Abstract
Purpose
To compare full-time occlusion (FTO) and part-time occlusion (PTO) therapy in the treatment of amblyopia, with the secondary aim of evaluating the minimum number of hours of part-time patching required for maximal effect from occlusion.
Methods
A literature search was performed in PubMed, Scopus, Science Direct, Ovid, Web of Science and Cochrane library. Methodological quality of the literature was evaluated according to the Oxford Center for Evidence Based Medicine and modified Newcastle-Ottawa scale. Statistical analyses were performed using Comprehensive Meta-Analysis (version 2, Biostat Inc., USA).
Results
The present meta-analysis included six studies [three randomized controlled trials (RCTs) and three non-RCTs]. Pooled standardized difference in the mean changes in the visual acuity was 0.337 [lower and upper limits: −0.009, 0.683] higher in the FTO as compared to the PTO group; however, this difference was not statistically significant (P = 0.056, Cochrane Q value = 20.4 (P = 0.001), I2 = 75.49%). Egger's regression intercept was 5.46 (P = 0.04). The pooled standardized difference in means of visual acuity changes was 1.097 [lower and upper limits: 0.68, 1.513] higher in the FTO arm (P < 0.001), and 0.7 [lower and upper limits: 0.315, 1.085] higher in the PTO arm (P < 0.001) compared to PTO less than two hours.
Conclusions
This meta-analysis shows no statistically significant difference between PTO and FTO in treatment of amblyopia. However, our results suggest that the minimum effective PTO duration, to observe maximal improvement in visual acuity is six hours per day.
Keywords: Occlusion, Amblyopia, Part-time, Full-time
Introduction
Amblyopia is a relatively common disorder, affecting 1–4% of the general population.1, 2, 3, 4 This condition features a unilateral or, less commonly, a bilateral loss of vision caused by abnormal development of the visual system during the critical period of visual development (the first 8–10 years of life). It represents visual loss at a cortical level where information first interacts between the two eyes. If not treated during the critical period, amblyopia can cause lifetime significant visual impairment.5 Although improvements are possible in adults with proper treatment, early detection and treatment still offer the best outcome.6, 7
The basic pathophysiologic mechanisms of amblyopia are abnormal binocular interaction and pattern vision deprivation. Amblyopia can be classified based on the underlying cause; strabismus, refractive error (anisometropia or bilateral high refractive error) and form deprivation.8 Strabismic and anisometropic amblyopia commonly co-exist.9
In amblyopia therapy, the first step is correction of the refractive error and constant use of spectacles and/or contact lenses until no further improvement in visual acuity is obtained.10 The next step is often occlusion therapy in order to force reliance upon the weaker eye by patching the dominant eye. Occlusion therapy and appropriate refractive correction remain the mainstay of treatment since the 18th century, and while newer approaches to treatment are emerging, occlusion retains its central place in amblyopia treatment in most clinical settings.11 Occlusion variables are classified according to the area of visual field occluded (total or full and partial or sectorial e.g. bi-nasal patch for promotion of alternate fixation), effect on light transmission (opaque or non-transmitting for light and form and attenuating or partial light transmission) and wearing time.12
Amongst clinicians, there are different opinions about the appropriate duration of occlusion therapy for maximum treatment effect, ranging from short periods of occlusion [part-time occlusion (PTO)] to full-time occlusion (FTO) for the treatment of amblyopia. Some clinicians are proponents of FTO, and believe that appropriately-monitored patients treated with FTO can have excellent outcomes.13, 14 However, supporters of PTO, by contrast, feel that less patching time is not inferior to FTO.15 Occlusion amblyopia, or the development of amblyopia in the originally better-seeing, patched eye, is a risk commonly cited by opponents of FTO. Although the incidence of occlusion amblyopia in children treated with FTO is admittedly significant (19.3%,16 25.8%,14), it is almost always reversible.12 Furthermore, after cessation of treatment, the final interocular difference in visual acuity was actually less in children with a history of occlusion amblyopia, suggesting that occlusion amblyopia can herald a better visual potential in the initially amblyopic eye.14, 16
Some studies suggest that FTO results in better improvement in visual acuity of amblyopic eyes than does PTO.15, 17, 18 One retrospective review in a small sample size (n = 45), demonstrated a trend toward better visual outcome and a more rapid improvement in patients treated with FTO compared to those treated with PTO (<6 h).13 However, there is continuing controversy regarding the number of hours of patching per day that should be prescribed for amblyopia, ranging from less than 2 hrs a day,15, 18 or between 2 and 6 hrs a day (part-time occlusion)15, 17 to more than 10 hrs a day, 7 days a week (i.e. FTO).17
The primary objective of this systematic review and meta-analysis was to investigate the efficacy of full-time versus PTO therapy in the process of rehabilitation of amblyopic patients.
Methods
Search strategy and inclusion criteria
For considering studies for this systematic review, we included randomized controlled trials (RCTs) and observational, peer-reviewed publications that compared the effects of two patching regimens: FTO (more than 10 hrs a day or all waking hours) and PTO (6 hrs or less). Participants in these trials were children diagnosed with amblyopia (strabismic, anisometropic, strabismic & anisometropic), had visual acuity in the weaker eye between 0.3 and 1.3 logMAR, visual acuity in the sound eye of 0.3 logMAR or better, no previous amblyopia therapy, no ocular pathology, no prior surgery. Additionally, where anisometropia was diagnosed, it was more than 0.5 diopter difference in the spherical equivalent refraction, and when strabismus was diagnosed, it was constant not intermittent. There was no restriction for time of follow-up as different studies had different time point for follow-up. Studies with combination therapies, those considering FTO or PTO as a treatment option alone, using atropine as a penalization method, limited to only one type of amblyopia, or those with any associated active treatment options were excluded from this meta-analysis.
For identification of studies, we searched PubMed, Scopus, Science Direct, Ovid, Web of Science and Cochrane library from their inception to March 2016. Search terms were “part-time”, “full-time”, “patching”, “occlusion”, “amblyopia” or “therapy”. In addition, reference lists of relevant articles were searched for additional trials and we used the Science Citation Index to search for articles that cited the included studies. No language limit was exerted on the search strategy. Unpublished papers were not included.
We used Der-Simonian and Laird method or random effects model in order to pool the studies. In this method, between study variability is taken into account for weighting and is more suitable for heterogeneous studies.19
Two authors (NY & AE) checked the titles and abstracts obtained by the searches to determine whether they met the inclusion criteria (mentioned above) for this review.
Statistical analysis
For each study, the mean difference in visual acuity recorded in logMAR notation was determined for the PTO and FTO groups. To pool the effect sizes across studies, a random effects model was used. Heterogeneity was evaluated by the Cochrane Q test (the significance level was considered to be 0.05.) and I2 index.20 Publication bias was evaluated graphically by funnel plots and statistically by Egger's regression intercept method.21
The quality of the RCTs was evaluated by the Oxford Center for Evidence Based Medicine checklist for RCTs.22 Observational studies were checked by the modified Newcastle-Ottawa scale for observational studies.23 Sub-group analyses according to the study design (RCT vs. non-RCT) and duration of part-time patching were also performed. All statistical analyses were performed using Comprehensive Meta-Analysis (version 2, Biostat Inc., USA).
Results
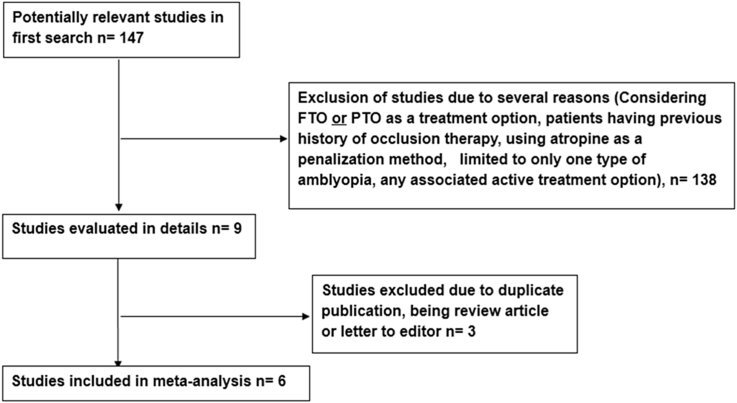
Fig. 1 shows the PRISMA flowchart for this review. Overall, six studies were included in this systematic review. Three of these studies had an RCT design, and the remainder were observational, non-randomized trials. Table 1 shows the characteristics of the six studies. Table 2, Table 3 show the quality assessment of the included studies.
Fig. 1.
PRISMA flowchart of studies evaluated in detail. FTO: Full-time occlusion, PTO: Part-time Occlusion.
Table 1.
Characteristics of the included studies.
| Authors | Study design | Region | Age (years) | Type of amblyopia | FTO (>10 h) duration sample size | PTO (2–6 h) duration sample size | PTO (<2 h) duration sample size | Follow-up | Mean improvement in visual acuity in lines from baseline | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|
| Stewart et al (2007)24 | RCT | United Kingdom | 3–8 | AA, SA, MA | 12 h n = 40 |
6 h n = 40 |
– | Every 2 W | FTO:2.4 PTO:2.6 |
PTO and FTO prescribed occlusion results in similar visual outcome. |
| Arikan et al (2005)15 | nRCT | Turkey | 3–12 | AA, SA, MA | All waking hours n = 39 | 2–6 h n = 70 |
Less than 1 h n = 19 | 6 M 10 Y |
FTO:5.8 PTO (2–6 h): 3.5 PTO (<2 h): 0.19 |
The amount of improvement in visual acuity was significantly higher in FTO group. |
| PEDIG (2003a)17 | RCT | United States | <7 | AA, SA, MA | All waking hours n = 90 | 6 h n = 85 |
– | 5 W 4 M |
FTO:4.7 PTO:4.8 |
Visual acuity in the amblyopic eye improved a similar amount. |
| PEDIG (2003b)34 | nRCT | United States | 3–7 | AA, SA, MA | >10 h n = 55 |
6 h n = 91 |
– | 5 W 16 W 6 M |
FTO:3.3 PTO:3.1 |
At 6 months, improvement appears to be similar with PTO vs FTO. |
| Hug (2004)13 | nRCT | United States | 3–7 | AA, SA | All waking hours n = 21 | <6 h n = 24 |
– | 1–3 M | FTO:3.5 PTO:2.5 |
FTO was more effective than PTO. |
| Singh et al (2008)4 | RCT | India | 7–12 | AA, SA, MA | All waking hours n = 25 | 6 h n = 25 |
Less than 2 h n = 25 |
18 W | FTO:3.6 PTO (2–6 h): 3.00 PTO (<2 h): 0.17 |
PTO (2–6) and FTO were more effective than two hours occlusion therapy. |
RCT: Randomized controlled trial, AA: Anisometropic amblyopia, SA: Strabismic amblyopia, MA: Mixed amblyopia, FTO: Full-time Occlusion, PTO: Part-time Occlusion, W: Weeks, Y: Years, hrs: Hours, M: Months, PEDIG: Pediatric Eye Disease Investigator Group.
Table 2.
Quality assessment of the randomized clinical studies.
| Article | Randomization method | Similarity of the groups | Aside from the allocated treatment, were groups treated equally? | Intention to treat? Lost to follow-up? | Objective measures? Blinding? |
|---|---|---|---|---|---|
| PEDIG (2003a)17 | Permuted-blocks design of varying block sizes, with a separate sequence of computer-generated random numbers for each clinical site. | Yes | Yes | Yes 18/157 |
Yes NA |
| Stewart (2007)24 | Using a random number generator in the statistical package “R” (www.r-project.org/), stratified, but not blocked, by type of amblyopia and implemented by means of a concealed typed allocation list. | Yes | Yes | Yes 10/90 |
Yes NA |
| Singh et al (2008)4 | Computer-generated random numbers | Yes | Yes | NA NA |
Yes NA |
NA: Not Available.
PEDIG: Pediatric Eye Disease Investigator Group.
Table 3.
Quality assessment of observational studies.
| Article | Inclusion criteria | Comparability | Outcome
|
|---|---|---|---|
| PEDIG (2003b)34 |
|
NA |
|
| Arikan et al (2005)15 |
|
The mean age at start of treatment was significantly higher for anisometropic amblyopia |
|
| Hug (2004)13 |
|
NA |
|
NA: Not Available.
PEDIG: Pediatric Eye Disease Investigator Group.
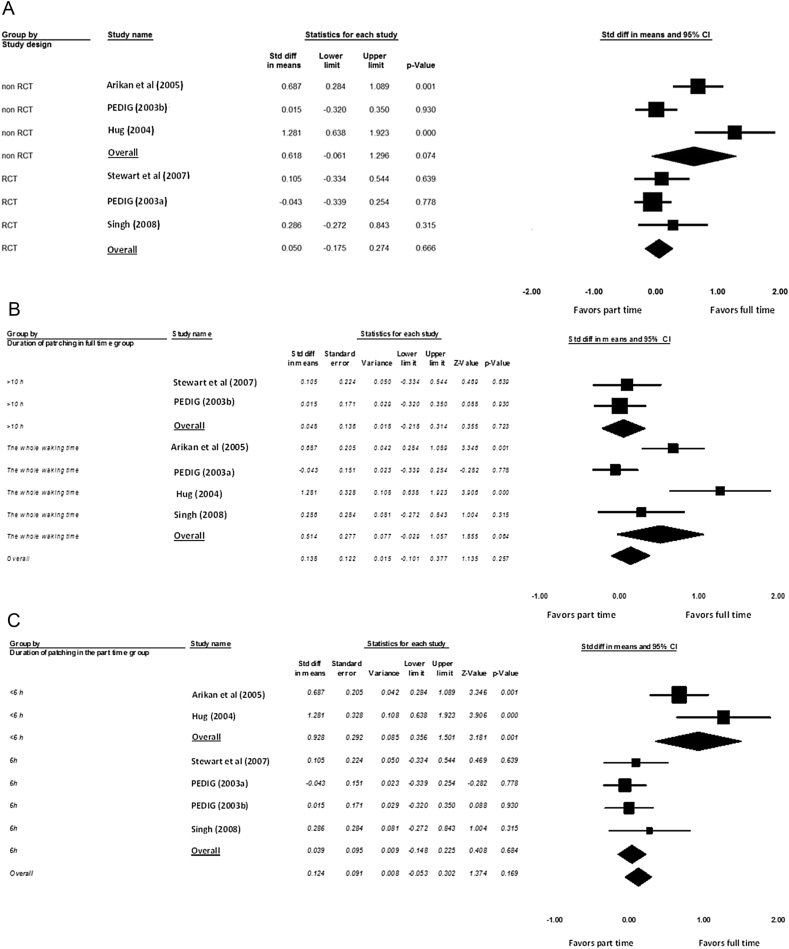
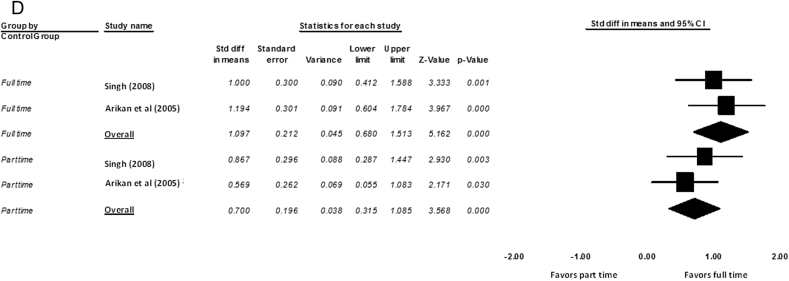
Pooled standardized difference in means of changes in the visual acuity was 0.337 [lower and upper limits: −0.009, 0.683] higher in the FTO as compared to the PTO group (P = 0.056, Cochrane Q value = 20.4 (P = 0.001), I2 = 75.49%), although this difference did not reach statistical significance. Fig. 2, Fig. 3 show the forest and funnel plots of this main analysis. Egger's regression intercept was 5.46, P = 0.04.
Fig. 2.
(A): Random-effect meta-analysis according to study design. (B): Random effects meta-analysis according to the duration of occlusion in the full-time group (>10 hrs and all waking hours). (C): Random effects meta-analysis according to the duration of part-time occlusion. (D): Random effects meta-analysis according to less than two hours of occlusion (minimal) analysis. PEDIG: Pediatric Eye Disease Investigator Group.
Fig. 3.
Funnel plot of standard error by standard difference in means. PEDIG: Pediatric Eye Disease Investigator Group.
Fig. 2A shows that in two of the non-RCT studies, the FTO was significantly better than PTO (P = 0.001 and P < 0.001). However, considering all non-RCT studies, this difference did not reach statistical significance (P = 0.074). Fig. 2A also illustrates that the FTO was not statistically different from PTO occlusion (P = 0.666) in RCT design studies.
Fig. 2B shows that FTO (considering both >10 hrs per day and all waking hours per day) was not statistically different from PTO (P = 0.257).
Fig. 2C shows that FTO and PTO of 2–6 h were significantly different (P = 0.001), however, the difference between FTO and PTO equal to 6 h did not reach statistical significance (P = 0.684).
Subgroup analyses according to the study design and duration of occlusion can be found in Table 4.
Table 4.
Subgroup analysis based on the study design and duration of patching.
| Variables | RCTs | Non-RCTs | FTO |
PTO |
||
|---|---|---|---|---|---|---|
| More than 10 hrs | All waking hrs | Equal to 6 hrs | Less than 6 hrs | |||
| Pooled Standardized difference in: means [lower and upper limits] P value [reference] |
0.105 [−0.334, 0.544] 0.63924 |
0.687 [0.284, 1.089] 0.00115 |
0.105 [−0.334, 0.544] 0.63924 |
0.687 [0.284, 1.089] 0.00115 |
0.105 [−0.334, 0.544] 0.63924 |
0.687 [0.284, 1.089] 0.00115 |
| −0.043 [−0.339, 0.254] 0.77817 |
0.015 [−0.320, 0.350] 0.93034 |
0.015 [−0.320, 0.350] 0.93034 |
−0.043 [−0.339, 0.254] 0.77817 |
−0.043 [−0.339, 0.254] 0.77817 |
1.281 [0.638, 1.923] <0.00113 |
|
| 0.286 [−0.272, 0.843] 0.3154 |
1.281 [0.638, 1.923] <0.00113 |
1.281 [0.638, 1.923] <0.00113 |
0.015 [−0.320, 0.350] 0.93034 |
|||
| 0.286 [−0.272, 0.843] 0.3154 |
0.286 [−0.272, 0.843] 0.3154 |
|||||
P value indicates the significance level of difference between modalities of occlusion therapy for each study. FTO: Full-time Occlusion, PTO: Part-time Occlusion, RCTs: Randomized control trials. hrs: Hours. Numbers in superscript formats refer to the reference (see bibliography).
Two studies evaluated PTO of less than two hours compared to the PTO of 2–6 hrs and FTO (>10 hrs/day) methods.15, 18 Pooled standardized difference in means of visual acuity changes was 1.097 [lower and upper limits: 0.68, 1.513] higher in the FTO arm (P = 0.0000002), and 0.7 [lower and upper limits: 0.315–1.085] higher in the PTO (2–6 h) arm (P = 0.0003) as compared to PTO less than two hours. Fig. 2D shows that both FTO and PTO (2–6 hrs) were statistically different compared to PTO (less than 2 hrs) (P < 0.001).
Discussion
This systematic review shows no statistically significant difference between PTO and FTO in treatment of amblyopia, although the mean improvement in visual acuity was clinically higher in FTO compared to PTO group (Fig. 2A). However, according to the results presented in this meta-analysis, the minimum effective PTO to observe maximal improvement in visual acuity is six hours per day (Fig. 2C and D).
According to the quality assessment of this meta-analysis, all included studies had very high heterogeneity (Fig. 3). This systematic review found that in RCT studies there was no significant difference between FTO and PTO. However, in observational studies, the therapeutic effect was statistically higher in FTO group compared to PTO group. Hence, the study design appears to influence the results, and the level of evidence plays an important role in heterogeneity of studies.
Studies differed significantly with respect to the duration of occlusion in PTO group. Consistent with previous findings,13, 15 results presented in this meta-analysis illustrated that PTO groups with 2–6 hrs occlusion showed lower therapeutic effect in comparison with FTO group. PTO of less than two hours appeared to be much less effective than FTO. However, there was no significant difference in visual acuity between PTO of 6 hrs and FTO. In addition, the duration of occlusion in FTO group (>10 hrs or all waking hours) did not have a significant effect on the pooled effect size.
The success of any treatment modality depends on its acceptability to the patient and, in the case of amblyopia, also to the parents or other principal caregivers. This issue is certainly true about the occlusion therapy for amblyopia. One important factor associated with successful occlusion therapy is the length of the treatment course as this is an important factor in compliance with treatment. Aside from the duration of the treatment course, another important aspect relating to compliance is the number of occlusion hours per day. Considerable variation in compliance has been reported with change of the occlusion dose, with higher doses of occlusion being associated with more variation in compliance.17, 24, 25 The nature of the interaction between daily dose and overall treatment duration has been studied; for example, one study found that most children achieved their best visual acuity with 150–250 hrs cumulative dose.26
Monitoring the occlusion dose is an important factor when judging the compliance with prescribed treatment. This is not something which is practical in clinical settings. Studies on the different types of amblyopia (anisometropic, strabismic and mixed) using objective occlusion dose monitoring have shown that the actual amount of occlusion undertaken is often considerably less than the amount prescribed.27, 28, 29 These findings highlight one advantage of prescribing FTO, because of the chance that the patient has occluded the sound eye for at least several hours.
Different criteria for a successful therapeutic outcome have been used in the different studies, for example achieving a specific level of visual acuity, including best corrected visual acuity of at least 20/70 (6/18),30 20/80 (6/24),31 20/25 (6/7.5),32 and 20/50 (6/15).33 When such different criteria are used, it becomes very difficult to compare the efficacy of different treatment modalities. In order to identify the optimum treatment regimen, the Pediatric Eye Disease Investigator Group (PEDIG) designed multi-center randomized clinical trials on children younger than 7 years old with either strabismic or anisometropic amblyopia.17, 25, 34 They stated their criterion for success as visual acuity of at least 20/32 or a gain of 3+ lines of visual acuity in the amblyopic eye at 4 months after initiation of therapy. Their purpose was to compare prescribed patching regimens of 2 hrs daily PTO to 6 hrs daily PTO in patients with moderate amblyopia,25 and prescribed patching regimens of 6 hrs daily PTO to FTO in those with severe amblyopia.17 Moderate and severe amblyopia were defined as visual acuity 20/40–20/80 and 20/100–20/400, respectively.17, 25 In the moderate amblyopia study, similar visual acuity outcomes were reported between the two PTO regimens of 2 and 6 hrs daily. Specifically, they found an equal percentage (62%) of patients in both groups who were ‘successfully’ treated at 4 months after initiation of therapy. Notably, however, there were more patients with visual acuity of 20/25 or better in the prescribed 6-hrs PTO group at the time of last follow-up.25 Comparing FTO and PTO in moderate amblyopia, they have also illustrated that increasing the occlusion time is more valuable (e.g. mean line change in PTO (6 hrs) and FTO: 3.1 and 3.3 lines, respectively).24 Thus, if the treatment goal is to obtain better visual acuity following treatment, it may be that longer daily doses of occlusion provide greater chances of success. If so, this would be consistent with the results of the current review and meta-analysis.
Visual acuity outcomes were reported between patients prescribed 6 hrs daily PTO and those prescribed FTO in the severe amblyopia study.17 There was a slight improvement in visual acuity in the patched eye in the PTO group but not in the FTO group, (e.g. mean line change in PTO (6 hrs) and FTO: 0.5 and 0.1, respectively); however, this difference was attributed by the authors to a learning effect, and felt to be unlikely due to occlusion amblyopia. This effect was transient and resolved on further follow-up. There were no differences between the two groups in terms of parent-reported ease of compliance or social stigma. This led to the PEDIG recommendation that patients with severe amblyopia should be prescribed 6 hrs of daily PTO.17 Because these studies compared prescribed patching duration and not what was actually undertaken, it is possible that the patients prescribed FTO actually wore the patch significantly less than full-time, with the result that the difference in amount of occlusion undertaken may not be as large as conceived by the designers of the study. If the latter is true, it would account for the similarity in treatment outcome of the PTO (6 hrs) and the FTO groups.17 This study suggests that PTO (6 hrs) is just as beneficial as FTO. FTO carries with a number of disadvantages including the fact that vision may be extremely poor in the affected eye making it very difficult to pursue normal living practices. Also, there is the possibility of occlusion amblyopia of the sound eye14, 16 and a greater likelihood that the child will experience negative psychosocial emotions,35 for example as a result of bullying at school, because the patching cannot only take place at home.36 Since PTO (6 hrs) appears to be just as effective as FTO, many of the disadvantages of FTO can be avoided it seems.
Our review suggests that PTO of 6 hrs per day is the minimum occlusion duration consistent with maximal treatment effect. Six hours per day still represents a considerable portion of a child's day. There has been much recent research interest in alternative (i.e. non atropine- or occlusion-based) approaches to treating amblyopia. In particular, recent technological approaches indicate similar treatment effects for active treatment of amblyopia compared to the occlusion.37, 38, 39 Notably, these treatment effects seem to accrue in much shorter durations. The methods being examined include use of the perceptual learning technique, in combination with dichoptic presentation of video games on a computer or electronic tablet. However, these newer approaches have not yet become part of standard clinical treatment of amblyopes, even in the developed world and, because of their greater (compared to occlusion therapy) financial cost, it is unlikely they will be in widespread use anytime soon. In the meantime, occlusion therapy remains more affordable and more feasible option for most countries.
Finally, this systematic review of literature shows that PTO and FTO have the same effect on treatment of amblyopia. However, according to the results presented in this meta-analysis, the minimum effective time to observe maximal improvement in visual acuity is six hours of PTO per day.
This study has some limitations. The studies included eyes with different inclusion criteria and variable length of follow-up. Therefore, any conclusion is limited by the characteristics of the studies. The only method in order to avoid publication bias is searching a broad number of databases to locate all possible studies. We did our best to increase the sensitivity of our search strategy. However, publication bias is a major concern in all systematic reviews and cannot be avoided altogether. Citation bias is always a concern in systematic reviews. However, we only used citation analysis as an adjunct to the main search strategy.
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
Disclosure: The authors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Hashemi H., Yekta A., Jafarzadehpur E. The prevalence of amblyopia in 7-year-old schoolchildren in Iran. Strabismus. 2014;22(4):152–157. doi: 10.3109/09273972.2014.971824. [DOI] [PubMed] [Google Scholar]
- 2.Chia A., Dirani M., Chan Y.-H. Prevalence of amblyopia and strabismus in young Singaporean Chinese children. Investig Ophthalmol Vis Sci. 2010;51(7):3411–3417. doi: 10.1167/iovs.09-4461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman D.S., Repka M.X., Katz J. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months: the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116(11):2128–2134. doi: 10.1016/j.ophtha.2009.04.034. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams C., Northstone K., Howard M., Harvey I., Harrad R.A., Sparrow J.M. Prevalence and risk factors for common vision problems in children: data from the ALSPAC study. Br J Ophthalmol. 2008;92(7):959–964. doi: 10.1136/bjo.2007.134700. [DOI] [PubMed] [Google Scholar]
- 5.Bhola R., Keech R.V., Kutschke P., Pfeifer W., Scott W.E. Recurrence of amblyopia after occlusion therapy. Ophthalmology. 2006 11;113(11):2097–2100. doi: 10.1016/j.ophtha.2006.04.034. [DOI] [PubMed] [Google Scholar]
- 6.Tsirlin I., Colpa L., Goltz H., Wong A. Plasticity in adult amblyopia: a meta-review and analysis. J Vis. 2015 Sep 1;15(12):656. [Google Scholar]
- 7.Khan T. Is there a critical period for amblyopia therapy? results of a study on older anisometropic amblyopes. J Clin Diagn Res JCDR. 2015;9(8):NC01–NC04. doi: 10.7860/JCDR/2015/13277.6288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noorden V. In: Binocular Vision and Ocular Motility. Lampert R., editor. 2002. [Google Scholar]
- 9.Barrett B.T., Bradley A., Candy T.R. The relationship between anisometropia and amblyopia. Prog Retin Eye Res. 2013;36:120–158. doi: 10.1016/j.preteyeres.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flynn J.T., Cassady J.C. Current trends in amblyopia therapy. Ophthalmology. 1978;85(5):428–450. doi: 10.1016/s0161-6420(78)35651-7. [DOI] [PubMed] [Google Scholar]
- 11.Taylor K., Elliott S. Interventions for strabismic amblyopia. Cochrane Database Syst Rev. 2014;7:CD006461. doi: 10.1002/14651858.CD006461.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grisham Ga. Butterworth-Heinemann; 2010. Binocular Anomalies: Diagnosis and Vision Therapy. [Google Scholar]
- 13.Hug T. Full-time occlusion compared to part-time occlusion for the treatment of amblyopia. Optometry. 2004;75(4):241–244. doi: 10.1016/s1529-1839(04)70051-2. [DOI] [PubMed] [Google Scholar]
- 14.Scott W.E., Kutschke P.J., Keech R.V., Pfeifer W.L., Nichols B., Zhang L. Amblyopia treatment outcomes. J AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus/Am Assoc Pediatr Ophthalmol Strabismus. 2005;9(2):107–111. doi: 10.1016/j.jaapos.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Arikan G., Yaman A., Berk A.T. Efficacy of occlusion treatment in amblyopia and clinical risk factors affecting the results of treatment. Strabismus. 2005;13(2):63–69. doi: 10.1080/09273970590922682. [DOI] [PubMed] [Google Scholar]
- 16.Longmuir S., Pfeifer W., Scott W., Olson R. Effect of occlusion amblyopia after prescribed full-time occlusion on long-term visual acuity outcomes. J Pediatr Ophthalmol Strabismus. 2013;50(2):94–101. doi: 10.3928/01913913-20121127-01. [DOI] [PubMed] [Google Scholar]
- 17.Pediatric Eye Disease Investigator Group A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110(11):2075–2087. doi: 10.1016/j.ophtha.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Singh I., Sachdev N., Brar G.S., Kaushik S. Part-time occlusion therapy for amblyopia in older children. Indian J Ophthalmol. 2008;56(6):459–463. doi: 10.4103/0301-4738.43365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins J.P.T., Green S. 2011. Cochrane Handbook for Systematic Reviews of Interventions.http://handbook.cochrane.org/chapter_9/9_4_3_1_random_effects_dersimonian_and_laird_method_for.htm Available from: [Google Scholar]
- 20.Huedo-Medina T.B., Sanchez-Meca J., Marin-Martinez F., Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 21.Song F., Khan K.S., Dinnes J., Sutton A.J. Asymmetric funnel plots and publication bias in meta-analyses of diagnostic accuracy. Int J Epidemiol. 2002;31(1):88–95. doi: 10.1093/ije/31.1.88. [DOI] [PubMed] [Google Scholar]
- 22.Centre for Evidence-Based Medicine. Critical Appraisal. www.cebm.net/index.aspx?o=1157 [updated (last accessed 22 November 2015)].
- 23.Wells G.A., Shea B., O'Connell D. Ottawa Health Research Institute; Ottawa (ON): 1999. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses. [Google Scholar]
- 24.Stewart C.E., Stephens D.A., Fielder A.R., Moseley M.J., Cooperative R. Objectively monitored patching regimens for treatment of amblyopia: randomised trial. BMJ. 2007;335(7622):707. doi: 10.1136/bmj.39301.460150.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Repka M.X., Beck R.W., Holmes J.M. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121(5):603–611. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 26.Stewart C.E., Stephens D.A., Fielder A.R., Moseley M.J., Cooperative M. Modeling dose-response in amblyopia: toward a child-specific treatment plan. Investig Ophthalmol Vis Sci. 2007;48(6):2589–2594. doi: 10.1167/iovs.05-1243. [DOI] [PubMed] [Google Scholar]
- 27.Stewart C.E., Fielder A.R., Stephens D.A., Moseley M.J. Treatment of unilateral amblyopia: factors influencing visual outcome. Investig Ophthalmol Vis Sci. 2005;46(9):3152–3160. doi: 10.1167/iovs.05-0357. [DOI] [PubMed] [Google Scholar]
- 28.Loudon S.E., Polling J.R., Simonsz H.J. A preliminary report about the relation between visual acuity increase and compliance in patching therapy for amblyopia. Strabismus. 2002;10(2):79–82. doi: 10.1076/stra.10.2.79.8143. [DOI] [PubMed] [Google Scholar]
- 29.Awan M., Proudlock F.A., Gottlob I. A randomized controlled trial of unilateral strabismic and mixed amblyopia using occlusion dose monitors to record compliance. Investig Ophthalmol Vis Sci. 2005;46(4):1435–1439. doi: 10.1167/iovs.04-0971. [DOI] [PubMed] [Google Scholar]
- 30.Robb R.M., Mayer D.L., Moore B.D. Results of early treatment of unilateral congenital cataracts. J Pediatr Ophthalmol Strabismus. 1987;24(4):178–181. doi: 10.3928/0191-3913-19870701-07. [DOI] [PubMed] [Google Scholar]
- 31.Birch E.E., Stager D.R. Prevalence of good visual acuity following surgery for congenital unilateral cataract. Arch Ophthalmol. 1988;106(1):40–43. doi: 10.1001/archopht.1988.01060130046025. [DOI] [PubMed] [Google Scholar]
- 32.Lundvall A., Kugelberg U. Outcome after treatment of congenital unilateral cataract. Acta Ophthalmol Scand. 2002;80(6):588–592. doi: 10.1034/j.1600-0420.2002.800606.x. [DOI] [PubMed] [Google Scholar]
- 33.Drummond G.T., Scott W.E., Keech R.V. Management of monocular congenital cataracts. Archives Ophthalmol. 1989;107(1):45–51. doi: 10.1001/archopht.1989.01070010047025. [DOI] [PubMed] [Google Scholar]
- 34.Pediatric Eye Disease Investigator Group The course of moderate amblyopia treated with patching in children: experience of the amblyopia treatment study. Am J Ophthalmol. 2003;136(4):620–629. doi: 10.1016/s0002-9394(03)00392-1. [DOI] [PubMed] [Google Scholar]
- 35.Webber A.L., Wood J.M., Gole G.A., Brown B. Effect of amblyopia on self-esteem in children. Optom Vis Sci. 2008;85(11):1074–1081. doi: 10.1097/OPX.0b013e31818b9911. [DOI] [PubMed] [Google Scholar]
- 36.Williams C., Horwood J., Northstone K., Herrick D., Waylen A., Wolke D. The timing of patching treatment and a child's wellbeing. Br J Ophthalmol. 2006;90(6):670–671. doi: 10.1136/bjo.2006.091082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li R.W., Ngo C., Nguyen J., Levi D.M. Video-game play induces plasticity in the visual system of adults with amblyopia. PLoS Biol. 2011;9(8):e1001135. doi: 10.1371/journal.pbio.1001135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Levi D.M., Li R.W. Perceptual learning as a potential treatment for amblyopia: a mini-review. Vis Res. 2009;49(21):2535–2549. doi: 10.1016/j.visres.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Astle A.T., Webb B.S., McGraw P.V. Can perceptual learning be used to treat amblyopia beyond the critical period of visual development? Ophthalmic Physiol Opt. 2011;31(6):564–573. doi: 10.1111/j.1475-1313.2011.00873.x. [DOI] [PMC free article] [PubMed] [Google Scholar]