Abstract
Objectives. To evaluate the impact of the April 2016 7.8-magnitude earthquake in Ecuador on the incidence of Zika virus (ZIKV) cases.
Methods. We used the national public health surveillance system for reportable transmissible conditions and included suspected and laboratory-confirmed ZIKV cases. We compared the number of cases before and after the earthquake in areas closer to and farther from the epicenter.
Results. From January to July 2016, 2234 patients suspected of having ZIKV infection were reported in both affected and control areas. A total of 1110 patients had a reverse transcription-polymerase chain reaction assay, and 159 were positive for ZIKV. The cumulative incidence of ZIKV in the affected area was 11.1 per 100 000 after the earthquake. The odds ratio of having ZIKV infection in those living in the affected area was 8.0 (95% CI = 4.4, 14.6; P < .01) compared with the control area and adjusted for age, gender, province population, and number of government health care facilities.
Conclusions. A spike in ZIKV cases occurred after the earthquake. Patients in the area closest to the epicenter had a delay in seeking care.
Zika virus (ZIKV) infection has reached epidemic proportions in South and Central America, significantly increasing the risk of complications such as Guillain-Barré–like syndrome and microcephaly.1 The main vector for ZIKV transmission is Aedes mosquitoes. However, the current pandemic has shown new modes of transmission: mother to fetus, blood product, and sexual.1
Mosquito-borne diseases have increased in the aftermath of natural disasters in South and Central America2 as a consequence of changes in habitats and increases in mosquito breeding sites.3,4 In the case of ZIKV, meteorological changes related to El Niño are thought to have been the initial trigger of the Zika epidemic in Brazil.5 However, the impact of a larger natural disaster on the ZIKV pandemic is unknown.
On April 16, 2016, Ecuador experienced a devastating 7.8-magnitude earthquake that claimed the lives of 663 people, injured 6274, and displaced 28 775.6 The aim of our study is to compare the association of the earthquake and the number of ZIKV total and pregnancy-related cases in an earthquake-affected area and in control areas with a similar vector distribution.
METHODS
We included all confirmed ZIKV cases in areas affected by the earthquake and in control areas that are similar in elevation, average temperature, proximity to the coast, and population size. We also included suspected ZIKV cases to evaluate the geographic relationship between these cases and those confirmed by laboratory.
The epicenter of the 2016 earthquake was 17 miles south–southeast of Muisne, Esmeraldas, in the northeastern part of the country. The Manabí and Esmeraldas provinces had the most earthquake-related damage, with 705 and 420 destroyed buildings, respectively.7 Before the earthquake, Manabí had 199 health centers and 15 hospitals. After the earthquake, 7 hospitals had major damage and were inoperative.8,9 Almost all earthquake-related deaths in Ecuador were reported in Manabí; the earthquake affected larger urban centers in Manabí than in Esmeraldas, Guayas, and Los Ríos.
Definitions of Earthquake-Affected Areas
We defined the earthquake-affected area as the province of Manabí, which is 30 miles south of the epicenter. The rationale for using only this province was that the roads to Esmeraldas province and the health care facilities most proximal to the epicenter were completely destroyed,10,11 preventing the collection of any confirmatory samples, whereas several facilities in nearby Manabí remained partially operational and accessible by car. Manabí has larger urban areas and more health care facilities and transportation infrastructure than Esmeraldas.
To better evaluate the relationship between earthquake-related damage and ZIKV incidence, we also collected data at the county level. Manabí has 22 counties. We collected the number of earthquake related-deaths in each county from the Ministry of Health (MOH) report.12
Definition of Control Area
We defined the control area as the provinces of Guayas and Los Ríos. These provinces are adjacent to Manabí and are 265 miles and 120 miles from the epicenter, respectively. In both the affected (Manabí) and the control (Guayas and Los Ríos) provinces, the Aedes mosquito is endemic.13 These 3 provinces are at sea level and, hence, below 2000 meters in elevation and with similar meteorological conditions. Compared with Manabí, Guayas has similar proximity to the coast and Los Ríos has similar population size.14–16
Definition of Zika Virus Cases
Ecuador’s MOH maintains a national public health surveillance system for reportable transmissible conditions including ZIKV, chikungunya, dengue, salmonellosis, shigellosis, yellow fever, malaria, leptospirosis, Guillain–Barré, meningitis, rubella, and varicella. Information is collected by MOH health centers and fed into the national database. We conducted a pre–post analysis of the registry for 2016, specifically epidemiological weeks 0 to 29 (January 1–July 26). We defined the pre-earthquake period as the days between epidemiological weeks 0 and 16 (January 1–April 16) and the postearthquake period as the days between epidemiological weeks 17 and 29 (April 17–July 26).
The MOH registry contains all clinically suspected ZIKV cases reported at the time they were seen at the MOH health care facility. The MOH recommended reporting suspected ZIKV cases when a participant experienced a maculopapular pruritic rash with 2 or more of the following symptoms: fever, conjunctivitis, arthralgia, myalgia, and periarticular edema.17
This registry contains the laboratory results for the subset of participants who underwent confirmatory testing. ZIKV became a reportable condition in Ecuador in January 2016. The confirmation test is the reverse transcription–polymerase chain reaction (RT-PCR), which is conducted at the National Institute of Public Health in Guayaquil, Guayas.
We defined incident confirmed ZIKV cases as those who had a positive RT-PCR result for ZIKV. The testing in Ecuador is done using CFX96 and CFX384 real-time RT-PCR systems (Bio-Rad Laboratories, Invitrogen, Hercules, CA). We used oligonucleotides ZIKV 1087/ZIKV 1163 and ZIKV-FAM probe in a final volume of reaction of 25 microliters, according to the Lanciotti protocol.18 The test has a sensitivity of 25 genomic copies per reaction.18 We collected all incident ZIKV cases and pregnancy-related cases. The registry reports pregnancy status at the time of the laboratory testing. It also contains the laboratory results for chikungunya.
Other Variables
We collected demographics from the MOH registry, which included age and gender. We collected the date when the participant first noticed having symptoms and the date on which the blood was drawn for the RT-PCR assay. We report the number of days between these 2 dates. We obtained average populations for the earthquake-affected and control areas from the 2010 Ecuadorian census14–16 and the average number of health care facilities in these areas from the MOH geocoding website.9
Statistical Analysis
We compared baseline characteristics of the suspected and confirmed ZIKV cases between the affected and control areas using the Pearson χ2 statistic for categorical variables and the t test or Kruskal–Wallis test for continuous measures. We calculated the number of cases by epidemiological week and the cumulative incidence per 10 000 and 100 000 of suspected and confirmed ZIKV cases. We used a similar analytical approach to compare incidence of chikungunya cases in affected and control areas.
To determine whether the number of cases differed by affected area and accounted for confounding, we used logistic regression to calculate the odds ratio (OR) of having ZIKV and the corresponding 95% confidence interval (CI). The dependent variable was having a confirmed incident ZIKV case, and the predictor variables were area (affected vs control), age, gender, average population of the province, and number of health care facilities.
To determine the relationship between the extent of earthquake-related destruction (defined as number of earthquake-related deaths) and incident ZIKV cases, we conducted a linear regression to calculate the standardized parameter estimates by county in the affected area.
Analyses were performed using Stata version 12.0 (StataCorp LP, College Station, TX), and all significance tests were 2-tailed.
RESULTS
From January 2016 to July 26, the MOH received reports of 2234 patients suspected of having ZIKV infection in both the affected and the control areas. Sixty seven percent of the suspected cases were among female patients. A total of 1110 patients had a RT-PCR assay (43% of the affected area cases had a RT-PCR assay and 60% of the control area cases had a RT-PCR assay; P < .01). Of those, 159 had a positive RT-PCR for ZIKV. Seventy-eight of the confirmed cases were among female patients. Ninety percent of the positive RT-PCR ZIKV cases were in the affected area.
Table 1 shows the baseline characteristics of the suspected and positive RT-PCR ZIKV patients. The mean age of the suspected ZIKV patients was similar in the affected and control areas (P = .14), but pregnant and nonpregnant women were more likely to be reported to have a suspected (P < .01) case when comparing the affected and control areas. Patients in the affected and control areas with a positive RT-PCR for ZIKV had similar demographics.
TABLE 1—
Baseline Characteristics of Suspected and Confirmed ZIKV Cases Before the April 2016 Ecuador Earthquake: January–July 2016
| Affected Area (Manabí) |
Control Area (Guayas and Los Ríos) |
P |
||||
| Characteristic | Suspected Cases (n = 1373), % or Mean (SD) | RT-PCR Positive ZIKV Cases (n = 143), % or Mean (SD) | Suspected Cases (n = 861), % or Mean (SD) | RT-PCR Positive ZIKV Cases (n = 16), % or Mean (SD) | Suspected Cases | RT-PCR Positive ZIKV Cases |
| Age, y | 26.0 (15.1) | 26.4 (13.4) | 27.0 (15.9) | 32.7 (20.1) | .14 | .13 |
| Female | 70 | 80 | 63 | 58 | .01 | .07 |
| Pregnant | 31 | 55 | 13 | 83 | .01 | .17 |
| Gestational week of pregnant women | 21.4 (9.8) | 21.3 (10) | 20.8 (8.1) | 21.6 (5.4) | .68 | .95 |
| No. of symptom days | 20.3 (14.9) | 50.5 (34.4) | 4.4 (4.9) | 3.7 (32.0) | < .01 | < .01 |
Note. RT-PCR = reverse transcription-polymerase chain reaction; ZIKV = Zika virus.
Source. Ministry of Health national public health surveillance system.
Number of Cases Before and After the Earthquake
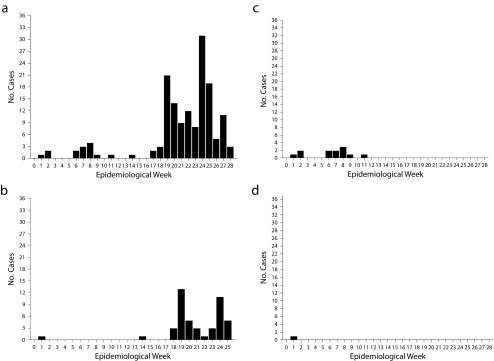
The cumulative incidence of ZIKV cases was 11.1 per 100 000 in the affected area compared with the incidence in the control areas of 1.79 and 0.06 per 100 000 (P < .01). Figure 1 shows the total number of ZIKV cases before and after the earthquake by epidemiological week and area. The affected area had more confirmed ZIKV cases after the earthquake (epidemiological week 16), and the control area had fewer cases after the earthquake (P < .01).
FIGURE 1—
Number of Confirmed Zika Virus Patients by Epidemiological Week Before and After the Earthquake for (a) All Cases in the Affected Area, (b) Pregnant Women in the Affected Area, (c) All Cases in the Control Area, and (d) Pregnant Women in the Control Area: Ecuador, January–July 2016
The same trend was seen for pregnant women (P < .01). Before the earthquake, Patients with cases of ZIKV were similar in age, gender, and pregnancy status (P > .05) to those after the earthquake. After the earthquake, patients took longer to seek medical care—50 days after the start of symptoms compared with 3 days before the earthquake (P < .01). The OR of those living in the affected area having ZIKV infection was 8.0 (95% CI = 4.4, 14.6; P < .01) compared with the control area, adjusted for age, gender, province population, and number of government health care facilities.
Table 2 shows the number of suspected ZIKV cases by county and the number of deaths related to the earthquake. The county with the highest number of deaths (211) had the highest ZIKV incidence per 10 000 (17.50), the second highest number of suspected ZIKV cases (396), and the third highest death rate per 10 000 (9.33). The standardized parameter estimate for the relationship between number of deaths and suspected ZIKV cases was 1.55 (95% CI = 0.71, 2.38; P < .01). The number of chikungunya cases before and after the earthquake did not differ.
TABLE 2—
Incidence of ZIKV in the 22 Counties of the Affected Area (Manabí) by Death Rate: Ecuador, January–July 2016
| Counties in the Affected Area | Population | No. of Deaths | Death Rate per 10 000 | No. of Suspected ZIKV Cases | ZIKV Incidence per 10 000 |
| Bolivar | 40 735 | 11 | 2.70 | 0 | 0.00 |
| Chone | 126 491 | 6 | 0.47 | 0 | 0.00 |
| El Carmen | 89 021 | 7 | 0.70 | 0 | 0.00 |
| Flavio Alfaro | 25 004 | 5 | 2.00 | 0 | 0.00 |
| Jama | 23 253 | 20 | 8.69 | 0 | 0.00 |
| Jaramijo | 18 486 | 0 | 0.00 | 15 | 8.15 |
| Jipijapa | 71 083 | 0 | 0.00 | 44 | 6.19 |
| Junin | 18 492 | 0 | 0.00 | 0 | 0.00 |
| Manta | 226 477 | 211 | 9.33 | 396 | 17.50 |
| Montecristi | 70 294 | 0 | 0.00 | 79 | 11.20 |
| Olmedo | 9 844 | 0 | 0.00 | 0 | 0.00 |
| Pajan | 37 073 | 0 | 0.00 | 0 | 0.00 |
| Pedernales | 55 128 | 173 | 31.3 | 1 | 0.18 |
| Pichincha | 30 244 | 0 | 0.00 | 0 | 0.00 |
| Portoviejo | 280 029 | 133 | 4.70 | 415 | 14.80 |
| Puerto Lopez | 20 451 | 0 | 0.00 | 4 | 2.00 |
| Rocafuerte | 33 469 | 8 | 2.39 | 1 | 0.30 |
| San Vicente | 22 025 | 38 | 17.20 | 3 | 1.36 |
| Santa Ana | 47 385 | 0 | 0.00 | 5 | 1.06 |
| Sucre | 57 159 | 28 | 4.90 | 50 | 8.70 |
| Tosagua | 38 341 | 1 | 0.26 | 0 | 0.00 |
| 24 de Mayo | 28 846 | 0 | 0.00 | 1 | 0.34 |
Note. ZIKV = Zika virus.
Source. Ministry of Health national public health surveillance system.
Pregnant Women and Zika Virus
A total of 538 women had suspected ZIKV infection, and 60 had confirmed ZIKV infection. The ages and weeks of gestation of pregnant women with confirmed ZIKV before the earthquake were similar to that of pregnant women with confirmed ZIKV after the earthquake. However, the mean time to seek medical care was longer after the earthquake (mean ±SD = 41 ±5) than before the earthquake (mean ±SD = 5.4 ±1.9). The OR of pregnant women in the affected area having ZIKV was 30.0 (95% CI = 3.3, 60.5; P < .01) compared with the control area, adjusted for age, province population, and number of government health care facilities.
Geographic Distribution of Suspected and Confirmed Cases
Shown in Figure A (available as a supplement to the online version of this article at http://www.ajph.org), most suspected and confirmed cases occurred in areas proximal to the 2 major cities in the province: Manta and Portoviejo. These 2 cities had high earthquake-related mortality. Nevertheless, most of the coastal areas affected by the earthquake reported suspected cases only. The earthquake-related mortality in these rural coastal areas was lower than in the cities, with the exception of Pedernales, which was closest to the epicenter.
DISCUSSION
We found that the number and cumulative incidence of cases of suspected and confirmed ZIKV among the general population and among pregnant women increased after the April 16, 2016, earthquake in Ecuador. This increase occurred in Manabí, a province significantly affected by the earthquake, but it did not occur in 2 comparable provinces that were not heavily affected. Nevertheless, the increase in reported cases in earthquake-affected areas was not homogeneous. Most of the suspected and confirmed cases originated in counties that suffered significant earthquake-related loss of life and property and that either included or were geographically closer to a large city.
In addition, we found a relationship between the number of earthquake-related deaths and the number of reported ZIKV cases. The majority of confirmed cases occurred among women, and the time to seek medical care was significantly longer in the areas affected by the earthquake. The strengths of the study are the inclusion of suspected, tested, and confirmed ZIKV cases and the use of 2 control provinces with similar population size, geography, and climate.
The present study has several limitations. First, we used national registry data; therefore, the study is subject to information bias. However, any decrease in reporting of ZIKV cases would be more likely to have occurred in the areas affected by the earthquake where the health care infrastructure was destroyed, not in the 2 control provinces that did not experience any damage to health care facilities. Second, only half of the suspected cases had a confirmatory RT-PCR assay, and this differed by province. Nevertheless, we reported suspected cases to provide information on the magnitude of the epidemic and to explore the relationship between suspected and confirmed cases and earthquake-related damage. Manabí had a significantly lower proportion of samples sent for laboratory testing compared with the control provinces, yet a significantly larger proportion of confirmed cases. Given that the testing rate was significantly lower in the earthquake area, excluding nonconfirmed cases most likely underestimated the difference in ZIKV cases between the affected and control areas.
Third, we did not have access to identifiable data and medical records to evaluate the symptoms and clinical presentation of the suspected or confirmed cases. However, all health centers followed MOH guidelines regarding the testing and management of suspected cases. Fourth, the significant delay in seeking care we observed in the affected area may have reduced the sensitivity of the RT-PCR to identifying viral RNA.19 Fifth, we did not include mild cases because they did not attend health care facilities, and we did not have data on them.
Colombia, a country that neighbors the earthquake-affected province of Esmeraldas, had a peak in the number of symptomatic and confirmed cases during January and February 2016 with a subsequent decline. However, this study reported cases through April 2016, limiting our ability to evaluate whether cases increased or not after that month. Nevertheless, our findings suggest that the significant increase in the number of confirmed cases from April to July 2016 occurred exclusively in the earthquake-affected province of Manabí and not in the nonaffected areas to the south and east, and possibly not the Colombian areas to the north. The positive RT-PCR rate in Colombia was 4% for the total population and 12% for pregnant women, whereas in Ecuador it was 10% for the general population and 13% for pregnant women.20
We recognize that we cannot prove causality between earthquakes and ZIKV infection, but the increase in ZIKV incidence may be associated with a number of factors previously linked to disease after natural disasters:
Displacement of populations and overcrowding may increase the exposure to vectors and to infected individuals.21
Destruction of property, sewage, and water infrastructure may increase the number of Aedes aegypti breeding sites.21,22
Stressful conditions increase the susceptibility of the population to developing symptomatic disease by changing the immune status, leading to more symptomatic viral illness.23
Health-seeking behavior increases after a disaster.24
Natural disasters or weather events are not uncommon. In the United States alone, there have been 23 severe storms across 17 states since January 2016 with associated flooding or mudslides that required a major disaster declaration.25 In many of these states, we have previously identified Aedes species26 that may transmit the ZIKV. In Latin America, the Pan-American Health Organization has mobilized resources for 5 major natural disasters since October 2015.27
Our data suggest that the occurrence of a natural disaster in any area below 2000 meters in elevation should prompt the public health system to consider the early deployment of strategies to prevent a ZIKV epidemic. The protection of women of reproductive age should be a priority; we, as well as others, have reported a higher prevalence of ZIKV among women in Latin America.20,28 Reasons for this finding among women include
increased access or reasons to seek health care,
greater exposure to the intradomiciliary mosquito vector,
increased risk of sexual transmission
enhanced reporting given the pregnancy-related risks, and
more severe symptomatology.28
The study’s results allow us to infer that several of these reasons may play a role because in our sample more women than men presented with symptoms of viral illness, more had their samples sent for RT-PCR testing, and more had confirmed cases.
The pattern of reporting ZIKV to the MOH and the delay in seeking care we found after the earthquake indicates several public health concerns. First, earthquake-affected areas that are far from large urban centers may experience an interruption in the mandatory reporting of communicable diseases, impeding the MOH’s ability to identify and react to emerging epidemics.
Second, the significant loss of life and property experienced in communities affected by natural disasters changes patients’ priorities, and those with mild symptoms could delay or withhold seeking care. For example, protecting one’s remaining belongings could become a priority that replaces the need to attend to a health center. Third, ZIKV viremia could last for a long period of time after the onset of symptoms, expanding the window for transmission and the need for public health strategies to address the epidemiological contacts. Fourth, many pregnant women have gotten infected with ZIKV in Ecuador since the April 2016 earthquake.29,30
These findings will inform the MOH on the need to actively collect ZIKV data for the areas closest to the earthquake epicenter where data are still lacking, to consider and deploy strategies to prevent the transmission of ZIKV at the population and individual levels, to educate the public on strategies to protect pregnant women and women of reproductive age, and to prepare for the occurrence of ZIKV complications such as microcephaly and Guillain–Barré syndrome.
In conclusion, our study shows that the April 2016 earthquake in Ecuador was associated with both an increase in the number of ZIKV cases and a significant delay in seeking care in the affected areas. All stakeholders should be aware of the potential increased risk of ZIKV complications after a natural disaster.
HUMAN PARTICIPANT PROTECTION
This research was exempt from institutional review board approval because the data were collected by the Ecuadorean Health Department surveillance system and did not include clinical or personal patient information.
REFERENCES
- 1.Paixão ES, Barreto F, da Glória Teixeira M, da Conceição N, Costa M, Rodrigues LC. History, epidemiology, and clinical manifestations of Zika: a systematic review. Am J Public Health. 2016;106(4):606–612. doi: 10.2105/AJPH.2016.303112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters. Emerg Infect Dis. 2007;13(1):1–5. doi: 10.3201/eid1301.060779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Norris DE. Mosquito-borne diseases as a consequence of land use change. EcoHealth. 2004;1(1):19–24. [Google Scholar]
- 4.Samson DM, Archer RS, Alimi TO et al. New baseline environmental assessment of mosquito ecology in northern Haiti during increased urbanization. J Vector Ecol. 2015;40(1):46–58. doi: 10.1111/jvec.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atif M, Azeem M, Sarwar MR, Bashir A. Zika virus disease: a current review of the literature. Infection. 2016;44(6):695–705. doi: 10.1007/s15010-016-0935-6. [DOI] [PubMed] [Google Scholar]
- 6.Secretaría de Gestión de Riesgos. Informe de situacion N° 71 – 19/05/2016 (20h30) terremoto 7.8 ° - Pedernales. Available at: http://www.gestionderiesgos.gob.ec/wp-content/uploads/downloads/2016/05/INFORME-n71-SISMO-78-20302.pdf. Accessed September 20, 2016.
- 7.Secretaría de Gestión de Riesgos. Informe de situación no. 30 (20/04/2016) 19h30 terremoto 7.8 ° Muisne. Available at: http://www.gestionderiesgos.gob.ec/wpcontent/uploads/downloads/2016/04/Informe-de-Situación-30-20042016-19H30.pdf. Accessed September 20, 2016.
- 8.El terremoto en Ecuador: Daños significativos a los servicios de salud; se desplegaron equipos médicos de emergencia. Desastres: Preparativos y Mitigación en las Américas. 2016;June(121). Available at: http://www.paho.org/disasters/newsletter/index.php?option=com_docman&task=doc_view&Itemid=&gid=132&lang=es. Accessed February 13, 2017.
- 9. Geosalud. Ministerio de Salud Pública. Available at: https://aplicaciones.msp.gob.ec/salud/publico/dniscg/geosalud/gui/index.php#. Accessed February 12, 2017.
- 10.Secretaría de Gestión de Riesgos. Informe de situación no. 57 (03/05/2016) 18H00 Terremoto 7.8 ° Pedernales. Available at: http://www.gestionderiesgos.gob.ec/wp-content/uploads/downloads/2016/05/INFORME-57-DEL-03-05-16-18H00.pdf. Accessed September 19, 2016.
- 11.Organización Panamericana de la Salud. Terremoto en Ecuador: reporte de situación no. 5 al 22 de abril de 2016. Available at: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0ahUKEwiZnsztx57PAhXFMyYKHQynChoQFggcMAA&url=http%3A%2F%2Fwww.paho.org%2Fdisasters%2Findex.php%3Foption%3Dcom_docman%26task%3Ddoc_download%26gid%3D2426%26Itemid%3D%26lang%3Den&usg=AFQjCNFdDtUkbOndjUXe5nIyrY6pkANT7w&bvm=bv.133387755,d.cWw. Accessed September 19, 2016.
- 12.Secretaría de Gestión de Riesgos. Informe de situación no. 57 (03/05/2016) 18H00 Terremoto 7.8 ° Pedernales. Available at: http://www.gestionderiesgos.gob.ec/wp-content/uploads/downloads/2016/05/INFORME-61-DEL-07-05-16H00.pdf. Accessed September 9, 2016.
- 13.Alimi TO, Fuller DO, Quinones ML et al. Prospects and recommendations for risk mapping to improve strategies for effective malaria vector control interventions in Latin America. Malar J. 2015;14:519. doi: 10.1186/s12936-015-1052-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Instituto Nacional de Estadistica y Censos. Fasciculo provincial manabi. Resultados del censo 2010 de poblacion y vivienda en el Ecuador. Available at: http://www.ecuadorencifras.gob.ec//wp-content/descargas/Manu-lateral/Resultados-provinciales/manabi.pdf. Accessed September 19, 2016.
- 15.Instituto Nacional de Estadistica y Censos. Fasciculo provincial guayas. Resultados del censo 2010 de poblacion y vivienda en el Ecuador. Available at: http://www.ecuadorencifras.gob.ec//wp-content/descargas/Manu-lateral/Resultados-provinciales/guayas.pdf. Accessed September 19, 2016.
- 16.Instituto Nacional de Estadistica y Censos. Fasciculo provincial los rios. Resultados del censo 2010 de poblacion y vivienda en el Ecuador. Available at: http://www.ecuadorencifras.gob.ec//wp-content/descargas/Manu-lateral/Resultados-provinciales/los_rios.pdf. Accessed September 19, 2016.
- 17.Pan American Health Organization. World Health Organization. Case definitions. Available at: http://www.paho.org/hq/index.php?option=com_content&view=article&id=11117&Itemid=41532&lang=en. Accessed September 20, 2016.
- 18.Lanciotti RS, Kosoy OL, Laven JJ et al. Genetic and serologic properties of Zika virus associated with an epidemic, Yap state, Micronesia, 2007. Emerg Infect Dis. 2008;14(8):1232–1239. doi: 10.3201/eid1408.080287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haug CJ, Kieny MP, Murgue B. The Zika challenge. N Engl J Med. 2016;374(19):1801–1803. doi: 10.1056/NEJMp1603734. [DOI] [PubMed] [Google Scholar]
- 20.Pacheco O, Beltran M, Nelson CA et al. Zika virus disease in Colombia—preliminary report. N Engl J Med. doi: 10.1056/NEJMoa1604037. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 21.Salazar MA, Pesigan A, Law R, Winkler V. Post-disaster health impact of natural hazards in the Philippines in 2013. Glob Health Action. 2016;9 doi: 10.3402/gha.v9.31320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feng J, Xia Z, Zhang L, Cheng S, Wang R. Risk assessment of malaria prevalence in Ludian, Yongshan, and Jinggu Counties, Yunnan Province, after 2014 earthquake disaster. Am J Trop Med Hyg. 2016;94(3):674–678. doi: 10.4269/ajtmh.15-0624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130(4):601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daniels A, Chapin E, Aspilcueta D, Doocy S. Access to health services and care-seeking behaviors after the 2007 Ica earthquake in Peru. Disaster Med Public Health Prep. 2009;3(2):97–103. doi: 10.1097/DMP.0b013e3181a20328. [DOI] [PubMed] [Google Scholar]
- 25.Disaster Declarations for 2016. Federal Emergency Management Agency. Available at: https://www.fema.gov/disasters/grid/year/2016?field_disaster_type_term_tid_1=7697. Accessed February 13, 2017.
- 26.Zika virus: potential range in US. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/zika/vector/range.html. Accessed September 26, 2016.
- 27.Department of Health Emergencies. Disaster archives. Pan American Health Organization. Available at: http://www.paho.org/disasters/index.php?option=com_content&view=article&id=1933&Itemid=915&lang=en&yr=2016. Accessed September 26, 2016.
- 28.dos Santos T, Rodriguez A, Almiron M et al. Zika virus and the Guillain-Barré syndrome—case series from seven countries. N Engl J Med. 2016;375(16):1598–1601. doi: 10.1056/NEJMc1609015. [DOI] [PubMed] [Google Scholar]
- 29.Driggers RW, Ho CY, Korhonen EM et al. Zika virus infection with prolonged maternal viremia and fetal brain abnormalities. N Engl J Med. 2016;374(22):2142–2151. doi: 10.1056/NEJMoa1601824. [DOI] [PubMed] [Google Scholar]
- 30.Meaney-Delman D, Oduyebo T, Polen KN et al. Prolonged detection of Zika virus RNA in pregnant women. Obstet Gynecol. 2016;128(4):724–730. doi: 10.1097/AOG.0000000000001625. [DOI] [PubMed] [Google Scholar]