Abstract
Marijuana initiation during adolescence, and early adolescence in particular, is associated with adverse health consequences. Our study used 2005–2014 data from the annual, cross-sectional National Survey on Drug Use and Health to study the prevalence and correlates of marijuana initiation, use, and marijuana use disorder (MUD; abuse or dependence) among 12- to 14-year olds living in civilian US households (n = 84 954). Examined correlates included age, sex, race/ethnicity, poverty status, metropolitan status, year of survey, depression, tobacco use, alcohol use, and fighting at school. Sex differences in the correlates of lifetime use and past year marijuana initiation were tested via interaction. Lifetime prevalence of marijuana use was 5.5%; 3.2% reported past year initiation. About 1 in 6 (16.8%) past year initiates progressed to MUD within 12 months of first use. Although men had higher prevalence of lifetime use than women, past year initiation did not differ by sex. On examining the sex*race/ethnicity interaction effects, findings determined that non-Hispanic black and Hispanic men had higher prevalence estimates of ever using marijuana and incidence of past year initiation as compared with non-Hispanic white men; these race/ethnicity differences were not found among women. Identifying correlates of initiation and progression to MUD among young adolescents is critical to improve prevention and treatment program targets.
Keywords: Adolescence, marijuana smoking, marijuana use disorder, epidemiology, sex differences, correlates
Introduction
Substance use among youth is a significant public health problem in the United States.1,2 Marijuana is the most widely used drug among adolescents3,4 and is the primary substance of abuse in 3 out of 4 adolescent substance use treatment discharges.5 The 2015 Monitoring the Future (MTF) study estimates of daily use and past month use of marijuana among high school seniors exceeded those of cigarettes for the first time in history.6 According to the 2015 National Survey on Drug Use and Health (NSDUH), the US prevalence of life-time marijuana use increases from 1.4% to 8.7% to 34.2% at 12, 14, and 17 years of age, respectively.7 Furthermore, rates of adolescent marijuana initiation in 2015 were higher than estimates from 2002 to 2008 surveys, although increasing trends appear to have stabilized since 2009.
In addition to the risk of developing a marijuana use disorder (MUD) and using other illegal substances, research has indicated significant associations between adolescent marijuana use and poor social and educational functioning8,9 as well as having other mental health problems,10–12 including psychosis and suicidality.13,14 Furthermore, adverse sequelae of marijuana use often extend into adulthood, including continued marijuana and other drug use and misuse, cognitive impairment, criminal justice involvement, and ongoing mental and physical health problems.15–17
Marijuana use during the early adolescent period may be particularly problematic. Early marijuana initiation is associated with increased amount and frequency of marijuana use, heightened risk of developing MUD, and faster progression to meeting MUD criteria.18 Moreover, early initiation of marijuana use is associated with greater severity of MUD, lower responsiveness to substance use treatment, and increased likelihood of negative social outcomes such as poor school performance, school dropout, and teenage pregnancy.19–21 Finally, marijuana use and abuse may disrupt the normal brain maturation processes that occur during the developmental period of young adolescence, which may have long-term consequences for users.22,23
Despite prior studies indicating that early adolescence may be a key window for prevention of marijuana initiation and subsequent use and development of MUD, there have been few US studies focused specifically on early adolescence that have included samples as young as 12 years of age from household populations. Much of what is known about early adolescent marijuana use in the United States, in the absence of national surveillance data from children and young adolescents, comes from studies that use samples of older adolescents or adults retrospectively recalling marijuana use during early adolescence, which may be subject to recall bias.24 Because much of the literature on adolescent marijuana use is based on data collected from clinical or school-based samples such as the MTF study6 and the Youth Risk Behavior Survey (YRBS),25 current epidemiology and clinical evidence about young adolescent marijuana use in the United States is further limited and not generalizable to a population that includes high-risk adolescents who are not enrolled in school or frequently absent from school or who have limited health care access. One exceptional study to this limitation used a nationally representative sample of adolescents aged 13 years or older from the nationally representative National Comorbidity Survey Adolescent Supplement (NCS-A) conducted between 2001 and 2004 to study marijuana use prevalence and correlates among adolescents. Findings from this study, however, are now over a decade old. In addition to providing a replication and update of the findings from the NCS-A investigation, this study permits the first investigation of marijuana use and also transitions to MUD among adolescents as young as 12 years old.
Few population-based US studies conducted among early adolescents have examined the nature and intensity of correlates of marijuana initiation, use, and MUD. It is unclear whether significant correlates found in prior studies conducted among older adolescents or young adults, who often need to retrospectively recall initiation and transitions to regular use and MUD, extend to younger adolescent samples from a nationally representative US household-based study, and whether correlates differ by stage of use (ie, initiation, regular use, patterns of use, and subsequent consequences that meet criteria for MUD).26,27 In addition, recent investigations using samples across a broader range of adolescence have determined that the patterns of use and progression to MUD as well as risk and protective factors may differ by sex.28–31 For example, studies have indicated that male adolescents are more likely than women to initiate and use marijuana. Whether these prior findings extend to a US nationally representative sample that include adequate samples of young adolescents and whether other correlates of marijuana initiation and use among young adolescents differ by sex is critical. Furthermore, at the forefront of scientific discussion as of late, replication of previous study findings is crucial to maintain confidence in findings, observe associations in different samples, and move the field forward.32–34
The development of effective marijuana prevention and intervention strategies for young adolescents requires identification of correlates along each stage of the trajectory from initiation to develop MUD. A better understanding of risk factors or correlates of MUD may come from conditioning the analyses on initial use. Importantly, failing to adjust for differences in initiation when examining correlates of use and harmful use by, for example, conditioning on initiation might lead to factors being identified as significant correlates only because of significant relationships with marijuana initiation but not use or harmful use once initiated. Thus, identifying correlates of developing MUD after initiation may lend clues about cause, mechanisms of expression, and course of illness, help clinicians identify patients at high risk of developing MUD,35 and determine how to target resources more effectively.
This study addresses these existing limitations by examining estimates and correlates of lifetime marijuana use, past year initiation, and progression to MUD among lifetime marijuana users and among past year initiates aged 12 to 14 years living in US households. Each of these analyses is important to examine different aspects of marijuana use and misuse. The study of prevalence and correlates of lifetime marijuana use and of past year initiation will illuminate factors associated with use up to and including the 12- to 14-year age range plus identify the correlates of first use among young adolescents aged 12 to 14 years. Primary prevention is critical, in part, because the detrimental neurocognitive effects of marijuana use remain even after abstinence.36 Similarly, it is important to study correlates of MUD among all users but specifically, young adolescents who rapidly progress from first using marijuana to having clinically significant problems with marijuana use. This information can help guide marijuana prevention and treatment efforts that target young adolescents who have not yet tried marijuana (correlates of initiation) and who recently tried marijuana and might be at risk of rapid development of a MUD (correlates of MUD among recent initiates). There is an urgent need for this study given the scant epidemiologic data of children’s marijuana use in the United States as young as 12 years of age, especially from household samples that include children not enrolled in school or who have high rates of absenteeism and thus might not be captured in a school-based survey.
Method
Sample
Data come from the public use files of the 2005–2014 NSDUH. Funded by the Substance Abuse and Mental Health Services Administration (SAMHSA), NSDUH is an annual, nationally representative cross-sectional survey of persons 12 years of age or older who are residents of households, noninstitutional group quarters, or civilians living on military bases. The Institutional Review Board (IRB) of the contracting organization (Research Triangle Institute [RTI] International) approved all study procedures; however, the analyses conducted for this study were exempt from additional IRB review because the public use files used consist only of de-identified data.
National Survey on Drug Use and Health interviews are conducted in US residential households. Data on demographics, mental health, and substance use examined in this analysis focus on 12- to 14-year olds surveyed between 2005 and 2014 (n = 84 954). After describing the study procedures to each participant, the NSDUH interviewer obtained informed consent verbally from a parent or guardian and assent verbally from each adolescent respondent. The NSDUH interviewer did not obtain written consent. To better assure confidentiality; the names of respondents are not used in the survey.37 The interviewer24 requested the sampled respondent to identify a private area in the home to conduct the interview away from other household members. Approximately three-fourths of NSDUH interviews with adolescents were conducted with no one else in the room, that is, in complete privacy.38 Each interview averaged about an hour and included a combination of computer-assisted personal interviewing (CAPI) and audio computer-assisted self-interviewing (ACASI) assessments. In the CAPI portion, the interviewer read the questions to the respondent and recorded the answers. In the ACASI portion of the interview, the respondent read questions on screen or listened to questions through headphones and then recorded his or her answers without the interviewer knowing the response.39 At the conclusion of the ACASI section, the interview returned to the CAPI mode with the interviewer completing the questionnaire. A $30 cash incentive was provided to each respondent who completed a full interview as a token of appreciation for his or her time. No personal identifying information about the respondent was captured in the record. The interviewer transmitted the completed interview data to RTI in Research Triangle Park, North Carolina.40 The NSDUH response rates averaged 84.3% for adolescents aged 12 to 17 years between 2005 and 2014 (range: 80.0%-87.1%). Additional details about the sample, study procedures, and interviewer training have been reported elsewhere.37
Variables
Marijuana initiation, past month use, lifetime use, and MUD
Respondents were asked, “Have you ever, even once, used marijuana or hashish.” Those who answered “yes” were determined to have lifetime use. They were then asked “How old were you the first time you used marijuana or hashish?” The age at first use was subtracted from the survey age, and those who had a difference of 1 or 0 (ie, used marijuana for the first time in the year prior to the survey year) were determined to be past year initiates. Those who had started using marijuana more than 1 year prior to the survey date were removed from the denominator when examining marijuana initiation. Past month use and past year use were determined by response to the question, “How long has it been since you last used marijuana or hashish?” A series of questions was used to classify adolescents as having a past year MUD based on meeting criteria for abuse or dependence as specified in the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition; DSM-IV).41 A respondent was defined as having marijuana dependence if he or she met 3 or more of the 7 dependence criteria. A respondent was defined as having marijuana abuse if he or she met one or more of the 4 abuse criteria and was determined not to be dependent on marijuana in the past year (ie, dependence took precedence over abuse). Those with either past year marijuana dependence or abuse were classified as having a past year MUD. Additional information about the creation of these variables in the NSDUH is provided elsewhere.39 Self-report–based diagnoses of MUD by adolescents have demonstrated reliability in prior studies, particularly when using a confidential assessment method such as NSDUH’s computer-assisted self-interviewing.42
Correlates
Potential correlates were selected based on results of prior studies. Demographic variables included age (12, 13, or 14 years), sex, and race/ethnicity categorized as non-Hispanic white, non-Hispanic black, non-Hispanic other, and Hispanic. Other sociodemographic information included poverty level based on a definition of poverty level that incorporates information on family income, size, and composition and is calculated as a percentage of the US Census Bureau’s poverty thresholds (less than 100% of the federal poverty level [FPL], 100% to 199% of the FPL, and 200% or greater), and metropolitan status, which categorized the place of residence as urban (located in a population segment in a core-based statistical area [CBSA] with 1 million or more persons), suburban (located in a population segment in a CBSA with fewer than 1 million persons), or rural (located in a population segment not in a CBSA). Survey year was included in analyses to adjust for differences in marijuana indicators over time. Assessment of lifetime major depressive episode (MDE) was based on the DSM-IV criteria.41 The NSDUH lifetime MDE measure is defined as having in the same 2-week period at least 5 of the 9 symptoms of a depressive episode, with at least one of the symptoms being depressed mood or loss of interest or pleasure in activities that had previously been pleasurable. It should be noted, however, that unlike the DSM-IV criteria for MDE, no exclusions were made in NSDUH for depressive symptoms caused by a medical illness, bereavement, or substance use.40 Lifetime alcohol use was classified according to the response to a question about whether the respondent had ever had at least one drink of an alcohol beverage such as beer, wine, liquor, brandy, or a mixed drink or cocktail in their lifetime. A “drink” was defined as “can or bottle of beer, a glass of wine or a wine cooler, a shot of liquor, or a mixed drink with liquor in it.” Occasions when the respondent only had a sip or 2 from an alcoholic beverage were not included in the definition of ever drinking. Lifetime tobacco use was defined as ever trying a tobacco product as defined as part or all of a cigarette, cigar, chewing tobacco, snuff, or a pipe. Serious fights at school or work were used as a proxy for externalizing problems/aggression/conduct problems, classified as affirming the question, “During the past 12 months, how many times have you gotten into a serious fight at school or work?”
Effect modifier
Sex was examined as a potential effect modifier between each correlate and lifetime marijuana use and, among those who had not initiated more than 12 months prior to the survey, past year marijuana initiation. Examination of sex as an effect modifier of associations with MUD among lifetime users and among past year initiates, however, was precluded by low prevalence estimates of MUD and initiation in this age group.
Statistical analyses
Analyses were conducted using SUDAAN (RTI, 2012) to account for the complex survey design via the use of analytic weights that incorporated design-based weights based on selection probabilities (see Center for Behavioral Health Statistics and Quality [CBHSQ]39 for additional information about the creation of analytic weights to use when analyzing NSDUH data). All statistical tests were 2-tailed at P < .05 to identify potentially significant correlates, given the partially exploratory nature of our analyses.
Next, unadjusted associations between model covariates and each outcome were tested using the Shah Wald F test. Then, the following 4 sets of logistic models were run:
Lifetime marijuana use;
Past year marijuana initiation among those who had not used marijuana as of 1 year prior to survey participation (n = 82 854);
Marijuana use disorder among lifetime users (n = 5010);
Marijuana use disorder among past year marijuana initiates (2910) to indicate “rapid progression” from initiation to MUD.
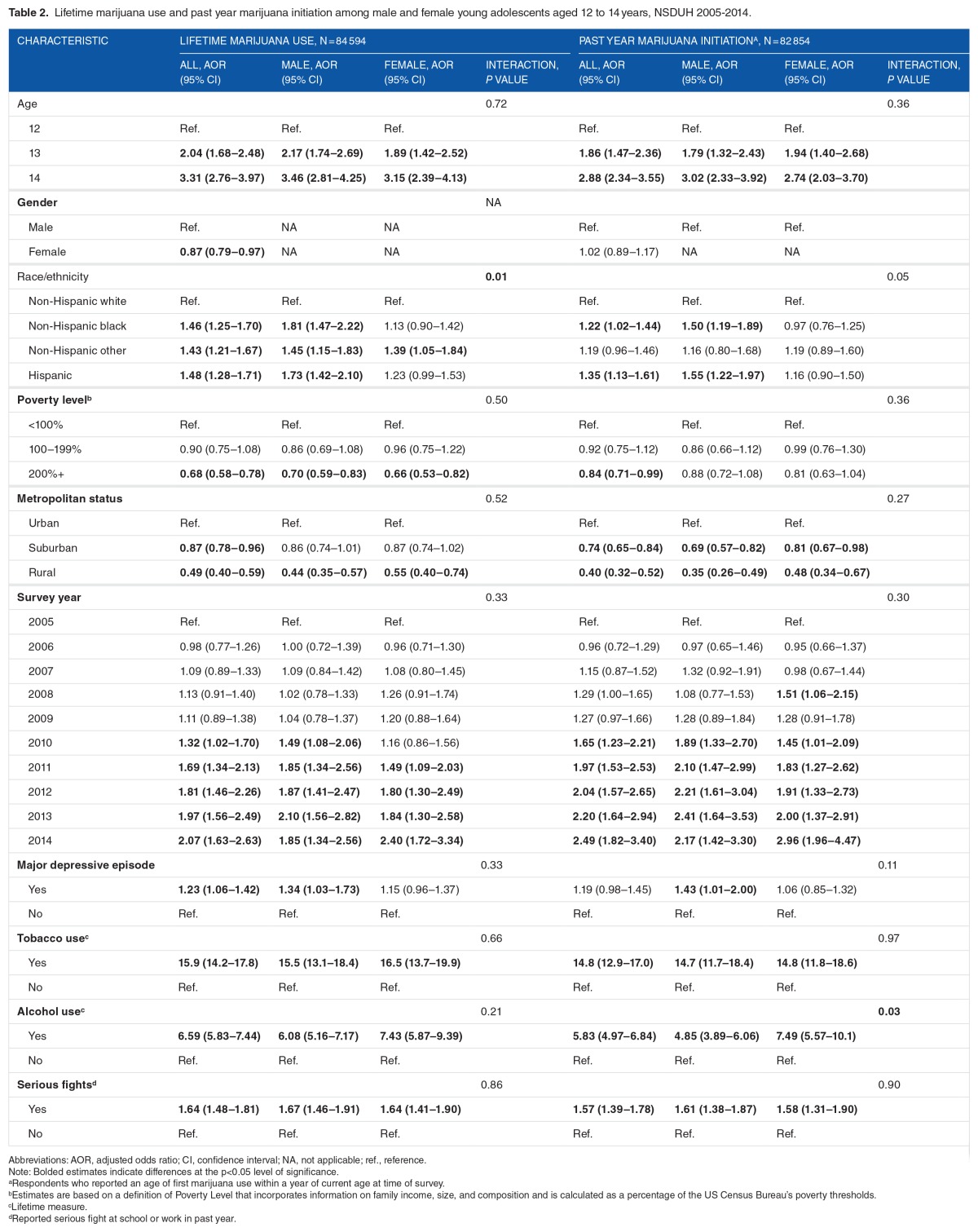
Lifetime marijuana use and past year marijuana initiation models (1 and 2, described above) first included all covariate main effects and all sex*covariate interactions. Table 2 presents Wald P values for each sex*covariate interaction. Next, models that included only main effects were run among the overall sample and among male and female respondents, separately. Adjusted odds ratio and 95% confidence intervals are reported for each covariate. Then, the 2 MUD models (3 and 4, described above) were run to include main effects only (no interactions) due to low sample sizes in some of the covariates by covariate cells.
Table 2.
Lifetime marijuana use and past year marijuana initiation among male and female young adolescents aged 12 to 14 years, NSDUH 2005–2014.
Although several covariates were correlated, no multicollinearity was detected on investigation of all covariates examined in each adjusted model tested (ie, variation inflation factor was less than 2 for each variable).
Results
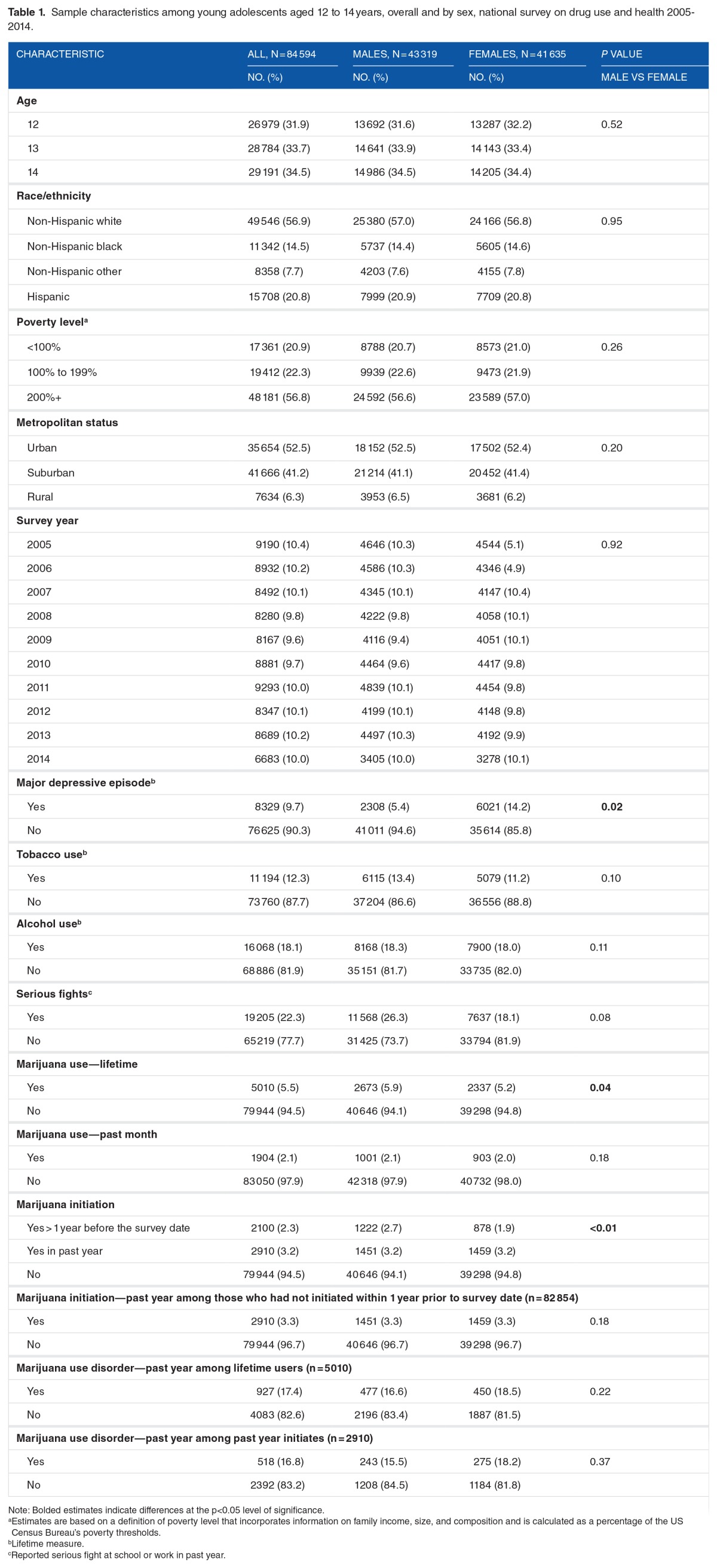
Sample characteristics are presented in Table 1 for the full sample of 12- to 14-year olds (n = 84 954) and also presented for men (n = 43 319) and women (n = 41 635), separately, with P values indicating significant sex differences. In the overall sample, 9.7% had past year MDE, 12.3% had used tobacco, 18.1% had used alcohol, and 22.3% had gotten into a serious fight at school or work in the past year. No sex differences in covariates were found except women were more likely than men to have past year MDE.
Table 1.
Sample characteristics among young adolescents aged 12 to 14 years, overall and by sex, national survey on drug use and health 2005–2014.
Marijuana initiation, past month use, and past year MUD
Among 12- to 14-year olds, 5.5% were lifetime marijuana users (2.3% had initiated more than 1 year prior to the survey and 3.2% had initiated in the past year), 2.1% were past month users, and 1.0% had past year MUD (Table 1). Among lifetime users, 17.4% met criteria for past year MUD. Among past year initiates, 16.8% met criteria for MUD within 1 year of initiating.
Men were more likely than women to be lifetime users of marijuana (5.9% vs 5.2%, P = .04) and more likely to have initiated more than 1 year prior to the survey (2.7% vs 1.9%), although there were no sex differences in past year marijuana initiation (3.2% for both men and women). There were no sex differences in past month marijuana use or past year MUD.
Lifetime marijuana use correlates
Bivariate analyses among all 12- to 14-year olds indicated significant associations between lifetime marijuana use and age, sex, race/ethnicity, poverty level, metropolitan status, lifetime MDE, lifetime alcohol use, lifetime tobacco use, and past year serious fights at school or work (Table 2). The association between survey year and lifetime marijuana use, however, was not significant.
Among all 12- to 14-year olds, adjusted models indicated significant main effects between past year marijuana initiation and age, sex, race/ethnicity, poverty level, metropolitan status, survey year, lifetime MDE, lifetime tobacco use, lifetime alcohol use, and serious fights in the past year. Of all, 13- and 14-year olds were more likely than 12-year olds, and men were more likely than women to be lifetime marijuana users. Non-Hispanic white adolescents were less likely than non-Hispanic black, non-Hispanic other, and Hispanic adolescents to be life-time marijuana users. Other correlates of lifetime marijuana use in adjusted models included poverty level of <100% of the FPL as compared with those at 200% or greater than the FPL, living in an urban area versus suburban or rural, participating in a more recent survey year, lifetime MDE, alcohol use, or tobacco use, and past year serious fights at school or work.
Among male and female young adolescents, significant correlates of past year marijuana initiation included age, poverty level, metropolitan status, survey year, lifetime tobacco use, lifetime alcohol use, and serious fights in the past year. The association between race/ethnicity and lifetime marijuana use and between lifetime MDE and marijuana use, however, differed by sex (P < .0001). Although non-Hispanic black, non-Hispanic other, and Hispanic male adolescents each had higher rates of lifetime marijuana use than non-Hispanic white men, only non-Hispanic other women had higher rates than non-Hispanic white women in adjusted models. There were no significant differences in lifetime marijuana use between non-Hispanic white and either non-His-panic black or Hispanic women. Men with lifetime MDE had higher odds of being a lifetime marijuana user than men without, but the MDE and marijuana use association among women did not reach significance.
Past year marijuana initiation correlates
Bivariate analyses in the determined significant associations between marijuana initiation and age, race/ethnicity, poverty level, lifetime MDE, lifetime alcohol use, lifetime tobacco use, and past year serious fights at school or work. Survey year and metropolitan status did not significantly correlate with past year marijuana initiation.
In the total sample, adjusted models indicated significant main effects between past year marijuana initiation and age, race/ethnicity, poverty level, metropolitan status, survey year, tobacco use, alcohol use, and serious fights in the past year, but not sex or MDE. Of all, 13- and 14-year olds were more likely to have had past year marijuana initiation as compared with 12-year olds, and non-Hispanic black and Hispanic adolescents were more likely to start using marijuana in the past year as compared with non-Hispanic white adolescents. Young adolescents with family incomes at 200% or higher of the FPL were less likely than those with family incomes less than 100% of the FPL to initiate marijuana. Young adolescents living in suburban or rural areas were less likely than those living in urban areas to initiate marijuana use in the past year. In addition, those participating in more recent surveys (2010–2014) were more likely to initiate marijuana use than those who participated in the 2005 survey. Those with lifetime tobacco use or serious fights in school or at work in the past year were more likely to initiate marijuana use than young adolescents without each of these characteristics, as well.
Among men and women, significant correlates of past year marijuana initiation included age, metropolitan status, survey year, lifetime tobacco use, lifetime alcohol use, and serious fights in the past year. Poverty was not significant in either of the sex-stratified models. Sex significantly moderated the effect between race/ethnicity and past year marijuana initiation (F = 2.67, df = 3, P < .001) and between alcohol use and past year marijuana initiation (F = 4.57, df = 1, P < .001). Both race/ethnicity and lifetime MDE were significant correlates of past year marijuana initiation among men, but these associations did not reach significance among women. Among men, non-Hispanic black and Hispanic young adolescents were more likely than non-Hispanic white men to initiate marijuana in the past year, and men with lifetime MDE were more likely than those without MDE. The significant interaction between sex and lifetime alcohol use resulted from a stronger association between alcohol and past year marijuana initiation among women than among men.
Past year MUD among lifetime marijuana users
Bivariate analyses in the overall sample of lifetime marijuana users determined significant associations between MUD and age, race/ethnicity, lifetime MDE, lifetime alcohol use, lifetime tobacco use, and past year serious fights at school or work. The associations between MUD and sex, poverty level, metropolitan status, and survey year did not reach significance in bivariate analyses.
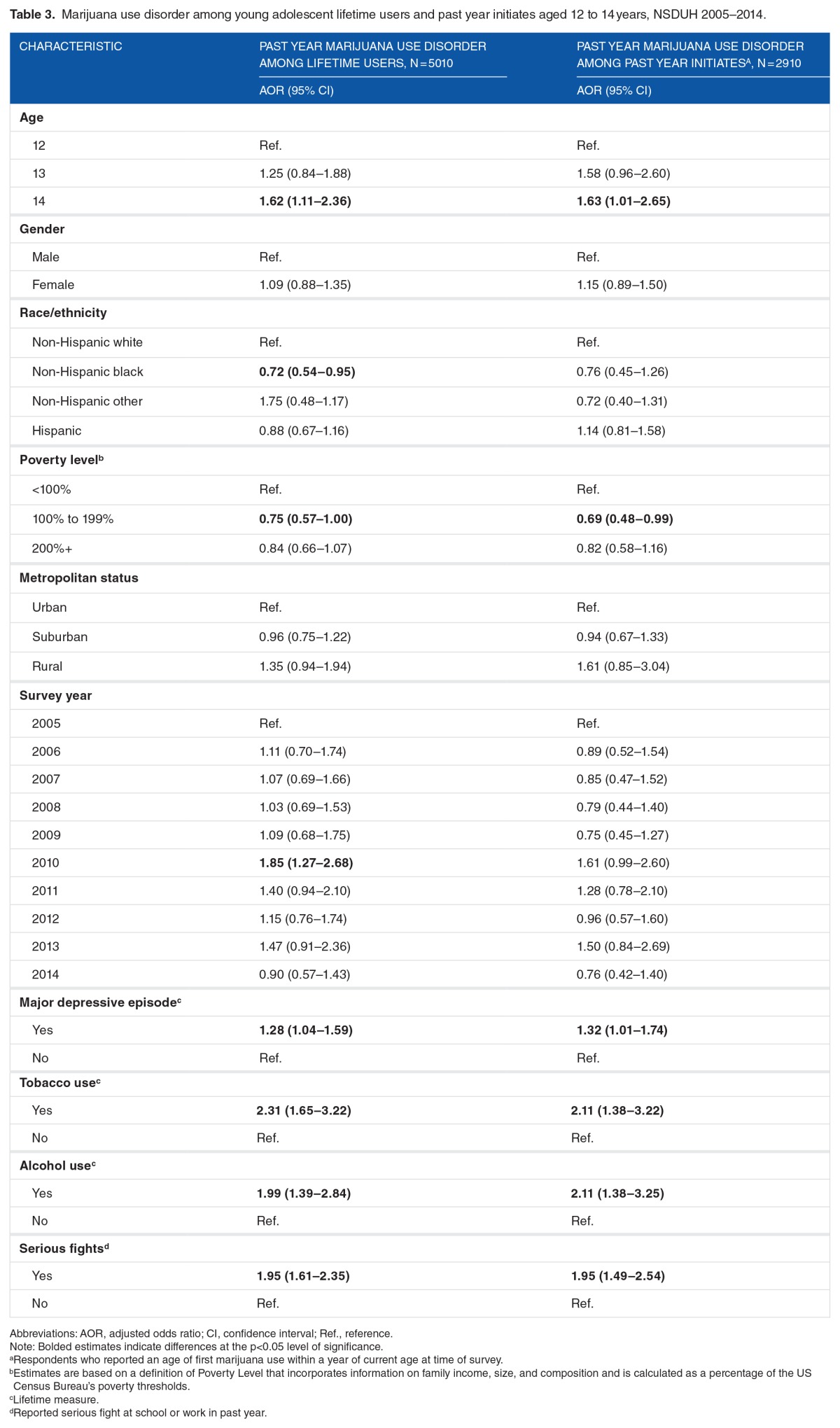
Among lifetime marijuana users, adjusted models indicated significant associations between MUD and age, race/ethnicity, poverty level, lifetime MDE, lifetime tobacco use, lifetime alcohol use, and serious fights in the past year, but not sex or metropolitan status (Table 3). The prevalence of MUD did not significantly differ between 12- and 13-year olds; however, 14-year olds lifetime marijuana users had higher odds of having past year MUD than their 12-year-old counterparts. The odds of non-Hispanic black adolescent lifetime marijuana users having past year MUD were lower than the odds among their non-Hispanic white counterparts. Young adolescent life-time marijuana users with family incomes of less than 100% of the FPL had higher odds of having a past year MUD than those with family incomes of 100% to 199% of the FPL, but these differences did not extend to youth at greater than 200% of the FPL. Among young adolescent lifetime marijuana users, odds of having a past year MUD did not differ by survey year in adjusted models (except between 2010 and 2015).
Table 3.
Marijuana use disorder among young adolescent lifetime users and past year initiates aged 12 to 14 years, NSDUH 2005–2014.
Past year MUD among past year initiates (“rapid progression”)
Bivariate analyses conducted among past year marijuana initiates revealed significant bivariate associations between MUD and lifetime MDE, lifetime alcohol use, lifetime tobacco use, and past year serious fights at school or work among past year initiates. Bivariate analyses revealed no significant associations between MUD and survey year or any of the demographic or socioeconomic variables tested (age, sex, race/ethnicity, poverty level, and metropolitan status).
Among past year marijuana initiates, adjusted models indicated significant associations between MUD and age, poverty level, lifetime MDE, lifetime tobacco use, lifetime alcohol use, and serious fights in the past year, but not sex, race/ethnicity, or metropolitan status (Table 3). The prevalence of MUD did not significantly differ between 12- and 13-year olds; however, 14-year-old past year marijuana initiates had higher odds of having past year MUD than 12-year olds. Young adolescents at 100% to 199% poverty level with past year marijuana initiation had lower odds than those at less than 100% of the poverty level, but these differences did not extend to youth at greater than 200% of the poverty level. There were no significant differences in MUD across survey years. The odds of MUD were higher for those with versus without lifetime MDE. The odds of MUD were about twice as high among those with lifetime tobacco use, lifetime alcohol use, or serious fights at school or work in the past year as compared with young adolescents with past year initiation without each of these characteristics.
Discussion
Our findings indicate that about 1 in 20 young adolescents aged 12 to 14 years had ever used marijuana. The rapid increase in lifetime marijuana use prevalence among 12-, 13-, and 14-year olds (1.4%, 4.6%, and 10.3%, respectively) and past year marijuana initiation (0.9%, 2.8%, and 6.1% among 12-, 13-, and 14-year olds who had not yet initiated, respectively) provides evidence that these ages represent a critical window for intervention efforts. By comparison, analyses of 2015 MTF data found that 15.5% of eighth graders (typically aged 13–14 years) were lifetime marijuana users.6 Differences in survey methodology such as place of administration (eg, MTF is administered at school versus the NSDUH, which is house-hold administered) and varied questionnaire structure and wording of assessment questions may explain the higher estimates found in the MTF study.38
Other identified correlates of lifetime marijuana use and marijuana initiation in our study, such as living in an urban metropolitan area, having a family income below the FPL, tobacco use, alcohol use, and having serious fights at school, are similar to those identified previously28,43,44 and suggest potential targets for preventive interventions. In addition, the prevalence of lifetime marijuana use and past year initiation appeared to be higher in more recent survey years when compared with the 2005 survey in adjusted (but not unadjusted) analyses. Prior studies have found stable or decreasing trends in lifetime marijuana use among all adolescents in analyses that were not adjusted for covariates.4,6 The increase found in this study in adjusted analyses may be explained by changing norms about marijuana use. Some shift in adolescent attitudes about marijuana use may be related to the increasing number of states legalizing marijuana use among adults.45 The proportion of adolescents who reported perceiving the use of marijuana once or twice a week to be of “great risk” has decreased in recent years, as well.46 Additional research on the effects of risk perception on marijuana use is needed.
Although our study confirmed one of the findings of the NCS-A study3 that men had higher lifetime prevalence estimates than women, past year initiation in our study did not significantly differ by sex, indicating that perhaps more men than women tend to experiment prior to age 12. This finding is consistent with prior research that has found earlier ages of marijuana initiation among men than women.47 Sex also moderated the associations between race/ethnicity and marijuana use and initiation, with non-Hispanic black and Hispanic men having higher lifetime prevalence and rates of initiation than non-Hispanic white men and no such differences found among women. Although the NCS-A study found that black 13- to 14-year olds had lower marijuana use prevalence estimates than women,3 a study of secondary school students from Connecticut found increased prevalence of lifetime marijuana use among black and Hispanic men but no such race/ethnicity differences among women, similar to our findings. The most recent YRBS found significantly increased prevalence of lifetime marijuana use among black and Hispanic men as compared with white men, as well, but also found these race/ethnicity patterns among women.25 Identifying racial/ethnicity differences are important because prior research has shown that minority youth are less likely than non-Hispanic white youth to receive substance use treatment.48
This study identified several mental health–related correlates of lifetime use and past year initiation, including tobacco use and serious fights at school in the past year. Although lifetime MDE was associated with both lifetime marijuana use and past year initiation among men in this study, there were no significant MDE-marijuana associations among women. This finding can be interpreted in light of research among Dutch secondary school youth that not only did not find a significant association between depression and marijuana use but also did not find sex differences for this association.49 Moreover, although alcohol use and marijuana use, and initiation were significantly correlated among young adolescents of both sex in this study, women demonstrated a stronger association than men. To our knowledge, this is a new finding and requires replication. It is possible that depressed women are more likely than men to only use marijuana after already having initiated alcohol use, whereas depressed men might choose one substance or the other to cope with their depression, and so, including alcohol use in the model may decrease the strength of the depression-marijuana use association.
With respect to prevalence and correlates of MUD among lifetime marijuana users, nearly 1 in 5 young adolescents with lifetime marijuana use met criteria for MUD in the past year. Correlates included older age (14 vs 12), non-Hispanic white race/ethnicity (as compared with non-Hispanic black), having a family income of less than 100% of the FPL level (as compared with 100%-199% of the FPL), lifetime MDE, tobacco use, alcohol use, and having had at least one serious fight at school or work in the past year. These findings are counter to those found in the Canadian adolescent cohort study that did not find that psychiatric morbidity predicted marijuana dependence, although analyses from that study were not conditioned on use.50 The race/ethnicity findings are consistent with prior NSDUH studies that have determine lower prevalence of substance use disorders among non-Hispanic black versus white adolescent substance users.51 Further exploration of these associations is needed to determine potential reasons for differences in estimates.
In addition, about 1 in 6 with past year marijuana initiation had already progressed to meeting MUD criteria (ie, had “rapid progression” to meeting MUD criteria). Estimates of the transition to MUD found in this study were much higher than those found in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study of adults, which determined that 2% of users reported development of marijuana dependence (abuse not reported) within a year of initiation.35 Sex and MUD were not significantly associated among past year initiates in this study. These findings contrast those of Wagner and Anthony,52 which determined that men have a higher risk of marijuana dependence within a few years of initiation, but in part supported those of Ridenour et al,53 which concluded that the faster progression from initiation to dependence among women did not significantly differ from that found among men. Lifetime MDE, tobacco use, alcohol use, and having serious fights at school or at home were each significantly associated with rapid progression to meet MUD criteria. These findings support prior research that has found that the strongest correlate of developing dependence after initiation is having a concomitant mental health problem (including use and abuse of other substances),54 potentially indicating a shared liability for disorders.17,55,56
Our findings complement and extend those of Swendsen and colleagues that used 2001–2004 NCS-A data to investigate prevalence and correlates of lifetime marijuana use that included analyses subset to 1598 13- to 14-year olds. Our study also included 12-year olds, which is important because the NCS-A findings showed increases in the cumulative prevalence of reported opportunity to use drugs and first drug use at ages younger than 12 years. Including 12-year olds in analyses may also improve the ability to identify potential risk factors for early stages of marijuana use among those at highest risk for developing MUD. Our substantial sample size (n = 84 954) permitted analyses to estimate the incidence and correlates of marijuana initiation and prevalence and correlates of past year MUD, among those who had lifetime use and among those with past year initiation, separately, to identify factors associated with rapid progression from initiation to abuse and dependence in this age group.
Findings suggest the need for additional studies of adolescent marijuana initiation and progression to misuse and clinically significant disorders. A more nuanced understanding of the particular symptoms of MUDs that young adolescents who meet diagnostic criteria soon after they initiate marijuana is needed, as is a better understanding of whether the symptom profiles of young adolescents with rapid progression to meet criteria for MUD differ from those who develop MUD later on in adolescence and into young adulthood. This study focused on marijuana abuse and dependence together (MUDs) rather than separate constructs in part because Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) criteria no longer distinguishes between abuse and dependence. In our sample, about half of young adolescent lifetime marijuana users with MUD met abuse criteria (50.9%) and the others (49.1%) met dependence criteria. Examining abuse and dependence together rather than as separate constructs is warranted because some abuse criteria may be more predictive of adverse outcomes than dependence criteria,57,58 and abuse and dependence criteria do not represent different levels of severity among adolescents.59
Certain strengths and limitations of our study should be noted. First, NSDUH data are cross-sectional, so the temporarily of associations between correlates and marijuana indicators could not be determined. Nevertheless, using age at first marijuana use and various recall periods of use enabled calculation of past year marijuana initiation. Analyses specifically of past year marijuana initiates allowed for testing the progression to use meeting criteria for MUD within the first 12 months following initiation. In addition, the likelihood for recall bias in young adolescents, who probably only recently initiated marijuana use, is minimal (eg, compared with adults providing retrospective ages of onset).60 Another potential limitation comes from average annual estimates being derived from combined 2005–2014 data, which gave some of the study analyses adequate power but may produce prevalence estimates that may not represent those found in the most recent years. Finally, the influence of conducting interviews in households with other people at home who might have been able to hear responses may have influenced adolescent reporting on marijuana use. In fact, the prevalence of lifetime marijuana use among young adolescents in the NSDUH who had their interviews con-ducted in the least private settings was lower than their counterparts who had interviews conducted in private settings. Because this likely lead to an underreporting of marijuana use and misuse, the actual rates of initiation, use, and MUD might be even higher than reported.38
A key strength of our study is having the power to conduct analyses of the large sample of adolescents aged 12 to 14 years, which allowed us to examine correlates of lifetime marijuana use, recent initiation, and develop of MUD among both groups (lifetime users and recent initiates who had rapid progression to MUD) in models adjusted for various important covariates. The investigation of correlates of the progression from initiation to use patterns and associated behaviors significant enough to meet MUD criteria in this study is critical to identifying potential prevention targets. The large sample size also allowed for the investigation of various marijuana indicators with each increased year of age (ie, among 12-, 13-, and 14-year olds, separately). This is the first time findings from a study of estimates and correlates of marijuana use among young adolescents aged 12 to 14 years from a US nationally representative, household sample have been reported.
Our findings have several implications for future research and clinical care. Differences in initiation, use, and progression to MUD found across different demographic, socioeconomic, and mental health characteristics suggest at-risk subpopulations identifiable to clinicians, parents, teachers, and other adults involved with adolescents that may help better target those in need of intervention and referral services. Future studies are needed to replicate our findings and to determine the temporal order of depression, tobacco use, alcohol use, conduct problems, and marijuana use among young adolescents. Further exploration of the sex by race/ethnicity interactions found in our study is needed. Perhaps findings from a Canadian study that indicated that adolescents may self-select into a predominantly alcohol-using or a predominantly marijuana-using life-style may help these future explorations.50 A recent study identified race/ethnicity differences in the order of first use of these 2 substances (alcohol first versus marijuana first), with a higher proportion of non-Hispanic black than white young adults reporting marijuana use prior to alcohol use. Additional investigations are needed to better identify race/ethnicity-specific needs for prevention and intervention efforts.61 Finally, future studies focused on how environmental, social, and con-textual factors such as peer and parental attitudes about drug use, perceived parental support and supervision, and exposure to violence determined as correlates of marijuana use and misuse among adolescents in non-nationally representative samples62,63 may influence marijuana initiation, use, and progression to MUD among young adolescents from a nationally representative sample are critically needed. Because preliminary studies of the effects of the state-specific legalization of adult marijuana use have on initiation and use among adolescents living in those states have been mixed,64 additional study will be needed to further guide prevention and treatment efforts with respect to changing attitudes toward marijuana use.45
The American Academy of Pediatrics (AAP) currently recommends that primary care providers educate and screen for substance use among adolescents during routine clinical care by incorporating the Screening for Substance Use, Brief Intervention, and/or Referral to Treatment (SBIRT) guidelines that were developed by SAMHSA.65 An algorithm-based approach guides clinicians in managing each unique patient. A recent AAP report called for the health care sector, including primary care providers and the medical home, to work together to increase capacity to prevent, screen, and assess adolescents for substance use and abuse and to intervene or refer those in need across different clinical settings in which adolescents may receive health care.66 Findings from this study can be used to better inform these public health efforts to improve the prevention, identification, and referral of young marijuana initiates and users to lessen the incidence and associated negative sequelae of marijuana use and MUD.
Footnotes
PEER REVIEW: Six peer reviewers contributed to the peer review report. Reviewers’ reports totaled 2593 words, excluding any confidential comments to the academic editor.
FUNDING: The author(s) received no financial support for the research, authorship, and/or publication of this article.
DECLARATION OF CONFLICTING INTERESTS: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions
VLF-H conceived and designed the experiments, analyzed the data, wrote the first draft of the manuscript, and contributed to the writing of the manuscript. VLF-H, CG, and KRB agree with manuscript results and conclusions; jointly developed the structure and arguments for the paper; and made critical revisions and approved final version. All authors reviewed and approved the final manuscript.
Disclosures and Ethics
As a requirement of publication, each author has provided to the publisher signed confirmation of compliance with legal and ethical obligations including but not limited to the following: authorship and contributorship, conflicts of interest, privacy and confidentiality, and (where applicable) protection of human and animal research subjects. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material.
REFERENCES
- 1.Levy S, Williams J. Adolescent substance use: the role of the medical home. Adolesc Med State Art Rev. 2014;25:1–14. [PubMed] [Google Scholar]
- 2.Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- 3.Swendsen J, Burstein M, Case B, et al. Use and abuse of alcohol and illicit drugs in US adolescents: results of the National Comorbidity Survey-Adolescent Supplement. Arch Gen Psychiatry. 2012;69:390–398. doi: 10.1001/archgenpsychiatry.2011.1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center for Behavioral Health Statistics and Quality (CBHSQ) Results From the 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: CBHSQ; 2016. [Google Scholar]
- 5.Mutter R, Ali M, Strashny A. Profile of Adolescent Discharges from Substance Abuse Treatment. The CBHSQ Report: April 1, 2015. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; Rockville, MD: [PubMed] [Google Scholar]
- 6.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2015: Overview, Key Findings on Adolescent Drug Use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- 7.Center for Behavioral Health Statistics and Quality (CBHSQ) 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: CBHSQ; 2016. [Google Scholar]
- 8.Fergusson DM, Horwood LJ, Beautrais AL. Cannabis and educational achievement. Addiction (Abingdon, England) 2003;98:1681–1692. doi: 10.1111/j.1360-0443.2003.00573.x. [DOI] [PubMed] [Google Scholar]
- 9.Bechtold J, Hipwell A, Lewis DA, Loeber R, Pardini D. Concurrent and sustained cumulative effects of adolescent marijuana use on subclinical psychotic symptoms. Am J Psychiat. 2016;173:781–789. doi: 10.1176/appi.ajp.2016.15070878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall WD. Cannabis use and the mental health of young people. Aust N Z J Psychiatry. 2006;40:105–113. doi: 10.1080/j.1440-1614.2006.01756.x. [DOI] [PubMed] [Google Scholar]
- 11.Dorard G, Berthoz S, Phan O, Corcos M, Bungener C. Affect dysregulation in cannabis abusers: a study in adolescents and young adults. Eur Child Adolesc Psychiatry. 2008;17:274–282. doi: 10.1007/s00787-007-0663-7. [DOI] [PubMed] [Google Scholar]
- 12.Medina KL, Nagel BJ, Park A, McQueeny T, Tapert SF. Depressive symptoms in adolescents: associations with white matter volume and marijuana use. J Child Psychol Psychiatry. 2007;48:592–600. doi: 10.1111/j.1469-7610.2007.01728.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Forti M, Morrison PD, Butt A, Murray RM. Cannabis use and psychiatric and cogitive disorders: the chicken or the egg? Curr Opin Psychiatry. 2007;20:228–234. doi: 10.1097/YCO.0b013e3280fa838e. [DOI] [PubMed] [Google Scholar]
- 14.Wong SS, Zhou B, Goebert D, Hishinuma ES. The risk of adolescent suicide across patterns of drug use: a nationally representative study of high school students in the United States from 1999 to 2009. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1611–1620. doi: 10.1007/s00127-013-0721-z. [DOI] [PubMed] [Google Scholar]
- 15.Patton GC, Coffey C, Lynskey MT, et al. Trajectories of adolescent alcohol and cannabis use into young adulthood. Addiction (Abingdon, England) 2007;102:607–615. doi: 10.1111/j.1360-0443.2006.01728.x. [DOI] [PubMed] [Google Scholar]
- 16.Grant I, Gonzalez R, Carey CL, Natarajan L, Wolfson T. Non-acute (residual) neurocognitive effects of cannabis use: a meta-analytic study. J Int Neuropsychol Soc. 2003;9:679–689. doi: 10.1017/S1355617703950016. [DOI] [PubMed] [Google Scholar]
- 17.Wittchen H-U, Fröhlich C, Behrendt S, et al. Cannabis use and cannabis use disorders and their relationship to mental disorders: a 10-year prospective-longitudinal community study in adolescents. Drug Alcohol Depend. 2007;88:S60–S70. doi: 10.1016/j.drugalcdep.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 18.Fergusson DM, Horwood LJ, Lynskey MT, Madden PA. Early reactions to cannabis predict later dependence. Arch Gen Psychiatry. 2003;60:1033–1039. doi: 10.1001/archpsyc.60.10.1033. [DOI] [PubMed] [Google Scholar]
- 19.Bray JW, Zarkin GA, Ringwalt C, Qi J. The relationship between marijuana initiation and dropping out of high school. Health Econ. 2000;9:9–18. doi: 10.1002/(sici)1099-1050(200001)9:1<9::aid-hec471>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 20.Ellickson PL, Tucker JS, Klein DJ, Saner H. Antecedents and outcomes of marijuana use initiation during adolescence. Prev Med. 2004;39:976–984. doi: 10.1016/j.ypmed.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Brook JS, Balka EB, Whiteman M. The risks for late adolescence of early adolescent marijuana use. Am J Public Health. 1999;89:1549–1554. doi: 10.2105/ajph.89.10.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gogtay N, Giedd JN, Lusk L, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A. 2004;101:8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schneider M. Puberty as a highly vulnerable developmental period for the consequences of cannabis exposure. Addict Biol. 2008;13:253–263. doi: 10.1111/j.1369-1600.2008.00110.x. [DOI] [PubMed] [Google Scholar]
- 24.Moffitt TE, Caspi A, Taylor A, et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40:899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kann L. Youth risk behavior surveillance—United States, 2015. MMWR Surveill Summ. 2016;65:1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 26.Kalaydjian A, Swendsen J, Chiu W-T, et al. Sociodemographic predictors of transitions across stages of alcohol use, disorders, and remission in the National Comorbidity Survey Replication. Compr Psychiatry. 2009;50:299–306. doi: 10.1016/j.comppsych.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Swendsen J, Anthony JC, Conway KP, et al. Improving targets for the prevention of drug use disorders: sociodemographic predictors of transitions across drug use stages in the national comorbidity survey replication. Prev Med. 2008;47:629–634. doi: 10.1016/j.ypmed.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Farhat T, Simons-Morton B, Luk JW. Psychosocial correlates of adolescent marijuana use: variations by status of marijuana use. Addict Behav. 2011;36:404–407. doi: 10.1016/j.addbeh.2010.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tu AW, Ratner PA, Johnson JL. Gender differences in the correlates of adolescents’ cannabis use. Subst Use Misuse. 2008;43:1438–1463. doi: 10.1080/10826080802238140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guxens M, Nebot M, Ariza C. Age and sex differences in factors associated with the onset of cannabis use: a cohort study. Drug Alcohol Depend. 2007;88:234–243. doi: 10.1016/j.drugalcdep.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Schepis TS, Desai RA, Cavallo DA, et al. Gender differences in adolescent marijuana use and associated psychosocial characteristics. J Addict Med. 2011;5:65. doi: 10.1097/ADM.0b013e3181d8dc62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maxwell SE, Lau MY, Howard GS. Is psychology suffering from a replication crisis? What does “failure to replicate” really mean? Am Psychol. 2015;70:487. doi: 10.1037/a0039400. [DOI] [PubMed] [Google Scholar]
- 33.Open Science Collaboration Estimating the reproducibility of psychological science. Science. 2015;349:aac4716. doi: 10.1126/science.aac4716. [DOI] [PubMed] [Google Scholar]
- 34.Peng RD, Dominici F, Zeger SL. Reproducible epidemiologic research. Am J Epidemiol. 2006;163:783–789. doi: 10.1093/aje/kwj093. [DOI] [PubMed] [Google Scholar]
- 35.Lopez-Quintero C, de los Cobos JP, Hasin DS, et al. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug Alcohol Depend. 2011;115:120–130. doi: 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schweinsburg AD, Nagel BJ, Schweinsburg BC, Park A, Theilmann RJ, Tapert SF. Abstinent adolescent marijuana users show altered fMRI response during spatial working memory. Psychiatry Res. 2008;163:40–51. doi: 10.1016/j.pscychresns.2007.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Center for Behavioral Health Statistics and Quality (CBHSQ) 2012 National Survey on Drug Use and Health: Methodological Resource Book. Rockville, MD: CBHSQ; 2014. [Google Scholar]
- 38.Substance Abuse and Mental Health Services Administration . Comparing and Evaluating Youth Substance Use Estimates from the National Survey on Drug Use and Health and Other Surveys. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. p. SMA 12-4727. [PubMed] [Google Scholar]
- 39.Center for Behavioral Health Statistics and Quality (CBHSQ) 2014 National Survey on Drug Use and Health: Methodological Summary and Definitions. Rockville, MD: CBHSQ; 2015. [Google Scholar]
- 40.Substance Abuse and Mental Health Services Administration . Results From the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. p. SMA 14-4863. [Google Scholar]
- 41.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Arlington, VA: American Psychiatric Publishing; 1994. [Google Scholar]
- 42.Gfroerer J. Influence of privacy on self-reported drug use by youths. NIDA Res Mg. 1985;57:22–30. [PubMed] [Google Scholar]
- 43.Heron J, Barker ED, Joinson C, et al. Childhood conduct disorder trajectories, prior risk factors and cannabis use at age 16: birth cohort study. Addiction (Abingdon, England) 2013;108:2129–2138. doi: 10.1111/add.12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Macleod J, Oakes R, Copello A, et al. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet. 2004;363:1579–1588. doi: 10.1016/S0140-6736(04)16200-4. [DOI] [PubMed] [Google Scholar]
- 45.Hopfer C. Implications of marijuana legalization for adolescent substance use. Subst Abus. 2014;35:331–335. doi: 10.1080/08897077.2014.943386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Substance Abuse and Mental Health Services Administration CfBHSaQ . The NSDUH Report: Trends in Adolescent Substance Use and Perception of Risk From Substance Use. Rockville, MD: Substance Abuse and Mental Health Services Administration CfBHSaQ; 2012. [Google Scholar]
- 47.Kandel DB, Chen K. Types of marijuana users by longitudinal course. J Stud Alcohol. 2000;61:367–378. doi: 10.15288/jsa.2000.61.367. [DOI] [PubMed] [Google Scholar]
- 48.Cummings JR, Wen H, Druss BG. Racial/ethnic differences in treatment for substance use disorders among U.S. adolescents. J Am Acad Child Adolesc Psychiatry. 2011;50:1265–1274. doi: 10.1016/j.jaac.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Monshouwer K, Van Dorsselaer S, Verdurmen J, Ter Bogt T, De Graaf R, Vollebergh W. Cannabis use and mental health in secondary school children. Br J Psychiatry. 2006;188:148–153. doi: 10.1192/bjp.188.2.148. [DOI] [PubMed] [Google Scholar]
- 50.Coffey C, Carlin JB, Lynskey M, Li N, Patton GC. Adolescent precursors of cannabis dependence: findings from the Victorian Adolescent Health Cohort Study. Br J Psychiatry. 2003;182:330–336. doi: 10.1192/bjp.182.4.330. [DOI] [PubMed] [Google Scholar]
- 51.Wu L-T, Woody GE, Yang C, Pan J-J, Blazer DG. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Arch Gen Psychiatry. 2011;68:1176–1185. doi: 10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wagner FA, Anthony JC. Male-female differences in the risk of progression from first use to dependence upon cannabis, cocaine, and alcohol. Drug Alcohol Depend. 2007;86:191–198. doi: 10.1016/j.drugalcdep.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 53.Ridenour TA, Lanza ST, Donny EC, Clark DB. Different lengths of times for progressions in adolescent substance involvement. Addict Behav. 2006;31:962–983. doi: 10.1016/j.addbeh.2006.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lev-Ran S, Imtiaz S, Rehm J, Le Foll B. Exploring the association between life-time prevalence of mental illness and transition from substance use to substance use disorders: results from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) Am J Addict. 2013;22:93–98. doi: 10.1111/j.1521-0391.2013.00304.x. [DOI] [PubMed] [Google Scholar]
- 55.Behrendt S, Wittchen H-U, Höfler M, Lieb R, Beesdo K. Transitions from first substance use to substance use disorders in adolescence: is early onset associated with a rapid escalation? Drug Alcohol Depend. 2009;99:68–78. doi: 10.1016/j.drugalcdep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 56.Degenhardt L, Chiu W, Conway K, et al. Does the “gateway” matter? Associations between the order of drug use initiation and the development of drug dependence in the National Comorbidity Study Replication. Psychol Med. 2009;39:157–167. doi: 10.1017/S0033291708003425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- 58.Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classifications of alcohol use disorders. Drug Alcohol Depend. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hartman CA, Gelhorn H, Crowley TJ, et al. Item response theory analysis of DSM-IV cannabis abuse and dependence criteria in adolescents. J Am Acad Child Adolesc Psychiatry. 2008;47:165–173. doi: 10.1097/chi.0b013e31815cd9f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health. 2003;33:436–457. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 61.Kennedy SM, Patel RP, Cheh P, Hsia J, Rolle IV. Tobacco and marijuana initiation among African American and white young adults. Nicotine Tob Res. 2016;18:S57–S64. doi: 10.1093/ntr/ntv194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kosterman R, Hawkins JD, Guo J, Catalano RF, Abbott RD. The dynamics of alcohol and marijuana initiation: patterns and predictors of first use in adolescence. Am J Public Health. 2000;90:360–366. doi: 10.2105/ajph.90.3.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lynskey MT, Heath AC, Bucholz KK, et al. Escalation of drug use in early-onset cannabis users vs co-twin controls. JAMA. 2003;289:427–433. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- 64.Wall MM, Poh E, Cerdá M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21:714–716. doi: 10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128:e1330–e1340. doi: 10.1542/peds.2011-1754. [DOI] [PubMed] [Google Scholar]
- 66.Levy SJ, Williams JF, Committee on Substance Use and Prevention Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016;138:e20161211. doi: 10.1542/peds.2016-1211. [DOI] [PubMed] [Google Scholar]