Abstract
The true burden (morbidity, mortality, disability, cost, pain, distress) of occupational and work-related diseases and injuries is unknown, and what is reported as burden is significantly underestimated. This underestimation affects the way decision-makers view investments in research and worker protection, which in turn has a substantial impact on national welfare and public health. To better describe the societal and individual burdens of occupational and work-related diseases and injuries, we propose an approach to gauge what is known about burden and where new assessments may be made.
This approach consists of 4 elements to consider in burden assessments: (1) utilizing multiple domains, including the individual worker, the worker’s family, the community in which the workplace is located, the employer, and society as a whole; (2) taking a broader view of the work-relatedness of disease and injury; (3) assessing the impact of the entire working-life continuum; and (4) applying the comprehensive concept of “well-being” as an indicator in addressing contemporary changes in the nature of work, the workplace, and the workforce.
Further research on burden and enhanced surveillance is needed to develop these elements.
The hazards associated with work have broad national and public health impact; however, the health, economic, and social consequences of occupational and work-related diseases and injuries—the burden resulting from hazards encountered while working—have not been characterized comprehensively. Changes in the nature of work, the workforce, and the workplace have increased the difficulty of such a characterization, and structural and technology-driven shifts in the modern economy require new approaches to assessing the burden of work and work hazards.1–3 Understanding the broad consequences of disease, injury, and distress resulting from work is critical to enabling policymakers and employers to target appropriate levels of resources toward research, prevention, and risk management.3–5
The burden of occupational and work-related diseases, injuries, and distress is the impact of these conditions as measured by morbidity, mortality, disability, economic cost, or other indicators.6–9 The box on the next page shows the major burden indicators of work-related disease, injury, and distress. Estimating this burden is a complex task. Despite indicating significant human tragedy, burden is woefully underestimated in terms of its magnitude, dimensionality, and societal impact. The burden of occupational and work-related disease and injury is underappreciated and not well used in decision-making.4–6
Useful Indicators of Burden of Occupational Disease, Injury, and Distress
| Attributable fraction |
| Morbidity rates and counts (incidence or prevalence based) |
| Mortality rates and counts |
| Fatality rates and counts |
| Injury rates and counts (incidence or prevalence based) |
| Disability rates and counts (incidence or prevalence based) |
| Disability-adjusted life-years (incidence or prevalence based) |
| • Years of life lived with disability |
| • Years of life lost |
| Quality-adjusted life-years |
| Medical costs incurred by workers, families, employers, insurance and disability systems, and society |
| Business costs |
| Productivity losses incurred by workers, families, employers, insurance and disability systems, and society |
Various partial indicators illustrate that the identified burden of work-related disease and injury is substantial.6–13 For example, one study estimated that the United States spent $250 billion in 2007 for medical costs and productivity losses7; another study, which used monetized quality-adjusted life-years to assess reductions of the overall health of the employed population aged 18 to 88, estimated annual costs of $340 billion in the mining sector and $14.8 trillion in the services sector.8 Globally, in 2012, it is estimated that 2.3 million workers died for reasons attributed to work; more than 2 million of those deaths were from diseases.9
Most burden estimates inadequately capture chronic diseases caused or aggravated by work (even if they are fatal), nonfatal diseases or injuries from work exposures, and conditions that are caused by exposures to psychosocial hazards.6,7,9,10 Burden is commonly estimated on the societal level for narrowly defined conditions and is directly tied to specific workplace exposures that have been included in epidemiological studies.6,7 Estimates have not taken into account the burden of disease that may result from all workplace exposures, whether acting alone, in combination with one another, or in conjunction with exposures from other life domains.
Fatal injury estimates, which have been the main driver of burden analyses, are widely considered more accurate than those for nonfatal injury estimates.4–8 Nevertheless, nonfatal occupational injuries and acute illnesses may be at least 5 to 10 times more common than indicated by national statistics.11 Occupational disease and injury statistics have been shown to be influenced by underrecognition, underreporting, and undercounting.4–6
Many diseases are not commonly included in occupational burden analyses because it is difficult to identify the specific exposure or cause of an adverse health effect when the time lag or latency between exposure and disease is years or even decades. Therefore, a large number of adverse health effects, such as musculoskeletal disorders, cancer, and mental health, pulmonary, and cardiovascular diseases and their economic and social impact, are often left out of some burden assessments, as is the broad complex area of work-related distress, which addresses anguish, anxiety, pain, and suffering.4–10
In addition, costs derived from workers’ compensation data do not include the associated “hidden” personal health expenses, wage losses, and Social Security disability benefit payments.5,12 Beyond the consequences of disease and injury that are expressed as cases, rates, costs, and reduction in health-related quality of life metrics, there are many other consequences suffered by workers, their families, employers, and society overall, including the examples given in Figure 1. The burdens in all of these domains have not been assessed comprehensively.
FIGURE 1—
Multiple Domains of Burden of Work-Related Injury, Disease, and Distress
AN APPROACH FOR ASSESSING BURDEN
The approach introduced in the following sections provides perspectives that could be useful in improving burden estimates. This approach is designed to encompass the many dimensions of burden on people and organizations, the resultant burden from different aspects of work and workplace hazards, and the changes that affect burden over a working lifetime. Accounting for all of these aspects of burden individually and comprehensively is the contribution of this approach.
Utilization of Multiple Domains
As noted previously,4–7 a narrow view of burden of occupational disease and injury, with an emphasis on injury, heretofore has been the norm. A more accurate accounting of burden should include a broader range of considerations. The burden of occupational and work-related disease and injury is multidimensional (Figure 1) and substantially affects not only workers but also their families, employers, communities, and society.6,9–13 For each of these groups, the burden occurs in and across many different realms: physical, psychosocial, functional, economic, and legal. Although the burden is generated in the worker’s domain, it spills over to all others. In particular, the burden on workers, their families, and employers is also felt in their communities.11–13 A study of the work-related disease and injury burden in Australia, based on 2008 to 2009 data, showed that the community bore 21% of the economic burden (which included social welfare payments, medical and health scheme costs, and loss of potential output and revenue).13 These issues present a challenge for researchers, public health professionals, and policymakers to gather data of different types from all of the domains of burden, which may include both quantitative measures (such as costs and mortality and morbidity statistics) and qualitative metrics (such as from interviews and focus groups of workers discussing issues such as the impact of emotional stress and pain on their lives).14 Portraying these data coherently and comprehensively will require research and development.2,6,9,10,13,14 Dembe has described a comprehensive approach to assess the complex and multifactorial social consequences of occupational disease and injury, which could serve as the foundation for burden assessments.14
A Broader View of Disease and Injury
To better understand the limitations of current burden estimates, it is helpful to consider terminology commonly used to describe the relationship of work and work hazards to disease, injury, and other adverse health outcomes. Two terms used frequently in the discussion of burden are occupational disease and injury and work-related disease and injury.1,15 The term “occupational disease and injury” is often used to describe morbidity, mortality, and injury caused by single identifiable and measurable physical, chemical, biological, and psychosocial exposures in the workplace and, more recently, the intensification and organization of work. Examples are mesothelioma and coal miners’ pneumoconiosis, conditions which are directly attributable to a workplace exposure to asbestos and coal mine dust, respectively.
The second term, “work-related disease and injury,” is used to describe multifactorial diseases and injuries in which the work environment plays a partial role in causation or leads to the aggravation of any existing disease of nonoccupational origin.15 Examples of work-related disease include musculoskeletal and chronic nonspecific respiratory, mental health, and various cardiovascular disorders.6,7,9,13,15
The spectrum of diseases caused or exacerbated by work can and should be considered, because the associated burden on workers, their families, employers, the community, and society is expected to be large.6–15 Consequently, there is a need for a broader consideration of the interaction of work and nonwork factors.14 Many diseases and injuries experienced by working people are multifactorial, especially as these people age. Many of the health conditions (such as hearing loss and arthritis) most prevalent in workers are not caused solely by workplace hazards.1,15 For counting and attribution purposes, the separation of work and nonwork is artificial, and such compartmentalization leads to undercounting and underreporting of health conditions that are substantially, but not exclusively, related to work. A more comprehensive understanding of burden is required to ensure effective prevention and control.
Accounting for multifactorial hazards where work plays a role requires a comprehensive approach.14 To advance such an approach, combinatorial models have been developed to describe the interaction of occupational and individual risk factors.16 These models describe (1) independent effects, (2) effect modification of an individual risk factor on an occupational exposure–disease association, (3) effect modification of an occupational risk factor on a individual risk factor–disease association, and (4) the interrelationship of 2 or more separate pathways. Additionally, some individual risk factors, such as obesity, can also be the result of workplace risk factors.16
A comprehensive description of burden that includes both the traditional occupational diseases and injuries and those that are work-related is becoming more attainable as concepts of work-related disease and injury evolve.1–3,14,17–19 Integral to various definitions is understanding the extent of the contribution of work.
A critical issue in the use of the concept of work-relatedness is how to assess the role of individual risk factors in diseases or disorders that have multiple interacting risk factors. This is illustrated in public health administrative programs such as the US federal program to compensate cancer victims who worked downwind of atomic bomb tests or in litigation related to injured individuals or groups.20 Various methods have been designed for allocating the total risk among individual risk factors to obtain what has been called the “partial attributable risk.”20 Ideally, work-related burden could be compiled from such a value, as has been done with attributable risk. In considering the total population, assessment of burden of work-related disease and injury requires thinking of the combinatorial patterns of many types of risk factors. The potential to pursue this is challenged by the dearth of data needed to conduct such analyses.
Assessment of the Working-Life Continuum
A rich literature describes the changing nature of work, the workforce, and the workplace.1–3,17–19 To better capture the burden of work-related disease and injury, it is necessary to examine both the occupational and work-related components of burden within the context of an individual’s entire working life.2,21–25 This is the continuum from prework to postwork periods, and it generally involves many jobs and periods of employment.24 US Bureau of Labor Statistics data for workers (born between 1957 and 1969) aged 18 to 48 years indicate that, on average, US workers have 11.7 paying jobs in their lifetime.26 Given that many people start working before the age of 18 years and continue to work well beyond age 48 years, this is likely an underestimate of the number of job changes an individual, particularly ones born in the 21st century, will experience.1,26 On the front end of the continuum, approximately 80% of young people begin working while still in high school, before the age of 18 years. On the back end of the age continuum, the 20th-century trend toward earlier retirement has reversed, and now a growing number of US persons are working longer and later in life.26
According to the Bureau of Labor Statistics, the US labor force will continue to age; the average growth rate of workers aged 55 years and older is projected to increase 1.8% annually, more than 3 times the rate of growth in the overall labor force. The share of the US labor force for workers aged 55 years and older is anticipated to be nearly 25% in 2024 (http://www.bls.gov/opub/mlr/2015/article/labor-force-projections-to-2024-1.htm). In addition, workers often do not immediately switch from one job to the next, so they will likely experience multiple pre- and postemployment periods throughout their working lives. On average, during ages 18 through 48 years, workers will have 5.6 periods of unemployment; the length, duration, and frequency of unemployment increases as educational level decreases (https://www.bls.gov/nls/nlsfaqs.htm).1 However, it is clear that many people will be in and out of work over their working lives, which can be stressful and possibly have various health and psychosocial effects.2,18,19 The discontinuities and distresses of working life are “hazards” of work. They can result in adverse health effects and need to be considered along with traditional occupational safety and health hazards.21–24
Furthermore, approximately 93 million US persons aged 16 years or older were not in the workforce in 2015 (http://www.bls.gov/news.release/pdf/empsit.pdf), mainly because of retirement, school, and disability (http://www.data.bls.gov/timeseries/LNS//300000). However, individuals in each of these unemployment categories may move in and out of the labor force.18,23,24
In addition to periods of unemployment, many workers face underemployment. This is defined as not having enough adequately paid work or not doing work that makes full use of skills or abilities. Friedland and Price delineate 4 categories of underemployment:
Hours-based—involuntarily working less than full-time,
Income-based—a less-than-livable wage even if working full-time,
Skill-based—a job that does not enable skills and training to be used, and
Status-based—a job that provides less job status than expected on the basis of background.25
Income-based underemployment has been particularly identified as a potential occupational health hazard.27
It is also important to consider the impact on workers of some nonstandard employment arrangements and of “precarious employment,” which is defined as an insecure relation to work.1–3,17–19 The potential effects of different employment arrangements are poorly understood, but evidence related to some of these effects is accumulating.3,17–19
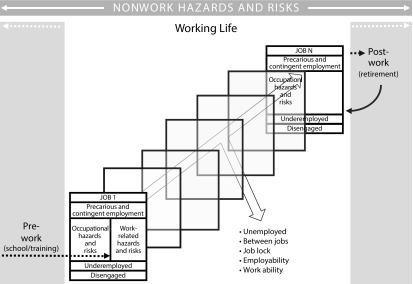
As depicted in Figure 2,28 working life is a dynamic continuum that spans all periods of employment, unemployment, and underemployment, as well as the time before entering the workforce and after retirement.2,24,28 Within the context of each job, 4 factors may affect health and overall well-being: occupational hazards and risks, work-related hazards and risks, effects of unemployment or underemployment, and effects of different employment arrangements. The movement in and out of employment depends on many factors pertaining to the individual and the labor market. Ingress and egress factors can be brought together in a concept known as “employability,” which emerged in the early 20th century in the United States and Europe and is a concept that accounts for the full range of personal and external factors in preventing or enabling job seekers to obtain work.29 This definition ties employability to the other factors and conditions in Figure 2 and, ultimately, to the burden of work-related disease and injury—including work-related stress—that is associated with employment and unemployment.
FIGURE 2—
Working-Life Continuum
The diminished potential to succeed in work is also an important factor in considering burden. This has been characterized by the concept of “work ability,” which was developed in Finland in the 1980s.30 It addresses the questions, “How good is the worker at present, in the near future and how able is he or she to do his or her work with respect to work demands, health, and mental resources?”30 The promotion of work ability has been shown to have an impact on such outcomes as rehabilitation of musculoskeletal disorders, successful aging, and productivity.30
In addition to occupational and work-related disease and injury, it is well established that unemployment itself is a source of ill health and has adverse physical and mental health effects.22–24 According to 1 study, job loss increases the odds of fair or poor health by 54% and the odds of developing new health conditions among those with no preexisting conditions by 83%.22 The association between unemployment and health is likely to be bidirectional: unemployment may cause poor health and poor health may increase the likelihood of unemployment.31 Underemployment appears to have health effects similar to those of unemployment.24
The lack of access to fringe benefits, including health insurance, can also adversely affect workers’ health and hence contribute to burden. The 2010 Affordable Care Act increased the number of Americans with access to health insurance by expanding Medicaid and providing tax credits and cost-sharing reductions to make private insurance coverage affordable, as well as eliminating the ability of insurers to deny or restrict coverage on the basis of preexisting conditions.32 Currently, the ability to get insurance coverage is no longer dependent on having a job that provides employer-sponsored insurance. In the first 3 months of 2016, on average, 8.6% of US persons lacked health insurance, down from 16.0% in 2010.32 Having health insurance is associated with many factors, including an individual’s occupation and the industry in which they work. For example, in one study, construction workers were more likely to be uninsured (25.2%) than workers in any other sector, and Hispanic workers and workers in small businesses accounted for the highest number of uninsured workers.33 Lack of health insurance affects whether and when people get preventative care and necessary medical care and, ultimately, how healthy they are.33 Access to health insurance is also linked to job mobility.34 Consequently, workers may be dissuaded from leaving their position because the new one may involve a new health care provider, different costs, coverage limits, and deductibles.34 Limited job mobility may add to the pressures a worker experiences and may affect the quality of working life and productivity.
In assessing burden, all components of working life need to be considered and investigated. In Figure 2, it is possible to envision 3 streams of health effects: those from (1) employment (occupational diseases and injuries, work-related diseases and injuries); (2) underemployment, disengagement, precarious employment, or job lock; and (3) unemployment. These effects may all be manifested at the time they first occur, but they also may carry over from one job to the next and be cumulative. Despite evidence to support these ideas, carryover and accumulating effects are hypotheses that require further investigation and research.18 Additionally, it is important to note that in Figure 2, the categories in each box have different dimensions and are used as examples in the absence of a more comprehensive system of classification of different employment arrangements. In addition, under each one of the existing categories in the jobs in Figure 2, a worker may or may not have a living wage or access to a variety of fringe benefits, which may also contribute to overall burden.
“Well-Being” as a Burden Indicator
The interactions of risk factors that can be derived from the 4 combinatorial models to address occupational and work-related diseases and injuries (described in section “A Broader View of Work-Related Disease and Injury”) may be too narrow to capture the full impact of the changing nature of work, the workforce, and the workplace.16 A more comprehensive indicator is needed. The concept of “well-being” has been suggested as a possible comprehensive burden indicator when it is lacking or absent altogether.35 However, this approach presents challenges because there is no consensus on how to define well-being for burden applications, and it is rarely defined for functional use.35 Well-being has been broadly conceptualized as flourishing and aspiring to a good life; it has been characterized by happiness, life satisfaction, positive emotion, and self-determination. It includes health, but it goes beyond that and has been linked to individual, enterprise, and national productivity, lower health care costs, reduced injury and illness, and lower rates of absenteeism and presenteeism.10,35 If well-being is to be a useful concept in occupational safety and health burden assessments, there are definitional questions to address as well as complex methodological issues to resolve about how to capture differences over time and among people.35 Consideration of well-being and the lack or absence of it may be what is needed to identify the appropriate parameters related to work, workplace hazards, and individual risk factors that lead to burden for workers, their families, employers, communities, and society. The challenge is how to institute well-being determinations on an ongoing basis and how to interpret differences in well-being among individuals and groups in relation to their work.
RESEARCH NEEDS
Developing a comprehensive approach to burden will depend on achieving a more far-reaching and complete quantification of burden and formulating ways to communicate it effectively. Of particular importance is how to attribute and quantify the adverse effects of exposures to work and work-related hazards over a life course. The box on the next page lists some major information and research needs for each element of burden included in the approach. Ultimately, the critical question is how to integrate all these measures of burden.
Important Research and Data Needs in Each Element of the Burden Approach
| Multiple Domains |
|
| Broader View of Work-Relatedness |
|
| Entire Working-Life Continuum |
|
| Well-Being as an Indicator |
|
PERSPECTIVE
The actual burden of occupational and work-related disease and injury needs to be more thoroughly investigated and communicated before it can fully inform policy considerations at both the workplace and public policy levels. The issues that arise from inadequate burden estimation limit the ability of decision-makers to initiate and prioritize targeted interventions and result in an inability to evaluate the effectiveness of those interventions.4,36 Ultimately, the importance of documenting burden is to use it to plan investment in occupational safety and health risk prevention, risk management, and research and to prompt decision-makers to allocate funds for such investments. Understanding of the extent of occupational and work-related disease and injury burden, and more clearly and widely communicating this burden, will better inform decision-making.
The importance of understanding the interaction between work and nonwork is increasingly supported.9 There might, however, be concerns that attention to nonwork factors dilutes precious resources dedicated to traditional occupational safety and health issues and that attention may be shifted from the employer’s responsibility of providing a safe and healthy workplace to an individual worker’s personal risk factors.37 The consideration of occupational and personal risk factors must be predicated on “the primacy of traditional health protection which prioritizes employer responsibilities for the organization of work over individual health behaviors.”38(p346)
The concerns about the interaction of work and nonwork factors could be addressed by having an accurate and comprehensive understanding of burden, to ensure appropriate focus on controlling or eliminating workplace exposures to better address both occupational and work-related disease and injury and to sustain the health and well-being of workers.38 Although a comprehensive view of the burden of occupational and work-related injuries and disease is an important objective, it should always be recognized that underlying this burden is the inherent right of workers to a safe and healthy workplace and that investments and controls need to be provided regardless of burden calculations.39
There are several reasons why the various sources of burden are not viewed comprehensively and are underreported. First, the current investment—intellectual, academic, and economic—may not be sufficient to advance burden assessments. In particular, the quality and quantity of data that would be useful in burden estimation are inadequate. A lack of multifactorial and multilevel research minimizes not only the availability of appropriate data for use in burden calculations but also the pressure to invest in collecting a broad range of burden statistics. Moreover, the availability of different types of burden data will depend on the extent to which surveillance, archival, and other infrastructural resources are funded and developed.
Second, developing standardized methods to integrate different types of burden data in composite indicators remains a challenge.40 It may be that developing a composite indicator of burden is not feasible in some cases. However, even presentation of multiple burden metrics, such as in a summarized “dashboard” fashion, is useful and should be considered. Progress can be made if there is a more concerted effort to develop comprehensive burden indicators. Researchers in occupational safety and health and related fields, such as the sociology of work, organizational psychology, economics, political science, and human resources, could more forcefully portray the full magnitude and extent of the burden of work, work hazards, work life, and their impact on public health and national welfare.
In summary, decision-makers on the enterprise and societal levels are not widely aware of the burden of work-related injury, illness, and distress, and therefore have not moved to support the need to address these issues in a comprehensive way, even though existing partial estimates of the burden—particularly economic ones—related to work and work-related hazards have shown it to be significant.6–12 However, worldwide attention to these burden issues is growing.9–13,19,21 Further utilization of the approach we describe could lead to the development of a more comprehensive understanding of the burden of work and workplace hazards and provide useful information for enterprise and national investment priorities.
ACKNOWLEDGMENTS
We thank Frank Pot, Knut Ringen, Allard Dembe, Lauren Menger-Ogle, Sergio Iavicoli, and Sheldon Samuels for comments on earlier drafts and Seleen Collins, Nicole Romero, and Amanda Keenan for support in preparing the article.
HUMAN PARTICIPANT PROTECTION
Because no human participants were involved in this research, no protocol approval was needed.
REFERENCES
- 1.Cappelli P, Keller JR. Classifying work in the new economy. Acad Manage Rev. 2013;38(4):575–596. [Google Scholar]
- 2.Amick BC, McLeod CB, Bültmann U. Labor markets and health: an integrated life course perspective. Scan J Work Environ Health. 2016;42(4):346–353. doi: 10.5271/sjweh.3567. [DOI] [PubMed] [Google Scholar]
- 3.Howard J. Nonstandard work arrangements and worker health and safety. Am J Ind Med. 2017;60(1):1–10. doi: 10.1002/ajim.22669. [DOI] [PubMed] [Google Scholar]
- 4.Rosenman KD, Kalush A, Reilly MJ, Gardiner JC, Reeves M, Luo Z. How much work-related injury and illness is missed by the current national surveillance system? J Occup Environ Med. 2006;48(4):357–365. doi: 10.1097/01.jom.0000205864.81970.63. [DOI] [PubMed] [Google Scholar]
- 5.Spieler EA, Wagner GR. Counting matters: implications of undercounting in the BLS survey of occupational injuries and illness. Am J Ind Med. 2014;57(10):1077–1084. doi: 10.1002/ajim.22382. [DOI] [PubMed] [Google Scholar]
- 6.Schulte PA. Characterizing the burden of occupational injury and disease. J Occup Environ Med. 2005;47(6):607–622. doi: 10.1097/01.jom.0000165086.25595.9d. [DOI] [PubMed] [Google Scholar]
- 7.Leigh JP. Economic burden of occupational injury and illness in the United States. Milbank Q. 2011;89(4):728–772. doi: 10.1111/j.1468-0009.2011.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tolbert DV, McCollister KE, LeBlanc WG, Lee DJ, Fleming LE, Muennig P. The economic burden of disease by industry: differences in quality-adjusted life years and associated costs. Am J Ind Med. 2014;57(7):757–763. doi: 10.1002/ajim.22322. [DOI] [PubMed] [Google Scholar]
- 9.Takala J, Hämäläinen P, Saarela KL et al. Global estimates of injury and illness at work in 2012. J Occup Environ Hyg. 2014;11(5):326–337. doi: 10.1080/15459624.2013.863131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cocker F, Martin A, Scott J, Venn A, Sanderson K. Psychological distress, related work attendance, and productivity loss in small-to-medium enterprise owner/managers. Int J Environ Res Public Health. 2013;10(10):5062–5082. doi: 10.3390/ijerph10105062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joe L, Roisman R, Beckmer S et al. Using multiple data sets for public health tracking of work-related injuries and illnesses in tracking of work-related injuries and illnesses in California. Am J Ind Med. 2014;57(10):1110–1119. doi: 10.1002/ajim.22361. [DOI] [PubMed] [Google Scholar]
- 12.O’Leary P, Boden LI, Seabury SA, Ozonoff A, Scherer E. Workplace injuries and the take-up of Social Security disability benefits. Soc Secur Bull. 2012;72(3):1–17. [PubMed] [Google Scholar]
- 13.The Cost of Work-Related Injury and Illness for Australian Employers, Workers, and the Community 2008–09. Canberra, Australia: Safe Work Australia; 2012. [Google Scholar]
- 14.Dembe AE. The social consequences of occupational injuries and illnesses. Am J Ind Med. 2001;40(4):403–417. doi: 10.1002/ajim.1113. [DOI] [PubMed] [Google Scholar]
- 15.el Batawi MA. Work-related diseases. A new program of the World Health Organization. Scand J Work Environ Health. 1984;10(6 spec no.):341–346. doi: 10.5271/sjweh.2309. [DOI] [PubMed] [Google Scholar]
- 16.Schulte PA, Pandalai S, Wulsin V, Chun H. Interaction of occupational and personal risk factors in workforce safety and health. Am J Public Health. 2012;102(3):434–448. doi: 10.2105/AJPH.2011.300249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cummings KJ, Kreiss K. Contingent workers and contingent health: risks of a modern economy. JAMA. 2008;299(4):448–450. doi: 10.1001/jama.299.4.448. [DOI] [PubMed] [Google Scholar]
- 18.Sirviö A, Ek E, Jokelainen J, Koiranen M, Järvikoski T, Taanila A. Precariousness and discontinuous work history in association with health. Scand J Public Health. 2012;40(4):360–367. doi: 10.1177/1403494812450092. [DOI] [PubMed] [Google Scholar]
- 19.László KD, Pikhart H, Kopp MS et al. Job insecurity and health: a study of 16 European countries. Soc Sci Med. 2010;70(6):867–874. doi: 10.1016/j.socscimed.2009.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Price B, MacNicoll M. Multiple interacting risk factors: on methods for allocating risk factor interactions. Risk Anal. 2015;35(5):931–940. doi: 10.1111/risa.12309. [DOI] [PubMed] [Google Scholar]
- 21.Virtanen P. The health effects of employment. Occup Environ Med. 2014;71(10):665–666. doi: 10.1136/oemed-2014-102143. [DOI] [PubMed] [Google Scholar]
- 22.Strully KW. Job loss and health in the US labor market. Demography. 2009;46(2):221–246. doi: 10.1353/dem.0.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Janlert U. Unemployment as disease and diseases of the unemployed. Scand J Work Environ Health. 1997;23(suppl 3):79–83. [PubMed] [Google Scholar]
- 24.Dooley D. Unemployment, underemployment, and mental health: conceptualizing employment status as a continuum. Am J Community Psychol. 2003;32(1–2):9–20. doi: 10.1023/a:1025634504740. [DOI] [PubMed] [Google Scholar]
- 25.Friedland DS, Price RH. Underemployment: consequences for the health and well-being of workers. Am J Community Psychol. 2003;32(1–2):33–45. doi: 10.1023/a:1025638705649. [DOI] [PubMed] [Google Scholar]
- 26.Bureau of Labor Statistics. Number of jobs held, labor market activity and earnings growth among the youngest baby boomers: results of a longitudinal survey. BLS News Release. USDL-15-0528. March 31, 2015. Available at: https://www.bls.gov/news.release/nlsoy.nr0.htm. Accessed May 12, 2017.
- 27.Leigh JP, De Vogli R. Low wages as occupational health hazards. J Occup Environ Med. 2016;58(5):444–447. doi: 10.1097/JOM.0000000000000717. [DOI] [PubMed] [Google Scholar]
- 28. Schulte PA. The burden of occupational injuries and disease. Paper presented at: 50th Anniversary of the Department of Environmental Health; October 2015; University of Cincinnati, Cincinnati, OH.
- 29.McQuaid RW, Lindsay C. The concept of employability. Urban Stud. 2005;42(2):197–219. [Google Scholar]
- 30.Ilmarinen J, Tuomi K, Seitsamo J. New dimensions of work ability. In: Costa G, Goedhard WJA, Ilmarinen J, editors. Assessment and Promotion of Work Ability, Health and Well-Being of Ageing Workers. Amsterdam, Netherlands: Elsevier; 2005. pp. 3–7. [Google Scholar]
- 31.Schuring M, Mackenbach J, Voorham T, Burdorf A. The effect of re-employment on perceived health. J Epidemiol Community Health. 2011;65(7):639–644. doi: 10.1136/jech.2009.103838. [DOI] [PubMed] [Google Scholar]
- 32.Gruessner V. Affordable Care Act reduced uninsurance to 8.6% in 2016. Health Payer Intelligence. Available at: https://healthpayerintelligence.com. Accessed September 28, 2016.
- 33.Wang T, Largay JA, Dong XS. Impact of the Affordable Care Act on Health Insurance Coverage and Health Care Utilization Among Construction Workers. CPWR Quarterly Data Report, Fourth Quarter 2015. Silver Spring, MD: CPWR—Center for Construction Research and Training; 2015. [Google Scholar]
- 34.Bailey J, Chorniy A. Employer-provided health insurance and job mobility: did the Affordable Care Act reduce job lock? Contemp Econ Policy. 2016;34(1):173–183. [Google Scholar]
- 35.Schulte PA, Guerin RJ, Schill AL et al. Considerations for incorporating “well-being” in public policy for workers and workplaces. Am J Public Health. 2015;105(8):e31–e44. doi: 10.2105/AJPH.2015.302616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosenman KD, Kica J, Largo T. Completeness of workers’ compensation data in identifying work-related injuries. In: Utterback D, Schnorr TM, editors. Use of Workers’ Compensation Data for Occupational Safety and Health: Proceedings From June 2012 Workshop. Cincinnati, OH: US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2013. pp. 89–95. DHHS (NIOSH) publication 2013–147. [Google Scholar]
- 37.Lax MB. The perils of integrating wellness and safety and health and the possibility of a worker-oriented alternative. New Solut. 2016;26(1):11–39. doi: 10.1177/1048291116629489. [DOI] [PubMed] [Google Scholar]
- 38.Howard J, Chosewood LC, Hudson HL. The perils of integrating wellness and safety and health and the possibility of a worker-oriented alternative [letter to editor] New Solut. 2016 doi: 10.1177/1048291116656631. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 39.Samuels SW. Philosophic perspectives: community, communications, and occupational disease causation. Int J Health Serv. 1998;28(1):153–164. doi: 10.2190/44MR-YPQF-KUKP-NPQY. [DOI] [PubMed] [Google Scholar]
- 40.Hyder AA, Puvanachandra P, Morrow RH. Measuring the health of populations: explaining composite indicators. J Public Health Res. 2012;1(3):222–228. doi: 10.4081/jphr.2012.e35. [DOI] [PMC free article] [PubMed] [Google Scholar]