Abstract
Objective
To evaluate the effect of the fetal head station at attempted operative vaginal delivery (aOVD), and specifically midpelvic or low aOVD, on female and male sexual function and symptoms of postpartum depression (PPD) at 6 months.
Design
Prospective population-based cohort study.
Setting
1,941 women with singleton term fetuses in vertex presentation with midpelvic or low aOVD between 2008 and 2013 in a tertiary care university hospital.
Methods
Symptoms of female sexual dysfunction using the Pelvic Organ Prolapse/Urinary Incontinence/Sexual Function Short Form Questionnaire (PISQ-12), symptoms of PPD using the Edinburgh Postnatal Depression Scale (EPDS) score, symptoms of male sexual dysfunction using the International Index of Erectile Function (IIEF-15) and perineal pain were assessed 6 months after aOVD. We measured the association between midpelvic or low aOVD and symptoms of female and male sexual function and symptoms of PPD at 6 months using multiple regression and adjusting for demographics, and risk factors of sexual dysfunction, symptoms of PPD and perineal pain with adjusted odds ratios (aORs) and 95% confidence intervals (95% CI).
Results
The study included 907 women (46.7%) who responded to the questionnaire; 18.4% (167/907) had midpelvic aOVD, and 81.6% (740/907) low. Most women (873/907 [96.3%]) of those with partners reported sexual activity at 6 months. No significant difference was observed for PISQ-12, EPDS, IIEF-15 scores and perineal pain between mid and low pelvic groups. Compared with low pelvic aOVD, midpelvic aOVD was not significantly associated with either female or male sexual dysfunction (p = 0.89 and p = 0.76, respectively), or maternal symptoms of PPD (p = 0.83). Perineal pain significantly increased the risk of male and female sexual dysfunction and maternal symptoms of PPD at 6 months (p = 0.02, p = 0.006, and p = 0.02, respectively).
Conclusion
Midpelvic compared with low pelvic aOVD was not associated with an increase in sexual dysfunction, nor with symptoms of PPD at 6 months.
Introduction
No obstetrician wants to deliver a fetus already or still high in the birth canal; this situation is risky for mother and child. But in some situations (long labor, suspicion of fetal distress), obstetricians are face with a choice and can feel required, because of the obstetric situation, to attempt a potentially difficult operative vaginal delivery (OVD) or perform a cesarean at full dilatation, each with immediate and long-term inherent maternal and neonatal risks. Furthermore, when the fetus is at low pelvic station, OVD is not discussed for maternal or fetal indication, and must be preferred to cesarean delivery [1]. We previously reported that midpelvic attempted operative vaginal delivery (aOVD) was not associated with a higher rate of severe short-term maternal and neonatal morbidity than attempted low pelvic delivery supporting the continued use of midpelvic delivery in appropriately selected candidates [2]. Nonetheless, midpelvic OVD may subsequently have hidden mid- and long-term effect, that may justify to privilege a cesarean delivery rather than an OVD when the fetus is at midpelvic. Thus, it is crucial to assess mid and long-term maternal outcome after midpelvic aOVD. Our previous report that neither urinary nor anal incontinence differed at 6 months among women who had midpelvic and low pelvic aOVD suggests that midpelvic aOVD is an appropriate option [3].
Postpartum depression (PPD) is determined by several determinants, including consequences of obstetrical factors, such as mode of delivery, pain during delivery [4,5], parity, pregnancy or delivery complications [6–8]. Some studies suggest that OVD, compared to spontaneous vaginal delivery, are associated with a higher risk for symptoms of PPD [9,10], some do not [11,12]. Discrepancies may be explained by methodological differences.
Quality of female sexual function in postpartum period is dependent of several different factors, including cultural, sexological, organic, neurological patterns, psychological wellbeing [13], and perinatal events, including perineal pain, episiotomy, symptoms of PPD [14–16]. OVD has not clearly been reported as an independent risk factor for alteration of sexual function [13,15,17,18]. Recently, Barbara et al. [19] reported that OVD (n = 45) might be associated with poorer female sexual functioning, and specifically poorer scores on arousal, lubrication, orgasm, and global sexual functioning compared with a cesarean section group (n = 92) and lower orgasm scores compared with a spontaneous vaginal delivery group (n = 132) [19]. But, no conclusions can be drawn from this study regarding the high rate of episiotomies, the impact of pelvic floor trauma (perineal laceration or episiotomy) on sexual functioning, the small sample size and the absence of multivariate models controlled for confounders. Concerning male sexual function, a review of 59 studies noted that data about fathers, sexual activities and feelings in postpartum period are scarce [20]. Nearly a third of men reported lower sexual desire along with decreases in sexual behavior during postpartum period [21]. The association between the mode of delivery and sexual function have been already analyzed [13,15,17,18] but, to our knowledge, none of these studies has specifically studied female and male sexual function and depressive symptoms in postpartum period according to the fetal head station at aOVD.
We aimed to analyse female sexual function, maternal symptoms of PPD and male sexual function at 6 months according to the fetal head station at aOVD (midpelvic compared to low pelvic aOVD), and to analyse the risk factors of sexual dysfunctions and symptoms of PPD on a large prospective population-based cohort study of women who underwent an OVD, using multivariate models adjusting for potential confounders.
Material and methods
Study sample
All participants were told about the study and were given oral information during pregnancy. Verbal consent was obtained by the medical team in charge of the study before inclusion, women and men were consented to participation after delivery in the labor ward or in the maternity unit. Written consent was not required for prospective population-based cohort study according to the French law, and the study protocol and this consent procedure were approved by the Institutional Review Board at the Angers University Hospital, France, on November 2008 (Study ID: 2008), before the beginning of the study [2].
Our post hoc analysis were done using data from a prospective population-based cohort study including all women with an aOVD in a tertiary care university hospital from December 2008 through October 2013. Inclusion criteria was defined by the placement of at least one blade for forceps or spatula or a vacuum, regardless of its success (i.e., whether delivery was finally vaginal or cesarean), and a live singleton pregnancy in vertex presentation at term (> 37 weeks of gestation) [2]. Exclusion criteria were multiple gestations, fetal growth restriction (FGR), defined as <10th percentile for gestational age on Hadlock curves [22,23], a known congenital anomaly, vaginal breech delivery, and the absence of fetal station information according to the American College of Obstetricians and Gynecologists (ACOG) classification [24]. Specifically, station was defined by the level of the leading bony point of the fetal head in centimetres at or below the level of maternal ischial spines (0 and +1 = midpelvic; +2 and +3 = low; +4 and +5 = outlet) [24]. As described in detail previously [2], the hospital had 19,786 deliveries during the study period: 15,836 (80.0%) were vaginal, including 2,153 (13.6%) successful OVD, and 3,950 (20.0%) were cesarean deliveries, including 39 (0.2% of all deliveries and 1% of all cesarean deliveries) after failed OVD. There were thus 2,192 deliveries with an aOVD: successes 98.2% and failures 1.8%. However, 28 neonates were twins (n = 14 women), 26 were preterm, and 14 were small for gestational age and were therefore excluded. Therefore, our sample comprised 2,138 deliveries with an aOVD: 18.3% (n = 391) midpelvic, 72.5% (n = 1,550) low, and 9.2% (n = 197) outlet. Among all women with a fetus at midpelvic station at delivery, only 17 (4.2%) had a cesarean delivery without an operative vaginal attempt [2].
As described in detail previously [2], pre-specified study design was to analyse severe short-term maternal and neonatal morbidity after aOVD according to the fetal head station using the ACOG classification, specifically to compare severe short-term maternal and neonatal morbidity associated with midpelvic and low pelvic aOVDs, and to prospectively analyse mid- and long-term maternal complication (pelvic floors disorders, sexual dysfunction, maternal postpartum depressive symptoms at 6 months) and children development at 5 years, specifically associated with midpelvic and low pelvic aOVDs. Two cohorts of women were assessed separately 6 months after aOVD: those with a midpelvic aOVD (n = 391; 20.6%), and a lowpelvic aOVD (n = 1,550; 79.4%).
Measures
Informations about sexual function in men and women, and maternal symptoms of PPD were obtained from a questionnaire sent 6 months after delivery. A second mailing was sent to the women from whom we received no response. Female sexual function was assessed with the Pelvic Organ Prolapse Urinary Incontinence Sexual Questionnaire (PISQ-12) [25–27]. The PISQ-12 is a self-administered questionnaire with responses measured on a 5-point Likert scale ranging from 0 (always) to 4 (never), which have been already used to evaluate female sexual function in postpartum period [26], and seemed to be appropriate in a population suffering from postpartum pelvic floor disorders [3]. The questionnaire contains 12 items divided into three domains: behavioral-emotive (items 1–4), physical (items 5–9) and partner-related (items 10–12). The behavioral/emotive domain evaluates sexual desire, frequency of sexual activity, and orgasmic capabilities, the physical domain assesses more directly the effect of urinary incontinence or prolapse on sexual function, and the partner-related domain assesses the patient’s perception of her partner’s response to the effect of her pelvic floor disorder on their sexual functioning [25–27]. Items 1–4 are reversely scored and a total of 48 is the maximum score; higher scores indicate better female sexual function. The PISQ-12 is reported as a single sexual function score. It does not report the separate domains. This questionnaire has been validated in French to evaluate female sexual function [28]. Participants were considered sexually active if they reported sexual activity with a partner in the prior month.
As previously reported [3,29], perineal pain was evaluated through the question: “Do you have chronic perineal pain (perineum designates the skin and muscle around the vaginal and anal outlets)?”, dyspareunia through the question: “Do you experience pain during sexual intercourse?”. These two questions were dichotomous with two possible answers: “yes” and “no”, with an option for women who do not have intercourse in the prior month [3,29]. Episiotomy complications were evaluated through the question: "Do you have any complications concerning your episiotomy (hematoma, abscess, scar disunion, surgery)?", and was defined by the existence of at least one of the following criteria: hematoma, abscess, scar disunion, or required surgery for episiotomy [3,29].
Maternal symptoms of PPD was assessed using the French version of the Edinburgh Postnatal Depression Scale (EPDS) [30,31]. The EPDS is a 10-item self-report scale, it sums score ranges from 0 to 30 points, with higher score indicating more symptoms. EPDS has good sensitivity and specificity for identifying probable clinical postpartum depression in community samples [32,33]. In accordance with recent studies, a score of ≥12 on the EPDS was used as a measure of symptoms of PPD [12,34].
The effect of the delivery on quality of male sexual relations was assessed by using the International Index of Erectile Function (IIEF-15) [35], which has been already used to evaluate male sexual function in post-partum period [36]. The partner of the included women answered to the IIEF-15 questionnaire, which is a a self-administered questionnaire with responses measured on a 5-point Likert scale. The questionnaire addresses the relevant domains of male sexual function and contains 15 items divided into five domains: erectile function (Q1-Q5, Q15), orgasmic function (Q9-10), sexual desire (Q11,12), intercourse satisfaction (Q6-Q8), and overall satisfaction(Q13-14) [35]. Higher scores indicate better male sexual function [34]. The French linguistic version of the IIEF-15 was used [37]. The questionnaire used for the study is available (S1 Questionnaire).
The principal endpoints were PISQ-12 for female sexual function and EPDS score≥12 for maternal symptoms of PPD. The secondary endpoint was IIEF-15 for male sexual function. For this study, we hypothesized that women with midpelvic aOVD would not have poorer sexual function and more symptoms of PPD compared to low pelvic aOVD, and male sexual function was not altered after midpelvic aOVD compared to low pelvic aOVD.
Statistical analysis
Continuous data were described by their means ± standard deviations and compared by t-tests (or Mann-Whitney tests when appropriate), and categorical data were described by percentages and compared by chi-square tests (or Fisher exact tests when appropriate). Univariate and multivariate logistic regression were used for studying the association between maternal symptoms of PPD at 6 months and aOVD classification. Univariate and multivariable linear regression analysis were used to study the association between female and male sexual function at 6 months (considered as a continuous variable) and aOVD classification. Multivariate models were build using a stepwise procedure based on the Akaike criterion [38,39], the covariate "fetal head station" being systematically forced into the considered models. Confounders associated in univariate analysis at a 0.2 level were included in this stepwise procedure. To check the fit of the multivariate models, we studied the studentized residuals. Standardized measures of Cohen's d effect sizes were analysed in all comparisons (female sexual function, maternal symptoms of PPD, male sexual function), and specifically, midpelvic compared to low pelvic aOVD. The association between the different scores (PISQ, IIEF and EPDS) were also studied through the Pearson’s correlation coefficient. STATA 13.1 software (StataCorp, College Station, TX) was used for all analyses. Statistical significance was defined as a P value < 0.05.
Results
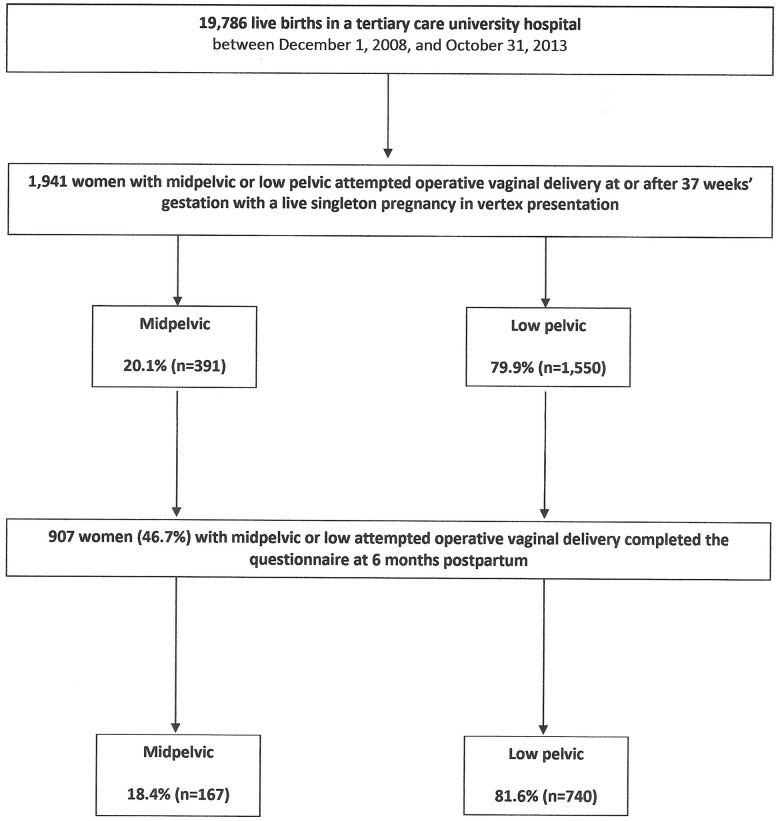
Six months after delivery, 907 women (46.7%) of the 1,941 deliveries with an aOVD completed the questionnaire: 18.4% (n = 167) had been midpelvic, and 81.6% (n = 740) low attempted deliveries (Fig 1). The difference between respondents and non-respondent were statistically significant in terms of maternal age at delivery, marital status, severe neonatal morbidity, rates of NICU transfer and prolonged hospitalization in NICU (p<0.05) (S1 Table).
Fig 1. Cohort flowchart.
Maternal and labor characteristics and maternal and neonatal outcomes in respondents according to the ACOG classification were developed in the Table 1. Concerning the female and male sexual function, 96.3% (873/907) of the couple (man-woman) reported sexual activity at 6 months postpartum. The entire cohort consisted of heterosexual couples. The mean PISQ-12 score among the 873 women who reported sexual activity at 6 months was 38.6±7.1 and did not differ between midpelvic and low pelvic aOVD (p = 0.82) (Table 1). The mean IIEF-15 score was 63.3±11.1 and was not significantly different according to the fetal head station. Perineal pain and dyspareunia did not differ between midpelvic and low pelvic aOVD (p = 0.14 and p = 0.79, respectively) (Table 1).
Table 1. Characteristics of mothers and their labor and maternal and neonatal outcomes in respondents, according to the ACOG classification.
| Mid (N = 167) | Low (N = 740) | P value | |
|---|---|---|---|
| Maternal and labor characteristics | |||
| Maternal age, (years)1 | 29.2 ± 5.3 | 29.0 ± 4.7 | 0.59* |
| Geographic origin | 0.34** | ||
| Europe, n (%) | 156 (93.4) | 699 (94.5) | |
| Sub-Saharan Africa, n (%) | 5 (3.0) | 8 (1.1) | |
| North Africa, n (%) | 1 (0.6) | 6 (0.8) | |
| Asia, n (%) | 2 (1.2) | 17 (2.3) | |
| Other, n (%) | 3 (1.8) | 10 (1.3) | |
| Married or living with a partner, n (%) | 158 (95.8) | 709 (96.2) | 0.79** |
| Nulliparity, n (%) | 118 (70.7) | 564 (76.2) | 0.13** |
| Previous cesarean delivery, n (%) | 20 (42.6) | 66 (37.5) | 0.52** |
| Previous 3rd or 4th-degree perineal lacerations, n (%) | 0 | 1 (0.6) | 0.60*** |
| Previous depression, n (%) | 5 (3.0) | 38 (5.1) | 0.25** |
| BMI before pregnancy (kg/m22)1 | 22.8 ± 4.1 | 22.7 ± 3.9 | 0.72* |
| Gestational weight gain (kg) 1 | 13.8 ± 4.5 | 13.3 ± 4.4 | 0.23* |
| Antenatal suspicion of macrosomia 2, n (%) | 18 (10.8) | 48 (6.5) | 0.05** |
| Gestational age at delivery (weeks) 1 | 39.5 ± 1.5 | 39.4 ± 1.4 | 0.63* |
| Induced labor, n (%) | 30 (18.0) | 125 (16.9) | 0.74** |
| Length of labor (min) 1 | 395.7 ± 179.1 | 388.4 ± 165.0 | 0.61* |
| Length of 2nd stage (min) 1 | 103.3 ± 73.8 | 108.8 ± 67.3 | 0.35* |
| Active phase of 2nd stage > 30 min, n (%) | 51 (30.5) | 267 (36.1) | 0.28** |
| Dose of oxytocin (mUI) 1 | 1976.3 ± 2228.8 | 1620.9 ± 2084.8 | 0.05* |
| Epidural analgesia, n (%) | 164 (98.2) | 698 (94.5) | 0.04** |
| Manual rotation, n (%) | 30 (18.0) | 81 (11.0) | 0.01** |
| Persistent occiput | 0.05** | ||
| Anterior, n (%) | 139 (83.2) | 662 (89.8) | |
| Posterior, n (%) | 21 (12.6) | 56 (7.6) | |
| Transverse, n (%) | 7 (4.2) | 19 (2.6) | |
| Indications for OVD | 0.02** | ||
| Non reassuring FHR only, n (%) | 86 (51.5) | 301 (40.7) | |
| Arrested progress only, n (%) | 51 (30.5) | 313 (42.3) | |
| Non reassuring FHR and arrested progress, n (%) | 30 (18.0) | 129 (17.4) | |
| OVD in operating room, n (%) | 12 (7.2) | 4 (0.5) | <0.001*** |
| Provider attending delivery | <0.001** | ||
| Senior obstetrician, n (%) | 88 (54.7) | 159 (21.7) | |
| Resident, n (%) | 73 (45.3) | 573 (78.3) | |
| Instrument type | |||
| Vacuum, n (%) | 13 (7.8) | 237 (32.0) | <0.001** |
| Forceps, n (%) | 20 (12.0) | 38 (5.1) | <0.001*** |
| Spatula, n (%) | 140 (84.3) | 485 (65.5) | <0.001** |
| Sequential use of instrument, n (%) | 6 (3.6) | 21 (2.8) | 0.59*** |
| Maternal outcome | |||
| Cesarean section after failed OVD, n (%) | 12 (7.2) | 4 (0.5) | <0.001*** |
| Episiotomy, n (%) | 144 (87.3) | 652 (88.1) | 0.77** |
| 3rd or 4th-degree perineal lacerations, n (%) | 3 (1.8) | 25 (3.4) | 0.30*** |
| Perineal hematomas, n (%) | 0 | 1 (0.1) | 0.63*** |
| Abscesses/hematoma required surgery, n (%) | 1 (0.7) | 3 (0.4) | 0.69*** |
| Postpartum hemorrhage (PPH), n (%) | 35 (20.9) | 128 (17.3) | 0.27** |
| Severe PPH (blood loss>1500mL), n (%) | 5 (3.0) | 16 (2.2) | 0.52*** |
| Second-line therapies3, n (%) | 1 (1.0) | 1 (0.2) | 0.25*** |
| Blood transfusion, n (%) | 7 (4.2) | 12 (1.6) | 0.04*** |
| Infections4, n (%) | 1 (0.7) | 1 (0.1) | 0.25*** |
| Thromboembolic events, n (%) | 0 | 2 (0.3) | 0.50*** |
| Maternal hospitalization in intensive care unit, n (%) | 0 | 0 | - |
| Severe maternal morbidity5, n (%) | 13 (7.8) | 64 (8.7) | 0.71** |
| Neonatal outcome | |||
| Birth weight≥4000 g, n (%) | 12 (7.2) | 38 (5.1) | 0.30** |
| 5-min Apgar score<7, n (%) | 1 (0.6) | 5 (0.7) | 0.91*** |
| pH<7.00, n (%) | 4 (2.5) | 10 (1.4) | 0.32*** |
| Transfer to NICU, n (%) | 9 (5.4) | 36 (4.9) | 0.78** |
| NICU hospitalisation>24 h, n (%) | 9 (5.4) | 29 (3.9) | 0.39** |
| Respiratory distress syndrome, n (%) | 8 (4.8) | 30 (4.1) | 0.66** |
| Neonatal trauma6, n (%) | 3 (1.8) | 3 (0.4) | 0.05*** |
| Shoulder dystocia, n (%) | 7 (4.4) | 15 (2.0) | 0.08*** |
| Need for resuscitation or intubation, n (%) | 0 | 8 (1.1) | 0.18*** |
| Severe neonatal morbidity7, n (%) | 25 (15.0) | 62 (8.4) | 0.01** |
| Registered variables at 6 months postpartum | |||
| Smoker (male), n (%) | 47 (39.8) | 218 (39.4) | 0.92** |
| Chronic disease (male), n (%) | 4 (3.4) | 34 (6.1) | 0.24** |
| Breastfeeding, n (%) | 95 (93.1) | 470 (93.3) | 0.63** |
| Pelvic floor muscle training, n (%) | 119 (77.8) | 544 (79.1) | 0.72** |
| Child in the parents’ bedroom during night, n (%) | 14 (11.9) | 63 (11.4) | 0.89** |
| Episiotomy complications8, n (%) | 54 (38.9) | 245 (37.7) | 0.80** |
| Perineal pain, n (%) | 26 (17.2) | 87 (12.7) | 0.14** |
| Sexually active, n (%) | 158 (94.6) | 715 (96.6) | 0.95** |
| Dyspareunia, n (%) | 40 (23.9) | 184 (24.8) | 0.79** |
| EPDS1 | 6.5 ± 5.5 | 6.7 ± 6.1 | 0.72* |
| EPDS score ≥ 12 | 40 (23.9) | 171 (23.1) | 0.81** |
| PISQ-12 in sexually active women1 | 37.2 ± 7.8 | 37.1 ± 6.6 | 0.82* |
| IIEF-15 in sexually active men1 | 64.0 ± 10.3 | 63.2 ± 11.3 | 0.46* |
1 Values are given as mean ± standard deviation.
2 Antenatal suspicion of macrosomia: fundal height measurement at delivery > 37cm and/or ultrasonographic fetal abdominal circumference > 90th p. for gestational age and sex on Hadlock curves [22].
3 Second-line therapies were uterine compression sutures, uterine artery embolization, and peripartum hysterectomy for management of massive primary postpartum hemorrhage after failure of uterine massage and uterotonic agents to stop bleeding [2].
4 Infections were defined by the existence of at least one of the following criteria: endometritis, episiotomy infection and wound infection needed surgery [2].
5 Severe maternal morbidity was defined by the existence of at least one of the following criteria: third or fourth-degree perineal lacerations, perineal hematomas, cervical laceration, extension of uterine incision at cesarean section, PPH>1500 mL, surgical haemostatic procedure, uterine artery embolization, blood transfusion, infections (endometritis, episiotomy infection, wound infection needed surgery), thromboembolic events (deep vein thrombophlebitis and pulmonary embolism), hospitalization in intensive care unit, and maternal death [2].
6 Neonatal trauma was defined by the existence of at least one of the following criteria: fracture of the clavicle or a long bone, brachial plexus injury, and cephalhematoma [2].
7 Severe neonatal morbidity was defined by at least one of the following criteria: 5-minute Apgar score<7, umbilical artery pH < 7.00, need for resuscitation or intubation, neonatal trauma, intraventricular hemorrhage > grade 2, admission to the NICU (neonatal intensive care unit) for>24 hours, convulsions, sepsis, and neonatal death [2].
8 Episiotomy complications were defined by the existence of at least one of the following criteria: hematoma, abscess, scar disunion, or required surgery for episiotomy.
* Student t test,
** χ2 test,
*** Fisher exact test. Statistical significance was defined as a P value < 0.05.
In the multivariable linear regression analysis, attempted midpelvic delivery (compared with low pelvic) was not associated with female sexual dysfunction at 6 months (p = 0.89), controlling for maternal age, indications for aOVD, the American College classification, 3rd or 4th-degree perineal lacerations, episiotomy complications, perineal pain, dyspareunia, and child in the parents' bedroom during night (Table 2). The PISQ-12 score was reduced on average of -0.10 points compared to low attempted delivery (95% confidence interval (CI) CI -1.57 to 1.38) (Table 2). Attempted midpelvic delivery (compared with low pelvic) was not also associated with male sexual dysfunction at 6 months (P = 0.76), controlling for maternal age, gestational age at delivery, the American College classification, indications for aOVD, instrument type, perineal pain, and smoker (male) (Table 3). The IIEF-15 score was reduced of -0.32 points compared to low attempted delivery (95% CI -2.43 to 1.79) (Table 3). Perineal pain, episiotomy complications and dyspareunia were each significantly associated with alterations of the female sexual function (Table 2). Forceps delivery and female perineal pain were significantly associated with alterations of the male sexual function (Table 3).
Table 2. Univariate and multiple linear regression analysis of female sexual function 6 months after midpelvic and low attempted operative vaginal delivery.
| Variables 1 | Female sexual function (PISQ-12 score) | |||||
|---|---|---|---|---|---|---|
| Crude R (95% CI) | Effect size | P value | Adjusted R (95% CI) | Effect size | P value | |
| ACOG classification | ||||||
| Mid | Reference | - | Reference | - | ||
| Low | -0.14 (-1.36–1.08) | -0.22 | 0.82 | -0.10 (-1.57–1.38) | -0.13 | 0.89 |
| Indications for aOVD | ||||||
| Arrested progress only | Reference | - | Reference | - | ||
| Non-reassuring FHR only | 1.43 (0.40–2.46) | 2.72 | 0.006 | 1.66 (0.45–2.87) | 2.69 | 0.007 |
| Non-reassuring FHR and arrested progress | 0.45 (-0.90–1.81) | 0.65 | 0.51 | 0.80 (-0.74–2.34) | 1.02 | 0.31 |
| 3rd or 4th-degree perineal lacerations | -2.54 (-5.26–0.18) | -1.83 | 0.06 | -2.84 (-6.00–0.31) | -1.76 | 0.08 |
| Episiotomy complications | -1.36 (-2.37- -0.35) | -2.64 | 0.008 | -1.30 (-2.42- -0.17) | -2.28 | 0.02 |
| Perineal pain | -3.43 (-4.79- -2.08) | -4.94 | <0.001 | -2.39 (-4.08- -0.70) | -2.77 | 0.006 |
| Dyspareunia | -2.06 (-1.02- -3.11) | -1.92 | <0.001 | -1.51 (-2.81- -0.21) | -2.28 | 0.02 |
| Child in the parents’ bedroom during night | -1.64 (-3.22- -0.06) | -2.03 | 0.04 | 1.50 (-3.25–0.26) | -1.68 | 0.09 |
| Cste | 36.6 (33.9–39.3) | |||||
Values are crude and adjusted coefficient's linear regression (R) with 95% confidence intervals (CI).
1 Controlling for maternal age, ACOG classification, indications for aOVD, 3rd or 4th-degree perineal lacerations, episiotomy complications, perineal pain, dyspareunia, and child in the parents' bedroom during night.
Table 3. Univariate and multiple linear regression analysis of male sexual function 6 months after midpelvic and low attempted operative vaginal delivery.
| Variables 1 | Male sexual function (IIEF-15 score) | |||||
|---|---|---|---|---|---|---|
| Crude R (95% CI) | Effect size | P value | Adjusted R (95% CI) | Effect size | P value | |
| Gestational age at delivery (per week) | -0.53 (-1.17–0.11) | -1.62 | 0.10 | -0.60 (-1.20- -0.003) | -1.96 | 0.049 |
| ACOG classification | ||||||
| Mid | Reference | - | Reference | - | ||
| Low | -0.82 (-3.02–1.37) | -0.73 | 0.46 | -0.32 (-2.43–1.79) | -0.30 | 0.76 |
| Instrument type | ||||||
| Other instrument | Reference | - | Reference | - | ||
| Forceps | -4.51 (-8.02- -1.01) | -2.52 | 0.01 | -4.96 (-8.30- -1.62) | -2.91 | 0.004 |
| Indications for aOVD | ||||||
| Arrested progress only | Reference | - | Reference | - | ||
| Non-reassuring FHR only | 3.52 (1.68–5.36) | 3.75 | <0.001 | 3.05 (1.29–4.81) | 3.40 | 0.001 |
| Non-reassuring FHR and arrested progress | 1.76 (-0.63–4.16) | 1.44 | 0.15 | 1.19 (-1.08–3.47) | 1.03 | 0.30 |
| Perineal pain | -2.45 (-4.98–0.08) | -1.90 | 0.06 | -2.74 (-5.10- -0.38) | -2.28 | 0.02 |
| Smoker (male) | 1.30 (-0.32–2.92) | 1.57 | 0.11 | 1.34 (-0.29–2.97) | 1.61 | 0.11 |
| Cste | 82.5 (58.4–106.6) | |||||
Values are crude and adjusted coefficient's linear regression (R) with 95% confidence intervals (CI).
1 Controlling for maternal age, gestational age at delivery, ACOG classification, indications for aOVD, instrument type, perineal pain, and smoker (male).
Concerning the assessment of maternal depressive symptoms at 6 months postpartum, the mean EPDS score was not significantly different between the groups (p = 0.72) (Table 1). Previous maternal PPD, BMI ≥ 30 kg/m22 before pregnancy, perineal pain, PISQ-12 and IIEF-15 scores were significantly different depending on the PPD status (Table 4). In multivariate analysis, attempted midpelvic (compared with low pelvic) delivery was not significantly associated with maternal symptoms of PPD (adjusted odds ratio (aOR) 0.95, 95% CI 0.58–1.53). BMI ≥ 30 kg/m22 before pregnancy and perineal pain were each significantly associated with maternal symptoms of PPD (Table 5). Correlation between IIEF-15 and PISQ-12 scores was 0.45 (95% CI 0.39 to 0.51), and correlation between EPDS and PISQ-12 scores was -0.31 (95% CI -0.37 to -0.24). Finally, small Cohen's d effect sizes were noted in all comparisons (female sexual function, maternal symptoms of PPD, male sexual function) concerning comparisons of midpelvic to low pelvic aOVD.
Table 4. Symptoms of postpartum depression according to characteristics of mothers and labor and maternal, paternal, and neonatal outcomes in women 6 months after midpelvic or low attempted operative vaginal delivery.
| Postpartum Depression (N = 211) | No-postpartum Depression (N = 603) | P value | |
|---|---|---|---|
| Maternal and labor characteristics | |||
| Maternal age1, (years) | 29.2 ± 5.3 | 29.0 ± 4.6 | 0.61* |
| Multiparity, n (%) | 49 (23.2) | 155 (25.7) | 0.47** |
| BMI ≥ 30 kg/m2 before pregnancy, n (%) | 23 (11.0) | 25 (4.2) | <0.001** |
| Gestational weight gain >20 kg, n (%) | 19 (9.3) | 47 (8.1) | 0.58** |
| Previous postpartum depression, n (%) | 23 (10.9) | 18 (3.0) | <0.001** |
| Gestational age at delivery1 (weeks) | 39.4 ± 1.5 | 39.4 ± 1.4 | 0.99* |
| Length of labor1 (min) | 396.4 ± 169.0 | 390.2 ± 165.4 | 0.64* |
| 2nd stage>3 hours, n (%) | 37 (17.5) | 101 (16.8) | 0.80** |
| Active phase of 2nd stage > 30 min, n (%) | 77 (36.5) | 212 (35.2) | 0.73** |
| Epidural analgesia, n (%) | 201 (95.3) | 576 (95.7) | 0.80** |
| Persistent occiput position, n (%) | 0.15** | ||
| Anterior | 183 (87.1) | 538 (89.5) | |
| Posterior | 17 (8.1) | 50 (8.3) | |
| Transverse | 10 (4.8) | 13 (2.2) | |
| ACOG classification, n (%) | 0.37** | ||
| Mid | 43 (20.4) | 106 (17.6) | |
| Low | 168 (79.6) | 497 (82.4) | |
| Obstetrician performing delivery, n (%) | 0.32** | ||
| Senior obstetrician | 51 (24.8) | 169 (28.3) | |
| Obstetric registrar | 155 (75.2) | 428 (71.7) | |
| Instrument type, n (%) | |||
| Vacuum | 60 (28.4) | 161 (26.7) | 0.63** |
| Forceps | 18 (8.5) | 34 (5.6) | 0.14** |
| Spatula | 140 (66.4) | 421 (69.8) | 0.35** |
| Sequential use of two instruments | 6 (2.8) | 14 (2.3) | 0.67*** |
| Indications for aOVD, n (%) | 0.47** | ||
| Non-reassuring FHR only | 88 (41.7) | 261 (43.3) | |
| Arrested progress only | 84 (39.8) | 248 (41.0) | |
| Non-reassuring FHR and arrested progress | 41 (19.4) | 95 (15.7) | |
| Maternal outcome | |||
| Cesarean delivery after failed operative vaginal delivery, n (%) | 4 (1.9) | 12 (2.0) | 0.93*** |
| Episiotomy, n (%) | 181 (85.8) | 532 (88.4) | 0.32** |
| 3rd or 4th-degree perineal lacerations, n (%) | 6 (2.8) | 20 (3.3) | 0.73** |
| PPH (blood loss>500mL), n (%) | 34 (16.1) | 114 (18.9) | 0.37** |
| Severe PPH (blood loss>1500 mL), n (%) | 6 (2.8) | 14 (2.3) | 0.67*** |
| Abscesses/hematoma requiring surgery, n (%) | 1 (0.5) | 2 (0.3) | 0.77*** |
| Severe maternal morbidity, n (%) | 17 (8.1) | 53 (8.8) | 0.74** |
| Neonatal outcome | |||
| Birth weight > 4000 g, n (%) | 15 (7.4) | 32 (5.3) | 0.33** |
| Neonatal trauma, n (%) | 2 (1.0) | 3 (0.5) | 0.47*** |
| Transfer to NICU, n (%) | 9 (4.3) | 33 (5.5) | 0.49** |
| Severe neonatal morbidity, n (%) | 18 (8.5) | 62 (10.3) | 0.46** |
| Registered variables at 6 months postpartum | |||
| Tobacco (male), n (%) | 71 (43.8) | 180 (37.3) | 0.14** |
| Chronic disease (male), n (%) | 11 (6.8) | 27 (5.6) | 0.57** |
| Breastfeeding, n (%) | 129 (90.8) | 377 (94.0) | 0.20** |
| Pelvic floor muscle training, n (%) | 157 (77.3) | 481 (80.0) | 0.41** |
| Child in the parents’ bedroom during night, n (%) | 19 (11.9) | 54 (11.2) | 0.82** |
| Episiotomy complications, n (%) | 119 (62.0) | 349 (61.9) | 0.98** |
| Perineal pain, n (%) | 36 (17.8) | 73 (12.2) | 0.04** |
| Dyspareunia, n (%) | 69 (37.3) | 177 (31.8) | 0.31** |
| PISQ-12 in sexually active women1 | 34.5 ± 7.9 | 38.1 ± 6.0 | <0.001* |
| IIEF-15 in sexually active men1 | 60.3 ± 14.3 | 64.5 ± 9.2 | <0.001* |
1 Values are given as mean ± standard deviation.
* Student t test,
** χ2 test,
*** Fisher exact test. Statistical significance was defined as a P value < 0.05.
Table 5. Univariate and multivariate logistic regression analysis of symptoms of postpartum depression 6 months after midpelvic or low attempted operative vaginal delivery.
| Maternal postpartum depression (N = 211) | ||||||
|---|---|---|---|---|---|---|
| Variables1 | Crude OR (95% CI) | Effect size | P value | Adjusted OR (95% CI) | Effect size | P value |
| BMI ≥ 30 kg/m2 before pregnancy | 3.07 (1.66–5.71) | 3.58 | <0.001 | 2.86 (1.51–5.40) | 3.22 | 0.001 |
| Persistent occiput | ||||||
| Anterior | Reference | - | Reference | - | ||
| Posterior | 1.41 (0.77–2.59) | 1.11 | 0.27 | 1.40 (0.75–2.62) | 1.06 | 0.30 |
| Transverse | 3.08 (1.31–7.29) | 2.58 | 0.01 | 2.89 (1.19–7.03) | 2.34 | 0.02 |
| ACOG classification | ||||||
| Mid | Reference | - | Reference | - | ||
| Low | 0.93 (0.59–1.47) | -0.31 | 0.75 | 0.95 (0.58–1.53) | -0.20 | 0.83 |
| Indications for aOVD | ||||||
| Arrested progress only | Reference | - | Reference | - | ||
| Non-reassuring FHR only | 0.68 (0.45–1.01) | -1.83 | 0.06 | 0.63 (0.41–0.97) | -2.11 | 0.04 |
| Non-reassuring FHR and arrested progress | 1.12 (0.68–1.84) | 0.45 | 0.65 | 1.08 (0.65–1.81) | 0.30 | 0.76 |
| Perineal pain | 1.83 (1.13–2.95) | 2.46 | 0.01 | 1.79 (1.10–2.91) | 2.34 | 0.02 |
Values are crude and adjusted coefficient's logistic regression (OR) with 95% confidence intervals (CI).
1 Controlling for maternal age, body mass index (BMI) before pregnancy, previous postpartum depression, persistent occiput orientation of fetal head, ACOG classification, indications for aOVD, and perineal pain.
Discussion
Main findings
This study reports a prospective population-based cohort analysis of women 6 months after midpelvic or low pelvic aOVD, and male and female sexual dysfunction and maternal symptoms of PPD according to the fetal head station. We found that midpelvic aOVD was not significantly associated with a higher rate in male and female sexual dysfunction and maternal symptoms of PPD than attempted low pelvic aOVD at 6 months postpartum. After multivariable analysis, postpartum perineal pain was an independent risk factor for male or female sexual dysfunction and maternal symptoms of PPD at 6 months after aOVD.
Interpretation
It is difficult to compare our results with the literature because previous studies of sexual function and maternal symptoms of PPD at 6 months or 1 year postpartum after OVD never detailed results according to the fetal head station at instrument's application [15,40]. The sample size of this prospective cohort (N = 907) was larger in size to other prospective [40–42] and retrospective studies [15,43] of maternal consequences after OVD. Our results are consistent with other findings in the literature concerning health problems after OVD, i.e. female sexual activity at 6 months postpartum [40,43–45], altered sexual function in women with postpartum perineal pain [15,42] or with postpartum dyspareunia [40,43,46], increased maternal postpartum depressive symptoms in women with persistent perineal pain [19,44,47,48]. Our data also included what the women and the men were saying concerning sexual function in postpartum period; therefore, this important factor in the assessment of the quality of life in couple was assessed. We showed that persistent female perineal pain 6 months after aOVD were significantly associated with alterations of the male sexual function. To our knowledge, no study has specifically studied male sexual function in postpartum period according to the fetal head station at aOVD.
Strengths and limitations
The principal strength of this study is the use of validated instruments for male and female sexual dysfunction and maternal symptoms of PPD at 6 months postpartum in a large, prospective population-based cohort study with carefully characterized obstetric patients. This allowed a complete characterization of symptoms in this population. In particular, this is, to our knowledge, the first prospective population-based cohort study, that directly compares midpelvic and low aOVDs for male and female sexual dysfunction and maternal symptoms of PPD at 6 months postpartum. Obstetric situation with a potentially difficult OVD or perform a caesarean at full dilatation seems to present the perfect setting for a randomised trial, which probably failed to achieve due to recruitment that is not feasible in the antenatal period. Furthermore, when the fetus is at low pelvic station, OVD is not discussed for maternal or fetal indication, and must be preferred to caesarean delivery. As our results showed no difference between low pelvic and midpelvic OVD regarding inherent immediate maternal outcomes [2] and 6 months after OVD [3], the continued use of midpelvic delivery in appropriately selected candidates should be considered.
Our study has some limitations. First, determination of the station of the fetal head and thus classification of the OVDs is quite subjective and is influenced by fetal head position, molding, and time of assessment (before or after regional analgesia) [2]. Nevertheless, the prevalence of midpelvic aOVD was similar to that in other study [41], and the rates of induced labour, persistent occiput posterior or transverse, manual rotation, forceps and spatula, aOVD performed by senior obstetricians and aOVD in an operating room were significantly higher in the midpelvic compared to the lowpelvic aOVD group, as previously shown [2]. This suggests that the risk of contamination between the two groups was low [2]. Second, episiotomy and perineal tears of third/fourth degree were not found to be associated with alteration of female sexual function or dyspareunia at 6 months, consistent with some studies [41,49,50], but not with others [15,51]. These discrepancies may be explained by methodological differences. Several hypotheses may explain the discrepancies between these data concerning female sexual function after childbirth: memory bias for obstetric variables in retrospective study [15,51], or length of time in the postpartum period chosen for evaluation, which may be an important bias due to anatomical change [41]. Third, we reported a relative low rate of respondents (46.7%), but this rate was consistent with others large postpartum evaluations using mailed questionnaire [40,43]. It is plausible that participants declining to respond to a questionnaire at 6 months were at higher risk of sexual dysfunction and/or depressive symptoms than participants included in the study. Nevertheless, the non-respondents differed mainly from the respondents in their rate of neonatal morbidity, a factor that was not related to either male and female sexual dysfunction and symptoms of PPD at 6 months in our study. Four, no power calculations were done before the analysis of the questionnaire at 6 months because the study was based on post hoc analysis from a prospective population-based cohort study without any pre-specified hypothesis concerning covariates which should be associated with the outcome (sexual function and maternal symptoms of depression) at 6 months. Nonetheless, we would like to underline that our sample size was sufficient to show an effect size of 0.24 (considered as a small effect size) with a power of 80% assessed according to the observed incidence of male and female sexual dysfunction and symptoms of PPD at 6 months. Five, the decision most often faced to the obstetrician is, arguably, the choice between midpelvic aOVD and emergency cesarean section at full dilatation, rather than mid- vs lowpelvic aOVD. From this perspective, the absence of any data on outcomes for women having an emergency cesarean section at full dilatation is a limitation of the study.
Conclusion
We found that both female and male sexual function as well as maternal depressive symptoms did not differ 6 months after childbirth among women who had experienced midpelvic and low pelvic aOVD. These findings at 6 months should help clinician to inform women and their partners about what to expect after a midpelvic aOVD. The data at 6 months postpartum are reassuring and need further studies at long-term to confirm these short-term data.
Supporting information
(DOC)
(DOC)
Acknowledgments
We particularly thank Pr Xavier Fritel who is the author of the original questionnaire used in the Besançon-Rothschild cohort to analyze perineal pain, painful intercourse and episiotomy complications in the postpartum period.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The Angers University Hospital provided the funding for the study. The funding source had no role in the design or conduct of the study, collection, analysis, or interpretation of the data, or writing the article or decision to submit for publication.
References
- 1.Committee on Practice Bulletins-Obstetrics (2015) ACOG Practice Bulletin No. 154: Operative Vaginal Delivery. Obstet Gynecol 126: e56–e65. 10.1097/AOG.0000000000001147 [DOI] [PubMed] [Google Scholar]
- 2.Ducarme G, Hamel JF, Bouet PE, Legendre G, Vandenbroucke L, Sentilhes L (2015) Maternal and neonatal morbidity after attempted operative vaginal delivery according to fetal head station. Obstet Gynecol 126: 521–529. 10.1097/AOG.0000000000001000 [DOI] [PubMed] [Google Scholar]
- 3.Ducarme G, Hamel J-F, Brun S, Madar H, Merlot B, Sentilhes L (2016) Pelvic floor disorders 6 Months after attempted operative vaginal delivery according to the fetal head station: a prospective cohort study. PLoS ONE 11:e0168591 10.1371/journal.pone.0168591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eisenach JC, Pan PH, Smiley R, Lavand'homme P, Landau R, Houle TT (2008) Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain 140: 87–94. 10.1016/j.pain.2008.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar RC (1997) "Anybody's child": severe disorders of mother-to-infant bonding. Br J Psychiatry 171: 175–181. [DOI] [PubMed] [Google Scholar]
- 6.Boyce PM, Todd AL (1992) Increased risk of postnatal depression after emergency caesarean section. Med J Aust 157: 172–174. [DOI] [PubMed] [Google Scholar]
- 7.Csatordai S, Kozinszky Z, Devosa I, Toth E, Krajcsi A, Sefcsik T (2007) Obstetric and sociodemographic risk of vulnerability to postnatal depression. Patient Educ Couns 67: 84–92. 10.1016/j.pec.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 8.Johnstone SJ, Boyce PM, Hickey AR, Morris-Yatees AD, Harris MG (2001) Obstetric risk factors for postnatal depression in urban and rural community samples. Austr N Z J Psychiatry 35: 69–74. 10.1046/j.1440-1614.2001.00862.x [DOI] [PubMed] [Google Scholar]
- 9.Blom EA, Jansen PW, Verhulst FC, Hofman A, Raat H, Jaddoe VW, et al. (2010) Perinatal complications increase the risk of postpartum depression. The Generation R Study. BJOG 117: 1390–1398. 10.1111/j.1471-0528.2010.02660.x [DOI] [PubMed] [Google Scholar]
- 10.Yang SN, Shen LJ, Ping T, Wang YC, Chien CW (2011) The delivery mode and season variation are associated with the development of postpartum depression. J Affect Disord 132: 158–164. 10.1016/j.jad.2011.02.009 [DOI] [PubMed] [Google Scholar]
- 11.Patel RR, Murphy DJ, Peters TJ (2005) Operative delivery and postnatal depression: a cohort study. BMJ 330:879 10.1136/bmj.38376.603426.D3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaillard A, Le Strat Y, Mandelbrot L, Keita H, Dubertret C (2014) Predictors of postpartum depression: prospective study of 264 women followed during pregnancy and postpartum. Psychiatry Res 215:341–346. 10.1016/j.psychres.2013.10.003 [DOI] [PubMed] [Google Scholar]
- 13.Serati M, Salvatore S, Siesto G, Cattoni E, Zanirato M, Khullar V, et al. (2010) Female sexual function during pregnancy and after childbirth. J Sex Med. 7:2782–2790. 10.1111/j.1743-6109.2010.01893.x [DOI] [PubMed] [Google Scholar]
- 14.Connolly A, Thorp J, Pahel L (2005) Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int J Urogynecol J Pelvic Floor Dysfunction 16:263–267. 10.1007/s00192-005-1293-6 [DOI] [PubMed] [Google Scholar]
- 15.Signorello LB, Harlow BL, Chekos AK, Repke JT (2001) Postpartum sexual functioning and its relationship to perineal trauma: A retrospective cohort study of primiparous women. Am J Obstet Gynecol 184:881–890. 10.1067/mob.2001.113855 [DOI] [PubMed] [Google Scholar]
- 16.Hicks TL, Goodall SF, Quattrone EM, Lydon-Rochelle MT (2004) Postpartum sexual functioning and method of delivery: summary of the evidence. J Midwifery Womens Health 49:430–436. 10.1016/j.jmwh.2004.04.007 [DOI] [PubMed] [Google Scholar]
- 17.Crane AK, Geller EJ, Bane H, Ju R, Myers E, Matthews CA (2013) Evaluation of pelvic floor symptoms and sexual function in primiparous women who underwent operative vaginal delivery versus cesarean delivery for second-stage arrest. Female Pelvic Med Reconstr Surg 19:13–16. 10.1097/SPV.0b013e31827bfd7b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fehniger JE, Brown JS, Creasman JM, Van Den Eeden SK, Thom DH, Subak LL, et al. (2013) Childbirth and female sexual function later in life. Obstet Gynecol 122:988–997. 10.1097/AOG.0b013e3182a7f3fc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbara G, Pifarotti P, Facchin F, Cortinovis I, Dridi D, Ronchetti C, et al. (2016) Impact of Mode of Delivery on Female Postpartum Sexual Functioning: Spontaneous Vaginal Delivery and Operative Vaginal Delivery vs. Cesarean Section. J Sex Med 13:393–401. 10.1016/j.jsxm.2016.01.004 . [DOI] [PubMed] [Google Scholar]
- 20.von Sydow K (1999) Sexuality during pregnancy and after childbirth: a metacontent analysis of 59 studies. J Psychosom Res 47:27–49. [DOI] [PubMed] [Google Scholar]
- 21.Olsson A, Robertson E, Björklund A, Nissen E (2010) Fatherhood in focus, sexual activity can wait: new fathers' experience about sexual life after childbirth. Scand J Caring Sci 24:716–725. 10.1111/j.1471-6712.2009.00768.x [DOI] [PubMed] [Google Scholar]
- 22.Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK (1985) Estimation of fetal weight with the use of head, body, and femur measurements–a prospective study. Am J Obstet Gynecol 151: 333–337. [DOI] [PubMed] [Google Scholar]
- 23.French College of Gynecologists and Obstetricians (2013) [Intra-uterine growth retardation: guidelines for clinical practice—short text]. J Gynecol Obstet Biol Reprod 42: 1018–1025. 10.1016/j.jgyn.2013.09.023 [DOI] [PubMed] [Google Scholar]
- 24.Obstetrics forceps ACOG commitee opinion, no. 59. Washington, DC: American College of Obstetricians and Gynecologists; (1988). [Google Scholar]
- 25.Rogers G, Coates K, Kammerer-Doak D, Khalsa S, Qualls C (2003) A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12) [published erratum appears in Int Urogynecol J Pelvic Floor Dysfunct 2004;15:219]. Int Urogynecol J Pelvic Floor Dysfunct 14:164–168. 10.1007/s00192-003-1063-2 [DOI] [PubMed] [Google Scholar]
- 26.Brubaker L, Handa VL, Bradley CS, Connolly A, Moalli P, Brown MB, et al. (2008) Sexual function 6 months after first delivery. Obstet Gynecol 111:1040–1044. 10.1097/AOG.0b013e318169cdee [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sentilhes L, Berthier A, Sergent F, Verspyck E, Descamps P, Marpeau L (2008) Sexual function in women before and after transvaginal mesh repair for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 196:763–772. 10.1007/s00192-007-0521-7 [DOI] [PubMed] [Google Scholar]
- 28.Fatton B, Letouzey V, Lagrange E, Mares P, Jacquetin B, de Tayrac R (2009) [Validation of a French version of the short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12)]. J Gynecol Obstet Biol Reprod 38:662–667. 10.1016/j.jgyn.2009.02.008 [DOI] [PubMed] [Google Scholar]
- 29.Fritel X, Schaal JP, Fauconnier A, Bertrand V, Levet C, Pigné A (2008) Pelvic floor disorders 4 years after first delivery: a comparative study of restrictive versus systematic episiotomy. BJOG 115: 247–252. 10.1111/j.1471-0528.2007.01540.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adouard F, Glangeaud-Freudenthal NM, Golse B (2005) Validation of the Edinburgh postnatal depression scale (EPDS) in a sample of women with high-risk pregnancies in France. Arch Womens Ment Health 8:89–95. 10.1007/s00737-005-0077-9 [DOI] [PubMed] [Google Scholar]
- 31.Guedeney N, Fermanian J (1998) Validation study of the French version of the Edinburgh Postnatal Depression Scale (EPDS): new results about use and psychometric properties. Eur Psychiatry 13:83–89. 10.1016/S0924-9338(98)80023-0 [DOI] [PubMed] [Google Scholar]
- 32.Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150:782–786. [DOI] [PubMed] [Google Scholar]
- 33.Cox JL (2003) Perinatal mental health: a guide to the Edinburg Postnatal Depression Scale (EPDS). London: Gaskell. [Google Scholar]
- 34.Sword W, Landy CK, Thabane L, Watt S, Krueger P, Farine D, et al. (2011) Is mode of delivery associated with postpartum depression at 6 weeks: a prospective cohort study. BJOG 118:966–977. 10.1111/j.1471-0528.2011.02950.x [DOI] [PubMed] [Google Scholar]
- 35.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830. [DOI] [PubMed] [Google Scholar]
- 36.Safarinejad MR, Kolahi AA, Hosseini L (2009) The effect of the mode of delivery on the quality of life, sexual function, and sexual satisfaction in primiparous women and their husbands. J Sex Med 6:1645–1667. 10.1111/j.1743-6109.2009.01232.x [DOI] [PubMed] [Google Scholar]
- 37.Giuliano F (2013) [Questionnaires in sexual medicine]. Prog Urol 23:811–821. [DOI] [PubMed] [Google Scholar]
- 38.Bozdogan H (1987) Model Selection and Akaike's Information Criterion (AIC): The General Theory and Its Analytical Extensions. Psychometrika 52: 345–370. [Google Scholar]
- 39.Burnham KP, Anderson DR (2002) Model Selection and Multimodel Inference: A Practical Information-Theoretic Approach (2nd ed.), Springer-Verlag. [Google Scholar]
- 40.Mous M, Muller SA, de Leeuw JW (2008) Long-term effects of anal sphincter rupture during vaginal delivery: Faecal incontinence and sexual complains. BJOG 115:234–238. 10.1111/j.1471-0528.2007.01502.x [DOI] [PubMed] [Google Scholar]
- 41.Murphy DJ, Liebling RE, Verity L, Swingler R, Patel R (2001) Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet 358: 1203–1207. 10.1016/S0140-6736(01)06341-3 [DOI] [PubMed] [Google Scholar]
- 42.Buhling KJ, Schmidt S, Robinson JN, Klapp C, Siebert G, Dudenhausen JW (2006) Rate of dyspareunia after delivery in primiparae according to mode of delivery. Eur J Obstet Gynecol Reprod Biol 124: 42–46. 10.1016/j.ejogrb.2005.04.008 [DOI] [PubMed] [Google Scholar]
- 43.Barrett G, Pendry E, Peacock J, Victor C, Thakar R, Manyonda I (2000) Women’s sexual health after childbirth. BJOG 107:186–195. [DOI] [PubMed] [Google Scholar]
- 44.Liebling RE, Swingler R, Patel RR, Verity L, Soothill PW, Murphy DJ (2004) Pelvic floor morbidity up to one year after difficult instrumental delivery and cesarean section in the second stage of labor: a cohort study. Am J Obstet Gynecol 191: 4–10. 10.1016/j.ajog.2004.01.013 [DOI] [PubMed] [Google Scholar]
- 45.McDonald EA, Brown SJ (2013) Does method of birth make a difference to when women resume sex after childbirth? BJOG 120:823–830. 10.1111/1471-0528.12166 [DOI] [PubMed] [Google Scholar]
- 46.McDonald EA, Gartland D, Small R, Brown SJ (2015) Dyspareunia and childbirth: a prospective cohort study. BJOG 122:672–679. 10.1111/1471-0528.13263 [DOI] [PubMed] [Google Scholar]
- 47.Thompson JF, Roberts CL, Currie M, Ellwood DA (2002) Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth 29:83–94. [DOI] [PubMed] [Google Scholar]
- 48.Woolhouse H, Gartland D, Perlen S, Donath S, Brown SJ (2014) Physical health after childbirth and maternal depression in the first 12 months post partum: results of an Australian nulliparous pregnancy cohort study. Midwifery 30:378–384. 10.1016/j.midw.2013.03.006 [DOI] [PubMed] [Google Scholar]
- 49.De Souza A, Dwyer P, Charity M, Thomas E, Ferreira C, Schierlitz L (2015) The effects of mode delivery on postpartum sexual function: a prospective study. BJOG 122:1410–1418. 10.1111/1471-0528.13331 [DOI] [PubMed] [Google Scholar]
- 50.Serati M, Salvatore S, Khullar V, Uccella S, Bertelli E, Ghezzi F, Bolis P (2008) Prospective study to assess risk factor for pelvic floor dysfunction after delivery. Acta Obstet Gynecol Scand 87:313–318. 10.1080/00016340801899008 [DOI] [PubMed] [Google Scholar]
- 51.Pauls RN, Occhino JA, Dryfhout VL (2008) Effects of pregnancy on female sexual function and body image: a prospective study. J Sex Med 5:1915–1922. 10.1111/j.1743-6109.2008.00884.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.