Abstract
Iodine deficiency remains a considerable challenge worldwide, even after decades of efforts to address the problem. The aim of this review is to present the current situation in historically iodine-deficient Pakistan regarding iodine nutritional status and place it in a global perspective. We collected relevant articles from online bibliographic databases and websites of concerned organizations that addressed prevalence of goiter/iodine deficiency and barriers to sustainable control. We divided the studies into pre- and post-1994, a landmark year when Pakistan formally adopted the universal salt iodization (USI) programme. Overall, 56 studies reported goiter/iodine deficiency prevalence in Pakistan. Before 1994, six studies (30%) reported a goiter prevalence ≥70%, while nine studies (45%) reported a goiter prevalence between 30% and 70%. Only five studies (25%) found a goiter prevalence less than 30%, of which only two studies reported prevalence <10%. From 1994 onwards, 15 studies (41.7%) reported a goiter/iodine deficiency (ID) prevalence ≥50%, of which seven studies reported prevalence ≥70%, while three studies (8.3%) found a goiter prevalence of 30%–49%, nine studies (25%) found a goiter prevalence of 10%–29%, and five studies (13.9%) reported prevalence of <10%. Four studies (11.1%) reported lower goiter prevalence but higher prevalence of iodine deficiency. The efforts in the past two decades resulted in up to a 50% decline in iodine deficiency disorders (IDD). Variable remaining factors and the recent results, however, indicate that this decline may be non-uniform and even over-estimated. Coordinated and regionally adopted efforts for eradication of IDD from all stakeholders should be pursued. Policy makers should take steps to protect future generations and alert concerned organizations about the importance of careful assessments and estimates of iodine nutritional status.
Keywords: Iodine deficiency disorder, Goiter prevalence, Iodine nutritional status, Salt iodization, Pakistan
Highlights
-
•
Since 1880, 58.9% of 56 studies reported goiter/iodine deficiency prevalence ≥30%.
-
•
Seventy five percent of studies reported ≥30% goiter prevalence before 1994.
-
•
From 1994 onwards, 32.1% of studies reported goiter/iodine deficiency prevalence ≥30%.
Introduction
Iodine deficiency remains a serious concern around the world even after decades of tremendous efforts targeting the problem.1 In 2008, economists participating in the Copenhagen Consensus ranked universal salt iodization (USI) as third on the list of the 10 biggest challenges in advancing global welfare.2 The International Child Development Steering Group has identified iodine deficiency as one of four key global health factors related to impaired child development.3 Even today, more than 1.88 billion people globally have inadequate iodine intake, and 241 million of them are children,4 who are at risk of the detrimental effects of iodine deficiency, including endemic goiter, cretinism, intellectual impairment, growth retardation, neonatal hypothyroidism, pregnancy loss, and infant mortality.1
Iodine deficiency disorders (IDDs) are still a challenge for both developed and less-developed countries.5 In 2011, seven of the top 10 affected countries were in Africa, and Europe had the highest proportion (44%) of children with inadequate iodine supply worldwide.6 Even today, 30% of European countries have an inadequate iodine supply among pregnant women, with 400 million people having no or only limited access to iodized salt.5 Of the 32 countries around the world declared as iodine deficient, 11 (34%) are located in Europe.4 In particular, the iodine status of pregnant women is inadequate in 62% of the countries in western and central Europe. In the United Kingdom, studies report more than 50% of women of child-bearing age to be iodine deficient.5 Recent studies have described mild to moderate iodine deficiency in Brazil, New Zealand, and Australia in population-based studies.5, 7, 8 Overall, 11 out of 54 African countries with available data, including Ethiopia, Algeria, Sudan, Morocco, and Ghana, are iodine deficient.6
Historically, iodine deficiency has been a public health problem in the Eastern Mediterranean Region (EMR) countries, particularly in Afghanistan, Algeria, Iraq, Iran, Morocco, Saudi Arabia, Sudan, Yemen, and Pakistan.9, 10, 11, 12, 13, 14, 15, 16 Iran took the first initiative in the region in 1989 and established the Iranian National Committee for control of IDD. Since then, Iran has conducted regular monitoring every 5 years. Afterwards, other countries of that region also initiated iodine prophylaxis. As a result, by 2004, 90% of the households in six countries of EMR were supplied with adequately iodized salt, and two countries, Iran and Tunisia, had already declared as IDD-free by World Health Organization-East Mediterranean Regional Office (WHO-EMRO) in 2000.17 However, some recent statistics still indicate high prevalence of goiter (10%–65%) in some of the countries (United Arab Emirates, Tunisia, Jordan, Lebanon, and Egypt).18, 19
Pakistan has seen a notable improvement in recent times20; however, the estimated decline in IDD may not be uniform and is possibly over-estimated in most parts of the country. The ultimate reason is lack of proper planning, political will, and monitoring. An effective and sustained program for the control and elimination of iodine deficiency, followed by periodic monitoring of the relevant indicators, are essential steps to achieve a sustainable IDD control programme. This may ultimately result in optimization of urinary iodine concentrations (UIC), following elimination of IDD.21 The aim of this review is to present the current situation and related figures for Pakistan regarding iodine nutritional status and to place these factors in a global perspective. The overall conclusions should motivate policy makers and concerned organizations to focus on careful assessments and estimates of iodine nutritional status.
Methods
Literature search
We searched general and specialized bibliographic databases including Medline, POPLINE, EMBASE, Index Medicus, and CAB. We also searched the websites of ministries of health in all provinces, various governmental and national and international non-governmental organizations (NGOs) for relevant reports and articles. In addition, we searched for publications of the Iodine Global Network (IGN), formerly known as the International Council for Control of Iodine Deficiency Disorders (ICCIDD). Reference lists of the identified articles were screened, and some additional publications were sourced from these bibliographies. We searched from December 2014 to March 2015. We did not apply language restrictions during search and selection of the articles. We used various combinations of the following terms: iodine, deficiency, supplementation, fortification, nutrition, salt, household, usage, laws, legislation, goiter, survey, study, school age children, thyroid, TSH, side effects, cost, myths, maternal, fetus, and Pakistan.
Selection criteria
Potentially eligible data included journal articles and published information from government or other agencies. Relevant articles were selected after reading through all titles and abstracts, and full texts were obtained if the information contained in the title or abstract was insufficient. We shortlisted only those articles which addressed the prevalence and severity of goiter/iodine deficiency and/or barriers to sustainable control, based on the recommended WHO and IGN guidelines. The studies were divided into the pre-1994 era (when Pakistan putatively adopted a USI program) and 1994 onwards.
Results
The effectiveness of the IDD prevention program in Pakistan can be distinguished in studies conducted before and after 1994 (Table 1, Table 2). There are considerable variations in goiter prevalence and IDD in consecutive years (even within the same area),22, 23, 24, 25, 26 as well as enormous regional differences (Table 1, Table 2). Around 25% of all the studies conducted in Pakistan have reported a goiter prevalence ≥70%, 38.5% of studies reported a goiter prevalence of 30%–69%, 23.1% of studies reported a goiter prevalence of 10%–29%, and 13.5% of studies found a goiter prevalence of ≤10%. Overall, 35.7% of the studies reported iodine deficiency prevalence alone.
Table 1.
Studies representing prevalence of goiter before 1994.
| Year of study | District/region | Total goiter prevalence (%) |
Reference | |
|---|---|---|---|---|
| SAC | Whole population | |||
| 1908 | Gilgit and Chitral | ─ | 80 | 16 |
| 1927 | Dainyor (Gilgit) | 65 | 30 | |
| 1955–56 | Multan Kasur |
52.2 (41.3♂, 72.3♀) 1.9 |
31 | |
| 1960 | Chitral | 72 | 80 | |
| 1960 | Gilgit | 76 | ─ | 35 |
| 1972 | Dainyor (Gilgit) | 74 | ─ | 81 |
| 1974 | Maroi (Chitral) | 31♂, 28♀ | a49.6♂, a62♀ | 32 |
| 1978 | Shigar, Baltistan | 72 | 61 Adolescents | 33 |
| 1979–82 | Multan | ─ | 4.43 (3.6♂, 6.07♀) | 82 |
| 1980 | Shigar, Baltistan | ─ | 77 | 83 |
| 1981 | Kalam (Swat) | ─ | 21.18 | 84 |
| 1981–86 | Gilgit, Baltistan | ─ | 34.3♂,49.3♀ | 58 |
| 1987 | Islamabad | 40 | ─ | 85 |
| 1988 | Mardan | 8.8 | 26.95 | 86 |
| 1988 | Swat | 37.21 | ─ | 87 |
| 1989 | Hazara | 71 | ─ | 88 |
| 1990 | Murree | 47.4 (47.9♀, 46.5♂) | ─ | 89 |
| 1990 | Gilgit | 33.3 | ─ | 35 |
| 1990 | Lotkoh (Chitral) | 12 | ─ | 35 |
| 1992 | Gilgit, Hunza | ─ | 4.68 | 60 |
SAC, School-age children.
These values are overall percentage averages for the prevalence in the age groups ≥21, 11–12, and 0–10 years (females: 55%, 63%, and 31%; males: 85%, 73%, and 28%, respectively).
Table 2.
Studies representing prevalence of goiter from 1994 onward.
| Punjab |
KP |
Sindh |
GB |
AJK |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Region/year | SP | GP/ID (%) | Region/year | SP | GP/ID (%) | Region/year | SP | GP/ID (%) | Region/year | SP | GP/ID (%) | Region/year | SP | GP/ID (%) |
| Punjab90 1995 | ─ | 81a | Swat22 1998 | 728 | 59.2 | Sindh42 2001 | ─ | ─ | Gilgit91 1995 | ─ | 22.2 | AJK42 2001 | – | 28 |
| Rawalpindi23 2001 | 210 | 9.5 | Abbotabad49 1999 | 1628 | 23.9/35.7 | Banbhore, MK92 2005 | 1028 | 0.3 BI 2.2 AI |
Gilgit42 2001 | ─ | 34 | Bagh93 2009 | 675 | 3.0a |
| Lahore94 2004 | 1295 | 13.5a | Swat24 1999 | ─ | 70 | MKK95 2007 | 485 | 52a | Ghanche96 2005 | 120 | 100 | AJK20 2011 | 65 | 65.4 |
| Punjab42 2001 | ─ | 21 | Swat62 2000 | 960 | 52♂,45♀ | Sindh20 2011 | 307 | 35.0a | Hunza61 2011 | 2550 | 0.47 | AJK97 2014 | 100 | 20 |
| Lahore98 2003 | 350 | 60.6 | Pehawar50 2001 | ─ | 20 | Hyderabad99 2013 | 50 | 30.5 | Gilgit100 2011 | 150 125 |
27.6 BI 19.2 AI |
|||
| Rawalpindi25 2005 | 369 | 52 | KP42 2001 | ─ | 27 | Sindh101 2013 | 40aSAC 60aPW |
GB20 2011 | 29 | 70.0a | ||||
| Rawalpindi26 2006 | 508 | 57.09 | Karak102 2006 | 1426 | 47 | |||||||||
| Lahore103 2009 | 660 | 8.8 | Pehawar104 2011 | ─ | 53/45.08 | |||||||||
| Lahore36 2009 | 254 | 31.8/79.5a | Peshawar104 2011 | 122 | 53.27a | |||||||||
| Lahore105 2011 | 110 | 100 aχ | KP20 2011 | 162 | 26.0a | |||||||||
| PakPattan106 2011 | 200 | 80 | Charsadda39 2013 | 1210 | 15.8/54.7 | |||||||||
| PakPattan107 2011 | 2335 | 28.7 | Karak37 2013 | 1194 | 14.5/87.3 | |||||||||
| Punjab20 2011 | 585 | 39.3a | Kohat38 2013 | 1170 | 35/92.7 | |||||||||
| Lahore108 2012 | 293 | 24.5 | Peshawar45 2015 | 251 | 14.8 | |||||||||
KPK, Khyber Pakhtunkhwa; GB, Gilgit Baltistan; AJK, Azad Jammu and Kashmir; SP, study population; GP, goiter prevalence; ID, iodine deficiency; BI, before intervention; AI, after intervention; MK, Mirpur Khas; MKK, Matiari, Khairpur, Karachi; SAC, school age children; PW, pregnant women.
Iodine deficiency percentage.
History of iodine deficiency in Pakistan (pre-1994)
Pakistan is located in a region that traces its recorded history of iodine deficiency to 326 BCE, when Alexander commonly observed swollen necks in residents of the northern areas of present-day Pakistan.27 One of the earliest recordings of goiter was found in a scene from the life of the Buddha in Gandharan art. This sculpture originates from an ancient kingdom that was located in the northwest of present-day Pakistan.28 Formal reports of goiter prevalence in this region can be traced back to 1880, when Macnamara29 highlighted the region with fractional prevalence of goiter. More importantly, a higher goiter prevalence was observed in areas that were afterwards reported as goiter-endemic areas. Later, in 190816 and 1927,30 McCarrison identified the region as severely iodine deficient (Table 1). Shortly after independence in 1947, a local newspaper in 1954 reported epidemics of goiter in Multan, which was later confirmed in formal investigations.31
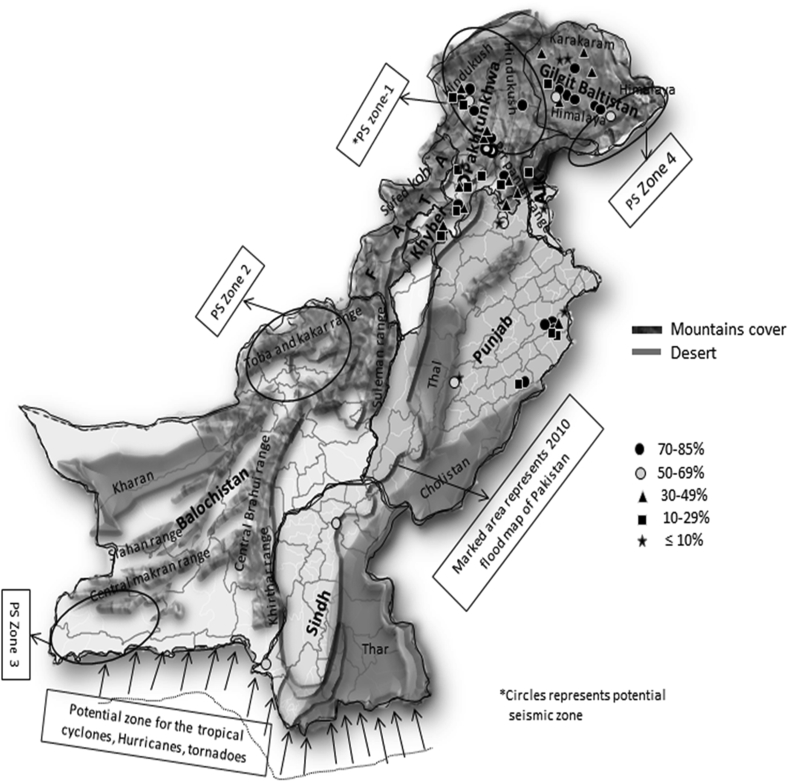
The far northern area of Pakistan, because of its mountainous characteristics and extensive network of Agha Khan Health Services (AKHS), a philonthropic organization, has been the focus of iodine deficiency-related studies before 1994. Prior to 1994, 12 of 20 studies (60%) were conducted in Gilgit-Baltistan and Chitral (Table 1 and Fig. 1). There were no reports from Federally Administered Tribal Areas (FATA), Azad Jammu and Kashmir, or Sindh and Balochistan.
Fig. 1.
Map of Pakistan showing potential natural factors influencing iodine deficiency and goiter prevalence/iodine deficiency across the country (1908–2015). No reports from Balochistan, FATA, AJK regarding prevalence of goiter, except the results of the 2011 national nutrition survey, and only a few studies conducted in Sindh province.
Before 1994, six (30%) of the total studies reported goiter prevalence above 70%, while nine studies (45%) reported prevalence above 30% (Table 1). In contrast, only three studies (15%) reported goiter prevalence of 10%–29%, while two studies (10%) reported goiter prevalence less than 10%. Two studies, which were conducted at the same time in school-age children and adolescents, reported conflicting results. One study conducted in children of the Maroi (Chitral) region showed a goiter prevalence of 31% in boys and 28% in girls in 1974, while prevalences were 49.6% in boys and 62% in girls among adolescents.32 Another study conducted in Shigar (Baltistan) in 1978 reported a goiter prevalence of 72% in school-age children and 62% in adolescents, respectively.33
The most common food fortification for iodine deficiency in Pakistan has been table salt iodization. Iodized salt has been in use since the mid-1950s, as Murray described iodized salt utilization for adolescents and child-bearing women in Multan in 1958.31 The first salt iodization plant was initiated in the late-1950s in Skardu, but it remained non-functional for 15 years. In 1980, a second iodization plant was started in Peshawar. Iodized salt utilization, paralleled by awareness campaigns, was formally begun in the northern areas in the 1970s, particularly in Gilgit Baltistan, then extended to the Swat region in the 1980s, but with unsatisfactory results.34 To overcome the iodine deficiency in severely iodine-deficient areas, some alternative fortification strategies—oil iodization in 1983 and iodized oil injection in 1986—were also practiced, but ended soon thereafter due to unsatisfactory results.35
Adoption of USI Programme (1994 onwards)
Overall, 36 studies, other than two national nutrition surveys (NNS), have reported goiter prevalence/iodine deficiency since 1994. Of those, seven studies (19.4%) reported a goiter/iodine deficiency prevalence ≥70%, while eight studies (22.2%) reported a goiter prevalence of 50%–69%. Only three studies (8.3%) reported a goiter/iodine deficiency prevalence of 30%–49%, while nine studies (25%) reported a goiter/iodine deficiency prevalence of 10%–29%. Alongside, only 5 (13.9%) studies have reported a goiter/iodine deficiency prevalence <10% (Table 2). Moreover, four studies (11.1%) reported differential results, with lower goiter prevalence but higher prevalence of iodine deficiency. A study conducted in Lahore reported a goiter prevalence of 31.8% but a prevalence of iodine deficiency of 79.5%.36 Similarly, a few recent studies conducted in Charsadda, Kohat, and Karak districts of Khyber Pakhtunkhwa (KP) province reported goiter prevalences of 15.8%, 14.5%, and 35%, respectively, but the reported iodine deficiency prevalences reported, based on UIC, were higher at 54.7%, 92.7%, and 87.3%, respectively (Table 2).37, 38, 39 Equal numbers of studies (12) were conducted in KP and Punjab. However, half of the studies in Punjab (6) were concentrated around Lahore, and only a few reports came from other areas, while studies in KP were predominately conducted around Peshawar 4 (33.3%) and Swat 3 (25%) regions. There were no reports from Balochistan and FATA areas. Only the 2011 NNS reported iodine deficiency (ID) to be 35.0% (n = 61), and 10.31% (n = 13) in Balochistan and FATA respectively.20 Two studies conducted in the capital (Islamabad) in 2003 and 2014 reported severe prevalences of goiter (71.6%)40 and iodine deficiency (87.5%), respectively.41
For the assessment of nutritional status (including iodine deficiency) of the population, two national surveys were conducted, the first in 2001 and the second a decade later in 2011.20, 42 The results of these NNSs revealed concomitant improvements. The iodine deficiency prevalence in school aged children (6–12 years) was reduced to 36.7% in 2011 from 63.7% in 2001, while prevalence in mothers of reproductive age (15–49) was reduced from 76.3% to 48%. The median UIC (of women) was 124 μg/L, and household iodized salt consumption also increased to 69.1% in 2011. The efforts in a decade resulted in a 50% decline in IDD prevalence,43 and the country attained adequate status, as per WHO recommended criteria (Table 3).44 Both of these surveys highlighted the northern regions of the country as more affected by iodine deficiency. However, the studies conducted after the 2011 NNS showed severe iodine deficiency in terms of higher goiter prevalence (14%–35%) and mild-to-moderate iodine deficiency based on median UIC levels (75.18 μg/L, 89.9 μg/L, 62.3 μg/L and 56 μg/L in Peshawar,45 Charsadda,39 Karak,37 and Kohat38 districts, respectively) (Table 2).
Table 3.
WHO recommended indicators for the assessment of iodine status.
| Indicator | Iodine intake |
Excessivea |
More than adequate |
Adequate |
Mild |
Moderate |
Severe |
|---|---|---|---|---|---|---|---|
| Iodine status | Risk of adverse health consequences | Above requirements | Sufficient | Insufficient | |||
| Total goiter rate (TGR) (%)109, 110 | 0–4.9 | 5–19.9 | 20–29.9 | 30 or more | |||
| MUICc SACd (6 years or older)b (μg/L)109, 110 | ≥300 | 200–299 | 100–199 | 50–99 | 20–49 | ≤20 | |
| MUIC Pregnant women (μg/L)111 | ≥500 | 250–499 | 150–249 | ≤150 | |||
| MUIC Lactating women and children under 2 years (μg/L)111 | ≥100 | ≤100 | |||||
| Salt coverage (countries or areas within the country) (%)109, 110 | ≥90 | 50–90 | 20–50 | ≤20 | |||
The term “excessive” means in excess of the amount required to prevent and control iodine deficiency.
Applies to adults, but not to pregnant and lactating women.
Median urinary iodine concentration.
School age children.
After formal adoption of the USI program in 1994, the results also were insufficient and not uniform (Table 2). Iodized salt consumption has not been effective initially; in Peshawar, only 19% of 1244 households were using iodized salt regularly, while 70% never did.46 However, in 2005, the salt iodization program was revitalized when the Micronutrient Initiative carried out the first Pakistan salt sector survey. Of the total edible salt processed by 1172 salt units in Pakistan at that time (0.935 million tons), only 14% was iodized.47 The Nutrition Wing of the Ministry of Health joined the Micronutrient Initiative in 2006, and a salt iodization project was initially piloted in 20 selected districts from all over Pakistan and expanded and scaled up by including 29 high-risk northern districts and FATA, with the help of the World Food Program. By 2010, the project was expanded to 102 districts in Pakistan and claimed 99% salt iodization throughout the country.48 Studies showed intermittent improvement in the following years, as awareness and use of iodized salt increased to 99% in Abbottabad and 80% in Peshawar, leading to decreases in goiter prevalence of 23% and 20%, respectively.49, 50 Furthermore, 91% of all housewives in Toba Tek Sigh,51 90.3% in Punjab, and 67% in the Sindh province were aware of the advantages of using iodized salt.52 Overall, 64% of housewives at the national level were aware of iodized salt in 2011, and household iodine use was 69%, compared to 17% in 2001.20, 42 However, some recent studies of school children (6–12 years) in the districts of Charsadda, Kohat, and Karak show a different picture, with 70%,39 56.5%,37 and 72.5%38 of the population using non-iodized salt. Even the most recent community-based intervention study revealed that only 2.6% of households were using iodized salt before the intervention.45
Barriers to sustainable control
The difference in results of studies reporting prevalence of goiter and IDD in Pakistan may be attributed to several factors that hamper the establishment of sustainable nationwide iodine fortification and monitoring programs in Pakistan, making the country a complicated unit for precise estimates of iodine nutritional status.
Geographic atlas and natural hazards
Pakistan comprises variable geographic and environmental features that include large badland areas, which enhances the iodine deficiency problem. The country is characterized by a vast range of mountains extending in a continuous tract in the north, west, and southwest (Fig. 1). The northern mountain system, which occupies one third of the northern part of the country, consists of the Karakoram, the Himalayas, and the Hindu Kush. Characteristically, these mountain slopes are steep and covered in snow and glaciers, with precipitous slopes that produce fragile watershed areas undergoing continuous natural erosion and landslides.53 The western mountain ranges, which are not as high in altitude as those in the north, comprise the Safed Koh and the Sulaiman, while the southwestern ranges form the high, dry, and cold Balochistan plateau.
The other major long-term factor threatening natural soil iodine in Pakistan is intervals of repeated downstream floods. Seven massive floods have occurred in the last 2 decades, with increasing frequency over the past few years, which strip the surface soil layer.54 Beyond flooding, the southwest monsoon, tropical storms, dust storms, continental air, tropical cyclones and tornadoes55 and repeated earthquakes56 may contribute to iodine deficiency.
Socioeconomic status
Pakistan is characterized by poverty and social disadvantage. Of its 183 million residents, 54% live below the poverty line,57 and the per capita annual income is 1380 USD. The growth rate since 2008 has been only 3.5%, but inflation was 7.9% in 2014.57 Currently, the only method of IDD eradication is promotion of iodized salt, but this strategy is gravely affected by its cost. In the last decade, the per kilogram price of iodized salt was 0.032 USD, reaching 0.2 USD in 2014, which is higher than the price of non-iodized salt.52 A study conducted in all districts of the Punjab and Sindh provinces revealed that 31.4% of the households used iodized salt occasionally, while 31.0% of the households never used iodized salt because of its high price.52 A cost-related non-use of iodized salt (79%) was observed in 96 households in Toba Tek Singh51 and in 26% of households in Peshawar.46 A recent study indicates that 37.5% of the shopkeepers and 28% of the community members think that the price of iodized salt is preventing its usage.45
Differential adaptation, awareness, and impact
Currently, one of the most important limitations is the lack of nationwide awareness campaigns for an integrated USI program using large-scale media sources, technical and educational materials, and academic curricula.
The most consistent awareness campaign was carried out in Gilgit Baltistan, where its success is attributable to AKHS, which formally started operating in 1988. Iodized salt was being used even before that in the 1970s, but with insufficient results; in 1981, only 1% of the people in Baltistan were using iodized salt.58 AKHS focused on health education and awareness about iodized salt at the community and household levels,35 and the AKHS program led to an increased use of iodized salt (92%) associated with 94% awareness among families.59 Because of the program's consistency and monitoring in Gilgit and Hunza, the prevalence of goiter was decreased from 61.4%33 to 4.7%,60 and then further to 0.5%61 in 2011, in school-age children.
Regional differences were highlighted in a study from the same year in the Swat region, which has almost the same topography as Gilgit Baltistan and a similar history of goiter endemism. After almost 10 years of USI adoption, 76%–80% of the households were using iodized salt, which led to a slight decrease in goiter prevalence from 59.5%22–45% in girls and 52% in boys.62 The difference in results between Swat and Gilgit Baltistan can be explained by later adoption of USI in Swat and the effectiveness of monitoring by AKHS in Gilgit Baltistan. AKHS was the direct effector of this success, with an extensive network of volunteers and trained staff, while in Swat the effort was supported by the United Nations Children's Fund (UNICEF) as the occasional funding partner.
Myths regarding iodized salt
Because of the low education status of the general population in Pakistan, most health-related campaigns with recognized international funding in support or as part of universal programs have faced implementation problems because of associated myths, Illiteracy, cultural tendencies, shadow religious beliefs, and communication mistakes63 that have led to belief in the myth that iodized salt use has contraceptive effects. Particularly, people in restricted cultures, tribes, and the illiterate have stronger beliefs in this myth, leading 44% of individuals in Peshawar to avoid iodized salt as a result.46 A total of 6.6% of household women in all districts of the Punjab and Sindh provinces52 and 0.6% in Toba Tek Singh51 have been reported to avoid using iodized salt because of this belief. Even a large proportion in the metropolitan area of Lahore (40%) believe in this myth.63 Overall, 30% of the people in Pakistan do not use iodized salt because of the contraceptive myth.63 The updated results further confirm this myth, since 35.7% of the iodized salt sellers believe that people avoid iodized salt purchase because of this myth.45
Legislative discrepancies
An important part of any health-related campaign is policy-making infrastructure, which is not supportive of the positive health reforms and their implementation for the benefits of every individual in Pakistan. Evidence of political commitment to USI and elimination of IDD usually comes in the form of legislation. Pakistan currently has no comprehensive or uniform legislation, national or provincial (except for Sindh Province), for compulsory salt iodization. The endorsements regarding IDD and USI are in response to the recommendations of international agencies (e.g., WHO, UNICEF, and IGN) as additions to the existing Pure Food Ordinance 1960, pertaining to the preparation and sale of foods.64 Amendments to the Pure Food Rules 1960 exist in the Khyber Pakhtunkhwa and Balochistan Provinces. There is a presidential order (since 2008) in Azad Jammu and Kashmir,48 while Punjab has amendments of by-laws of Pure Food Rules 1960 in the majority of the districts. Gilgit Baltistan Province introduced a new IDD Bill in 2009, and the first Sindh Compulsory Iodization of Salt, NO. XXXVII of 2013 act was passed in Sindh Province.65 Unfortunately, a uniform act for the whole country, the IDD Control Bill 2009, is still pending approval and implementation. The policy-making infrastructure comprises IDD control advisory boards and committees, at national and provincial levels, made up of nutrition/IDD experts and industry and consumer organizations.66 The standards for salt fortification include 30 ppm iodine or 50 ppm KIO3 at production level and 15–25 ppm at distribution level. The fortifiers used in Pakistan include potassium iodide (with stabilizing agent), iodate, and calcium iodate. The table salt iodization is mandatory, as declared in the drafted National IDD Control Bill, but facing implementation problems because of legislation issues.66
An additional concern is insufficiently-iodized table salt, which may contain only minimum concentrations of iodine. In Peshawar, 50% of salt sold in the market was either unionized or contained very low concentrations of iodine,50 and 52% of salt sold had an iodine content less than the recommended level At the household level, whether because of non-recommended packaging or lack of awareness about the volatile nature of iodine, the actual concentration of iodine is further reduced. A number of studies have reported an insufficient amount of iodine in household iodized salt (in individual studies, 59.5% had iodine content <5 ppm,49 54.5% had iodine content less than 20 ppm,22 26% had iodine content as low as 0–7 ppm,62 and only 12.5% of all household salts had optimal iodine concentrations39).
Food preferences and cooking practices
The geometric mean concentration of iodine (40 μg/d) in the daily food intake preferences of average Pakistani men is far lower than the international recommendations, mainly because of reduced or absent seafood consumption, diet composition, suboptimal intake of milk, intake of goitrogenic foods, and losses during cooking.67 The normal cooking practice in Pakistan involves heating food for 15–45 min at or above 100 °C. Because of the volatile nature of iodine at temperatures of 58 °C and above during frying, grilling, and boiling, losses are reported to be 20%, 30%, and 58%, respectively.68 With these losses, the 40 μg/d is further reduced.67 Another traditional stumbling block in Pakistan is infrequent use of processed foods; only 20%–30% of food consumed in Pakistan comes from food manufacturers, and this processed food is eaten primarily in urban settings, while around 70% of the rural population generally consumes home-made foods.69
Accessibility to regions
The current estimates may be limited by the fact that researchers have had limited accessibility to large parts of Pakistan in the past decade. In most regions, the primary reason is the war on terrorism, but certain long-lasting associated factors, such as cultural values, illiteracy, and feudalistic influence, also contribute. In some FATA regions and Balochistan, the main factors are terrorism, cultural values, illiteracy, and feudalism; in Swat, they are terrorism, cultural values, and illiteracy; and in the eastern, southeastern, and northwestern parts of Sindh, the primary influences are illiteracy and feudalism. The fear factor arising from previous incidents stops people from attempting to engage in research in these areas,70 and, of all the studies listed in Table 2, not one published study is based on the largest province Balochistan and FATA.
Organizations working for the elimination of iodine deficiency disorders and regulatory monitoring
Several actors led by the government of Pakistan are working to achieve the goal of USI in that country (Table 4).64 There seems to be a lack of coordination of the multi-sectorial partnership, however, as reflected in recent results that are highly divergent and sometimes hard to interpret (Table 2).20 The Micronutrient Initiative has played a useful role in ongoing data gathering and analysis related to production and the iodization process of salt.48 The overall market situation seems to be suboptimal, though, regarding companies involved in production and distribution of iodized salt, the role of small-scale producers, and government-driven prices of iodized salt.
Table 4.
Role of the organizations working for the elimination of iodine deficiency disorder in Pakistan.
| Name of organization | Role in IDD prevention program |
|---|---|
| UNICEF | Focuses on advocacy, demand generation, monitoring and legislation64 |
| Micronutrient Initiative | Supports salt iodization program implementation through financial and technical assistance to salt producers, government, and departments of health112 |
| World Food Program (WFP) | Provides funding for IDD prevention program112 |
| WHO | Provides funding, recommendations, standards, and protocols64 |
| Global Alliance for Improved Nutrition (GAIN) | Focuses on the supply and quality of iodized salt production, monitoring, and evaluation113 |
| World Bank | Provides funding for the IDD prevention program64 |
| Bill and Melinda Gates Foundation | Provides funding for the GAIN-UNICEF partnership project in 16 countries including Pakistan113 |
| South East Asia Iodine Deficiency Disorders Elimination Action Group (SEA-IDDEA) | Reviews the status of USI, looking for constraints and remedies and partners for action against IDD64 |
| The Nutrition Wing of the Ministry of Health | Provides overall policy formulation, strategy approval, monitoring and supervision of program implementation, quality control and regulatory enforcement of the salt processors in their respective areas64 |
| Pakistan Standard and Quality Control Authority | Works on quality control and quality assurance, helps in development of internal and external monitoring protocols, with assistance of DoH, Micronutrient Initiative, UNICEF64 |
In Pakistan, because of poorly developed and insufficient legislation, clarity is lacking about the roles and responsibilities of different government and international agencies in regulatory monitoring.64 Even in the presence of well-known partner organizations, a not-so-robust monitoring and evaluation framework exists in Pakistan. The identified weaknesses—insufficient resources; over-reliance on spot-test results; insufficient consideration of quality assurance systems; and poorly established study protocols, laboratory resources, and expertise—are the main factors limiting the monitoring mechanism.64
Discussion
Iodine deficiency has been historically present in Pakistan,16, 29, 30 although the country has taken some steps to improve the situation in the 68 years since its founding. However, the recent results demand the need for a well-planned, well-monitored, and sustainable IDD control programme in Pakistan. Iran and China are two examples in the neighbourhood for successful IDD prevention programmes, which could be adapted by Pakistan. Iran may not have the same geography as Pakistan, but historically their IDD story is very similar.71, 72 After establishment of the Iranian National Committee for Control of IDDs in 1989, it has shown tremendous progress. The IDD control programme was launched uniformly throughout the country, with standardization and quality control at production, distribution, and consumption of iodized salt. The most important factor in Iranian experience was periodic monitoring every 5 years.21 Iran was declared an IDD-free country17 a decade after the start of the IDD control programme. Two decades after the launch of the USI programme, the well-monitored salt iodization program in Iran has ultimately resulted in optimization of UIC, with a current median of 140 μg/L, and drastically decreased the goiter rate to 6.5%, although the effect on goiter prevalence appeared some years after normalization of UIC.21 China, which is also an IDD-endemic area, made substantial efforts to eradicate IDD by the end of last century through political commitments, repeated monitoring, fortification strategies, and swift national actions Iodized salt consumption exceeded 90% of the population in most parts of the country, while goiter was reduced to less than 15% in most regions, with median UIC reaching a satisfactory level of more than 100 μg/L.73 However, there was over-saturation in some regions, as UIC reached to levels more than 300 μg/L, levels at which adverse health effects emerge (Table 3).
In comparison, places where IDD re-emerges are in a more critical situation,5 and similar issues that interfere with the elimination of IDD in Pakistan continue to plague other communities in the developed world. Barriers to a USI program to eradicate iodine deficiency may be different in the different social tiers of these regions, but the lethal outcomes are the same.5 Pakistan may represent a paradigmatic example of the relevant socioeconomics, which remains a key barrier in many parts of the world. In Africa, countries like Ethiopia, Algeria, Sudan, Morocco, Ghana, and Mozambique have a poor salt coverage of less than 50%, which is attributed to socioeconomics.6 Of utmost importance is the socioeconomic discrimination affecting iodine supplementation. Although the evidence of socioeconomic discrimination specifically related to iodine supplementation in the general population or a specific group is sparse, it has been reported from developed parts of the world, such as among pregnant women in Australia.74
The myth problem around iodized salt consumption is also not limited to Pakistan. Even in other developed countries where health is a concerning public issue, myths have led to non-usage of iodized food products. In some European populations, such as Germany, groups argue against iodine fortification because of putative risks of allergies, skin disorders, and cancer, neglecting dose-response relationships between iodine use and such disorders.75 In other countries, including the United Kingdom76 and the United States,1 salt intake is reduced because of potential risks of cardiovascular health, which subsequently leads to suboptimal iodine intake. In fact, salt reduction does reduce the risk of cardiovascular diseases, but proper management of salt use and level of fortification can balance risks on both sides.77
In Pakistan, iodized salt coverage is even less than in some of the low-income countries in Africa. States like Kenya, Uganda, Rwanda, and Tanzania have salt coverage of greater than 80%.6 On the other hand, even in some industrialized countries, the situation is worse, as in the United Kingdom and Russia, where the iodized salt coverage rates are only 5% and 35%, respectively.5, 78 In parallel, inadequately iodized salt on the market has been reported from India81 and the United Kingdom (11.5 mg/kg).76
Legislation and regulatory monitoring are the cornerstones of sustaining IDD prevention programs. Legislation may strictly define the monitoring mechanism, along with other aspects. In 2005, the World Health Assembly resolved that member states should monitor and report the iodine nutrition status of their respective populations every 3 years.79 Although Pakistan produced data regarding the iodine nutritional status of the population 5 years ago, it did not produce data about the extent and severity of iodine deficiency, as did most other countries in Asia, Africa, and Europe.5, 6, 79 A recent survey of iodine status was performed within the last 2 years in only 16 out of 35 western and central European countries,5 while iodine data were available for 44 out of the 54 African countries in 2013, covering 96% of the African population.6 A recent update about Europe shows that there was no ongoing monitoring of the iodine status in 17 countries in western and central Europe, while Spain and the United Kingdom, two of the most populous countries in Europe, have no national monitoring.5
As in Pakistan, regional accessibility is a limitation for monitoring IDD prevention programs. One famous example is Yemen, where the major concern about conducting surveys in remote areas is security.14 Furthermore, issues with security in some African and Arab nations are also well known.
Conclusions
Iodine deficiency-related problems represent serious community health issues, and lessons can be learned from Pakistan and other countries. Coordinated serious efforts are needed for eradication of IDD from all stakeholders, including legislative commitments, awareness through various means, effective monitoring of salt iodization, alternative fortification strategies, and regional and local campaigning.
Conflicts of interest
None declared.
Acknowledgements
This project has received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No. 634453.
We also received a partial support for the analyses from the German Research Foundation under the project number DFG-VO955/10-2.
Footnotes
Peer review under responsibility of the Japan Epidemiological Association.
References
- 1.Pearce E.N., Andersson M., Zimmermann M.B. Global iodine nutrition: where do we stand in 2013? Thyroid. 2013;23(5):523–528. doi: 10.1089/thy.2013.0128. [DOI] [PubMed] [Google Scholar]
- 2.Horton S., Mannar V., Wesley A. Copenhagen Consensus Center, Copenhagen Business School; Denmark: 2008. Best Practice Paper: Food Fortification with Iron and Iodine. [Google Scholar]
- 3.Resegue R., Puccini R.F., Silva EMKd. Risk factors associated with developmental abnormalities among high-risk children attended at a multidisciplinary clinic. Sao Paulo Med J. 2008;126(1):145–157. doi: 10.1590/S1516-31802008000100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andersson M., Karumbunathan V., Zimmermann M.B. Global iodine status in 2011 and trends over the past decade. J Nutr. 2012;142(4):744–750. doi: 10.3945/jn.111.149393. [DOI] [PubMed] [Google Scholar]
- 5.Lazarus J.H. Iodine status in Europe in 2014. Eur Thyroid J. 2014;3(1):3–6. doi: 10.1159/000358873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jooste P., Andersson M., Assey V. Iodine nutrition in Africa: an update for 2014. Sight Life. 2014;27(3):50–55. [Google Scholar]
- 7.Ferreira S.M.S., Navarro A.M., Ribeiro M.P.K., Maciel L.M.Z. Iodine insufficiency in pregnant women from the state of Sao Paulo. Arq Bras Endocrinol Metab. 2014;58(3):282–287. doi: 10.1590/0004-2730000002979. [DOI] [PubMed] [Google Scholar]
- 8.Gallego G., Goodall S., Eastman C.J. Iodine deficiency in Australia: is iodine supplementation for pregnant and lactating women warranted. Med J Aust. 2010;192(8):461–463. doi: 10.5694/j.1326-5377.2010.tb03586.x. [DOI] [PubMed] [Google Scholar]
- 9.Eltom M., Hofvander Y., Torelm I., Fellström B. Endemic goitre in the Darfur region (Sudan) Acta Medica Scand. 1984;215(5):467–475. doi: 10.1111/j.0954-6820.1984.tb17680.x. [DOI] [PubMed] [Google Scholar]
- 10.Azizi F. 2002. Assessment, Monitoring and Evaluation of Iodine Deficiency Disorders in the Middle East and Eastern Mediterranean Region. [Google Scholar]
- 11.Coble Y., Davis J., Schulert A., HETA F., AWAD A.Y. Goiter and iodine deficiency in Egyptian oases. Am J Clin Nutr. 1968;21(4):277–283. doi: 10.1093/ajcn/21.4.277. [DOI] [PubMed] [Google Scholar]
- 12.Caughey J., Follis R. Endemic goitre and iodine malnutrition in Iraq. Lancet. 1965;285(7394):1032–1034. doi: 10.1016/s0140-6736(65)91311-5. [DOI] [PubMed] [Google Scholar]
- 13.Al-Nuaim A.R., Al-Mazrou Y., Kamel M., Al-Attas O., Al-Daghari N., Sulimani R. Iodine deficiency in Saudi Arabia. Ann Saudi Med. 1997;17:293–297. doi: 10.5144/0256-4947.1997.293. [DOI] [PubMed] [Google Scholar]
- 14.Zein A.Z., Al-Haithamy S., Obadi Q., Noureddin S. The epidemiology of iodine deficiency disorders (IDD) in Yemen. Public Health Nutr. 2000;3(02):245–252. doi: 10.1017/s1368980000000288. [DOI] [PubMed] [Google Scholar]
- 15.Azizi F., Mehran L. Experiences in the prevention, control and elimination of iodine deficiency disorders: a regional perspective. East Mediterr Health J. 2004;10(6):761–770. [PubMed] [Google Scholar]
- 16.McCarrison R. Observations on endemic cretinism in the Chitral and Gilgit valleys. Lancet. 1908;31:1275–1280. [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization . WHO; Dubai: 2000. Regional Meeting for the Promotion of Iodized Salt in the Eastern Mediterranean, Middle East and North Africa: Report of an Inter-Country Meeting. [Google Scholar]
- 18.Alsanosy R.M.A., Gaffar A.M., Khalafalla H.E.E., Mahfouz M.S., Zaid A.N.S., Bani I.A. Current iodine nutrition status and progress toward elimination of iodine deficiency disorders in Jazan, Saudi Arabia. BMC Public Health. 2012;12(1):1. doi: 10.1186/1471-2458-12-1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Network for Sustainable Elimination of Iodine Deficiency . UNICEF; New York: 2010. Global Scorecard.http://www.unicef.org/publications/index_44271.html Available at: Accessed 10 December 2014. [Google Scholar]
- 20.Agha Khan University P, editor. National Nutrition Survey of Pakistan. PMRC, Nutrition Wing, Cabinet Division, Government of Pakistan; Islamabad: 2011. pp. 33–34. [Google Scholar]
- 21.Delshad H., Amouzegar A., Mirmiran P., Mehran L., Azizi F. Eighteen years of continuously sustained elimination of iodine deficiency in the Islamic Republic of Iran: the vitality of periodic monitoring. Thyroid. 2012;22(4):415–421. doi: 10.1089/thy.2011.0156. [DOI] [PubMed] [Google Scholar]
- 22.Bano S., Haq M., Khan S.M., Shah S.A., Iqbal N. Iodine deficiency still a major health problem in some areas of Swat. Pak J Med Res. 1999;38(1):3–6. [Google Scholar]
- 23.Ghayur S., Slddlqul S., Alam M.M., Shaukat A., Khan F.A. 2001. Spectrum of Iodine Deficiency in School Children of Rawalpindi. [Google Scholar]
- 24.Rafiq M. UNICEF/NIH; Islamabad: 1998. Prevalence Survey of Iodine Deficiency Disorders in 8–10 Years Old School Children and Use of Iodized Salt. Swat NWFP: Pakistan, Report. [Google Scholar]
- 25.Mahmood U.A. University of Punjab; Lahore: 2005. Assesment of Nutritional Status of Adolescent School Girls at Rawalpind. [Google Scholar]
- 26.Shahid A., Siddique F.R., Bhatti M.A., Ahmed M., Khan M.W. Assessment of nutritional status of adolescent college girls at Rawalpindi. Annals. 2009;15(1):11–16. [Google Scholar]
- 27.Khawar H. The pinch of salt. Dly Dawn. 2007 [Google Scholar]
- 28.Blumberg B.S. Goiter in Gandharan representation in a second to third century AD Frieze. JAMA. 1964;189(13):1008–1012. [PubMed] [Google Scholar]
- 29.Macnamara F.N. Longmans; Green: 1880. Climate and Medical Topography in Their Relation to the Disease-distribution of the Himalayan and Sub-Himalayan Districts of British India: With Reasons for Assigning a Malarious Origin to Goitre and Some Other Diseases. [Google Scholar]
- 30.McCarrison R., Newcomb C., Viswanath B., Norris R. The relation of endemic goitre to the iodine-content of soil and drinking-water. Indian J Med Res. 1927;15:207–246. [Google Scholar]
- 31.Murray M.M., Wilson D.C., Exley D., Hasan S. Investigation of an epidemic of goitre in West Pakistan. Trans R Soc Trop Med Hyg. 1958;52(3):223–229. doi: 10.1016/0035-9203(58)90080-4. [DOI] [PubMed] [Google Scholar]
- 32.Sardar-ul-Mulk, Shahid M.A., Grant I.S. Endemic goitre in chitral. J Pak Med Assoc. 1974;Aug:171–176. [Google Scholar]
- 33.Anonymous . Nutrition Cell of Planning Division of Government of Pakistan; Islamabad: 1978. Shigar School Children. [Google Scholar]
- 34.Rafiq M. Swat success with salt iodization. IDD Newsletters. 2002;18:10–12. ICCIDD. [Google Scholar]
- 35.AKHSP . 1990. Assessment of PHC Program. Indications of AKHSP in Northern Areas and Chitral, Gilgit. Karachi. [Google Scholar]
- 36.Elahi S., Rizvi N.B., Nagra S.A. Iodine deficiency in pregnant women of Lahore. J Pak Med Assoc. 2009;59(11):741–743. [PubMed] [Google Scholar]
- 37.Jahangir M., Khattak R., Shahab M., Tauseef I., Khattak M. Prevalence of goiter and iodine nutritional status in school age children of district Karak, Khyber Pakhtunkhwa, Pakistan. Acta Endocrinol (BUC) 2015;11(3):337–342. [Google Scholar]
- 38.Subhan F., Jahangir M., Saira S. Prevalence of goiter and iodine status among 6–12 years school age children in district Kohat, Pakistan. South East Asia J Public Health. 2015;4(2):42–46. [Google Scholar]
- 39.Saira S., Khattak R.M., Khan A.A., Rehman A., Khattak M.N.K. Prevalence of goiter and assessment of iodine status in 6–12 years school children and pregnant women of district Charsadda, Pakistan. Acta Endocrinol Bucharest. 2014;10(1):65–75. [Google Scholar]
- 40.Ali T.Z., Anis R.A., Shami S.A., Ijlal F., Aqeer F.I.F. Prevalence of goiter in school-going children in a union council near Islamabad. Pak J Med Res. 2007;46(4) [Google Scholar]
- 41.Rafi M., Tufail M., Chaudhry M., Irfan N. Assessment of iodine status among hostel employees and students of a University in Islamabad, Pakistan. J Chem Soc Pak. 2010;32(5):620–625. [Google Scholar]
- 42.National Nutrition Survey (NNS) Aga Khan University; In collaboration UNICEF-Pakistan Medical Research Council (PMRC), Nutrition Wing, Cabinet Division, Ministry of Health, Pakistan; Islamabad: 2001. [Google Scholar]
- 43.ICCIDD Striking progress against IDD in Pakistan; 50% decrease in iodine deficiency in children over the past decade. IDD News Lett. 2013;2(41):5–20. [Google Scholar]
- 44.Iodine Global Network . 2014. Global Iodine Nutrition Scorecard; p. 2016.http://www.ign.org/cm_data/Scorecard_2015_August_26_new.pdf Available at: Accessed 25 January 2016. [Google Scholar]
- 45.Lowe N., Westaway E., Munir A. Increasing awareness and use of iodised salt in a marginalised community setting in North-West Pakistan. Nutrients. 2015;7(11):9672–9682. doi: 10.3390/nu7115490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ul Haq M., Salarzai I.A., Khan S.M. Iodized salt use in Peshawar: its iodine content, price and use by the people. ICCIDD Newsl. 1996;12(2):33. [Google Scholar]
- 47.Solutions for Hidden Hunger; MI partners to push forward the case of Universal Salt Iodization (USI) Legislation in Pakistan. Micronutrient Initiative; 2008. http://www.micronutrient.org/2008/07/mi-partners-push-forward-case-universal-salt-iodization-usi-legislation-pakistan/ [Google Scholar]
- 48.Micronutrient Initiative. GIS for Salt Sector of Pakistan. Welcome to Iodine Deficiency Disorders/Universal Salt Iodization Programme (IDD/USI), Pakistan. Available at: http://pakusi.naqsha.net/web/Default.aspx. Accessed 10 December 2014.
- 49.Iqbal N., Ul Haq M.U., Khan S.M., Bano S. Assessment of iodine deficiency in school going children in Abbott Abad-Pakistan. Specialist. 1999;15(4):325–329. [Google Scholar]
- 50.Zahoor U., Tasleem A., Aakif U.K., Gul N., Ul Haq M. Goiter in school children versus use of iodized salt in Peshawar. Pak J Med Res. 2001;40:90–94. [Google Scholar]
- 51.Imdad S., Shoukat M.S., Khalid M. Appraisal of the knowledge & practices about iodized salt amongst housewives in Toba Tek Singh city and the impact of socio economic factors on such knowledge and practices. Pak J Med Health Sci. 2011;5(4):796–799. [Google Scholar]
- 52.Khan G.N., Hussain I., Soofi S.B., Rizvi A., Bhutta Z.A. A study on the household use of iodised salt in Punjab and Sindh Provinces, Pakistan: implications for policy makers. J Pharm Nutr Sci. 2012;2:148–154. [Google Scholar]
- 53.Syed A.K., Ford R.W. Oxford University Press; 1966. A Geography of Pakistan. [Google Scholar]
- 54.Tariq M.A.U.R., Nick van de G. Floods and flood management in Pakistan. Phys Chem Earth Parts A/B/C. 2012;47(48):11–20. [Google Scholar]
- 55.Sarfaraz S., Dube S.K. Numerical simulation of storm surges associated with severe cyclones land falling Pakistan coast during 1999–2010. Pak J Meteorol. 2012;8(16):11–20. [Google Scholar]
- 56.Gill M.W.A. Pakistan Meteorological Department (PMD), Regional Meteorological Center; Lahore, Pakistan: 2009. Tectonic Activities in Pakistan. [Google Scholar]
- 57.Tariq M., Idress A., Abid M., Samin T. Rationale effects of poverty in Pakistan. IMPACT IJRBM. 2014;2(6) [Google Scholar]
- 58.Stewart A.G. Drifting continents and endemic goitre in northern Pakistan. BMJ Br Med J. 1990;300(6738):1507. doi: 10.1136/bmj.300.6738.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Khoja S., Luby S., Ahmed Z., Akber A. Effectiveness of health education in promoting the use of iodized salt in Lotkoh, Tehsil Chitral, Pakistan. J Pak Med Assoc. 2000;50(9):296–300. [PubMed] [Google Scholar]
- 60.Ali A., Khan M.M., Malik Z.U., Charania B.A., Bhojani F.A., Baig S.M. Impact of the long term supply of iodised salt to the endemic goitre area. J Pak Med Assoc. 1992;42(6):138–140. [PubMed] [Google Scholar]
- 61.Baig J., Shah S.A., Ul Haq M. Paper Presented at: Proc. Pakistan Congr. Zool. 2011. GILGIT; reduction in iodine deficiency disorders: a perspective study of 2550 school children in district Gilgit. [Google Scholar]
- 62.Akhtar T., Ullah Z. Goitre in district Swat, NWFP-Pakistan: current situation. Pak J Med Res. 2003;42(2):74–76. [Google Scholar]
- 63.Leiby R. Post; Washington: 2012. Myths about Iodine in Salt Lead to Health Crisis in Pakistan. [Google Scholar]
- 64.Stakeholder Report on Regulatory Monitoring of Salt, Wheat Flour and Oil Fortification Programmes in Pakistan. 2012. http://www.pc.gov.pk/hot.links/2012/Stakeholder Consultation on Regulatory Monitoring.pdf [Google Scholar]
- 65.Sindh Go, editor. Vol No. XXXVII. Provincial Assembly of Sindh; Karachi: 2013. The Sind compulsory iodization of salt act. (PAS/Legis-B-22/2013). [Google Scholar]
- 66.Review of National Legislation for Universal Salt Iodization: South Asia and East Asia and the Pacific. UNICEF EAPRO; Bangkok: March, 2013. [Google Scholar]
- 67.Akhter P., Orfi S.D., Ahmad N. Assessment of iodine levels in the Pakistani diet. Nutrition. 2004;20(9):783–787. doi: 10.1016/j.nut.2004.05.019. [DOI] [PubMed] [Google Scholar]
- 68.Organization WH . 1973. Trace Elements in Human Nutrition; p. 532. Report of a WHO Expert Committee. [Google Scholar]
- 69.Ohlhorst S.D., Slavin M., Bhide J.M., Bugusu B. Use of iodized salt in processed foods in select countries around the world and the role of food processors. Compr Rev Food Sci Food Saf. 2012;11(2):233–284. [Google Scholar]
- 70.Tribune T.E. 2013. The Express Tribune: Polio Threat: Five New Cases Surface in FATA, Attacks Continue.http://tribune.com.pk/story/652183 Available at: Accessed 10 December 2014. [Google Scholar]
- 71.Azizi F., Sarshar A., Nafarabadi M. Impairment of neuromotor and cognitive development in iodine-deficient schoolchildren with normal physical growth. Acta Endocrinol. 1993;129(6):501–504. doi: 10.1530/acta.0.1290501. [DOI] [PubMed] [Google Scholar]
- 72.Azizi F., Kalani H., Kimiagar M. Physical, neuromotor and intellectual impairment in non-cretinous schoolchildren with iodine deficiency. Int J Vitam Nutr Res Int Zeitschrift fur Vitamin-und Ernahrungsforschung J Int de vitaminologie de Nutr. 1994;65(3):199–205. [PubMed] [Google Scholar]
- 73.Zhao J., van der Haar F. Progress in salt iodization and improved iodine nutrition in China, 1995–99. Food Nutr Bull. 2004;25(4):337–343. doi: 10.1177/156482650402500403. [DOI] [PubMed] [Google Scholar]
- 74.El Mani S., Karen C., Flood V.M., Judy M. Limited knowledge about folic acid and iodine nutrition in pregnant women reflected in supplementation practices. Nutr Diet. 2014:1–14. [Google Scholar]
- 75.Völzke H., Craesmeyer C., Nauck M. Association of socioeconomic status with iodine supply and thyroid disorders in Northeast Germany. Thyroid. 2013;23(3):346–353. doi: 10.1089/thy.2012.0416. [DOI] [PubMed] [Google Scholar]
- 76.Bath S.C., Button S., Rayman M.P. Availability of iodised table salt in the UK-is it likely to influence population iodine intake? Public Health Nutr. 2014;17(02):450–454. doi: 10.1017/S1368980012005496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pearce E.N., Stagnaro-Green A., Bibbins-Domingo K., Chertow G.M., Coxson P.G. Dietary salt reductions and cardiovascular disease. N Engl J Med. 2010;2010(362):2224–2226. doi: 10.1056/NEJMc1003765. [DOI] [PubMed] [Google Scholar]
- 78.UNICEF . United Nations Children's Fund; New York, USA: 2014. The State of the World's Children 2014, In Numbers; Every Child Counts-revealing Disparitiea, Advancing Children's Rights. 1.6.2016. [Google Scholar]
- 79.Eastman C.J. Iodine deficiency disorders continue to be a problem in the Asia Pacific Region. J ASEAN Fed Endocr Soc. 2014;27(2):170. [Google Scholar]
- 80.Matovinović J., Ramalingaswami V. Therapy and prophylaxis of endemic goitre. Bull World Health Organ. 1958;18(1-2):233. [PMC free article] [PubMed] [Google Scholar]
- 81.Chapman J.A., Grant I.S., Taylor G., Mahmud K., Mulk S.U., Shahid M.A. Endemic goitre in the Gilgit Agency, West Pakistan with an appendix on dermatoglyphics and taste-testing. Philos Trans R Soc B Biol Sci. 1972;263(856):459–490. doi: 10.1098/rstb.1972.0007. [DOI] [PubMed] [Google Scholar]
- 82.Zafar M.H., Malik G.Q., Sahu M.H., Captan K.M., Saeed T., Iqbal I. Prevalence of goitre in schools and colleges of Multan. J Pak Med Assoc. 1985;35:45–48. [PubMed] [Google Scholar]
- 83.Amacha M.H. Department of Zoology, University of Punjab; Lahore: 1980. Goitre and Cretinism Survey in Shigar Valley. [Dissertation] [Google Scholar]
- 84.Paindakhel S.M. Goitre in north of Kalam. J Pak Med Assoc. 1981;31:178. [PubMed] [Google Scholar]
- 85.Khan M.R., Charania B.A. National Institute of Health; EMRO Alexandria, Egypt. Pakistan: 1987. IDD in Pakistan. An Overview Presented at the Inter-country Consultation on IDD Control. [Google Scholar]
- 86.Mohammad S., Ullah Z., Khattak I., Zia S., Akhtar T. Goiter prevalence and quality of drinking water in district Mardan. Pak J Med Res. 1988;27(1):53–56. [Google Scholar]
- 87.Ahmad S., Mannan A., Qureshi H.I., Khan S.M., Ahmad I. Iodine determination in water SAMPLES from goiter endemic areas using NAA. J Radiol Nucl Chem. 1988;120(1):89–95. [Google Scholar]
- 88.Godwin P., Moti-ur-Rehman-Khan M., Anis R.A., Sughra F. National Institute of Health, Government of Pakistan; Islamabad: 1989. Report of a Qualitative Survey of People's Perception of IDD in a Village of Hazara Division. [Google Scholar]
- 89.Zafar A., Cheema K., Hassan K., Latif S., Saeed S. Goiter in school going children in Murree hills. Specialist. 1991;8(1):27–30. [Google Scholar]
- 90.UNICEF . A Better Future for Children and Women in Pakistan. UNICEF; Lahore: 1995. Punjab: socio-economic profile. [Google Scholar]
- 91.AKHSP . Agha Khan Health Services (AKHSP); Karachi: 2000. Northern Areas and Chitral. Annual report. [Google Scholar]
- 92.Hussain I., Soofi S.B., Hasan S. Impact on health and nutrition outcomes in Sindh province, Pakistan. IDS Bull. 2013;44(3):38–47. [Google Scholar]
- 93.Husain S., Muhammad A. Nutritional survey of 8th October 2005 earthquake hit area of District Bagh. Pak J Med Res. 2009;48(3):51–54. [Google Scholar]
- 94.Elahi S., Sayed Z., Nagra S.A. Status of iodine deficiency disorders as estimated by neonatal cord serum thyrotropin in Lahore, Pakistan. Nutr Res. 2004;24(12):1005–1010. [Google Scholar]
- 95.Hussain I., Khan G.N., Soofi S.B., Bhutta Z.A. Iodized salt use: assessment of iodine deficiency among underfive children and women of reproductive age in Sindh province, Pakistan. Sight Life Mag. 2009;2:23–24. [Google Scholar]
- 96.Ali H., Siddiqui P.Q.R., Alam J.M., Kazmi T.H. Severe IDD in pregnancy in northern Pakistan: a sentinel study. ICCIDD Newsl. 2009;May:2. [Google Scholar]
- 97.Sarwar S., Saeed I., Razzaq Z. Urinary iodine levels in residents of Azad Jammu and Kashmir. J Rawalpindi Med Coll. 2014;18(1):142–144. [Google Scholar]
- 98.Elahi S., Manzoor-ul-Hassan A., Syed Z., Nazeer L., Nagra S., Hyder S. A study of goiter among female adolescents referred to centre for nuclear medicine, Lahore. Pak J Med Sci. 2005;21(1):56–62. [Google Scholar]
- 99.Kandhro A.H., Khand F. Study of biochemical risk factors involved in the pathogenesis of goiter in adults in Sindh. J Clin Exp Pathol. 2013:2013. [Google Scholar]
- 100.Shah N., Uppal A.M., Ahmed H. 2014. Impact of a School-Based Intervention to Address Iodine Deficiency Disorder in Adolescent Girls in Gilgit, Pakistan. [Google Scholar]
- 101.Ronald I. Iodine deficiency- the risk and solutions. Nation. Febraury 20, 2013 http://nation.com.pk/business/21-Apr-2009/Iodine-deficiency--the-risks-and-solutions [Google Scholar]
- 102.Khattak M.N.K., Haq M., Khan A., Cheema A. Prevalence of endemic goiter and urinary iodine contents in the population of Lawaghar and Chontra areas of district Karak (North Western Frontier Province), Pakistan. Pak J Sci Res. 2006;58(1-2):1–4. [Google Scholar]
- 103.Imdad S., Muzaffar R., Shoukat M.S. Evaluation of impact of dietary pattern on iodine and thyroid status of adolescent girls in lahore. Biomedica. 2013;29:139. [Google Scholar]
- 104.Arif M., Bangash J.A., Khan F.A. Iodine status of children (8–11 years) in district Peshawar, Pakistan. J Agric Biol Sci. 2011;6(8):1–6. [Google Scholar]
- 105.Elahi S., Khan M., Rasool S., Khalid A., Tasneem A. Paper Presented at: Third Chemistry Conference on Recent Trends in Chemistry. 2011. Environmental iodine intake and pattern of thyroid diseases: experience at nuclear medicine centre, Mayo Hospital. [Google Scholar]
- 106.Aslam M., Iqbal H., Amanullah M., Akbar A., Altaf S. The cluster analysis, BMI status and dietary habits of the patients with thyroid disorder in Pakpattan, Pakistan. Pak J Nutr. 2013;12(7):642. [Google Scholar]
- 107.Jawa A., Jawad A., Riaz S.H. Turmeric use is associated with reduced goitrogenesis: thyroid disorder prevalence in Pakistan (THYPAK) study. Indian J Endocrinol Metab. 2015;19(3):347. doi: 10.4103/2230-8210.152768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Saira Bashir I.S., Riaz Hussain, Misbahul Islam, Muhammad Aasim Thyroid status and urinary iodine levels in women of endemic goiter area. Pak J Med Res. 2012;51(4):136–138. [Google Scholar]
- 109.WHO/UNICEF/ICCIDD . 3rd ed. World Health Organization; 2007. 2013. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers.http://whqlibdoc.who.int/publications/2007/9789241595827_eng.pdf Accessed 25 January 2016. [Google Scholar]
- 110.WHO, ICCIDD, UNICEF . World Health Organization; Geneva: 1994. Indicators for Assessing Iodine Deficiency Disorders and Their Control through Salt Iodization. [Google Scholar]
- 111.Secretariat W.H.O., Andersson M., de Benoist B., Delange F., Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the technical consultation. Public Health Nutr. 2007;10(12A):1606–1611. doi: 10.1017/S1368980007361004. [DOI] [PubMed] [Google Scholar]
- 112.Initiative M. 2014. Micronutrient Initiative: GIS for Salt Sector of Pakistan/. Welcome to Iodine Deficiency Disorders/Universal Salt Iodization Programme (IDD/USI), Pakistan.http://pakusi.naqsha.net/web/Default.aspx Available at: Accessed 10 December 2014. [Google Scholar]
- 113.GAIN-UNICEF Universal Salt Iodization . 2008. Partnership Project. Global Alliance for Improved Nutrition (GAIN) [Google Scholar]