Abstract
Purpose
To compare four tonometry techniques: Goldmann applanation tonometer (GAT), Dynamic contour tonometer (DCT), Non-contact tonometer (NCT), and Ocular Response Analyzer (ORA) in the measurement of intraocular pressure (IOP) and the impact of some corneal biomechanical factors on their performance.
Methods
In this cross-sectional study, volunteers with normal ophthalmic examination and no history of eye surgery (except for uncomplicated cataract surgery) or trauma were selected. Twenty-five subjects were male, and 21 were female. The mean age was 48 ± 19.2 years. Anterior segment parameters were measured with Scheimpflug imaging. IOP was measured with GAT, DCT, NCT, and ORA in random order. A 95% limit of agreement of IOPs was analyzed. The impact of different parameters on the measured IOP with each device was evaluated by regression analysis.
Results
The average IOP measured with GAT, DCT, NCT, and ORA was 16.4 ± 3.5, 18.1 ± 3.4, 16.2 ± 3.9, and 17.3 ± 3.4 mmHg, respectively. The difference of IOP measured with NCT and GAT was not significant (P = 0.382). Intraocular pressure was significantly different between GAT with DCT and IOPCC (P < 0.001 and P = 0.022, respectively). The 95% limit of agreement of DCT, NCT, and IOPCC with GAT was −5.7 to 2.5, −4.1 to 4.7, and −5.3–3.7 mmHg, respectively. Simple regression model corneal resistance factor (CRF) and central corneal thickness (CCT) and multivariate model CRF had a significant relationship with IOP measured with the four devices.
Conclusion
Although the mean difference of measured IOP by NCT, DCT, and ORA with GAT was less than 2 mmHg, the limit of agreement was relatively large. CCT and CRF were important influencing factors in the four types of tonometers.
Keywords: Intraocular pressure, Tonometry, Goldmann applanation tonometer, Dynamic contour tonometer, Non-contact tonometer, Ocular response analyze
Introduction
Accurate intraocular pressure (IOP) measurement has an important role in diagnosis and follow-up of patients with glaucoma. All common methods of IOP measurement are transcorneal. Hence, corneal characteristics can affect their measurements. For example, various studies have shown that goldmann applanation tonometer (GAT) gives a higher IOP in thicker corneas and a lower pressure in thinner ones. Non-contact tonometers like GAT are also seemingly affected by central corneal thickness (CCT).1, 2 On the other hand, CCT is only one of the many factors that affect transcorneal IOP measurement. Several studies indicated that other properties such as viscoelastic properties of the cornea can also have an effect on it.3
In recent years, dynamic contour tonometer (DCT) and ocular response analyzer (ORA) have been introduced as methods that are less affected by the biomechanical corneal properties.4
This study compared existing tonometers and the impact of some of corneal structural and biomechanical properties on IOP measured with GAT, DCT, non-contact tonometer (NCT), and ORA in a sample of the Iranian population.
Methods
This cross-sectional study was done in the Glaucoma Clinic of Noor Eye Hospital. Volunteers were selected among people who met the inclusion criteria. The Ethics Committee of Tehran University of Medical Sciences approved the study protocol, which was conducted in accord with the tenets of the Declaration of Helsinki. First, ophthalmology examinations including visual acuity measurement, slit-lamp examination, and fundus examination were performed. Subjects with abnormal ocular examination, history of ocular surgery (except for uncomplicated cataract surgery), and trauma were excluded. Scheimpflug imaging [Pentacam HR (Oculus, Inc., Lynnwood, WA)] was performed for qualified people by a trained technician to assess corneal curvature, radius, and topographic maps, as well as corneal thickness and volume, and depth of anterior chamber. In the next step, low coherence interferometry (IOL Master, Carl Zeiss Meditec, Germany) was performed by another technician. Since Pentacam and IOL Master are non-contact methods, they were chosen for the measurements. To minimize the possible effect of a measurement on the others, measurements with GAT, DCT, NCT, and ORA were performed in random order. Measurements with GAT were performed twice on each eye, and the average of the measurements was recorded. The test was repeated if the difference between the two measurements was more than 3 mmHg. To measure the IOP, NCT uses a very short pulse of air to applanate the cornea. The device uses an infrared light source and a sensor to receive the reflected light. When the cornea becomes flat, the sensor detects maximal light reflection, and IOP is recorded at this point. Measurements with NCT (Keeler Pulsair EasyEye tonometer, Nigeria) were performed three times, and the average value was recorded. Again, if the difference between the measurements was more than 3 mmHg, the extreme number was discarded, and another measurement was performed.
Dynamic contour tonometer (Pascal DCT, Swiss Microtechnology AG, Port, Switzerland) is a digital contact tonometer. The concave contact surface has a diameter of 7 mm, and the mean apical radius of curvature is 10.5 mm. It could be fitted on most corneas in normal range. There is a sensor at the center of the tip. When the tip of tonometer fits on the corneal surface, the sensor measures the transcorneal pressure. The assumption is that it does not cause significant distortion of the cornea and is less affected by corneal thickness and corneal curvature. IOP is shown on a digital display. In addition, it shows a number as the quality of measurement. Only measurements with a quality of 1 or 2 were accepted. If the quality was more than 2, measurements were repeated to achieve a quality of 2 or less; otherwise, the subject was excluded from the study. The ORA (Reichert Ophthalmic Instruments, Depew, NY) also uses an air pulse and a light sensor like NCT, but it records IOP at two applanation positions (inward and outward). Because of the viscoelastic properties of the cornea, inward applanation pressure and outward applanation pressure are not the same. The difference is defined as corneal hysteresis (CH) which is a measure of viscoelastic properties of the cornea. Based on CH, the device calculates the intraocular pressure as IOPCC and is claimed that it is less dependent on biomechanical properties of cornea. It also offers an IOP called IOPG, a similar IOP obtained from GAT. Another parameter is corneal resistance factor (CRF) which is calculated based on CH and a coefficient. It is an expression of corneal rigidity. A normal ORA graph has regular and relatively symmetric appearance of the peaks. The measurements with ORA were taken down by a trained technician. The measurements were done 4 times, and the average value was recorded.
Statistical analysis
Statistical analysis of this study was conducted by the Statistical Package for Social Sciences (SPSS) Version 20.0 (Chicago, IL, USA) and MedCalc V13 (MedCalc, USA).
Pearson correlation coefficient was used for showing the correlation CCT and corneal volume with CRF and CH. To demonstrate the agreement of each tonometer with GAT, Bland and Altman plot with a 95% limit of agreement was used. Paired t test was used for comparison between the two devices. Simple and multivariate linear regression analysis was used to study the relationship between factors such as corneal thickness, volume, curvature, axial length, and CRF, with IOP measured with each device. The coefficients were then reported. A P-value less than 0.05 was considered significant.
Results
Forty-six eyes of 25 males (54.3%) and 21 females (45.7%) were analyzed. The mean age of the subjects was 48 years (SD 19.2, range 18–80 years). Table 1 shows characteristics of the studied parameters.
Table 1.
Characteristics of studied parameters.
| Mean ± SD | Range | |
|---|---|---|
| SE (diopter) | −0.4 ± 1.6 | −5.5–2.3 |
| IOP-GAT (mmHg) | 16.4 ± 3.5 | 10.0–26.0 |
| IOP-NCT (mmHg) | 16.2 ± 3.9 | 9.0–26.7 |
| IOP-DCT (mmHg) | 18.1 ± 3.4 | 11.7–28.3 |
| ORA-IOPCC (mmHg) | 17.3 ± 3.4 | 11–26.2 |
| ORA-IOPG (mmHg) | 15.6 ± 4.2 | 7.2–26.5 |
| CH (mmHg) | 9.2 ± 1.6 | 5.1–12.6 |
| CRF(mmHg) | 9.5 ± 2.2 | 3.6–14.7 |
| Axial length mm | 23.9 ± 1.3 | 21.2–27.1 |
| CCT apex (μm) | 527.9 ± 36.6 | 429–610 |
| Mean K (diopter) | 43.6 ± 2.2 | 39.2–49.7 |
| Corneal volume (mm3) | 58.3 ± 4.8 | 50.7–70.9 |
| Chamber volume (mm3) | 174.7 ± 40.5 | 97–267 |
| ACD (mm) | 3.1 ± 0.6 | 2.3–4.9 |
SE: Spherical equivalent.
IOP-GAT: IOP measured by Goldmann applanation tonometer.
IOP-NCT: IOP measured by Non-contact tonometer.
IOP-DCT: IOP measured by Dynamic contour tonometer.
ORA-IOPCC: Corneal compensated IOP measured by Ocular Response Analyzer.
ORA-IOPG: Godmann correlated IOP measured by Ocular Response Analyzer.
CH: Corneal hysteresis measured by Ocular Response Analyzer.
CRF: Corneal resistance factor measured by Ocular Response Analyzer.
CCT: Central corneal thickness.
ACD: Anterior chamber depth.
Table 2 shows the relationship between the studied variables and IOP measured with the four devices. Age and sex did not have a significant relationship with the IOP measured with any device. Simple regression analysis showed that CH has a significant effect on IOP measured with NCT and IOPG. Linear regression analysis showed that CRF has a significant effect on IOP measured with all devices. The highest effect of CRF on IOP was with NCT, and the least was with IOPCC. CCT had a significant effect on IOP measured with all devices in simple regression model. The highest effect of corneal thickness was on IOP measured with IOPG followed by NCT, and the minimum effect observed with IOPCC. In a multivariate model, it was shown that only CRF had a significant correlation with IOP measured with the four devices.
Table 2.
Simple regressions analysis for intraocular pressure (IOP) and the studied variables.
| Variable | GAT |
NCT |
DCT |
IOPCC |
IOPG |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Co | P Value | Co | P Value | Co | P Value | Co | P Value | Co | P Value | |
| Age (year) | 0.02 | 0.550 | 0.01 | 0.688 | 0.02 | 0.552 | 0.04 | 0.097 | 0.04 | 0.249 |
| Gender | 0.67 | 0.520 | 1.39 | 0.230 | 1.08 | 0.293 | −0.68 | 0.510 | 0.81 | 0.518 |
| SE (Diopter) | 0.44 | 0.172 | 0.44 | 0.219 | 0.25 | 0.444 | 0.49 | 0.126 | 0.62 | 0.109 |
| CH | 0.47 | 0.137 | 0.96 | 0.005 | 0.04 | 0.908 | −0.29 | 0.369 | 0.89 | 0.018 |
| CRF | 0.99 | <0.001 | 1.25 | <0.001 | 0.71 | 0.002 | 0.67 | 0.004 | 1.55 | <0.001 |
| Axial length (mm) | −0.49 | 0.232 | −0.37 | 0.424 | −0.79 | 0.052 | −0.60 | 0.144 | −0.78 | 0.116 |
| CCT | 0.04 | 0.006 | 0.06 | <0.001 | 0.04 | 0.009 | 0.03 | 0.030 | 0.07 | <0.001 |
| mean-K | 0.27 | 0.252 | −0.08 | 0.757 | 0.22 | 0.357 | 0.29 | 0.213 | 0.18 | 0.530 |
| Corneal volume | 0.09 | 0.423 | 0.14 | 0.240 | 0.02 | 0.823 | −0.07 | 0.509 | 0.08 | 0.541 |
Co: Coefficient.
SE: Spherical equivalents.
CH: Corneal hysteresis.
CRF: Corneal resistance factor.
CCT: Central Corneal Thicknesses.
GAT: Goldmann applanation tonometer
NCT: Non-contact tonometer
DCT: Dynamic contour tonometer
IOPCC: Corneal compensated IOP
IOPG: Godmann correlated IOP
The analysis of CH and CRF relationship with studied variables showed a direct and significant relation between CH, and also CRF with CCT and corneal volume.
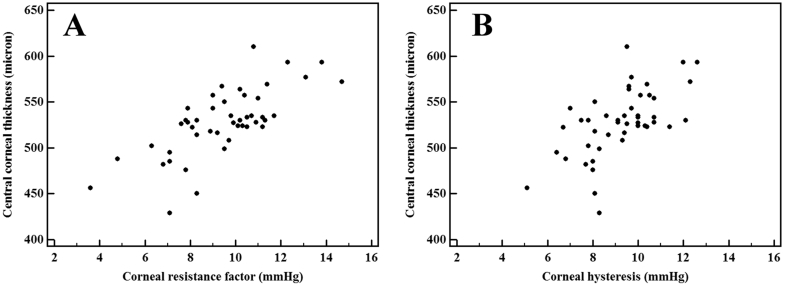
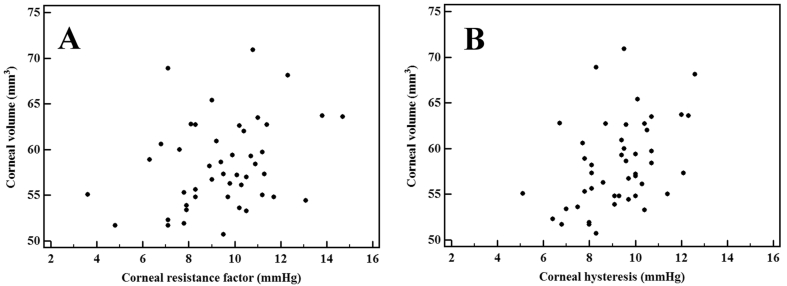
Fig. 1, Fig. 2 show the correlation between CH, and CRF with CCT and corneal volume.
Fig. 1.
Correlation between central corneal thickness (CCT) with corneal resistance factor (CRF) (A) and corneal hysteresis (CH) (B).
Fig. 2.
Correlation between corneal volume (CV) with corneal resistance factor (CRF) (A) and corneal hysteresis (CH) (B).
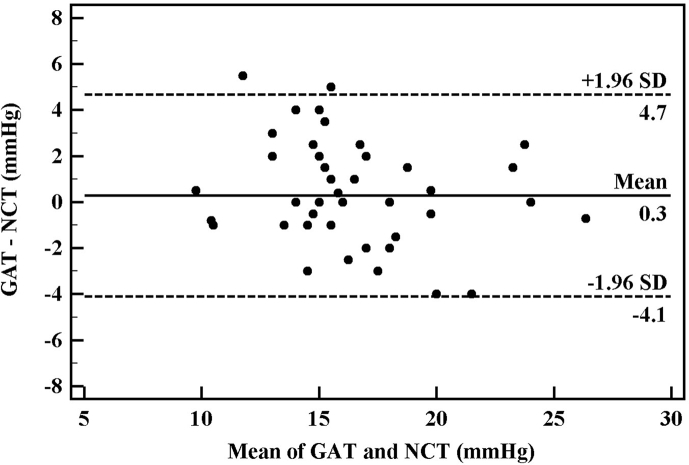
GAT and NCT
A significant correlation was observed between GAT and NCT (P < 0.001, Pearson correlation coefficient = 0.820). The IOP difference measured by the two methods was not statistically significant (0.3 ± 2.2 mmHg, P = 0.382). The 95% agreement range of IOP measured with GAT and NCT was from −4.1 to 4.7 mmHg. Fig. 3 shows the agreement of the measurements.
Fig. 3.
Agreement between Goldmann applanation tonometer (GAT) and Non-contact tonometer measurements (NCT) of the intraocular pressure (IOP). The middle line indicates the mean difference, and the two dashed side lines show the 95% limits of agreement.
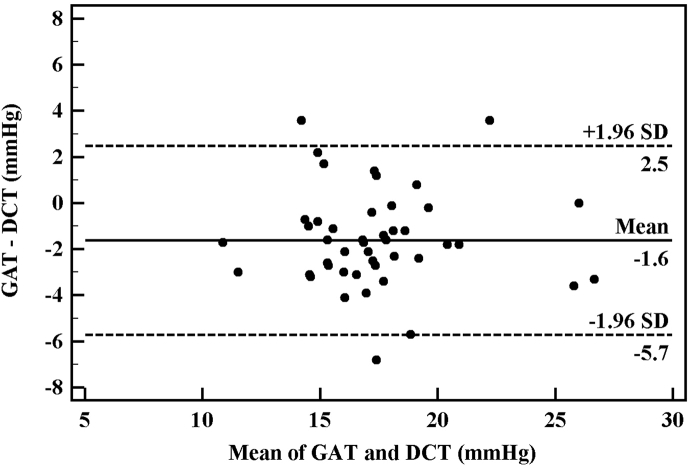
GAT and DCT
Although correlation between GAT and DCT was significant (P < 0.001, Pearson correlation coefficient = 0.812), IOP measured with GAT and DCT showed 1.6 ± 2.1 mmHg difference that was statistically significant (P < 0.001).
The 95% agreement range of IOP measured with GAT and DCT was from −5.7 to 2.5 mmHg (Fig. 4).
Fig. 4.
Agreement between Goldmann applanation tonometer (GAT) and Dynamic contour tonometer (DCT) measurements of the intraocular pressure (IOP). The middle line indicates the mean difference, and the two dashed side lines show the 95% limits of agreement.
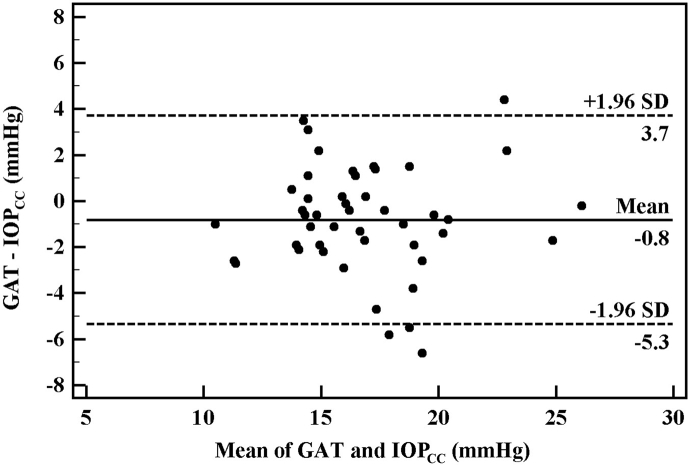
GAT and IOPCC
A comparison of measured IOP with GAT and ORA-IOPCC showed significant correlation (P < 0.001, Pearson correlation coefficient = 0.776). However, the difference in IOP measurements with GAT and ORA-IOPCC was statistically significant (0.8 ± 2.3 mmHg, P = 0.022). The 95% agreement range in IOP measurement was relatively large (from −5.3 to 3.7 mmHg) (Fig. 5).
Fig. 5.
Agreement between Goldmann applanation tonometer (GAT) and Ocular Response Analyzer (IOPCC) measurements of the intraocular pressure (IOP). The middle line indicates the mean difference, and the two dashed side lines show the 95% limits of agreement.
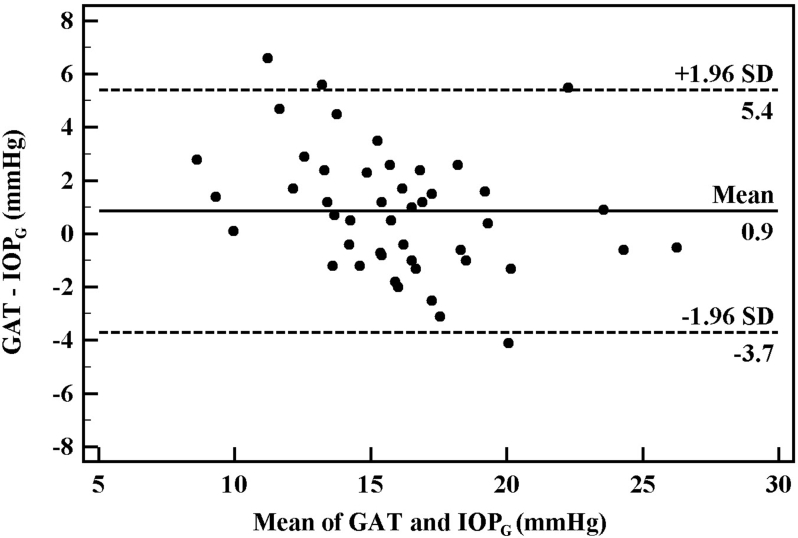
GAT and IOPG
IOP compared with GAT and IOPG showed a significant correlation (P < 0.001, Pearson correlation coefficient = 0.832). Mean and standard deviation of IOP difference measured with GAT and IOPG was 0.86 ± 2.32 mmHg, respectively (P = 0.016) and the 95% agreement range between them was from −3.7 to 5.4 mmHg (Fig. 6).
Fig. 6.
Agreement between Goldmann applanation tonometer (GAT) and Ocular Response Analyzer (IOPG) measurements of the intraocular pressure (IOP). The middle line indicates the mean difference, and the two dashed side lines show the 95% limits of agreement.
Considering Goldmann tonometer as the standard method of IOP measurement, the mathematical equations in Table 3 can be used for predicting IOP measured with each device by linear regression analysis.
Table 3.
Prediction of the measured intraocular pressure (IOP) by Non-contact tonometer (NCT), Dynamic contour tonometer (DCT), ORA IOPCC and IOPG based on GAT by linear regression analysis.
| IOP by GAT = 1.05 + IOP by NCT × 0.92 |
| IOP by GAT = 4.7 + IOP by DCT × 0.81 |
| IOP by GAT = 4.56 + IOP by IOPCC × 0.77 |
| IOP by GAT = −0.96 + IOP by IOPG × 1.01 |
GAT: Goldmann applanation tonometer
NCT: Non-contact tonometer
DCT: Dynamic contour tonometer
IOPCC: Corneal compensated IOP
IOPG: Godmann correlated IOP
Discussion
In the present study, there was no significant difference between IOP measured with GAT and NCT. Ogbuehi et al2 also reported that Topcon non-contact tonometer is similar to GAT from an accuracy and reliability point of view. CCT was one of the effective factors on IOP measured with these two devices. An increase in CCT had a significant relationship with an increase in IOP. Based on obtained regression coefficients, it seems that changes of CCT are more effective on IOP measured with NCT. The linear relationship between the IOP and CCT in our study has also been confirmed by previous studies. Babalola et al1 and Tonnu et al5 also showed that changes in IOP measured with NCT are more dependent on CCT than IOP measured by Goldmann tonometer.
In this study, IOP measured with DCT is on average 1.6 mmHg more than GAT, which was statistically significant. Pache et al6 also compared these two devices in a report and showed that measurements with DCT were 1 mmHg more than GAT. The difference between these two devices was also statistically significant (P = 0.001). In his report, the 95% agreement range of two units in IOP measurement was from −6.29 to 4.18 compared to −5.7–2.5 mmHg in the present study. In a study that compared the two units, Martinez et al7 mentioned a 4.4 mmHg difference between the two devices (P = 0.001). The populations of these two studies were different. The population of this study included normal people while Martinez studied those with open angle glaucoma. The agreement range difference between his study and the current study is obvious: he showed that the 95% agreement range of the two devices was from −0.7 to 9.5 mmHg. From these two studies, it can be suggested that in different IOP values, especially in higher values, the two units can have a different performance. The higher the IOP mean is, the more the difference between GAT and DCT will be. The present study showed the relation between IOP measured with DCT and CCT. Unlike our study, many studies7, 8, 9 reported no relationship between CCT and IOP measurements with DCT. Lee et al10 reported that IOP measured by DCT was affected by CCT only in eyes with a high CCT (more than 550 microns).
In the present study, the limits of agreement between ORA IOPcc and GAT were the largest compared to the other pairs. Although the relationship between CCT and IOP measured with ORA was statistically significant, considering their regression coefficients, it is understood that IOP measured with ORA is less affected by CCT than GAT. There is conflicting evidence regarding the effect of CCT on IOP measure by ORA. For example, Medeiros and Weinreb11 showed no significant relationship between IOP measured by ORA and CCT, but another study12 showed a weak but significant relationship. In multivariate analysis, the only effective factor on IOP was the CRF. Although CCT had a significant role in simple regression analysis, it seems that in IOP measurements, CRF has a greater effect than corneal thickness. Mollan et al13 also reported a similar result. Ang et al14 also showed the effects of these factors on IOP measured with Goldmann tonometers. He showed that IOP by GAT has a reverse relationship with CH and a direct one with CRF. Touboul et al15 emphasized that a weak CH can be a reason for overestimation of IOP measured with GAT.
In this study we found a significant relationship between CCT and corneal volume with CH and CRF (Fig. 1, Fig. 2). In another study, a positive correlation was found between CRF and CH with CCT in primary open angle glaucoma (POAG) and ocular hypertension (OHT) patients.16 Bayoumi et al17 also reported a correlation between CCT and CH and CRF. The exact contribution of CCT and corneal volume on clinically measurable biomechanical properties of cornea is not well understood and needs further investigation.
In conclusion, this study showed that individual corneal properties including CCT and CRF were important influencing factors on the performance of all four studied tonometers. Despite previous studies, our results did not show independence of DCT and ORA measurements from these corneal properties. Although the difference of mean IOP measurement by these tonometers seems clinically acceptable, the agreement limit is relatively large. More studies are needed to evaluate the effect of different individual corneal properties and their clinical relevance on the IOP measurement.
Footnotes
Financial interest: This project was supported by Iran National Science Foundation.
Conflicts of interest: No conflicting relationship exists for any author.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Babalola O.E., Kehinde A.V., Iloegbunam A.C., Akinbinu T., Moghalu C., Onuoha I. A comparison of the Goldmann applanation and non-contact (Keeler Pulsair EasyEye) tonometers and the effect of central corneal thickness in indigenous African eyes. Ophthalmic Physiol Opt. 2009;29(2):182–188. doi: 10.1111/j.1475-1313.2008.00621.x. [DOI] [PubMed] [Google Scholar]
- 2.Ogbuehi K.C. Assessment of the accuracy and reliability of the Topcon CT80 non-contact tonometer. Clin Exp Optom. 2006;89(5):310–314. doi: 10.1111/j.1444-0938.2006.00068.x. [DOI] [PubMed] [Google Scholar]
- 3.Kniestedt C., Punjabi O., Lin S., Stamper R.L. Tonometry through the ages. Surv Ophthalmol. 2008;53(6):568–591. doi: 10.1016/j.survophthal.2008.08.024. [DOI] [PubMed] [Google Scholar]
- 4.ElMallah M.K., Asrani S.G. New ways to measure intraocular pressure. Curr Opin Ophthalmol. 2008;19(2):122–126. doi: 10.1097/ICU.0b013e3282f391ae. [DOI] [PubMed] [Google Scholar]
- 5.Tonnu P.A., Ho T., Newson T. The influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, non-contact tonometry, the Tono-Pen XL, and Goldmann applanation tonometry. Br J Ophthalmol. 2005;89(7):851–854. doi: 10.1136/bjo.2004.056622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pache M., Wilmsmeyer S., Lautebach S., Funk J. Dynamic contour tonometry versus goldmann applanation tonometry: a comparative study. Ger J Ophthalmol. 2005;243(8):763–767. doi: 10.1007/s00417-005-1124-y. [DOI] [PubMed] [Google Scholar]
- 7.Martinez-de-la-Casa J.M., Garcia-Feijoo J., Vico E. Effect of corneal thickness on dynamic contour, rebound, and goldmann tonometry. Ophthalmology. 2006;113(12):2156–2162. doi: 10.1016/j.ophtha.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 8.Kaufmann C., Bachmann L.M., Thiel M.A. Comparison of dynamic contour tonometry with goldmann applanation tonometry. Invest Ophthalmol Vis Sci. 2004;45(9):3118–3121. doi: 10.1167/iovs.04-0018. [DOI] [PubMed] [Google Scholar]
- 9.Kotecha A., White E., Schlottmann P.G., Garway-Heath D.F. Intraocular pressure measurement precision with the Goldmann applanation, dynamic contour, and ocular response analyzer tonometers. Ophthalmology. 2010;117(4):730–737. doi: 10.1016/j.ophtha.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 10.Lee J., Lee C.H., Choi J. Comparison between dynamic contour tonometry and goldmann applanation tonometry. Korean J Ophthalmol. 2009;23(1):27–31. doi: 10.3341/kjo.2009.23.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Medeiros F.A., Weinreb R.N. Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzer. J Glaucoma. 2006;15(5):364–370. doi: 10.1097/01.ijg.0000212268.42606.97. [DOI] [PubMed] [Google Scholar]
- 12.Martinez-de-la-Casa J.M., Garcia-Feijoo J., Fernandez-Vidal A., Mendez-Hernandez C., Garcia-Sanchez J. Ocular response analyzer versus Goldmann applanation tonometry for intraocular pressure measurements. Invest Ophthalmol Vis Sci. 2006;47(10):4410–4414. doi: 10.1167/iovs.06-0158. [DOI] [PubMed] [Google Scholar]
- 13.Mollan S.P., Wolffsohn J.S., Nessim M. Accuracy of goldmann, ocular response analyser, pascal and tonopen XL tonometry in keratoconic and normal eyes. Br J Ophthalmol. 2008;92(12):1661–1665. doi: 10.1136/bjo.2007.136473. [DOI] [PubMed] [Google Scholar]
- 14.Ang G.S., Bochmann F., Townend J., Azuara-Blanco A. Corneal biomechanical properties in primary open angle glaucoma and normal tension glaucoma. J Glaucoma. 2008;17(4):259–262. doi: 10.1097/IJG.0b013e31815c3a93. [DOI] [PubMed] [Google Scholar]
- 15.Touboul D., Roberts C., Kerautret J. Correlations between corneal hysteresis, intraocular pressure, and corneal central pachymetry. J Cataract Refract Surg. 2008;34(4):616–622. doi: 10.1016/j.jcrs.2007.11.051. [DOI] [PubMed] [Google Scholar]
- 16.Detry-Morel M., Jamart J., Pourjavan S. Evaluation of corneal biomechanical properties with the reichert ocular response analyzer. Eur J Ophthalmol. 2010;21(2):138–148. doi: 10.5301/ejo.2010.2150. [DOI] [PubMed] [Google Scholar]
- 17.Bayoumi N.H., Bessa A.S., El Massry A.A. Ocular response analyzer and goldmann applanation tonometry: a comparative study of findings. J Glaucoma. 2010;19(9):627–631. doi: 10.1097/IJG.0b013e3181ca7e01. [DOI] [PubMed] [Google Scholar]