Abstract
Background
The relation of income and socioeconomic status with suicide rates remains unclear. Most previous studies have focused on the relationship between suicide rates and macroeconomic factors (e.g., economic growth rate). Therefore, we aimed to identify the relationship between individuals' socioeconomic position and suicide risk.
Methods
We analyzed suicide mortality rates across socioeconomic positions to identify potential trends using observational data on suicide mortality collected between January 2003 and December 2013 from 1,025,340 national health insurance enrollees. We followed the subjects for 123.5 months on average. Socioeconomic position was estimated using insurance premium levels. To examine the hazard ratios of suicide mortality in various socioeconomic positions, we used Cox proportional hazard models.
Results
We found that the hazard ratios of suicide showed an increasing trend as socioeconomic position decreased. After adjusting for gender, age, geographic location, and disability level, Medicaid recipients had the highest suicide hazard ratio (2.28; 95% CI, 1.87–2.77). Among the Medicaid recipients, men had higher hazard ratios than women (2.79; 95% CI, 2.17–3.59 vs. 1.71; 95% CI, 1.25–2.34). Hazard ratios also varied across age groups. The highest hazard ratio was found in the 40–59-year-old group (3.19; 95% CI, 2.31–4.43), whereas the lowest ratio was found in those 60 years and older (1.44; 95% CI, 1.09–1.87).
Conclusions
Our results illuminate the relationship between socioeconomic position and suicide rates and can be used to design and implement future policies on suicide prevention.
Keywords: Suicide rate, Income, Socioeconomic position
Highlights
-
•
Suicide showed an increasing trend as income levels decreased.
-
•
Suicide was most frequent in Medicaid recipients.
-
•
Suicide showed different trends across gender and age groups.
Introduction
Suicide is a global issue important enough to have prompted the World Health Organization to announce the Mental Health Action Plan in 2013 in an effort to reduce suicide rates worldwide.1 Addressing suicide is even more pressing in South Korea, where the national suicide rate has been the highest of all Organization for Economic Co-operation and Development (OECD) countries in the last decade. The rate of death by suicide in Korea is at 28.5 per 100,000 people in 2013, which is as much as 5 times higher than other OECD countries (OECD on average, 12.1; Italia, 5.8; United States, 12.5; and Japan, 20.9 per 100,000 people).2 The number of individuals who attempted suicide within the last year is 7.5 times the rate of actual suicide deaths during that same period, while the number of individuals who have attempted suicide more than once in their lifetime is 10.7 times that rate. These figures indicate that there is currently a high-risk population comprising about 1.2 million individuals with a history of suicide attempts.3 Consequently, a great deal of research is being conducted in South Korea on how to address this suicide problem. About 851 academic thesis papers on suicide, covering a wide range of subjects and causes, were published between 1966 and 2014.4
Suicide rates are thought to be affected by economics, an assumption rooted in the work of Durkheim.5 Many scholars have reported a correlation between economic factors and suicide rates in Korea,6, 7, 8, 9, 10, 11, 12 and researchers of various countries have also reported the impact of economic factors on suicide.13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 However, it is difficult to make definite conclusions about this relation because contradictory results are continually emerging.25, 26 Due to limited data and various other reasons, the majority of existing studies on economic factors and suicide rates have focused on the relationship in terms of macroeconomic factors, such as economic growth rate, unemployment rate, and income disparity,10, 11, 12, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 or have suggested the influence of individuals' economic circumstances on suicidal ideation and attempts.6, 7, 8, 9, 13, 14 Therefore, we sought to identify the relationship between individuals' socioeconomic position (SEP) and suicide hazard ratios (HRs) using retrospective cohort data collected from about 1 million Koreans over 11 years. We also tried to find out the impact of SEP on suicide HRs across gender and age groups because Korea shows a different pattern of age-specific suicide rates compared to other OECD countries.4 Kim et al have also reported that suicidal ideation differed by gender.6 For these reasons, we aimed to identify HRs of suicide across SEPs and to identify trends in HRs of suicide across gender and age groups.
Methods
Ethics statement
The current study was reviewed by the institutional review board of Seoul National University Hospital. Because we utilized only secondary data, the approval process was waived. All data were encoded to protect subjects' privacy.
Data
We used the National Health Insurance Service-National Sample Cohort data, which was built using National Health Insurance claims data provided by the National Health Insurance Service. In Korea, the healthcare system consists of national health insurance and medical aid that covers almost all Koreans. The total number of registrants was approximately 51,878,000 as of June 2015, and the coverage rate of this healthcare system was about 100%.27 The National Health Insurance Service-National Sample Cohort data were sampled from the 2002 database of qualified people for national health insurance and medical aid using a proportional allocation, with stratified sampling according to gender, age, and income. The dataset consists of demographic information (gender, age, and region), income quantiles, disability levels, causes of death, and date of death. We used the data established from January 2003 to December 2013, and we analyzed 1,017,468 subjects out of 1,025,340, after excluding those with missing data.
SEP measurement
The insurance premium in Korea can be considered a proxy indicator for SEP. Therefore, prior studies in Korea have used insurance premium levels as an SEP indicator.28, 29 For this reason, the current study also used SEP criteria created using insurance premiums of the National Health Insurance System. South Korea's national health insurance is compulsory and universal, and offers three types of coverage: workplace health insurance (for employees), community insurance (for self-employed), and Medicaid (for those who do not qualify for workplace or community insurance). As of June 2015, 69.6% of Koreans were enrolled in workplace insurance, 27.7% in community insurance, and 2.7% in Medicaid.27 For workplace insurance, the premium is calculated based on the individual's monthly wage, whereas community insurance premiums are calculated according to the individual's household income (including monthly income and assets, such as property, vehicles owned, and other valuables). All calculations of premiums utilize the average income earned during the previous 12 months; the premiums for individuals without an income source (e.g., homemakers and students) depend on the income of principal enrollees (i.e., the people supporting these individuals financially), for whom the same methods of calculation apply. To calculate insurance premiums, income is divided into deciles, with the 1st to 4th deciles being low SEP, the 5th to 8th deciles being middle SEP, and the 9th and 10th deciles being high SEP; individuals with no income receive healthcare coverage through the Medicaid system. These classification criteria were based on those of the Ministry of Land.30
Statistical analysis
In January 2003, the total number of subjects included in the study was 1,017,468. Monitoring began in January 2003 and ended in December 2013. During the monitoring period, we found 2791 cases of suicide mortality. The length of survival for each individual was calculated in months. Each suicide death was processed as “1” and each non-suicide as “0”. The latter includes those censored in the survival analysis. Suicide deaths were classified as X60–X84 according to the International Statistical Classification of Diseases and Related Health Problems (ICD)-10. Geographical location was classified according to administrative districts, which are divided into nine provinces and seven metropolitan cities. Thus, we classified the geographical location as “Metropolitan city” or “Province”. In order to clarify the HRs of suicide associated with age, subjects were stratified by age group (10–19, 20–39, 40–59, and ≥60 years) for the analysis. This classification of age groups was based on research by Kim et al.6
To examine the independent effect of SEP on suicide rates, we included age, gender, geographic location, and disability level as control variables. All variables were categorized, including age, and their relations with income were evaluated individually. And we have created stepwise models that includes related variables. To analyze suicide HRs across SEPs, we used Cox proportional hazard models. This method does not assume any particular distribution because it is impossible to presume a theoretical distribution regarding subjects' survival time. As such, the method is advantageous in the sense that the data's baseline hazard function provides a stable estimate of coefficients. However, to apply the Cox model, which measures the baseline hazard function's proportional changes dependent on the independent variable's influence, it is worthwhile to confirm the proportionality assumption — namely, that the independent variable's HR is indeed independent of time.31 We confirmed this assumption via a correlation analysis of the independent variable's Schoenfeld residuals and the variable representing the order of incidents. Using the Cox proportional hazard model, HRs and 95% confidence intervals (CIs) were obtained while controlling for gender, age, geographical location, and disability level. Statistical significance level was two-sided at P < 0.05, and all analyses were performed with SPSS version 21 (IBM SPSS Inc., Chicago, IL, USA).
Results
The demographic characteristics (age, geographical location, disability level, and SEP) of the 1,017,468 subjects are presented in Table 1. The geographical location was composed of nine provinces: Gyonggi, Gangwon, Chungbuk, Chungnam, Jeonbuk, Jeonnam, Gyeongbuk, Gyeongnam, and Jeju; and seven metropolitan cities: Seoul, Busan, Daegu, Inchon, Gwangju, Daejon, and Ulsan. Subjects were followed for 10.3 years on average. The median follow-up period was 132 months, with a minimum period of 1 month and maximum period of 132 months. During the follow-up period, we found 2791 cases of suicide mortality during a total of 10,469,881 person-years. The suicide rate showed an increasing trend with decreasing SEP (Table 2).
Table 1.
General characteristics of study subjects by gender.
| Male |
Female |
|
|---|---|---|
| n = 509,213 (50.1%) | n = 508,255 (49.9%) | |
| Age, years | ||
| Pre-adolescent (0–9 years) | 67,755 (13.4) | 61,286 (12.1) |
| Adolescent (10–19 years) | 73,451 (14.4) | 65,925 (13.0) |
| 20 s | 82,447 (16.2) | 80,809 (15.9) |
| 30 s | 94,662 (18.6) | 91,179 (17.9) |
| 40 s | 87,349 (17.2) | 83,624 (16.5) |
| 50 s | 49,385 (9.7) | 49,594 (9.8) |
| 60 s | 35,786 (7.0) | 42,005 (8.3) |
| 70 s | 14,063 (0.8) | 23,546 (4.6) |
| ≥80 | 4315 (0.8) | 10,287 (2.0) |
| Geographical locations | ||
| Metropolitan city | 240,590 (47.2) | 240,586 (47.3) |
| Province | 268,623 (52.8) | 267,669 (52.7) |
| Disability level | ||
| None | 488,579 (95.9) | 497,623 (97.9) |
| Moderate disability | 6470 (1.3) | 4133 (0.8) |
| Mild disability | 14,164 (2.8) | 6499 (1.3) |
| Socioeconomic position | ||
| Medicaid recipients | 13,410 (2.6) | 18,279 (3.6) |
| Low | 133,130 (26.1) | 143,283 (28.2) |
| Middle | 224,343 (44.1) | 212,855 (41.9) |
| High | 138,330 (27.2) | 133,838 (26.3) |
Table 2.
Suicide rates across socioeconomic position groups.
| Socioeconomic position | n | Suicide cases | Person-years | Suicide rate (per 100,000 person-years) | 95% confidence interval | |
|---|---|---|---|---|---|---|
| High | 10th decile | 138,059 | 271 | 1,427,360.5 | 18.99 | 16.83–21.35 |
| 9th decile | 134,109 | 310 | 1,386,140.7 | 22.36 | 19.98–24.96 | |
| Middle | 8th decile | 126,207 | 278 | 1,302,842.9 | 21.34 | 18.94–23.96 |
| 7th decile | 114,555 | 261 | 1,183,292.5 | 22.06 | 19.50–24.86 | |
| 6th decile | 102,898 | 262 | 1,066,953.3 | 24.56 | 21.71–27.67 | |
| 5th decile | 93,538 | 266 | 969,873.7 | 27.43 | 24.28–30.88 | |
| Low | 4th decile | 82,505 | 264 | 850,819.4 | 31.03 | 27.45–34.95 |
| 3rd decile | 71,153 | 205 | 732,698.3 | 27.98 | 24.34–32.01 | |
| 2nd decile | 61,962 | 227 | 633,214.9 | 35.85 | 31.41–40.75 | |
| 1st decile | 60,793 | 271 | 613,498.3 | 44.17 | 39.15–49.67 | |
| Medicaid recipients | 31,689 | 176 | 303,186.4 | 58.05 | 49.94–67.12 | |
Hazard ratios across socioeconomic positions
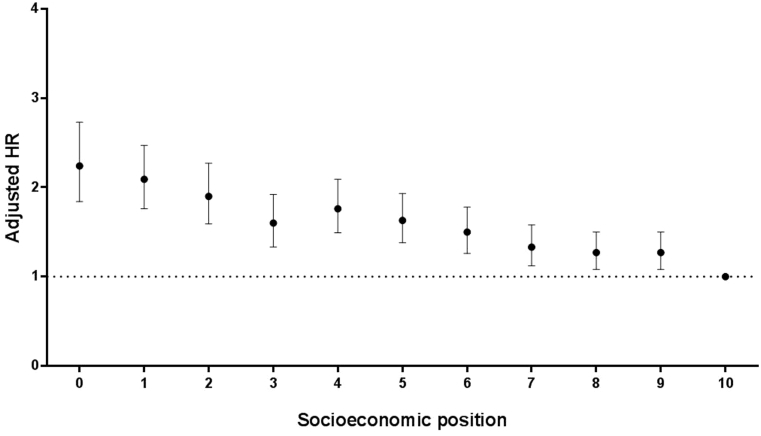
In models 1, 2, and 3, HRs of suicide according to SEP showed a similar trend. After adjusting for gender, age, geographic location, and disability level, the highest HR of suicide was found in Medicaid recipients compared to 10th-decile subjects (2.28; 95% CI, 1.87–2.77) (Table 3), and the HRs of suicide showed an increasing trend with decreasing SEP (Fig. 1). After considering the interaction of gender*SEP and age*SEP, significantly high HRs were observed among Medicaid recipients, as well as those in the 1st, 2nd, and 4th deciles compared to those in the 10th decile (Table 3).
Table 3.
Hazard ratios across socioeconomic positions.
| Socioeconomic position | Hazard ratio (95% confidence interval) |
|||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2a | Model 3b | Model 4c | Model 5d | ||
| High | 10th decile | 1 | 1 | 1 | 1 | 1 |
| 9th decile | 1.17 (1.00–1.39)* | 1.30 (1.10–1.53)* | 1.27 (1.08–1.50)* | 1.08 (0.82–1.42) | 1.15 (0.88–1.50) | |
| Middle | 8th decile | 1.12 (0.95–1.33) | 1.30 (1.10–1.54)* | 1.27 (1.08–1.50)* | 1.27 (0.97–1.66) | 1.22 (0.93–1.61) |
| 7th decile | 1.16 (0.98–1.38) | 1.37 (1.16–1.63)** | 1.33 (1.12–1.58)** | 1.04 (0.78–1.40) | 1.31 (0.98–1.75) | |
| 6th decile | 1.29 (1.09–1.53)* | 1.54 (1.30–1.83)** | 1.50 (1.26–1.78)** | 1.29 (0.97–1.72) | 1.30 (0.95–1.77) | |
| 5th decile | 1.44 (1.22–1.71)** | 1.69 (1.42–2.00)** | 1.63 (1.38–1.93)** | 1.18 (0.87–1.60) | 1.36 (0.99–1.86) | |
| Low | 4th decile | 1.64 (1.38–1.94)** | 1.83 (1.55–2.17)** | 1.76 (1.49–2.09)** | 1.42 (1.06–1.90)* | 1.61 (1.20–2.16)* |
| 3rd decile | 1.47 (1.23–1.76)** | 1.66 (1.38–1.99)** | 1.60 (1.33–1.92)** | 1.31 (0.97–1.78) | 1.33 (0.95–1.85) | |
| 2nd decile | 1.89 (1.59–2.56)** | 1.97 (1.65–2.35)** | 1.90 (1.59–2.27)** | 1.38 (1.01–1.88)* | 1.47 (1.08–2.01)* | |
| 1st decile | 2.33 (1.97–2.76)** | 2.20 (1.86–2.60)** | 2.09 (1.76–2.47)** | 1.46 (1.10–1.93)* | 1.62 (1.24–2.11)** | |
| Medicaid recipients | 3.10 (2.54–3.72)** | 2.60 (2.15–3.15)** | 2.24 (1.84–2.73)** | 1.62 (1.19–2.20)* | 1.39 (1.03–1.87)* | |
*P < 0.05, **P < 0.001.
Age was categorized into 10–19, 20–39, 40–59, and ≥60 years in the interaction.
Adjusted for gender and age.
Adjusted for gender, age, geographical location, and disability level.
Adjusted for gender, age, geographical location, disability level, and interaction (gender*SEP).
Adjusted for gender, age, geographical location, disability level, and interaction (age*SEP).
Fig. 1.
Hazard ratios across socioeconomic positions (in deciles, with 0 representing Medicaid recipients). HRs adjusted for gender, age, geographical location, and disability level. HR, hazard ratio.
HRs across socioeconomic positions stratified by gender
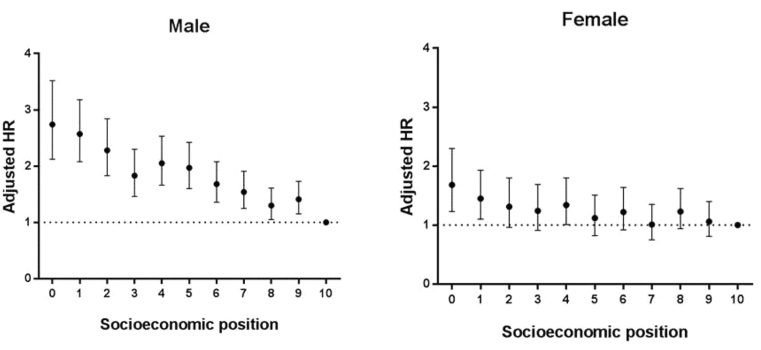
Overall, a similar trend was shown between crude and adjusted HRs. However, the overall trend of HRs of suicide according to SEP differed between genders (Table 4). Males showed significantly high HRs in almost all SEP groups, whereas females only showed significantly high HRs in the Medicaid recipients group and among those in the 1st and 4th deciles of SEP (Fig. 2).
Table 4.
Hazard ratios across socioeconomic positions, stratified by gender.
| Socioeconomic position | Hazard ratio (95% confidence interval) |
||||
|---|---|---|---|---|---|
| Men |
Women |
||||
| Model 1 | Model 3a | Model 1 | Model 3a | ||
| High | 10th decile | 1 | 1 | 1 | 1 |
| 9th decile | 1.29 (1.05–1.58)* | 1.41 (1.15–1.73)* | 1.00 (0.76–1.31) | 1.06 (0.81–1.40) | |
| Middle | 8th decile | 1.14 (0.92–1.41) | 1.30 (1.05–1.61)* | 1.10 (0.84–1.44) | 1.23 (0.94–1.62) |
| 7th decile | 1.33 (1.08–1.64)* | 1.54 (1.25–1.91)** | 0.88 (0.66–1.18) | 1.01 (0.75–1.35) | |
| 6th decile | 1.43 (1.16–1.76)* | 1.68 (1.36–2.08)** | 1.06 (0.80–1.42) | 1.22 (0.92–1.64) | |
| 5th decile | 1.71 (1.39–2.10)** | 1.97 (1.60–2.42)** | 1.00 (0.74–1.35) | 1.12 (0.82–1.51) | |
| Low | 4th decile | 1.87 (1.51–2.30)** | 2.05 (1.66–2.53)** | 1.27 (0.95–1.71) | 1.34 (1.01–1.80)* |
| 3rd decile | 1.70 (1.36–2.13)** | 1.83 (1.46–2.30)** | 1.19 (0.87–1.61) | 1.24 (0.91–1.69) | |
| 2nd decile | 2.32 (1.87–2.88)** | 2.28 (1.83–2.84)** | 1.34 (0.98–1.82) | 1.31 (0.96–1.80) | |
| 1st decile | 2.97 (2.40–3.66)** | 2.57 (2.08–3.18)** | 1.75 (1.33–2.32)** | 1.45 (1.10–1.93)* | |
| Medicaid recipients | 3.73 (2.93–4.76)** | 2.74 (2.12–3.52)** | 2.62 (1.93–3.55)** | 1.68 (1.23–2.30)* | |
*P < 0.05, **P < 0.001.
Adjusted for age, geographical location, and disability level.
Fig. 2.
Hazard ratios across socioeconomic positions (in deciles, with 0 representing Medicaid recipients stratified by gender. HRs adjusted for age, geographical location, and disability level. HR, hazard ratio.
Hazard ratios across socioeconomic positions stratified by age groups
Overall, a similar trend of HRs was shown between crude and adjusted HRs. Compared to the high SEP group, the HRs of suicide according to SEP were found to be different across age groups (Table 5). First, the HR was higher in Medicaid recipients than those with high SEP for all age groups. However, in the 10–19-year age group, significantly increased HRs were not shown in the middle and low SEP groups. In the 20–39-year age group, HRs were shown to be significantly increased across all SEP groups; for middle SEP subjects, the HR was 1.28 (95% CI, 1.04–1.68), while it was 1.88 (95% CI, 1.54–2.34) for low SEP subjects and 2.91 (95% CI, 1.86–4.49) for Medicaid recipients, after adjusting for gender, geographical location, and disability level. A similar trend was observed among subjects in the 40–59-year age group. For subjects aged ≥60 years, the HR was not higher in the middle SEP than the high SEP. However, it differed from low SEP/Medicaid subjects (1.37; 95% CI, 1.15–1.63 for low SEP subjects and 1.44; 95% CI, 1.09–1.87for Medicaid subjects).
Table 5.
Hazard ratios across socioeconomic positions, stratified by age groups.
| Socioeconomic position | Hazard ratio (95% confidence interval) |
|||
|---|---|---|---|---|
| 10–19 years |
20–39 years |
|||
| Model 1 | Model 3a | Model 1 | Model 3a | |
| High | 1 | 1 | 1 | 1 |
| Middle | 1.29 (0.87–1.92) | 1.31 (0.88–1.95) | 1.29 (1.05–1.60)* | 1.27 (1.03–1.56)* |
| Low | 1.44 (0.92–2.25) | 1.46 (0.93–2.28) | 1.93 (1.57–2.38)** | 1.87 (1.51–2.30)** |
| Medicaid recipients |
2.73 (1.48–5.01)* |
2.78 (1.50–5.20)** |
4.31 (2.90–6.40)** |
2.82 (1.81–4.39)** |
| Socioeconomic position | 40–59 years | 60 years and older | ||
| Model 1 | Model 3a | Model 1 |
Model 3a |
|
| High | 1 | 1 | 1 | 1 |
| Middle | 1.42 (1.19–1.69)** | 1.40 (1.17–1.66)** | 1.17 (0.98–1.39) | 1.13 (0.94–1.34) |
| Low | 1.66 (1.39–1.99)** | 1.70 (1.42–2.04)** | 1.40 (1.17–1.66)** | 1.37 (1.15–1.63)* |
| Medicaid recipients | 3.32 (2.48–4.45)** | 3.05 (2.22–4.19)** | 1.31 (1.01–1.71)* | 1.44 (1.10–1.89)* |
*P < 0.05, **P < 0.001.
Adjusted for gender, geographical location, and disability level.
Discussion
We examined the HRs of suicide across SEPs while controlling for various demographic factors, including gender, age, geographic location, and disability level. There were the HRs of suicide among all SEP (i.e., Medicaid recipients and 1st to 9th deciles subjects). After considering the interaction between the variables (gender and age) and SEP, significantly high HRs were observed for Medicaid recipients, as well as those in the 1st, 2nd, and 4th deciles compared to 10th-decile subjects. However, the HRs of suicide by gender showed different correlations with SEP. HRs of suicide differed significantly across age groups. Subjects in the 20–39-year and 40–59-year age groups showed higher HRs of suicide across SEPs, whereas adolescent subjects showed a significantly high HR only in the Medicaid recipients group compared to the high SEP group. In subjects aged ≥60 years, income had a relatively weak effect on suicide risk. However, our results should be interpreted cautiously because mental illnesses, such as depression and alcoholism, or physical conditions may have caused the suicide deaths. We could not include all variables (including depression) that potentially contribute to suicidal behavior due to the limits of our dataset. Therefore, it is rational to consider that low SEP is a factor contributing to suicide.
Previous studies have suggested a link between suicide and various macroscopic factors. Bando et al reported that suicide risk is higher in low-income communities.18 Inoue et al reported that suicide rates were associated with household disposable income.32 Furthermore, Suzuki reported that changes in income level have an effect on individuals' suicide decisions.33 However, it is difficult to identify individual-level factors of suicide through a macroscopic perspective. Therefore, in our study, we confirmed HRs of suicide across SEPs to identify suicide factors at an individual level. As a result, HRs of suicide increased with decreasing SEP, even after controlling for gender, age, and geographical location. This study also found that the relation between suicide risk and SEP differed slightly by gender, with the relation being stronger in males than females. Kim et al also reported that suicidal ideation differed by gender,6 a finding which highlights the importance of considering gender in suicide prevention efforts.
HRs of suicide for different SEPs varied across age groups, with subjects in the 20–39-year and 40–59-year age groups showing relatively high ratios across all SEPs. Kim et al examined factors influencing suicidal thoughts across age groups and found that household income was a risk factor for suicidal thoughts among subjects in these same age groups, whereas it did not have a significant influence on subjects ≥60 years.6 In the 10–19-year age group of the current study, a significantly increased risk was shown in the Medicaid recipients, but not in middle- and low-SEP groups. In subjects aged ≥60 years, income had relatively weak effects on HRs in the low-SEP group and in Medicaid recipients. A study by Lee concerning the influence of income level on suicide risk among adolescents aged 10–19 years identified emotional state, drug use, use of alcohol, and exposure to violence as significant contributors to suicide attempts, rather than socioeconomic factors,34 while Chong & Jeong reported domestic violence, school violence, and academic difficulties as major risk factors of suicide in teenagers.35 However, Park & Jang noted that adolescents' suicide risk increased when their parents were welfare recipients,36 a finding which supports the current study's results regarding the high suicide risk among adolescent subjects in the Medicaid group. Kim et al reported that more diverse factors contribute to suicidal thoughts in the elderly, such as educational level, history of depression, tobacco use, health status, diet and nutrition, and whether or not they have a surviving spouse.37 Erlangsen et al reported that health problem, such as complex physical conditions, contribute to suicidal thoughts in the elderly,38 while Chong & Jeong presented both financial crises and health status as factors influencing suicidal thoughts in the elderly.35 Taken together, our findings suggest that it is worth noting how the effects of income on suicide risk vary across ages. According to the Korean statistics bureau's data, the suicide rates among individuals in their 30 s and 40 s is continuing to increase, while the suicide rates per 100,000 population over the ages of 60, 70, and 80 are 37.5, 57.6, and 78.6, respectively, all of which are significantly higher than the population average of 27.3.39 Thus, suicide-prevention efforts for individuals in their 30 s and 40 s should consider the effects of economic factors, while those for individuals ≥60 years should target mental and physical health, as well as SEP. We also need to consider the possibility that the high welfare budget currently set aside for the elderly may have contributed to the reduced effect of economic factors on suicidal thoughts in the elderly.40 Nevertheless, incorporating these findings into future suicide-prevention policies may be useful in terms of choosing the target subjects and methods of intervention.
The present study has a few limitations. SEP for people without an income source (e.g., some women, children, and elderly) were calculated using the income of principal enrollees. Although prior studies also used this method,28, 29 there has been a debate about the validity of SEP indicators using the income of principal enrollees. We classified the geographical location by administrative districts. This classification of geographical location was composed of finer classification of 16 districts; however, it may not accurately characterize the geographical location of all study subjects. Despite these limitations, our study found that the HR of suicide showed an increasing trend with decreasing SEP, and the effects of SEP on suicide risk are higher in males than females. HRs of suicide are particularly high among individuals in the 20–39-year and 40–59-year age groups. Thus, additional research that considers this issue is needed. In addition, consideration should be given to factors that protect people with low SEP.
The current study offers data regarding the link between SEP and suicidal behavior, which can be used to design and implement future suicide-prevention policies. For instance, Japan has taken a social reinforcement approach to suicide prevention, through which support is provided using community suicide-prevention funds, phone counseling for individuals with multiple debts, loan services and counseling support for low-income individuals, and welfare loan services. Some 10 government agencies are cooperating closely with these efforts to establish adequate suicide-prevention policies.41 In South Korea, although a suicide prevention act and related policies are being implemented, the policy scope is considered rather limited to mental health projects focusing on individuals, and socioeconomic support is lacking.42 The current study results indicate that economic factors must be considered in suicide-prevention efforts, and that suicide is a problem for all socioeconomic levels. In other words, because suicide is not an issue solely rooted in either psychology or economic hardship, a bio-psycho-social approach is necessary to understand it.
Therefore, various government agencies, in addition to public health and healthcare sectors, will have to cooperate closely to address this issue. In particular, because the effects of SEP on suicide HRs are greater among individuals in the 20–39-year and 40–59-year age groups, further in-depth research regarding these age groups' suicide risks and how they relates to SEP is necessary to suggest a clearer direction for policies.
Funding
The authors have no external funding sources for this study.
Conflicts of interest
None declared.
Footnotes
Peer review under responsibility of the Japan Epidemiological Association.
References
- 1.World Health Organization . World Health Organization; Geneva: 2013. Mental Health Action Plan 2013−2020. [Google Scholar]
- 2.Organization for Economic Co-operation and Development.org [homepage on the Internet]. OECD Health Data 2013. [cited 2015 June 30]. Available from: http://www.oecd-ilibrary.org/social-issues-migration-health/suicides_20758480-table10.
- 3.Jeon H.J. Epidemiologic studies on depression and suicide. J Korean Med Assoc. 2012;55(4):322–328. [in Korean] [Google Scholar]
- 4.Korea Suicide Prevention Center . Ministry of Health and Welfare; Korea: 2014. Suicide White Book. [Google Scholar]
- 5.Durkheim E. The Free Press; New York: 1996. On Suicide: a Study in sociology [1897] Translated by JA Spaulding and G. Simpson. [Google Scholar]
- 6.Kim S.Y., Jung M.Y., Kim K.N. Factors associated with suicidal ideation by age group among Korean adults using the fifth Korea national health and nutrition examination survey. Korean J Health Educ Promot. 2014;31(2):1–14. [in Korean] [Google Scholar]
- 7.Kim J.W., Kwon S.M. The impact of regional employment unstability on suicide rate in the younger generation. Soc Secur Res. 2014;30(2):117–141. [in Korean] [Google Scholar]
- 8.Woo H.K., Cho Y.T. Poverty dynamics and suicidal ideation. Pub Health Soc Sci. 2013;34:5–35. [in Korean] [Google Scholar]
- 9.Um H.J., Jun H.J. Predictive factors for mid-aged male and female adults' suicidal ideation. Ment Health Soc Work. 2014;42(2):35–62. [in Korean] [Google Scholar]
- 10.Kim S.W., Choi S.M. Evaluation of growth-oriented macroeconomic policies: relationship among growth, distribution, and social indicators. J Korean Soc Trend Persp. 2014;91:262–295. [in Korean] [Google Scholar]
- 11.Lee M.A., Kang J.H. Changes in suicide rates and social integration in Korea: a community-level panel data analysis. Korea J Pop Stud. 2014;37(2):1–19. [in Korean] [Google Scholar]
- 12.Ham W.S. A study on the factors affecting suicide in the Republic of Korea. Korea Law Enforc Res. 2014;12(3):375–402. [in Korean] [Google Scholar]
- 13.Kalist D.E., Molinari N.A., Siahaan F. Income, employment and suicidal behavior. J Ment Health Policy Econ. 2007;10(4):177–187. [PubMed] [Google Scholar]
- 14.Nock M.K., Borges G., Bromet E.J. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen J., Choi Y.J., Sawada Y. How is suicide different in Japan? Jpn World Econ. 2009;21(2):140–150. [Google Scholar]
- 16.Chuanc H.L., Huang W.C. Economic and social correlates of regional suicide rates: a pooled cross-section and time-series analysis. J Socio Econ. 1997;26(3):277–289. [Google Scholar]
- 17.Koo J., Cox W.M. An economic interpretation of suicide cycles in Japan. Contemp Econ Policy. 2008;26(1):162–174. [Google Scholar]
- 18.Bando D.H., Brunoni A.R., Benseñor I.M., Lotufo P.A. Suicide rates and income in Sao Paulo and Brazil: a temporal and spatial epidemiologic analysis from 1996 to 2008. BMC Psychiatry. 2012;12(1):127. doi: 10.1186/1471-244X-12-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andres A.R. Income inequality, unemployment, and suicide: a panel data analysis of 15 European countries. Appl Econ. 2005;37(4):439–451. [Google Scholar]
- 20.Milner A., McClure R., De Leo D. Socioeconomic determinants of suicide: an ecological analysis of 35 countries. Soc Psychiatry Psychiatr Epidemiol. 2012;47(1):19–27. doi: 10.1007/s00127-010-0316-x. [DOI] [PubMed] [Google Scholar]
- 21.Rehkopf D.H., Buka S.L. The association between suicide and the socioeconomic characteristics of geographical areas: a systematic review. Psychol Med. 2006;36(02):145–157. doi: 10.1017/S003329170500588X. [DOI] [PubMed] [Google Scholar]
- 22.Suzuki E., Kashima S., Kawachi I., Subramanian S.V. Prefecture-level economic conditions and risk of suicide in Japan: a repeated cross-sectional analysis 1975–2010. Eur J Public Health. 2014;24(6):949–954. doi: 10.1093/eurpub/cku023. [DOI] [PubMed] [Google Scholar]
- 23.Rezaeian M., Dunn G., St Leger S., Appleby L. Ecological association between suicide rates and indices of deprivation in the north west region of England: the importance of the size of the administrative unit. J Epidemiol Comm Health. 2006;60(11):956–961. doi: 10.1136/jech.2005.043109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith N.D.L., Kawachi I. State-level social capital and suicide mortality in the 50 US states. Soc Sci Med. 2014;120:269–277. doi: 10.1016/j.socscimed.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 25.Saurina C., Bragulat B., Saez M., López-Casasnovas G. A conditional model for estimating the increase in suicides associated with the 2008–2010 economic recession in England. J Epidemiol Comm Health. 2013;67:779–787. doi: 10.1136/jech-2013-202645. [DOI] [PubMed] [Google Scholar]
- 26.Mackenbach J.P., Looman C.W. Changing patterns of mortality in 25 European countries and their economic and political correlates, 1955–1989. Int J Pub health. 2013;58(6):811–823. doi: 10.1007/s00038-013-0509-7. [DOI] [PubMed] [Google Scholar]
- 27.National Health Insurance Corporation.org [homepage on the Internet]. National Health Insurance Corporation data. [cited 2015 November 01]. Available from: http://www.nhis.or.kr/menu/retriveMenuSet.xx?menuId=B2220.
- 28.Khang Y.H., Bahk J., Yi N., Yun S.C. Age-and cause-specific contributions to income difference in life expectancy at birth: findings from nationally representative data on one million South Koreans. Eur J Public Heal. 2015;128 doi: 10.1093/eurpub/ckv128. [DOI] [PubMed] [Google Scholar]
- 29.Jung-Choi K., Khang Y.H., Cho H.J. Socioeconomic differentials in cause-specific mortality among 1.4 million South Korean public servants and their dependents. J Epidemiol Comm Health. 2011;65(7):632–638. doi: 10.1136/jech.2009.100651. [DOI] [PubMed] [Google Scholar]
- 30.Ministry of Land, Transport and Maritime Affairs. Housing Survey. Ministry of Land, Transport and Maritime Affairs; Korea: 2012. [Google Scholar]
- 31.Allison P.D. Survival analysis. In: Hancock G.R., Mueller R.O., editors. The Reviewer's Guide to Quantitative Methods in the Social Sciences. Routledge; New York: 2010. pp. 413–425. [Google Scholar]
- 32.Inoue K., Nishimura Y., Okazazi Y., Fukunaga T. Discussion based on analysis of the suicide rate and the average disposable income per household in Japan. West Indian Med J. 2014;63(4):344–347. doi: 10.7727/wimj.2012.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Suzuki T. How will a risk of income fluctuations influence the suicidal decision making? Insights from a three-period model of suicide. Eurasian Econ Rev. 2015;5(2):1–13. [Google Scholar]
- 34.Lee G.Y. Factors influencing attempted suicide among adolescents in Korea. J Korea Acad Ind Coop Soc. 2015;16(5):139–147. [in Korean] [Google Scholar]
- 35.Chong Y.S., Jeong Y.J. A review on variables related to suicide of the Korean youth and elderly: an application of vulnerability stress model to suicide. Korean J Dev Psychol. 2015;28(3):227–254. [in Korean] [Google Scholar]
- 36.Park D.H., Jang S.N. Influence of parental socioeconomic status on stress, depression and suicidal ideation among Korean adolescents. J Korea Acad Ind Coop Soc. 2013;14(6):2667–2676. [in Korean] [Google Scholar]
- 37.Kim K.H., Kim J.S., Lee B.S., Lee E.K., Ahn Y.M., Choi M.H. A study about the factors affecting the suicidal thought in Korean elders. J Korean Acad Psychiatr Ment Health Nurs. 2010;19(4):391–399. [in Korean] [Google Scholar]
- 38.Erlangsen A., Stenager E., Conwell Y. Physical diseases as predictors of suicide in older adults: a nationwide, register-based cohort study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(9):1427–1439. doi: 10.1007/s00127-015-1051-0. [DOI] [PubMed] [Google Scholar]
- 39.Korea National Statistical Office. [homepage on the Internet]. 2014 Cause-of-Death Statistics Results. [cited 2015 October 30]. Available from: http://kosis.kr/statisticsList/statisticsList_01List.jsp?vwcd=MT_ZTITLE&parentId=D#SubCont.
- 40.Park DH. Welfare budget per elderly KRW 1.3 million; 5 times that of teenagers. The 300. [Internet]. 2015 Nov [cited 2015 Nov 12]. Available from: http://the300.mt.co.kr/newsView.html?no=2015111004547648558 [in Korean].
- 41.Lee C.J., Kim S.G. National Assembly Budget Office; Korea: 2013. Issue of Suicide Prevention Projects and Improvement Projects. [Google Scholar]
- 42.Kang E.J., Lee S.H. Korea Institute for Health and Social Affairs; Korea: 2010. Causes of Suicide and Prevention: Beyond the Psychiatric Approach. [Google Scholar]