Abstract
Purpose
To evaluate and compare the attitudes of ophthalmologists and gynecologists in suggesting appropriate approach to pregnancy in different ocular conditions.
Methods
Specialty-specific questionnaires on delivery mode and abortion indications for ophthalmic patients (refractive, vascular, oncologic, retinal, glaucoma, postoperation, posttrauma, and infectious) were designed and distributed among physician staff of Farabi Eye Hospital and Yas Women Hospital in Tehran. Attitudes and preferences of the ophthalmologists and gynecologists were quantified and compared.
Results
Participants were 29 ophthalmologists and 19 gynecologists. Their mean age was 49.73 ± 7.57 and 46.79 ± 1.36 years, respectively. More than 50–70% ophthalmologists were in favor of normal vaginal delivery (NVD) in all ocular diseases. All gynecologists (100%) expressed their need for an ophthalmologist's opinion for decision-making. Ophthalmologists' top choices for conditions potentially requiring a caesarean section were corneal transplants (34.5%), high myopia (23%), retinal detachment (29%), and orbital tumors (34.5%), while two gynecologists recommended abortion in the presence of intraocular and orbital tumors and retinal detachment.
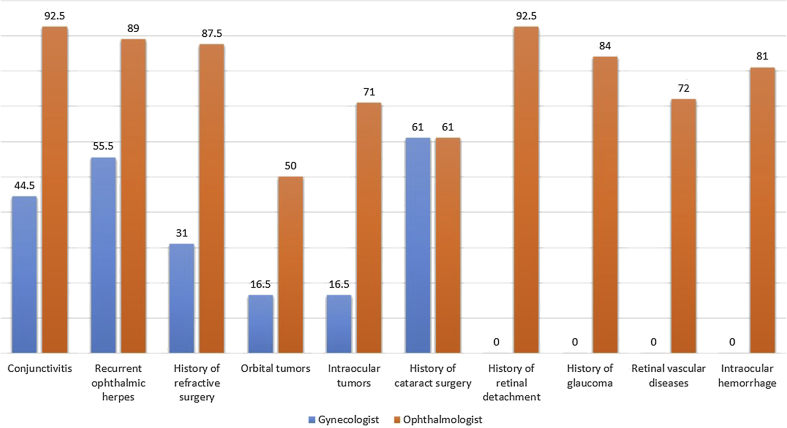
In the case of a history of refractive surgery, orbital tumor and intraocular tumor, ophthalmologists recommend NVD over caesarean section twice as much as their gynecologist peers. For history of retinal detachment, glaucoma, retinal vascular accident and intraocular hemorrhage, no single gynecologist recommend NVD. The corresponding figure for ophthalmologist-recommended NVD were 67, 84, 72, and 81%.
Conclusions
There is extreme inconsistency among ophthalmologists and gynecologists in managing ophthalmic-obstetric scenarios, especially for caesarean section indications. Clinical guideline development and consultation for decision-making in challenging cases are recommended.
Keywords: Eye diseases, Caesarean section, Attitude, Abortion
Introduction
The significant increase in the rate of caesarean-section (C-section) delivery worldwide is one of the major problems in health systems.1 In Iran, the rate of C-section delivery (35–41.9%) is 2–3 times higher than the optimal rate recommended by the World Health Organization (WHO) (10–15%).2, 3, 4 It is obvious that medically unindicated C-section deliveries impose enormous burden on healthcare budgets. Furthermore, unnecessary caesarean surgeries carry great risk to the mother and baby. Risks to the mother include infection, bleeding, anesthesia complications, psychological complications, and a possible need for transfusion, while the baby might suffer respiratory problems and premature birth.3, 4, 5, 6, 7 Therefore, reducing the proportion of C-section deliveries is one of the health system goals, and normal vaginal delivery (NVD) rate is a major indicator of the mother and fetus health.8
According to studies, eye diseases are one of the main non-midwifery reasons for performing C-section delivery. Eye problems reported during pregnancy include refractive errors, diabetic retinopathy, retinal detachment, glaucoma, ocular tumors, and reversible blindness.9, 10, 11 Some of these diseases occur in the context of other medical conditions related to pregnancy such as diabetes and hypertension.12, 13 Some others may be present before pregnancy but they may undergo remission or exacerbation during pregnancy, or their medical intervention pose a challenge to fetal health.14 Thus, issues of family planning (contraception), pregnancy termination (abortion and C-section) or type of term delivery (normal vaginal or caesarean), and the type of anesthesia become controversial.15
We are all so sensitive about our eyes. When this organ has a problem/disease (like high myopia) or has undergone surgery (like refractive surgery or corneal graft), a groundless fear forms: “What if my cornea which is thinner, because of surgery, because of the strain during NVD (Valsalva reflex or increasing venous pressure) be ruptured?” It is likely that pregnant women unconsciously seek a reason to avoid NVD and the caring gynecologist accordingly offers C-section delivery instead; this is not an evidence-based practice.
Frequent consultations with ophthalmologists regarding the need for a caesarean delivery in ophthalmic patients suggest the fact that patients and gynecologists have certain concerns and expectations.
The purpose of this study is to survey and compare the conception of the ophthalmologists and gynecologists in type of delivery in different maternal ocular conditions.
Methods
The survey was conducted among faculty ophthalmologist in Farabi Eye Hospital and gynecologist faculty in Yas Women's Hospital, as referral centers in Tehran, Iran. The questionnaire was comprised of two sections: questions about the academic profile of ophthalmologists and gynecologists, and questions related to their attitudes and perceptions about the type of delivery, necessity for performing abortion, and need for consultation in eye diseases and special eye conditions. Completing the questionnaire is considered participants' consent.
Questionnaire development (validity and reliability)
A list of ocular diseases and conditions, sorted anatomically, was provided; they were found in literature and previous reports6, 7, 15, 16 or otherwise assumed to be related to pregnancy. The list included structural, refractive, vascular, and infectious disorders, as well as trauma and previous surgery (content validity). Respondents could select the “no comments” option, too (Table 1). In addition to baseline and demographic characteristics of the respondents, we calculated their preferences with respect to various obstetric choices in the presence of different ocular conditions by specialty, i.e. ophthalmology vs. obstetrics.
Table 1.
A generic view of the questionnaires.
| Offer abortion in first trimester |
Suggested delivery types |
Needing consultation with an ophthalmologist |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | No comment | Normal vaginal | Caesarean-section |
No comment | Yes | No | ||
| With general anesthesia | With local anesthesia | ||||||||
| Ocular diseases and conditions | |||||||||
Based on the specialty, i.e. obstetrics versus ophthalmology, two customized versions of questionnaire were developed. In the gynecologists' version, we used more general terms for the ophthalmic list. These lists were independently reviewed by one ophthalmologist and a gynecologist to cover all important and specific eye diseases and conditions (face validity).
The questionnaire was distributed among all faculty members of Farabi Eye Hospital and gynecologists of the Yas Women's Hospital. One of the researchers was present on site while respondents completed the questionnaire. There were also open-ended questions and spaces for free comments.
Descriptive statistics were used to summarize and compare results. Relative frequencies were determined, and bar diagrams were used to illustrate results. The mean age and years of practice of the two professions were analyzed with student t test.
The study protocol was reviewed and approved by Tehran University of Medical Sciences Research Council, and was granted partial support (grant# 90-04-43-15451).
Results
Participants were 29 ophthalmologists and 19 gynecologists. The mean age of these two groups was 49.73 ± 7.57 years and 46.79 ± 1.36 years, respectively (P = 0.18). Twenty-five of the ophthalmologists (86%) were men, and all gynecologists were women. Mean years of practice was 18.04 ± 8.7 for ophthalmologists and 15.67 ± 6.12 years for gynecologists (P = 0.3). Among ophthalmologists, there were 6 assistant professors (24%), 10 associate professors (40%), and the remaining were full professors. In the gynecologists' group, there were 6 assistant professors (32%), 8 associate professors (42%), and 5 held the title of professor (26%).
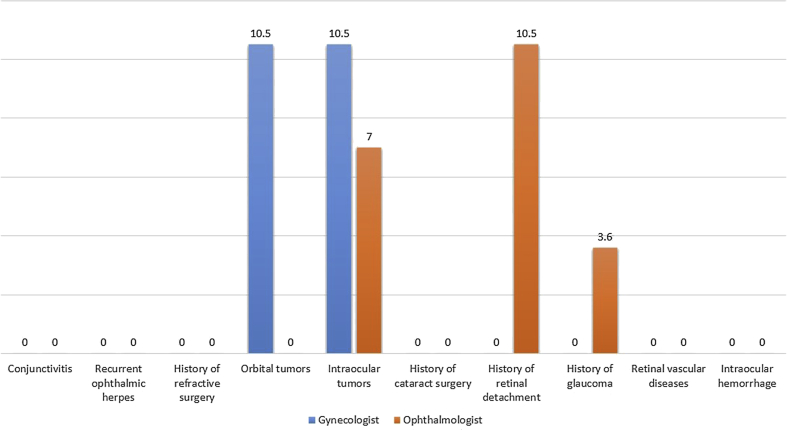
Abortion recommendation
Two gynecologists (10.5%) were in favor of suggesting abortion in the presence of intraocular tumors, orbital tumors, or a history of retinal detachment. The others chose ‘no comment’. One ophthalmologist (3.4%) agreed with suggesting abortion in advanced uncontrolled glaucoma and 2 (7.1%) in the presence of melanoma (intraocular tumors) (Fig. 1).
Fig. 1.
Comparison of ophthalmologists and gynecologists on elective abortion in ophthalmic patients (figures are in percentages).
Normal vaginal delivery versus caesarean-section delivery
The highest consensus among gynecologists in favor of NVD (no need for C-section delivery) was related to the history of eye surgery (cataract, ocular trauma, and intraocular lens implantation) and recurrent ocular herpes. These views are summarized in Table 2 and Fig. 2.
Table 2.
Attitude of gynecologists on the choice of delivery type in ophthalmic patients.
| n (%) Disease or specific condition | NVD | CS + GA | CS + LA | No comment |
|---|---|---|---|---|
| History of glaucoma | 0 | 4 (25) | 0 | 12 (75) |
| Severe refractive errors | 1 (6.2) | 4 (25) | 1 (6.2) | 10 (52.6) |
| History of refractive surgery | 5 (31.2) | 3 (18.8) | 1 (6.2) | 7 (43.8) |
| Active conjunctivitis | 8 (44.4) | 1 (5.6) | 0 | 9 (50) |
| Recurrent ophthalmic herpes | 10 (55.6) | 0 | 0 | 8 (44.4) |
| Intraocular hemorrhage | 0 | 6 (33.3) | 2 (11.1) | 10 (55.6) |
| Retinal vascular disorders | 0 | 6 (33.3) | 2 (11.1) | 10 (55.6) |
| Diabetic retinopathy | 4 (21.1) | 4 (21.1) | 3 (15.8) | 8 (42.1) |
| History of ophthalmic surgery such as cataract, IOL implantation or trauma | 12 (66.7) | 0 | 0 | 6 (33.3) |
| Intraocular tumors | 4 (22.3) | 0 | 0 | 14 (77.8) |
| Orbital tumors | 4 (22.3) | 0 | 0 | 14 (77.8) |
| History of retinal detachment | 0 | 4 (22.2) | 2 (10.5) | 12 (66.7) |
NVD: Normal Vaginal Delivery, CS: Caesarean Section, GA: General Anesthesia, LA: Local Anesthesia.
Fig. 2.
Comparison of ophthalmologists and gynecologists recommending normal vaginal delivery (NVD) in ophthalmic patients (figures are in percentages).
Among ophthalmologists, there was an overwhelming agreement in favor of NVD in the presence of various ocular diseases and conditions (Table 3 and Fig. 2). In orbital tumor, ophthalmologists suggest NVD 3 times more than gynecologists, in the history of refractive surgery 2.8 times, in the conjunctivitis 2 times, and in the recurrent ocular herpes 1.6 times more.
Table 3.
Attitude of ophthalmologists on the choice of delivery type in ophthalmic patients.
| n (%) Disease or specific condition | NVD | CS + GA | CS + LA | No comment | |
|---|---|---|---|---|---|
| Active conjunctivitis | 25 (92.6) | 2 (7.4) | |||
| Recurrent ophthalmic herpes | 24 (88.9) | 1 (3.7) | 2 (7.4) | ||
| History of refractive surgery | PRK5 | 22 (91.7) | 2 (8.3) | ||
| LASIK | 21 (87.5) | 1 (4.2) | 2 (8.3) | ||
| Phakic IOL | 23 (92) | 2 (8) | |||
| RK6 | 21 (84) | 1 (4) | 1 (4) | 2 (8) | |
| Keratoconus | 22 (84.6) | 1 (4.4) | 1 (3.3) | 2 (7.7) | |
| History of cataract surgery and pseudophakic eye | 24 (92.3) | 2 (7.7) | |||
| Uncontrolled glaucoma | 21 (84) | 1 (4) | 1 (4) | 2 (8) | |
| Advanced glaucoma | 22 (84.6) | 1 (4.4) | 1 (3.3) | 2 (7.7) | |
| History of surgery because of trauma | 22 (84.6) | 1 (3.3) | 1 (3.3) | 2 (7.7) | |
| High myopia | 19 (73.1) | 2 (7.7) | 4 (15.4) | 1 (3.8) | |
| Retinal break | 16 (64) | 4 (16) | 4 (16) | 1 (4) | |
| History of retinal detachment | 16 (66.7) | 3 (12.5) | 4 (16.7) | 1 (4.2) | |
| Macular edema or PDR | 22 (81.5) | 1 (3.7) | 2 (7.4) | 2 (7.4) | |
| Vitreous cavity hemorrhage | 21 (80.8) | 1 (3.8) | 2 (7.7) | 2 (7.7) | |
| Intraocular tumor such as melanoma | 17 (70.8) | 1 (4.2) | 6 (25) | ||
| Retinal vascular disorder or anomaly | 18 (72) | 1 (4) | 2 (8) | 4 (16) | |
| Orbital tumor | 13 (50) | 5 (19.2) | 4 (15.4) | 4 (15.4) | |
| PKP | 15 (50) | 11 (36.7) | 3 (10) | 1 (3.3) | |
| Others | |||||
NVD: Normal Vaginal Delivery, CS: Caesarean Section, GA: General Anesthesia, LA: Local Anesthesia, PRK: Photorefractive Keratectomy, LASIK: Laser-Assisted in Situ Keratomileusis, RK: Radial Keratotomy, PDR: Proliferative Diabetic Retinopathy, PKP: Penetrating Keratoplasty.
All gynecologists expressed the need for consultation for making decisions in the presence of ocular conditions.
Discussion
Recommendation on abortion or caesarean section in various eye diseases
Ophthalmologists and gynecologists had limited reasons for recommending abortion. This may be because eye diseases are basically not life-threatening. Legal, religious, and cultural considerations in Iran are probably influential as well.
While many non-midwifery-related C-section deliveries are performed because of eye diseases, ophthalmologists believe there is no specific indication for a caesarean section in ophthalmic patients.16, 17
In Iran, very few cases of abortion have been requested due to the presence of an eye condition. In a study in Sanandaj (northwestern Iran) of the 58 cases of abortion during 2003–2007, 34 were legally approved, and only one case was attributed to maternal uveitis.17 In Kerman, of the 47 cases of abortion, 24 of which were legally approved had an ophthalmic reason for abortion in 2005.18
In a study on 13,079 deliveries in Poland during 1990–1994, eye diseases were the reason for 2.04% of all C-sections and 20% of non-midwifery-related causes. These causes included hypertension (33%), eye disorders (20%), uterine myoma (16%), heart disease (10%), pelvis complications (8.75%), neurological disorders (8–12%) etc. Eye problems were the second most common non-midwifery reason.8, 16 In another study in Poland on 4895 deliveries in 2010, the most frequent eye diseases associated with C-sections delivery were refractive errors (myopia) (57%), followed by retinopathy (20%), retinal detachment (7%), and glaucoma (5%).16
In a study of the 4895 C-section records, 2.04% of C-sections were recommended by an ophthalmologists for this type of delivery. The frequency of C-sections due to ocular indications continued to increase during 2000–2005. The most common ophthalmic disorders included myopia (57%), retinopathy (20%), glaucoma (5%), imminent retinal detachment (4%), and past retinal detachment (3%). In this study, 45% of records indicated eye pathology as the only reason for C-section.9
In our study, the most common reasons for ophthalmologists recommending a C-section delivery were corneal transplantation (46.7%), high myopia (23.1%), retinal disorders such as history of retinal detachment (29.2%), and orbital tumors (34.6%), while retinal vascular disorders (44.4%) were the most common reasons for gynecologists (more than 3.7 times of ophthalmologists). All gynecologists felt obliged to consult an ophthalmologist about eye disorders; cases with eye tumors and a history of glaucoma were the most ambiguous ones for them.
The hormonal, metabolic, and hematologic changes that occur during normal pregnancy cause a variety of changes throughout the body. Some retinal diseases are more common during pregnancy (such as central serous chorioretinopathy and uveal melanoma), some may exacerbate during pregnancy, but it is not generally acceptable to recommend abortion on such grounds.19, 20, 21, 22, 23, 24, 25, 26, 27, 28 On the other hand, some disease conditions such as autoimmunity (e.g. uveitis and allergic conjunctivitis) and high intraocular pressure (IOP), improve during pregnancy.19, 28 However, the risk of teratogenicity of ophthalmic medications, although not confirmed in humans, should be considered in any of the chronic ocular diseases. A group of retinal diseases are seen during pregnancy in association with systemic diseases such as preeclampsia/eclampsia and disseminated intravascular coagulation (DIC). Retinal detachment, optic nerve ischemia (probably because of retinal edema), and central serous chorioretinopathy (in all three trimesters of pregnancy) have been reported along with eclampsia.5, 29, 30, 31, 32, 33, 34, 35, 36, 37 Therefore, it is recommended for pregnant women (especially in the presence of underlying disease such as diabetes or hypertension) to have complete eye examinations and receive specialty ophthalmic treatment as needed.7 It is worth mentioning that many ophthalmic diagnostic tests and treatments such as photography, retinal laser, and intraocular drug injections are not invasive or have no impact on the physiology of pregnancy or fetal health. The general notion for being inclined to do a C-section in retinal diseases is the specialists' misbelief that physical stress from the Valsalva manoeuvre may affect the eyes and cause complications.
Diabetic retinopathy
A considerable percentage of gynecologists (37%) were in favor of performing C-section in cases of retinopathy (42% had no comment), while ophthalmologists did not believe caesarean was necessary. This is consistent with results of the study by Prost20 that stated there is no indication for abortion or caesarean delivery in women with diabetic retinopathy and retinal detachment. However, many studies have shown that these conditions worsen during pregnancy.20, 21, 22, 23 Thus, it has been emphasized to have regular eye examinations before pregnancy and then every three months during pregnancy and, if necessary, further tests depending on their physician's opinion; and to deliver standard treatments that are applied to non-pregnant patients (such as retinal laser and intraocular injections).24, 25 It should be noted that there have been cases of spontaneous recovery after delivery without treatment of diabetic macular edema.26 It is clear that these issues are not relevant to the mode of delivery anyway.
Other retinal disorders
Gynecologists were most likely to recommend a C-section delivery for cases with retinal disorders, including vascular diseases (45%), intraocular hemorrhage (45%), and a history of retinal detachment (33%) (Table 1). A similar tendency, however with lower rates was expressed by the ophthalmologists; they recommended a C-section delivery for cases with a retinal tear (32%), retinal detachment (29%), vitreous cavity hemorrhage (10%), and retinal vascular disorders (12%) (Table 2).
Krasnoshchekova and colleagues studied ocular changes in 188 women during pregnancy and puerperium over a 2-year period and reported no significant difference between women who delivered by NVD or caesarean section.27
Glaucoma
In the present study, while 96% of the ophthalmologists did not recommend abortion because of glaucoma, only 57% of the gynecologists opposed abortion, and the rest had no comment. There is a physiological IOP decrease during pregnancy (in normal and glaucomatous eyes).35, 37 For example, in one study, IOP changes were studied among 44 pregnant women with healthy eyes and 32 pregnant women with high IOP against 44 non-pregnant woman with normal IOP, and 32 non-pregnant women with high IOP. The average IOP decrease was 20% in the healthy pregnant women and 24% in the pregnant women with high IOP. In both groups, IOP reduction was independent from blood pressure, weight, height, and gravidity.38 This magnitude is very much close to the average amount of drop caused by IOP-lowering eye drops of 20–30%. Another study has demonstrated that IOP decreases even in the third trimester when systolic blood pressure increases; the higher the gestational age, the greater the IOP decrease was.39 It is important to note that all anti-glaucoma medications are class C drugs except Brimonidine and Dipivefrin which are class B; thus, there can be serious risks for the fetus if multiple medications are required.40
C-section delivery for women with glaucoma was recommended by 25% of the gynecologists, and the rest had no comment, but 84% of the ophthalmologists recommended NVD. Gynecologists seem to recommend C-section delivery whenever they feel there is a “potential risk” because they consider C-section delivery to be a more manageable situation than NVD. We may consider abortion or early delivery (C-section) for patients with advanced or uncontrolled glaucoma who are expected to need multiple anti-glaucoma eye drops or an eye surgery. Anti-glaucoma medications may interfere with the process of delivery (for instance beta blockers). On the other hand, it is very difficult to perform glaucoma surgery in a pregnant women in either local or general anesthesia. Efforts should be made to perform glaucoma surgery prior to pregnancy. These are special and rare conditions with no clear evidence for the approach in the literature.
High myopia and retinal detachment
None of the ophthalmologists recommended abortion because of high myopia, and 31% of the gynecologists had no comment. However, 0.6% of the gynecologists and 73% of the ophthalmologists chose and recommended NVD, and this difference is very notable. Chiu and colleagues conducted a survey in 2015 among ophthalmologists and obstetrician-gynecologists on the mode of delivery in women with risk factors for rhegmatogenous retinal detachment including myopia. Thirty-four percent of obstetrician-gynecologists recommended C-section or instrumental delivery compared to only 4% of ophthalmologists.41 This high degree of consensus among ophthalmologists may act as a reference expert opinion till empiric evidence is made available.
During pregnancy, corneal sensitivity decreases, while corneal thickness and curvature increases. While these changes can change the refractive status of patients,26 they are generally reversible after delivery, and there is no evidence of disease progression or worsening that could be related to the type of delivery.42, 43 Therefore, women with high myopia can have NVD, and it is advised that they wait for a few weeks after delivery before updating their glasses.42
According to the literature, vaginal delivery is not correlated with new retinal detachment in female with high myopia.31, 44 Hannah and colleagues did a survey of the two specialists of ophthalmology and obstetrics, to assess their recommendation in the type of delivery in healthy females with risk factor for retinal detachment (high myopia, history of retinal surgery, history of retinal hole or retinal detachment). They concluded that obstetricians may recommend unnecessary surgical intervention in these females.38
Intraocular tumors (e.g. melanoma)
Gynecologists had considerable concern about intraocular tumors: 78% of them had no comment and 22% preferred NVD over caesarean, while 71% of the ophthalmologists recommended NVD. The few studies available on this issue stress that the size of malignant eye tumors such as melanomas may slightly increase as an effect of estrogen during pregnancy,45, 46, 47 but their prognosis and 5-year survival rate were no different from cases without a history of pregnancy.48 These studies reported the effect of the pregnancy itself and not the delivery mode, and therefore, it may not be possible to make a connection between the prognosis of the tumor with the delivery type. A rare special, if ever scenario requiring prompt termination of pregnancy would be a pregnant woman who needs to be treated with cytotoxic agents or radiation therapy.
Ophthalmic herpes
Ocular herpes is independent from genital herpes, and consequently, there is no concern of having NVD. In this study, both groups of experts recommended NVD in these patients. Despite this, ophthalmologists frequently (26%) preferred a consultation in the case of recurrent ophthalmic delivery. In any event, both NVD and C-section delivery are considered stressful and theoretically may cause herpes recurrence.
Other ocular diseases
In other situations, for example, where there is a history of eye surgery (e.g. for cataract), a history of ocular trauma or active conjunctivitis, gynecologists still showed varying degrees of confusion in decision making on the method of delivery. Nonetheless, similar to ophthalmologists' views, C-section delivery was not the preferred choice for them. Although clear evidence does not exist, it seems that the mode of delivery does not affect the ocular disease. Until evidence-based recommendations are generated, the decision can be made according to obstetric indications and priorities.
The authors would like to emphasize that the current survey focuses on pregnancy and eye diseases. Other related aspects like pregnancy planning and eye diseases and acute ophthalmic conditions at the time of delivery are not covered. It should also be noted that this is a study on attitudes which might be different from actual practice. For this reason, an observation study could be devised. Nonetheless, there is a general agreement, compatible with some preliminary evidence that the rate of recommendation for C-sections is higher than needed, and our study clarified that ophthalmologists are not in agreement with their gynecologist peers in such situations.
Our study has limitations in terms of study population (size and framework), scope (as it reports attitudes of practitioners and not real evidence of safety), and lack of a standardized questionnaire. Authors would like to emphasize their intent to highlight a relevant and timely issue along with opinions of practitioners.
In conclusion, although pregnancy, NVD, and breastfeeding have various physiological and pathologic effects on different parts of the body including the eyes, and they are considered stressful biologic events, it does not sound logical to ascribe these changes to the type of delivery and to presume NVD more stressful than C-section. Although C-section delivery is recommended for the purpose of early pregnancy termination in specific clinical situations, it has no proven advantage over NVD for term delivery. With regular ophthalmic examinations during pregnancy (every three months), we argue that eye diseases are not an indication for C-section delivery at term.10, 41, 49 This is in overall agreement with the previously published surveys.
We cannot overemphasize the necessity to establish a close relationship between professionals to make the best decision for the patient and the fetus in complicated cases. For instance, a person who has a serious or uncontrolled ophthalmic disease should use a reliable method of contraception until she reaches a stable condition.
It is noteworthy that we are reporting opinion of a group of gynecologists and ophthalmologists and not empirical evidence on safeties. Until evidence is generated and in order to create consistency and consensus among health system staff regarding the choice of delivery in a variety of eye diseases and to reduce the number of unnecessary C-section deliveries associated with ophthalmic conditions, it is advisable to develop clinical practice guidelines for specialists on the indications for contraception, termination of pregnancy, and C-section delivery in the context of ophthalmic conditions.
Footnotes
Conflict of interest: There is not any conflict of interest. The study was partially funded by grant #90-04-43-15451 of Tehran University of Medical Sciences.
Dr Mohammadi and Ms Letafat-Nejad had equal contribution.
Peer review under responsibility of the Iranian Society of Ophthalmology.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.joco.2016.09.010.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Karska-Basta I., Tarasiewicz M., Kubicka-Trząska A., Miniewicz J., Romanowska-Dixon B. Cesarean section and eye disorders. Ginekol Pol. 2016;87:217–221. doi: 10.17772/gp/61752. [DOI] [PubMed] [Google Scholar]
- 2.Chaichian S., Akhlaghi A., Rousta F., Safavi M. Experience of water birth delivery in Iran. Arch Iran Med. 2009 Sep;12:468–471. [PubMed] [Google Scholar]
- 3.World Health Organization Appropriate technology for birth. Lancet. 1985;2:2. [PubMed] [Google Scholar]
- 4.Ahmad-Nia S., Delavar B., Eini-Zinab H., Kazemipour S., Mehryar A.H., Naghavi M. Caesarean section in the Islamic Republic of Iran: prevalence and some socio-demographic correlates. East Mediterr Health J. 2009;15:10. [PubMed] [Google Scholar]
- 5.Bost B. Cesarean delivery on demand: what will it cost? Am J Obstet Gynecol. 2003;188:1418–1421. doi: 10.1067/mob.2003.455. [DOI] [PubMed] [Google Scholar]
- 6.Fry W. Extensive bilateral retinal detachment in eclampsia, with complete reattachment: report of two cases. Arch Ophthalmol. 1929;1:609–614. [Google Scholar]
- 7.Dehghan M.H., Aghadoust D. Pregnancy and retinal disease. Bina J Ophthalmol. 2001;6:303–312. [Google Scholar]
- 8.Puzio M., Szczurowicz A., Rogoza A., Szczurowicz A., Zwaliński M. Non-obstetric indications for caesarean section from five years of material. Ginekol Pol. 1996;67:383–386. [PubMed] [Google Scholar]
- 9.Socha M., Piotrowiak I., Jagielska I. Retrospective analysis of ocular disorders and frequency of cesarean sections for ocular indications in 2000–2008-our own experience. Ginekol Pol. 2010;81:188–191. [PubMed] [Google Scholar]
- 10.Hart N., Jünemann A., Siemer J., Meurer B., Goecke T., Schild R. Eye disease and mode of delivery. Z Geburtshilfe Neonatol. 2007;211:139–141. doi: 10.1055/s-2007-981235. [DOI] [PubMed] [Google Scholar]
- 11.Taskapili M., Kocabora S., Gulkilik G. Unusual ocular complications of the HELLP syndrome: persistent macular elevation and localized tractional retinal detachment. Ann Ophthalmol (Skokie) 2007;39:261–263. doi: 10.1007/s12009-007-0022-9. [DOI] [PubMed] [Google Scholar]
- 12.Gotovac M., Kastelan S., Lukenda A. Eye and pregnancy. Coll Antropol. 2013;37(suppl 1):189–193. [PubMed] [Google Scholar]
- 13.Swende T., Abwa T. Reversible blindness in fulminating preeclampsia. Ann Afr Med. 2009;8:189–191. doi: 10.4103/1596-3519.57247. [DOI] [PubMed] [Google Scholar]
- 14.Travkin A., Logutova L., Akhvlediani K., Petrova T., Bogorad M. The specific features of delivery in women with gestosis and myopia. Vestn Oftalmol. 2007;123:26–29. [PubMed] [Google Scholar]
- 15.Kuba G., Kroll P. Are there indications for abortion or caesarean section and contraindications for spontaneous delivery in ophthalmologic diseases? Case report and overview. Zentralbl Gynakol. 1998;120:406–412. [PubMed] [Google Scholar]
- 16.Liu S., Heaman M., Kramer M., Demissie K., Wen S., Marcoux S. Length of hospital stay, obstetric conditions at child birth, and maternal readmission: a population-based cohort study. Am J Obstet Gynecol. 2002;187:681–687. doi: 10.1067/mob.2002.125765. [DOI] [PubMed] [Google Scholar]
- 17.Sayedoshohadaie F., Zandvakili F., Yousefinejad V., Yousefi Z., Gharibi F. Investigation of the causes of therapeutic abortion requests in legal medicine organization in Sanandaj, from 2004 to 2008. Sci J Kurdistan Univ Med Sci. 2011;16:76–83. [Google Scholar]
- 18.Ghadipasha M., Aminian Z. The study of abortion licences being issued by legal medicine office of Kerman in 2005 and a short comparison with last years issued licences. J Kerman Univ Med Sci. 2007;14:147–152. [Google Scholar]
- 19.Krasnoshchekova E., Pankrushova T., Boĭko E. Peripheral vitreochorioretinal dystrophies and retinal detachment in pregnant women: diagnosis, treatment, and choice of a delivery procedure. Vestn Oftalmol. 2009;125:40–42. [PubMed] [Google Scholar]
- 20.Junemann A.G., Sterk N., Rejdak R. Influence of mode of delivery on pre-existing eye diseases. Der Ophthalmol. 2012;109:229–234. doi: 10.1007/s00347-011-2460-4. [DOI] [PubMed] [Google Scholar]
- 21.Prost M. Severe myopia and delivery. Klin Ocz. 1996;98:129–130. [PubMed] [Google Scholar]
- 22.Moloney J., Drury M. The effect of pregnancy on the natural course of diabetic retinopathy. Am J Ophthalmol. 1982;93:745–756. doi: 10.1016/0002-9394(82)90471-8. [DOI] [PubMed] [Google Scholar]
- 23.Phelps R., Sakol P., Metzger B., Jampol L., Freinkel N. Changes in diabetic retinopathy during pregnancy, correlations with regulation of hyperglycemia. Arch Ophthalmol. 1986;104:1806–1810. doi: 10.1001/archopht.1986.01050240080044. [DOI] [PubMed] [Google Scholar]
- 24.Egan A.M., McVicker L., Heerey A., Carmody L., Harney F., Dunne F.P. Diabetic retinopathy in pregnancy: a population-based study of women with pregestational diabetes. J Diabetes Res. 2015:310239. doi: 10.1155/2015/310239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Group TDRSR Four risk factors for severe visual loss in diabetic retinopathy. The third report from the diabetic retinopathy study. Arch Ophthalmol. 1979;97:654–655. doi: 10.1001/archopht.1979.01020010310003. [DOI] [PubMed] [Google Scholar]
- 26.Sheth B., Mieler W. Ocular complications of pregnancy. Curr Opin Ophthalmol. 2001;12:455–463. doi: 10.1097/00055735-200112000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Pescosolido N., Campagna O., Barbato A. Diabetic retinopathy and pregnancy. Int Ophthalmol. 2014;34:989–997. doi: 10.1007/s10792-014-9906-z. [DOI] [PubMed] [Google Scholar]
- 28.Ataş M., Duru N., Ulusoy D.M. Evaluation of anterior segment parameters during and after pregnancy. Contact Lens Anterior Eye. 2014;37:447–450. doi: 10.1016/j.clae.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 29.Sunness J., Haller J., Fine S. Central serous chorioretinopathy and pregnancy. Arch Ophthalmol. 1993;111:360–364. doi: 10.1001/archopht.1993.01090030078043. [DOI] [PubMed] [Google Scholar]
- 30.Saito Y., Tano Y. Retinal pigment epithelial lesions associated with choroidal ischemia in preeclampsia. Retina. 1998;18:103–108. doi: 10.1097/00006982-199818020-00002. [DOI] [PubMed] [Google Scholar]
- 31.Mackensen F., Paulus W.E., Max R., Ness T. Ocular changes during pregnancy. Dtsch Arztebl Int. 2014;111:567–576. doi: 10.3238/arztebl.2014.0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park S.J., Choi N.-K., Seo K.H., Park K.H., Woo S.J. Retinal vein occlusion and pregnancy, pre-eclampsia, and eclampsia: the results from a nationwide, population-based study using the national claim database. PLoS One. 2015;10:e0120067. doi: 10.1371/journal.pone.0120067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Olusanya B.A., Oluleye T.S. Unilateral central serous chorioretinopathy in a pregnant Nigerian woman. Niger Med J. 2015;56:372–374. doi: 10.4103/0300-1652.170380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aoyagi R., Hayashi T., Tsuneoka H. Choroidal thickening and macular serous retinal detachment in pregnancy-induced hypertension. Int Med Case Rep J. 2015;8:291–294. doi: 10.2147/IMCRJ.S95442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schultz K., Birnbaum A., Goldstein D. Ocular disease in pregnancy. Curr Opin Ophthalmol. 2005;16:308–314. doi: 10.1097/01.icu.0000179803.42218.cc. [DOI] [PubMed] [Google Scholar]
- 36.Paterson G., Miller S. Hormonal influence in simple glaucoma: a preliminary report. Br J Ophthalmol. 1963;47:129–137. doi: 10.1136/bjo.47.3.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Phillips C., Gore S. Ocular hypotensive effect of late pregnancy with and without high blood pressure. Br J Ophthalmol. 1985;69:117–119. doi: 10.1136/bjo.69.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qureshi I. Intraocular pressure and pregnancy: a comparison between normal and ocular hypertensive subjects. Arch Med Res. 1997;28:397–400. [PubMed] [Google Scholar]
- 39.Qureshi I., Xi X., Wu X. Intraocular pressure trends in pregnancy and in the third trimester hypertensive patients. Acta Obstet Gynecol Scand. 1996;75:816–819. doi: 10.3109/00016349609054709. [DOI] [PubMed] [Google Scholar]
- 40.Razeghinejad M.R., Tai T.Y.T., Fudemberg S.J., Katz L.J. Pregnancy and glaucoma. Surv Ophthalmol. 2011;56:324–335. doi: 10.1016/j.survophthal.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 41.Chiu H., Steele D., McAlister C., Lam W. Delivery recommendations for pregnant females with risk factors for rhegmatogenous retinal detachment. Can J Ophthalmol. 2015;50:4. doi: 10.1016/j.jcjo.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 42.Katsulov A., Todorova T., Denovska M., Iankov M. Myopia and labor. Akush Ginekol (Sofiia) 1999;38:51–54. [PubMed] [Google Scholar]
- 43.Pizzarello L. Refractive changes in pregnancy. Graefe's archive for clinical and experimental ophthalmology graefes. Arch Clin Exp Ophthalmol. 2003;241:484–488. doi: 10.1007/s00417-003-0674-0. [DOI] [PubMed] [Google Scholar]
- 44.Sharma S., Rekha W., Sharma T., Downey G. Refractive issues in pregnancy. Aust N Z J Obstet Gynaecol. 2006;46:186–188. doi: 10.1111/j.1479-828X.2006.00569.x. [DOI] [PubMed] [Google Scholar]
- 45.Hartge P., Tucker M., Shields J., Augsburger J., Hoover R., Fraumeni J.J. Case-control study of female hormones and eye melanoma. Cancer Res. 1989;49:4622–4625. [PubMed] [Google Scholar]
- 46.Seddon J., MacLaughlin D., Albert D., Gragoudas E., Ference M. Uveal melanomas presenting during pregnancy and the investigation of oestrogen receptors in melanomas. Br J Ophthalmol. 1982;66:695–704. doi: 10.1136/bjo.66.11.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Siegel R., Ainslie W. Malignant ocular melanoma during pregnancy. JAMA. 1963;185:542–543. doi: 10.1001/jama.1963.03060060140028. [DOI] [PubMed] [Google Scholar]
- 48.Shields C., Shields J., Eagle R.J., De Potter P., Menduke H. Uveal melanoma and pregnancy. A report of 16 cases. Ophthalmology. 1991;11:1667–1673. doi: 10.1016/s0161-6420(91)32060-8. [DOI] [PubMed] [Google Scholar]
- 49.Juenemann A.M., Nowomiejska K., Oleszczuk A., Ksiazek P., Oleszczuk J., Rejdak R. Mode of delivery and eye diseases. Ginekol Pol. 2012;83:613–617. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.