Antakya, Turkey for 17 nurses working in Syrian hospitals. They were given lectures on basic ventilator management, advanced cardiac life support, and acute trauma care. They were also trained in case presentation skills and to receive and implement telephone orders from distant providers. The nurses brought back to their Syrian ICUs two ventilators, two cardiac monitors, a defibrillator, and other ICU basic devices such as endotracheal tubes, central venous catheters, and critical care medications. They also received a Turkish satellite Internet phone, Internet protocol (IP) cameras, a laptop computer, and Bluetooth headphones. Encouraged by this initial experience, A.M. recruited other Syrian Americans to participate in designing and staffing a tele-ICU program designed to support clinicians serving seriously ill or injured civilians in Syrian ICUs. Tele-ICU operations commenced in December 2012 and cared for 40 injured patients at the frontline in a suburban area of the city of Idlib in northern Syria.
In March 2013, the Syria Tele-ICU program expanded to provide remote critical care at the largest trauma center in the section of Aleppo not under Syrian government control. On the basis of patient logs kept by tele-providers and the on-site ICU, within 3 months the tele-ICU program was caring for approximately 40 patients per month with monitoring of three beds and three ventilators. In June 2013, at the request of the Aleppo medical committee, the only medical authority in the city, the program expanded to support two other trauma centers in Aleppo. By the end of 2013, the Syria Tele-ICU program served approximately 90 patients per month in Aleppo. On the basis of incomplete records kept by the tele-ICU program and the on-site facilities, patients were mostly civilians between 20 and 30 years of age. Approximately 80% of the patients suffered multiple traumatic injuries. Approximately 40% died, and 20% required transfer to hospitals in Turkey.
In January 2014, tele-ICU services were expanded to assist two physicians caring for patients at the Bab Al-Hawa Hospital, which is a referral center at the Syria–Turkey border. This center used tele-ICU services for 7 months but stopped after a physician trained in critical care started working on site and declined tele-ICU assistance. In May 2015, tele-ICU was started at a major hospital in a Damascus suburb. In June 2015, a small ICU in Idlib that has only nurses on site was added.
Additional support was obtained to add three more ICUs in the Idlib area. One of those centers is to be a referral center with nine ICU beds. In summary, the Syria Tele-ICU program currently supports five ICUs and plans to support 10 more hospitals in early 2016.
Technology
The Syria Tele-ICU program uses satellite Internet, IP cameras, and laptops at each site. Free social media and communication applications such as Skype, Viber, Google Hangout, and WhatsApp allow communication in Arabic with text, audio, still images, and video (Figure 1). Progress notes were initially recorded in Google Docs. The program then changed to documenting patient reports in group messaging rooms in the Viber or WhatsApp application.
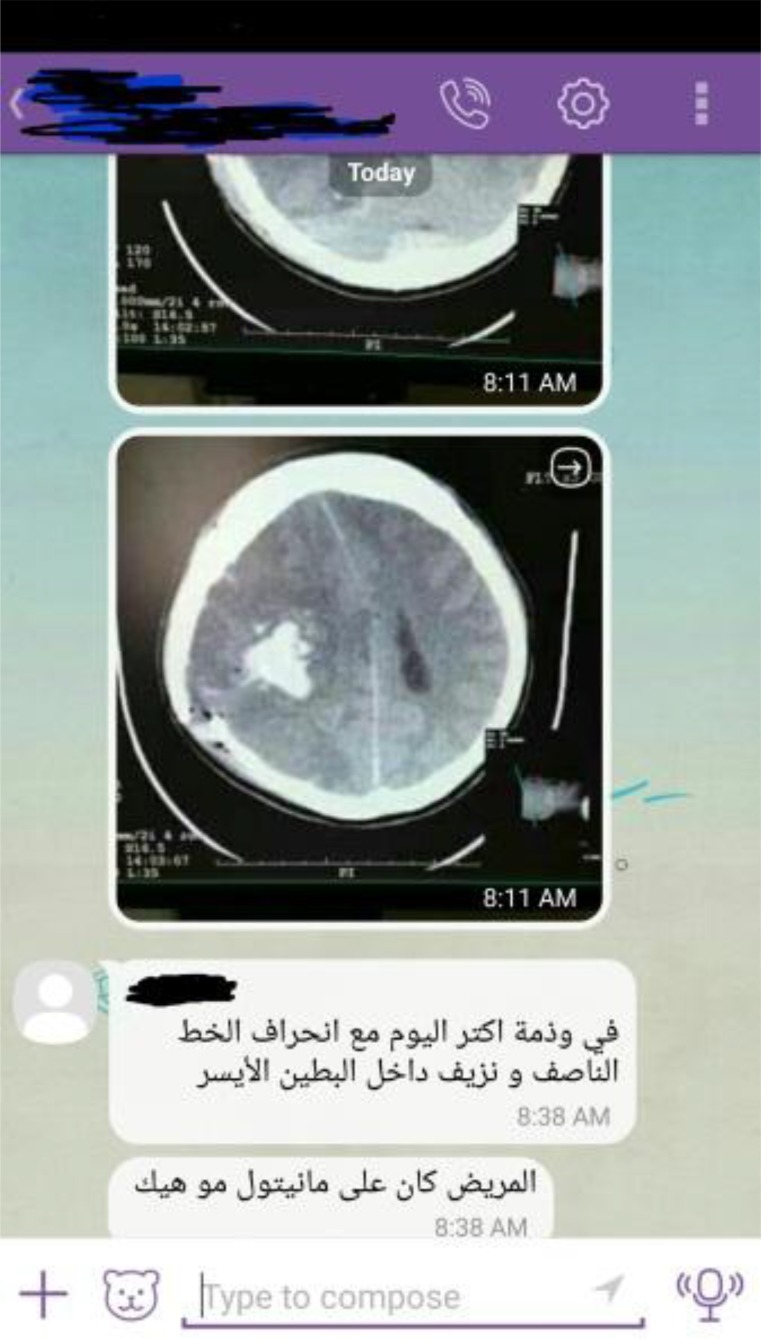
Figure 1.
De-identified screen shot taken from a tele-ICU physician’s smartphone using the Viber application. This is an example of a real-time chat room with texted discussion about findings on a head CT examination that was photographed on site and made available to the clinicians in the chat room. For this case, the primary intensivist, a neuro–critical care physician, and several on-site physicians were simultaneously managing the patient with brain injury. The text in the boxes was written by the neuro-intensivist and is translated as “There is worsening edema and right intraventricular hemorrhage. The patient is still on mannitol, correct?”
In August 2015, a more structured EMR system was implemented using web-based software provided by a commercial EMR company for $200. The EMR was modified to operate in Arabic and in a low-resource environment with the frequent connectivity difficulties that are inherent in a conflict area (Figure 2; and see Figures E1–E3 in the online supplement).
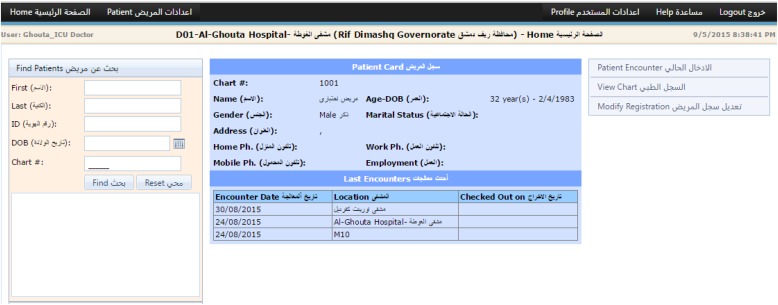
Figure 2.
Picture of the main electronic medical record (EMR) page developed for the tele-ICU program, showing a “test” patient. This EMR software was donated by Basil Bakri and Orient Innovations, LLC. Many modules were removed or simplified so that the EMR could run on a slow Internet connection. Headers were translated into Arabic.
The EMR has unique medical record numbers with patient identifiers anonymized to the remote physicians. There is a Progress Notes section; a Medication Administration Record, where nurses can chart medication times; and an integrated on-line call schedule for tele-intensivists and on-site personnel. All notes are written in Arabic, including nurses’ end-of-shift notes, except for “sign-out” notes written in English by the tele-ICU physicians to communicate among themselves. Even though the new EMR has greater data capability than the “home-grown” applications used in the first 3 years, implementation has been slow because it requires more user training, runs slowly on limited Internet bandwidth, and takes busy nurses away from the bedside to document their care plan in the EMR.
The EMR allows direct viewing of radiology images within the EMR application if the images are obtained by digital technology. Previously, on-site providers used smartphones to take still or video recordings of the radiology images and then send the images to the remote physicians (Figure 3). Because chest and portable radiographs are still performed using hard-copy films, the photograph–send method continues for some images. The EMR also has a planned, automated inventory control; when a device or medication falls below 30% of stock inventory, an e-mail would be sent to relief agencies such as SAMS to resupply. Because of EMR and e-mail compatibility issues, this process is not yet active.
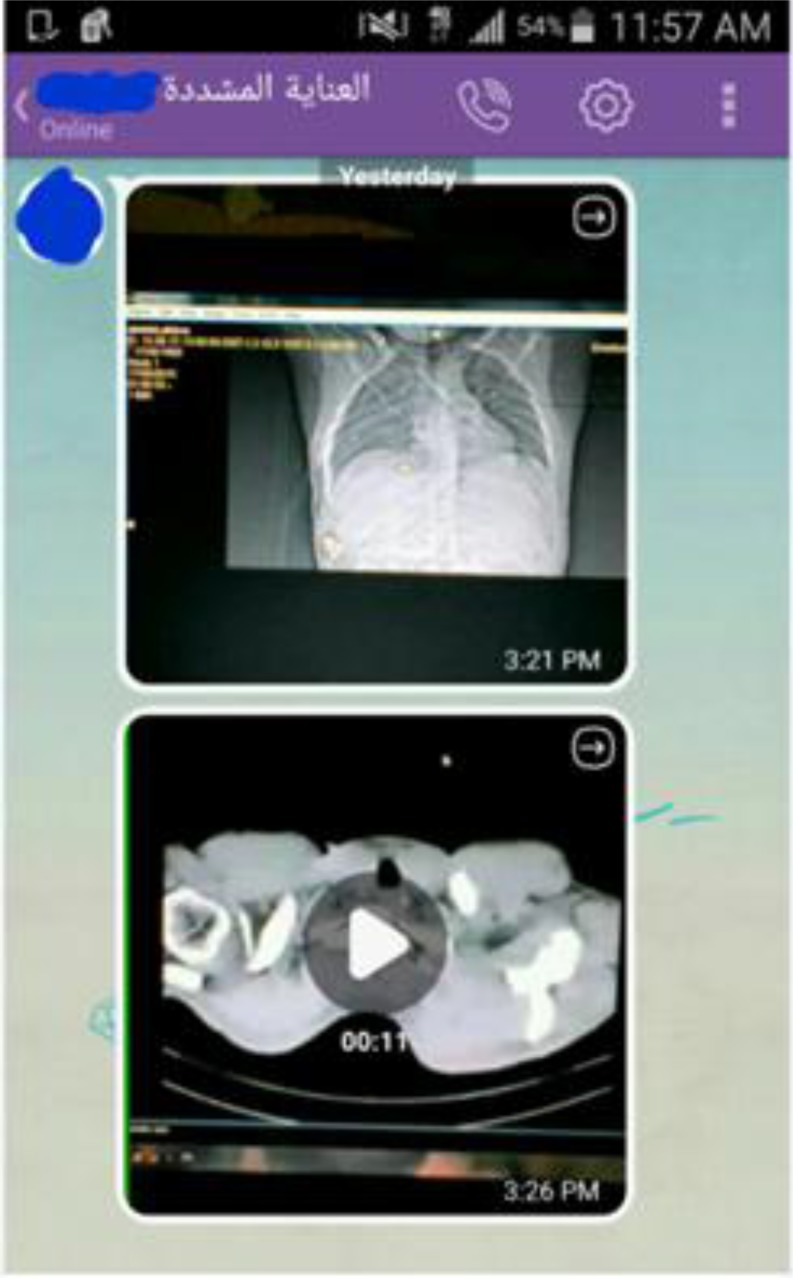
Figure 3.
De-identified screen shot taken from a tele-ICU physician’s smartphone using the Viber application. This shows how chest CT images were transmitted before the new electronic medical record (EMR) was available. An on-site provider shot a smartphone video of the hospital’s computer screen while scrolling through the CT images. The tele-ICU physician then replayed the video on his or her smartphone or laptop.
Operations
At the time of this writing 20 physicians participate in the telemedicine program. Some learned about the program as members of SAMS; others have learned by word of mouth. Most of the current participants have trained in pulmonary and critical care medicine. There are also neurological intensivists. Others are consultants in thoracic surgery, orthopedics, pediatrics, and radiology. Almost all reside in the United States and Canada. All of the work is unpaid. There is minimal training. The time commitment can be substantial.
Medical education and patient care in Syria is conducted in Arabic. Many speakers of Arabic who have not lived in Syria or other Arabic-speaking regions for many years have forgotten Arabic words for medical terminology. Sometimes a Syria Tele-ICU physician has to ask for assistance from a younger colleague who has practiced medicine in Arabic more recently.
Routinely, pairs of intensivists are scheduled to provide real-time telemedicine support 24 hours a day on 7-day rotations. They cover all of the patients in one or two ICUs, depending on the patient care load. One physician creates the tele-schedule. There is no formal peer-review process for medical care. There are ad hoc electronic meetings of the program leaders to discuss issues and to plan program development.
The 7- to 8-hour time zone disparity makes tele-ICU care difficult. Tele-rounds, educational sessions, and chat rooms are started as early as possible in Syria (6:00–7:00 a.m.). The starting time is 10:00–11:00 p.m. in the U.S. Midwest. Teaching sessions at 7:00 a.m. educate on-site clinicians who are completing and starting 24-hour shifts. Any follow-up calls during the day in Syria take place in the middle of the night in the United States, making sleep interruption common. Similarly, patient care needs in the evening in Syria require the attention of the tele-ICU physician during their busy regular working day. Mass casualty situations require many hours of continuous tele-ICU time.
Working on this schedule, Syria Tele-ICU physicians have cared for patients injured in attacks causing multiple causalities. For instance, on April 30, 2014 tele-ICU physicians remotely cared for the surviving victims of the Ein Jalout school attack, where more than 30 children and teachers were killed (10). After emergency department treatment, the tele-ICU triaged victims, managed postoperative care, provided orders to the nursing staff, and directed transfers between local hospitals or to Turkey when needed. In May 2014, the program cared for five female victims of chlorine gas attacks in a suburb of Idlib (11). All developed acute respiratory distress syndrome and required mechanical ventilation. All survived, with one patient needing transfer to Turkey.
Syria Tele-ICU system physicians also assist in triage decisions. The severity of each case is evaluated by a tele-ICU provider, who makes recommendations to transfer the patient to another facility or neighboring country or to continue care on site. If transfer is needed, the intensivist can remotely evaluate the capacity of each referral center and assess available expertise and supplies.
It is important to note that these decisions are made in a rapidly changing war-time environment. Battle lines and besieged areas can change unexpectedly, so “transfer protocols” are quickly obsolete. Some ICUs cannot be evacuated and patients live or die on site. Some transfer decisions are made on the basis of estimated length of stay. Longer term patients are moved to Turkey, if possible, to open up beds closer to the front lines.
In 2014, the program began to connect different providers to manage a single patient. For instance, a virtual Skype room was formed to discuss thoracic surgery cases in Aleppo. Thoracic surgeons in the United States advised general surgeons whether to proceed with procedures on site or to transfer stabilized patients to border hospitals where thoracic surgeons were available. At times, five physicians with different specialty skills in five locations across the globe used the tele-ICU system to care for the same patient (Figure E4).
By providing direct patient care, Syria Tele-ICU physicians learn which patient care protocols are most needed by on-site staff and how to modify them for implementation in a resource-limited environment. The first protocols were for ventilator weaning, antibiotic use, sedation, and treatment of chlorine gas exposure.
The extent of tele-ICU assistance depends on on-site resources. Some hospitals in northern Syria only have nurses in the ICUs to care for patients. When there is a need, the nurse calls the scheduled covering tele-physician within 20 minutes of admission. The case is discussed online and physician orders are placed afterward. Throughout the day, the nurses follow up with the tele-intensivist through text messaging and video applications. If the primary tele-ICU physician does not answer or is not available, a designated back-up physician responds.
Communication is by real-time voice or text or, more recently, by the Viber speech-recording application. A clinician can record a 20-second voice message communicating a clinical question or recommendation or a medical order and send it so that the message can be played back almost immediately by the receiver. This type of communication is faster than texting, more reliable with spotty Internet connections, and safer to use when the tele-ICU physicians are driving. If necessary, tele-physicians can view patients via IP cameras when on-site consent is given (Figure 4).
Figure 4.
Photograph of an ICU bed in one of the tele-ICU hospitals. The white device at the top is the tele-ICU camera. There is a telemetry monitor on the wall, a ventilator, and unidentified equipment by the bed. The bed is located in a five-bed cluster in an ICU ward. Four beds are for patient care; the remaining one is for the ICU nurse to sleep. In this hospital, ICU nurses work 12-hour shifts, alternating with a paired nurse. They have 2- to 3-month commitments during which they rarely leave the hospital.
Another method of tele-ICU coverage engages on-site physicians in training who are not yet fully capable in critical care medicine, often because their formal training was interrupted by the conflict. Medical students and some residents rotate on service for 24-hour shifts. They are expected to contact the assigned tele-ICU physician shortly after seeing a critically ill patient. The program developed an on-line virtual conference room that nurses, medical students, and physicians attend. The tele-intensivists “round” daily on the patients as they are presented by the on-site staff while also providing general lectures on critical care topics.
Planned Program Expansion
In 2015, SAMS received an $850,000 grant to expand ICU capacity in Syria. The plan includes provision of tele-ICU services in new ICUs. The funding will enable expansion of the Syria Tele-ICU program to support 10 hospitals in addition to an existing surgical/medical intensive care unit in a suburb of Damascus. The grant will provide partial salary support for on-site nurses and physicians, but that is independent of the tele-ICU program. Portable pulmonary function and electrocardiogram machines will be purchased. Training videos for on-site personnel will be produced and streamed over a faster, but more costly, Internet connection.
Program expansion will require recruiting additional Arabic-speaking intensivists from around the world. Although many intensivists want to help in this humanitarian project, language is often an obstacle.
Obstacles
The greatest obstacle to patient care inside Syria is patient and medical staff safety. Each of the tele-ICU hospitals located in the northern part of Syria has been attacked, sometimes leading to loss of life of providers and partial or total destruction of facility or tele-ICU equipment (Figures 5A–5C). For instance, there was no real-time video camera coverage in Aleppo for 6 months. The program had to use recorded video or cellphone webcams instead.
Figure 5.
Photographs of damage to one of the hospitals with a tele-ICU near Aleppo after an attack in February 2014. (A) An ICU patient room damaged by bombing. The white device on the boom is the tele-ICU camera. There are two bag-mask resuscitation devices on the wall and medical equipment strewn about the room. (B) Damaged operating room with portable lights, operating table, anesthesia machine, and monitor. (C) Damaged emergency medical vehicle and automobiles just outside the hospital
When a hospital is located in a besieged area, defective medical or communication equipment cannot be replaced, so tele-ICU services are interrupted. Also, the satellite phone Internet connections do not always work, and therefore land-based alternatives must be developed. The tele-ICU program operates in areas where various fighting groups are in active conflict. To provide medical care under the ethics of the medical profession that requires that all patients be treated equally, the tele-ICU program provides services to hospitals without military or political relationships. Patients are de-identified for the tele-ICU program and on-site providers are expected to provide equal care to every patient.
Discussion
An aphorism for telemedicine is “Move knowledge, not patients.” In dangerous environments, that precept is even more relevant because the absence of even a few doctors can negatively affect the survival of hundreds of patients. Early experience implementing the Syria Tele-ICU program demonstrates that widely available, low-cost, web-based communication technology can be quickly assembled by a few individuals to provide clinical critical care decision support from thousands of miles away (Figure 6). Elements common to U.S. domestic tele-ICU programs such as care protocols, electronic progress notes, remote video viewing of patients and conversations with on-site staff, real-time medical orders based on the patient’s current condition, patient triage decisions, and physician shift scheduling can be implemented at a great distance under adverse conditions.
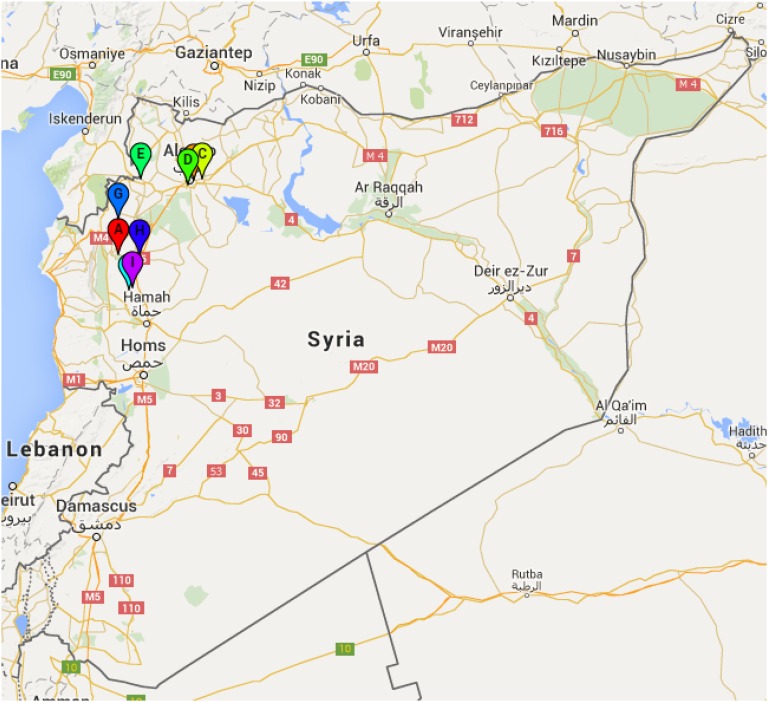
Figure 6.
Google map of Syria and surrounding area, with markers for hospitals served by the tele-ICU program. The Mediterranean Sea is to the west, on the left side of the map, Turkey to the north, and Iraq to the south. Aleppo, in the northern region, is partially obscured by the markers. Hospital A (orange marker near Aleppo) was the first tele-ICU, but is no longer in service because of multiple attacks. Hospitals B, C, D, and H (light blue, yellow, green, and dark blue markers) are currently in service. Two other health care facilities are also in service, but we have not located them on the map because of security concerns. Hospital E (light green marker) was in the tele-ICU program, but stopped service when they had sufficient personnel on site to function independently. Sites G and I (light blue and purple markers) are expected start operating shortly, along with one other site not located on the map for security reasons.
Although informed by the experience of domestic U.S. tele-ICU programs (3), the Syria Tele-ICU program differs from those programs in key respects. Time from initiation of planning to implementation is one example. The Syria Tele-ICU program started serving patients within 2 months of inception. Speedy implementation was possible in part because the program was designed to be “bare bones” in structure. The absence of civil society in areas of Syria meant that bureaucratic obstacles such as program accreditation or credentialing were absent.
The operating costs for the Syria Tele-ICU medicine program also differ dramatically from costs for U.S. domestic tele-ICU services. Most tele-ICU programs in the United States are funded by hospitals, health systems, or independent tele-ICU companies and have operating budgets measured in hundreds of thousands or millions of dollars annually. They support secure, well-equipped ICUs that often have on-site, overnight physician staff coverage. They use proprietary and costly ICU data management systems and tele-communication technology, have contingency plans for loss of power or communication, and compile monthly reports on outcomes and user experience (3).
Because the Syria Tele-ICU program is a virtual network, there is no need to build and equip tele-ICU physical command centers. Participating clinicians are unpaid, and there are no paid tele-ICU nurses engaged in patient monitoring. At present, the annual operating budget for the Syria Tele-ICU program is about $1,000 per year not including out-of-pocket expenses for program volunteers and compensation for clinicians working within Syria. Almost all of the operating budget covers satellite Internet costs. Capital support for new cameras or medications comes from nongovernmental organization grants, physician humanitarian organizations such as SAMS and the Syrian Expatriates Organization. Free communication software and tablet apps can be updated or replaced expeditiously at no additional expense. The low operating costs of this program are contrary to expectations communicated in a 2014 report summarizing a 2008 survey on the state of telemedicine in Syria. The authors concluded that “Given the poor condition of infrastructure, the application of telemedicine in Syria will incur a considerable cost” (12).
Other nongovernmental transnational telemedicine programs are serving patients residing in low-resource countries elsewhere in the world. One publication describes nine tele-health programs plus three others supported by the Médecins Sans Frontières organization (13, 14). Most such transnational nongovernmental telemedicine programs are supported by long-term contracts with university, government, or humanitarian organizations. Many operate in geographically remote ambulatory care settings using “store-and-forward” technology to transmit clinical information and advice between local clinicians and distant experts. Consultants read a medical history and view static images depicting surface lesions, radiographs, and histopathology slides as appropriate. A review of six mature programs, functioning for at least 7 years, reported that the average response time for medical advice was 24 hours (14). The Syria Tele-ICU program differs operationally from these other transnational efforts in the speed of direct, two-way communications and the need for real-time engagement in medical decision-making that is required to provide acute critical care services.
The Syria Tele-ICU program also contrasts with many “disaster preparedness” programs developed by national or regional governmental agencies or medical professional organizations. Detailed planning documents have been developed to advise hospitals and civil response teams on preparing for and responding to mass casualty incidents, natural disasters, or epidemics. One prominent example is a consensus statement published by the American College of Chest Physicians on the care of the critically ill and injured during pandemics and disasters (15).
Most of these programs prepare emergency respondents to provide short- or intermediate-term health care support in the event of an unanticipated disaster or an infectious disease outbreak that overwhelms otherwise high-functioning local health care resources and facilities for a limited period of time. Full cooperation of government authorities and surviving health care providers is assumed. Planning efforts focus on rapid deployment of health care personnel and expedited delivery of medical supplies to the affected area. In contrast, the Syria Tele-ICU program is designed to operate remotely in a hostile environment where local health care providers function under continuing threat. Because there are no short-term prospects for restoration of local critical care medicine capacity in the targeted service areas, the Syria Tele-ICU program is designed to continue operations for an indefinite period of time.
Conclusions
The meteoric rise of the information technology industry has occurred, in part, through the creation of low-cost technologies that allow instantaneous human communication at great distances. For many physicians and nurses, social media applications are a convenient way to communicate with family and friends. The early success of the Syria Tele-ICU program shows how a small number of committed physicians can use this same technology to support in real time, from afar, the critical care of acutely ill or injured civilians in a high-conflict country. Anticipated expansion of the program to support more ICUs within Syria will enable further refinement of the Syria Tele-ICU operating model and initiation of outcomes research that can be applied to future tele-ICU programs in other war zones worldwide.
Acknowledgments
Acknowledgment
The authors acknowledge all of the Syrian tele-ICU participating physicians who have volunteered effort in support of the program since inception. Individuals listed below provided patient care, helped other physicians, made protocols or schedules, or refined logistics. Some physicians asked to remain anonymous, so the authors list their initials or their home city: Jaber Monla Hassan, M.D., Knoxville, TN; Abdul Ghani Sankari, M.D., Detroit, MI; Dr. A.G., Detroit, MI; Dr. M.B., Detroit, MI; Dr. M.K.; Dr. Maher Sakkour, and his neuro-intensive care team, Canada; Dr. K.K. and Dr. G.D., Canada, for efforts in pediatric critical care; Dr. Abbara, UK, for contributions to the infectious disease protocol; Dr. Abdulla Shahin, Boston, MA, for support as previous chair of Syrian Expatriate Organization; Dr. T.Z., Springfield, IL, Medical Committee Director, Syrian Expatriate Organization; Dr. B.G., Minneapolis MN; Zaher Sahloul, M.D., for logistics assistance; Amjad Rass, M.D., Detroit, MI; Ahmad Haj Hossein, M.D., Pittsburg, PA; Dr. N.A., for contributions in pediatric intensive care; Anas Alkassem, M.D., trauma surgery; Oussama Rifai, M.D., for contribution in nephrology; Dr. E.A., Detroit, MI; Dr. Y.R., Detroit, MI; Dr. N.N., radiology; Dr. R.M.; Dr. A.H. Detroit, MI; Dr. M.S., trauma surgery; Dr. A.T., surgery; Dr. T.Y., cardiology; Dr. A.A., Detroit, MI; Dr. E.K., Missouri; Dr. A.G., Indiana; Abu Luay, M.D., orthopedic surgery. The authors are also grateful for the assistance of organizations that provided scientific, financial, or logistic support to the tele-ICU program or to the hospitals in Syria: the Syrian American Medical Society, the Aleppo (Syria) Medical Committee, and the Syrian Expatriates Organization. Basil Bakri provided the EMR technology and, as a member of the Syrian American Engineering Association, provided technical assistance to the tele-ICU program.
Footnotes
Supported by the Syrian American Medical Society for clinical and tele-ICU equipment; the Syrian American Medical Society had no input in manuscript preparation.
Author Contributions: A.M.: Program design and implementation, manuscript preparation and final approval of the version submitted for publication. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. C.W.: Manuscript preparation and final approval of the version submitted for publication. Interpretation of data. Revising manuscript for critically important content. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
This article has an online supplement, which is accessible from this issue’s table of contents online at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Meldrum A. 130 Doctors Without Borders staff disappear in Sudan. February 2012. CBS News [accessed 2015 June 30]. Available from: http://www.cbsnews.com/news/130-doctors-without-borders-staff-disappear-in-sudan/
- 2.Red Cross and Red Crescent Movement. [Accessed 2015 Jan 5]. Available from: http://healthcareindanger.org/
- 3.Lilly CM, Zubrow MT, Kempner KM, Reynolds HN, Subramanian S, Eriksson EA, Jenkins CL, Rincon TA, Kohl BA, Groves RH, Jr, et al. Society of Critical Care Medicine Tele-ICU Committee. Critical care telemedicine: evolution and state of the art. Crit Care Med. 2014;42:2429–2436. doi: 10.1097/CCM.0000000000000539. [DOI] [PubMed] [Google Scholar]
- 4.United Nations High Commission for Refugees (UNHCR). Global trends in forced displacement for 2014 [accessed 2015 June 30]. Available from: http://www.unhcr.org/556725e69.html
- 5.Moughrabieh M, Weinert C, Zaza T. Rapid deployment of international tele-ICU services during conflict in Syria [abstract] Am J Respir Crit Care Med. 2014;189:A3630. [Google Scholar]
- 6.Facilities and Services at Damascus University Hospitals. 2011 [Accessed 2015 June 30]. Available from: http://damasuniv.edu.sy/english/hospitals.
- 7.Ahsan S. Syria, doctors beware. New York Times. 2013 October 3 [accessed 2015 June 30]. Available from: http://www.nytimes.com/2013/10/04/opinion/in-syria-doctors-beware.html.
- 8.MacFarquhar N, Droubi H.Syria’s civil war, doctors find themselves in cross hairs New York TimesMarch 23, 2013[accessed 2015 June 30]. Available from: http://www.nytimes.com/2013/03/24/world/middleeast/on-both-sides-in-syrian-war-doctors-are-often-the-target.html
- 9.Human Rights Watch Safeguarding health in conflict: attacks on health: global reportMay 2015[accessed 2015 June 30]. Available from: https://www.hrw.org/sites/default/files/related_material/HHR%20Attacks%20on%20Hospitals%20brochure%200515%20LOWRES.pdf
- 10.Barnard A, Saad H.Children’s art at Syria school, and then a bomb New York TimesApril 30, 2014[accessed 2015 June 30]. Available from: http://www.nytimes.com/2014/05/01/world/middleeast/syria.html
- 11.Organisation for the Prohibition of Chemical Weapons. OPCW fact finding mission: “compelling confirmation” that chlorine gas used as weapon in Syria. September 10, 2014 [accessed 2015 June 30]. Available from: http://www.opcw.org/news/article/opcw-fact-finding-mission-compelling-confirmation-that-chlorine-gas-used-as-weapon-in-syria/
- 12.Jaber M, Ghani M, Herman N. A review of adoption of telemedicine in Middle East countries: towards building Iraqi telemedicine framework. Sci. Int (Lahore) 2014;26:1795–1800. [Google Scholar]
- 13.Wootton R, Bonnardot L.Telemedicine in low-resource settings Front Public Health 2015. 3:3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wootton R, Vladzymyrskyy A, Zolfo M, Bonnardot L.Experience with low-cost telemedicine in three different settings: recommendations based on a proposed framework for network performance evaluation Glob Health Action 20114) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christian MD, Devereaux AV, Dichter JR, Rubinson L, Kissoon N Task Force for Mass Critical Care. Introduction and executive summary: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146:8S–34S. doi: 10.1378/chest.14-0732. [DOI] [PMC free article] [PubMed] [Google Scholar]