Abstract
Objective
To understand perceived barriers to providing cardiopulmonary resuscitation (CPR) education, implementation processes, and practices in high schools.
Study design
Iowa has required CPR as a graduation requirement since 2011 as an unfunded mandate. A cross-sectional study was performed through multiple choice surveys sent to Iowa high schools to collect data about school demographics, details of CPR programs, cost, logistics, and barriers to implementation, as well as automated external defibrillator training and availability.
Results
Eighty-four schools responded (26%), with the most frequently reported school size of 100-500 students and faculty size of 25-50. When the law took effect, 51% of schools had training programs already in place; at the time of the study, 96% had successfully implemented CPR training. Perceived barriers to implementation were staffing, time commitment, equipment availability, and cost. The average estimated startup cost was <$1000 US, and the yearly maintenance cost was <$500 with funds typically allocated from existing school resources. The facilitator was a school official or volunteer for 81% of schools. Average estimated training time commitment per student was <2 hours. Automated external defibrillators are available in 98% of schools, and 61% include automated external defibrillator training in their curriculum.
Conclusions
Despite perceived barriers, school CPR training programs can be implemented with reasonable resource and time allocations.
Survival of out-of-hospital cardiac arrest (OHCA), defined as survival to hospital discharge, has remained unchanged at 10%-12% over several decades.1,2 Despite these overall poor survival outcomes, studies have identified several predictors that improve survival in OHCA: witnessed arrest, bystander cardiopulmonary resuscitation (CPR), ventricular fibrillation as the initial rhythm, early defibrillation, and minimized delay in the arrival of emergency services personnel.3 In a witnessed arrest, prompt initiation of bystander CPR can double a patient's likelihood of survival.4 The Public Access Defibrillation trial also documented that survival for victims of cardiac arrest doubled, with a low risk of adverse events, in communities where automated external defibrillators (AEDs) were available and cardiac arrest emergency response plans were implemented.5 Various studies have demonstrated that training in basic life support, including knowledge of high-quality CPR and the use of AEDs, increases the likelihood of bystander intervention and victim survival.6-8 However, the overall prevalence of CPR training in the US is low. Anderson et al9 looked at individual counties in the US and found that median prevalence of CPR training in the middle tertile was 2.4% per year.
Many US states have adopted school instruction to improve the number of persons trained in CPR. To date, 32 states have passed legislation with variable language requiring high school students be trained in CPR techniques before graduation. In the majority of cases, the legislation does not contain specific language or guidelines as to how to implement or pay for these programs. Iowa has had CPR training as a high school graduation requirement since 2011 through a legislative mandate that provided no funds to the schools to pay for the programs. The objective of this study was to evaluate the implementation process, practices, and perceived barriers to providing CPR and AED education to high school students. We surveyed all Iowa high schools to help provide guidance for new programs based on over 4 years of experience.
Methods
A cross-sectional study was performed through electronic surveys sent to all 346 Iowa high schools. A 20-item multiple choice questionnaire was developed to obtain descriptive data (Appendix; available at www.jpeds.com). Email contact addresses for each school principal or superintendent were obtained from publicly available athletic association directories. Each survey was accompanied by a short introductory email explaining the purposes of the questionnaire. Compensation was not provided for participation in the survey. Prospective participants were contacted up to 3 times via email: the initial survey followed by a reminder 2 weeks after distribution and a final reminder in 6 weeks. The survey distributed online was open for response for 60 days after distribution from March 2, 3015, to May 1, 2015. We used the Qualtrics (Provo, Utah), Internet-based survey software that allows viewing and completion across multiple platforms, to distribute, collect, and analyze the data. The responses of the survey were recorded and tabulated in real time and the submitted data could be viewed as individual responses or in aggregate for ease of analysis. The survey did not require approval by the University of Iowa Institutional Review Board because it did not collect identifying information. Data are presented as most common response (mode) with range.
Results
Completed surveys were received from 84 high schools across Iowa, a response rate of 26%. A flow diagram of the completed surveys demonstrates the breakdown of responses (Figure 1; available at www.jpeds.com). When the law took effect in 2011, 51% of schools had training programs already in place, and at the time of the survey 96% of schools had successfully implemented CPR training. Responding high schools were distributed throughout the state and represented a range of student body sizes, from fewer than 100 and up to 2500-5000 students (Figure 2; available at www.jpeds.com). The Table provides the school demographics and characteristics of CPR training programs. Perceived barriers to implementation, ranked by number of responses, were staffing, time commitment, equipment availability, and cost in decreasing order (Figure 3). No responding schools identified liability concerns as a barrier.
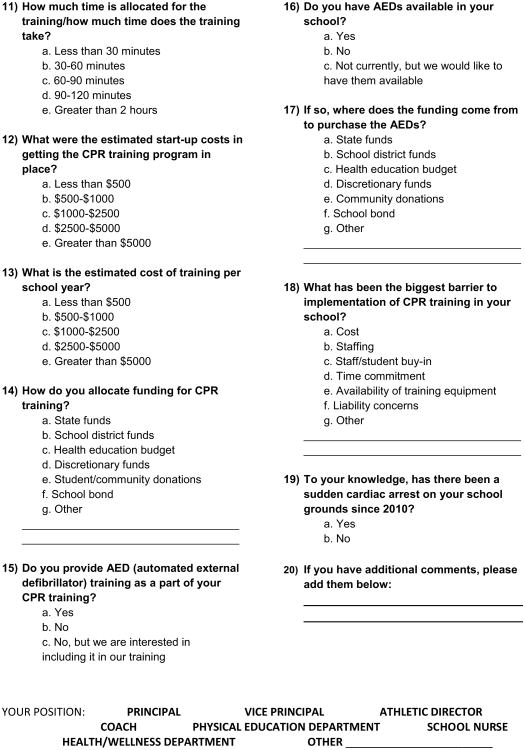
Figure 1.
Breakdown of survey responses. Incomplete surveys were not included in reported data.
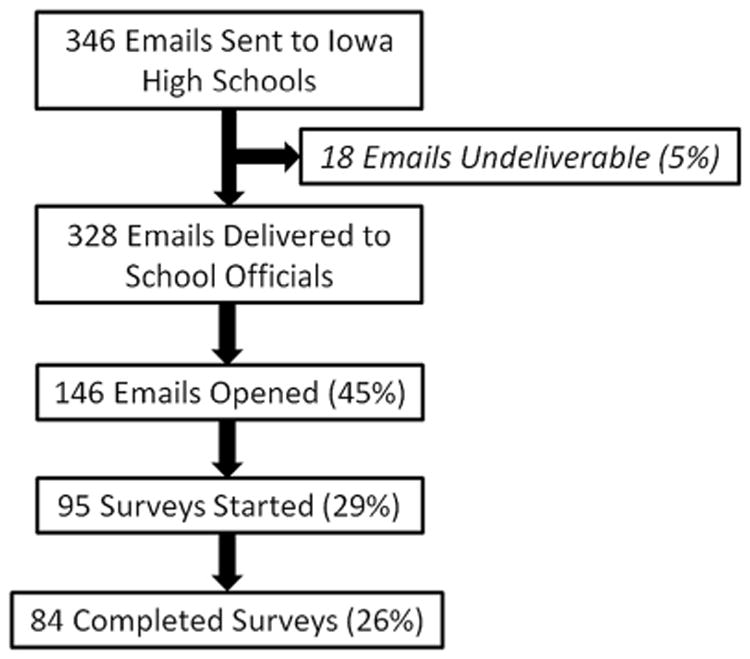
Figure 2.
Map of responding Iowa high schools as identified by IP address. Stars indicate location of responding schools.
Figure 3.
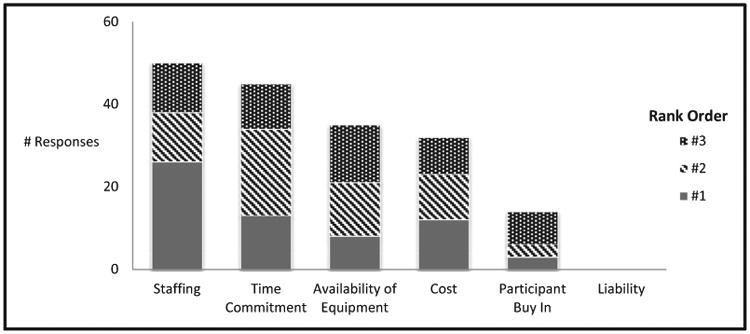
Perceived barriers to implementation of CPR training. Respondents were asked to rank perceived barriers from 1 (most significant) to 3 (least significant).
The training facilitator was a school employee or unpaid volunteer in 81% of schools; 19% reported a paid instructor. Average estimated time commitment for training was <2 hours per student and training most commonly occurred during school hours; only 7% of schools responded that their students and staff participated in training outside of established school hours (Figure 4, A). The most common estimated startup costs were ≤$1000 and the yearly maintenance costs were <$500, with funds typically allocated from existing school district funds (Figure 4, B). Training equipment was obtained from diverse sources (Figure 4, C). The AEDs are available in 98% of responding schools, but only 61% of schools include AED instruction in their training curriculum. The AEDs were purchased or obtained from various sources (Figure 4, D). Schools were also asked if there had been a sudden cardiac arrest on their campus since 2010, just before the state mandate took effect. Five percent of schools responding to the survey reported that there had been a witnessed cardiac arrest on their school grounds within the last 5 years.
Figure 4.
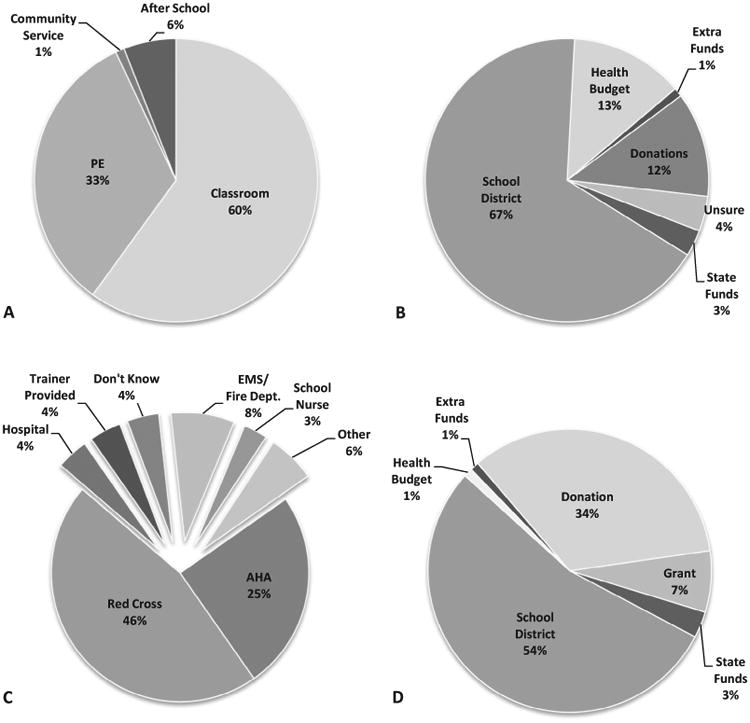
Responses to survey questions. A, Setting of high school CPR training. B, Sources of funding for high school CPR training programs. C, Suppliers of CPR training equipment. D: Sources of funding for purchase of AEDs.
Survey results also show a low proportion of staff is trained in CPR: 43% of schools have <10 staff members who are CPR trained and 88% of schools do not ask about CPR training during the faculty hiring process.
Discussion
The results of our survey of Iowa high schools show that, once the training programs were started successfully, anticipated obstacles did not match with the reality of implementation. The perceived barriers identified by the responses to the multiple choice survey were similar to a 2003 report describing high school CPR programs in Washington state that identified the most significant barriers were time within the curriculum to teach CPR, lack of funds, and instructor scheduling difficulties.10 The majority of legislative directives are not subsidized at the state level and do not give guidance as to how to implement CPR training programs. In light of this, these perceived barriers are understandable for an individual school. However, this survey demonstrates that, in actuality, the burden on individual schools to start and maintain these programs was minimal.
High-quality CPR has been shown to be associated with improved outcomes after witnessed cardiac arrest.7 The goal of a CPR training program should be to train students to provide high-quality resuscitative techniques if called upon. This survey was focused on the execution of CPR training programs in Iowa high schools and we did not attempt any qualitative measures of the individual programs. When Iowa initially wrote the mandate into state law, it specified that “every pupil physically able to do so shall have completed a psychomotor course that leads to certification in cardiopulmonary resuscitation” and the classes “may be taught during the school day by either a school or school district employee or by a volunteer, as long as the person is certified to teach a course that leads to certification in CPR.”11 The survey results also demonstrate that the majority of schools are employing CPR training programs from well-established sources, predominantly the American Red Cross and the American Heart Association. Given that the initial law required certification before graduation and the responding schools used well-tested resources for CPR education, it could be speculated that the quality of CPR training was excellent. Regardless, any bystander CPR, even with poor quality chest compressions and ineffective ventilations, improves survival in cardiac arrest over not receiving any re-suscitative efforts.7 Therefore, any training that improves bystander response may be of benefit to the victims of sudden cardiac arrest.
Bystander CPR and appropriate use of an AED have been shown to improve dramatically the likelihood of survival in witnessed sudden cardiac arrest. Individuals without medical training are often reluctant to perform CPR on a stranger.12 The most common reasons cited for reluctance to initiate a potentially life-saving intervention include fear of infection, concern that CPR may be harmful to the victim, and fear of legal consequences. However, training in the basic life support techniques of CPR and use of AEDs improves bystander willingness to initiate therapy significantly.6,13 Reluctance to perform CPR has also further decreased with the adoption of compression-only CPR for first responders.6 Additionally, training increases the understanding of the importance of early activation of emergency medical services and use of an AED. Prior AED training has also been correlated with a significant increase in willingness to provide life support to a stranger.14 The knowledge that lay responders do not need specific medical training to use an AED14 is also important, because ventricular arrhythmias, which require immediate defibrillation, are associated with increased survival, particularly if there is prompt initiation of bystander CPR.15 Our survey demonstrated that AEDs are becoming more common in Iowa high schools, but a large proportion of schools did not report that AED training had been incorporated as a part of their resuscitation curriculum.
Among the strongest recommendations of the 2015 Institute of Medicine report on cardiac arrest16 was a call to action for increased public education and training in CPR, including promotion and facilitation of CPR and AED training as a graduation requirement for middle and high school students. This endorsement of increased CPR training for school-age children echoes the statements from the American Heart Association17 and the European Resuscitation Council,18 including the European Resuscitation Council statement “Kids Save Lives,” which received the endorsement of the World Health Organization.19 Training lay people in techniques of CPR and use of AEDs has been demonstrated to improve significantly bystander willingness to initiate therapy as well as victim survival.6,13 The goal of training students through school-based CPR programs would increase significantly the number of lay people with knowledge of these life-saving techniques nationwide. According to the National Center for Education Statistics, 3.3 million students were expected to graduate from high school in 2014-2015 in the US. Training young adults in a high school setting is ideal for multiple reasons: students in a classroom are a “captive audience”; the majority of high school students are physically mature and able to learn and perform the psychomotor skills of CPR; and training students in their adolescent years prepares them for a life-long knowledge of CPR. Surveys of high school students have demonstrated their willingness to perform CPR.10 There is broad support from leading worldwide organizations committed to improving survival after cardiac arrest for widespread CPR training of school-age children.
The current rates of CPR training in the US are low with broad regional variations in training. The lowest rates are seen in rural communities, those with higher proportions of black and Hispanic residents, and those with lower median household incomes.9 There is also a disparity in populations who are likely to receive bystander CPR: black and Hispanic arrest victims are less likely to receive CPR than their white counterparts.20,21 School-based training of students in urban and rural communities may help to address the disparities in CPR training and bystander provision in low-income and ethnically diverse populations. With improved education and reduction of barriers to providing bystander CPR, the potential public health benefit and improvement in the overall health of the nation could be substantial.
The benefits of a large-scale, national training program have been demonstrated previously in Sweden through a nationwide effort to increase CPR training beginning in 1983.22 Using a train-the-trainer method, by the mid 1990s they estimated that approximately 20% of the general population had been trained in CPR. Bystander CPR was initiated in 36% of OHCA and 56% of these first responders were lay people. Most notably, they also were able to demonstrate that bystander CPR was associated with a 2- to 3-fold increase in survival during the study period.22 A follow-up study looking at outcomes of OHCA from 1992-2009 again reinforced the relationship between bystander CPR survival to hospital admission as well as survival at 1 month, and they estimated that the percentage of patients receiving bystander CPR increased from approximately 46% to 73% during this time period.23 It is conceivable that, with broad CPR training of high school students, similar results could be seen in the US.
There are limitations intrinsic to studies conducted through surveys, primarily response bias. One-quarter of schools that were sent the survey responded and there was broad regional and size distribution of the responding schools. It is possible that the schools that did not respond had more difficulty implementing CPR programs in their schools or encountered significant barriers during the implementation process. Our response rate was similar to other studies that used web-based surveys, however.24 Schools responded that the average startup costs associated with the CPR training programs were <$1000, which may be subject to recall bias. A review of publicly available CPR training material marketed for school CPR training programs have advertised prices of $625-$1000 for inclusive kits for student training.25,26 It also stands to reason that, had the initial cost been onerous, then it would be likely that the school official's recollection of the initial cost would be much greater. Iowa has a small population and is on average well educated: 2014 US census data estimate a population of 3 107 126; 23.4% of the population is 18 years of age or younger and 91% of the population 25 years of age or older has completed a high school education or beyond, and these factors have been associated previously with an increased likelihood of providing bystander CPR.11 Because of this, our results may not be generalizable to other states with larger populations or different regional demographics.
CPR is a vital link in the chain of survival for sudden cardiac arrest; therefore, increasing bystander CPR through community training initiatives like CPR programs in high schools should be a goal worldwide. Our survey shows that, after 4 years of successful implementation after passage of an unfunded state mandate, high school CPR programs can be implemented and maintained with minimal resource allocation.
Demographics of responding schools and characteristics of CPR training programs.
| Mode | Range | |
|---|---|---|
| School size | 100-500 | <100 to 2500-5000 |
| Faculty size | 25-50 | <25 to >250 |
| Staff members trained in CPR | <10 | <10 to >50 |
| Start-up cost | <$500 | <$500 to >$5000 |
| Maintenance cost | <$500 | <$500 to >$5000 |
| Time commitment | 90-120 minutes | <30 minutes to >2 hours |
Acknowledgments
We thank the educators, administrators, and school officials who participated in the survey and for their ongoing efforts to educate and train their students in effective CPR techniques.
Glossary
- AED
Automated external defibrillator
- CPR
Cardiopulmonary resuscitation
- OHCA
Out-of-hospital cardiac arrest
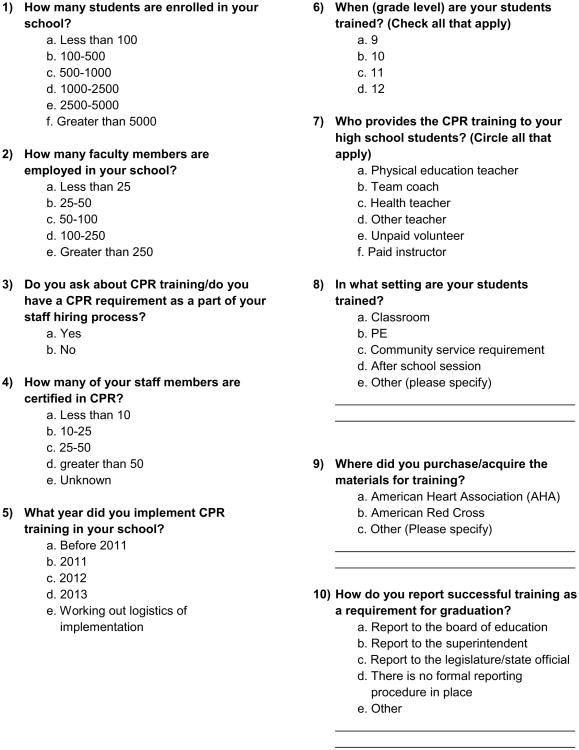
Appendix.
Figure 1.
University of Iowa Children's Hospital high school CPR training program survey.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 3.Herlitz J, Engdahl J, Svensson L, Angquist KA, Young M, Holmberg S. Factors associated with an increased chance of survival among patients suffering from an out-of-hospital cardiac arrest in a national perspective in Sweden. Am Heart J. 2005;149:61–6. doi: 10.1016/j.ahj.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 4.Weston CFM, Wilson RJ, Jones SD. Predicting survival from out-of-hospital cardiac arrest: a multivariate analysis. Resuscitation. 1997;34:27–34. doi: 10.1016/s0300-9572(96)01031-3. [DOI] [PubMed] [Google Scholar]
- 5.Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Cristenson J, McBurnie MA, et al. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–46. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 6.Cho GC, Sohn YD, Kang KH, Lee WW, Lim KS, Kim W, et al. The effect of basic life support education on laypersons' willingness in performing bystander hands only cardiopulmonary resuscitation. Resuscitation. 2010;81:691–4. doi: 10.1016/j.resuscitation.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 7.Gallagher EJ, Lombardi G, Gennis P. Effectiveness of bystander cardio-pulmonary resuscitation and survival following out-of-hospital cardiac arrest. JAMA. 1995;274:1922–5. [PubMed] [Google Scholar]
- 8.Herlitz J, Svensson L, Holmberg S, Angquist KA, Young M. Efficacy of bystander CPR: intervention by lay people and by health care professionals. Resuscitation. 2005;66:291–5. doi: 10.1016/j.resuscitation.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 9.Anderson ML, Cox M, Al-Khatib SM, Nichol G, Thomas KL, Chan PS, et al. Rates of cardiopulmonary resuscitation training in the United States. JAMA Intern Med. 2014;174:194–201. doi: 10.1001/jamainternmed.2013.11320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reder S, Quan L. Cardiopulmonary resuscitation training in Washington state public high schools. Resuscitation. 2003;56:283–8. doi: 10.1016/s0300-9572(02)00376-3. [DOI] [PubMed] [Google Scholar]
- 11.The Iowa Legislature. Amendment 12.5(20) [Accessed April 19, 2016]; http://www.legis.iowa.gov/docs/aco/arc/7504B.rtf.
- 12.Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR trained bystanders perform CPR? Acad Emerg Med. 2006;13:596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 13.Kanstad BK, Nilsen SA, Fredriksen K. CPR knowledge and attitude to performing bystander CPR among secondary school students in Norway. Resuscitation. 2011;82:1053–9. doi: 10.1016/j.resuscitation.2011.03.033. [DOI] [PubMed] [Google Scholar]
- 14.Hamasu S, Morimoto T, Kuramoto N, Horiguchi M, Iwami T, Nishiyama C, et al. Effects of BLS training on factors associated with attitude toward CPR in college students. Resuscitation. 2009;80:359–64. doi: 10.1016/j.resuscitation.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 15.Swor R, Jackson RE, Cynar M, Sadler E, Basse E, Boji B, et al. Bystander CPR, ventricular fibrillation, and survival in witnessed, unmonitored out-of-hospital cardiac arrest. Ann Emerg Med. 1995;25:780–4. doi: 10.1016/s0196-0644(95)70207-5. [DOI] [PubMed] [Google Scholar]
- 16.IOM (Institute of Medicine) Strategies to improve cardiac arrest survival: a time to act. Washington DC: The National Academies Press; 2015. [PubMed] [Google Scholar]
- 17.Cave DM, Aufderheide TP, Beeson J, Ellison A, Gregory A, Hazinski MF, et al. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools: a scientific advisory from the American Heart Association. Circulation. 2011;123:691–706. doi: 10.1161/CIR.0b013e31820b5328. [DOI] [PubMed] [Google Scholar]
- 18.Greif R, Lockey AS, Conaghan P, Lippert A, De Vries W, Monsieurs KG. European Resuscitation Council guidelines for resuscitation 2015: section 10. Education and implementation of resuscitation. Resuscitation. 2015;95:288–301. doi: 10.1016/j.resuscitation.2015.07.032. [DOI] [PubMed] [Google Scholar]
- 19.Böttiger BW, Van Aken H. Kids save lives—Training school children in cardiopulmonary resuscitation worldwide is now endorsed by the World Health Organization (WHO) Resuscitation. 2015;94:A5–7. doi: 10.1016/j.resuscitation.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Moon S, Bobrow BJ, Vadeboncoeur TF, Kortuem W, Kisakye M, Sasson C, et al. Disparities in bystander CPR provision and survival from out-of-hospital cardiac arrest according to neighborhood ethnicity. Am J Emerg Med. 2014;32:1041–5. doi: 10.1016/j.ajem.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 21.Brookoff D, Kellermann AL, Hackman BB, Somes G, Dobyns P. Do blacks get bystander cardiopulmonary resuscitation as often as whites? Ann Emerg Med. 1994;24:1147–50. doi: 10.1016/s0196-0644(94)70246-2. [DOI] [PubMed] [Google Scholar]
- 22.Holmberg M, Holmberg S, Herlitz J. Effect of bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients in Sweden. Resuscitation. 2000;47:59–70. doi: 10.1016/s0300-9572(00)00199-4. [DOI] [PubMed] [Google Scholar]
- 23.Adielsson A, Hollenberg J, Karlsson T, Lindqvist J, Lundin S, Silfverstolpe J, et al. Increase in survival and bystander CPR in out-of-hospital shock-able arrhythmia: bystander CPR and female gender are predictors of improved outcome. Experience from Sweden in an 18-year perspective. Heart. 2011;97:1391–6. doi: 10.1136/hrt.2011.222711. [DOI] [PubMed] [Google Scholar]
- 24.Kaplowitz MD, Hadlock TD, Levine R. A comparison of web and mail survey response rates. Public Opin Q. 2004;68:94–101. [Google Scholar]
- 25.The American Heart Association. CPR in schools training kits. [Accessed April 19, 2016]; http://cpr.heart.org/AHAECC/CPRAndECC/Training/CPRInSchoolsTrainingKits/UCM_473191_CPR-In-Schools-Training-Kits.jsp.
- 26.American Red Cross. Red Cross store. [Accessed April 19, 2016]; http://www.redcrossstore.org/home.