Abstract
[Purpose] To examine the efficacy of Ai Chi in relieving the pain and stiffness of knee osteoarthritis and improving, physical functioning, proprioception and quality of life. [Subjects and Methods] Twenty-five persons with knee osteoarthritis completed 5 weeks Ai Chi practice (60 minutes per session, twice per week, 10 sessions in total). Knee pain and stiffness were measured before and after the intervention program. [Results] Significant improvements in pain, self-perceived physical functioning and self-perceived stiffness were observed after the Ai-Chi intervention. On average, no significant change in knee range of motion, 6-minute walk test distances or proprioception was observed. [Conclusion] A five-week Ai Chi intervention can improve the pain and stiffness of knee osteoarthritis and self-perceived physical functions and quality of life improvement. Ai Chi may be another treatment choice for people with knee OA to practice in the community.
Keywords: Aquatic exercise, Knee osteoarthritis, Tai Chi
INTRODUCTION
Osteoarthritis (OA) of the knee is a common degenerative disease among the elderly, causing pain and functional disability. The prevalence of knee OA in Hong Kong among those aged over 65 is expected to increase from 12% in 2005 to 32.5% in 20501). Medication, physiotherapy, exercise and dietary advice may help control the knee OA1). In severe cases, joint replacement surgery would be considered to alleviate the symptoms. The average cost of medical services to the government is estimated to be about HK $10,120 to $195,630 per patient per year2). Knee OA is a significant problem that is only going to grow. This brings a tremendous socioeconomic burden to Hong Kong society, and effective treatments are urgently needed.
Individuals with knee OA usually complain of pain and joint stiffness, which might affect the physical functions of patients such as walking endurance and ability in coping with the activities of daily life. Evidence has shown that knee OA often involves poor knee proprioception and lower quality of life due to reduced physical activity3, 4). Evidence supports the efficacy of exercise, individually tailored physiotherapy and group (standardized) treatment. This also includes tai chi5). However, not all individuals with knee OA can tolerate exercise involving full weight bearing.
Aquatic exercise programs have been proposed to address the needs of such individuals, and there is evidence that they are effective. Aquatic therapy may alleviate OA symptoms and improve physical functioning. Water’s buoyancy, hydrostatic pressure and warmth help relieve pain and relax muscles6). Aquatic therapy has been shown to benefit knee OA patients in terms of pain, stiffness, physical functioning, balance and quality of life4, 7, 8). However, the aquatic exercise programs developed and tested to date require significant therapist involvement and supervision, increasing their cost, and making them less practical for addressing the increasing demand for such programs.
Ai Chi is a novel aquatic therapy which combines the tai chi concepts with conventional aquatic therapy techniques9, 12). It involves a total of 19 standardized movement patterns emphasizing the coordination of body movements with breathing patterns. No published study has yet investigated the effect of Ai Chi on knee OA. Ai Chi is safe, standardized, requires no equipment and thus allows self-regulated practice. It should be promoted if it can be shown to bring beneficial outcomes to knee OA patients. Ai Chi potentially address the need for an aquatic exercise intervention that can be taught in a group setting and then allow individuals to continue treatment on their own if they choose.
This study was designed to investigate the effect of Ai Chi on pain, stiffness, knee proprioception and physical functioning among those with OA and on their quality of life.
SUBJECTS AND METHODS
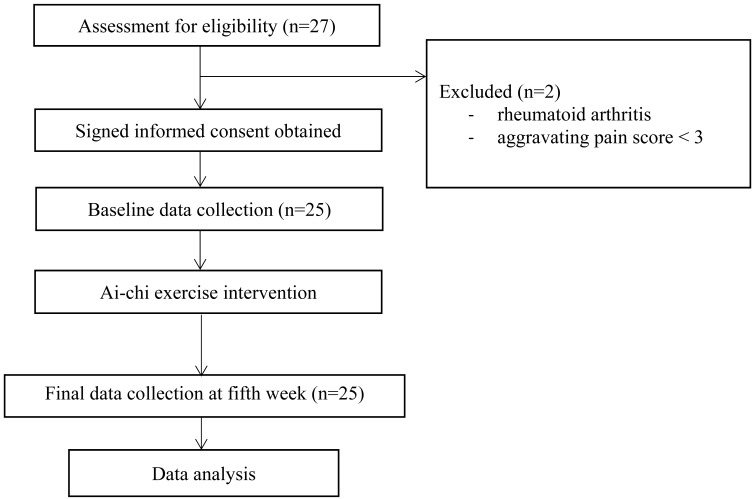
Patients with knee OA were recruited by convenience sampling from the Chinese YMCA and from private clinics in Hong Kong. To be included candidates had to be aged less than 65 and to have experienced knee pain for at least a year. The minimum inclusion criteria for pain was 3/10 on the Numeric Pain Rating Scale (NPRS) during self-reported aggravating activities (Fig. 1). They also had to fulfill at least three of the six OA criteria of the American College of Rheumatology’s clinical classification scheme10):
Fig. 1.
Study flow chart
Age greater than 50
Stiffness less than 30 minutes
Crepitus present
Bony tenderness
Bony Enlargement
No palpable warmth
Those criteria correlate well with articular cartilage damage in patients with OA and accurately predict cartilage damage as assessed by arthroscopy11).
Candidates were excluded if they had hydrophobia, any skin diseases, open wounds, incontinence, an unstable cardiopulmonary condition, neurological disease, previous surgery on the knee to be investigated, dysphasia, any psychiatric disorder, impaired cognition, rheumatoid arthritis or systemic lupus erythematosus.
Written informed consent was obtained from all of the participants prior to their being enrolled. Ethical approval (Reference Number: HSEARS20160603002) for the study was obtained from the ethics committee of The Hong Kong Polytechnic University and the study was conducted following the guidelines of the Declaration of Helsinki.
The physiotherapist-supervised five-week Ai Chi program (60 minutes per session, twice per week, 10 sessions in total) was conducted in a warm (31 °C) pool 120 cm deep. The participants were instructed to half-squat so that the water level was around shoulders during Ai Chi practice. The first 16 movement patterns of Ai Chi were introduced following a pre-determined class schedule. New movement patterns were added in each session according to the schedule (Appendix 1). Each movement pattern was repeated three times on both the left and right sides. Subjects who had learned all Ai Chi movement patterns were considered to have successfully completed the course regardless of the quality of their execution. Land and water warm-ups were delivered to minimize the risk of injury. Safety precautions were strictly administered during the intervention.
All of the outcome measures were assessed at baseline and at the conclusion of the course except the aggravating pain score, which was measured at baseline, half way through and at the end. Each subject was asked about the maximum pain they perceived during aggravating activities using Numeric Pain Rating Scale. The NPRS is an 11-point scale ranging from “0” representing “no pain” to 10 for “the most intense pain imaginable”. The NPRS has demonstrated excellent construct validity (0.94) and good to excellent test-retest reliability ranging from 0.79 to 0.9513). The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was used to assess pain, stiffness and physical function. It includes 24 items self-rated on an ordinal scale of “0” to “4”. A higher score indicates greater difficulty in performing certain activities. The index’s test-retest reliability is 0.74 for pain, 0.58 for stiffness and 0.92 for functioning14, 15). It has been shown to have moderate to high construct validity for OA patients14, 15).
The six-minute walk test (6MWT) was also administrated. It is a cost-effective, reliable and validated tool measuring a subject’s functional capacity. It has been reported to have excellent test-retest reliability of 0.88–0.94 and convergent validity with treadmill test of 0.71–0.8216). The 6MWT was conducted according to the standard protocol published by the American Thoracic Society17) except that the hallway was only eight metres long instead of the recommended 30 metres, which was not available at the assessment center. The test was performed twice with 20 minutes of rest between trials, and the distance covered in the best trial was used in the analysis.
The active and passive range of motion (ROM) of both knees in flexion and extension were measured in supine lying for three times by standard goniometry. The average value was used in the analysis. ROM indicates joint stiffness with excellent test-retest reliability (0.98–0.99) and validity (0.97–0.99)18). Knee proprioception was measured using a passive-active procedure. The knee the subject self-reported as more-affected was passively positioned to 17°, 34°, 50° or 67° of flexion. Three seconds were given to memorize the reference angle. The subject was then asked to actively reposition the knee to the reference angle, and the resulting angle was measured. Absolute angular error between the reference angle and the performed angle was calculated. The more affected knee joint was selected for the measurement since there is normally no between-knee difference in proprioception associated with knee OA3). The intra-rater reliability of this proprioceptive recall protocol has been reported as 0.89–0.903). Subjects were directed to close their eyes, and visual and auditory cues to the subjects were not provided to maintain quiet environment because of eliminating influences of feedback effects except proprioception. These procedures were standardized among all of the assessors.
The general health of the participants was also surveyed using a short-form self-reported questionnaire (SF-12) with 12 questions. It generated a physical composite score (PCS) and a mental composite score (MCS). Higher score represents better physical or mental health. The instrument’s test-retest reliability has been demonstrated as 0.89 and 0.86 for the PCS and MCS respectively, and its construct validities are 0.67 and 0.9719).
The statistical analysis was performed with SPSS (version 23.0). The Shapiro-Wilk test was used to check the normality of data. The results of the six outcome measures were compared between the baseline and post-intervention using Friedman’s test for the aggravating pain results; paired t-tests for the 6MWT distances, proprioception, knee ROM and SF-12; and Wilcoxon signed rank tests for the WOMAC scores, as the normality requirement was not fulfilled. Correlations were tested using Pearson’s correlation coefficient for the interval and ratio data or Spearman’s rho for the ordinal and nominal data. The significant p value was set at <0.05, but the significance level was adjusted to 0.017 for post-hoc comparison of the aggravating pain scores.
RESULTS
Of the 27 subjects, the results for 25 (10 males, 15 females) were included in the statistical analysis. Two subjects were excluded: one with rheumatoid arthritis and one with an aggravating pain score <3. Data describing the subjects are shown in Table 1. Twenty-three of the 25 (92%) attended at least 8 of the 10 sessions of Ai Chi training offered. The mean body mass index (BMI) before and after the Ai Chi program were 25.49 ± 4.31 and 25.21 ± 3.87, respectively.
Table 1. Baseline characteristics.
| Variables | Male (n=10) | Female (n=15) | Total (n=25) | |
|---|---|---|---|---|
| Age | 54.10 ± 8.40 | 57.20 ± 3.95 | 55.96 ± 6.16 | |
| BMI | 26.31 ± 2.64 | 24.94 ± 5.16 | 25.49 ± 4.31 | |
| Onset of knee OA (years) | 6.90 ± 5.38 | 5.77 ± 4.80 | 6.22 ± 4.97 | |
| Legs involved | ||||
| Bilateral, No. (%) | 5 (50) | 9 (60) | 14 (56) | |
| Unilateral, No. (%) | 5 (50) | 6 (40) | 11 (44) | |
BMI: body mass index; Knee OA: knee osteoarthritis; n: sample size. Data are presented as mean ± standard deviation, unless indicated otherwise
Table 2 summarizes the observations, except for the knee ROM measurements which are shown in Table 3. The aggravating pain score improved significantly from 6.04 to 3.04 between the baseline and post-intervention. All three domains of the WOMAC, pain, stiffness and physical function, significantly improved from 4.80 to 2.48 (48%, p≤0.01; Table 2), 1.80 to 1.08 (40%, p≤0.05) and 13.04 to 9.04 (31%, p≤0.05), respectively. The knee ROM results were analyzed by grouping the results from the subjects’ self-reported “more affected side” and “less affected side”. There was no significant improvement after the intervention, except for the range of passive extension of the more affected knee (p≤0.05; Table 3).
Table 2. Outcome measures.
| Outcome measures | Mean ± SD | 95% CI of difference (Lower, Upper) |
||
|---|---|---|---|---|
| Baseline | Post-intervention | |||
| Aggravating pain score* | 6.04 ± 2.01 | 3.04 ± 2.50 | - | |
| WOMAC | ||||
| Pain* | 4.80 ± 4.01 | 2.48 ± 3.12 | (–3.77, –1.06) | |
| Stiffness* | 1.8 ± 2.04 | 1.08 ± 1.68 | (–1.53, 0.03) | |
| Physical Function* | 13.04 ± 11.23 | 9.04 ± 10.88 | (–7.90, –0.44) | |
| Knee ROM (Refer to Table 3) | ||||
| 6MWT (m) | 373.03 ± 75.88 | 381.83 ± 62.32 | (–31.30, 13.70) | |
| Proprioception (angular error) | ||||
| 17° Reference angle | 5.42 ± 3.17 | 4.19 ± 3.32 | (–0.63, 3.08) | |
| 34° Reference angle | 3.85 ± 2.79 | 5.11 ± 2.87 | (–2.88, 0.36) | |
| 50° Reference angle | 4.99 ± 2.04 | 4.99 ± 2.68 | (–1.27, 1.27) | |
| 67° Reference angle | 4.82 ± 3.10 | 4.99 ± 2.68 | (–1.96, 1.63) | |
| SF-12 score | ||||
| PCS | 40.78 ± 9.15 | 43.69 ± 8.77 | (–6.24, 0.42) | |
| MCS | 53.13 ± 8.47 | 54.93 ± 8.47 | (–4.84, 1.24) | |
*Statistically significant at the p≤0.05 level of confidence. 6MWT: six-minute walk test; MCS: SF-12 mental component summary; PCS: SF-12 physical component summary; ROM: range of motion; SF-12: Short-Form 12-item health survey; WOMAC: Western Ontario and McMaster Universities Arthritis Index
Table 3. The knee ROM results.
| Mean ± SD | Mean change | 95% CI of difference (Lower, Upper) |
|||
|---|---|---|---|---|---|
| Baseline mean | Post-intervention mean | ||||
| ROM of the more affected knee | |||||
| Flexion AROM | 121.77° ± 10.07° | 121.67° ± 11.40° | 0.10° | (3.25, –3.05) | |
| Flexion PROM | 126.59° ± 10.02° | 126.71° ± 11.82° | –0.12° | (2.91, –3.15) | |
| Extension AROM | –2.54° ± 3.29° | –1.45° ± 4.12° | –1.09° | (0.26, –2.44) | |
| Extension PROM* | 0.91° ± 2.71° | 2.80° ± 3.27° | –1.89° | (–0.25, –3.54) | |
| ROM of the less affected knee | |||||
| Flexion AROM | 123.78° ± 8.55° | 125.44° ± 9.43° | –1.65° | (1.06, –4.37) | |
| Flexion PROM | 128.62° ± 7.62° | 130.51° ± 8.91° | –1.88° | (1.08, –4.85) | |
| Extension AROM | –0.94° ± 2.97° | 0.36° ± 3.48° | –1.30° | (0.28, –2.89) | |
| Extension PROM | 2.32° ± 4.57° | 4.13° ± 3.62° | –1.81° | (0.09, –3.72) | |
*Statistically significant at the p≤0.05 level of confidence. AROM: active range of motion; PROM: passive range of motion
The mean distance covered in the 6-mintue walk test (6MWD) was 373.03 m at baseline and 381.83 m in the post-intervention assessment. These were not significantly different (Table 2). There was also no significant difference in absolute angular error in knee positioning at any of the reference angles tested (Table 2). The baseline and post-intervention results on the PCS and MCS components of the SF-12 assessment also did not differ significantly (Table 2).
DISCUSSION
Pain is a common symptom of knee OA, so pain management is crucial for OA. The results demonstrate significant improvement in both the pain associated with aggravating activities and in WOMAC pain scores after five weeks Ai Chi intervention. The significant results support those of other studies showing reduction of pain through aquatic therapy4, 7, 8). The decrease in aggravating pain score (NPRS=2.60) reached the level of a minimal clinically-important difference (MCID) for chronic pain patients (1.70)20). The improvement in WOMAC pain score of 48% was also clinically significant, exceeding the suggested 17 to 26%20). Those improvements should, however, be interpreted with caution, as the predicted causal relationship with the Ai Chi intervention cannot be established without a control group.
A number of possible reasons for the improvement in pain suggest themselves. As the Ai Chi intervention was delivered in a warm pool at 31 °C, the water’s warmth should have helped relieve the pain by blocking the nociceptive inputs with inputs from thermal receptors as explained by the pain gate theory4, 6). Beyond that, a recent systematic review has confirmed that conventional aquatic exercise can help to relieve knee OA pain21). The hydrostatic pressure can facilitate venous return, reducing peripheral edema and thus relieving pain21). Additionally, buoyancy helps reduce loading to the lower limb by 90% with a water level around the shoulders21). In addition to the water properties, Ai Chi can progressively increase the complexity and diversity of movement on a reducing base of support. Ai Chi involves both closed and open chain movement patterns, the knee OA participant experience weight shifting, partial weight bearing and pivoting on stance leg during the training9). Ai Chi provides metacentric principles demand muscular control with direction changes which facilitate the improvement in knee proprioception and pain9). Also, Ai Chi focuses on the combination of movement patterns and breathing patterns which helps to relieve muscle activation and spasm.
However, the lack of any significant difference in aggravating pain score between the midterm to post-intervention assessments could be due to the comparatively challenging movement patterns taught in the second half of the intervention (Appendix 1) and the relatively slower rate of improvement after the immediate pain reduction that subjects experienced in the first half of the intervention. Three subjects reported very mild pain in their knees while performing patterns 13 and 16 involving large-amplitude body movements in single-leg stance and jumping, respectively. A follow-up assessment might be indicated for further evaluation of changes in pain patterns.
Stiffness is usually one of the symptoms of knee OA, and it is associated with high levels of disability in knee OA patients21). Stiffness was measured using objective ROM measurements and subjective WOMAC scores. Significant improvements in subjective perceptions of knee stiffness were observed, but not in the objective measurements. The characteristics of Ai Chi and the water’s effects may explain the differences Ai Chi involves slow, gentle movements that stretch and move every part of the body9). Buoyancy reduces loading on the knee joints which allows better joint mobility21,22,23). The hydrostatic pressure and warmth may reduce pain and provide sensory input to thermal and mechanical receptors on the skin’s surface. Hence, subjects may feel less restriction in their knee joints, improving perceptions of stiffness even if there has been no objective improvement. The observed changes in ROM may also have been muted because the majority of the subjects were close to normal at baseline. They had little scope for benefitting from the Ai Chi intervention. As subjects practicing Ai Chi were half-squatting most of time during the training, the end range of the knee joints was seldom recruited. It is not surprising, therefore, to observe no significant changes in ROM.
Changes in physical functioning were evaluated in terms of the physical function score of the WOMAC index and 6MWDs. An average 34% improvement in WOMAC physical function scores was observed, but 6MWDs did not improve significantly. According to the feedback from the subjects, pain is one of the most limiting factors in functional activities. The improvement in pain increased their capacity in performing the activities of daily life, which is what in the WOMAC’s physical function domain quantifies. A previous study revealed a strong correlation between pain and the physical function domains in WOMAC scores22, 24, 25). In this study there was no significant correlation between the changes in pain and the changes in the physical function scores after intervention (rs=0.399, p=0.054). The limited sample size may explain the underpowered correlation.
Research has shown that 6MWDs can be affected by physiological, psychological and health predictors including vision, reaction time, postural sway and balance26). Knee pain may cause fear of falls, and that has been found to cause gait changes in a knee OA population26,27,28). The lack of any significant change in 6MWDs despite the improvements in aggravating pain score is probably due to the limited strengthening and cardiopulmonary-training components of Ai Chi. Water turbulence is the only resistance to the Ai Chi maneuvers, and that might not be enough to bring enough improvement in muscle endurance to be reflected in 6MWDs. Asahina and his colleagues have reported29) that even with 40 minutes of aquatic walking exercise the heart rates of the osteoarthritic elderly decreased. Any aquatic exercise involving less exertion than that might not be able to improve cardiopulmonary fitness significantly. The exertion of the Ai Chi protocol tested is probably too mild to achieve the purpose. If so, it is not surprising that no significant improvement in average 6MWD was noted.
Work by Tsang and Hui-Chan has shown that tai chi, the progenitor of Ai Chi, can improve knee proprioceptive acuity30), but no published study has previously investigated the effect of Ai Chi on the proprioception of knee OA patients. Proprioception affects balance and correlates with knee pain and physical activity limitations3). On average, no significant improvement in knee proprioception was observed after the 5-week Ai Chi program. Proprioception involves peripheral and central components. At the peripheral level, muscle spindles are the major mechanoreceptors of proprioceptive information, which was believed to improve upon muscle contraction31). When compared with tai chi’s land-based exercise, water buoyancy reduces loading on the lower limbs during Ai Chi, thus insufficient muscle activity may not be able to enhance the muscle spindles’ performance for better proprioceptive acuity. Another factor is that the subjects in Tsang and Hui-Chan’s tai chi study had about 10 years of experience practicing tai chi, compared with this study’s five weeks of training. Five weeks may not be long enough to induce the changes in cortical mapping involved in increasing proprioceptive acuity30).
The average changes in the PCS and MCS components of the SF-12 were not statistically significant. This despite that a review by Bartels and his colleagues has shown that aquatic therapy in general is effective in improving the PCS scores of knee OA patients4). The small sample size may have contributed to the non-significant result observed in this study. The MCS result aligns with those of other studies which have shown that the MCS component is not improved significantly by aquatic therapy. In fact, these subjects had an average baseline MCS score (53.13) comparable with that of age-equivalent healthy individuals (53.90), so the potential for any of improvement was limited32).
This was a pilot study on the effect of Ai Chi for OA knee, its small sample size limited its power in finding statistically significant effects. And without a control group, no causal relationships could be established. This suggests obvious avenues for future study.
Ai Chi can be an effective alternative treatment for knee OA. If a pool is available, it is easy to implement as a class-based intervention. The training can promote self-management to control the progression of knee OA if patients continue exercising on their own. Results show that Ai Chi exercise can relieve pain, reduce self-perceived stiffness and alleviate disease-specific limitations on physical functioning, all of which should promote a better quality of life.
Acknowledgments
We thank the Chinese YMCA of Hong Kong providing the test venue and for its help in recruiting subjects. The Hong Kong Society for Rehabilitation also assisted in the recruitment.
Appendix 1.
Ai-chi movement patterns tested and the program schedule
REFERENCES
- 1.Lee A, Tsang CK, Siu HK, et al. : GP management of osteoarthritic pain in Hong Kong. Aust Fam Physician, 2008, 37: 874–877. [PubMed] [Google Scholar]
- 2.Woo J, Lau E, Lau CS, et al. : Socioeconomic impact of osteoarthritis in Hong Kong: utilization of health and social services, and direct and indirect costs. Arthritis Rheum, 2003, 49: 526–534. [DOI] [PubMed] [Google Scholar]
- 3.Knoop J, Steultjens MP, van der Leeden M, et al. : Proprioception in knee osteoarthritis: a narrative review. Osteoarthritis Cartilage, 2011, 19: 381–388. [DOI] [PubMed] [Google Scholar]
- 4.Bartels EM, Lund H, Hagen KB, et al. : Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev, 2007, 17: CD005523. [DOI] [PubMed] [Google Scholar]
- 5.Fransen M, Nairn L, Winstanley J, et al. : Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum, 2007, 57: 407–414. [DOI] [PubMed] [Google Scholar]
- 6.Audette JF, Bailey A: Integrative pain medicine: the science and practice of complementary and alternative medicine in pain management. Human Press, 2008. [Google Scholar]
- 7.Nekouei P, Sadeghi-Demneh E, Mahdavinejad R, et al. : The effects of aquatic exercise and joint supplements on pain and function of women with knee osteoarthritis. Arch Phys Med Rehabil, 2015, 96: e104–e105. [Google Scholar]
- 8.Gill SD, McBurney H: Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil, 2013, 94: 164–176. [DOI] [PubMed] [Google Scholar]
- 9.Lambeck J, Bommer A: Ai Chi®: applications in clinical practice. In: Comprehensive aquatic therapy, 3rd ed. Washington State University Publishing, 2010. [Google Scholar]
- 10.Altman R, Asch E, Bloch D, et al. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association: Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum, 1986, 29: 1039–1049. [DOI] [PubMed] [Google Scholar]
- 11.Wu C, Morrell R, Concoff A, et al. : Validation of American College of Rheumatology Classification Criteria for knee osteoarthritis using Arthroscopically Defined Cartilage Damage Scores. Seminars in Arthritis and Rhematism, 2005, 35: 197–201. [DOI] [PubMed]
- 12.Brody LT, Geigle PR: Aquatic exercise for rehabilitation and training. Human Kinetics, 2009. [Google Scholar]
- 13.Jensen MP, McFarland CA: Increasing the reliability and validity of pain intensity measurement in chronic pain patients. Pain, 1993, 55: 195–203. [DOI] [PubMed] [Google Scholar]
- 14.Roos EM, Klässbo M, Lohmander LS: WOMAC osteoarthritis index. Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Western Ontario and MacMaster Universities. Scand J Rheumatol, 1999, 28: 210–215. [DOI] [PubMed] [Google Scholar]
- 15.McConnell S, Kolopack P, Davis AM: The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum, 2001, 45: 453–461. [DOI] [PubMed] [Google Scholar]
- 16.Rikli RE, Jones CJ: The reliability and validity of a 6-minute walk test as a measure of physical endurance in older adults. J Aging Phys Act, 1998, 6: 363–375. [Google Scholar]
- 17.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories: ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med, 2002, 166: 111–117. [DOI] [PubMed] [Google Scholar]
- 18.Gogia PP, Braatz JH, Rose SJ, et al. : Reliability and validity of goniometric measurements at the knee. Phys Ther, 1987, 67: 192–195. [DOI] [PubMed] [Google Scholar]
- 19.Ware J, Jr, Kosinski M, Keller SD: A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care, 1996, 34: 220–233. [DOI] [PubMed] [Google Scholar]
- 20.Farrar JT, Young JP, Jr, LaMoreaux L, et al. : Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain, 2001, 94: 149–158. [DOI] [PubMed] [Google Scholar]
- 21.Hall J, Swinkels A, Briddon J, et al. : Does aquatic exercise relieve pain in adults with neurologic or musculoskeletal disease? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil, 2008, 89: 873–883. [DOI] [PubMed] [Google Scholar]
- 22.White DK, Keysor JJ, Lavalley MP, et al. : Clinically important improvement in function is common in people with or at high risk of knee OA: the MOST study. J Rheumatol, 2010, 37: 1244–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Behrens BJ, Beinert H: Physical agents: theory and practice. Philadelphia: FA Davis, 2004. [Google Scholar]
- 24.Watanabe H, Urabe K, Takahira N, et al. : Quality of life, knee function, and physical activity in Japanese elderly women with early-stage knee osteoarthritis. J Orthop Surg (Hong Kong), 2010, 18: 31–34. [DOI] [PubMed] [Google Scholar]
- 25.Pua YH, Cowan SM, Wrigley TV, et al. : Discriminant validity of the Western Ontario and McMaster Universities Osteoarthritis index physical functioning subscale in community samples with hip osteoarthritis. Arch Phys Med Rehabil, 2009, 90: 1772–1777. [DOI] [PubMed] [Google Scholar]
- 26.Lord SR, Menz HB: Physiologic, psychologic, and health predictors of 6-minute walk performance in older people. Arch Phys Med Rehabil, 2002, 83: 907–911. [DOI] [PubMed] [Google Scholar]
- 27.Stubbs B, Binnekade T, Eggermont L, et al. : Pain and the risk for falls in community-dwelling older adults: systematic review and meta-analysis. Arch Phys Med Rehabil, 2014, 95: 175–187.e9. [DOI] [PubMed] [Google Scholar]
- 28.Demura T, Demura S, Uchiyama M, et al. : Examination of factors affecting gait properties in healthy older adults: focusing on knee extension strength, visual acuity, and knee joint pain. J Geriatr Phys Ther, 2014, 37: 52–57. [DOI] [PubMed] [Google Scholar]
- 29.Asahina M, Asahina MK, Yamanaka Y, et al. : Cardiovascular response during aquatic exercise in patients with osteoarthritis. Am J Phys Med Rehabil, 2010, 89: 731–735. [DOI] [PubMed] [Google Scholar]
- 30.Tsang WW, Hui-Chan CW: Effects of tai chi on joint proprioception and stability limits in elderly subjects. Med Sci Sports Exerc, 2003, 35: 1962–1971. [DOI] [PubMed] [Google Scholar]
- 31.Proske U, Wise AK, Gregory JE: The role of muscle receptors in the detection of movements. Prog Neurobiol, 2000, 60: 85–96. [DOI] [PubMed] [Google Scholar]
- 32.Gandek B, Ware JE, Aaronson NK, et al. : Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol, 1998, 51: 1171–1178. [DOI] [PubMed] [Google Scholar]